Environmental Health Risk Assessment of HA-MRSA Transmission Control
VerifiedAdded on 2023/04/19
|8
|3492
|100
Report
AI Summary
This report presents an environmental health risk assessment (EHRA) focused on controlling healthcare-acquired methicillin-resistant Staphylococcus aureus (HA-MRSA) transmission through multiple interventions. It begins by formulating a PICO question to guide the research, followed by a literature review highlighting the significance of HA-MRSA as a nosocomial pathogen and the challenges posed by antibiotic resistance. The assessment delves into the biological plausibility of MRSA-related complications, emphasizing the impact of interventions such as mupirocin administration and hygiene protocols. The methods section identifies risk factors for MRSA acquisition, including patient demographics, environmental conditions, and medical devices. It also covers hazard notification procedures, dose-response considerations for antibiotic treatments, and exposure assessment strategies based on surveillance data and prevalence rates. The report concludes with risk characterization, focusing on source identification and outbreak prevention, and proposes a risk communication strategy to reduce MRSA spread through improved hand hygiene and responsible antibiotic use. The report utilises existing studies to support its findings and suggests implementing comprehensive control measures to minimize HA-MRSA transmission in healthcare settings.
1. Research (PICO) question
Can transmission of healthcare acquired methicillin-resistant Staphylococcus aureus
(HA-MRSA) be controlled by multiple interventions?
P (population) - patients and nursing staffs
I (intervention) – Addressing the need to tackle transmission of methicillin-resistant
Staphylococcus aureus (MRSA) in hospital settings and examine the good practices
C (comparison) – various strategies to minimise the acquisitions of MRSA
O (outcome) – curbing healthcare acquired (HA) complications by MRSA
2. Background
i. Literature review
The review of several literatures were conducted utilising the search databases such as
CINAHL, PubMed and EBSCOhost, Additionally the search items include methicillin-
resistant Staphylococcus aureus, control of infection by MRSA and implementation of
control measures for patients and nurses. The literature search consisted of 53 articles out of
which 20 were chosen to identify the problems, notification on hazard, response to dose,
exposure assessment and characterize the risk.
Globally, healthcare acquired infections are one of the major implications of mortality.
Morbidity and excessive financial burden. Staphylococcus aureus is most potent nosocomial
pathogen leading to healthcare acquired complications such as pneumonia, meningitis and
bacteraemia. The administration of antibiotics and antimicrobial agents has significantly
increased in the recent past; as a result there has been a drastic reduction in infection and
death rates (Littman and Viens, 2015). As antibiotics have been the major line of treatment
for a long period, few bacteria have developed resistance towards the antibiotics thereby
rendering the treatment ineffective (Lloyd et al., 2005). Currently, antibiotic resistance has
become a problem worldwide and research is being done to curb antibiotic resistance
(Fukunaga et al., 2016). As such, MRSA, a strain of S. aureus exhibits resistance against
methicillin and is a serious concern to public health owing to its elevated levels in mortality
rates among the antibiotic resistant organisms.
ii. Rational and significance
One of the studies revealed that the risk of mortality was twice higher than that of methicillin-
sensitive S. aureus which significantly increases the duration of stay, utilizing resources of
the healthcare facilities, medication and extra nursing staffs for care thus leading to economic
burden for the patient (Kundrapu et al., 2012). MRSA has the ability to survive on hospital
surfaces such as catheters, surgical instruments, hospital floor and furniture and cause
outbreaks if left uncontrolled. Consequently, it is important to understand the disease burden
and the potential factors associated with the spread of infection in order to manage HA-
MRSA (Fox et al., 2015). Furthermore, identifying the risk factors will ensure formulation of
guidelines and recommendations for prevention policies, in particular, good hand hygiene,
adequate care of vascular devices and cleanliness of the hospital environment (Minhas et al.,
2011).
Can transmission of healthcare acquired methicillin-resistant Staphylococcus aureus
(HA-MRSA) be controlled by multiple interventions?
P (population) - patients and nursing staffs
I (intervention) – Addressing the need to tackle transmission of methicillin-resistant
Staphylococcus aureus (MRSA) in hospital settings and examine the good practices
C (comparison) – various strategies to minimise the acquisitions of MRSA
O (outcome) – curbing healthcare acquired (HA) complications by MRSA
2. Background
i. Literature review
The review of several literatures were conducted utilising the search databases such as
CINAHL, PubMed and EBSCOhost, Additionally the search items include methicillin-
resistant Staphylococcus aureus, control of infection by MRSA and implementation of
control measures for patients and nurses. The literature search consisted of 53 articles out of
which 20 were chosen to identify the problems, notification on hazard, response to dose,
exposure assessment and characterize the risk.
Globally, healthcare acquired infections are one of the major implications of mortality.
Morbidity and excessive financial burden. Staphylococcus aureus is most potent nosocomial
pathogen leading to healthcare acquired complications such as pneumonia, meningitis and
bacteraemia. The administration of antibiotics and antimicrobial agents has significantly
increased in the recent past; as a result there has been a drastic reduction in infection and
death rates (Littman and Viens, 2015). As antibiotics have been the major line of treatment
for a long period, few bacteria have developed resistance towards the antibiotics thereby
rendering the treatment ineffective (Lloyd et al., 2005). Currently, antibiotic resistance has
become a problem worldwide and research is being done to curb antibiotic resistance
(Fukunaga et al., 2016). As such, MRSA, a strain of S. aureus exhibits resistance against
methicillin and is a serious concern to public health owing to its elevated levels in mortality
rates among the antibiotic resistant organisms.
ii. Rational and significance
One of the studies revealed that the risk of mortality was twice higher than that of methicillin-
sensitive S. aureus which significantly increases the duration of stay, utilizing resources of
the healthcare facilities, medication and extra nursing staffs for care thus leading to economic
burden for the patient (Kundrapu et al., 2012). MRSA has the ability to survive on hospital
surfaces such as catheters, surgical instruments, hospital floor and furniture and cause
outbreaks if left uncontrolled. Consequently, it is important to understand the disease burden
and the potential factors associated with the spread of infection in order to manage HA-
MRSA (Fox et al., 2015). Furthermore, identifying the risk factors will ensure formulation of
guidelines and recommendations for prevention policies, in particular, good hand hygiene,
adequate care of vascular devices and cleanliness of the hospital environment (Minhas et al.,
2011).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

iii. Biological plausibility
The biological plausibility includes prolonged bacteraemia resulting in severe complications
such as meningitis and septic shock. In addition these complications result in prolonged
bacteraemia (Green, 2015). In addition MRSA based interventions have a significant impact
in surgery, For instance mupirocin administered intranasally has significantly minised MRSA
associated infections at the site of surgery in orthopaedic and cardiothoracic surgery, however
not effective in general surgery. The causes for such reasons remain unclear, however a
dosage regimen to decolonise MRSA prior to surgery and development of rapid diagnostic
assays can be effective to curb MRSA transmission. Also utilisation of two interventions such
as hygiene and antibiotics or placement of patients in isolation rooms or proper screening can
be effective in the prevention and control.
3. Methods
i. Problem identification
The chances of acquiring MRSA at healthcare increase with immunocompetent and
immunosusceptible patients, elderly, recipients’ of organ transplant, cancer patients with
prolonged chemotherapy, diabetics, chronic diseases, steroid therapy, intravenous drug users,
and those with prolonged medication with antibiotics. The Centre for Disease Control states
the 5 C’s such as crowding, skin-skin contact especially between patients, their family
members and nursing staffs in the hospital settings, compromised skin, contamination and
lack of cleanliness as the prime factors for transmission of MRSA. In addition, patients with
previous colonisation with the strain, indwelling devices such as prolonged vascular access,
urinary catheter, endoscopic gastrostomy and drains in wound (Bode et al., 2010).
Furthermore chronic wounds and admission in high risk areas in the hospitals such as
intensive critical care unit and burns may also be a major risk problem with MRSA
(Haverstick et al., 2017).
One of the studies conducted by Fox et al. (2015) assessed the rate of MRSA associated
hospital infections such as urinary tract infection due to in-dwellers and central line
associated systemic infection over a period of twelve months. The study was based on a
cardiovascular intensive care unit which is considered a high risk area where 1 nurse took
care of 2 patients. A protocol for hand hygiene was followed in the premises by patients that
were admitted in addition the nursing staffs of that unit. The intervention consisted of wiping
the hand of patients thrice a day using the wipes containing the disinfectant chlorohexidine
gluconate (2%) and the medial report was noted down. Results revealed a reduction in the
mean monthly rate of catheter associated urinary tract infection from 9.1 to 5.6 in one
thousand catheter days and a reduction from 1 to 0.50 in one thousand catheter days for
central line associated bloodstream infections. These results indicated that following the
protocol for hand hygiene significantly reduced MRSA associated hospital infections than the
results obtained prior to the twelve month period (Fox et al., 2015).
In another study, assessment of providing health education to patients, nursing staffs and
usage of hand hygiene protocol was performed to minimise MRSA transmission via
increased usage of hand hygiene protocol and educating the patients to utilise hand hygiene
wipes. This study was conducted for over a 19 month period and results indicated that the
rates for MRSA drastically reduced by 63% post-intervention (Strigley et al., 2016).
The biological plausibility includes prolonged bacteraemia resulting in severe complications
such as meningitis and septic shock. In addition these complications result in prolonged
bacteraemia (Green, 2015). In addition MRSA based interventions have a significant impact
in surgery, For instance mupirocin administered intranasally has significantly minised MRSA
associated infections at the site of surgery in orthopaedic and cardiothoracic surgery, however
not effective in general surgery. The causes for such reasons remain unclear, however a
dosage regimen to decolonise MRSA prior to surgery and development of rapid diagnostic
assays can be effective to curb MRSA transmission. Also utilisation of two interventions such
as hygiene and antibiotics or placement of patients in isolation rooms or proper screening can
be effective in the prevention and control.
3. Methods
i. Problem identification
The chances of acquiring MRSA at healthcare increase with immunocompetent and
immunosusceptible patients, elderly, recipients’ of organ transplant, cancer patients with
prolonged chemotherapy, diabetics, chronic diseases, steroid therapy, intravenous drug users,
and those with prolonged medication with antibiotics. The Centre for Disease Control states
the 5 C’s such as crowding, skin-skin contact especially between patients, their family
members and nursing staffs in the hospital settings, compromised skin, contamination and
lack of cleanliness as the prime factors for transmission of MRSA. In addition, patients with
previous colonisation with the strain, indwelling devices such as prolonged vascular access,
urinary catheter, endoscopic gastrostomy and drains in wound (Bode et al., 2010).
Furthermore chronic wounds and admission in high risk areas in the hospitals such as
intensive critical care unit and burns may also be a major risk problem with MRSA
(Haverstick et al., 2017).
One of the studies conducted by Fox et al. (2015) assessed the rate of MRSA associated
hospital infections such as urinary tract infection due to in-dwellers and central line
associated systemic infection over a period of twelve months. The study was based on a
cardiovascular intensive care unit which is considered a high risk area where 1 nurse took
care of 2 patients. A protocol for hand hygiene was followed in the premises by patients that
were admitted in addition the nursing staffs of that unit. The intervention consisted of wiping
the hand of patients thrice a day using the wipes containing the disinfectant chlorohexidine
gluconate (2%) and the medial report was noted down. Results revealed a reduction in the
mean monthly rate of catheter associated urinary tract infection from 9.1 to 5.6 in one
thousand catheter days and a reduction from 1 to 0.50 in one thousand catheter days for
central line associated bloodstream infections. These results indicated that following the
protocol for hand hygiene significantly reduced MRSA associated hospital infections than the
results obtained prior to the twelve month period (Fox et al., 2015).
In another study, assessment of providing health education to patients, nursing staffs and
usage of hand hygiene protocol was performed to minimise MRSA transmission via
increased usage of hand hygiene protocol and educating the patients to utilise hand hygiene
wipes. This study was conducted for over a 19 month period and results indicated that the
rates for MRSA drastically reduced by 63% post-intervention (Strigley et al., 2016).

ii. Hazard notification
In cases where the laboratory in the healthcare facility confirms MRSA that has been isolated
from a patient who is admitted in the hospital, the person in-charge, either the general
practitioner, coordinator of infection control, the nursing staffs who take care of that patient
or the unit and personnel who are recommended as per the guidelines of the healthcare
facilities (Peters et al., 2017). In case the notification of hazard occurred after the working
hours of the unit responsible for infection control and prevention, there has to be a system to
ensure the notification is conveyed to the personnel in the unit at the earliest. However the
duty nurse can be informed in such scenario. Furthermore hazard analysis involves the routes
of exposure and transmission to other people within the healthcare. As suc, a hospital
estimation model using Bayesian analysis might be necessary to estimate the rate of
transmission.
iii. Dose response
Due to the drug resistance of MRSA, medical practitioners have stopped prescribing
conventional antibiotics to methicillin resistant Staph infections. Alternatively, intravenous
vancomycin hydrochloride is considered as the gold standard for treating MRSA associated
infections. However new antibiotics such as dalfopristin, linezolid and tigecycline are
mentioned to have delirious effects on MRSA (Lee et al., 2013), however they are expensive
and not much of clinical research has been done. In addition, sub-minimum inhibitory
concentration of beta-lactam antibiotics induced biofilm formation and the dose response was
not effective. In most of the isolates of MRSA, beta-lactam resistance is purely expressed
based on the clone and population which has been revealed by population analysis whereby
detection is based on culture with varying frequencies and a broad MIC range. At home, the
treatment involves oral antibiotic dose regimen for almost 10 days. Antibiotics such as
minocycline and doxycycline might be prescribed, however instructions have to be followed
while taking antibiotics. It denotes that the prescribed antibiotics needed to be taken the entire
course and should not be withdrawn when the patient recovered during the dose regimen. In
case the oral antibiotic was not effective, the general practitioner might prescribe a different
antibiotic. Furthermore, the specialist might drain the infected area with a small incision
using a needle and it is performed to minimise the amount of pus thereby assisting in healing.
In addition hand hygiene with chlorhexidine and application of mupirocin ointment may be
advised by the physician however may not always be effective.
People who are hospitalized for infections with MRSA will be treated with intravenous
vancomycin,, chlorhexidine for ensuring hand hygiene and mupirocin as ointment. However
they are not often effective owing to multi-drug resistant nature of MRSA. Patients would be
prescribed antibiotics even after discharge for up to 8 weeks in order to assess the recurrence
of infection. One of the main reasons for completing the dose regimen for antibiotics is to
prevent re-treatment.
iv. Exposure assessment
In cases where the laboratory in the healthcare facility confirms MRSA that has been isolated
from a patient who is admitted in the hospital, the person in-charge, either the general
practitioner, coordinator of infection control, the nursing staffs who take care of that patient
or the unit and personnel who are recommended as per the guidelines of the healthcare
facilities (Peters et al., 2017). In case the notification of hazard occurred after the working
hours of the unit responsible for infection control and prevention, there has to be a system to
ensure the notification is conveyed to the personnel in the unit at the earliest. However the
duty nurse can be informed in such scenario. Furthermore hazard analysis involves the routes
of exposure and transmission to other people within the healthcare. As suc, a hospital
estimation model using Bayesian analysis might be necessary to estimate the rate of
transmission.
iii. Dose response
Due to the drug resistance of MRSA, medical practitioners have stopped prescribing
conventional antibiotics to methicillin resistant Staph infections. Alternatively, intravenous
vancomycin hydrochloride is considered as the gold standard for treating MRSA associated
infections. However new antibiotics such as dalfopristin, linezolid and tigecycline are
mentioned to have delirious effects on MRSA (Lee et al., 2013), however they are expensive
and not much of clinical research has been done. In addition, sub-minimum inhibitory
concentration of beta-lactam antibiotics induced biofilm formation and the dose response was
not effective. In most of the isolates of MRSA, beta-lactam resistance is purely expressed
based on the clone and population which has been revealed by population analysis whereby
detection is based on culture with varying frequencies and a broad MIC range. At home, the
treatment involves oral antibiotic dose regimen for almost 10 days. Antibiotics such as
minocycline and doxycycline might be prescribed, however instructions have to be followed
while taking antibiotics. It denotes that the prescribed antibiotics needed to be taken the entire
course and should not be withdrawn when the patient recovered during the dose regimen. In
case the oral antibiotic was not effective, the general practitioner might prescribe a different
antibiotic. Furthermore, the specialist might drain the infected area with a small incision
using a needle and it is performed to minimise the amount of pus thereby assisting in healing.
In addition hand hygiene with chlorhexidine and application of mupirocin ointment may be
advised by the physician however may not always be effective.
People who are hospitalized for infections with MRSA will be treated with intravenous
vancomycin,, chlorhexidine for ensuring hand hygiene and mupirocin as ointment. However
they are not often effective owing to multi-drug resistant nature of MRSA. Patients would be
prescribed antibiotics even after discharge for up to 8 weeks in order to assess the recurrence
of infection. One of the main reasons for completing the dose regimen for antibiotics is to
prevent re-treatment.
iv. Exposure assessment
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MRSA assessment is based on the results of culture and system to screen patients with
confirmed history for MRSA. Clinical isolates from MRSA infected patients have to be the
major component for management of surveillance within the healthcare settings (Currie et al.,
2013). Facilities that follow strict surveillance program can identify the reservoirs or carriers
of MRSA. It is mandatory for exposure assessment to track patients who are positive for
MRSA via screening based on location, patient proportion and service provide clinically. The
data should be consistent in order for the evaluation to be relevant and appropriate and
comparative for studies prior and after therapy (Mishal et al., 2001). The prevalence of
MRSA is the ratio of the patients who colonize and are infected with MRSA and the number
of patients in the population study at one point of time. In addition the exposure assessment
should possess definitions for all the measurements. Acquisition of the infection is related to
hospitalization if MRSA infection is detected more than 2 days following admission (Borg et
al., 2012).
At hospitals it is important to follow and notify the rates of prevalence for every high risk
unit (Dickmann et al., 2017). It is important to identify populations and service lines at high
risk, analyse the transmission of MRSA in the population of patients over a period of time
before and after the interventions, compare the spread of MRSA to evaluate whether multiple
interventions are necessary, prioritise interventions for specific patient care units and among
specific populations and develop a dosage regimen and effectively communicate to the
nursing staffs. One of the evaluations for the exposure assessment of MRSA is determined as
follows:
No. of new MRSA casesper unitper month/no. of patient days * 1000 = HA-MRSA rates per
1000 unit patient days
v Risk characterization
Once the disease has been identified in a patient, the medical practitioner might have a
conversation with the patients and inform about decolonisation which is mostly done to treat
MRSA which utilise antiseptic wash and nasal ointment for up to 1 week. The reason is to get
rid of MRSA prior to discharge from the hospital. In addition risk characterization mostly
consists of identifying the source and preventing outbreaks in the healthcare facility.
4. Risk communication
The communication of risks involves several approaches to reduce the spread of MRSA in
healthcare settings such as wiping the hands regularly to minimise infection and carriage.
Contamination of the hand of healthcare staffs is one of the major reasons for the
transmission of MRSA among patients. Hand gloves, instruments and aprons utilised by the
healthcare workers may be the source of infection. One of the studies conducted by Boyce et
al (1997) revealed that 42% of the gloves used by the nurse are contaminated however they
had no direct contact with the MRSA infected patients but experienced contact with the
surface of the room where the patients were admitted.
The clothing of the nurses is considered as one of the factors for transmission among patients.
Instruments utilised in the patient’s care such as thermometers, blood pressure monitoring
devices and otoscopes act as agents for the spread of infection (Schoeder A et al., 2015). In
addition, the use of antibiotics is considered a risk communication factor. Furthermore, most
of the complaints from patients and their family members include improper communication
confirmed history for MRSA. Clinical isolates from MRSA infected patients have to be the
major component for management of surveillance within the healthcare settings (Currie et al.,
2013). Facilities that follow strict surveillance program can identify the reservoirs or carriers
of MRSA. It is mandatory for exposure assessment to track patients who are positive for
MRSA via screening based on location, patient proportion and service provide clinically. The
data should be consistent in order for the evaluation to be relevant and appropriate and
comparative for studies prior and after therapy (Mishal et al., 2001). The prevalence of
MRSA is the ratio of the patients who colonize and are infected with MRSA and the number
of patients in the population study at one point of time. In addition the exposure assessment
should possess definitions for all the measurements. Acquisition of the infection is related to
hospitalization if MRSA infection is detected more than 2 days following admission (Borg et
al., 2012).
At hospitals it is important to follow and notify the rates of prevalence for every high risk
unit (Dickmann et al., 2017). It is important to identify populations and service lines at high
risk, analyse the transmission of MRSA in the population of patients over a period of time
before and after the interventions, compare the spread of MRSA to evaluate whether multiple
interventions are necessary, prioritise interventions for specific patient care units and among
specific populations and develop a dosage regimen and effectively communicate to the
nursing staffs. One of the evaluations for the exposure assessment of MRSA is determined as
follows:
No. of new MRSA casesper unitper month/no. of patient days * 1000 = HA-MRSA rates per
1000 unit patient days
v Risk characterization
Once the disease has been identified in a patient, the medical practitioner might have a
conversation with the patients and inform about decolonisation which is mostly done to treat
MRSA which utilise antiseptic wash and nasal ointment for up to 1 week. The reason is to get
rid of MRSA prior to discharge from the hospital. In addition risk characterization mostly
consists of identifying the source and preventing outbreaks in the healthcare facility.
4. Risk communication
The communication of risks involves several approaches to reduce the spread of MRSA in
healthcare settings such as wiping the hands regularly to minimise infection and carriage.
Contamination of the hand of healthcare staffs is one of the major reasons for the
transmission of MRSA among patients. Hand gloves, instruments and aprons utilised by the
healthcare workers may be the source of infection. One of the studies conducted by Boyce et
al (1997) revealed that 42% of the gloves used by the nurse are contaminated however they
had no direct contact with the MRSA infected patients but experienced contact with the
surface of the room where the patients were admitted.
The clothing of the nurses is considered as one of the factors for transmission among patients.
Instruments utilised in the patient’s care such as thermometers, blood pressure monitoring
devices and otoscopes act as agents for the spread of infection (Schoeder A et al., 2015). In
addition, the use of antibiotics is considered a risk communication factor. Furthermore, most
of the complaints from patients and their family members include improper communication
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
about MRSA. The groups for patient advocacy have given importance for rapid and increased
information on MRSA in hospital settings (Gigerenzer and Werwerth, 2013). This
communication strategy will assist in clinical governance and adhering to professional and
ethical guidelines as per the national and hospital guidelines. Proper education to the patients
will ensure the patients informing about the requirement for screening and subsequent entry
for admission in the hospital. Furthermore sharing of information and hand hygiene can
reduce the transmission of MRSA. Lack of knowledge about informing the status of MRSA
is one of the barriers that result in the spread of infection (Fukunaga et al., 2017). In addition
the process of documentation has to be made simple and the feedback from audits on the
patient proportions have to be recorded. Also the patient’s MRSA-positive status should be
notified to the new healthcare settings where the patients were to be transferred.
Collaboration with nursing staffs, planning in the discharge and management of patient’s case
are effective measures. In addition it is essential to develop a transfer tool that is similar to
the tool developed by the Centre for Disease Control.
Major findings in the developing strategies are:
i) hand hygiene with chlorhexidine significantly reduced the acquisition of MRSA and
systemic infections (Climno et al., 2013)
ii) information about screening and outcomes to the patient
iii) disinfection of touch surfaces in patient’s rooms infected with MRSA significantly
minimised the transmission of infection via hands of nursing staffs and other healthcare
workers who took care of the patients.
iv) patients with positive MRSA can have recurrent infections due to drug resistance,
prolongEd admission in hospitals and be a carrier for MRSA (Littman and Viens, 2015).
v) Isolation of contact and deceased patients from other patients in the unit and nurses.
5. Conclusion
The healthcare workers, in particular the nurses who work in accordance with the patients
infected with MRSA have to abide by the guidelines and implement effective strategies to
prevent the transmission of MRSA within the healthcare settings. In addition, education about
MRSA to patients, prompt techniques of disinfection can effectively prevent and control
MRSA transmission. Consequently multiple interventions can promote effective management
of MRSA in hospitals. This will prevent prolonged stays in the hospital, charges that cannot
be reimbursed from Medicare and Medicaid and ensure rduction in the financial burden of the
patient.
6. References
Fox C., Wavra T., Drake D., Mulligan D., Bennett Y., Nelson C., Kirkwood P., Jones L.,
Bader M. (2015). Use of a patient hand hygiene protocol to reduce hospital acquired
infections and improve nurses hand washing. American Journal of Critical Care. Vol 24 (3).
217-223.
Strigley J. A., Furness C. D., Gardam M. (2016). Interventions to improve patient hand
hygiene: a systematic review. Journal of Hospital Infection. Vol 94 (1). 23-29
information on MRSA in hospital settings (Gigerenzer and Werwerth, 2013). This
communication strategy will assist in clinical governance and adhering to professional and
ethical guidelines as per the national and hospital guidelines. Proper education to the patients
will ensure the patients informing about the requirement for screening and subsequent entry
for admission in the hospital. Furthermore sharing of information and hand hygiene can
reduce the transmission of MRSA. Lack of knowledge about informing the status of MRSA
is one of the barriers that result in the spread of infection (Fukunaga et al., 2017). In addition
the process of documentation has to be made simple and the feedback from audits on the
patient proportions have to be recorded. Also the patient’s MRSA-positive status should be
notified to the new healthcare settings where the patients were to be transferred.
Collaboration with nursing staffs, planning in the discharge and management of patient’s case
are effective measures. In addition it is essential to develop a transfer tool that is similar to
the tool developed by the Centre for Disease Control.
Major findings in the developing strategies are:
i) hand hygiene with chlorhexidine significantly reduced the acquisition of MRSA and
systemic infections (Climno et al., 2013)
ii) information about screening and outcomes to the patient
iii) disinfection of touch surfaces in patient’s rooms infected with MRSA significantly
minimised the transmission of infection via hands of nursing staffs and other healthcare
workers who took care of the patients.
iv) patients with positive MRSA can have recurrent infections due to drug resistance,
prolongEd admission in hospitals and be a carrier for MRSA (Littman and Viens, 2015).
v) Isolation of contact and deceased patients from other patients in the unit and nurses.
5. Conclusion
The healthcare workers, in particular the nurses who work in accordance with the patients
infected with MRSA have to abide by the guidelines and implement effective strategies to
prevent the transmission of MRSA within the healthcare settings. In addition, education about
MRSA to patients, prompt techniques of disinfection can effectively prevent and control
MRSA transmission. Consequently multiple interventions can promote effective management
of MRSA in hospitals. This will prevent prolonged stays in the hospital, charges that cannot
be reimbursed from Medicare and Medicaid and ensure rduction in the financial burden of the
patient.
6. References
Fox C., Wavra T., Drake D., Mulligan D., Bennett Y., Nelson C., Kirkwood P., Jones L.,
Bader M. (2015). Use of a patient hand hygiene protocol to reduce hospital acquired
infections and improve nurses hand washing. American Journal of Critical Care. Vol 24 (3).
217-223.
Strigley J. A., Furness C. D., Gardam M. (2016). Interventions to improve patient hand
hygiene: a systematic review. Journal of Hospital Infection. Vol 94 (1). 23-29
Haverstick S., Goodrich C., Freeman R., James S., Kullar R., Ahrens M. (2017). Patient’s
hand washing and reducing hospital acquired infection. Critical Care Nurse. Vol 37 (3).
Climno M. W., Yokoe D. S., Warren D. K., Perl T. M., Bolon M., Herwaldt L.A., Wong E. S.
(2013). Effect of daily chlorohexidine bathing on hospital-acquired infection. N Engl J Med.
Vol 368. 533-542
Currie K., Knussen C., Price L., Reilly J. (2013). Methicillin-resistant Staphylococcus aureus
screening aas a patient safety initiative using patients experiences to improve the quality of
screening practices. Journal of Clinical Nursing. Doi: 10.111/joen.12386
Kundrapu s., Sunkesula V., Jury I. A., Sitzlar B. M., Donskey C. J. (2012). Daily disinfection
of high touch surfaces in isolation rooms to reduce contamination of healthcare workers
hands. Infect Control Hosp Epidemiology. Vol 33 (10). 1039-1042
Minhas P., Perl T. M., Carroll K. C., Shepard J. W., Shagraw K. A et al (2011). Risk factors
for positive admission surveillance cultures for methicillin resistant Staphylococcis aureus
and vancomycin-resistant eneterococci in neurocritical care unit. Critical care Med. Vol 39.
2322-2329
Mishal J., Sherer Y., Levin Y., Katz D., Embon E. (2001). Two stage evaluation and
intravention program for control of methicillin resistant Staphylococcus aureus in the hospital
setting. Scandinavian Journal of Infectious Diseases. Vol 33 (7). 498-501
Schroeder A., Schroeder M. A., D’Amico F (2009). What’s growing on your stethoscope?
And what you can do about it. J Fam Pract. Vol 58. 408-409
Dickmann P et al. (2017). Communicating the risk of MRSA: the role of clinical practice,
regulation and other policies in five European countries. Frontiers in Public Health. Vol 5
(44). Doi: 10.3389/fpubh.2017/00044
Lee et al. (2013). Comparison of strategies to reduce methicillin resistant Staphylococcus
aureus rates in surgical patients: a controlled multicentre intervention trial. Infectious
Diseases. Vol 3 (9).
Green B. N. (2012). Methicillin resistant Staphylococcus aureus: an overview for manual
therapists. J Chirop Med. Vol 11 (1), 64-75
Gigerenzer G., Wegwarth O. (2013). Five year survival rates can mislead. BMJ. Vol 348
Borg M. A., Camilleri L., Waisfisz B. (2012). Understanding the epidemiology of MRSA in
Europe: do we need to think outside the box? J Hosp Infect. Vol 81 (4). 251-256
Lloyd S. J. O., Svhreiber S. J., Kopp P. E et al. (2005). Superspreading and the effect of
individual variation on disease emergence. Nature. Vol 438. 355-359
Bode L. G., Kloytmans J .A., Wertherirn H. F. et al. (2010). Preventing surgical site
infections in nasal carriers of Staphylococcus aureus. N Eng J Med. 2010. Vol 362. 9-17.
Fukunaga B. T., Sumida W. K., Taira D. A., Davis J. W., Seto T. B. (2016). Hospital
acquired methicillin resistant Staphylococcus aureus bacteremia related to Medicare
antibiotic prescriptions: a state level analysis. Hawaii J Med Public Health. Vol 75 (10). 303-
309
hand washing and reducing hospital acquired infection. Critical Care Nurse. Vol 37 (3).
Climno M. W., Yokoe D. S., Warren D. K., Perl T. M., Bolon M., Herwaldt L.A., Wong E. S.
(2013). Effect of daily chlorohexidine bathing on hospital-acquired infection. N Engl J Med.
Vol 368. 533-542
Currie K., Knussen C., Price L., Reilly J. (2013). Methicillin-resistant Staphylococcus aureus
screening aas a patient safety initiative using patients experiences to improve the quality of
screening practices. Journal of Clinical Nursing. Doi: 10.111/joen.12386
Kundrapu s., Sunkesula V., Jury I. A., Sitzlar B. M., Donskey C. J. (2012). Daily disinfection
of high touch surfaces in isolation rooms to reduce contamination of healthcare workers
hands. Infect Control Hosp Epidemiology. Vol 33 (10). 1039-1042
Minhas P., Perl T. M., Carroll K. C., Shepard J. W., Shagraw K. A et al (2011). Risk factors
for positive admission surveillance cultures for methicillin resistant Staphylococcis aureus
and vancomycin-resistant eneterococci in neurocritical care unit. Critical care Med. Vol 39.
2322-2329
Mishal J., Sherer Y., Levin Y., Katz D., Embon E. (2001). Two stage evaluation and
intravention program for control of methicillin resistant Staphylococcus aureus in the hospital
setting. Scandinavian Journal of Infectious Diseases. Vol 33 (7). 498-501
Schroeder A., Schroeder M. A., D’Amico F (2009). What’s growing on your stethoscope?
And what you can do about it. J Fam Pract. Vol 58. 408-409
Dickmann P et al. (2017). Communicating the risk of MRSA: the role of clinical practice,
regulation and other policies in five European countries. Frontiers in Public Health. Vol 5
(44). Doi: 10.3389/fpubh.2017/00044
Lee et al. (2013). Comparison of strategies to reduce methicillin resistant Staphylococcus
aureus rates in surgical patients: a controlled multicentre intervention trial. Infectious
Diseases. Vol 3 (9).
Green B. N. (2012). Methicillin resistant Staphylococcus aureus: an overview for manual
therapists. J Chirop Med. Vol 11 (1), 64-75
Gigerenzer G., Wegwarth O. (2013). Five year survival rates can mislead. BMJ. Vol 348
Borg M. A., Camilleri L., Waisfisz B. (2012). Understanding the epidemiology of MRSA in
Europe: do we need to think outside the box? J Hosp Infect. Vol 81 (4). 251-256
Lloyd S. J. O., Svhreiber S. J., Kopp P. E et al. (2005). Superspreading and the effect of
individual variation on disease emergence. Nature. Vol 438. 355-359
Bode L. G., Kloytmans J .A., Wertherirn H. F. et al. (2010). Preventing surgical site
infections in nasal carriers of Staphylococcus aureus. N Eng J Med. 2010. Vol 362. 9-17.
Fukunaga B. T., Sumida W. K., Taira D. A., Davis J. W., Seto T. B. (2016). Hospital
acquired methicillin resistant Staphylococcus aureus bacteremia related to Medicare
antibiotic prescriptions: a state level analysis. Hawaii J Med Public Health. Vol 75 (10). 303-
309
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Littman J., Viens A. M. (2015). The ethical significance of antimicrobial resistance. Public
Health Ethics. Vol 8 (3). 209-224.
Peters C., Dulon M., Kleimuller O., Nienhaus A., Schabion A. (2017). MRSA prevalence and
risk factors among health personnel and residents in nursing homes in Hamburg, Germany-a
cross sectional study. PLoS One. Vol 12 (1). E0169425
Health Ethics. Vol 8 (3). 209-224.
Peters C., Dulon M., Kleimuller O., Nienhaus A., Schabion A. (2017). MRSA prevalence and
risk factors among health personnel and residents in nursing homes in Hamburg, Germany-a
cross sectional study. PLoS One. Vol 12 (1). E0169425
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
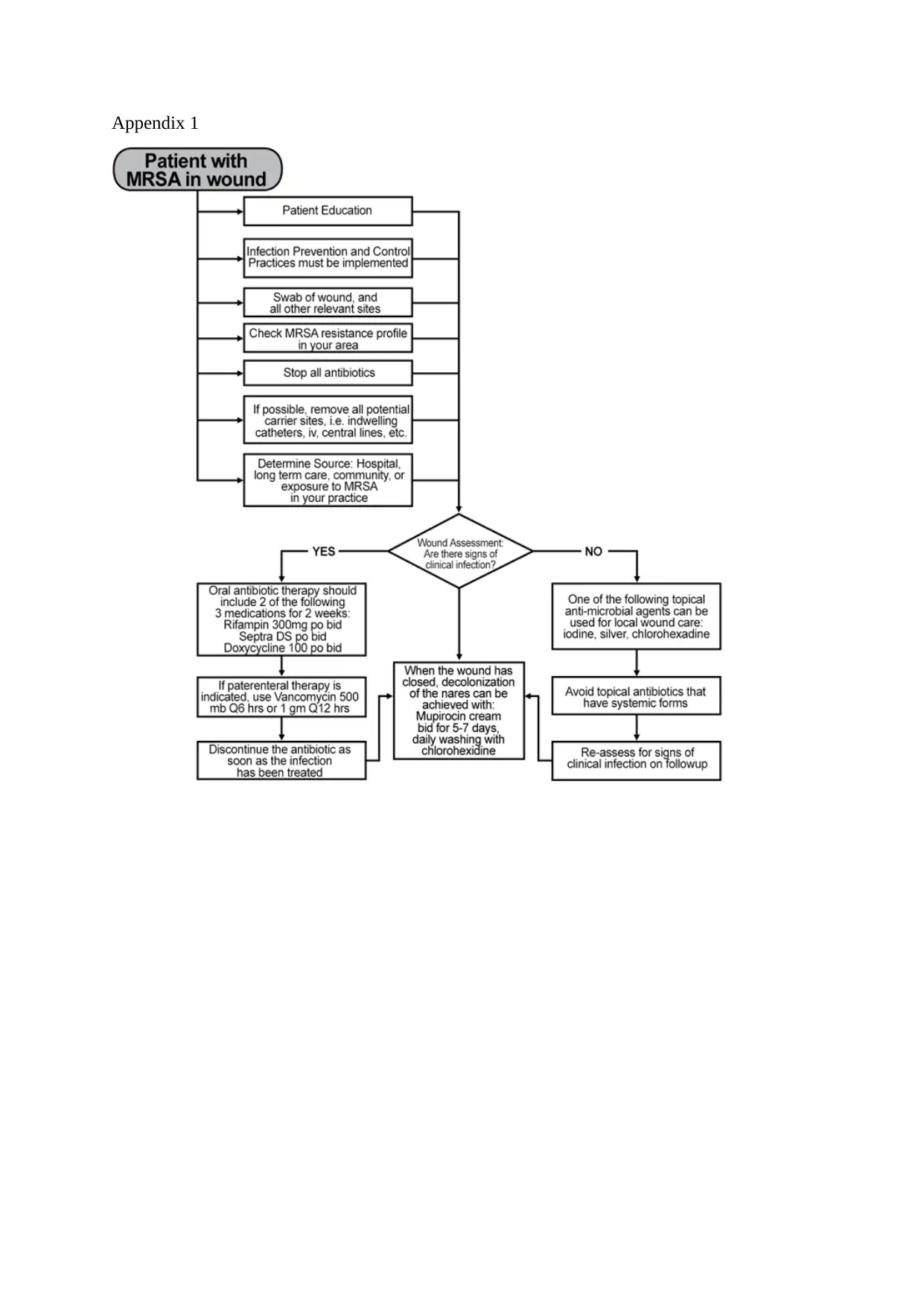
Appendix 1
1 out of 8