SOAP Documentation for Patient with Psoriasis
VerifiedAdded on 2022/10/01
|18
|5639
|331
AI Summary
Read the SOAP documentation for a patient with psoriasis, including their medical history, symptoms, and physical examination. The patient has a family history of psoriasis and experiences widespread scaly rash associated with itching and redness. The physical examination reveals a PASI score range of 15-18, indicating severe clinical manifestations and poor prognosis.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
1 | P a g e
SOAP Documentation
Date of History / Assessment: 2nd September 2019
General Patient Information: Robert: Age: 47 years Sex: male
Source and Reliability of Information: or patient advocate
Chief Complaint:
The patient experiences widespread scaly rash associated with itching and redness.
History of Present Illness:
The patient continues to experience psoriasis manifestations since the age of 5 years. However,
his initial medical assessment occurred in April-2000 that revealed a waxing and waning course
of psoriasis signs and symptoms. He experienced significant flares that were effectively treated
by the dermatologist. The patient’s mother, grandmother, and three brothers also experienced
psoriasis in the past. The patient’s family history of psoriasis potentially contributed to her
psoriasis severity in the context of inducing the development of her erythematous phenotypes
(Solmaz et al., 2019). The patient’s psoriasis manifestations substantially impact his health-
related quality of life and psychosocial outcomes. The consistent itching not only causes general
discomfort but also disrupts the quality of his sleep pattern (Jensen, Zachariae, Sskov, &
Zachariae, 2018). The patient reportedly reveals the occurrence of Fitzpatrick skin type II based
on pale skin and blonde hairs. The patient also experiences a high risk for skin peels, burns, and
freckles. His poor skin tanning warrants considerable protection against ultraviolet radiation.
Accordingly, the patient proves to be a subject of intense pulsed light and non-ablative
fractionated laser therapies (Knight & Kautz, 2019). The patient’s major symptoms are based on
the following attributes.
1. Location: The erythematous plaques widely invaginate the major portions of scalp, upper
trunk, and limbs
2. Quality: Dry, scaly, and well-demarcated erythematous psoriasis plaques/patches
surrounded with a silvery scale (Kim, Jerome, & Yeung, 2017)
Master of Nursing: Patient Assessment 1
Patient
SOAP Documentation
Date of History / Assessment: 2nd September 2019
General Patient Information: Robert: Age: 47 years Sex: male
Source and Reliability of Information: or patient advocate
Chief Complaint:
The patient experiences widespread scaly rash associated with itching and redness.
History of Present Illness:
The patient continues to experience psoriasis manifestations since the age of 5 years. However,
his initial medical assessment occurred in April-2000 that revealed a waxing and waning course
of psoriasis signs and symptoms. He experienced significant flares that were effectively treated
by the dermatologist. The patient’s mother, grandmother, and three brothers also experienced
psoriasis in the past. The patient’s family history of psoriasis potentially contributed to her
psoriasis severity in the context of inducing the development of her erythematous phenotypes
(Solmaz et al., 2019). The patient’s psoriasis manifestations substantially impact his health-
related quality of life and psychosocial outcomes. The consistent itching not only causes general
discomfort but also disrupts the quality of his sleep pattern (Jensen, Zachariae, Sskov, &
Zachariae, 2018). The patient reportedly reveals the occurrence of Fitzpatrick skin type II based
on pale skin and blonde hairs. The patient also experiences a high risk for skin peels, burns, and
freckles. His poor skin tanning warrants considerable protection against ultraviolet radiation.
Accordingly, the patient proves to be a subject of intense pulsed light and non-ablative
fractionated laser therapies (Knight & Kautz, 2019). The patient’s major symptoms are based on
the following attributes.
1. Location: The erythematous plaques widely invaginate the major portions of scalp, upper
trunk, and limbs
2. Quality: Dry, scaly, and well-demarcated erythematous psoriasis plaques/patches
surrounded with a silvery scale (Kim, Jerome, & Yeung, 2017)
Master of Nursing: Patient Assessment 1
Patient
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
2 | P a g e
3. Quantity (severity): The severity of widespread plaques has substantially increased in the
past few years
4. Timing (onset, duration, frequency): Chronic onset based on frequently reported waxes,
wanes, relapses, and flares from the age of 5 years until the date
5. Setting: Not related to setting
6. Aggravating and relieving factors (what makes it better or worse): The flares intensify
during winters; however, the administration of systemic medication sometimes reduces
the intensity of waxing and waning
7. Associated manifestations: Generalised pain and joint aches
Past Medical History:
1. Overall general health: The patient appears well oriented to person place and time. The
GCS (Glasgow Coma Scale) score of 14 effectively affirms his elevated consciousness
level (Jain, Teasdale, & Iverson, 2019, pp. 1-7).
2. Immunisation history: The patient’s medical record reveals his vaccination status based
on Diphtheria, Tetanus, Pertussis (DTaP), Polio (IPV), Measles, Mumps, Rubella (MMR)
Chickenpox (Varicella), Hepatitis A and B, H. influenzae (Hib), and Pneumococcal
(PCV13).
3. Allergies: Burning sensation following the administration of ultraviolet therapy based on
sensitive skin.
4. Past hospitalisations: Not reported.
5. Past medical: Plaque psoriasis and hypercholesterolaemia (care continues under the
supervision of general practitioner).
6. Psychiatric/mental disorders: Not reported.
7. Medications: The patient utilised topical creams and ointments including daivonex
50mcg/g cream, daiobet 50/500mcg/g ointment, diprosone 0.5mg/g cream, and Enstilar
50mcg/500mcg per 1g foam spray during the past 18 years. The systemic treatment
Master of Nursing: Patient Assessment 2
3. Quantity (severity): The severity of widespread plaques has substantially increased in the
past few years
4. Timing (onset, duration, frequency): Chronic onset based on frequently reported waxes,
wanes, relapses, and flares from the age of 5 years until the date
5. Setting: Not related to setting
6. Aggravating and relieving factors (what makes it better or worse): The flares intensify
during winters; however, the administration of systemic medication sometimes reduces
the intensity of waxing and waning
7. Associated manifestations: Generalised pain and joint aches
Past Medical History:
1. Overall general health: The patient appears well oriented to person place and time. The
GCS (Glasgow Coma Scale) score of 14 effectively affirms his elevated consciousness
level (Jain, Teasdale, & Iverson, 2019, pp. 1-7).
2. Immunisation history: The patient’s medical record reveals his vaccination status based
on Diphtheria, Tetanus, Pertussis (DTaP), Polio (IPV), Measles, Mumps, Rubella (MMR)
Chickenpox (Varicella), Hepatitis A and B, H. influenzae (Hib), and Pneumococcal
(PCV13).
3. Allergies: Burning sensation following the administration of ultraviolet therapy based on
sensitive skin.
4. Past hospitalisations: Not reported.
5. Past medical: Plaque psoriasis and hypercholesterolaemia (care continues under the
supervision of general practitioner).
6. Psychiatric/mental disorders: Not reported.
7. Medications: The patient utilised topical creams and ointments including daivonex
50mcg/g cream, daiobet 50/500mcg/g ointment, diprosone 0.5mg/g cream, and Enstilar
50mcg/500mcg per 1g foam spray during the past 18 years. The systemic treatment
Master of Nursing: Patient Assessment 2

3 | P a g e
includes methotrexate 10mg/week, cyclosporin >2mg/kg/day, neotigason/acitretin
>0.4mg/kg. The patient also received ultraviolet therapy three times per week, that he
could not continue based on the reported occurrence of burning sensation.
8. Habits: The patient does not effectively comply with the recommended
pharmacotherapeutic regimen. The patient is a homosexual male.
9. Sleep patterns: The patient continues to experience sleep disturbance under the impact of
sustained itching due to psoriasis (Czarnecka-Operacz et al., 2015).
10. Exercise habits/ health maintenance: The patient minimally engages himself in exercise
and physical activity.
11. Last menstrual period or date of menopause: Not applicable.
12. Education / cultural: The patient renders services on the profile of a musical supervisor
and also pays the organ inside a Church at Grafton.
Review of Systems:
A. General: NAD (No Abnormality Diagnosed).
B. Skin: Red, scaly and itchy rashes widely spread over upper trunk, limbs, and scalp despite
receiving systemic treatment for psoriasis.
C. Head/face/sinuses: No sinus complication and headache.
D. Eyes: No redness and pain; normal vision.
E. Ears: No vertigo or earache; normal hearing status.
F. Nose: No nasal bleeding or stiffness.
G. Mouth/throat: No sore tongue, hoarseness, or bleeding gums.
H. Neck: No neck pain or swollen glands.
I. Respiratory: No shortness of breath and cough.
Master of Nursing: Patient Assessment 3
includes methotrexate 10mg/week, cyclosporin >2mg/kg/day, neotigason/acitretin
>0.4mg/kg. The patient also received ultraviolet therapy three times per week, that he
could not continue based on the reported occurrence of burning sensation.
8. Habits: The patient does not effectively comply with the recommended
pharmacotherapeutic regimen. The patient is a homosexual male.
9. Sleep patterns: The patient continues to experience sleep disturbance under the impact of
sustained itching due to psoriasis (Czarnecka-Operacz et al., 2015).
10. Exercise habits/ health maintenance: The patient minimally engages himself in exercise
and physical activity.
11. Last menstrual period or date of menopause: Not applicable.
12. Education / cultural: The patient renders services on the profile of a musical supervisor
and also pays the organ inside a Church at Grafton.
Review of Systems:
A. General: NAD (No Abnormality Diagnosed).
B. Skin: Red, scaly and itchy rashes widely spread over upper trunk, limbs, and scalp despite
receiving systemic treatment for psoriasis.
C. Head/face/sinuses: No sinus complication and headache.
D. Eyes: No redness and pain; normal vision.
E. Ears: No vertigo or earache; normal hearing status.
F. Nose: No nasal bleeding or stiffness.
G. Mouth/throat: No sore tongue, hoarseness, or bleeding gums.
H. Neck: No neck pain or swollen glands.
I. Respiratory: No shortness of breath and cough.
Master of Nursing: Patient Assessment 3
4 | P a g e
J. Breasts and axillae: NAD.
K. Cardiovascular: Elevated triglycerides.
L. Peripheral vascular: No lump or mass.
M. Gastrointestinal: No indigestion or heartburn
N. Urinary: No hesitancy, urgency, or haematuria.
O. Genito-reproductive: NAD.
P. Musculoskeletal: Occasional joint pain.
Q. Neurological: No memory problem or headache.
R. Psychiatric: No depression, anxiety, mood changes, or nervousness.
S. Endocrine: No excessive hunger/sweating.
T. Hematological/coagulation: No bleeding and anaemia.
U. “Is there anything else you would like to add about your health and past illness?” None
Objective Information
Physical Examination:
A. Vital signs: BP-135/80, Temp-36.7, PR-76, RR-16 regular.
B. General survey: The patient appears well-oriented and well-groomed in shirt and long sleeve
pants.
C. Skin: Widespread red scaly rash manifested in terms of psoriatic plaques that impact more
than 50% area of the patient’s whole body. The PASI (Psoriasis Area and Severity Index) score
range of 15-18 affirms an elevated severity of the patient’s psoriasis. The rashes majorly occupy
the patient’s legs, trunk, upper extremities, neck, and head. The elevated PASI score is indicative
of severe clinical manifestations and poor prognosis (Fink, Uhlmann, Klose, & Haenssle, 2018).
Master of Nursing: Patient Assessment 4
J. Breasts and axillae: NAD.
K. Cardiovascular: Elevated triglycerides.
L. Peripheral vascular: No lump or mass.
M. Gastrointestinal: No indigestion or heartburn
N. Urinary: No hesitancy, urgency, or haematuria.
O. Genito-reproductive: NAD.
P. Musculoskeletal: Occasional joint pain.
Q. Neurological: No memory problem or headache.
R. Psychiatric: No depression, anxiety, mood changes, or nervousness.
S. Endocrine: No excessive hunger/sweating.
T. Hematological/coagulation: No bleeding and anaemia.
U. “Is there anything else you would like to add about your health and past illness?” None
Objective Information
Physical Examination:
A. Vital signs: BP-135/80, Temp-36.7, PR-76, RR-16 regular.
B. General survey: The patient appears well-oriented and well-groomed in shirt and long sleeve
pants.
C. Skin: Widespread red scaly rash manifested in terms of psoriatic plaques that impact more
than 50% area of the patient’s whole body. The PASI (Psoriasis Area and Severity Index) score
range of 15-18 affirms an elevated severity of the patient’s psoriasis. The rashes majorly occupy
the patient’s legs, trunk, upper extremities, neck, and head. The elevated PASI score is indicative
of severe clinical manifestations and poor prognosis (Fink, Uhlmann, Klose, & Haenssle, 2018).
Master of Nursing: Patient Assessment 4
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
5 | P a g e
D. Head/face/sinuses: The patient’s scalp and hairline are manifested with thickened, silvery-
white, and red scaly patches. His cranial and accessory nerves appear intact and functional.
E. Eyes: The patient’s pupils appear reactive and equal in diameter. No conjunctival pallor
noted. Two plaques across the patient’s right infraorbital ocular region reveal xanthelasma. The
patient utilises glasses for reading. He successfully qualified the visual acuity test after reading
the content on a standard chart. The patient exhibits normal extraocular movements in the
absence of nystagmus. The ophthalmoscopic exam reveals normal vasculature, optic disc, fundus,
and lens.
F. Ears: The patient does not exhibit any hearing complications. The ears appear normal in
shape and alignment with outer canthus. The otoscopic exam reveals normal cerumen without
any sign of fluid accumulation across the tympanic membrane.
G. Nose: The nares appear patent in the absence of drainage and septal deviation.
H. Mouth and pharynx: The oral structures do not reveal exudation, redness, or cyanosis. The
buccal mucosa, gums, roof of the mouth, sublingual mucosa, and teeth appear intact. No tongue
deviation or midline protrusion recorded. The patient exhibits gag reflex without any structural
abnormality in the pharynx and soft palate.
I. Neck: The lymph nodes appear normal in size. No tenderness recorded across submental,
tonsillar, occipital, postauricular, and preauricular regions. No tracheal tug or displacement
recorded.
J. Respiratory: The depth of the patient’s respiratory rate (i.e. 16) appears normal. The normal
rhythm and depth of breathing indicate the patient’s normal respiratory function. The chest
auscultation does not reveal crackles or wheezes. The patient does not use accessory muscles for
breathing. The chest wall appears symmetric with normal thoracic expansion.
K. Breasts and axillae: The inspection and palpation do not reveal any breast tissue abnormality.
No abnormality recorded in pectoral, sub-scapular, and lateral lymph nodes.
Master of Nursing: Patient Assessment 5
D. Head/face/sinuses: The patient’s scalp and hairline are manifested with thickened, silvery-
white, and red scaly patches. His cranial and accessory nerves appear intact and functional.
E. Eyes: The patient’s pupils appear reactive and equal in diameter. No conjunctival pallor
noted. Two plaques across the patient’s right infraorbital ocular region reveal xanthelasma. The
patient utilises glasses for reading. He successfully qualified the visual acuity test after reading
the content on a standard chart. The patient exhibits normal extraocular movements in the
absence of nystagmus. The ophthalmoscopic exam reveals normal vasculature, optic disc, fundus,
and lens.
F. Ears: The patient does not exhibit any hearing complications. The ears appear normal in
shape and alignment with outer canthus. The otoscopic exam reveals normal cerumen without
any sign of fluid accumulation across the tympanic membrane.
G. Nose: The nares appear patent in the absence of drainage and septal deviation.
H. Mouth and pharynx: The oral structures do not reveal exudation, redness, or cyanosis. The
buccal mucosa, gums, roof of the mouth, sublingual mucosa, and teeth appear intact. No tongue
deviation or midline protrusion recorded. The patient exhibits gag reflex without any structural
abnormality in the pharynx and soft palate.
I. Neck: The lymph nodes appear normal in size. No tenderness recorded across submental,
tonsillar, occipital, postauricular, and preauricular regions. No tracheal tug or displacement
recorded.
J. Respiratory: The depth of the patient’s respiratory rate (i.e. 16) appears normal. The normal
rhythm and depth of breathing indicate the patient’s normal respiratory function. The chest
auscultation does not reveal crackles or wheezes. The patient does not use accessory muscles for
breathing. The chest wall appears symmetric with normal thoracic expansion.
K. Breasts and axillae: The inspection and palpation do not reveal any breast tissue abnormality.
No abnormality recorded in pectoral, sub-scapular, and lateral lymph nodes.
Master of Nursing: Patient Assessment 5
6 | P a g e
L. Cardiovascular: The patient exhibits a normal breathing pattern. No clubbing of fingers,
splinter hemorrhages, peripheral oedema, and visible pulsations recorded. The blood pressure
assessment reveals the systolic/diastolic pressures of 135/75 mmHg. The radial pulse is recorded
as 16 per minute. The jugular venous pressure is recorded as 2.5cm at 45 degrees during the
inspection. The auscultation does not reveal the occurrence of mitral murmurs or abnormal
cardiac rhythm and rate. The palpation reveals normal carotid pulses.
M. Peripheral Vascular: The inspection did not reveal extremity oedema and varicosities. The
capillary refill time was recorded as 2 seconds. The palpation revealed 4+ bilateral dorsalis pedis,
femoral, and radial peripheral pulses.
N. Abdomen: The inspection does not reveal heaves, pulsations, and abdominal distention. The
auscultation reveals bowel sounds in the absence of abdominal arterial bruits. The percussion
does not reveal urinary bladder distention. However, abdominal quadrants do not reveal any pain
or tenderness. The palpation reveals normal liver border and aortic pulsation in the absence of
splenic enlargement, masses, and abdominal tenderness. The inguinal lymph nodes appear
inflamed.
O. Renal: The urinalysis reveals a pH of 6.5 and a specific gravity of 1.025. However, the
urinalysis findings do not reveal the occurrence of WBC nitrites, ketones, RBCs, protein, and
glucose. The kidneys appear normal in size and structure. The costovertebral angle does not
reveal any tenderness.
P. Genito-reproductive: The patient did not allow the physical assessment.
Q. Musculoskeletal: The patient’s movable joints reveal a normal range of motion. The feet and
legs exhibit normal alignment and mobility patterns. The patient also exhibits normal gait and
spine symmetry.
R. Neurological: The patient remains oriented to place, person, and time. He also appropriately
answers the open-ended questions. The mini-mental status exam does not reveal any abnormality.
The mental assessment reveals the appropriate judgment, problem-solving skills, memory,
concentration, and focus of the patient.
Master of Nursing: Patient Assessment 6
L. Cardiovascular: The patient exhibits a normal breathing pattern. No clubbing of fingers,
splinter hemorrhages, peripheral oedema, and visible pulsations recorded. The blood pressure
assessment reveals the systolic/diastolic pressures of 135/75 mmHg. The radial pulse is recorded
as 16 per minute. The jugular venous pressure is recorded as 2.5cm at 45 degrees during the
inspection. The auscultation does not reveal the occurrence of mitral murmurs or abnormal
cardiac rhythm and rate. The palpation reveals normal carotid pulses.
M. Peripheral Vascular: The inspection did not reveal extremity oedema and varicosities. The
capillary refill time was recorded as 2 seconds. The palpation revealed 4+ bilateral dorsalis pedis,
femoral, and radial peripheral pulses.
N. Abdomen: The inspection does not reveal heaves, pulsations, and abdominal distention. The
auscultation reveals bowel sounds in the absence of abdominal arterial bruits. The percussion
does not reveal urinary bladder distention. However, abdominal quadrants do not reveal any pain
or tenderness. The palpation reveals normal liver border and aortic pulsation in the absence of
splenic enlargement, masses, and abdominal tenderness. The inguinal lymph nodes appear
inflamed.
O. Renal: The urinalysis reveals a pH of 6.5 and a specific gravity of 1.025. However, the
urinalysis findings do not reveal the occurrence of WBC nitrites, ketones, RBCs, protein, and
glucose. The kidneys appear normal in size and structure. The costovertebral angle does not
reveal any tenderness.
P. Genito-reproductive: The patient did not allow the physical assessment.
Q. Musculoskeletal: The patient’s movable joints reveal a normal range of motion. The feet and
legs exhibit normal alignment and mobility patterns. The patient also exhibits normal gait and
spine symmetry.
R. Neurological: The patient remains oriented to place, person, and time. He also appropriately
answers the open-ended questions. The mini-mental status exam does not reveal any abnormality.
The mental assessment reveals the appropriate judgment, problem-solving skills, memory,
concentration, and focus of the patient.
Master of Nursing: Patient Assessment 6
7 | P a g e
Sensory: The patient qualifies the visual acuity test and exhibits normal smelling ability.
The corneal reflex appears positive, while the pupils equally respond to light while
following the directions of the eyes’ movement.
Motor: The patient does not report any abnormality related to hearing and facial
movements. Gag reflex appears normal. The patient does not report neck stiffness or pain.
The patient’s shrugging of shoulders reveals his normal scapular rotation activity (Choi et
al., 2015).
Cerebellar/Coordination/Basal nuclei: The patient’s normal body coordination and the
absence of tremors reveal his normal cerebellar function (Boisgontier et al., 2018).
Deep Tendon Reflexes (DRT): The DRT scale reveals a finding of 2+ (i.e. average level)
reveals the absence of neurological disease (Kim, 2015).
Superficial Reflex: The Babinski reflex reveals the patient’s normal structure and
physiological function of the cortical spinal tract (Acharya, Jamil, & Dewey, 2019).
S. Endocrine: The patient’s palpation and inspection of the thyroid gland reveal the absence of
goiter. The normal thyroid function test based on anti-TPO antibodies, free T-4 and TSH reveal
the absence of hyperthyroidism and hypothyroidism (Sheehan, 2016).
T. Nutritional Assessment: The patient’s weight, height, and BMI are recorded as 74kg, 160cm,
and 28.9 respectively. The patient’s BMI elevation substantially increases his risk of
cardiovascular complications and comorbidity/mortality (Khan, et al., 2018). However, his eating
habits are based on morning/afternoon tea and consumption of three meals per day. The patient
spends limited time in physical activities and his engagement in playing the piano is based on the
professional requirement. He is capable of preparing meals; however, does not effectively
accomplish his dietary requirements of minerals, vitamins, carbohydrates, fats, and proteins. The
patient actively purchases food items but does not possess sound knowledge related to his
metabolic demands and nutritional requirements.
Master of Nursing: Patient Assessment 7
Sensory: The patient qualifies the visual acuity test and exhibits normal smelling ability.
The corneal reflex appears positive, while the pupils equally respond to light while
following the directions of the eyes’ movement.
Motor: The patient does not report any abnormality related to hearing and facial
movements. Gag reflex appears normal. The patient does not report neck stiffness or pain.
The patient’s shrugging of shoulders reveals his normal scapular rotation activity (Choi et
al., 2015).
Cerebellar/Coordination/Basal nuclei: The patient’s normal body coordination and the
absence of tremors reveal his normal cerebellar function (Boisgontier et al., 2018).
Deep Tendon Reflexes (DRT): The DRT scale reveals a finding of 2+ (i.e. average level)
reveals the absence of neurological disease (Kim, 2015).
Superficial Reflex: The Babinski reflex reveals the patient’s normal structure and
physiological function of the cortical spinal tract (Acharya, Jamil, & Dewey, 2019).
S. Endocrine: The patient’s palpation and inspection of the thyroid gland reveal the absence of
goiter. The normal thyroid function test based on anti-TPO antibodies, free T-4 and TSH reveal
the absence of hyperthyroidism and hypothyroidism (Sheehan, 2016).
T. Nutritional Assessment: The patient’s weight, height, and BMI are recorded as 74kg, 160cm,
and 28.9 respectively. The patient’s BMI elevation substantially increases his risk of
cardiovascular complications and comorbidity/mortality (Khan, et al., 2018). However, his eating
habits are based on morning/afternoon tea and consumption of three meals per day. The patient
spends limited time in physical activities and his engagement in playing the piano is based on the
professional requirement. He is capable of preparing meals; however, does not effectively
accomplish his dietary requirements of minerals, vitamins, carbohydrates, fats, and proteins. The
patient actively purchases food items but does not possess sound knowledge related to his
metabolic demands and nutritional requirements.
Master of Nursing: Patient Assessment 7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

8 | P a g e
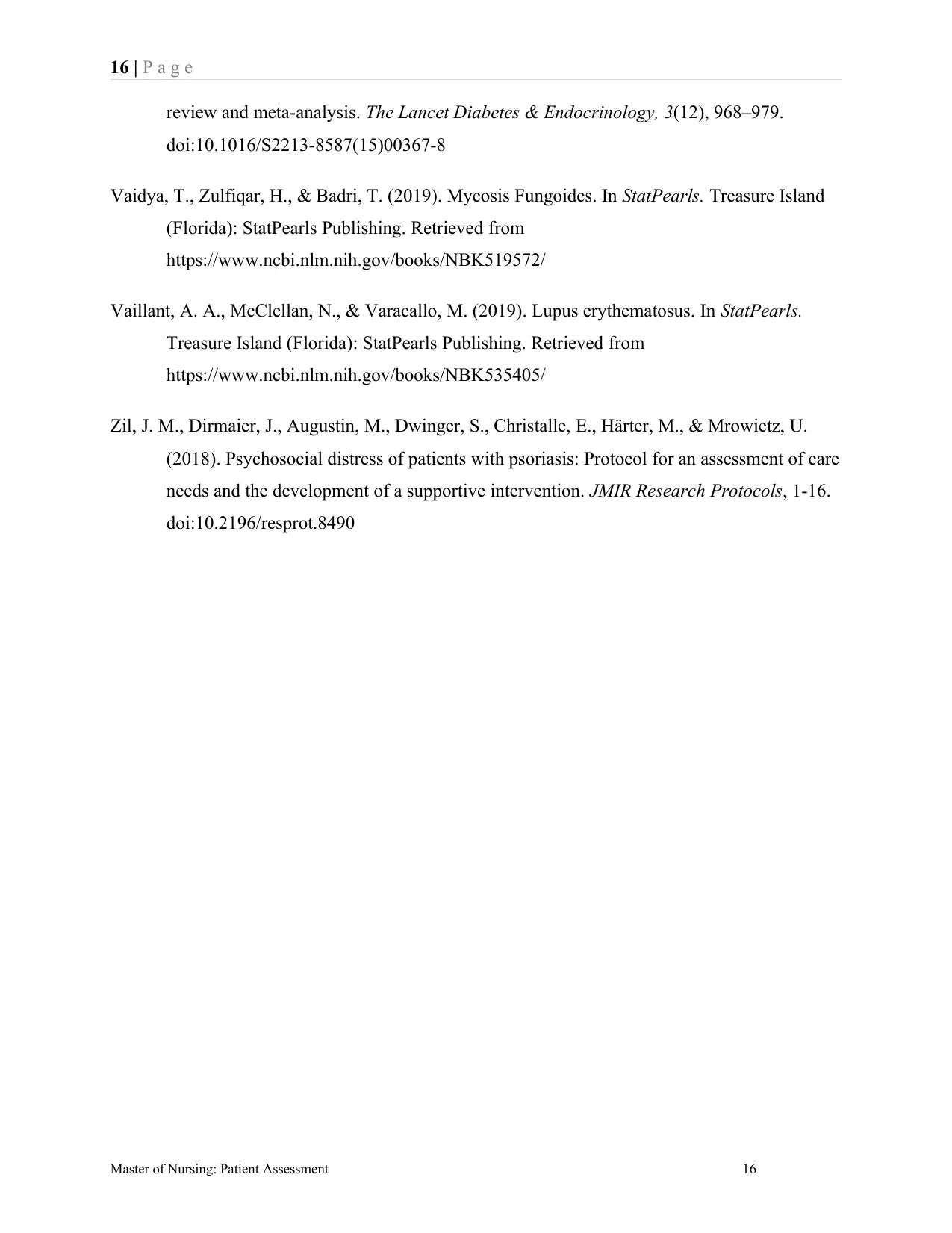
Laboratory Findings:
Refer to the appendix.
The Rationale for the Requested Tests:
The assessment of serum triglycerides/HDL cholesterol is based on the patient’s reported
hypercholesterolaemia. Accordingly, the assessment of serum triglycerides is required to evaluate
the patient’s risk for cardiovascular disease or atherosclerosis (Soran et al., 2018). The secondary
causes associated with the patient’s triglyceride elevation might include cholestasis, nephrotic
syndrome, hyperglycaemia, and hypothyroidism (Ibrahim & Jialal, 2019). Accordingly,
triglyceride assessment is also required to effectively rule out these secondary comorbidities.
Psoriasis proves to be a significant risk factor for the development of non-alcoholic fatty liver
disease (Prussick, Prussick, & Nussbaum, 2015). The administration of systemic medication also
elevates the patient’s risk of hepatic complications. Accordingly, ALT (alanine transaminase)
assessment and liver function tests are effectively undertaken to rule out toxic hepatitis and/or
other potential liver complications (Liu, Que, Xu, & Peng, 2014). The administration of
complete/full blood count is undertaken to evaluate the influence of systemic medication on the
patient’s inflammatory psoriatic pathways (Rendon & Schäkel, 2019). The midstream urine
specimen evaluation is undertaken to rule out the patient’s urinary tract infection comorbidity
(Holm & Aabenhus, 2016). Furthermore, the client’s cultural conventions do not restrict the
administration of diagnostic modalities for the systematic assessment of serum triglycerides,
ALT, FBC. LFT, HDL cholesterol, and MSU. These recommended minimally invasive
diagnostic interventions also remain highly accessible to the patient without causing any
significant inconvenience.
Assessment:
A. Differential diagnoses:
The patient’s differential diagnoses are based on the following disease conditions.
1. Dermatitis: The flares of itching, redness, and rashes across the patient’s trunk and extremities
substantiate the requirement of ruling out atopic dermatitis based on aetiology and causative
factors (Griffiths, Kerkhof, & Czarnecka-Operacz, 2017). Since the burden of psoriasis is directly
Master of Nursing: Patient Assessment 8
Laboratory Findings:
Refer to the appendix.
The Rationale for the Requested Tests:
The assessment of serum triglycerides/HDL cholesterol is based on the patient’s reported
hypercholesterolaemia. Accordingly, the assessment of serum triglycerides is required to evaluate
the patient’s risk for cardiovascular disease or atherosclerosis (Soran et al., 2018). The secondary
causes associated with the patient’s triglyceride elevation might include cholestasis, nephrotic
syndrome, hyperglycaemia, and hypothyroidism (Ibrahim & Jialal, 2019). Accordingly,
triglyceride assessment is also required to effectively rule out these secondary comorbidities.
Psoriasis proves to be a significant risk factor for the development of non-alcoholic fatty liver
disease (Prussick, Prussick, & Nussbaum, 2015). The administration of systemic medication also
elevates the patient’s risk of hepatic complications. Accordingly, ALT (alanine transaminase)
assessment and liver function tests are effectively undertaken to rule out toxic hepatitis and/or
other potential liver complications (Liu, Que, Xu, & Peng, 2014). The administration of
complete/full blood count is undertaken to evaluate the influence of systemic medication on the
patient’s inflammatory psoriatic pathways (Rendon & Schäkel, 2019). The midstream urine
specimen evaluation is undertaken to rule out the patient’s urinary tract infection comorbidity
(Holm & Aabenhus, 2016). Furthermore, the client’s cultural conventions do not restrict the
administration of diagnostic modalities for the systematic assessment of serum triglycerides,
ALT, FBC. LFT, HDL cholesterol, and MSU. These recommended minimally invasive
diagnostic interventions also remain highly accessible to the patient without causing any
significant inconvenience.
Assessment:
A. Differential diagnoses:
The patient’s differential diagnoses are based on the following disease conditions.
1. Dermatitis: The flares of itching, redness, and rashes across the patient’s trunk and extremities
substantiate the requirement of ruling out atopic dermatitis based on aetiology and causative
factors (Griffiths, Kerkhof, & Czarnecka-Operacz, 2017). Since the burden of psoriasis is directly
Master of Nursing: Patient Assessment 8
9 | P a g e
related to psychological comorbidities, the patient’s allergy testing is highly needed to identify
the onset of atopic dermatitis based on the appearance of dry scaly rashes. Furthermore, the
patient’s sensitive skin remains highly predisposed to the development of allergic conditions. The
patient’s family history of skin complications, early-onset, and dryness of skin include some of
the potential complications that appear common with the clinical manifestations of psoriasis
(Thomsen, 2014). Accordingly, the differentiation of dermatitis from psoriasis is essentially
needed to retrieve the definitive diagnosis.
2. Lupus Erythematosus: The patient’s skin sensitivity or photosensitivity, joint pain, and red
raised patches over the skin raise the suspicion of lupus erythematosus (Vaillant, McClellan, &
Varacallo, 2019). Accordingly, the assessment of antinuclear/antiphospholipid antibodies is
highly needed to evaluate the aetiology of the suspected disease condition. Lupus erythematosus
is a multifactorial disease condition that impacts the immune tolerance of the patient under the
impact of environmental factors. The generation of pathogenic autoantibodies under the impact of
lupus erythematosus deteriorates the tissue structure while inducing several pathophysiological
pathways including neutrophil activation, complement fixation, and immune complex deposition.
Since the disease potentially damages the skin surface, the assessment of antinuclear antibodies
and lupus band test are essentially required to rule out or affirm its occurrence in the affected
patient.
3. Mycosis Fungoides: The differential diagnosis of mycosis fungoides is based on the reported
occurrence of skin plaques and patches that manifest through the development of scaly atrophic
lesions (Vaidya, Zulfiqar, & Badri, 2019). These plaques also raise the suspicion of parapsoriasis
that could eventually acquire the shape of erythematous-purplish papules. Accordingly, the
assessment of the reported skin plaques is required to effectively evaluate the TCR gene
rearrangement clonality. The staging of the reported skin patches is also needed to differentiate or
rule out mycosis fungoides as compared to psoriasis.
B. Actual, Confirmed diagnoses and problems:
1. The chronic plaque psoriasis is majorly based on the patient’s genetic predisposition and
family history (Badri, Kumar, & Oakley, 2019). The acute onset of the patient’s chronic plaque is
reflected through variable waxing and waning.
Master of Nursing: Patient Assessment 9
related to psychological comorbidities, the patient’s allergy testing is highly needed to identify
the onset of atopic dermatitis based on the appearance of dry scaly rashes. Furthermore, the
patient’s sensitive skin remains highly predisposed to the development of allergic conditions. The
patient’s family history of skin complications, early-onset, and dryness of skin include some of
the potential complications that appear common with the clinical manifestations of psoriasis
(Thomsen, 2014). Accordingly, the differentiation of dermatitis from psoriasis is essentially
needed to retrieve the definitive diagnosis.
2. Lupus Erythematosus: The patient’s skin sensitivity or photosensitivity, joint pain, and red
raised patches over the skin raise the suspicion of lupus erythematosus (Vaillant, McClellan, &
Varacallo, 2019). Accordingly, the assessment of antinuclear/antiphospholipid antibodies is
highly needed to evaluate the aetiology of the suspected disease condition. Lupus erythematosus
is a multifactorial disease condition that impacts the immune tolerance of the patient under the
impact of environmental factors. The generation of pathogenic autoantibodies under the impact of
lupus erythematosus deteriorates the tissue structure while inducing several pathophysiological
pathways including neutrophil activation, complement fixation, and immune complex deposition.
Since the disease potentially damages the skin surface, the assessment of antinuclear antibodies
and lupus band test are essentially required to rule out or affirm its occurrence in the affected
patient.
3. Mycosis Fungoides: The differential diagnosis of mycosis fungoides is based on the reported
occurrence of skin plaques and patches that manifest through the development of scaly atrophic
lesions (Vaidya, Zulfiqar, & Badri, 2019). These plaques also raise the suspicion of parapsoriasis
that could eventually acquire the shape of erythematous-purplish papules. Accordingly, the
assessment of the reported skin plaques is required to effectively evaluate the TCR gene
rearrangement clonality. The staging of the reported skin patches is also needed to differentiate or
rule out mycosis fungoides as compared to psoriasis.
B. Actual, Confirmed diagnoses and problems:
1. The chronic plaque psoriasis is majorly based on the patient’s genetic predisposition and
family history (Badri, Kumar, & Oakley, 2019). The acute onset of the patient’s chronic plaque is
reflected through variable waxing and waning.
Master of Nursing: Patient Assessment 9
10 | P a g e
2. The patient’s arthralgia is probably the outcome of suspected psoriatic arthritis (Sankowski,
Łebkowska, Ćwikła, Walecka, & Walecki, 2013).
3. The patient’s hypercholesterolaemia is reportedly based on his sedentary lifestyle and
physical activity limitation (Ibrahim & Jialal, 2019).
Plan:
A. Non-pharmacologic management
The non-pharmacologic management of the patient’s psoriasis is based on the administration of
psychosocial support to effectively reduce his sleeping problems and enhance the overall health-
related behaviour (Zil et al., 2018). The nurse practitioner requires utilising therapeutic
communication to emphasise the use of medicated soap, scalp care shampoo, and skin cleanser to
reduce the intensity of itching/burning sensation. Furthermore, the proactive prevention of throat
infection is highly needed through the utilisation of mouth wash and over-the-counter antibiotics.
The nurse practitioner requires administering a diet based on low carbohydrate/salt/fat not only to
reduce the patient’s weight but also to control his hypercholesterolaemia (Tobias, et al., 2015).
The exercise management for the patient is also recommended for enhancing his cardiovascular
physiology.
B. Pharmacologic management
The utilisation of pharmacotherapy in the presented case is not recommended based on the
reported failure/side-effects of various systemic and topical drugs (described under medication
history). However, the intravenous or subcutaneous administration of biological response
modifiers or biologic therapies will assist in controlling the patient’s immune system-mediated
inflammatory complications (Rønholt & Iversen, 2017). For example, the subcutaneously
administered Ustekinumab – Stelara (45mg) will require repetition for a duration of 4-weeks
followed by 12-weekly administration. The nurse practitioner will require evaluating the patient
for tuberculosis before the initiation of biologic therapy. The administration of rosuvastatin
(20mg) is required for the management of hypercholesterolaemia (Hu & Tomlinson, 2013). The
administration of NSAIDs (for example, ibuprofen (SOS) – 200/400 mg) is required for the
therapeutic management of the patient’s joint pain (Ngo & Bajaj, 2019).
Master of Nursing: Patient Assessment 10
2. The patient’s arthralgia is probably the outcome of suspected psoriatic arthritis (Sankowski,
Łebkowska, Ćwikła, Walecka, & Walecki, 2013).
3. The patient’s hypercholesterolaemia is reportedly based on his sedentary lifestyle and
physical activity limitation (Ibrahim & Jialal, 2019).
Plan:
A. Non-pharmacologic management
The non-pharmacologic management of the patient’s psoriasis is based on the administration of
psychosocial support to effectively reduce his sleeping problems and enhance the overall health-
related behaviour (Zil et al., 2018). The nurse practitioner requires utilising therapeutic
communication to emphasise the use of medicated soap, scalp care shampoo, and skin cleanser to
reduce the intensity of itching/burning sensation. Furthermore, the proactive prevention of throat
infection is highly needed through the utilisation of mouth wash and over-the-counter antibiotics.
The nurse practitioner requires administering a diet based on low carbohydrate/salt/fat not only to
reduce the patient’s weight but also to control his hypercholesterolaemia (Tobias, et al., 2015).
The exercise management for the patient is also recommended for enhancing his cardiovascular
physiology.
B. Pharmacologic management
The utilisation of pharmacotherapy in the presented case is not recommended based on the
reported failure/side-effects of various systemic and topical drugs (described under medication
history). However, the intravenous or subcutaneous administration of biological response
modifiers or biologic therapies will assist in controlling the patient’s immune system-mediated
inflammatory complications (Rønholt & Iversen, 2017). For example, the subcutaneously
administered Ustekinumab – Stelara (45mg) will require repetition for a duration of 4-weeks
followed by 12-weekly administration. The nurse practitioner will require evaluating the patient
for tuberculosis before the initiation of biologic therapy. The administration of rosuvastatin
(20mg) is required for the management of hypercholesterolaemia (Hu & Tomlinson, 2013). The
administration of NSAIDs (for example, ibuprofen (SOS) – 200/400 mg) is required for the
therapeutic management of the patient’s joint pain (Ngo & Bajaj, 2019).
Master of Nursing: Patient Assessment 10
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
11 | P a g e
C. Patient/family education
The organisation of patient/family education sessions is highly needed to effectively improve
knowledge of the patient and his caretakers regarding infection risk factors and other
comorbidities associated with psoriasis. Family education is also required to facilitate the shared
decision-making process in the context of selecting the most appropriate treatment options for the
patient’s psoriasis, arthralgia, and hypercholesterolaemia (Bae, 2017). The nurse practitioner
needs to encourage the patient’s engagement in a healthy diet and exercise in the context of
improving his cholesterol/ALT level and cardiovascular outcomes.
D. Follow up
The nurse practitioner will need to undertake the patient’s urinalysis (before dermatologist
appointment) for the assessment of his protein level to rule out proteinuria (based on rosuvastatin
administration) (Idzerda, Pena, Parving, de-Zeeuw, & Heerspink, 2019). The patient’s 6-monthly
nursing/dermatological assessment is highly needed to improve the provision of concomitant
therapy.
E. Referrals
The patient will require obtaining PBS approval from Medicare (AGDOHS, 2019). He will also
need to coordinate with the Biologics nurse practitioner in the context of sharing his demographic
details. The referral to the rheumatologist will substantiate the joint pain assessment through x-
ray intervention. Furthermore, the patient’s referral to a dermatologist is based on the requirement
of regular skin assessment.
F. Evaluation
The patient’s PASI (Psoriasis Area Severity Index) assessment will assist in evaluating the
intensity of psoriasis following the administration of recommended treatment (Talamonti et al.,
2018). The assessment of LFT, UEC, and FBE tests will help in evaluating the patient’s hepatic
physiology, renal function, and immune system outcomes (Gounden & Jialal, 2019). These
assessments are essentially required to evaluate/rule out the onset of comorbidities that might
develop under the impact of psoriasis or recommended therapy. The assessment of joint pain and
BMI is required to rule out the occurrence of psoriatic arthritis and obesity (Klingberg et al.,
Master of Nursing: Patient Assessment 11
C. Patient/family education
The organisation of patient/family education sessions is highly needed to effectively improve
knowledge of the patient and his caretakers regarding infection risk factors and other
comorbidities associated with psoriasis. Family education is also required to facilitate the shared
decision-making process in the context of selecting the most appropriate treatment options for the
patient’s psoriasis, arthralgia, and hypercholesterolaemia (Bae, 2017). The nurse practitioner
needs to encourage the patient’s engagement in a healthy diet and exercise in the context of
improving his cholesterol/ALT level and cardiovascular outcomes.
D. Follow up
The nurse practitioner will need to undertake the patient’s urinalysis (before dermatologist
appointment) for the assessment of his protein level to rule out proteinuria (based on rosuvastatin
administration) (Idzerda, Pena, Parving, de-Zeeuw, & Heerspink, 2019). The patient’s 6-monthly
nursing/dermatological assessment is highly needed to improve the provision of concomitant
therapy.
E. Referrals
The patient will require obtaining PBS approval from Medicare (AGDOHS, 2019). He will also
need to coordinate with the Biologics nurse practitioner in the context of sharing his demographic
details. The referral to the rheumatologist will substantiate the joint pain assessment through x-
ray intervention. Furthermore, the patient’s referral to a dermatologist is based on the requirement
of regular skin assessment.
F. Evaluation
The patient’s PASI (Psoriasis Area Severity Index) assessment will assist in evaluating the
intensity of psoriasis following the administration of recommended treatment (Talamonti et al.,
2018). The assessment of LFT, UEC, and FBE tests will help in evaluating the patient’s hepatic
physiology, renal function, and immune system outcomes (Gounden & Jialal, 2019). These
assessments are essentially required to evaluate/rule out the onset of comorbidities that might
develop under the impact of psoriasis or recommended therapy. The assessment of joint pain and
BMI is required to rule out the occurrence of psoriatic arthritis and obesity (Klingberg et al.,
Master of Nursing: Patient Assessment 11

12 | P a g e
2019). The assessment of the lipid profile is also required to evaluate the patient’s HDL and
serum triglyceride following their therapeutic management (França, Mendes, & Ferreira, 2018).
References
Acharya, A. B., Jamil, R. T., & Dewey, J. J. (2019). Babinski reflex. In StatPearls. Treasure
Island (Florida): StatPearls Publishing. Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK519009/
AGDOHS. (2019, 09 20). PBS Authorities. Retrieved from Australian Government Department
of Human Services: https://www.humanservices.gov.au/organisations/health-
professionals/services/medicare/pbs-prescribers/managing/pbs-authorities
Badri, T., Kumar, P., & Oakley, A. M. (2019). Plaque psoriasis. In StatPearls. Treasure Island
(Florida): StatPearls Publishing. Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK430879/
Bae, J. M. (2017). Shared decision making: relevant concepts and facilitating strategies.
Epidemiology and Health, 1-5. doi:10.4178/epih.e2017048
Boisgontier, M. P., Cheval, B., van-Ruitenbeek , P., Cuypers , K., Leunissen , I., Sunaert , S., . . .
Swinnen , S. P. (2018). Cerebellar gray matter explains bimanual coordination
performance in children and older adults. Neurobiology of Aging, 109-120.
doi:10.1016/j.neurobiolaging.2018.01.016
Choi, W. J., Cynn, H. S., Lee, C. H., Jeon, H. S., Lee, J. H., Jeong, H. J., & Yoon, T. L. (2015).
Shrug exercises combined with shoulder abduction improve scapular upward rotator
activity and scapular alignment in subjects with scapular downward rotation impairment.
Journal of Electromyography and Kinesiology, 25(2), 363-370.
doi:10.1016/j.jelekin.2014.12.001
Czarnecka-Operacz, M., Polańska, A., Klimańska, M., Teresiak-Mikołajczak, E., Molińska-
Glura, M., Adamski, Z., & Jenerowicz, D. (2015). Itching sensation in psoriatic patients
and its relation to body mass index and IL-17 and IL-31 concentrations. Advances in
Dermatology and Allergology, 32(6), 426-430. doi:10.5114/pdia.2015.56097
Master of Nursing: Patient Assessment 12
2019). The assessment of the lipid profile is also required to evaluate the patient’s HDL and
serum triglyceride following their therapeutic management (França, Mendes, & Ferreira, 2018).
References
Acharya, A. B., Jamil, R. T., & Dewey, J. J. (2019). Babinski reflex. In StatPearls. Treasure
Island (Florida): StatPearls Publishing. Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK519009/
AGDOHS. (2019, 09 20). PBS Authorities. Retrieved from Australian Government Department
of Human Services: https://www.humanservices.gov.au/organisations/health-
professionals/services/medicare/pbs-prescribers/managing/pbs-authorities
Badri, T., Kumar, P., & Oakley, A. M. (2019). Plaque psoriasis. In StatPearls. Treasure Island
(Florida): StatPearls Publishing. Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK430879/
Bae, J. M. (2017). Shared decision making: relevant concepts and facilitating strategies.
Epidemiology and Health, 1-5. doi:10.4178/epih.e2017048
Boisgontier, M. P., Cheval, B., van-Ruitenbeek , P., Cuypers , K., Leunissen , I., Sunaert , S., . . .
Swinnen , S. P. (2018). Cerebellar gray matter explains bimanual coordination
performance in children and older adults. Neurobiology of Aging, 109-120.
doi:10.1016/j.neurobiolaging.2018.01.016
Choi, W. J., Cynn, H. S., Lee, C. H., Jeon, H. S., Lee, J. H., Jeong, H. J., & Yoon, T. L. (2015).
Shrug exercises combined with shoulder abduction improve scapular upward rotator
activity and scapular alignment in subjects with scapular downward rotation impairment.
Journal of Electromyography and Kinesiology, 25(2), 363-370.
doi:10.1016/j.jelekin.2014.12.001
Czarnecka-Operacz, M., Polańska, A., Klimańska, M., Teresiak-Mikołajczak, E., Molińska-
Glura, M., Adamski, Z., & Jenerowicz, D. (2015). Itching sensation in psoriatic patients
and its relation to body mass index and IL-17 and IL-31 concentrations. Advances in
Dermatology and Allergology, 32(6), 426-430. doi:10.5114/pdia.2015.56097
Master of Nursing: Patient Assessment 12
13 | P a g e
Fink, C., Uhlmann, L., Klose, C., & Haenssle, H. A. (2018). Automated, computer-guided PASI
measurements by digital image analysis versus conventional physicians’ PASI
calculations: study protocol for a comparative, single-centre, observational study. BMJ
Open, 1-4. doi:10.1136/bmjopen-2017-018461
França, C. N., Mendes, C. C., & Ferreira, C. E. (2018). Time collection and storage conditions of
lipid profile. Brazilian Journal of Medical and Biological Research, 1-4.
doi:10.1590/1414-431X20176955
Gounden, V., & Jialal, I. (2019). Renal function tests. In StatPearls. Treasure Island (Florida):
StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK507821/
Griffiths, C. E., Kerkhof, P. V., & Czarnecka-Operacz, M. (2017). Psoriasis and atopic
dermatitis. Dermatology and therapy, 7(1), 31-41. doi:10.1007/s13555-016-0167-9
Holm, A., & Aabenhus, R. (2016). Urine sampling techniques in symptomatic primary-care
patients: a diagnostic accuracy review. BMC Family Practice, 1-9. doi:10.1186/s12875-
016-0465-4
Hu, M., & Tomlinson, B. (2013). Current perspectives on rosuvastatin. Integrated Blood
Pressure Control, 15-25. doi:10.2147/IBPC.S34814
Ibrahim , M. A., & Jialal, I. (2019). Hypercholesterolemia. In StatPearls. Treasure Island
(Florida): StatPearls Publishing. Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK459188/
Idzerda, N. M., Pena, M. J., Parving , H. H., de-Zeeuw, D., & Heerspink , H. J. (2019).
Proteinuria and cholesterol reduction are independently associated with less renal function
decline in statin-treated patients; a post hoc analysis of the PLANET trials. Nephrology,
Dialysis, Transplantation, 34(10), 1699-1706. doi:10.1093/ndt/gfy159
Jain, S., Teasdale, G. M., & Iverson, L. M. (2019). Glasgow Coma Scale. In StatPearls (pp. 1-7).
Treasure Island (Florida): StatPearls Publishing. Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK513298/
Master of Nursing: Patient Assessment 13
Fink, C., Uhlmann, L., Klose, C., & Haenssle, H. A. (2018). Automated, computer-guided PASI
measurements by digital image analysis versus conventional physicians’ PASI
calculations: study protocol for a comparative, single-centre, observational study. BMJ
Open, 1-4. doi:10.1136/bmjopen-2017-018461
França, C. N., Mendes, C. C., & Ferreira, C. E. (2018). Time collection and storage conditions of
lipid profile. Brazilian Journal of Medical and Biological Research, 1-4.
doi:10.1590/1414-431X20176955
Gounden, V., & Jialal, I. (2019). Renal function tests. In StatPearls. Treasure Island (Florida):
StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK507821/
Griffiths, C. E., Kerkhof, P. V., & Czarnecka-Operacz, M. (2017). Psoriasis and atopic
dermatitis. Dermatology and therapy, 7(1), 31-41. doi:10.1007/s13555-016-0167-9
Holm, A., & Aabenhus, R. (2016). Urine sampling techniques in symptomatic primary-care
patients: a diagnostic accuracy review. BMC Family Practice, 1-9. doi:10.1186/s12875-
016-0465-4
Hu, M., & Tomlinson, B. (2013). Current perspectives on rosuvastatin. Integrated Blood
Pressure Control, 15-25. doi:10.2147/IBPC.S34814
Ibrahim , M. A., & Jialal, I. (2019). Hypercholesterolemia. In StatPearls. Treasure Island
(Florida): StatPearls Publishing. Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK459188/
Idzerda, N. M., Pena, M. J., Parving , H. H., de-Zeeuw, D., & Heerspink , H. J. (2019).
Proteinuria and cholesterol reduction are independently associated with less renal function
decline in statin-treated patients; a post hoc analysis of the PLANET trials. Nephrology,
Dialysis, Transplantation, 34(10), 1699-1706. doi:10.1093/ndt/gfy159
Jain, S., Teasdale, G. M., & Iverson, L. M. (2019). Glasgow Coma Scale. In StatPearls (pp. 1-7).
Treasure Island (Florida): StatPearls Publishing. Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK513298/
Master of Nursing: Patient Assessment 13
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
14 | P a g e
Jensen, P., Zachariae , C., Sskov, L., & Zachariae , R. (2018). Sleep disturbance in psoriasis: A
case-controlled study. The British Journal of Dermatology, 179(6), 1376-1384.
doi:10.1111/bjd.16702
Khan, S. S., Ning, H., Wilkins, J. T., Allen, N., Carnethon, M., Berry, J. D., . . . Lloyd-Jones , D.
M. (2018). Association of body mass index with lifetime risk of cardiovascular disease
and compression of morbidity. JAMA Cardiology, 3(4), 280-287.
doi:10.1001/jamacardio.2018.0022
Kim, W. B., Jerome, D., & Yeung, J. (2017). Diagnosis and management of psoriasis. Can Fam
Physician, 63(4), 278-285. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5389757/
Kim, Y. W. (2015). Clinical availability of the deep tendon reflex test using a novel apparatus in
healthy subjects. Journal of Physical Therapy Science, 27(2), 317-320.
doi:10.1589/jpts.27.317
Klingberg, E., Bilberg, A., Björkman, S., Hedberg, M., Jacobsson, L., Forsblad-d’Elia, H., . . .
Larsson, I. (2019). Weight loss improves disease activity in patients with psoriatic
arthritis and obesity: an interventional study. Arthritis Research and Therapy, 1-10.
doi:10.1186/s13075-019-1810-5
Knight, J. M., & Kautz, G. (2019). Sequential facial skin rejuvenation with intense pulsed light
and non ablative fractionated laser resurfacing in fitzpatrick skin type II–IV patients: A‐
prospective multicenter analysis. Lasers in Surgery and Medicine, 141-149.
doi:10.1002/lsm.23007
Liu, Z., Que, S., Xu, J., & Peng, T. (2014). Alanine aminotransferase-old biomarker and new
concept: A review. International Journal of Medical Sciences, 925-935.
doi:10.7150/ijms.8951
Ngo, V. T., & Bajaj, T. (2019). Ibuprofen. In StatPearls. Treasure Island (Florida): StatPearls
Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK542299/
Prussick, R., Prussick, L., & Nussbaum, D. (2015). Nonalcoholic Fatty Liver Disease and
Psoriasis-What a Dermatologist Needs to Know. The Journal of Clinical Aesthetic
Master of Nursing: Patient Assessment 14
Jensen, P., Zachariae , C., Sskov, L., & Zachariae , R. (2018). Sleep disturbance in psoriasis: A
case-controlled study. The British Journal of Dermatology, 179(6), 1376-1384.
doi:10.1111/bjd.16702
Khan, S. S., Ning, H., Wilkins, J. T., Allen, N., Carnethon, M., Berry, J. D., . . . Lloyd-Jones , D.
M. (2018). Association of body mass index with lifetime risk of cardiovascular disease
and compression of morbidity. JAMA Cardiology, 3(4), 280-287.
doi:10.1001/jamacardio.2018.0022
Kim, W. B., Jerome, D., & Yeung, J. (2017). Diagnosis and management of psoriasis. Can Fam
Physician, 63(4), 278-285. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5389757/
Kim, Y. W. (2015). Clinical availability of the deep tendon reflex test using a novel apparatus in
healthy subjects. Journal of Physical Therapy Science, 27(2), 317-320.
doi:10.1589/jpts.27.317
Klingberg, E., Bilberg, A., Björkman, S., Hedberg, M., Jacobsson, L., Forsblad-d’Elia, H., . . .
Larsson, I. (2019). Weight loss improves disease activity in patients with psoriatic
arthritis and obesity: an interventional study. Arthritis Research and Therapy, 1-10.
doi:10.1186/s13075-019-1810-5
Knight, J. M., & Kautz, G. (2019). Sequential facial skin rejuvenation with intense pulsed light
and non ablative fractionated laser resurfacing in fitzpatrick skin type II–IV patients: A‐
prospective multicenter analysis. Lasers in Surgery and Medicine, 141-149.
doi:10.1002/lsm.23007
Liu, Z., Que, S., Xu, J., & Peng, T. (2014). Alanine aminotransferase-old biomarker and new
concept: A review. International Journal of Medical Sciences, 925-935.
doi:10.7150/ijms.8951
Ngo, V. T., & Bajaj, T. (2019). Ibuprofen. In StatPearls. Treasure Island (Florida): StatPearls
Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK542299/
Prussick, R., Prussick, L., & Nussbaum, D. (2015). Nonalcoholic Fatty Liver Disease and
Psoriasis-What a Dermatologist Needs to Know. The Journal of Clinical Aesthetic
Master of Nursing: Patient Assessment 14
15 | P a g e
Dermatology, 8(3), 43-45. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4382145/
Rendon , A., & Schäkel, K. (2019). Psoriasis pathogenesis and treatment. International Journal
of Molecular Sciences, 20(6), 1-28. doi:10.3390/ijms20061475
Rønholt, K., & Iversen, L. (2017). Old and new biological therapies for psoriasis. International
Journal of Molecular Sciences, 18(11), 1-23. doi:10.3390/ijms18112297
Sankowski, A. J., Łebkowska, U. M., Ćwikła, J., Walecka, I., & Walecki, J. (2013). Psoriatic
arthritis. Polish Journal of Radiology, 78(1), 7-17. doi:10.12659/PJR.883763
Sheehan, M. T. (2016). Biochemical testing of the thyroid: TSH is the best and, oftentimes, only
test needed – A review for primary care. Clinical medicine and research, 14(2), 83-92.
doi:10.3121/cmr.2016.1309
Solmaz, D., Bakirci , S., Kimyon, G., Kasapoglu, G. E., Dogru, A., Bayindir, O., . . . Aydin , S.
Z. (2019). The impact of having family history of psoriasis or psoriatic arthritis on
psoriatic disease. Arthritis Care and Research. doi:10.1002/acr.23836
Soran, H., Adam, S., Mohammad, J. B., Ho, J. H., Schofield, J. D., Kwok, S., . . . Durrington, P.
N. (2018). Hypercholesterolaemia – practical information for non-specialists. Archives of
Medical Science, 14(1), 1-21. doi:10.5114/aoms.2018.72238
Talamonti, M., Galluzzo , M., Bernardini , N., Caldarola , G., Persechino , S., Cantoresi , F., . . .
Bianchi, L. (2018). Psoriasis Area and Severity Index response in moderate-severe
psoriatic patients switched to adalimumab: Results from the OPPSA study. Journal of the
European Academy of Dermatology and Venerology, 32(10), 1737-1744.
doi:10.1111/jdv.15077
Thomsen, S. F. (2014). Atopic dermatitis: Natural history, diagnosis, and treatment. ISRN
Allergy, 1-7. doi:10.1155/2014/354250
Tobias, D. K., Chen, M., Manson, J. E., Ludwig, D. S., Willett, W., & Hu, F. B. (2015). Effect of
low-fat vs. other diet interventions on long-term weight change in adults: A systematic
Master of Nursing: Patient Assessment 15
Dermatology, 8(3), 43-45. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4382145/
Rendon , A., & Schäkel, K. (2019). Psoriasis pathogenesis and treatment. International Journal
of Molecular Sciences, 20(6), 1-28. doi:10.3390/ijms20061475
Rønholt, K., & Iversen, L. (2017). Old and new biological therapies for psoriasis. International
Journal of Molecular Sciences, 18(11), 1-23. doi:10.3390/ijms18112297
Sankowski, A. J., Łebkowska, U. M., Ćwikła, J., Walecka, I., & Walecki, J. (2013). Psoriatic
arthritis. Polish Journal of Radiology, 78(1), 7-17. doi:10.12659/PJR.883763
Sheehan, M. T. (2016). Biochemical testing of the thyroid: TSH is the best and, oftentimes, only
test needed – A review for primary care. Clinical medicine and research, 14(2), 83-92.
doi:10.3121/cmr.2016.1309
Solmaz, D., Bakirci , S., Kimyon, G., Kasapoglu, G. E., Dogru, A., Bayindir, O., . . . Aydin , S.
Z. (2019). The impact of having family history of psoriasis or psoriatic arthritis on
psoriatic disease. Arthritis Care and Research. doi:10.1002/acr.23836
Soran, H., Adam, S., Mohammad, J. B., Ho, J. H., Schofield, J. D., Kwok, S., . . . Durrington, P.
N. (2018). Hypercholesterolaemia – practical information for non-specialists. Archives of
Medical Science, 14(1), 1-21. doi:10.5114/aoms.2018.72238
Talamonti, M., Galluzzo , M., Bernardini , N., Caldarola , G., Persechino , S., Cantoresi , F., . . .
Bianchi, L. (2018). Psoriasis Area and Severity Index response in moderate-severe
psoriatic patients switched to adalimumab: Results from the OPPSA study. Journal of the
European Academy of Dermatology and Venerology, 32(10), 1737-1744.
doi:10.1111/jdv.15077
Thomsen, S. F. (2014). Atopic dermatitis: Natural history, diagnosis, and treatment. ISRN
Allergy, 1-7. doi:10.1155/2014/354250
Tobias, D. K., Chen, M., Manson, J. E., Ludwig, D. S., Willett, W., & Hu, F. B. (2015). Effect of
low-fat vs. other diet interventions on long-term weight change in adults: A systematic
Master of Nursing: Patient Assessment 15
16 | P a g e
review and meta-analysis. The Lancet Diabetes & Endocrinology, 3(12), 968–979.
doi:10.1016/S2213-8587(15)00367-8
Vaidya, T., Zulfiqar, H., & Badri, T. (2019). Mycosis Fungoides. In StatPearls. Treasure Island
(Florida): StatPearls Publishing. Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK519572/
Vaillant, A. A., McClellan, N., & Varacallo, M. (2019). Lupus erythematosus. In StatPearls.
Treasure Island (Florida): StatPearls Publishing. Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK535405/
Zil, J. M., Dirmaier, J., Augustin, M., Dwinger, S., Christalle, E., Härter, M., & Mrowietz, U.
(2018). Psychosocial distress of patients with psoriasis: Protocol for an assessment of care
needs and the development of a supportive intervention. JMIR Research Protocols, 1-16.
doi:10.2196/resprot.8490
Master of Nursing: Patient Assessment 16
review and meta-analysis. The Lancet Diabetes & Endocrinology, 3(12), 968–979.
doi:10.1016/S2213-8587(15)00367-8
Vaidya, T., Zulfiqar, H., & Badri, T. (2019). Mycosis Fungoides. In StatPearls. Treasure Island
(Florida): StatPearls Publishing. Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK519572/
Vaillant, A. A., McClellan, N., & Varacallo, M. (2019). Lupus erythematosus. In StatPearls.
Treasure Island (Florida): StatPearls Publishing. Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK535405/
Zil, J. M., Dirmaier, J., Augustin, M., Dwinger, S., Christalle, E., Härter, M., & Mrowietz, U.
(2018). Psychosocial distress of patients with psoriasis: Protocol for an assessment of care
needs and the development of a supportive intervention. JMIR Research Protocols, 1-16.
doi:10.2196/resprot.8490
Master of Nursing: Patient Assessment 16
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
17 | P a g e
Appendix
Laboratory Findings
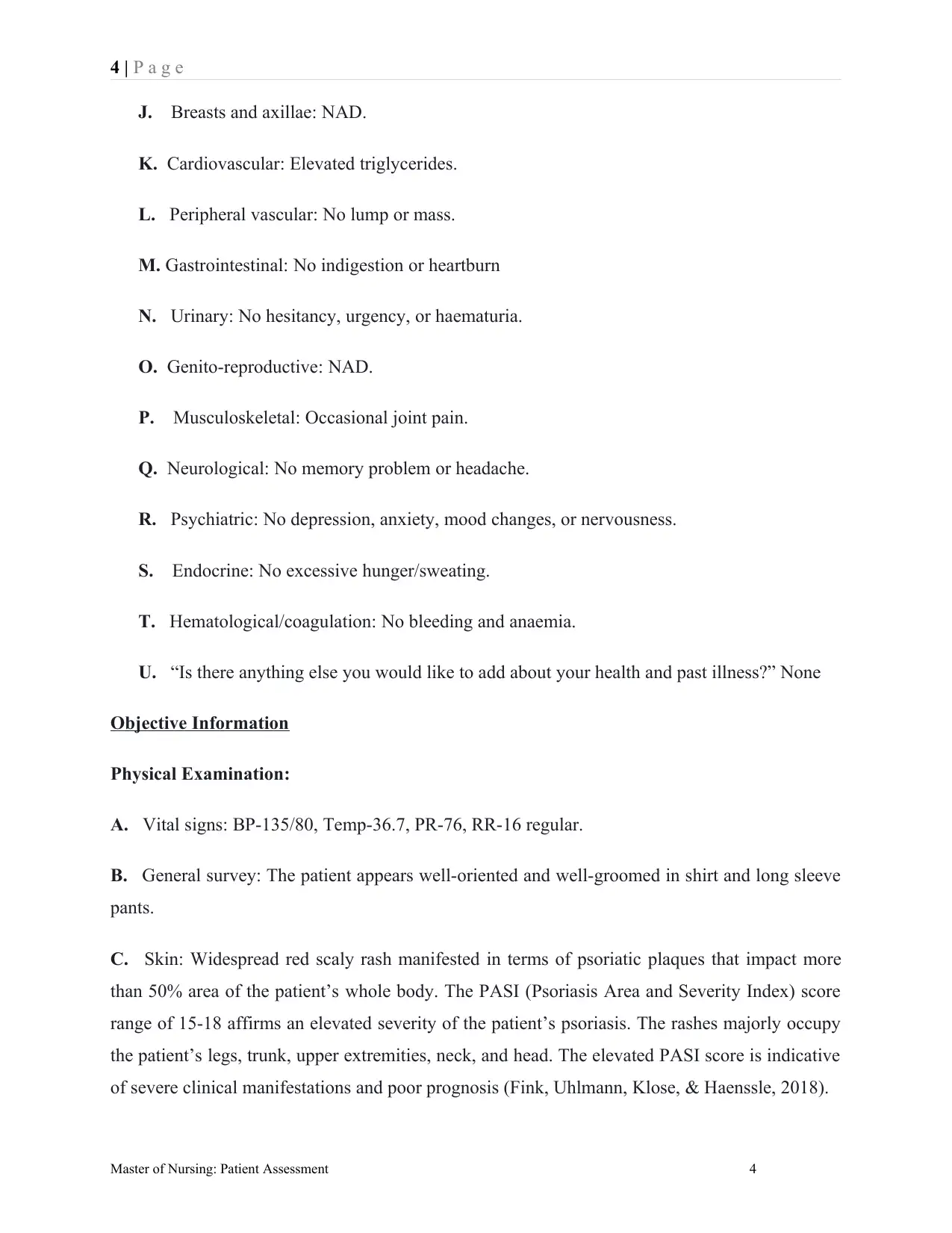
Lab Test Outcome Normal Range Inference
Serum triglycerides 3.3 0.6-2.0 Elevated
ALT 70 5-40 Elevated
FBC NAD
LFT NAD
HDL cholesterol 3.9-5.5 NAD
MSU (midstream
specimen of urine)
NAD
Master of Nursing: Patient Assessment 17
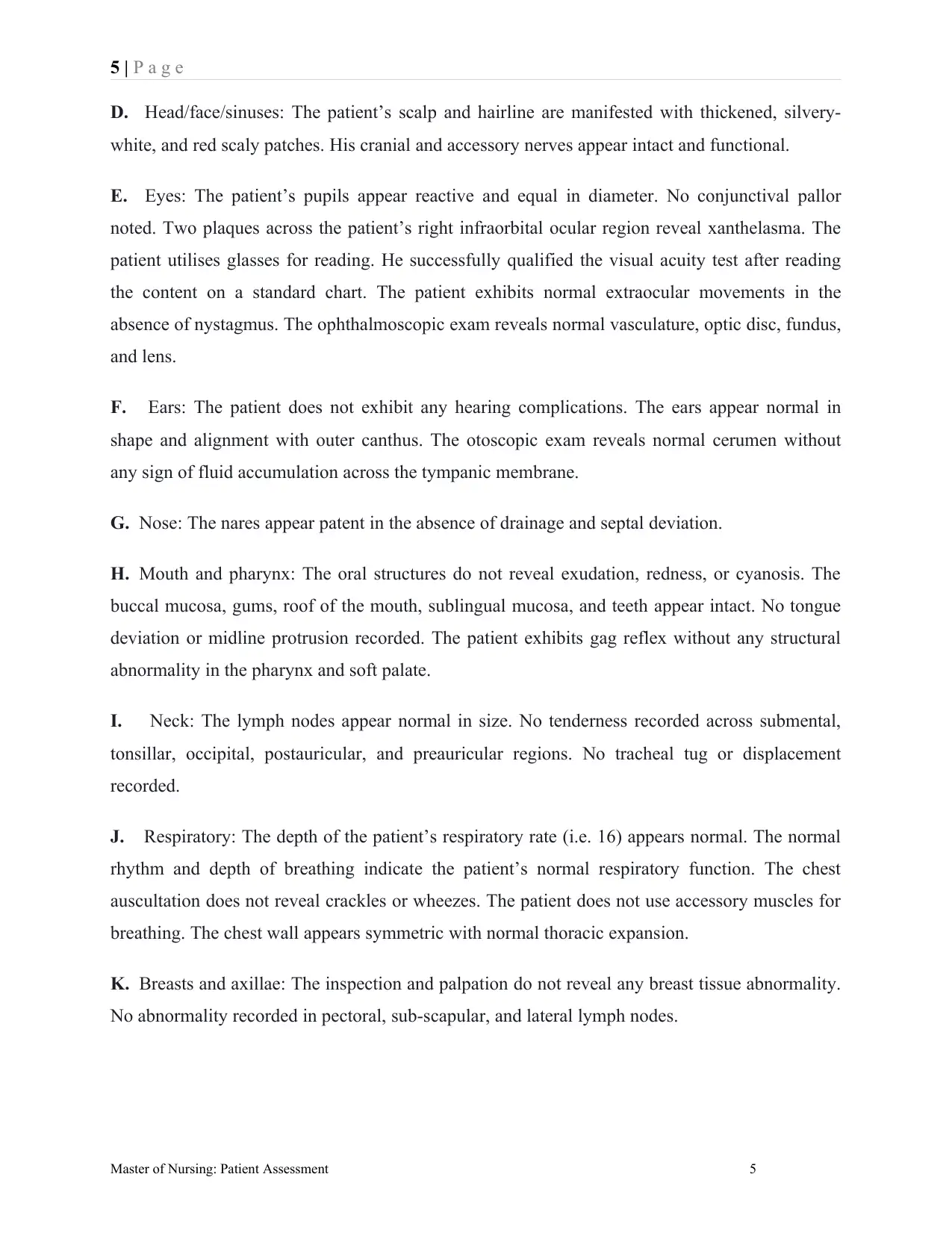
Appendix
Laboratory Findings
Lab Test Outcome Normal Range Inference
Serum triglycerides 3.3 0.6-2.0 Elevated
ALT 70 5-40 Elevated
FBC NAD
LFT NAD
HDL cholesterol 3.9-5.5 NAD
MSU (midstream
specimen of urine)
NAD
Master of Nursing: Patient Assessment 17
18 | P a g e
Referral Letter
Referral Subject: Robert’s Follow-up dermatologic assessment requirement
Dear Physician,
The 47 years old male patient ‘Robert’ is under my active treatment and experiencing chronic
plaque psoriasis from the age of 5 years until date. His signs/symptoms are based on the
appearance of dry, scaly, and well-demarcated erythematous psoriasis plaques/patches
surrounded with a silvery scale. The waxing and waning of skin flares continue in a variable
pattern. The patient is undertaking biologic therapy based on 4-12 weekly administration of
Ustekinumab – Stelara (45mg, subcutaneous). The patient also exhibits a strong family history of
psoriasis. He possesses a highly photosensitive skin. His plaques could not heal through any
pharmacological intervention. Robert requires a 6-monthly skin assessment before each follow-
up session. Accordingly, I request you to consider his case for dermatological assessment and
share your findings to support the recommended follow-up interventions.
Thanks, and Sincere Regards,
Dr. ______________________
Dated: ____/_____/_________
Master of Nursing: Patient Assessment 18
Referral Letter
Referral Subject: Robert’s Follow-up dermatologic assessment requirement
Dear Physician,
The 47 years old male patient ‘Robert’ is under my active treatment and experiencing chronic
plaque psoriasis from the age of 5 years until date. His signs/symptoms are based on the
appearance of dry, scaly, and well-demarcated erythematous psoriasis plaques/patches
surrounded with a silvery scale. The waxing and waning of skin flares continue in a variable
pattern. The patient is undertaking biologic therapy based on 4-12 weekly administration of
Ustekinumab – Stelara (45mg, subcutaneous). The patient also exhibits a strong family history of
psoriasis. He possesses a highly photosensitive skin. His plaques could not heal through any
pharmacological intervention. Robert requires a 6-monthly skin assessment before each follow-
up session. Accordingly, I request you to consider his case for dermatological assessment and
share your findings to support the recommended follow-up interventions.
Thanks, and Sincere Regards,
Dr. ______________________
Dated: ____/_____/_________
Master of Nursing: Patient Assessment 18
1 out of 18
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.