Reflection and Reflective Practice in Healthcare: A Report
VerifiedAdded on 2023/01/20
|15
|3845
|34
Report
AI Summary
This report delves into the significance of reflection and reflective practice within the healthcare domain, emphasizing its pivotal role in enhancing professional development and ensuring quality patient care. The assignment begins by defining reflection and its impact on improving clinical practice, highlighting the importance of the code of conduct in guiding healthcare professionals. The core of the report focuses on a critical incident involving a 24-year-old patient admitted to the ICU with flu-like symptoms. The analysis employs the Gibbs reflective cycle, systematically dissecting the incident through description, feelings, evaluation, analysis, conclusion, and action plan stages. The student reflects on the events, their emotions, and the decisions made, leading to a critical evaluation of the actions taken and the identification of areas for improvement. The report concludes with an action plan designed to prevent similar incidents and promote better patient outcomes in the future. This assignment provides a practical application of reflective practice, underscoring its value in learning from experiences and optimizing healthcare delivery.
0
REFLECTION
Student’s Name
Course Studied
Course Code
City
State
Date
REFLECTION
Student’s Name
Course Studied
Course Code
City
State
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
Healthcare professional
Introduction
A Health care professional refers to an individual related to either discipline or
specialty and allowed by specific regulatory bodies to give healthcare services to the ill
people. Health care professionals usually maintain human health through the application of
the necessary principles and procedures of caring and evidence-based medicine. Health care
professionals have several tasks that they perform to ensure good health among the patients.
Besides conducting diagnosis, treatment, and prevention of human diseases, injury and other
mental and physical impairments the healthcare professionals also conduct research, develop
theories, operational methods and concepts to improve the evidence-based healthcare.
Examples of health care professionals include Medical Doctors, Public Health Doctors,
Midwives, Dentists, Pharmacists, and Public Health Nurses. This paper is set to discuss the
importance of reflection and its role in coming up with reflective practice, Perform the
critical incident analysis and application of the reflective model from the identified
significant model, describe the stages of critical incident reflective analysis and the action
plan of the Gibbs reflective cycle in my critical incident analysis.
Task One
Reflection and its role in developing reflective practice
Reflection refers to the process that invites someone to look behind on the most
important events that took place in his/her task and enhancing self-development based on the
challenges faced (Eng, and Pai, 2015). Reflection entails the description of what happened,
the feelings, that is the thought that makes someone feel, and the evaluation which is the
assessment of what is bad and what is good about the experience. The evaluation also
encompasses the analysis which may include thinking differently how things would have
Healthcare professional
Introduction
A Health care professional refers to an individual related to either discipline or
specialty and allowed by specific regulatory bodies to give healthcare services to the ill
people. Health care professionals usually maintain human health through the application of
the necessary principles and procedures of caring and evidence-based medicine. Health care
professionals have several tasks that they perform to ensure good health among the patients.
Besides conducting diagnosis, treatment, and prevention of human diseases, injury and other
mental and physical impairments the healthcare professionals also conduct research, develop
theories, operational methods and concepts to improve the evidence-based healthcare.
Examples of health care professionals include Medical Doctors, Public Health Doctors,
Midwives, Dentists, Pharmacists, and Public Health Nurses. This paper is set to discuss the
importance of reflection and its role in coming up with reflective practice, Perform the
critical incident analysis and application of the reflective model from the identified
significant model, describe the stages of critical incident reflective analysis and the action
plan of the Gibbs reflective cycle in my critical incident analysis.
Task One
Reflection and its role in developing reflective practice
Reflection refers to the process that invites someone to look behind on the most
important events that took place in his/her task and enhancing self-development based on the
challenges faced (Eng, and Pai, 2015). Reflection entails the description of what happened,
the feelings, that is the thought that makes someone feel, and the evaluation which is the
assessment of what is bad and what is good about the experience. The evaluation also
encompasses the analysis which may include thinking differently how things would have
2
been tackled or getting an overall sense of its significance by weighing up the situation.
Finally, evaluation displays the action plan which entails what someone will do if the same
situation happens again in the future. Furthermore, reflection can be used to identify the
weaknesses and strengths allowing enhancement in the progression of areas required to be
improved.
Reflective practice is a basic component of progressing professional development
(Miraglia, and Asselin, 2015; Garneau, 2016). It is also essential to all the healthcare
professionals’ regulatory bodies to retain the registration. However, the reflective practice is
usually represented as an option for health professionals for it to be either reflective or not
about the medical and clinical practice. Reflection ensures health professionals share ideas
and knowledge with their colleagues for the purpose of benefiting the practice and also helps
the medical practitioners to make logic of challenging as well as complicated situations
which help in the improvement of interprofessional relationships and work practice
optimization. For quality improvement of our work, reflection is set to allow objective to
check at our practice.
Reflective practice usually reflects on what someone does. Reflective practice is linked to the
model of learning from experience whereby someone thinks about what he/she did or what
happened and decide on an action plan. Example of reflective practices includes superficial
reflection, deep reflection, and medium reflection. Reflection plays a vital role in clinical
simulation (Husebø, O'Regan, and Nestel, 2015). Self-reflections serves a fundamental role in
improving the nurses' competency (Pai, 2015). There are many different models of reflection
practice they include Graham Gibbs Reflective cycle which outline the structure to learning
from past experiences and the David Kolb’s theory which deals with the cognitive processes
of the learner.
been tackled or getting an overall sense of its significance by weighing up the situation.
Finally, evaluation displays the action plan which entails what someone will do if the same
situation happens again in the future. Furthermore, reflection can be used to identify the
weaknesses and strengths allowing enhancement in the progression of areas required to be
improved.
Reflective practice is a basic component of progressing professional development
(Miraglia, and Asselin, 2015; Garneau, 2016). It is also essential to all the healthcare
professionals’ regulatory bodies to retain the registration. However, the reflective practice is
usually represented as an option for health professionals for it to be either reflective or not
about the medical and clinical practice. Reflection ensures health professionals share ideas
and knowledge with their colleagues for the purpose of benefiting the practice and also helps
the medical practitioners to make logic of challenging as well as complicated situations
which help in the improvement of interprofessional relationships and work practice
optimization. For quality improvement of our work, reflection is set to allow objective to
check at our practice.
Reflective practice usually reflects on what someone does. Reflective practice is linked to the
model of learning from experience whereby someone thinks about what he/she did or what
happened and decide on an action plan. Example of reflective practices includes superficial
reflection, deep reflection, and medium reflection. Reflection plays a vital role in clinical
simulation (Husebø, O'Regan, and Nestel, 2015). Self-reflections serves a fundamental role in
improving the nurses' competency (Pai, 2015). There are many different models of reflection
practice they include Graham Gibbs Reflective cycle which outline the structure to learning
from past experiences and the David Kolb’s theory which deals with the cognitive processes
of the learner.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
The code of conduct displays the expected standard of conduct of social care workers and
support workers. The code outlines the attitude and behavior that should be expected to
experience the signed workers. The code also plays a significant role in directing social
workers to provide safe and quality healthcare services. Health workers have to reflect on
their nursing practices to ensure that their services comply with the standards enshrined
within the code of contact. Therefore, the code of conduct directs medical practitioners on the
expected standards upon the completion of the reflection process.
Part Two
A 24-year-old lady with no reliable medical history presented to ED with flu-like
symptoms. The lady complained of general body pain and had a fever of 37.9. The lady had
been administered on over the counter medicine for the past two weeks without any signs
relief. Instead, the condition worsened leading to breathe shortness and cough.
The abnormal CT scan of the chest revealed elevated white blood count and
abnormality in the functioning of the liver. The physician of the emergency department
admitted the patient to the Intensive Care Unit. The patient was started on oxygen and
antibiotic therapy. During the initial examination, the patients were free from respiratory
distress and responding excellently to the therapy. However, the potassium level (2.9) was
below the normal range (3.5-5.0) as realized by the physician.
The physician ordered the addition of 30mEq of potassium to the intravenous fluid of
the patient (infused at 80ml/hr.). Two days later, the potassium level was at 3.0 which made
the physician to recommend an 80mEq oral administration of potassium. However, the
patient vomited all the medicine, and as a result, the physician ordered the administration of
two doses of 40mEq via the intravenous fluid for four hours.
The code of conduct displays the expected standard of conduct of social care workers and
support workers. The code outlines the attitude and behavior that should be expected to
experience the signed workers. The code also plays a significant role in directing social
workers to provide safe and quality healthcare services. Health workers have to reflect on
their nursing practices to ensure that their services comply with the standards enshrined
within the code of contact. Therefore, the code of conduct directs medical practitioners on the
expected standards upon the completion of the reflection process.
Part Two
A 24-year-old lady with no reliable medical history presented to ED with flu-like
symptoms. The lady complained of general body pain and had a fever of 37.9. The lady had
been administered on over the counter medicine for the past two weeks without any signs
relief. Instead, the condition worsened leading to breathe shortness and cough.
The abnormal CT scan of the chest revealed elevated white blood count and
abnormality in the functioning of the liver. The physician of the emergency department
admitted the patient to the Intensive Care Unit. The patient was started on oxygen and
antibiotic therapy. During the initial examination, the patients were free from respiratory
distress and responding excellently to the therapy. However, the potassium level (2.9) was
below the normal range (3.5-5.0) as realized by the physician.
The physician ordered the addition of 30mEq of potassium to the intravenous fluid of
the patient (infused at 80ml/hr.). Two days later, the potassium level was at 3.0 which made
the physician to recommend an 80mEq oral administration of potassium. However, the
patient vomited all the medicine, and as a result, the physician ordered the administration of
two doses of 40mEq via the intravenous fluid for four hours.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
Due to problematic documentation, I took the instruction differently and administered
two doses of 20mEq in one hour as opposed to the prescription. I recorded the heart rate of
the patient throughout the day but failed to notify the physician. The physician noticed
dropping white blood and platelet count. However, the count war above the normal range.
However, the vital symptoms were within the normal range with no symptoms of respiratory
distress. The physician ordered the pulmonary consult for bronchoscopy but argued that
aggressive pulmonary treatment and vasopressors were not necessary at that time as the
patient was stable. The physician then ordered the transfer of the patient to the High-Density
Unit. My documentation failed to indicate the exact time of transfer. It also failed to validate
that the patient was on cardiac monitor and oxygen therapy during the stay in the intensive
care unit. As a result, the patient arrived in the HDU without the monitor. To worsen the
matter, the HDU unit was not only in an overflow but also the central monitoring station was
not functioning. Shortly after the transfer, the patient became unresponsive and unconscious.
A MET was approached, and a critical response team tried to resuscitate the patient but
failed. The patient went into a cardiac arrest and died.
Part Three
Stages of reflection of Gibbs reflective cycle
The Gibbs Reflective cycle usually encourages individuals to systematically think
about the last experiences they encountered during a specific event, activity or situation. In
diagrammatic representation especially a circle, the reflection on the experiences can also be
demonstrated in phases, and this frequently encourages people to deliberately think about an
event, experience, and activity in detail making them understand well of their actions and
enable them to change and adjust their behavior for their benefit. A complete Gibbs
Due to problematic documentation, I took the instruction differently and administered
two doses of 20mEq in one hour as opposed to the prescription. I recorded the heart rate of
the patient throughout the day but failed to notify the physician. The physician noticed
dropping white blood and platelet count. However, the count war above the normal range.
However, the vital symptoms were within the normal range with no symptoms of respiratory
distress. The physician ordered the pulmonary consult for bronchoscopy but argued that
aggressive pulmonary treatment and vasopressors were not necessary at that time as the
patient was stable. The physician then ordered the transfer of the patient to the High-Density
Unit. My documentation failed to indicate the exact time of transfer. It also failed to validate
that the patient was on cardiac monitor and oxygen therapy during the stay in the intensive
care unit. As a result, the patient arrived in the HDU without the monitor. To worsen the
matter, the HDU unit was not only in an overflow but also the central monitoring station was
not functioning. Shortly after the transfer, the patient became unresponsive and unconscious.
A MET was approached, and a critical response team tried to resuscitate the patient but
failed. The patient went into a cardiac arrest and died.
Part Three
Stages of reflection of Gibbs reflective cycle
The Gibbs Reflective cycle usually encourages individuals to systematically think
about the last experiences they encountered during a specific event, activity or situation. In
diagrammatic representation especially a circle, the reflection on the experiences can also be
demonstrated in phases, and this frequently encourages people to deliberately think about an
event, experience, and activity in detail making them understand well of their actions and
enable them to change and adjust their behavior for their benefit. A complete Gibbs
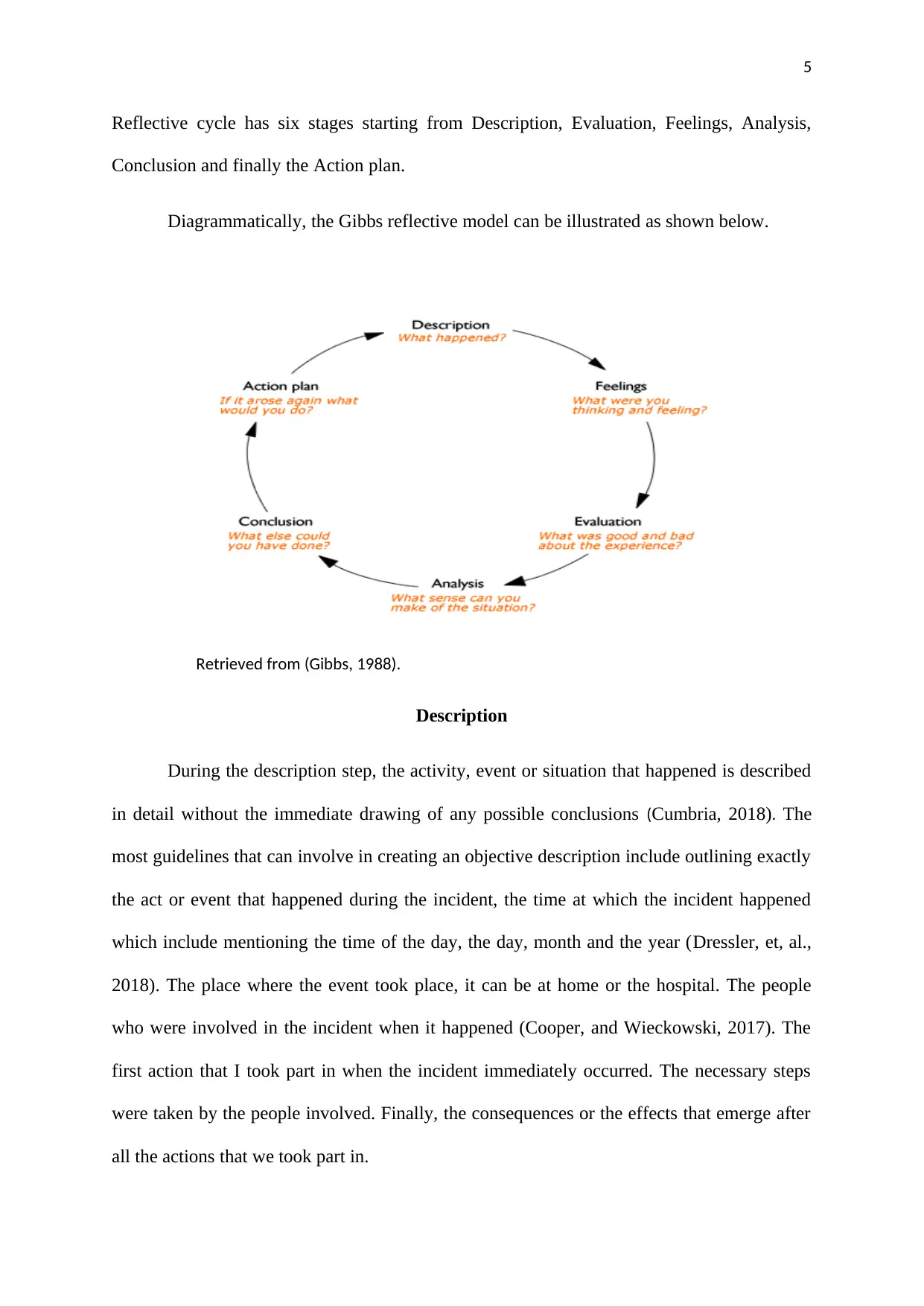
5
Reflective cycle has six stages starting from Description, Evaluation, Feelings, Analysis,
Conclusion and finally the Action plan.
Diagrammatically, the Gibbs reflective model can be illustrated as shown below.
Retrieved from (Gibbs, 1988).
Description
During the description step, the activity, event or situation that happened is described
in detail without the immediate drawing of any possible conclusions (Cumbria, 2018). The
most guidelines that can involve in creating an objective description include outlining exactly
the act or event that happened during the incident, the time at which the incident happened
which include mentioning the time of the day, the day, month and the year (Dressler, et, al.,
2018). The place where the event took place, it can be at home or the hospital. The people
who were involved in the incident when it happened (Cooper, and Wieckowski, 2017). The
first action that I took part in when the incident immediately occurred. The necessary steps
were taken by the people involved. Finally, the consequences or the effects that emerge after
all the actions that we took part in.
Reflective cycle has six stages starting from Description, Evaluation, Feelings, Analysis,
Conclusion and finally the Action plan.
Diagrammatically, the Gibbs reflective model can be illustrated as shown below.
Retrieved from (Gibbs, 1988).
Description
During the description step, the activity, event or situation that happened is described
in detail without the immediate drawing of any possible conclusions (Cumbria, 2018). The
most guidelines that can involve in creating an objective description include outlining exactly
the act or event that happened during the incident, the time at which the incident happened
which include mentioning the time of the day, the day, month and the year (Dressler, et, al.,
2018). The place where the event took place, it can be at home or the hospital. The people
who were involved in the incident when it happened (Cooper, and Wieckowski, 2017). The
first action that I took part in when the incident immediately occurred. The necessary steps
were taken by the people involved. Finally, the consequences or the effects that emerge after
all the actions that we took part in.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
Feelings
This step talks about the feelings triggered by the event and how the thoughts of the
people were during the situation, event or activity which is outlined in the description step
(Mindtools, 2018). The emotions need not be judged or evaluated (Brown, 2016). The most
important aim of this phase is awareness. Helpful guidelines are the feeling that leads up to
the exact event, the feeling during the event, the feelings after the event, someone’s thinking
about other individuals feeling of the event and looking back on the circumstance after it has
happened.
Evaluation
The Evaluation phase is where a person asks himself or herself whether the
experiences of the description step was either good or bad, the well worked approaches and
the approaches that didn’t work well (Husebø, O'Regan, and Nestel, 2015). For a proper
evaluation the following guidelines may apply; the approaches that went well during the
activity or the event and the reason behind that. The approaches that didn't go well during the
event and the reason behind that. The contribution of the person and other people during the
event.
Analysis
The Analysis phase describes what has been learned from the event, activity or
situation (Al-Jubouri, and Al-Jubouri, 2019). Someone get to know what to tackle in similar
situations in the future because of the last experience. The positive and negative occurrences
or problems of someone's experience needs to be written down and personally analyzed.
Conclusion
Feelings
This step talks about the feelings triggered by the event and how the thoughts of the
people were during the situation, event or activity which is outlined in the description step
(Mindtools, 2018). The emotions need not be judged or evaluated (Brown, 2016). The most
important aim of this phase is awareness. Helpful guidelines are the feeling that leads up to
the exact event, the feeling during the event, the feelings after the event, someone’s thinking
about other individuals feeling of the event and looking back on the circumstance after it has
happened.
Evaluation
The Evaluation phase is where a person asks himself or herself whether the
experiences of the description step was either good or bad, the well worked approaches and
the approaches that didn’t work well (Husebø, O'Regan, and Nestel, 2015). For a proper
evaluation the following guidelines may apply; the approaches that went well during the
activity or the event and the reason behind that. The approaches that didn't go well during the
event and the reason behind that. The contribution of the person and other people during the
event.
Analysis
The Analysis phase describes what has been learned from the event, activity or
situation (Al-Jubouri, and Al-Jubouri, 2019). Someone get to know what to tackle in similar
situations in the future because of the last experience. The positive and negative occurrences
or problems of someone's experience needs to be written down and personally analyzed.
Conclusion
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
The "conclusion" phase is where someone asks himself or herself what could have
been done in the event (Oham, Pestano, and Allen, 2016). The information collected earlier
becomes very vital in this phase and encourage the person to come to a useful conclusion.
The conclusion involves mentioning of the positive or negative experience did the activity,
event or situation lead to, the steps the person will take if the activity, situation or event
strikes again in future and the skills the person needs to develop in a similar situation, event
or activity.
Action plan
The action plan is the final step where actions are generated for future events,
situations or activities (Okamoto, et, al., 2017). The intention is usually to keep the promises
that were made in the conclusion step. The courses of action are executed according to how
the events went. If the case went fine, the promises could remain the same, but the strategies
can be amended in a situation where the scenario didn't go well.
Part Four
Description
The description part is as entailed in part two of this paper.
Feeling
Upon receiving the patient, a sense of optimism overwhelmed me. I knew things
would be right. Usually, more complicated incidences occur in the Intensive Care Unit.
Concerning this patient, it was such a minor event. I think a similar feeling was felt by the
other practitioners. My thought in this care expresses their dominance through the physician
who realizes that the patient is responded well to the oxygen and antibiotic therapy.
The "conclusion" phase is where someone asks himself or herself what could have
been done in the event (Oham, Pestano, and Allen, 2016). The information collected earlier
becomes very vital in this phase and encourage the person to come to a useful conclusion.
The conclusion involves mentioning of the positive or negative experience did the activity,
event or situation lead to, the steps the person will take if the activity, situation or event
strikes again in future and the skills the person needs to develop in a similar situation, event
or activity.
Action plan
The action plan is the final step where actions are generated for future events,
situations or activities (Okamoto, et, al., 2017). The intention is usually to keep the promises
that were made in the conclusion step. The courses of action are executed according to how
the events went. If the case went fine, the promises could remain the same, but the strategies
can be amended in a situation where the scenario didn't go well.
Part Four
Description
The description part is as entailed in part two of this paper.
Feeling
Upon receiving the patient, a sense of optimism overwhelmed me. I knew things
would be right. Usually, more complicated incidences occur in the Intensive Care Unit.
Concerning this patient, it was such a minor event. I think a similar feeling was felt by the
other practitioners. My thought in this care expresses their dominance through the physician
who realizes that the patient is responded well to the oxygen and antibiotic therapy.
8
Furthermore, the fact that the patient does not impress any signs and symptoms of respiratory
distress illustrates the optimism among the other practitioners.
My feeling was greatly altered by the proceeding event. The abnormality presented by
the concentration of potassium in the bloodstream of the patient is a fundamental issue. The
potassium level is maintained below the normal range even after addition into the intravenous
fluid. This is a worrying incident as the patient goes to the extent of vomiting the entire
medication that is administered orally. I think the other relevant practitioners felt the same.
For instance, the medical physician in charge of the patients in the intensive care unit tried his
level best but failed to maintain wellbeing in the patient. Additionally, the critical response
team attempted to resuscitate the patients with no success. Towards the end of the incident, I
was sorrowful and felt guilty of incompetence. It was too bad that my ignorance has resulted
in such a messy outcome. I think a similar thought was felt among the other medical
practitioners. The physician in charge of the patient in the intensive care unit failed to make a
follow up to the delivery of health services thus leading to the death of the patient. I expect
any practitioner to regret heavily after having failed in executing her health services.
Evaluation
A few things went right with regard to the incident. A typical example is an excellent
response to oxygen and antibiotic therapy. Secondly, the patient showed no symptoms of
respiratory distress. Diagnosis part of the essay was successful as all the abnormalities were
excellently identified. However, several events didn’t occur as expected. For instance, lower
potassium concentration in the bloodstream of the patients presented a fundamental problem.
The issue was never settled after potassium administration through the intravenous fluid.
Furthermore, the patient vomits all the oral drug administered to her. Also, increasing
Furthermore, the fact that the patient does not impress any signs and symptoms of respiratory
distress illustrates the optimism among the other practitioners.
My feeling was greatly altered by the proceeding event. The abnormality presented by
the concentration of potassium in the bloodstream of the patient is a fundamental issue. The
potassium level is maintained below the normal range even after addition into the intravenous
fluid. This is a worrying incident as the patient goes to the extent of vomiting the entire
medication that is administered orally. I think the other relevant practitioners felt the same.
For instance, the medical physician in charge of the patients in the intensive care unit tried his
level best but failed to maintain wellbeing in the patient. Additionally, the critical response
team attempted to resuscitate the patients with no success. Towards the end of the incident, I
was sorrowful and felt guilty of incompetence. It was too bad that my ignorance has resulted
in such a messy outcome. I think a similar thought was felt among the other medical
practitioners. The physician in charge of the patient in the intensive care unit failed to make a
follow up to the delivery of health services thus leading to the death of the patient. I expect
any practitioner to regret heavily after having failed in executing her health services.
Evaluation
A few things went right with regard to the incident. A typical example is an excellent
response to oxygen and antibiotic therapy. Secondly, the patient showed no symptoms of
respiratory distress. Diagnosis part of the essay was successful as all the abnormalities were
excellently identified. However, several events didn’t occur as expected. For instance, lower
potassium concentration in the bloodstream of the patients presented a fundamental problem.
The issue was never settled after potassium administration through the intravenous fluid.
Furthermore, the patient vomits all the oral drug administered to her. Also, increasing
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
heartbeats are presented despite the normal conditions being normal. Lastly, the patient
experiences a cardiac arrest and dies.
Analysis
Following the incident, documentation is a fundamental crisis. It has come to my
mind that proper documentation is vital for patients’ safety in the nursing profession. I have
realized that ignorance is a vital crisis in the nursing profession. I ignored the increasing
heartbeats of the patient which might have caused the entire problems in the case provided.
Therefore, assumptions need to be avoided for the effective delivery of medical services.
Conclusion
Apart from what I did in the incident provided, I feel proper documentation would
have played a fundamental role in curbing the crisis. Cooperation could have also played a
fundamental role. For instance, telling the physician about the rising heartbeats would have
promoted wellbeing the scenario. The scenario also required knowledge and skills in the
detection and management of body variations. Suppose such happens again in future, I will
execute a proper monitoring and evaluation strategy and bee kin on every alteration of the
patient.
Action
The following strategies shall be implemented in order to promote competency in the
delivery of health care services with regard to the incident discussed above
Action 1: Digitalization (Ommaya, et, al., 2018). The crisis in the incident resulted
from a failure to execute appropriate documentation. Therefore, digitalization shall play a
vital role in promoting documentation in the paper. The manual system of documentation
heartbeats are presented despite the normal conditions being normal. Lastly, the patient
experiences a cardiac arrest and dies.
Analysis
Following the incident, documentation is a fundamental crisis. It has come to my
mind that proper documentation is vital for patients’ safety in the nursing profession. I have
realized that ignorance is a vital crisis in the nursing profession. I ignored the increasing
heartbeats of the patient which might have caused the entire problems in the case provided.
Therefore, assumptions need to be avoided for the effective delivery of medical services.
Conclusion
Apart from what I did in the incident provided, I feel proper documentation would
have played a fundamental role in curbing the crisis. Cooperation could have also played a
fundamental role. For instance, telling the physician about the rising heartbeats would have
promoted wellbeing the scenario. The scenario also required knowledge and skills in the
detection and management of body variations. Suppose such happens again in future, I will
execute a proper monitoring and evaluation strategy and bee kin on every alteration of the
patient.
Action
The following strategies shall be implemented in order to promote competency in the
delivery of health care services with regard to the incident discussed above
Action 1: Digitalization (Ommaya, et, al., 2018). The crisis in the incident resulted
from a failure to execute appropriate documentation. Therefore, digitalization shall play a
vital role in promoting documentation in the paper. The manual system of documentation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
should be replaced with an electronic system to enhance effective documentation.
Implementing this strategy will enable me to effectively follow the prescription of the doctor.
Action 2. Initiating a training and development program (Price, and Reichert, 2017).
Following the incident, it is clear that intensive care unit care requires specific skills and
knowledge (Sweet et al., 2018). Among the skills that are vital in the profession include good
communication skills. In the incident, I failed to communicate the changes in the heartbeat to
the physician. A training and development program promotes the unity of the nursing staff by
preventing violence among nurses (Crombie, Hooker, and Reisenhofer, 2017). Also, the
documentation presented to the High-Density Unit failed to validate that the patient was to
arrive with a monitor. Therefore, developing communication skills is fundamental for proper
adherence to physician prescriptions.
Actions 3: Policy centered care. Ignorance is one of the fundamental problems
curbing medical institutions across the globe. The health care practitioners tend to ignore
small cases which consequently result in fundamental issues. Such assumptions among
nursing professionals risk patients' safety. Therefore, policy-oriented care should be
implemented for wellbeing in society. Medical practitioners who are found guilty of making
assumptions should face the consequences of their outcomes in the court of law.
Action four: Initiating proper monitoring and evaluation strategies (Vinichenko, et,
al., 2016). As from the physician who failed to periodically monitor and evaluate the
performance of the patient, I learned that it is important to make a follow up whenever you
make an order. Furthermore, I will promote unity in the hospital entity for the smooth-
running of operations. I realized whatever is said by the physician is not what will be
implemented by the nursing professionals. Therefore, harmony should be enhanced in
promoting effective delivery of health services thus promotion of patients’ safety.
should be replaced with an electronic system to enhance effective documentation.
Implementing this strategy will enable me to effectively follow the prescription of the doctor.
Action 2. Initiating a training and development program (Price, and Reichert, 2017).
Following the incident, it is clear that intensive care unit care requires specific skills and
knowledge (Sweet et al., 2018). Among the skills that are vital in the profession include good
communication skills. In the incident, I failed to communicate the changes in the heartbeat to
the physician. A training and development program promotes the unity of the nursing staff by
preventing violence among nurses (Crombie, Hooker, and Reisenhofer, 2017). Also, the
documentation presented to the High-Density Unit failed to validate that the patient was to
arrive with a monitor. Therefore, developing communication skills is fundamental for proper
adherence to physician prescriptions.
Actions 3: Policy centered care. Ignorance is one of the fundamental problems
curbing medical institutions across the globe. The health care practitioners tend to ignore
small cases which consequently result in fundamental issues. Such assumptions among
nursing professionals risk patients' safety. Therefore, policy-oriented care should be
implemented for wellbeing in society. Medical practitioners who are found guilty of making
assumptions should face the consequences of their outcomes in the court of law.
Action four: Initiating proper monitoring and evaluation strategies (Vinichenko, et,
al., 2016). As from the physician who failed to periodically monitor and evaluate the
performance of the patient, I learned that it is important to make a follow up whenever you
make an order. Furthermore, I will promote unity in the hospital entity for the smooth-
running of operations. I realized whatever is said by the physician is not what will be
implemented by the nursing professionals. Therefore, harmony should be enhanced in
promoting effective delivery of health services thus promotion of patients’ safety.
11
References
Al-Jubouri, A.H.H., and Al-Jubouri, M.H.M., 2019. The Effectiveness of Teaching in the
Gibbs Model in the Decision-Making to Solve the Environmental Problems among Students
of the College of Education. Indian Journal of Public Health Research &
Development, 10(1), pp.732-736.
Brown, M.M., 2016. Reflective Supervision. Reflective Practice, 10(5), pp.339-420
Cooper, L.D. and Wieckowski, A.T., 2017. A structured approach to reflective practice
training in a clinical practicum. Training and Education in Professional Psychology, 11(4),
p.252.
Crombie, N., Hooker, L. and Reisenhofer, S., 2017. Nurse and midwifery education and
intimate partner violence: a scoping review. Journal of clinical nursing, 26(15-16), pp.2100-
2125.
References
Al-Jubouri, A.H.H., and Al-Jubouri, M.H.M., 2019. The Effectiveness of Teaching in the
Gibbs Model in the Decision-Making to Solve the Environmental Problems among Students
of the College of Education. Indian Journal of Public Health Research &
Development, 10(1), pp.732-736.
Brown, M.M., 2016. Reflective Supervision. Reflective Practice, 10(5), pp.339-420
Cooper, L.D. and Wieckowski, A.T., 2017. A structured approach to reflective practice
training in a clinical practicum. Training and Education in Professional Psychology, 11(4),
p.252.
Crombie, N., Hooker, L. and Reisenhofer, S., 2017. Nurse and midwifery education and
intimate partner violence: a scoping review. Journal of clinical nursing, 26(15-16), pp.2100-
2125.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15