NRSG353 Case Study: Exogenous Cushing Syndrome and Nursing Care
VerifiedAdded on 2023/04/10
|5
|1883
|81
Case Study
AI Summary
This case study comprehensively analyzes Exogenous Cushing Syndrome in a patient, Ms. Maureen Smith, focusing on its causes, incidence, risk factors, and impact on the patient and her family. It discusses three common signs and symptoms—central obesity, hypertension, and hyperglycemia—explaining their underlying pathophysiology. The analysis includes the pharmacodynamics and pharmacokinetics of mifepristone, a relevant drug for managing Cushing's syndrome, and provides a nursing care plan prioritizing patient stabilization, blood pressure management, discontinuation of corticosteroids, mifepristone administration, and patient education. The care plan outlines goals, interventions, and rationales for the first 8 hours post-ward admission, emphasizing the importance of understanding the disease process and treatment regimen. The case study also highlights potential complications and indicators for notifying the physician.
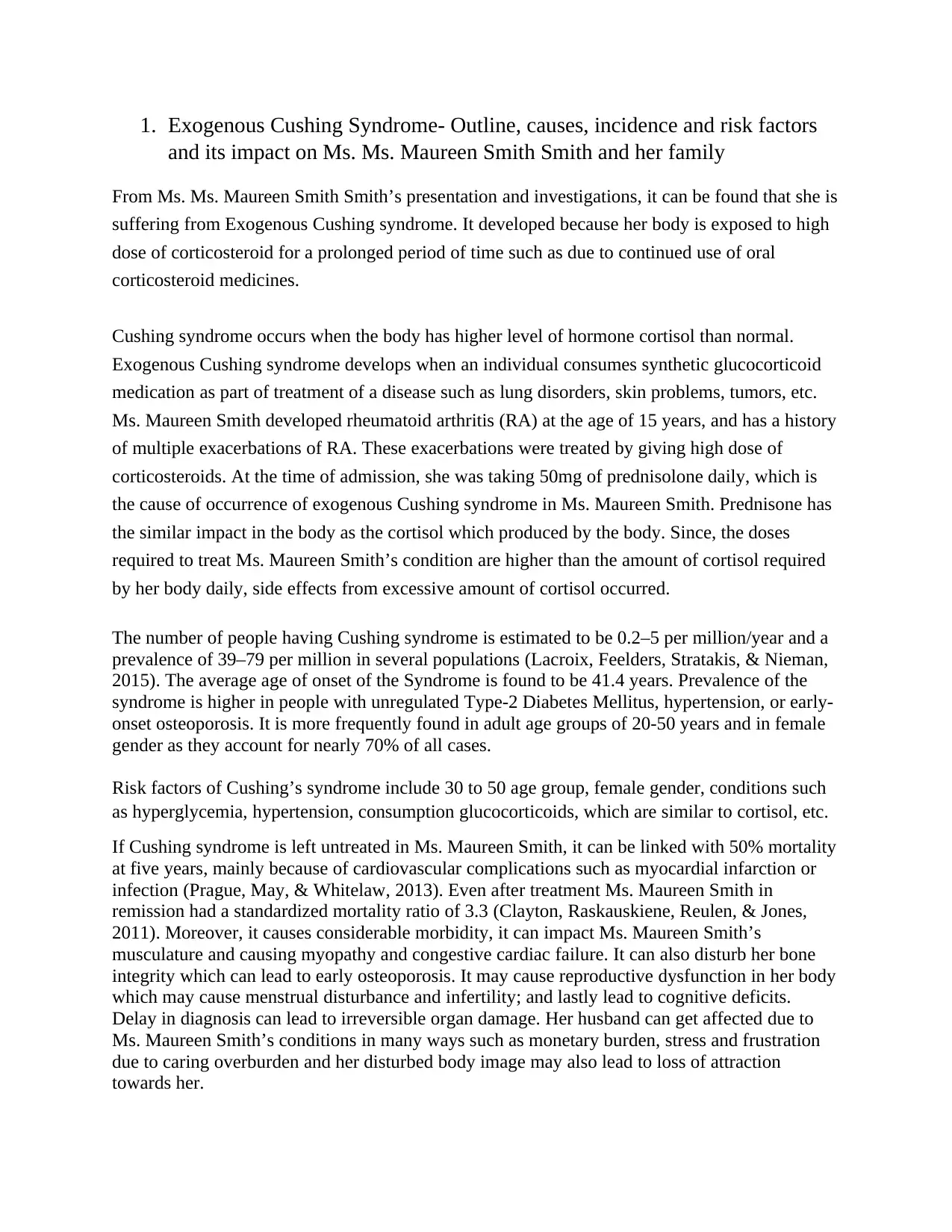
1. Exogenous Cushing Syndrome- Outline, causes, incidence and risk factors
and its impact on Ms. Ms. Maureen Smith Smith and her family
From Ms. Ms. Maureen Smith Smith’s presentation and investigations, it can be found that she is
suffering from Exogenous Cushing syndrome. It developed because her body is exposed to high
dose of corticosteroid for a prolonged period of time such as due to continued use of oral
corticosteroid medicines.
Cushing syndrome occurs when the body has higher level of hormone cortisol than normal.
Exogenous Cushing syndrome develops when an individual consumes synthetic glucocorticoid
medication as part of treatment of a disease such as lung disorders, skin problems, tumors, etc.
Ms. Maureen Smith developed rheumatoid arthritis (RA) at the age of 15 years, and has a history
of multiple exacerbations of RA. These exacerbations were treated by giving high dose of
corticosteroids. At the time of admission, she was taking 50mg of prednisolone daily, which is
the cause of occurrence of exogenous Cushing syndrome in Ms. Maureen Smith. Prednisone has
the similar impact in the body as the cortisol which produced by the body. Since, the doses
required to treat Ms. Maureen Smith’s condition are higher than the amount of cortisol required
by her body daily, side effects from excessive amount of cortisol occurred.
The number of people having Cushing syndrome is estimated to be 0.2–5 per million/year and a
prevalence of 39–79 per million in several populations (Lacroix, Feelders, Stratakis, & Nieman,
2015). The average age of onset of the Syndrome is found to be 41.4 years. Prevalence of the
syndrome is higher in people with unregulated Type-2 Diabetes Mellitus, hypertension, or early-
onset osteoporosis. It is more frequently found in adult age groups of 20-50 years and in female
gender as they account for nearly 70% of all cases.
Risk factors of Cushing’s syndrome include 30 to 50 age group, female gender, conditions such
as hyperglycemia, hypertension, consumption glucocorticoids, which are similar to cortisol, etc.
If Cushing syndrome is left untreated in Ms. Maureen Smith, it can be linked with 50% mortality
at five years, mainly because of cardiovascular complications such as myocardial infarction or
infection (Prague, May, & Whitelaw, 2013). Even after treatment Ms. Maureen Smith in
remission had a standardized mortality ratio of 3.3 (Clayton, Raskauskiene, Reulen, & Jones,
2011). Moreover, it causes considerable morbidity, it can impact Ms. Maureen Smith’s
musculature and causing myopathy and congestive cardiac failure. It can also disturb her bone
integrity which can lead to early osteoporosis. It may cause reproductive dysfunction in her body
which may cause menstrual disturbance and infertility; and lastly lead to cognitive deficits.
Delay in diagnosis can lead to irreversible organ damage. Her husband can get affected due to
Ms. Maureen Smith’s conditions in many ways such as monetary burden, stress and frustration
due to caring overburden and her disturbed body image may also lead to loss of attraction
towards her.
and its impact on Ms. Ms. Maureen Smith Smith and her family
From Ms. Ms. Maureen Smith Smith’s presentation and investigations, it can be found that she is
suffering from Exogenous Cushing syndrome. It developed because her body is exposed to high
dose of corticosteroid for a prolonged period of time such as due to continued use of oral
corticosteroid medicines.
Cushing syndrome occurs when the body has higher level of hormone cortisol than normal.
Exogenous Cushing syndrome develops when an individual consumes synthetic glucocorticoid
medication as part of treatment of a disease such as lung disorders, skin problems, tumors, etc.
Ms. Maureen Smith developed rheumatoid arthritis (RA) at the age of 15 years, and has a history
of multiple exacerbations of RA. These exacerbations were treated by giving high dose of
corticosteroids. At the time of admission, she was taking 50mg of prednisolone daily, which is
the cause of occurrence of exogenous Cushing syndrome in Ms. Maureen Smith. Prednisone has
the similar impact in the body as the cortisol which produced by the body. Since, the doses
required to treat Ms. Maureen Smith’s condition are higher than the amount of cortisol required
by her body daily, side effects from excessive amount of cortisol occurred.
The number of people having Cushing syndrome is estimated to be 0.2–5 per million/year and a
prevalence of 39–79 per million in several populations (Lacroix, Feelders, Stratakis, & Nieman,
2015). The average age of onset of the Syndrome is found to be 41.4 years. Prevalence of the
syndrome is higher in people with unregulated Type-2 Diabetes Mellitus, hypertension, or early-
onset osteoporosis. It is more frequently found in adult age groups of 20-50 years and in female
gender as they account for nearly 70% of all cases.
Risk factors of Cushing’s syndrome include 30 to 50 age group, female gender, conditions such
as hyperglycemia, hypertension, consumption glucocorticoids, which are similar to cortisol, etc.
If Cushing syndrome is left untreated in Ms. Maureen Smith, it can be linked with 50% mortality
at five years, mainly because of cardiovascular complications such as myocardial infarction or
infection (Prague, May, & Whitelaw, 2013). Even after treatment Ms. Maureen Smith in
remission had a standardized mortality ratio of 3.3 (Clayton, Raskauskiene, Reulen, & Jones,
2011). Moreover, it causes considerable morbidity, it can impact Ms. Maureen Smith’s
musculature and causing myopathy and congestive cardiac failure. It can also disturb her bone
integrity which can lead to early osteoporosis. It may cause reproductive dysfunction in her body
which may cause menstrual disturbance and infertility; and lastly lead to cognitive deficits.
Delay in diagnosis can lead to irreversible organ damage. Her husband can get affected due to
Ms. Maureen Smith’s conditions in many ways such as monetary burden, stress and frustration
due to caring overburden and her disturbed body image may also lead to loss of attraction
towards her.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2. Three common signs and symptoms of exogenous Cushing Syndrome and
underlying pathophysiology
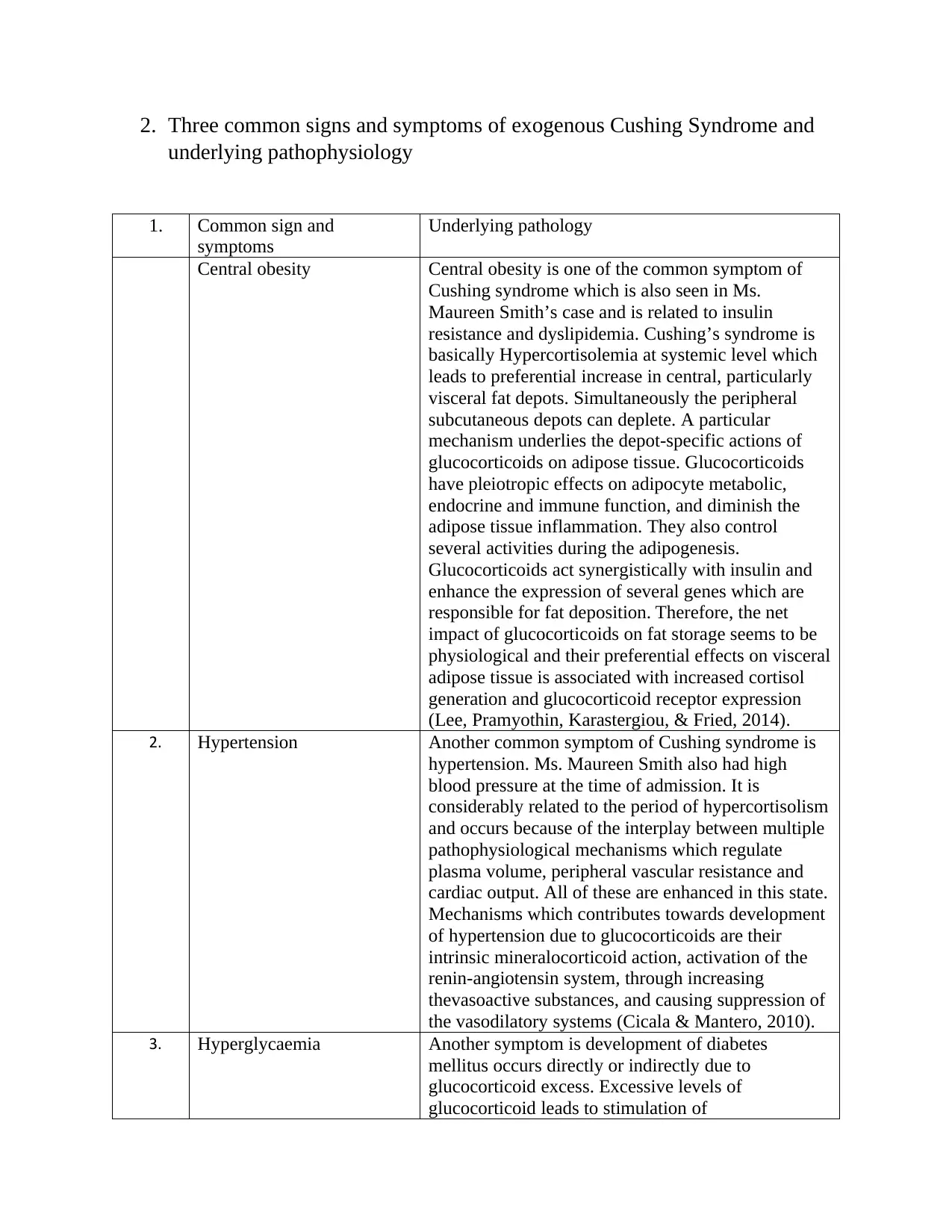
1. Common sign and
symptoms
Underlying pathology
Central obesity Central obesity is one of the common symptom of
Cushing syndrome which is also seen in Ms.
Maureen Smith’s case and is related to insulin
resistance and dyslipidemia. Cushing’s syndrome is
basically Hypercortisolemia at systemic level which
leads to preferential increase in central, particularly
visceral fat depots. Simultaneously the peripheral
subcutaneous depots can deplete. A particular
mechanism underlies the depot-specific actions of
glucocorticoids on adipose tissue. Glucocorticoids
have pleiotropic effects on adipocyte metabolic,
endocrine and immune function, and diminish the
adipose tissue inflammation. They also control
several activities during the adipogenesis.
Glucocorticoids act synergistically with insulin and
enhance the expression of several genes which are
responsible for fat deposition. Therefore, the net
impact of glucocorticoids on fat storage seems to be
physiological and their preferential effects on visceral
adipose tissue is associated with increased cortisol
generation and glucocorticoid receptor expression
(Lee, Pramyothin, Karastergiou, & Fried, 2014).
2. Hypertension Another common symptom of Cushing syndrome is
hypertension. Ms. Maureen Smith also had high
blood pressure at the time of admission. It is
considerably related to the period of hypercortisolism
and occurs because of the interplay between multiple
pathophysiological mechanisms which regulate
plasma volume, peripheral vascular resistance and
cardiac output. All of these are enhanced in this state.
Mechanisms which contributes towards development
of hypertension due to glucocorticoids are their
intrinsic mineralocorticoid action, activation of the
renin-angiotensin system, through increasing
thevasoactive substances, and causing suppression of
the vasodilatory systems (Cicala & Mantero, 2010).
3. Hyperglycaemia Another symptom is development of diabetes
mellitus occurs directly or indirectly due to
glucocorticoid excess. Excessive levels of
glucocorticoid leads to stimulation of
underlying pathophysiology
1. Common sign and
symptoms
Underlying pathology
Central obesity Central obesity is one of the common symptom of
Cushing syndrome which is also seen in Ms.
Maureen Smith’s case and is related to insulin
resistance and dyslipidemia. Cushing’s syndrome is
basically Hypercortisolemia at systemic level which
leads to preferential increase in central, particularly
visceral fat depots. Simultaneously the peripheral
subcutaneous depots can deplete. A particular
mechanism underlies the depot-specific actions of
glucocorticoids on adipose tissue. Glucocorticoids
have pleiotropic effects on adipocyte metabolic,
endocrine and immune function, and diminish the
adipose tissue inflammation. They also control
several activities during the adipogenesis.
Glucocorticoids act synergistically with insulin and
enhance the expression of several genes which are
responsible for fat deposition. Therefore, the net
impact of glucocorticoids on fat storage seems to be
physiological and their preferential effects on visceral
adipose tissue is associated with increased cortisol
generation and glucocorticoid receptor expression
(Lee, Pramyothin, Karastergiou, & Fried, 2014).
2. Hypertension Another common symptom of Cushing syndrome is
hypertension. Ms. Maureen Smith also had high
blood pressure at the time of admission. It is
considerably related to the period of hypercortisolism
and occurs because of the interplay between multiple
pathophysiological mechanisms which regulate
plasma volume, peripheral vascular resistance and
cardiac output. All of these are enhanced in this state.
Mechanisms which contributes towards development
of hypertension due to glucocorticoids are their
intrinsic mineralocorticoid action, activation of the
renin-angiotensin system, through increasing
thevasoactive substances, and causing suppression of
the vasodilatory systems (Cicala & Mantero, 2010).
3. Hyperglycaemia Another symptom is development of diabetes
mellitus occurs directly or indirectly due to
glucocorticoid excess. Excessive levels of
glucocorticoid leads to stimulation of
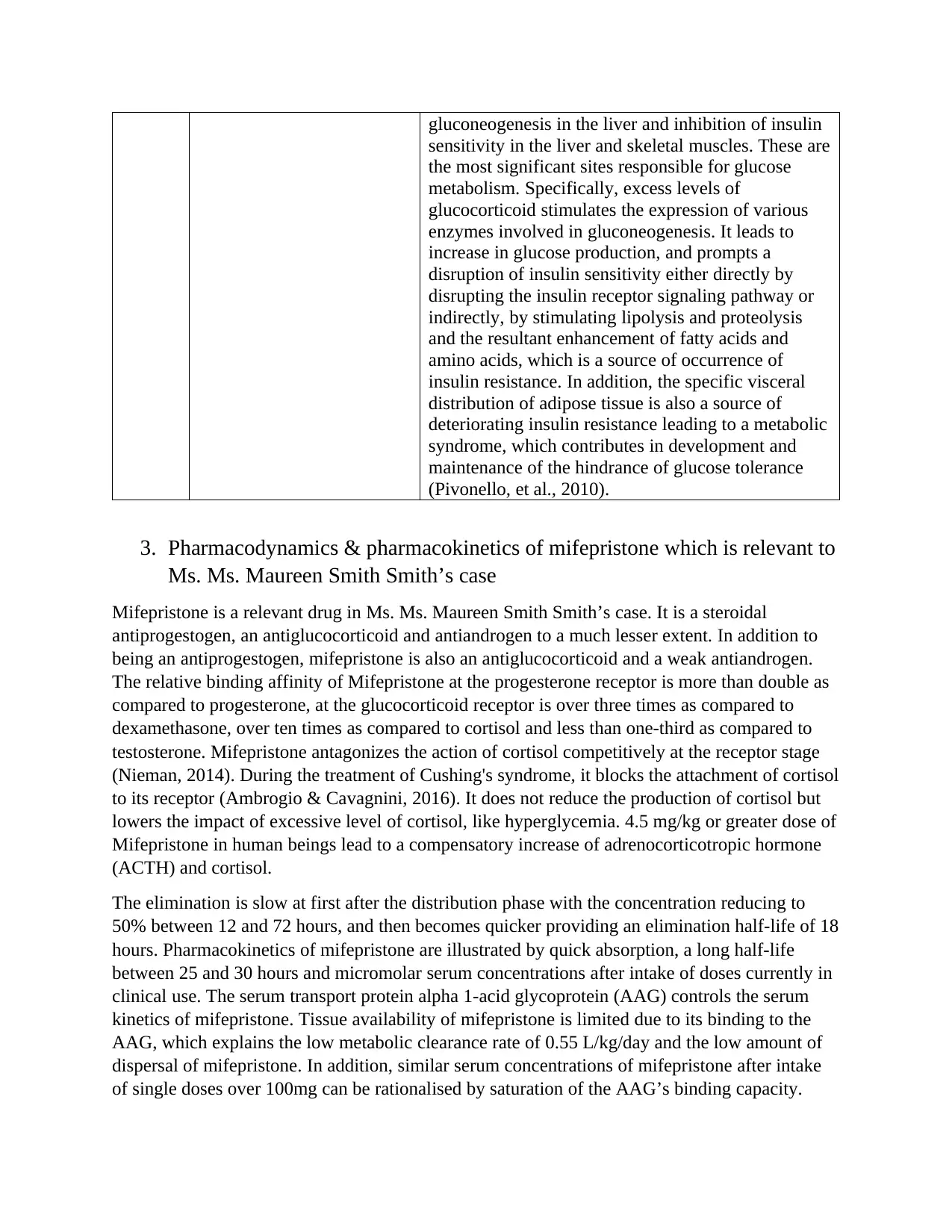
gluconeogenesis in the liver and inhibition of insulin
sensitivity in the liver and skeletal muscles. These are
the most significant sites responsible for glucose
metabolism. Specifically, excess levels of
glucocorticoid stimulates the expression of various
enzymes involved in gluconeogenesis. It leads to
increase in glucose production, and prompts a
disruption of insulin sensitivity either directly by
disrupting the insulin receptor signaling pathway or
indirectly, by stimulating lipolysis and proteolysis
and the resultant enhancement of fatty acids and
amino acids, which is a source of occurrence of
insulin resistance. In addition, the specific visceral
distribution of adipose tissue is also a source of
deteriorating insulin resistance leading to a metabolic
syndrome, which contributes in development and
maintenance of the hindrance of glucose tolerance
(Pivonello, et al., 2010).
3. Pharmacodynamics & pharmacokinetics of mifepristone which is relevant to
Ms. Ms. Maureen Smith Smith’s case
Mifepristone is a relevant drug in Ms. Ms. Maureen Smith Smith’s case. It is a steroidal
antiprogestogen, an antiglucocorticoid and antiandrogen to a much lesser extent. In addition to
being an antiprogestogen, mifepristone is also an antiglucocorticoid and a weak antiandrogen.
The relative binding affinity of Mifepristone at the progesterone receptor is more than double as
compared to progesterone, at the glucocorticoid receptor is over three times as compared to
dexamethasone, over ten times as compared to cortisol and less than one-third as compared to
testosterone. Mifepristone antagonizes the action of cortisol competitively at the receptor stage
(Nieman, 2014). During the treatment of Cushing's syndrome, it blocks the attachment of cortisol
to its receptor (Ambrogio & Cavagnini, 2016). It does not reduce the production of cortisol but
lowers the impact of excessive level of cortisol, like hyperglycemia. 4.5 mg/kg or greater dose of
Mifepristone in human beings lead to a compensatory increase of adrenocorticotropic hormone
(ACTH) and cortisol.
The elimination is slow at first after the distribution phase with the concentration reducing to
50% between 12 and 72 hours, and then becomes quicker providing an elimination half-life of 18
hours. Pharmacokinetics of mifepristone are illustrated by quick absorption, a long half-life
between 25 and 30 hours and micromolar serum concentrations after intake of doses currently in
clinical use. The serum transport protein alpha 1-acid glycoprotein (AAG) controls the serum
kinetics of mifepristone. Tissue availability of mifepristone is limited due to its binding to the
AAG, which explains the low metabolic clearance rate of 0.55 L/kg/day and the low amount of
dispersal of mifepristone. In addition, similar serum concentrations of mifepristone after intake
of single doses over 100mg can be rationalised by saturation of the AAG’s binding capacity.
sensitivity in the liver and skeletal muscles. These are
the most significant sites responsible for glucose
metabolism. Specifically, excess levels of
glucocorticoid stimulates the expression of various
enzymes involved in gluconeogenesis. It leads to
increase in glucose production, and prompts a
disruption of insulin sensitivity either directly by
disrupting the insulin receptor signaling pathway or
indirectly, by stimulating lipolysis and proteolysis
and the resultant enhancement of fatty acids and
amino acids, which is a source of occurrence of
insulin resistance. In addition, the specific visceral
distribution of adipose tissue is also a source of
deteriorating insulin resistance leading to a metabolic
syndrome, which contributes in development and
maintenance of the hindrance of glucose tolerance
(Pivonello, et al., 2010).
3. Pharmacodynamics & pharmacokinetics of mifepristone which is relevant to
Ms. Ms. Maureen Smith Smith’s case
Mifepristone is a relevant drug in Ms. Ms. Maureen Smith Smith’s case. It is a steroidal
antiprogestogen, an antiglucocorticoid and antiandrogen to a much lesser extent. In addition to
being an antiprogestogen, mifepristone is also an antiglucocorticoid and a weak antiandrogen.
The relative binding affinity of Mifepristone at the progesterone receptor is more than double as
compared to progesterone, at the glucocorticoid receptor is over three times as compared to
dexamethasone, over ten times as compared to cortisol and less than one-third as compared to
testosterone. Mifepristone antagonizes the action of cortisol competitively at the receptor stage
(Nieman, 2014). During the treatment of Cushing's syndrome, it blocks the attachment of cortisol
to its receptor (Ambrogio & Cavagnini, 2016). It does not reduce the production of cortisol but
lowers the impact of excessive level of cortisol, like hyperglycemia. 4.5 mg/kg or greater dose of
Mifepristone in human beings lead to a compensatory increase of adrenocorticotropic hormone
(ACTH) and cortisol.
The elimination is slow at first after the distribution phase with the concentration reducing to
50% between 12 and 72 hours, and then becomes quicker providing an elimination half-life of 18
hours. Pharmacokinetics of mifepristone are illustrated by quick absorption, a long half-life
between 25 and 30 hours and micromolar serum concentrations after intake of doses currently in
clinical use. The serum transport protein alpha 1-acid glycoprotein (AAG) controls the serum
kinetics of mifepristone. Tissue availability of mifepristone is limited due to its binding to the
AAG, which explains the low metabolic clearance rate of 0.55 L/kg/day and the low amount of
dispersal of mifepristone. In addition, similar serum concentrations of mifepristone after intake
of single doses over 100mg can be rationalised by saturation of the AAG’s binding capacity.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
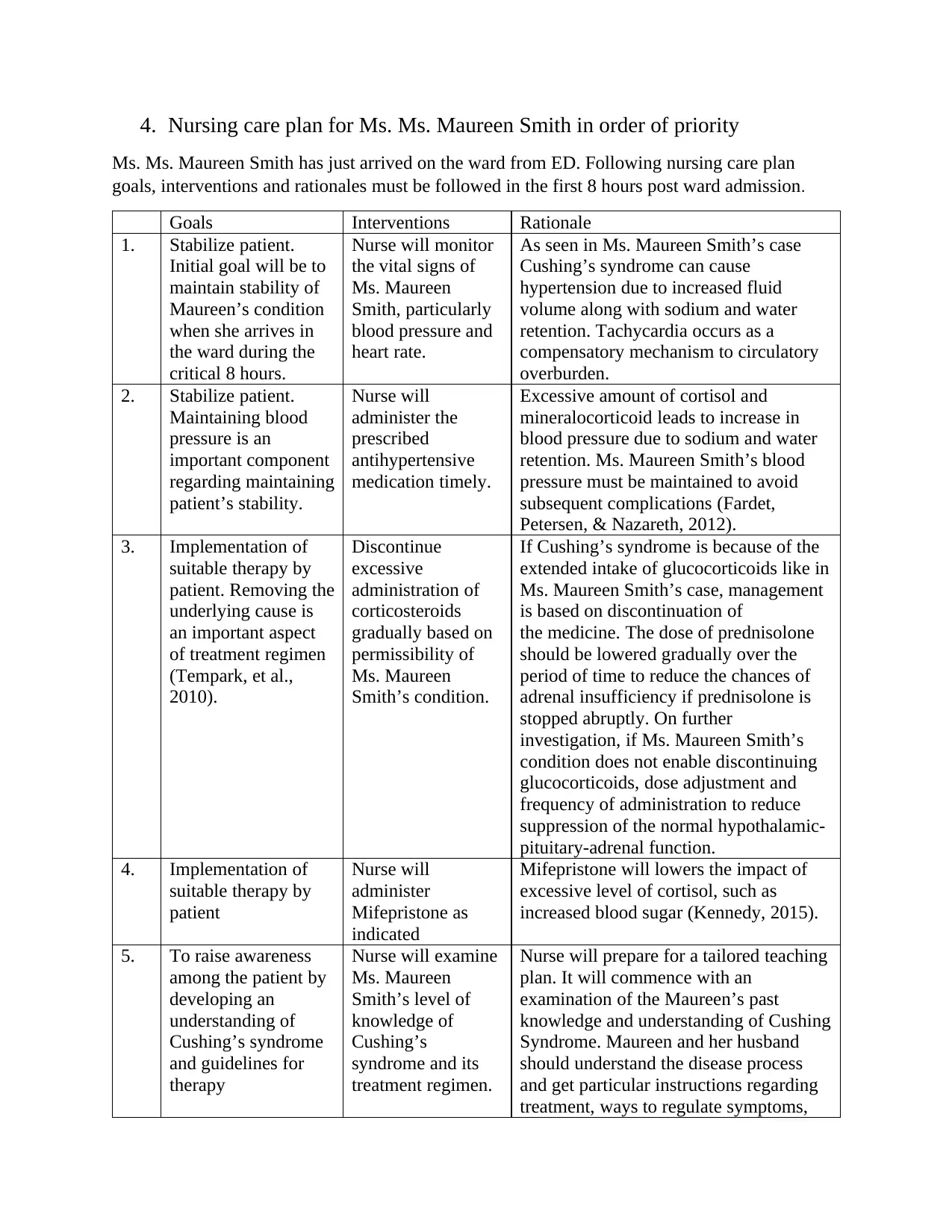
4. Nursing care plan for Ms. Ms. Maureen Smith in order of priority
Ms. Ms. Maureen Smith has just arrived on the ward from ED. Following nursing care plan
goals, interventions and rationales must be followed in the first 8 hours post ward admission.
Goals Interventions Rationale
1. Stabilize patient.
Initial goal will be to
maintain stability of
Maureen’s condition
when she arrives in
the ward during the
critical 8 hours.
Nurse will monitor
the vital signs of
Ms. Maureen
Smith, particularly
blood pressure and
heart rate.
As seen in Ms. Maureen Smith’s case
Cushing’s syndrome can cause
hypertension due to increased fluid
volume along with sodium and water
retention. Tachycardia occurs as a
compensatory mechanism to circulatory
overburden.
2. Stabilize patient.
Maintaining blood
pressure is an
important component
regarding maintaining
patient’s stability.
Nurse will
administer the
prescribed
antihypertensive
medication timely.
Excessive amount of cortisol and
mineralocorticoid leads to increase in
blood pressure due to sodium and water
retention. Ms. Maureen Smith’s blood
pressure must be maintained to avoid
subsequent complications (Fardet,
Petersen, & Nazareth, 2012).
3. Implementation of
suitable therapy by
patient. Removing the
underlying cause is
an important aspect
of treatment regimen
(Tempark, et al.,
2010).
Discontinue
excessive
administration of
corticosteroids
gradually based on
permissibility of
Ms. Maureen
Smith’s condition.
If Cushing’s syndrome is because of the
extended intake of glucocorticoids like in
Ms. Maureen Smith’s case, management
is based on discontinuation of
the medicine. The dose of prednisolone
should be lowered gradually over the
period of time to reduce the chances of
adrenal insufficiency if prednisolone is
stopped abruptly. On further
investigation, if Ms. Maureen Smith’s
condition does not enable discontinuing
glucocorticoids, dose adjustment and
frequency of administration to reduce
suppression of the normal hypothalamic-
pituitary-adrenal function.
4. Implementation of
suitable therapy by
patient
Nurse will
administer
Mifepristone as
indicated
Mifepristone will lowers the impact of
excessive level of cortisol, such as
increased blood sugar (Kennedy, 2015).
5. To raise awareness
among the patient by
developing an
understanding of
Cushing’s syndrome
and guidelines for
therapy
Nurse will examine
Ms. Maureen
Smith’s level of
knowledge of
Cushing’s
syndrome and its
treatment regimen.
Nurse will prepare for a tailored teaching
plan. It will commence with an
examination of the Maureen’s past
knowledge and understanding of Cushing
Syndrome. Maureen and her husband
should understand the disease process
and get particular instructions regarding
treatment, ways to regulate symptoms,
Ms. Ms. Maureen Smith has just arrived on the ward from ED. Following nursing care plan
goals, interventions and rationales must be followed in the first 8 hours post ward admission.
Goals Interventions Rationale
1. Stabilize patient.
Initial goal will be to
maintain stability of
Maureen’s condition
when she arrives in
the ward during the
critical 8 hours.
Nurse will monitor
the vital signs of
Ms. Maureen
Smith, particularly
blood pressure and
heart rate.
As seen in Ms. Maureen Smith’s case
Cushing’s syndrome can cause
hypertension due to increased fluid
volume along with sodium and water
retention. Tachycardia occurs as a
compensatory mechanism to circulatory
overburden.
2. Stabilize patient.
Maintaining blood
pressure is an
important component
regarding maintaining
patient’s stability.
Nurse will
administer the
prescribed
antihypertensive
medication timely.
Excessive amount of cortisol and
mineralocorticoid leads to increase in
blood pressure due to sodium and water
retention. Ms. Maureen Smith’s blood
pressure must be maintained to avoid
subsequent complications (Fardet,
Petersen, & Nazareth, 2012).
3. Implementation of
suitable therapy by
patient. Removing the
underlying cause is
an important aspect
of treatment regimen
(Tempark, et al.,
2010).
Discontinue
excessive
administration of
corticosteroids
gradually based on
permissibility of
Ms. Maureen
Smith’s condition.
If Cushing’s syndrome is because of the
extended intake of glucocorticoids like in
Ms. Maureen Smith’s case, management
is based on discontinuation of
the medicine. The dose of prednisolone
should be lowered gradually over the
period of time to reduce the chances of
adrenal insufficiency if prednisolone is
stopped abruptly. On further
investigation, if Ms. Maureen Smith’s
condition does not enable discontinuing
glucocorticoids, dose adjustment and
frequency of administration to reduce
suppression of the normal hypothalamic-
pituitary-adrenal function.
4. Implementation of
suitable therapy by
patient
Nurse will
administer
Mifepristone as
indicated
Mifepristone will lowers the impact of
excessive level of cortisol, such as
increased blood sugar (Kennedy, 2015).
5. To raise awareness
among the patient by
developing an
understanding of
Cushing’s syndrome
and guidelines for
therapy
Nurse will examine
Ms. Maureen
Smith’s level of
knowledge of
Cushing’s
syndrome and its
treatment regimen.
Nurse will prepare for a tailored teaching
plan. It will commence with an
examination of the Maureen’s past
knowledge and understanding of Cushing
Syndrome. Maureen and her husband
should understand the disease process
and get particular instructions regarding
treatment, ways to regulate symptoms,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

signs of infection, complications, and
indicators of time at which physician
should be notified (Raff, Sharma, &
Nieman, 2014).
References
Ambrogio, A. G., & Cavagnini, F. (2016). Role of “old” pharmacological agents in the treatment
of Cushing’s syndrome. J Endocrinol Invest., 39, 957-65.
Cicala, & Mantero. (2010). Hypertension in Cushing's syndrome: from pathogenesis to
treatment. Neuroendocrinology, 92(1), 44-9.
Clayton, Raskauskiene, Reulen, & Jones. (2011). Mortality and morbidity in Cushing’s disease
over 50 years in Stoke-on-Trent, UK: audit and meta-analysis of literature. J Clin
Endocrinol Metab, 96, 632-42.
Fardet, Petersen, & Nazareth. (2012). Risk of cardiovascular events in people prescribed
glucocorticoids with iatrogenic Cushing’s syndrome: cohort study. BMJ, 345(492).
Kennedy, L. (2015). MIFEPRISTONE AND CUSHING SYNDROME: A COMMENTARY.
Endocrine Practice, 21(10), 1175-77.
Lacroix, A., Feelders, R. A., Stratakis, C. A., & Nieman, L. K. (2015). Cushing’s syndrome.
Lancet (London, England), 386(9996), 913-927.
Lee, M.-J., Pramyothin, P., Karastergiou, K., & Fried, S. K. (2014). Deconstructing the roles of
glucocorticoids in adipose tissue biology and the development of central obesity.
Biochim Biophys Acta, 1842(3), 473-81.
Nieman, L. K. (2014). Update in the medical therapy of Cushing’s disease. Curr Opin
Endocrinol Diabetes Obes, 20(4), 330-334.
Pivonello, Leo, D., Vitale, Cozzolino, Simeoli, Martino, D., . . . Colao. (2010). Pathophysiology
of diabetes mellitus in Cushing's syndrome. Neuroendocrinology, 92(1), 77-81.
Prague, J. K., May, S., & Whitelaw, B. C. (2013). Cushing’s syndrome. BMJ, 346.
Raff, H., Sharma, S. T., & Nieman, L. K. (2014). Physiological Basis for the Etiology,
Diagnosis, and Treatment of Adrenal Disorders: Cushing’s Syndrome, Adrenal
Insufficiency, and Congenital Adrenal Hyperplasia. Compr Physiol, 4(2), 739-69.
Tempark, Phatarakijnirund, Chatproedprai, Watcharasindhu, Supornsilchai, & Wananukul.
(2010). Exogenous Cushing’s syndrome due to topical corticosteroid application: case
report and review literature. Endocrine, 38, 328-34.
indicators of time at which physician
should be notified (Raff, Sharma, &
Nieman, 2014).
References
Ambrogio, A. G., & Cavagnini, F. (2016). Role of “old” pharmacological agents in the treatment
of Cushing’s syndrome. J Endocrinol Invest., 39, 957-65.
Cicala, & Mantero. (2010). Hypertension in Cushing's syndrome: from pathogenesis to
treatment. Neuroendocrinology, 92(1), 44-9.
Clayton, Raskauskiene, Reulen, & Jones. (2011). Mortality and morbidity in Cushing’s disease
over 50 years in Stoke-on-Trent, UK: audit and meta-analysis of literature. J Clin
Endocrinol Metab, 96, 632-42.
Fardet, Petersen, & Nazareth. (2012). Risk of cardiovascular events in people prescribed
glucocorticoids with iatrogenic Cushing’s syndrome: cohort study. BMJ, 345(492).
Kennedy, L. (2015). MIFEPRISTONE AND CUSHING SYNDROME: A COMMENTARY.
Endocrine Practice, 21(10), 1175-77.
Lacroix, A., Feelders, R. A., Stratakis, C. A., & Nieman, L. K. (2015). Cushing’s syndrome.
Lancet (London, England), 386(9996), 913-927.
Lee, M.-J., Pramyothin, P., Karastergiou, K., & Fried, S. K. (2014). Deconstructing the roles of
glucocorticoids in adipose tissue biology and the development of central obesity.
Biochim Biophys Acta, 1842(3), 473-81.
Nieman, L. K. (2014). Update in the medical therapy of Cushing’s disease. Curr Opin
Endocrinol Diabetes Obes, 20(4), 330-334.
Pivonello, Leo, D., Vitale, Cozzolino, Simeoli, Martino, D., . . . Colao. (2010). Pathophysiology
of diabetes mellitus in Cushing's syndrome. Neuroendocrinology, 92(1), 77-81.
Prague, J. K., May, S., & Whitelaw, B. C. (2013). Cushing’s syndrome. BMJ, 346.
Raff, H., Sharma, S. T., & Nieman, L. K. (2014). Physiological Basis for the Etiology,
Diagnosis, and Treatment of Adrenal Disorders: Cushing’s Syndrome, Adrenal
Insufficiency, and Congenital Adrenal Hyperplasia. Compr Physiol, 4(2), 739-69.
Tempark, Phatarakijnirund, Chatproedprai, Watcharasindhu, Supornsilchai, & Wananukul.
(2010). Exogenous Cushing’s syndrome due to topical corticosteroid application: case
report and review literature. Endocrine, 38, 328-34.
1 out of 5
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





