Establishing a Therapeutic Alliance in Substance Abuse Treatment and Intake Assessment Tool
VerifiedAdded on 2022/10/04
|37
|7990
|71
AI Summary
This document discusses the importance of establishing a therapeutic alliance in substance abuse treatment and the intake assessment process. It also provides a list of questions to ask during the intake assessment. COUADD803A
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

1
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Student Name –
Course title - COUADD803A
Assessment 1,2,3 & 4
Date -
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Student Name –
Course title - COUADD803A
Assessment 1,2,3 & 4
Date -
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
2
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Assessment task 1
Part A- Assessment
1. The choice to seek treatment for substance abuse is no easy one, and the development
of conviction and trust between the patient and the counsellors. Therefore, it is
imperative for the counsellors to make efforts for the growth of a strong bond with
the patients, also known as a therapeutic alliance. Resilient alliances like this
guarantee that the patient interprets the counsellors as dependable and recognises that
their best interests and wellbeing are on the front. This permits the patient and the
counsellors to work under situations that even encompass tribulation. While such
trust takes time to grow, patients ultimately feel contented speaking spontaneously
during sessions, and demonstrate an inclination of not withholding any information
(Pihkala, Dimova-Bränström & Sandlund, 2017). In order to establish such openness
and honesty, counsellors should ensure that the patient knows that there is an interest
in looking after their mental health and wellbeing. In addition, demonstration of
attentiveness at the time of the counselling sessions, and asking open-ended questions
also helps the patient to present his opinions and motivations behind the behaviour of
substance abuse. Letting the patient know that the counsellor is ready to empathise
with the issues faced by the former is a crucial aspect of the sessions that helps in
communicating clearly about the expectations of the treatment, thereby playing an
important role in recovery from substance abuse (Moyers et al., 2016). The patient
needs to be completely informed about the care process and communication must be
initiated at a time and location that makes them feel comfortable (Green et al., 2018).
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Assessment task 1
Part A- Assessment
1. The choice to seek treatment for substance abuse is no easy one, and the development
of conviction and trust between the patient and the counsellors. Therefore, it is
imperative for the counsellors to make efforts for the growth of a strong bond with
the patients, also known as a therapeutic alliance. Resilient alliances like this
guarantee that the patient interprets the counsellors as dependable and recognises that
their best interests and wellbeing are on the front. This permits the patient and the
counsellors to work under situations that even encompass tribulation. While such
trust takes time to grow, patients ultimately feel contented speaking spontaneously
during sessions, and demonstrate an inclination of not withholding any information
(Pihkala, Dimova-Bränström & Sandlund, 2017). In order to establish such openness
and honesty, counsellors should ensure that the patient knows that there is an interest
in looking after their mental health and wellbeing. In addition, demonstration of
attentiveness at the time of the counselling sessions, and asking open-ended questions
also helps the patient to present his opinions and motivations behind the behaviour of
substance abuse. Letting the patient know that the counsellor is ready to empathise
with the issues faced by the former is a crucial aspect of the sessions that helps in
communicating clearly about the expectations of the treatment, thereby playing an
important role in recovery from substance abuse (Moyers et al., 2016). The patient
needs to be completely informed about the care process and communication must be
initiated at a time and location that makes them feel comfortable (Green et al., 2018).
3
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
2. In substance abuse treatment, the motivation of the patient to change has frequently
been a foundation of frustration, ever since counsellors have slight regulation over a
patient’s aspiration to change. The underlying reasons behind substance abuse
are mostly environmental and genetic. The genetic makeup of an individual increases
his likelihood of adopting sensation-seeking behaviour (Hines et al., 2015).
Furthermore, several life events such as, stress, trauma, and early exposure to
addictive substances also increase the vulnerability of the person. Generation of a
therapeutic alliance is largely dependent on the reliance that the patient feels with the
counsellors, thus permitting them to feel susceptible while arranging out their
difficulties and working together efficiently. Besides genetic predisposition, familial
risk factors like childhood maltreatment (abuse and neglect), marital status of
parents, parental education, parental or familial substance abuse, familial
socioeconomic status, parent-child relationships, and child perception that parents
approve of their substance use must be considered (Soron et al., 2017). Furthermore,
being a victim of sexual or physical assault increases risk of substance abuse
(Mokma et al., 2016). Efforts must also be taken to determine the influence of peers
and parental involvement on substance use. Research has highlighted that adorning
the character of the bully has been linked with increased alcohol consumption (Jones
et al., 2019). Furthermore, it must also be checked if the patient suffers from
depression since comorbidity of depression that encompasses feelings of pain, gloom,
sadness and anger have been related with substance abuse that creates an impact on
daily lives.
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
2. In substance abuse treatment, the motivation of the patient to change has frequently
been a foundation of frustration, ever since counsellors have slight regulation over a
patient’s aspiration to change. The underlying reasons behind substance abuse
are mostly environmental and genetic. The genetic makeup of an individual increases
his likelihood of adopting sensation-seeking behaviour (Hines et al., 2015).
Furthermore, several life events such as, stress, trauma, and early exposure to
addictive substances also increase the vulnerability of the person. Generation of a
therapeutic alliance is largely dependent on the reliance that the patient feels with the
counsellors, thus permitting them to feel susceptible while arranging out their
difficulties and working together efficiently. Besides genetic predisposition, familial
risk factors like childhood maltreatment (abuse and neglect), marital status of
parents, parental education, parental or familial substance abuse, familial
socioeconomic status, parent-child relationships, and child perception that parents
approve of their substance use must be considered (Soron et al., 2017). Furthermore,
being a victim of sexual or physical assault increases risk of substance abuse
(Mokma et al., 2016). Efforts must also be taken to determine the influence of peers
and parental involvement on substance use. Research has highlighted that adorning
the character of the bully has been linked with increased alcohol consumption (Jones
et al., 2019). Furthermore, it must also be checked if the patient suffers from
depression since comorbidity of depression that encompasses feelings of pain, gloom,
sadness and anger have been related with substance abuse that creates an impact on
daily lives.
4
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Part B- Intake tool for assessment
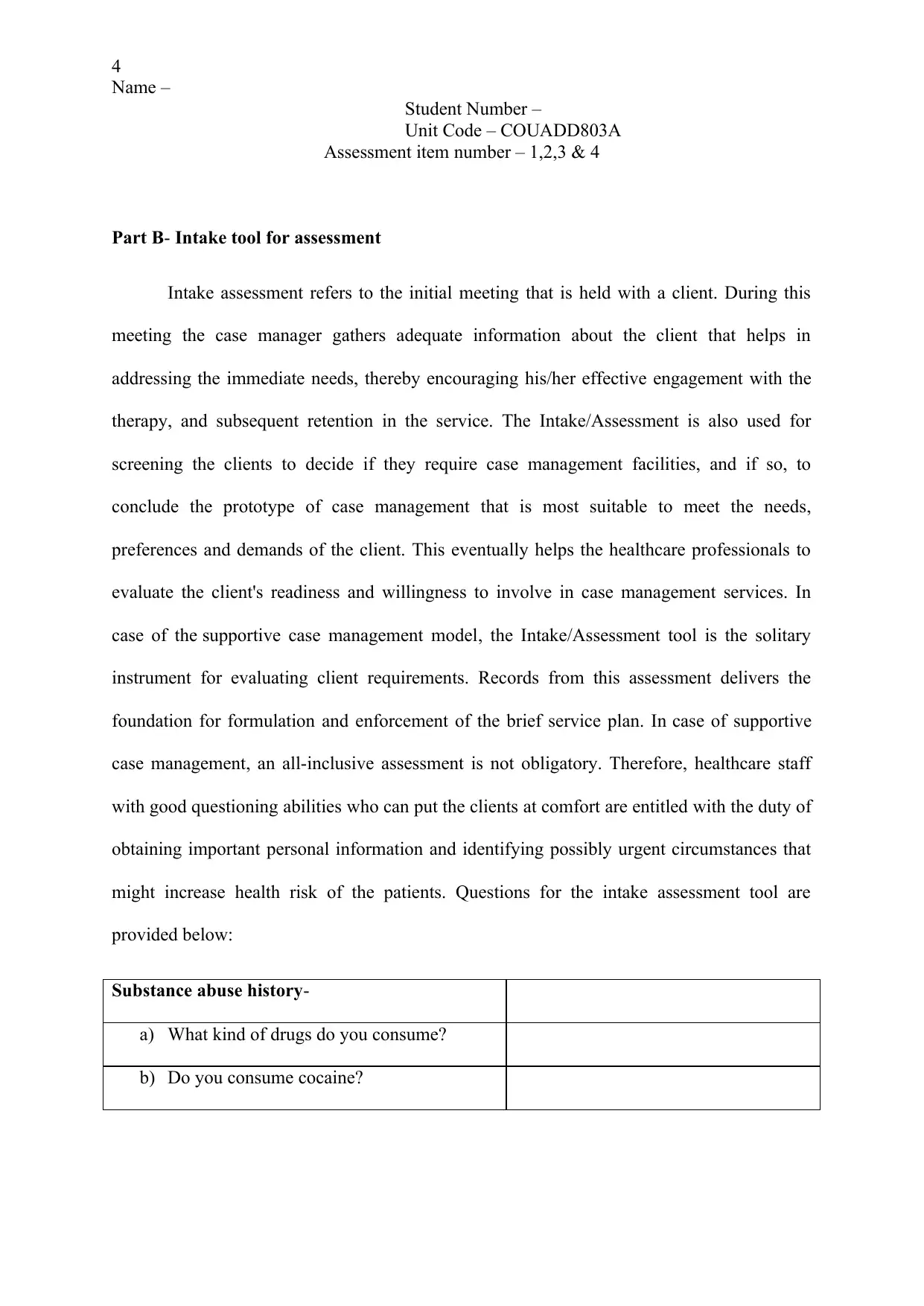
Intake assessment refers to the initial meeting that is held with a client. During this
meeting the case manager gathers adequate information about the client that helps in
addressing the immediate needs, thereby encouraging his/her effective engagement with the
therapy, and subsequent retention in the service. The Intake/Assessment is also used for
screening the clients to decide if they require case management facilities, and if so, to
conclude the prototype of case management that is most suitable to meet the needs,
preferences and demands of the client. This eventually helps the healthcare professionals to
evaluate the client's readiness and willingness to involve in case management services. In
case of the supportive case management model, the Intake/Assessment tool is the solitary
instrument for evaluating client requirements. Records from this assessment delivers the
foundation for formulation and enforcement of the brief service plan. In case of supportive
case management, an all-inclusive assessment is not obligatory. Therefore, healthcare staff
with good questioning abilities who can put the clients at comfort are entitled with the duty of
obtaining important personal information and identifying possibly urgent circumstances that
might increase health risk of the patients. Questions for the intake assessment tool are
provided below:
Substance abuse history-
a) What kind of drugs do you consume?
b) Do you consume cocaine?
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Part B- Intake tool for assessment
Intake assessment refers to the initial meeting that is held with a client. During this
meeting the case manager gathers adequate information about the client that helps in
addressing the immediate needs, thereby encouraging his/her effective engagement with the
therapy, and subsequent retention in the service. The Intake/Assessment is also used for
screening the clients to decide if they require case management facilities, and if so, to
conclude the prototype of case management that is most suitable to meet the needs,
preferences and demands of the client. This eventually helps the healthcare professionals to
evaluate the client's readiness and willingness to involve in case management services. In
case of the supportive case management model, the Intake/Assessment tool is the solitary
instrument for evaluating client requirements. Records from this assessment delivers the
foundation for formulation and enforcement of the brief service plan. In case of supportive
case management, an all-inclusive assessment is not obligatory. Therefore, healthcare staff
with good questioning abilities who can put the clients at comfort are entitled with the duty of
obtaining important personal information and identifying possibly urgent circumstances that
might increase health risk of the patients. Questions for the intake assessment tool are
provided below:
Substance abuse history-
a) What kind of drugs do you consume?
b) Do you consume cocaine?
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
5
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
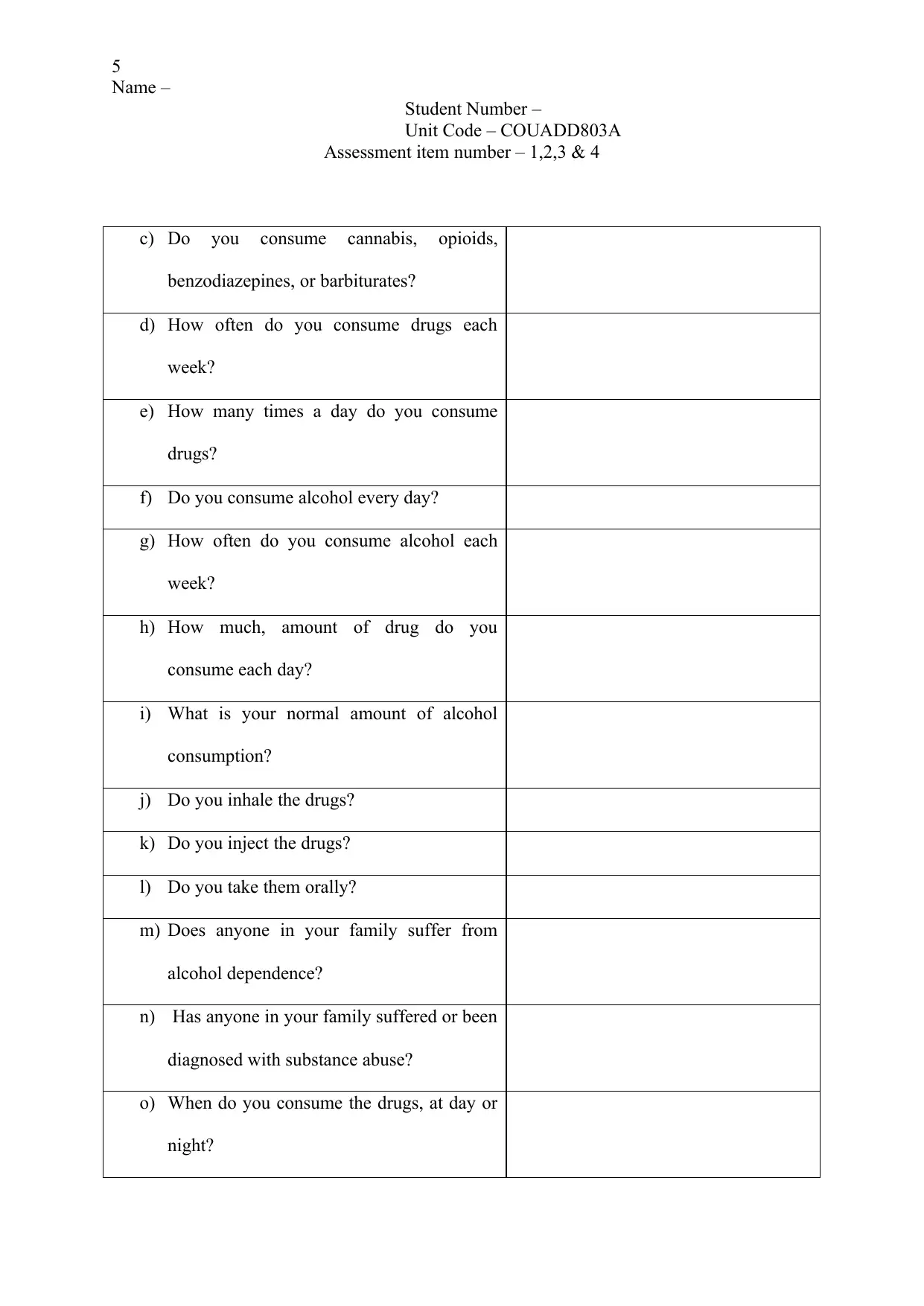
c) Do you consume cannabis, opioids,
benzodiazepines, or barbiturates?
d) How often do you consume drugs each
week?
e) How many times a day do you consume
drugs?
f) Do you consume alcohol every day?
g) How often do you consume alcohol each
week?
h) How much, amount of drug do you
consume each day?
i) What is your normal amount of alcohol
consumption?
j) Do you inhale the drugs?
k) Do you inject the drugs?
l) Do you take them orally?
m) Does anyone in your family suffer from
alcohol dependence?
n) Has anyone in your family suffered or been
diagnosed with substance abuse?
o) When do you consume the drugs, at day or
night?
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
c) Do you consume cannabis, opioids,
benzodiazepines, or barbiturates?
d) How often do you consume drugs each
week?
e) How many times a day do you consume
drugs?
f) Do you consume alcohol every day?
g) How often do you consume alcohol each
week?
h) How much, amount of drug do you
consume each day?
i) What is your normal amount of alcohol
consumption?
j) Do you inhale the drugs?
k) Do you inject the drugs?
l) Do you take them orally?
m) Does anyone in your family suffer from
alcohol dependence?
n) Has anyone in your family suffered or been
diagnosed with substance abuse?
o) When do you consume the drugs, at day or
night?
6
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
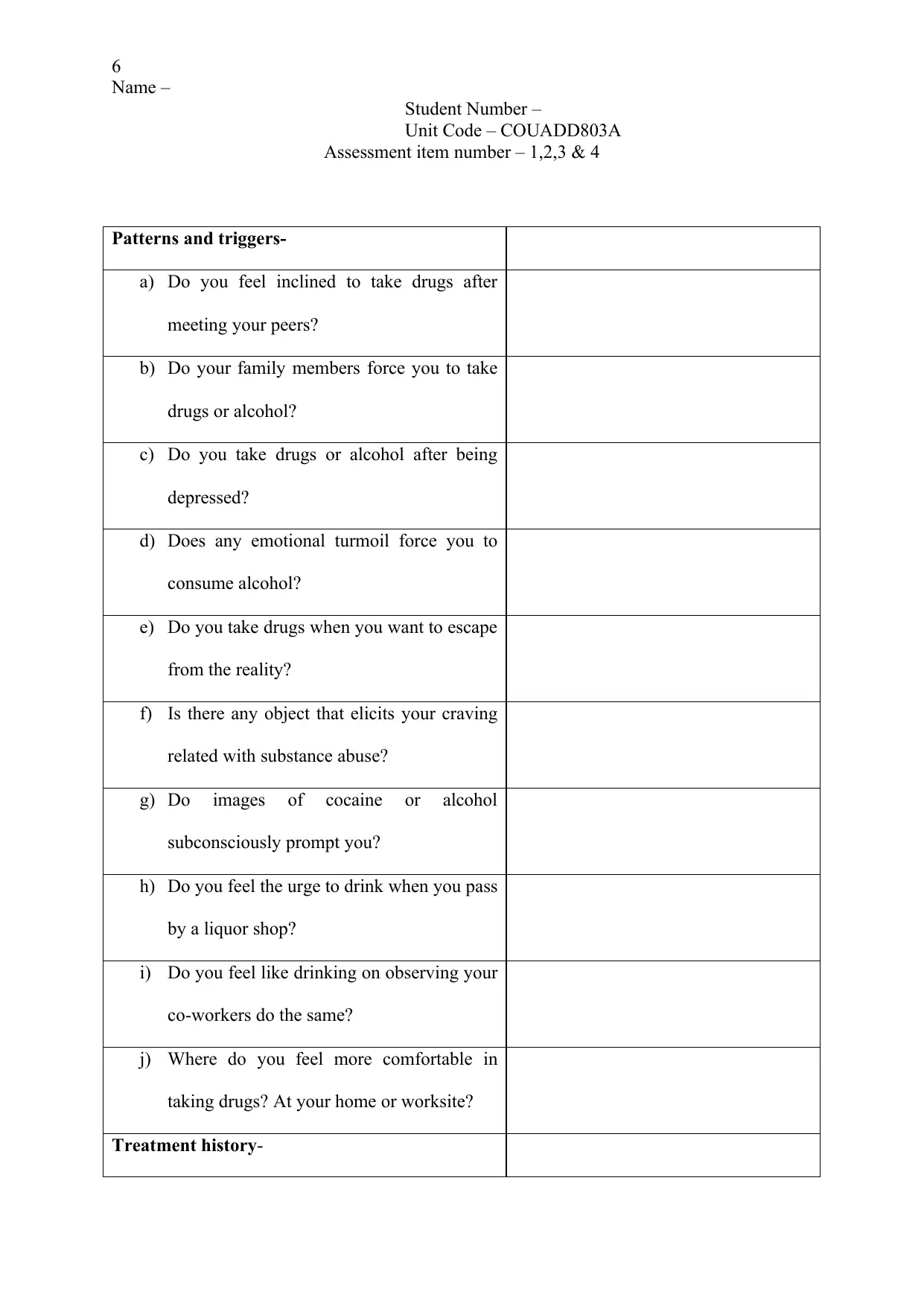
Patterns and triggers-
a) Do you feel inclined to take drugs after
meeting your peers?
b) Do your family members force you to take
drugs or alcohol?
c) Do you take drugs or alcohol after being
depressed?
d) Does any emotional turmoil force you to
consume alcohol?
e) Do you take drugs when you want to escape
from the reality?
f) Is there any object that elicits your craving
related with substance abuse?
g) Do images of cocaine or alcohol
subconsciously prompt you?
h) Do you feel the urge to drink when you pass
by a liquor shop?
i) Do you feel like drinking on observing your
co-workers do the same?
j) Where do you feel more comfortable in
taking drugs? At your home or worksite?
Treatment history-
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Patterns and triggers-
a) Do you feel inclined to take drugs after
meeting your peers?
b) Do your family members force you to take
drugs or alcohol?
c) Do you take drugs or alcohol after being
depressed?
d) Does any emotional turmoil force you to
consume alcohol?
e) Do you take drugs when you want to escape
from the reality?
f) Is there any object that elicits your craving
related with substance abuse?
g) Do images of cocaine or alcohol
subconsciously prompt you?
h) Do you feel the urge to drink when you pass
by a liquor shop?
i) Do you feel like drinking on observing your
co-workers do the same?
j) Where do you feel more comfortable in
taking drugs? At your home or worksite?
Treatment history-
7
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
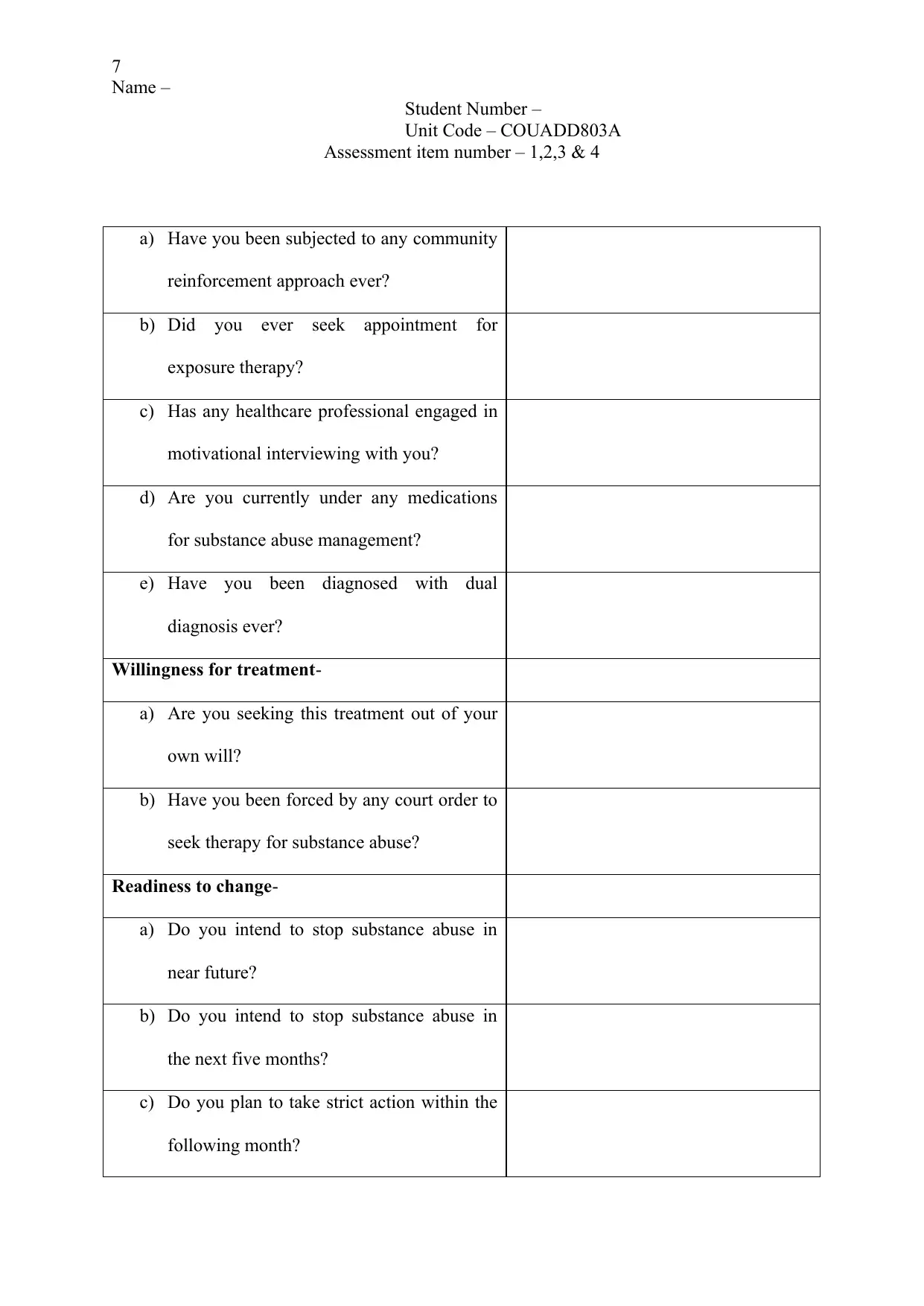
a) Have you been subjected to any community
reinforcement approach ever?
b) Did you ever seek appointment for
exposure therapy?
c) Has any healthcare professional engaged in
motivational interviewing with you?
d) Are you currently under any medications
for substance abuse management?
e) Have you been diagnosed with dual
diagnosis ever?
Willingness for treatment-
a) Are you seeking this treatment out of your
own will?
b) Have you been forced by any court order to
seek therapy for substance abuse?
Readiness to change-
a) Do you intend to stop substance abuse in
near future?
b) Do you intend to stop substance abuse in
the next five months?
c) Do you plan to take strict action within the
following month?
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
a) Have you been subjected to any community
reinforcement approach ever?
b) Did you ever seek appointment for
exposure therapy?
c) Has any healthcare professional engaged in
motivational interviewing with you?
d) Are you currently under any medications
for substance abuse management?
e) Have you been diagnosed with dual
diagnosis ever?
Willingness for treatment-
a) Are you seeking this treatment out of your
own will?
b) Have you been forced by any court order to
seek therapy for substance abuse?
Readiness to change-
a) Do you intend to stop substance abuse in
near future?
b) Do you intend to stop substance abuse in
the next five months?
c) Do you plan to take strict action within the
following month?
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
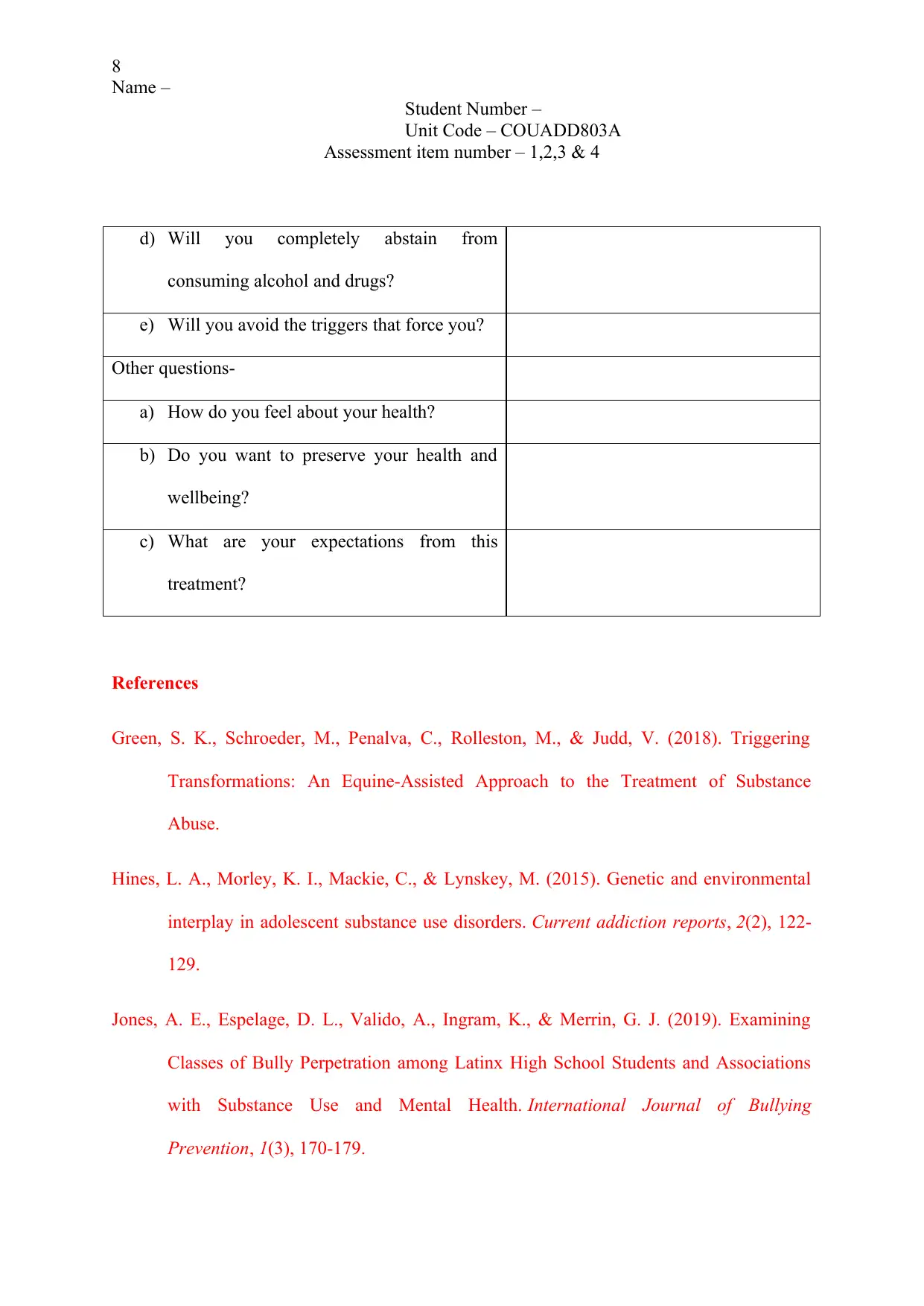
d) Will you completely abstain from
consuming alcohol and drugs?
e) Will you avoid the triggers that force you?
Other questions-
a) How do you feel about your health?
b) Do you want to preserve your health and
wellbeing?
c) What are your expectations from this
treatment?
References
Green, S. K., Schroeder, M., Penalva, C., Rolleston, M., & Judd, V. (2018). Triggering
Transformations: An Equine-Assisted Approach to the Treatment of Substance
Abuse.
Hines, L. A., Morley, K. I., Mackie, C., & Lynskey, M. (2015). Genetic and environmental
interplay in adolescent substance use disorders. Current addiction reports, 2(2), 122-
129.
Jones, A. E., Espelage, D. L., Valido, A., Ingram, K., & Merrin, G. J. (2019). Examining
Classes of Bully Perpetration among Latinx High School Students and Associations
with Substance Use and Mental Health. International Journal of Bullying
Prevention, 1(3), 170-179.
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
d) Will you completely abstain from
consuming alcohol and drugs?
e) Will you avoid the triggers that force you?
Other questions-
a) How do you feel about your health?
b) Do you want to preserve your health and
wellbeing?
c) What are your expectations from this
treatment?
References
Green, S. K., Schroeder, M., Penalva, C., Rolleston, M., & Judd, V. (2018). Triggering
Transformations: An Equine-Assisted Approach to the Treatment of Substance
Abuse.
Hines, L. A., Morley, K. I., Mackie, C., & Lynskey, M. (2015). Genetic and environmental
interplay in adolescent substance use disorders. Current addiction reports, 2(2), 122-
129.
Jones, A. E., Espelage, D. L., Valido, A., Ingram, K., & Merrin, G. J. (2019). Examining
Classes of Bully Perpetration among Latinx High School Students and Associations
with Substance Use and Mental Health. International Journal of Bullying
Prevention, 1(3), 170-179.
9
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Mokma, T. R., Eshelman, L. R., & Messman-Moore, T. L. (2016). Contributions of child
sexual abuse, self-blame, posttraumatic stress symptoms, and alcohol use to women’s
risk for forcible and substance-facilitated sexual assault. Journal of child sexual
abuse, 25(4), 428-448.
Moyers, T. B., Houck, J., Rice, S. L., Longabaugh, R., & Miller, W. R. (2016). Therapist
empathy, combined behavioural intervention, and alcohol outcomes in the COMBINE
research project. Journal of consulting and clinical psychology, 84(3), 221.
Pihkala, H., Dimova-Bränström, N., & Sandlund, M. (2017). Talking about parental
substance abuse with children: eight families’ experiences of Beardslee’s family
intervention. Nordic journal of psychiatry, 71(5), 395-401.
Soron, T. R., Siddike, P. M. A., Ahmed, H. U., & Chowdhury, C. A. (2017). Social and
Family Determinants of Substance Abuse among the Patients of Two Hospitals in
Bangladesh. J Addict Res Ther, 8(340), 2.
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Mokma, T. R., Eshelman, L. R., & Messman-Moore, T. L. (2016). Contributions of child
sexual abuse, self-blame, posttraumatic stress symptoms, and alcohol use to women’s
risk for forcible and substance-facilitated sexual assault. Journal of child sexual
abuse, 25(4), 428-448.
Moyers, T. B., Houck, J., Rice, S. L., Longabaugh, R., & Miller, W. R. (2016). Therapist
empathy, combined behavioural intervention, and alcohol outcomes in the COMBINE
research project. Journal of consulting and clinical psychology, 84(3), 221.
Pihkala, H., Dimova-Bränström, N., & Sandlund, M. (2017). Talking about parental
substance abuse with children: eight families’ experiences of Beardslee’s family
intervention. Nordic journal of psychiatry, 71(5), 395-401.
Soron, T. R., Siddike, P. M. A., Ahmed, H. U., & Chowdhury, C. A. (2017). Social and
Family Determinants of Substance Abuse among the Patients of Two Hospitals in
Bangladesh. J Addict Res Ther, 8(340), 2.
10
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Assessment task 2
- Working with a coerced or mandated client
Introduction- Mandated clients refer to those who seek treatment under the
compulsion of a lawful body or force from family members and organizations (Wild et al.,
2016). According to Janssens (2017) court-ordered therapy is destined to be a facilitator for
variation, for a person who often remains involved with the legitimate system. Such patients
are generally ordered by a magistrate or judge to engage in treatment delivered by a mental
health provider. In addition, coerced abstinence refers to a drug rehabilitation policy that uses
everyday monitoring and instantaneous punishment to diminish drug use amid participants.
This policy can affectedly reduce re-offense rates amid chronic drug users, particularly for
people who are under parole or probation. This essay will elaborate on a case study that
involved Max who had been mandated to appear for drug rehabilitation counselling.
Discussion- Under circumstances when mental health disorders underwrite violent or
hazardous behaviour, create an impact on the manner an individual treat their families, or
increases the peril of recidivism, treatment might be ordered by a court. A court often
compels treatment if an individual is considered a danger to themselves or others (Bouchard,
Brulin-Solignac& Lodetti, 2017). Furthermore, laws of the state that govern the court-
mandated treatment generally differ, as do the agendas and errands that a person needs to
complete as measure of court-ordered treatment.
a)In other words, mandated treatment permits judicial systems, clinicians, and
treatment facilities gain a substantial control over the life of a client. Factually, mandated
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Assessment task 2
- Working with a coerced or mandated client
Introduction- Mandated clients refer to those who seek treatment under the
compulsion of a lawful body or force from family members and organizations (Wild et al.,
2016). According to Janssens (2017) court-ordered therapy is destined to be a facilitator for
variation, for a person who often remains involved with the legitimate system. Such patients
are generally ordered by a magistrate or judge to engage in treatment delivered by a mental
health provider. In addition, coerced abstinence refers to a drug rehabilitation policy that uses
everyday monitoring and instantaneous punishment to diminish drug use amid participants.
This policy can affectedly reduce re-offense rates amid chronic drug users, particularly for
people who are under parole or probation. This essay will elaborate on a case study that
involved Max who had been mandated to appear for drug rehabilitation counselling.
Discussion- Under circumstances when mental health disorders underwrite violent or
hazardous behaviour, create an impact on the manner an individual treat their families, or
increases the peril of recidivism, treatment might be ordered by a court. A court often
compels treatment if an individual is considered a danger to themselves or others (Bouchard,
Brulin-Solignac& Lodetti, 2017). Furthermore, laws of the state that govern the court-
mandated treatment generally differ, as do the agendas and errands that a person needs to
complete as measure of court-ordered treatment.
a)In other words, mandated treatment permits judicial systems, clinicians, and
treatment facilities gain a substantial control over the life of a client. Factually, mandated
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
11
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
treatment was widespread with abuse. Individuals sent to mental health amenities might
spend ages in those services, getting a wide variety of uncorroborated and
possibly traumatic therapies. Patients might be required to experience electroconvulsive
therapy, be controlled for days, or exposed to violent abuse. Thus, while offering mandated
treatment, it is imperative for the person to review all options, particularly if there lies the
provision of selecting among different facilities or therapists. However, the healthcare
professionals have to encounter several challenges while delivering mandated treatment to
the patients. Decreasing client attrition for the duration of the treatment is a major priority for
the providers. Client attributes allied with greater dropout rates are considered “red flags”,
and the challenge of client dropout is related with factors such as, racial minorities,
economically disadvantaged, recent hospitalization, absence of a professional skill, and
family history of abuse (Werb et al., 2016).
Demonstrating awareness about these red flags facilitates the clinicians to intervene
early. Relapse is another challenge that occurs during the initial months of treatment.
Mandated clients residing in the community are subjected to stresses to relapse, frequently
while combating their yearnings and own battle to change. This calls for the need of helping
clients use relapse prevention approaches, upon their exposure to drugs and alcohol.
Furthermore, a client who has been subjected to court-ordered therapy might have one or
more kin or family members who are patients of substance abuse (Rosenthal, 2017). In
addition, research evidences have suggested that people who have been diagnosed with
substance abuse demonstrate an increased likelihood of having family histories of drug and
alcohol abuse, in comparison to their healthy counterparts. This eventually acts as a challenge
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
treatment was widespread with abuse. Individuals sent to mental health amenities might
spend ages in those services, getting a wide variety of uncorroborated and
possibly traumatic therapies. Patients might be required to experience electroconvulsive
therapy, be controlled for days, or exposed to violent abuse. Thus, while offering mandated
treatment, it is imperative for the person to review all options, particularly if there lies the
provision of selecting among different facilities or therapists. However, the healthcare
professionals have to encounter several challenges while delivering mandated treatment to
the patients. Decreasing client attrition for the duration of the treatment is a major priority for
the providers. Client attributes allied with greater dropout rates are considered “red flags”,
and the challenge of client dropout is related with factors such as, racial minorities,
economically disadvantaged, recent hospitalization, absence of a professional skill, and
family history of abuse (Werb et al., 2016).
Demonstrating awareness about these red flags facilitates the clinicians to intervene
early. Relapse is another challenge that occurs during the initial months of treatment.
Mandated clients residing in the community are subjected to stresses to relapse, frequently
while combating their yearnings and own battle to change. This calls for the need of helping
clients use relapse prevention approaches, upon their exposure to drugs and alcohol.
Furthermore, a client who has been subjected to court-ordered therapy might have one or
more kin or family members who are patients of substance abuse (Rosenthal, 2017). In
addition, research evidences have suggested that people who have been diagnosed with
substance abuse demonstrate an increased likelihood of having family histories of drug and
alcohol abuse, in comparison to their healthy counterparts. This eventually acts as a challenge
12
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
since the client may be in consistent contact with a close friend, family members, partners, or
spouse who uses substances, thereby gaining access to drugs and/or alcohol. Often, the
clients also demonstrate unwillingness to continue with treatment if they do not feel
supported, accepted, and fail to obtain kindness and compassion from the treatment group
(Wallace, 2019). Several issues can disturb group work and hamper the improvement of
clients, such as the clients might be troublemaking or inhibited, demonstrate poor
comprehension and language skills, and also attend the sessions intermittently.
B) With the aim of fostering an honest, open and cooperative therapeutic alliance with
Max, several strategies need to be adopted. Efforts will be taken to foster an
understanding and respectful relation with Max, which will reduce his resistance and
help him successfully engage while working towards treatment goals that are
mutually defined (Rooney & Mirick, 2018). Help will be offered to him to facilitate
working through ambivalence by encouraging his efforts towards transformation and
facilitating him identify inconsistencies between his goals and principles and
substance use. Clients frequently feel vulnerable or indecisive during the initial few
weeks of therapy. Hence, Max needs to be contacted regularly during this time for
enhancing retention. Hence, contact with Max will be maintained by e-mail,
telephone, or letter. Furthermore, the support of his spouse and family members will
also be used for preventing them from sabotaging the mandated treatment (Lunze et
al., 2016).
C)A functional analysis of substance abuse will be conducted that will not only
facilitate the identification of high risk circumstances but will also permit recognition of the
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
since the client may be in consistent contact with a close friend, family members, partners, or
spouse who uses substances, thereby gaining access to drugs and/or alcohol. Often, the
clients also demonstrate unwillingness to continue with treatment if they do not feel
supported, accepted, and fail to obtain kindness and compassion from the treatment group
(Wallace, 2019). Several issues can disturb group work and hamper the improvement of
clients, such as the clients might be troublemaking or inhibited, demonstrate poor
comprehension and language skills, and also attend the sessions intermittently.
B) With the aim of fostering an honest, open and cooperative therapeutic alliance with
Max, several strategies need to be adopted. Efforts will be taken to foster an
understanding and respectful relation with Max, which will reduce his resistance and
help him successfully engage while working towards treatment goals that are
mutually defined (Rooney & Mirick, 2018). Help will be offered to him to facilitate
working through ambivalence by encouraging his efforts towards transformation and
facilitating him identify inconsistencies between his goals and principles and
substance use. Clients frequently feel vulnerable or indecisive during the initial few
weeks of therapy. Hence, Max needs to be contacted regularly during this time for
enhancing retention. Hence, contact with Max will be maintained by e-mail,
telephone, or letter. Furthermore, the support of his spouse and family members will
also be used for preventing them from sabotaging the mandated treatment (Lunze et
al., 2016).
C)A functional analysis of substance abuse will be conducted that will not only
facilitate the identification of high risk circumstances but will also permit recognition of the
13
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
strategies by which triggers are associated to the signs and symptoms manifested by Max.
Efforts will be taken to formulate a relapse prevention plan that will encompass coping
strategies, avoiding visit to places where Max had used drugs previously, acknowledging
good impacts of a substance-free life, and maintaining regular contact over telephone with the
sponsors (Kleinman, 2017). A sense of belonging and an effective therapeutic relationship
will also be established by assessing his comprehension and language skills, and delivering
tailored mentoring, just to ensure that information related to the mandated treatment is
understood and conveyed (Floris et al., 2017). Adjusting the treatment plan for including the
preferences and demands of the client will also help him understand that the treatment is
being offered in his best interest, and would thereby establish trust, and reduce his resistance.
3)Summary- Therapeutic alliance has been identified imperative in counselling and
encompasses the association between a client and a healthcare professional. An effective
therapeutic alliance will be developed in this case for engaging Max with the mandated
therapy, and ensuring beneficial changes in his psychological outcomes. Hence, Max will be
empowered to have the self-esteem and confidence for free expression of his feelings and
emotions. A bond will be creates such that it permits Max to develop faith on the counsellor.
Though the course of treatment might be challenging, demonstration of empathy and a
willingness to listen will act imperative in enhancing mental health outcomes, by increasing
adherence of the client to the goals and objectives of the therapy. With the aim of developing
therapeutic alliance, it is essential that Max must feel comfortable and relaxed. Hence, it is
necessary for promoting a sense of collaboration to make Max feel that he is being provided
with the much needed support.
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
strategies by which triggers are associated to the signs and symptoms manifested by Max.
Efforts will be taken to formulate a relapse prevention plan that will encompass coping
strategies, avoiding visit to places where Max had used drugs previously, acknowledging
good impacts of a substance-free life, and maintaining regular contact over telephone with the
sponsors (Kleinman, 2017). A sense of belonging and an effective therapeutic relationship
will also be established by assessing his comprehension and language skills, and delivering
tailored mentoring, just to ensure that information related to the mandated treatment is
understood and conveyed (Floris et al., 2017). Adjusting the treatment plan for including the
preferences and demands of the client will also help him understand that the treatment is
being offered in his best interest, and would thereby establish trust, and reduce his resistance.
3)Summary- Therapeutic alliance has been identified imperative in counselling and
encompasses the association between a client and a healthcare professional. An effective
therapeutic alliance will be developed in this case for engaging Max with the mandated
therapy, and ensuring beneficial changes in his psychological outcomes. Hence, Max will be
empowered to have the self-esteem and confidence for free expression of his feelings and
emotions. A bond will be creates such that it permits Max to develop faith on the counsellor.
Though the course of treatment might be challenging, demonstration of empathy and a
willingness to listen will act imperative in enhancing mental health outcomes, by increasing
adherence of the client to the goals and objectives of the therapy. With the aim of developing
therapeutic alliance, it is essential that Max must feel comfortable and relaxed. Hence, it is
necessary for promoting a sense of collaboration to make Max feel that he is being provided
with the much needed support.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
14
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
References
Bouchard, J. P., Brulin-Solignac, D., & Lodetti, C. (2017). Court-ordered therapy, a measure
for preventing reoffending. Soins. Psychiatrie, 38(309), 12-16.
Floris, E., De, A. J., Cano, J. P., Raymondaud, S., Rouveyrol, É., & Bouchard, J. P. (2017).
Therapeutic approaches in court-ordered therapy. Soins. Psychiatrie, 38(309), 25-30.
Janssens, M. (2017). Court-ordered therapy, the case of sex offenders in Belgium. Soins.
Psychiatrie, 38(309), 40-42.
Kleinman, T. (2017). Family court ordered “reunification therapy:” junk science in the guise
of helping parent/child relationships?. Journal of Child Custody, 14(4), 295-300.
Lunze, K., Idrisov, B., Golichenko, M., & Kamarulzaman, A. (2016). Mandatory addiction
treatment for people who use drugs: global health and human rights
analysis. Bmj, 353, i2943.
Rooney, R. H., & Mirick, R. G. (Eds.). (2018). Strategies for work with involuntary clients.
Columbia University Press.
Rosenthal, J. T. A. (2017). Therapeutic jurisprudence and drug treatment courts: Integrating
law and science. In Drug Courts (pp. 145-171). Routledge.
Wallace, B. C. (2019). Making mandated addiction treatment work. Rowman & Littlefield.
Werb, D., Kamarulzaman, A., Meacham, M. C., Rafful, C., Fischer, B., Strathdee, S. A., &
Wood, E. (2016). The effectiveness of compulsory drug treatment: a systematic
review. International Journal of Drug Policy, 28, 1-9.
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
References
Bouchard, J. P., Brulin-Solignac, D., & Lodetti, C. (2017). Court-ordered therapy, a measure
for preventing reoffending. Soins. Psychiatrie, 38(309), 12-16.
Floris, E., De, A. J., Cano, J. P., Raymondaud, S., Rouveyrol, É., & Bouchard, J. P. (2017).
Therapeutic approaches in court-ordered therapy. Soins. Psychiatrie, 38(309), 25-30.
Janssens, M. (2017). Court-ordered therapy, the case of sex offenders in Belgium. Soins.
Psychiatrie, 38(309), 40-42.
Kleinman, T. (2017). Family court ordered “reunification therapy:” junk science in the guise
of helping parent/child relationships?. Journal of Child Custody, 14(4), 295-300.
Lunze, K., Idrisov, B., Golichenko, M., & Kamarulzaman, A. (2016). Mandatory addiction
treatment for people who use drugs: global health and human rights
analysis. Bmj, 353, i2943.
Rooney, R. H., & Mirick, R. G. (Eds.). (2018). Strategies for work with involuntary clients.
Columbia University Press.
Rosenthal, J. T. A. (2017). Therapeutic jurisprudence and drug treatment courts: Integrating
law and science. In Drug Courts (pp. 145-171). Routledge.
Wallace, B. C. (2019). Making mandated addiction treatment work. Rowman & Littlefield.
Werb, D., Kamarulzaman, A., Meacham, M. C., Rafful, C., Fischer, B., Strathdee, S. A., &
Wood, E. (2016). The effectiveness of compulsory drug treatment: a systematic
review. International Journal of Drug Policy, 28, 1-9.
15
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Wild, T. C., Yuan, Y., Rush, B. R., & Urbanoski, K. A. (2016). Client engagement in legally-
mandated addiction treatment: A prospective study using self-determination
theory. Journal of substance abuse treatment, 69, 35-43.
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Wild, T. C., Yuan, Y., Rush, B. R., & Urbanoski, K. A. (2016). Client engagement in legally-
mandated addiction treatment: A prospective study using self-determination
theory. Journal of substance abuse treatment, 69, 35-43.
16
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Assessment task 3
Part A- Treatment planning
1. Psychiatrists, social workers, mental health counsellors, psychologists, and
behavioural health professionals emphasise on the concept of treatment planning as an
effective tool for the management of patients. The importance of having a
collaborative treatment plan is that it will be tailored to the individual demands of the
patient and will also increase patient engagement in the care process. Such a treatment
planning is needed for Roy, and it will comprise of his personal information,
demographics, and psychological history (DiClemente et al., 2016). Though treatment
in specialty locations is significant for persons with severe dependence, inadequate
availability and dishonour suggest that specialty care only is inadequate to address
treatment requirements. Thus, collaborative care planning will be implemented for
increasing evidence based treatment delivery, which in turn will improve his health
outcomes. The steps that will be followed for this collaborative treatment planning are
as follows:
Engaging with Roy during the discussions
Probing naturally and asking follow-up questions that will make Roy discuss
about his recent past
Validating and complementing client experience
Having a discussion on the life domains that are considered vital
Asking open-ended questions and complimenting willingness to help gain a
sound understanding about his life
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Assessment task 3
Part A- Treatment planning
1. Psychiatrists, social workers, mental health counsellors, psychologists, and
behavioural health professionals emphasise on the concept of treatment planning as an
effective tool for the management of patients. The importance of having a
collaborative treatment plan is that it will be tailored to the individual demands of the
patient and will also increase patient engagement in the care process. Such a treatment
planning is needed for Roy, and it will comprise of his personal information,
demographics, and psychological history (DiClemente et al., 2016). Though treatment
in specialty locations is significant for persons with severe dependence, inadequate
availability and dishonour suggest that specialty care only is inadequate to address
treatment requirements. Thus, collaborative care planning will be implemented for
increasing evidence based treatment delivery, which in turn will improve his health
outcomes. The steps that will be followed for this collaborative treatment planning are
as follows:
Engaging with Roy during the discussions
Probing naturally and asking follow-up questions that will make Roy discuss
about his recent past
Validating and complementing client experience
Having a discussion on the life domains that are considered vital
Asking open-ended questions and complimenting willingness to help gain a
sound understanding about his life
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
17
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Inviting Roy to suggest how he might want his life to be diverse or better after
the formal treatment
Asking empathetic questions for uncovering information about coping skills
Thanking Roy for his contribution and thoughtful comments.
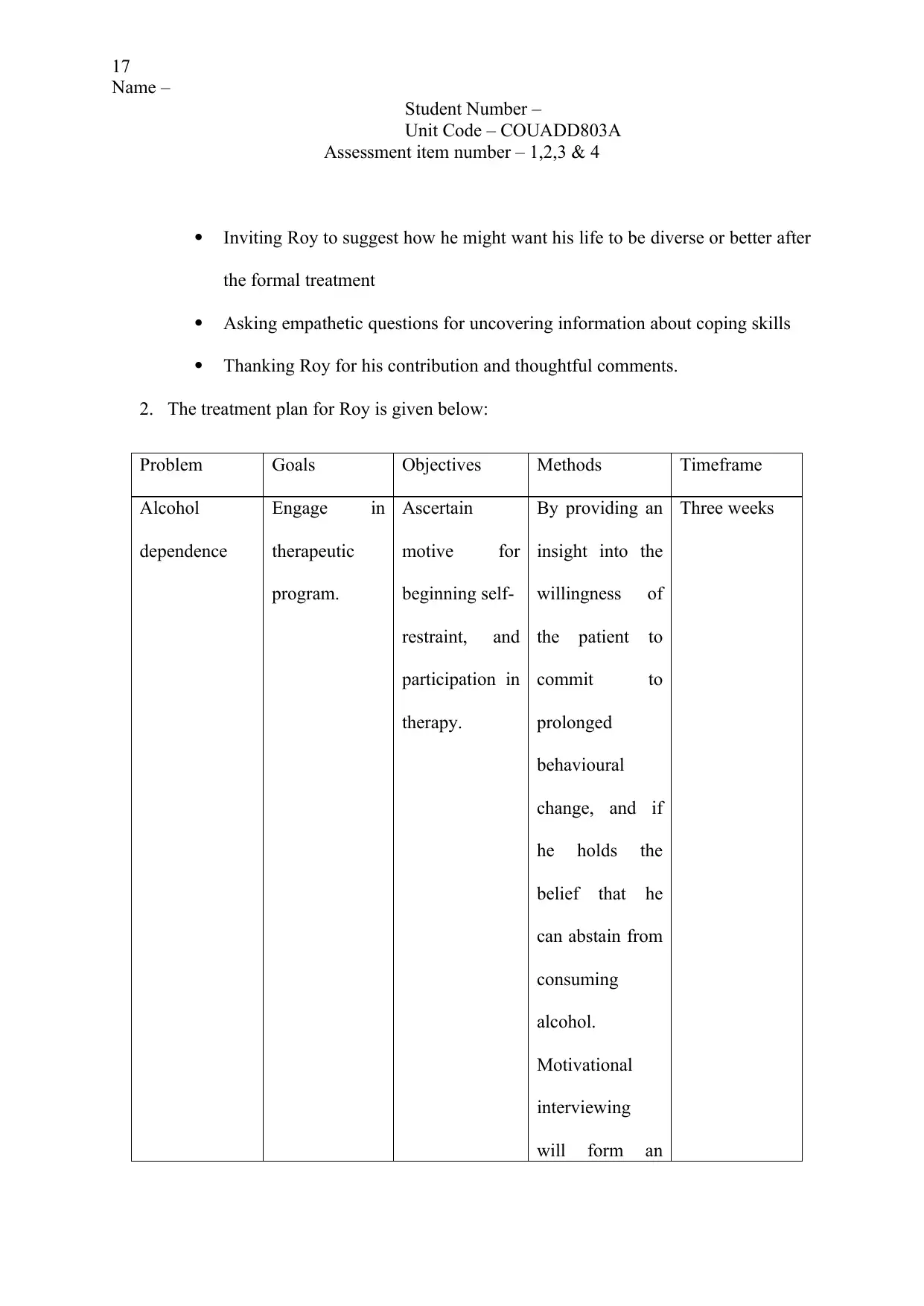
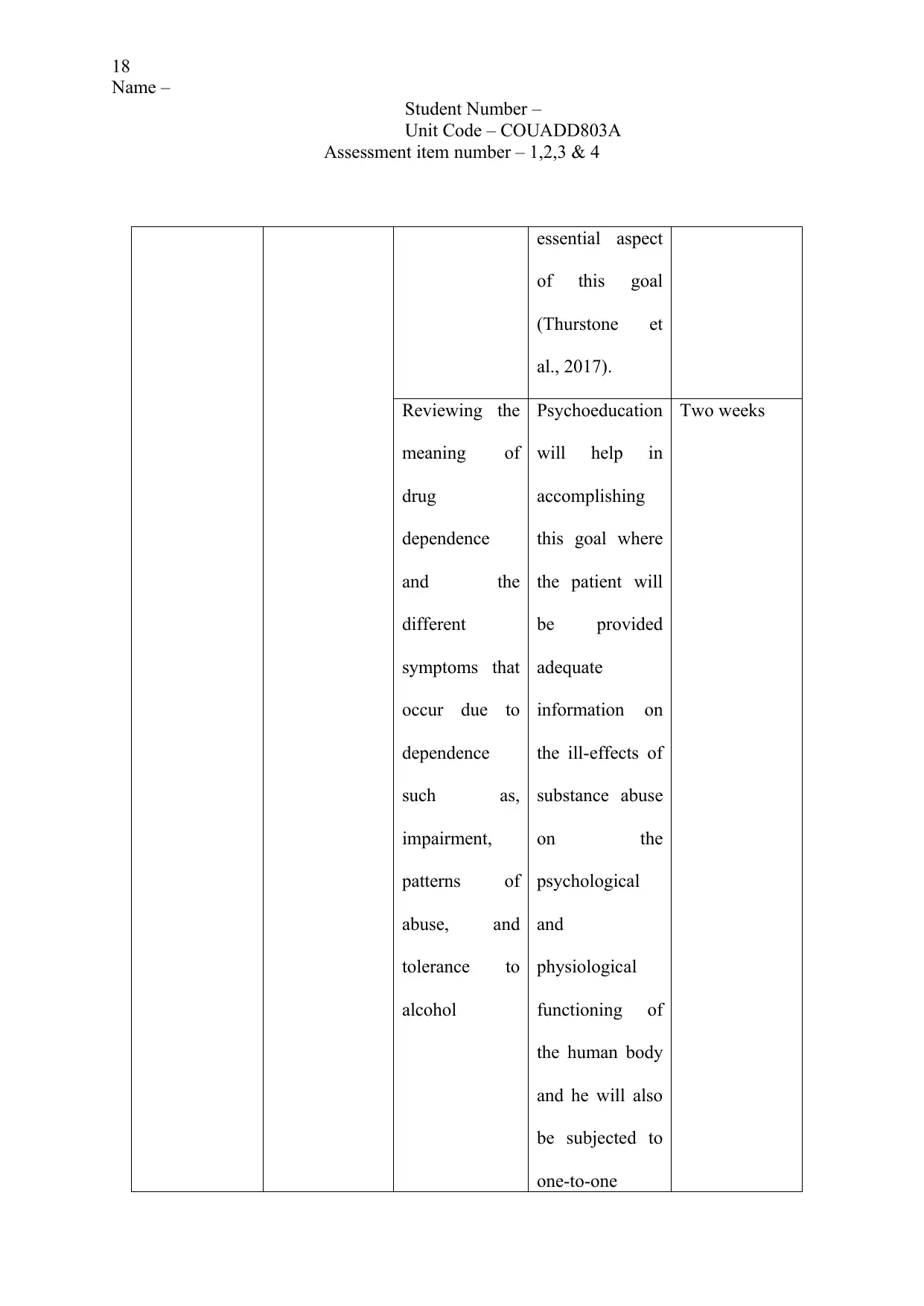
2. The treatment plan for Roy is given below:
Problem Goals Objectives Methods Timeframe
Alcohol
dependence
Engage in
therapeutic
program.
Ascertain
motive for
beginning self-
restraint, and
participation in
therapy.
By providing an
insight into the
willingness of
the patient to
commit to
prolonged
behavioural
change, and if
he holds the
belief that he
can abstain from
consuming
alcohol.
Motivational
interviewing
will form an
Three weeks
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Inviting Roy to suggest how he might want his life to be diverse or better after
the formal treatment
Asking empathetic questions for uncovering information about coping skills
Thanking Roy for his contribution and thoughtful comments.
2. The treatment plan for Roy is given below:
Problem Goals Objectives Methods Timeframe
Alcohol
dependence
Engage in
therapeutic
program.
Ascertain
motive for
beginning self-
restraint, and
participation in
therapy.
By providing an
insight into the
willingness of
the patient to
commit to
prolonged
behavioural
change, and if
he holds the
belief that he
can abstain from
consuming
alcohol.
Motivational
interviewing
will form an
Three weeks
18
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
essential aspect
of this goal
(Thurstone et
al., 2017).
Reviewing the
meaning of
drug
dependence
and the
different
symptoms that
occur due to
dependence
such as,
impairment,
patterns of
abuse, and
tolerance to
alcohol
Psychoeducation
will help in
accomplishing
this goal where
the patient will
be provided
adequate
information on
the ill-effects of
substance abuse
on the
psychological
and
physiological
functioning of
the human body
and he will also
be subjected to
one-to-one
Two weeks
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
essential aspect
of this goal
(Thurstone et
al., 2017).
Reviewing the
meaning of
drug
dependence
and the
different
symptoms that
occur due to
dependence
such as,
impairment,
patterns of
abuse, and
tolerance to
alcohol
Psychoeducation
will help in
accomplishing
this goal where
the patient will
be provided
adequate
information on
the ill-effects of
substance abuse
on the
psychological
and
physiological
functioning of
the human body
and he will also
be subjected to
one-to-one
Two weeks
19
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
discussions that
will help him
realise the
possible risks of
the treatment
program (Koc et
al., 2016).
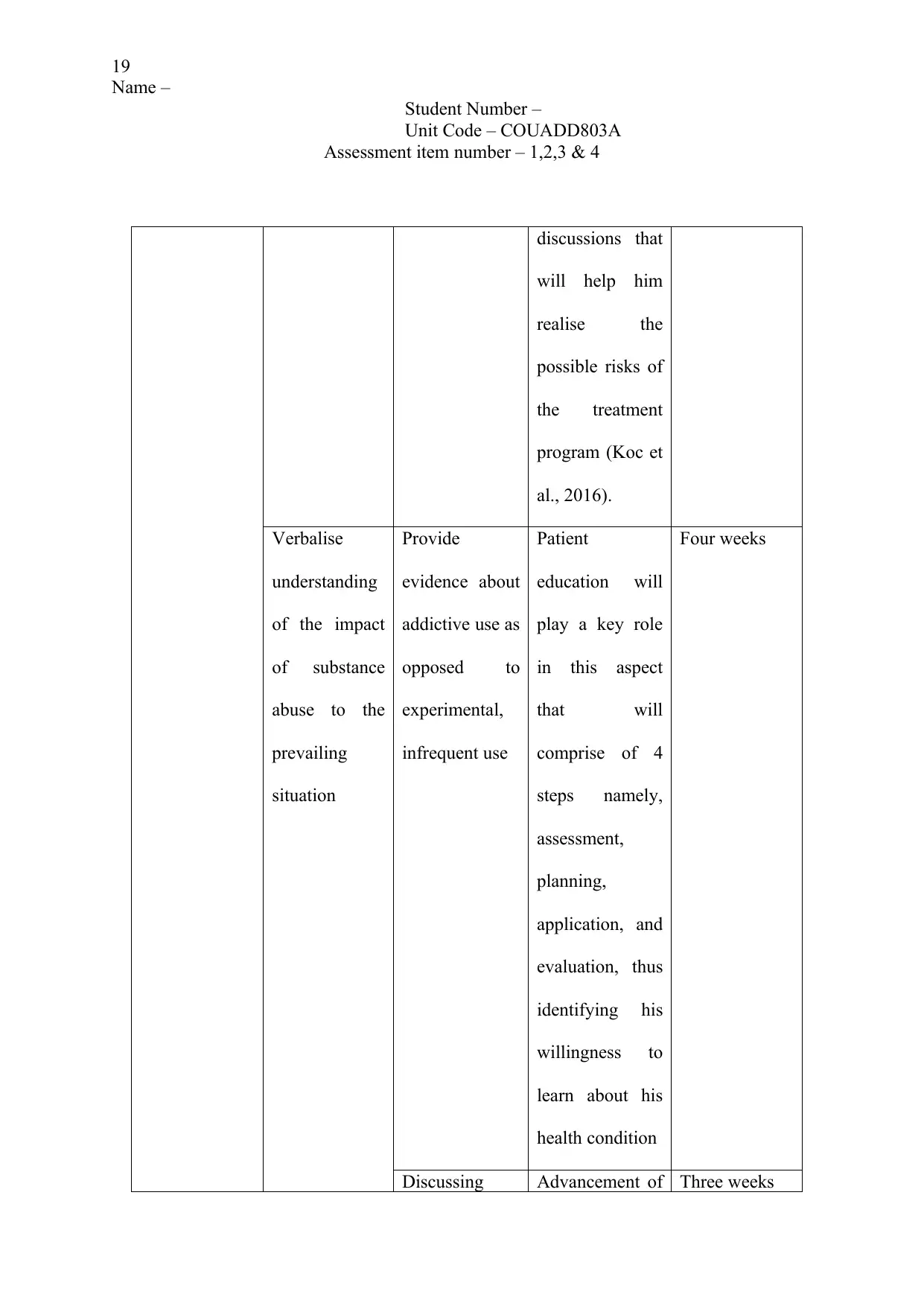
Verbalise
understanding
of the impact
of substance
abuse to the
prevailing
situation
Provide
evidence about
addictive use as
opposed to
experimental,
infrequent use
Patient
education will
play a key role
in this aspect
that will
comprise of 4
steps namely,
assessment,
planning,
application, and
evaluation, thus
identifying his
willingness to
learn about his
health condition
Four weeks
Discussing Advancement of Three weeks
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
discussions that
will help him
realise the
possible risks of
the treatment
program (Koc et
al., 2016).
Verbalise
understanding
of the impact
of substance
abuse to the
prevailing
situation
Provide
evidence about
addictive use as
opposed to
experimental,
infrequent use
Patient
education will
play a key role
in this aspect
that will
comprise of 4
steps namely,
assessment,
planning,
application, and
evaluation, thus
identifying his
willingness to
learn about his
health condition
Four weeks
Discussing Advancement of Three weeks
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
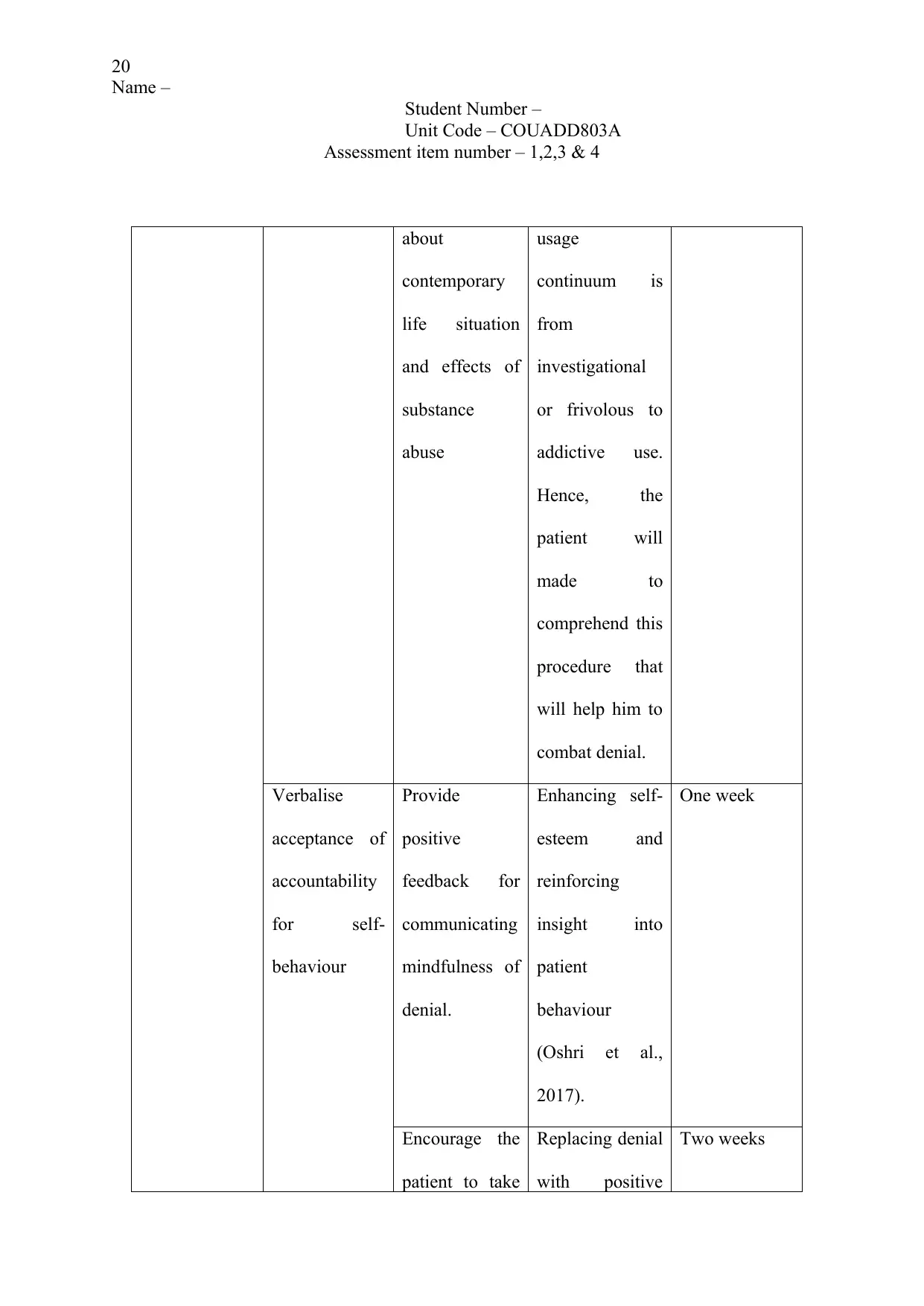
20
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
about
contemporary
life situation
and effects of
substance
abuse
usage
continuum is
from
investigational
or frivolous to
addictive use.
Hence, the
patient will
made to
comprehend this
procedure that
will help him to
combat denial.
Verbalise
acceptance of
accountability
for self-
behaviour
Provide
positive
feedback for
communicating
mindfulness of
denial.
Enhancing self-
esteem and
reinforcing
insight into
patient
behaviour
(Oshri et al.,
2017).
One week
Encourage the
patient to take
Replacing denial
with positive
Two weeks
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
about
contemporary
life situation
and effects of
substance
abuse
usage
continuum is
from
investigational
or frivolous to
addictive use.
Hence, the
patient will
made to
comprehend this
procedure that
will help him to
combat denial.
Verbalise
acceptance of
accountability
for self-
behaviour
Provide
positive
feedback for
communicating
mindfulness of
denial.
Enhancing self-
esteem and
reinforcing
insight into
patient
behaviour
(Oshri et al.,
2017).
One week
Encourage the
patient to take
Replacing denial
with positive
Two weeks
21
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
accountability
for own
recovery
action when the
patient accepts
the authenticity
of own
responsibility.
3. Treatment plan objectives for patients who are subjected to substance abuse generally
comprises of providing necessary support for the pronouncement to discontinue
substance use, , enable learning of new habits to decrease anxiety, reinforce individual
coping abilities, simplify family evolution and development, promote family
participation in a rehabilitation program, and offer data about the prognosis and
treatment requirements. The aforementioned plan has been developed taking into
consideration the fact that Roy might demonstrate denial that can be evidenced by a
delay in seeking healthcare service, or refusing healthcare attention. The primary
objectives of this treatment plan were that the patient would be express his actual
feelings that are correlated with heavy alcohol dependence, as a major strategy to
cope with demanding conditions. Furthermore, the objectives also focus on the fact
that Roy will be able to verbalise the negative impacts of alcohol dependence and
seek professional assistance for the problem. Motivational interviewing has been
identified as a major strategy for accomplishing the goals of this treatment plan. It has
been identified as a client-centred and directive counselling approach for stimulating
behaviour change by facilitating clients to discover and decide ambivalence.
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
accountability
for own
recovery
action when the
patient accepts
the authenticity
of own
responsibility.
3. Treatment plan objectives for patients who are subjected to substance abuse generally
comprises of providing necessary support for the pronouncement to discontinue
substance use, , enable learning of new habits to decrease anxiety, reinforce individual
coping abilities, simplify family evolution and development, promote family
participation in a rehabilitation program, and offer data about the prognosis and
treatment requirements. The aforementioned plan has been developed taking into
consideration the fact that Roy might demonstrate denial that can be evidenced by a
delay in seeking healthcare service, or refusing healthcare attention. The primary
objectives of this treatment plan were that the patient would be express his actual
feelings that are correlated with heavy alcohol dependence, as a major strategy to
cope with demanding conditions. Furthermore, the objectives also focus on the fact
that Roy will be able to verbalise the negative impacts of alcohol dependence and
seek professional assistance for the problem. Motivational interviewing has been
identified as a major strategy for accomplishing the goals of this treatment plan. It has
been identified as a client-centred and directive counselling approach for stimulating
behaviour change by facilitating clients to discover and decide ambivalence.
22
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Associated with non-directive counselling, this method has been identified to be more
goal-directed an focused, and generally deviates from the out-dated Rogerian client-
centred method. While implementing this approach, efforts will be taken to influence
the client to make several changes in his behaviour (Vazquez & Bergin, 2019).
Another approach that has been selected for accomplishment of goals is
psychoeducation. This therapeutic intervention will provide necessary support and
information to Roy for helping him cope with the illness. Selection of this method can
be accredited to the fact that it has earlier proved effective in reducing rate of
hospitalisation and enhancing health outcomes (Winters et al., 2018). Moreover,
reflective listening will also be practiced to help ensure that the patient feels honoured
and dignified, and a genuine interest is displayed to provide information on the
harmful effects of substance abuse on health and wellbeing. Time constraint, lack of
empathy towards the client, preconceived notions about healthcare professionals,
previous traumatic experience, stigma and discrimination, and disjointed organization
of mental health services might act as significant barriers to the treatment plan.
Stigma refers to typecasts and prejudicial insolences held by the community for
people who consume alcohol or drugs (Stringer & Baker, 2018). These disapproving
attitudes might persuade Roy to reject, fear, and distance him from the healthcare
professionals who will participate in the treatment plan. Connexions between diverse
settings are imperative for the recognition and treatment of substance abuse.
However, long waiting time might also make the patient develop resistance to
treatment. In order to eliminate these barriers, efforts will be taken to assist Roy in
developing inconsistencies between the existing self and what he intends to be like in
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Associated with non-directive counselling, this method has been identified to be more
goal-directed an focused, and generally deviates from the out-dated Rogerian client-
centred method. While implementing this approach, efforts will be taken to influence
the client to make several changes in his behaviour (Vazquez & Bergin, 2019).
Another approach that has been selected for accomplishment of goals is
psychoeducation. This therapeutic intervention will provide necessary support and
information to Roy for helping him cope with the illness. Selection of this method can
be accredited to the fact that it has earlier proved effective in reducing rate of
hospitalisation and enhancing health outcomes (Winters et al., 2018). Moreover,
reflective listening will also be practiced to help ensure that the patient feels honoured
and dignified, and a genuine interest is displayed to provide information on the
harmful effects of substance abuse on health and wellbeing. Time constraint, lack of
empathy towards the client, preconceived notions about healthcare professionals,
previous traumatic experience, stigma and discrimination, and disjointed organization
of mental health services might act as significant barriers to the treatment plan.
Stigma refers to typecasts and prejudicial insolences held by the community for
people who consume alcohol or drugs (Stringer & Baker, 2018). These disapproving
attitudes might persuade Roy to reject, fear, and distance him from the healthcare
professionals who will participate in the treatment plan. Connexions between diverse
settings are imperative for the recognition and treatment of substance abuse.
However, long waiting time might also make the patient develop resistance to
treatment. In order to eliminate these barriers, efforts will be taken to assist Roy in
developing inconsistencies between the existing self and what he intends to be like in
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
23
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
the upcoming days, following implementation of the treatment plan (Schuman et al.,
2015). The healthcare professionals might have a tendency to contend the client,
particularly when he is ambivalent about his behavioural change, and this is
specifically accurate when "resistance" is encountered from the client, However,
while enforcing the change, it will be ensured that no arguments are made, thus
preventing the client from being defensive (Coker, Stefanovics & Rosenheck, 2016).
This plan is thought to be effective since it will lead to stronger client self-efficacy
that has been identified as a noteworthy predictor of accomplishment in behaviour
change (Jiang, Wu & Gao, 2017).
During the treatment planning of the patient, the symptoms of the patients must be
taken into consideration. In-toxication of different drugs or combination of different
drugs promotes the expression of different symptoms. For example, the intoxicating
effects of barbiturates are identical to that of alcohol and this makes the framing of the
overall treatment plan confusing. The distinctive symptoms of the barbiturates include
decreased level of moor function, decrease in the level of seizure activity, increased
level of drowsiness, sleep and dizziness. Muscle twitching, weakness, nausea, visual
distortions are some of the other physical symptoms of barbiturates. The behavioural
symptoms of the patient include uncoordinated level of thoughts, shallow breathing,
slow rate of reaction and slurred speech. The cognitive functioning also decreases
along with increase in the level of depression, high level of irritability and intense
level of emotions (Lake, 2019).
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
the upcoming days, following implementation of the treatment plan (Schuman et al.,
2015). The healthcare professionals might have a tendency to contend the client,
particularly when he is ambivalent about his behavioural change, and this is
specifically accurate when "resistance" is encountered from the client, However,
while enforcing the change, it will be ensured that no arguments are made, thus
preventing the client from being defensive (Coker, Stefanovics & Rosenheck, 2016).
This plan is thought to be effective since it will lead to stronger client self-efficacy
that has been identified as a noteworthy predictor of accomplishment in behaviour
change (Jiang, Wu & Gao, 2017).
During the treatment planning of the patient, the symptoms of the patients must be
taken into consideration. In-toxication of different drugs or combination of different
drugs promotes the expression of different symptoms. For example, the intoxicating
effects of barbiturates are identical to that of alcohol and this makes the framing of the
overall treatment plan confusing. The distinctive symptoms of the barbiturates include
decreased level of moor function, decrease in the level of seizure activity, increased
level of drowsiness, sleep and dizziness. Muscle twitching, weakness, nausea, visual
distortions are some of the other physical symptoms of barbiturates. The behavioural
symptoms of the patient include uncoordinated level of thoughts, shallow breathing,
slow rate of reaction and slurred speech. The cognitive functioning also decreases
along with increase in the level of depression, high level of irritability and intense
level of emotions (Lake, 2019).
24
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
If the treatment planning is done based on the usage of the benzodiazepine then
overdose of the benzodiazepine must be taken into consideration through effective
monitoring of the patient. For example, the long-term and over use of the
benzodiazepines include high level of muscle weakness, weight gain, appearance of
skin rash, increase or decrease in libido, lack of motivation, fatigue, nausea, difficult n
sleeping, breathing, anxiety, depression and change in personality (Lake, 2019).
Initial usage of benzodiazepines, the patient must feel sleepy and uncoordinated.
However, the effects can dissipate gradually after the body get adjusted to the intake
of chemical. The increase in the tolerance of the drugs occurs with time (Lake, 2019).
Part B- Evaluating a treatment plan
1. The treatment plan developed for Clarie focuses on motivating her to refrain from the
consumption of marijuana, in order to enhance her health and wellbeing, and sustain
her employment. The effectiveness of this treatment can be accredited to the fact that
it combines humanistic strategies and cognitive-behavioural interventions that will
play an important role invoking inwardly motivated change in the patient (Webb et
al., 2017). The treatment plan will also prove effective in helping Clarie cope with her
conditions by fostering empathy and trust that will help in the establishment of a sense
of unity and will also enhance self-efficacy in the client. It has often been established
that unlike other counselling programs of therapy process, motivation therapy of
clients instils in them a willingness to combat their addiction, through the use of self-
motivational statements (Murphy et al., 2018). Nonetheless, one major issue that
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
If the treatment planning is done based on the usage of the benzodiazepine then
overdose of the benzodiazepine must be taken into consideration through effective
monitoring of the patient. For example, the long-term and over use of the
benzodiazepines include high level of muscle weakness, weight gain, appearance of
skin rash, increase or decrease in libido, lack of motivation, fatigue, nausea, difficult n
sleeping, breathing, anxiety, depression and change in personality (Lake, 2019).
Initial usage of benzodiazepines, the patient must feel sleepy and uncoordinated.
However, the effects can dissipate gradually after the body get adjusted to the intake
of chemical. The increase in the tolerance of the drugs occurs with time (Lake, 2019).
Part B- Evaluating a treatment plan
1. The treatment plan developed for Clarie focuses on motivating her to refrain from the
consumption of marijuana, in order to enhance her health and wellbeing, and sustain
her employment. The effectiveness of this treatment can be accredited to the fact that
it combines humanistic strategies and cognitive-behavioural interventions that will
play an important role invoking inwardly motivated change in the patient (Webb et
al., 2017). The treatment plan will also prove effective in helping Clarie cope with her
conditions by fostering empathy and trust that will help in the establishment of a sense
of unity and will also enhance self-efficacy in the client. It has often been established
that unlike other counselling programs of therapy process, motivation therapy of
clients instils in them a willingness to combat their addiction, through the use of self-
motivational statements (Murphy et al., 2018). Nonetheless, one major issue that
25
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
might develop, in relation to the goals and methods is the lack of motivation in Clarie
owing to reduced social interaction, and withdrawal from her partner and friends. The
fact that Clarie realises that her determination has begun to wane is a major obstacle
that will act as an impediment in the treatment plan. One major drawback of this
treatment plan is that adequate time will be required to build an effective relationship
with the client. In addition, Clarie must demonstrate sufficient cognitive clarity and
outside influences from her partner and peers might make the motivation to cease.
2. One major change that would be made in this treatment plan comprises of the
introduction of the biofeedback method. This method will help Clarie to monitor the
physiological processes of her body that bring about a psychological change. She will
be connected to a technological equipment, following which her immediate biological
parameters will be recorded such as, skin conductance, muscle tension, and heart rate
(Sosin et al., 2017). Watching the physiological reactions of the body improve over
time, while abstaining from marijuana consumption will help Clarie gain a sound
understanding of the essential skill and proficiency of self-regulation that is
imperative in addiction recovery. She will also be subjected to contingency
management (CM) that would encompass application of operant conditioning that
uses positive reinforcement and stimulus control for altering behaviour (Becker et al.,
2016). While positive behaviour from the client will be less punished or rewarded,
failure to demonstrate adherence to the rules of the treatment plan would lead to
punishment. Clarie will be provided with the occasion to win prizes and vouchers, in
order to promote abstinence from marijuana. Hence, the primary goal of this strategy
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
might develop, in relation to the goals and methods is the lack of motivation in Clarie
owing to reduced social interaction, and withdrawal from her partner and friends. The
fact that Clarie realises that her determination has begun to wane is a major obstacle
that will act as an impediment in the treatment plan. One major drawback of this
treatment plan is that adequate time will be required to build an effective relationship
with the client. In addition, Clarie must demonstrate sufficient cognitive clarity and
outside influences from her partner and peers might make the motivation to cease.
2. One major change that would be made in this treatment plan comprises of the
introduction of the biofeedback method. This method will help Clarie to monitor the
physiological processes of her body that bring about a psychological change. She will
be connected to a technological equipment, following which her immediate biological
parameters will be recorded such as, skin conductance, muscle tension, and heart rate
(Sosin et al., 2017). Watching the physiological reactions of the body improve over
time, while abstaining from marijuana consumption will help Clarie gain a sound
understanding of the essential skill and proficiency of self-regulation that is
imperative in addiction recovery. She will also be subjected to contingency
management (CM) that would encompass application of operant conditioning that
uses positive reinforcement and stimulus control for altering behaviour (Becker et al.,
2016). While positive behaviour from the client will be less punished or rewarded,
failure to demonstrate adherence to the rules of the treatment plan would lead to
punishment. Clarie will be provided with the occasion to win prizes and vouchers, in
order to promote abstinence from marijuana. Hence, the primary goal of this strategy
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

26
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
would be to help the client gain an access to the natural reinforcement community,
thus preventing further addiction.
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
would be to help the client gain an access to the natural reinforcement community,
thus preventing further addiction.
27
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
References
Becker, S. J., Squires, D. D., Strong, D. R., Barnett, N. P., Monti, P. M., & Petry, N. M.
(2016). Training opioid addiction treatment providers to adopt contingency
management: A prospective pilot trial of a comprehensive implementation science
approach. Substance abuse, 37(1), 134-140.
Bouchard, J. P., Brulin-Solignac, D., & Lodetti, C. (2017). Court-ordered therapy, a measure
for preventing reoffending. Soins. Psychiatrie, 38(309), 12-16.
Coker, K. L., Stefanovics, E., & Rosenheck, R. (2016). Correlates of improvement in
substance abuse among dually diagnosed veterans with post-traumatic stress disorder
in specialized intensive VA treatment. Psychological trauma: theory, research,
practice, and policy, 8(1), 41.
DiClemente, C. C., Norwood, A. E., Gregory, W. H., Travaglini, L., Graydon, M. M., &
Corno, C. M. (2016). Consumer-centered, collaborative, and comprehensive care: the
core essentials of recovery-oriented system of care. Journal of addictions
nursing, 27(2), 94-100.
Jiang, S., Wu, L., & Gao, X. (2017). Beyond face-to-face individual counseling: A systematic
review on alternative modes of motivational interviewing in substance abuse
treatment and prevention. Addictive behaviours, 73, 216-235.
Koc, M., Iskender, M., Soyer, F., Dusunceli, B., & Colak, T. S. (2016). The Effectiveness of
the Psychoeducational Effective Parenting Program Application on Symptoms of
Psychoactive Substance Use. Studies on Ethno-Medicine, 10(2), 206-215.
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
References
Becker, S. J., Squires, D. D., Strong, D. R., Barnett, N. P., Monti, P. M., & Petry, N. M.
(2016). Training opioid addiction treatment providers to adopt contingency
management: A prospective pilot trial of a comprehensive implementation science
approach. Substance abuse, 37(1), 134-140.
Bouchard, J. P., Brulin-Solignac, D., & Lodetti, C. (2017). Court-ordered therapy, a measure
for preventing reoffending. Soins. Psychiatrie, 38(309), 12-16.
Coker, K. L., Stefanovics, E., & Rosenheck, R. (2016). Correlates of improvement in
substance abuse among dually diagnosed veterans with post-traumatic stress disorder
in specialized intensive VA treatment. Psychological trauma: theory, research,
practice, and policy, 8(1), 41.
DiClemente, C. C., Norwood, A. E., Gregory, W. H., Travaglini, L., Graydon, M. M., &
Corno, C. M. (2016). Consumer-centered, collaborative, and comprehensive care: the
core essentials of recovery-oriented system of care. Journal of addictions
nursing, 27(2), 94-100.
Jiang, S., Wu, L., & Gao, X. (2017). Beyond face-to-face individual counseling: A systematic
review on alternative modes of motivational interviewing in substance abuse
treatment and prevention. Addictive behaviours, 73, 216-235.
Koc, M., Iskender, M., Soyer, F., Dusunceli, B., & Colak, T. S. (2016). The Effectiveness of
the Psychoeducational Effective Parenting Program Application on Symptoms of
Psychoactive Substance Use. Studies on Ethno-Medicine, 10(2), 206-215.
28
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Lake, J. H. (2019). Treatment Planning in Integrative Mental Health Care. In An Integrative
Paradigm for Mental Health Care (pp. 151-193). Springer, Cham.
Murphy, C. M., Ting, L. A., Jordan, L. C., Musser, P. H., Winters, J. J., Poole, G. M., & Pitts,
S. C. (2018). A randomized clinical trial of motivational enhancement therapy for
alcohol problems in partner violent men. Journal of substance abuse treatment, 89,
11-19.
Oshri, A., Carlson, M. W., Kwon, J. A., Zeichner, A., & Wickrama, K. K. (2017).
Developmental growth trajectories of self-esteem in adolescence: Associations with
child neglect and drug use and abuse in young adulthood. Journal of youth and
adolescence, 46(1), 151-164.
Schuman, D. L., Slone, N. C., Reese, R. J., & Duncan, B. (2015). Efficacy of client feedback
in group psychotherapy with soldiers referred for substance abuse
treatment. Psychotherapy Research, 25(4), 396-407.
Sosin, I., Chuev, Y., Volkov, A., & Goncharova, O. (2017). Anti-craving biofeedback
program in clinical course of pathological addictions. European Psychiatry, 41, S879.
Stringer, K. L., & Baker, E. H. (2018). Stigma as a barrier to substance abuse treatment
among those with unmet need: an analysis of parenthood and marital status. Journal
of family issues, 39(1), 3-27.
Thurstone, C., Hull, M., Timmerman, J., & Emrick, C. (2017). Development of a
motivational interviewing/acceptance and commitment therapy model for adolescent
substance use treatment. Journal of contextual behavioural science, 6(4), 375-379.
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Lake, J. H. (2019). Treatment Planning in Integrative Mental Health Care. In An Integrative
Paradigm for Mental Health Care (pp. 151-193). Springer, Cham.
Murphy, C. M., Ting, L. A., Jordan, L. C., Musser, P. H., Winters, J. J., Poole, G. M., & Pitts,
S. C. (2018). A randomized clinical trial of motivational enhancement therapy for
alcohol problems in partner violent men. Journal of substance abuse treatment, 89,
11-19.
Oshri, A., Carlson, M. W., Kwon, J. A., Zeichner, A., & Wickrama, K. K. (2017).
Developmental growth trajectories of self-esteem in adolescence: Associations with
child neglect and drug use and abuse in young adulthood. Journal of youth and
adolescence, 46(1), 151-164.
Schuman, D. L., Slone, N. C., Reese, R. J., & Duncan, B. (2015). Efficacy of client feedback
in group psychotherapy with soldiers referred for substance abuse
treatment. Psychotherapy Research, 25(4), 396-407.
Sosin, I., Chuev, Y., Volkov, A., & Goncharova, O. (2017). Anti-craving biofeedback
program in clinical course of pathological addictions. European Psychiatry, 41, S879.
Stringer, K. L., & Baker, E. H. (2018). Stigma as a barrier to substance abuse treatment
among those with unmet need: an analysis of parenthood and marital status. Journal
of family issues, 39(1), 3-27.
Thurstone, C., Hull, M., Timmerman, J., & Emrick, C. (2017). Development of a
motivational interviewing/acceptance and commitment therapy model for adolescent
substance use treatment. Journal of contextual behavioural science, 6(4), 375-379.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
29
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Vazquez, V. E., & Bergin, A. (2019). Effectiveness of a Specialized Inpatient Treatment
Program for Substance and Alcohol Abusing Pregnant Women. Journal of Drug
Issues, 0022042619831986.’
Webb, H. J., Thomas, R., McGregor, L., Avdagic, E., & Zimmer-Gembeck, M. J. (2017). An
evaluation of parent–child interaction therapy with and without motivational
enhancement to reduce attrition. Journal of Clinical Child & Adolescent
Psychology, 46(4), 537-550.
Winters, K. C., Botzet, A. M., Stinchfield, R., Gonzales-Castaneda, R., Finch, A. J., Piehler,
T. F., ... & Hemze, A. (2018). Adolescent substance abuse treatment: A review of
evidence-based research. In Adolescent Substance Abuse(pp. 141-171). Springer,
Cham.
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Vazquez, V. E., & Bergin, A. (2019). Effectiveness of a Specialized Inpatient Treatment
Program for Substance and Alcohol Abusing Pregnant Women. Journal of Drug
Issues, 0022042619831986.’
Webb, H. J., Thomas, R., McGregor, L., Avdagic, E., & Zimmer-Gembeck, M. J. (2017). An
evaluation of parent–child interaction therapy with and without motivational
enhancement to reduce attrition. Journal of Clinical Child & Adolescent
Psychology, 46(4), 537-550.
Winters, K. C., Botzet, A. M., Stinchfield, R., Gonzales-Castaneda, R., Finch, A. J., Piehler,
T. F., ... & Hemze, A. (2018). Adolescent substance abuse treatment: A review of
evidence-based research. In Adolescent Substance Abuse(pp. 141-171). Springer,
Cham.
30
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Assessment task 4
Part A- Referral strategies
1. Dual diagnosis is an umbrella term that refers to the condition during which a patient
suffers from substance abuse problem and a comorbid mental disorder, such as,
depression and alcoholism (Cutter et al., 2018). The indications that suggest the
presence of dual diagnosis in George are that he regularly consumes cocaine and
marijuana, thus suffers from substance abuse. In addition, he has been found arguing
with himself and also reports hearing voices that do not exist in real, which are
symptoms of a mental disorder (schizophrenia).
2. Individuals experiencing a mental disorder typically turn to drugs or alcohol as a type
of self-medication for enhancing the psychological symptoms they experience.
Combined treatment includes a unified combination of interventions into a distinct
coherent treatment bundle. Abuse counsellors are expected to create a treatment plan
that is based on detoxification, inpatient rehabilitation, psychotherapy, and self-help.
Detoxification will focus on monitoring George for seven days, to few weeks during
which tapering quantity of cocaine and marijuana, or their medical alternative will be
administered to reduce the withdrawal symptoms (Sofer, Kaptsan & Anson, 2018).
Inpatient rehabilitation will prove effective since it will focus on administration of
therapy, medication, support, and health services for addressing substance abuse and
its underlying factors. Psychotherapy will form an essential aspect of the care plan
since it will help George to cope with his emotions and will also alter ineffective
thinking patterns, thus improving his symptoms (Chilton, Crone & Tyson, 2018).
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Assessment task 4
Part A- Referral strategies
1. Dual diagnosis is an umbrella term that refers to the condition during which a patient
suffers from substance abuse problem and a comorbid mental disorder, such as,
depression and alcoholism (Cutter et al., 2018). The indications that suggest the
presence of dual diagnosis in George are that he regularly consumes cocaine and
marijuana, thus suffers from substance abuse. In addition, he has been found arguing
with himself and also reports hearing voices that do not exist in real, which are
symptoms of a mental disorder (schizophrenia).
2. Individuals experiencing a mental disorder typically turn to drugs or alcohol as a type
of self-medication for enhancing the psychological symptoms they experience.
Combined treatment includes a unified combination of interventions into a distinct
coherent treatment bundle. Abuse counsellors are expected to create a treatment plan
that is based on detoxification, inpatient rehabilitation, psychotherapy, and self-help.
Detoxification will focus on monitoring George for seven days, to few weeks during
which tapering quantity of cocaine and marijuana, or their medical alternative will be
administered to reduce the withdrawal symptoms (Sofer, Kaptsan & Anson, 2018).
Inpatient rehabilitation will prove effective since it will focus on administration of
therapy, medication, support, and health services for addressing substance abuse and
its underlying factors. Psychotherapy will form an essential aspect of the care plan
since it will help George to cope with his emotions and will also alter ineffective
thinking patterns, thus improving his symptoms (Chilton, Crone & Tyson, 2018).
31
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
While treating such a patient might be challenging, allowing George to access support
groups will help him share his emotions. During designing of the treatment, it must be
taken into consideration what is the source of the referrals. The source of the referrals
can be voluntary that is sourced by the client himself or involuntary that is sourced by
the friends or the family member of the patient. Depending on the nature of the
referrals, the treatment planning will be framed.
3. While the choice to make a referral is a serious one, it is frequently problematic.
Furthermore, identifying patients who require intervention and directing rapid
referrals to suitable organisations when desired is essential to the roles of a
professional counsellor. Some major strategies that will be adopted for a coordinated
referral for George are namely, (i) development of a therapeutic alliance with
clinician, (ii) increasing access to primary mental service, (iii) fostering contact with
psychiatric disability rehabilitation service, and (iv) establishing connection with
alcohol and drug treatment facility (Jackson et al., 2016). Referral to primary mental
health service will help in effective diagnosis of the mental disorder that George is
suffering from, followed by application of major behavioural and psychological skills
like counselling, interviewing, and interpersonal skills that will improve health
outcomes. The disability rehabilitation service providers will support George
throughout his recovery and will also meet his social and employment needs (Searby,
Maude & McGrath, 2017). The drug treatment service will also prove effective in
addiction recovery. Furthermore, a coordinator will also be required during the
transition of the client between the different services, and such coordinator will either
be a peer or a lived experience consultant.
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
While treating such a patient might be challenging, allowing George to access support
groups will help him share his emotions. During designing of the treatment, it must be
taken into consideration what is the source of the referrals. The source of the referrals
can be voluntary that is sourced by the client himself or involuntary that is sourced by
the friends or the family member of the patient. Depending on the nature of the
referrals, the treatment planning will be framed.
3. While the choice to make a referral is a serious one, it is frequently problematic.
Furthermore, identifying patients who require intervention and directing rapid
referrals to suitable organisations when desired is essential to the roles of a
professional counsellor. Some major strategies that will be adopted for a coordinated
referral for George are namely, (i) development of a therapeutic alliance with
clinician, (ii) increasing access to primary mental service, (iii) fostering contact with
psychiatric disability rehabilitation service, and (iv) establishing connection with
alcohol and drug treatment facility (Jackson et al., 2016). Referral to primary mental
health service will help in effective diagnosis of the mental disorder that George is
suffering from, followed by application of major behavioural and psychological skills
like counselling, interviewing, and interpersonal skills that will improve health
outcomes. The disability rehabilitation service providers will support George
throughout his recovery and will also meet his social and employment needs (Searby,
Maude & McGrath, 2017). The drug treatment service will also prove effective in
addiction recovery. Furthermore, a coordinator will also be required during the
transition of the client between the different services, and such coordinator will either
be a peer or a lived experience consultant.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
32
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
4. The overall presentation of the issue needs to be evaluated in detail and this will
involve a detail discussion with the client about the main psychological complications
that he is facing along with the social, financial or legal barriers of any. The risk
assessment needs to done based on the overall presentation of the client issue. The
client issue needs to be presented with the help of clinical interview. The factors that
must be considered in the clinical interview include, the tendency of self-harm, the
generation of thoughts of harming others. The interview must also focus on the
previous treatments undertaken by the client and what they feel is particularly helpful
for them. During the assessment of the client for the identification of the clinical
priority before channelizing the referrals, the personal strength and weakness along
with the personal family history must also be taken under active consideration (Foley‐
Nicpon & Assouline, 2015). This information mainly steams from the initiative of
collection of the other assessment data or by the help of direct inquiry. The
observation of the client throughout the process of interview can help the counsellor
to extract the general pictures of the mental state of the client. The key consideration
of the that must observed by the counsellor after the referral include the change of
mood of the client, the pattern of speech of the client, behaviour, the movements of
eyes and complexicty of thoughts (Foley‐Nicpon & Assouline, 2015).
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
4. The overall presentation of the issue needs to be evaluated in detail and this will
involve a detail discussion with the client about the main psychological complications
that he is facing along with the social, financial or legal barriers of any. The risk
assessment needs to done based on the overall presentation of the client issue. The
client issue needs to be presented with the help of clinical interview. The factors that
must be considered in the clinical interview include, the tendency of self-harm, the
generation of thoughts of harming others. The interview must also focus on the
previous treatments undertaken by the client and what they feel is particularly helpful
for them. During the assessment of the client for the identification of the clinical
priority before channelizing the referrals, the personal strength and weakness along
with the personal family history must also be taken under active consideration (Foley‐
Nicpon & Assouline, 2015). This information mainly steams from the initiative of
collection of the other assessment data or by the help of direct inquiry. The
observation of the client throughout the process of interview can help the counsellor
to extract the general pictures of the mental state of the client. The key consideration
of the that must observed by the counsellor after the referral include the change of
mood of the client, the pattern of speech of the client, behaviour, the movements of
eyes and complexicty of thoughts (Foley‐Nicpon & Assouline, 2015).
33
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Part B- Evaluating referral process
1. Alcoholism, also referred to as alcohol dependence refers to a serious type of drinking
issue and outlines the uncontrollable and strong urge to drink (Bogenschutz et al.,
2015). Sarah visited the community drop-in centre with the aim of seeking help for
her alcohol dependence symptoms. On visiting the drop-in centre, Sarah was provided
with a contact number for the inpatient clinic and was also not informed about the
charges that would be associated with the care seeking process. However, the
worker’s actions were not appropriate since it is imperative for a drop-in centre to
create a friendly environment that helps people to cope with their psychological
struggles (Chechak, Dunlop & Holosko, 2019). If I were in place of the worker, I
would have tried to address the major concerns that Sarah is facing such as,
homelessness, addiction, and unemployment. I would have referred her to government
homelessness welfare services that have proved their efficacy in preventing
homelessness for low-income individuals and families. She would have been given
the names of different organisations that provide employment to vulnerable and
disadvantaged individuals, regardless of their psychological condition (Tucker et al.,
2018). In addition, I would have also established contact with an addiction referral
centre that would have created a healthy environment to promote recovery of the
client from substance abuse.
2. Outpatient treatment for alcohol and drugs is generally problematic owing to the fact
that the clients endure to sustain their lives, as they progress through the recovery
process, in contrast to spending their time in inpatient facilities. The major
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Part B- Evaluating referral process
1. Alcoholism, also referred to as alcohol dependence refers to a serious type of drinking
issue and outlines the uncontrollable and strong urge to drink (Bogenschutz et al.,
2015). Sarah visited the community drop-in centre with the aim of seeking help for
her alcohol dependence symptoms. On visiting the drop-in centre, Sarah was provided
with a contact number for the inpatient clinic and was also not informed about the
charges that would be associated with the care seeking process. However, the
worker’s actions were not appropriate since it is imperative for a drop-in centre to
create a friendly environment that helps people to cope with their psychological
struggles (Chechak, Dunlop & Holosko, 2019). If I were in place of the worker, I
would have tried to address the major concerns that Sarah is facing such as,
homelessness, addiction, and unemployment. I would have referred her to government
homelessness welfare services that have proved their efficacy in preventing
homelessness for low-income individuals and families. She would have been given
the names of different organisations that provide employment to vulnerable and
disadvantaged individuals, regardless of their psychological condition (Tucker et al.,
2018). In addition, I would have also established contact with an addiction referral
centre that would have created a healthy environment to promote recovery of the
client from substance abuse.
2. Outpatient treatment for alcohol and drugs is generally problematic owing to the fact
that the clients endure to sustain their lives, as they progress through the recovery
process, in contrast to spending their time in inpatient facilities. The major
34
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
recommendation will be based on development and implementation of interventions
that would promote reintegration of the patients to the healthy environment, besides
lowering the manifestation of harmful behaviour among individuals who have been
identified vulnerable (Catanzano et al., 2018). The key recommendations will focus
on the need for identifying consumer choice, in relation to access to place to sleep,
food, stay clean, and spend reduced time on the streets. The drop-in centre will be
asked to adopt a philosophy that is based on the significance of unrestricted positive
regard, candidness and understanding among program workforce towards the clients.
Emphasis will be placed on presence of a secure funding from charitable organisation,
private donors and government source, and creation of a layout where there must be
different spaces or rooms that would reduce conflict and crowd (Zolala et al., 2016).
The staff must also be provided training and education for addressing the concerns of
their clients, and obtaining feedback.
References
Bogenschutz, M. P., Forcehimes, A. A., Pommy, J. A., Wilcox, C. E., Barbosa, P. C. R., &
Strassman, R. J. (2015). Psilocybin-assisted treatment for alcohol dependence: a
proof-of-concept study. Journal of psychopharmacology, 29(3), 289-299.
Catanzano, M., Souray, R., Tibber, M., Kothari, R., Bennett, S., Liang, H., ... & Shafran, R.
(2018). 052 Evaluation of a mental health and psychological wellbeing drop-in centre
in a paediatric hospital setting.
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
recommendation will be based on development and implementation of interventions
that would promote reintegration of the patients to the healthy environment, besides
lowering the manifestation of harmful behaviour among individuals who have been
identified vulnerable (Catanzano et al., 2018). The key recommendations will focus
on the need for identifying consumer choice, in relation to access to place to sleep,
food, stay clean, and spend reduced time on the streets. The drop-in centre will be
asked to adopt a philosophy that is based on the significance of unrestricted positive
regard, candidness and understanding among program workforce towards the clients.
Emphasis will be placed on presence of a secure funding from charitable organisation,
private donors and government source, and creation of a layout where there must be
different spaces or rooms that would reduce conflict and crowd (Zolala et al., 2016).
The staff must also be provided training and education for addressing the concerns of
their clients, and obtaining feedback.
References
Bogenschutz, M. P., Forcehimes, A. A., Pommy, J. A., Wilcox, C. E., Barbosa, P. C. R., &
Strassman, R. J. (2015). Psilocybin-assisted treatment for alcohol dependence: a
proof-of-concept study. Journal of psychopharmacology, 29(3), 289-299.
Catanzano, M., Souray, R., Tibber, M., Kothari, R., Bennett, S., Liang, H., ... & Shafran, R.
(2018). 052 Evaluation of a mental health and psychological wellbeing drop-in centre
in a paediatric hospital setting.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
35
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Chechak, D. J., Dunlop, J. M., & Holosko, M. J. (2019). Evaluating Youth Drop-In
Programs: The Utility of Process Evaluation Methods. Canadian Journal of Program
Evaluation, 34(1).
Chilton, J., Crone, D., & Tyson, P. J. (2018). Clinical Outcomes From a 10-Week Follow-Up
Psychoeducational Program for Dual Diagnosis. Journal of dual diagnosis, 14(2),
102-110.
Cutter, C., Buono, F., Ackerman, S., Brennan, M., Mueller, D., Cerbone, M., ... & Savage, S.
(2018). Dual diagnosis inpatient treatment outcomes for individuals with co-occurring
chronic pain and opioid use disorder. The Journal of Pain, 19(3), S32.
Foley‐Nicpon, M., & Assouline, S. G. (2015). Counseling considerations for the twice‐
exceptional client. Journal of Counseling & Development, 93(2), 202-211.
Jackson, L., Felstead, B., Bhowmik, J., Avery, R., & Nelson-Hearity, R. (2016). Towards
holistic dual diagnosis care: physical health screening in a Victorian community-
based alcohol and drug treatment service. Australian journal of primary health, 22(2),
81-85.
Searby, A., Maude, P., & McGrath, I. (2017). The experiences of clinicians caring for older
adults with dual diagnosis: An exploratory study. Issues in mental health
nursing, 38(10), 805-811.
Sofer, M. M., Kaptsan, A., & Anson, J. (2018). Factors Associated with Unplanned Early
Discharges from a Dual Diagnosis Inpatient Detoxification Unit in Israel. Journal of
dual diagnosis, 14(3), 137-147.
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Chechak, D. J., Dunlop, J. M., & Holosko, M. J. (2019). Evaluating Youth Drop-In
Programs: The Utility of Process Evaluation Methods. Canadian Journal of Program
Evaluation, 34(1).
Chilton, J., Crone, D., & Tyson, P. J. (2018). Clinical Outcomes From a 10-Week Follow-Up
Psychoeducational Program for Dual Diagnosis. Journal of dual diagnosis, 14(2),
102-110.
Cutter, C., Buono, F., Ackerman, S., Brennan, M., Mueller, D., Cerbone, M., ... & Savage, S.
(2018). Dual diagnosis inpatient treatment outcomes for individuals with co-occurring
chronic pain and opioid use disorder. The Journal of Pain, 19(3), S32.
Foley‐Nicpon, M., & Assouline, S. G. (2015). Counseling considerations for the twice‐
exceptional client. Journal of Counseling & Development, 93(2), 202-211.
Jackson, L., Felstead, B., Bhowmik, J., Avery, R., & Nelson-Hearity, R. (2016). Towards
holistic dual diagnosis care: physical health screening in a Victorian community-
based alcohol and drug treatment service. Australian journal of primary health, 22(2),
81-85.
Searby, A., Maude, P., & McGrath, I. (2017). The experiences of clinicians caring for older
adults with dual diagnosis: An exploratory study. Issues in mental health
nursing, 38(10), 805-811.
Sofer, M. M., Kaptsan, A., & Anson, J. (2018). Factors Associated with Unplanned Early
Discharges from a Dual Diagnosis Inpatient Detoxification Unit in Israel. Journal of
dual diagnosis, 14(3), 137-147.
36
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Tucker, J. S., Pedersen, E. R., Parast, L., & Klein, D. J. (2018). Factors associated with drop-
in center utilization among unaccompanied youth experiencing
homelessness. Children and Youth Services Review, 91, 347-354.
Zolala, F., Mahdavian, M., Haghdoost, A. A., & Karamouzian, M. (2016). Pathways to
addiction: A gender-based study on drug use in a triangular clinic and drop-in center,
Kerman, Iran. International journal of high risk behaviours & addiction, 5(2).
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Tucker, J. S., Pedersen, E. R., Parast, L., & Klein, D. J. (2018). Factors associated with drop-
in center utilization among unaccompanied youth experiencing
homelessness. Children and Youth Services Review, 91, 347-354.
Zolala, F., Mahdavian, M., Haghdoost, A. A., & Karamouzian, M. (2016). Pathways to
addiction: A gender-based study on drug use in a triangular clinic and drop-in center,
Kerman, Iran. International journal of high risk behaviours & addiction, 5(2).

37
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
Name –
Student Number –
Unit Code – COUADD803A
Assessment item number – 1,2,3 & 4
1 out of 37
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.




