Diabetes Prevalence: Indigenous vs. Non-Indigenous Populations Report
VerifiedAdded on 2022/08/13
|22
|5639
|37
Report
AI Summary
This report presents a comparative analysis of diabetes burden, focusing on the Australian and United States populations. It examines the prevalence of diabetes among indigenous and non-indigenous groups within both countries. The report begins by introducing diabetes mellitus (DM) as a significant health priority, outlining its impact and the context within the Australian Health Priority Areas. It then delves into a literature review, comparing data on diabetes prevalence between indigenous and non-indigenous populations in Australia and the United States. The analysis considers various factors influencing the disease burden, including lifestyle, genetic predisposition, and socio-economic factors. Furthermore, the report highlights the role of social determinants in shaping health outcomes and concludes with a discussion on the implications of these findings, relating to the importance of capacity building, collaboration, and sustainability in addressing the health priority. The paper is divided into two parts, Part A focusing on the comparison and Part B on a novel strategy plan to help the selected population to recover from the diseased condition.

Running head: EPIDEMIOLOGY
COMPARE AND CONTRAST DISEASE BURDEN
Name of the Student
Name of the University
Author Note
Table of Content
COMPARE AND CONTRAST DISEASE BURDEN
Name of the Student
Name of the University
Author Note
Table of Content
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1EPIDEMIOLOGY
s
Part A...............................................................................................................................................3
Introduction..................................................................................................................................3
Australian Health Priority Area...................................................................................................3
Literature analysis........................................................................................................................4
Disease burden in Australia (indigenous and non-indigenous)...................................................5
Disease burden in the United States (indigenous and non-indigenous)......................................5
Comparison of burden in both the countries................................................................................7
Conclusion...................................................................................................................................8
Part B...............................................................................................................................................8
Introduction..................................................................................................................................8
Area of the highest prevalence....................................................................................................9
Strategy to reduce the prevalence..............................................................................................11
Aim of the strategy................................................................................................................11
Focus group...........................................................................................................................11
Strategy..................................................................................................................................11
Collaboration.........................................................................................................................12
Sustainability.........................................................................................................................13
Capacity building...................................................................................................................13
Relation of the strategy to health-specific determinants............................................................14
s
Part A...............................................................................................................................................3
Introduction..................................................................................................................................3
Australian Health Priority Area...................................................................................................3
Literature analysis........................................................................................................................4
Disease burden in Australia (indigenous and non-indigenous)...................................................5
Disease burden in the United States (indigenous and non-indigenous)......................................5
Comparison of burden in both the countries................................................................................7
Conclusion...................................................................................................................................8
Part B...............................................................................................................................................8
Introduction..................................................................................................................................8
Area of the highest prevalence....................................................................................................9
Strategy to reduce the prevalence..............................................................................................11
Aim of the strategy................................................................................................................11
Focus group...........................................................................................................................11
Strategy..................................................................................................................................11
Collaboration.........................................................................................................................12
Sustainability.........................................................................................................................13
Capacity building...................................................................................................................13
Relation of the strategy to health-specific determinants............................................................14
2EPIDEMIOLOGY
Conclusion.................................................................................................................................14
References......................................................................................................................................16
Conclusion.................................................................................................................................14
References......................................................................................................................................16
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3EPIDEMIOLOGY
This paper will be divided into two parts. The first part will discuss the prevalence of one
of the Australian Nine health priorities areas and its burden in a comparison country. The next
part will discuss a novel strategy plan to help the selected population to recover from the
diseased condition. This paper will focus on the difference between the indigenous and non-
indigenous population based on diabetes as the chosen health priority area.
Part A
Introduction
DM (Diabetes mellitus) is primarily known as diabetes which is a group of metabolic
health disorders associated with a high sugar level of blood over a long time period. This disease
has been found to be referred to as a disease group that affects the way in which the human body
uses glucose (blood sugar) (Asmat, Abad & Ismail, 2016). Diabetes has also been found to
contribute very little to the rates of mortality among the people who are under the age of 55 years
and has been found to contribute less to the prevalence of diabetes. According to various pieces
of literature, it can be stated that Pimas are associated with the HLA-A2 phenotype and two
genetic markers on chromosome 4q and 7q which are linked to insulin resistance. No matter
what type of diabetes occurs in an individual, it will lead to the presence of excess sugar in their
blood. According to the statistical reports it can be stated that around 1.7 million people in
Australia have diabetes today. This calculation includes all the diagnosis types including 1.2
million as registered diabetes patients and 500,000 as undiagnosed type 2 diabetes patients
(Zimmet et al., 2016). This section will discuss the difference between diabetes prevalence
among the indigenous and non-indigenous people of Australia compared to the indigenous and
non-indigenous groups of the United States (US). This part will focus on the collection of data
This paper will be divided into two parts. The first part will discuss the prevalence of one
of the Australian Nine health priorities areas and its burden in a comparison country. The next
part will discuss a novel strategy plan to help the selected population to recover from the
diseased condition. This paper will focus on the difference between the indigenous and non-
indigenous population based on diabetes as the chosen health priority area.
Part A
Introduction
DM (Diabetes mellitus) is primarily known as diabetes which is a group of metabolic
health disorders associated with a high sugar level of blood over a long time period. This disease
has been found to be referred to as a disease group that affects the way in which the human body
uses glucose (blood sugar) (Asmat, Abad & Ismail, 2016). Diabetes has also been found to
contribute very little to the rates of mortality among the people who are under the age of 55 years
and has been found to contribute less to the prevalence of diabetes. According to various pieces
of literature, it can be stated that Pimas are associated with the HLA-A2 phenotype and two
genetic markers on chromosome 4q and 7q which are linked to insulin resistance. No matter
what type of diabetes occurs in an individual, it will lead to the presence of excess sugar in their
blood. According to the statistical reports it can be stated that around 1.7 million people in
Australia have diabetes today. This calculation includes all the diagnosis types including 1.2
million as registered diabetes patients and 500,000 as undiagnosed type 2 diabetes patients
(Zimmet et al., 2016). This section will discuss the difference between diabetes prevalence
among the indigenous and non-indigenous people of Australia compared to the indigenous and
non-indigenous groups of the United States (US). This part will focus on the collection of data
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4EPIDEMIOLOGY
through a literature analysis process in order to analyze the comparison between the before stated
conditions.
Australian Health Priority Area
There are nine Australian Health priority areas. The national health priority areas
(NHPAs) were established in response to the WHO (World Health Organisation's) Global Health
Strategy for all from the year 2000 (Lazzarini et al., 2018). This framework focused on the health
policy and public attention on various areas that were considered to significantly contribute to
the disease burden in Australia. By the burden of a disease, it can be stated that it is a way to
measure the disease's impact on population injuries and death. The nine health priority regions of
Australia includes cancer control, cardiovascular health, prevention of injury and control, mental
health (1996), Diabetes mellitus (1997), Asthma (1999), Arthritis and musculoskeletal conditions
(2002), obesity and dementia (2008) and (2012) respectively (Kapp & Santamaria, 2015). The
national strategic framework associated with chronic conditions has been found to be associated
with the current document policy on chronic diseases in 2017. This policy has been found to
migrate to a disease-specific focus and provides guidance to the national response delivery and
health systems that respond in a more effective way. This paper will select Diabetes as a health
priority from 9 NHPAs in order to do the comparison study.
Literature analysis
According to Keel et al., (2017), the prevalence of self-reported diabetes among the
Indigenous and non-Indigenous Australian population varied to a high extent. The overall
prevalence of self-reported diabetes was reported to be very high and it was calculated to be four
times higher than among the Indigenous Australians. The rapidly increasing prevalence
through a literature analysis process in order to analyze the comparison between the before stated
conditions.
Australian Health Priority Area
There are nine Australian Health priority areas. The national health priority areas
(NHPAs) were established in response to the WHO (World Health Organisation's) Global Health
Strategy for all from the year 2000 (Lazzarini et al., 2018). This framework focused on the health
policy and public attention on various areas that were considered to significantly contribute to
the disease burden in Australia. By the burden of a disease, it can be stated that it is a way to
measure the disease's impact on population injuries and death. The nine health priority regions of
Australia includes cancer control, cardiovascular health, prevention of injury and control, mental
health (1996), Diabetes mellitus (1997), Asthma (1999), Arthritis and musculoskeletal conditions
(2002), obesity and dementia (2008) and (2012) respectively (Kapp & Santamaria, 2015). The
national strategic framework associated with chronic conditions has been found to be associated
with the current document policy on chronic diseases in 2017. This policy has been found to
migrate to a disease-specific focus and provides guidance to the national response delivery and
health systems that respond in a more effective way. This paper will select Diabetes as a health
priority from 9 NHPAs in order to do the comparison study.
Literature analysis
According to Keel et al., (2017), the prevalence of self-reported diabetes among the
Indigenous and non-Indigenous Australian population varied to a high extent. The overall
prevalence of self-reported diabetes was reported to be very high and it was calculated to be four
times higher than among the Indigenous Australians. The rapidly increasing prevalence
5EPIDEMIOLOGY
percentage has been found to be indicated by the NHS (National Health Survey). The authors
found that the likely risk factors of diabetes were associated with an increase in age, obesity, and
growth of the population (Ashby-Mitchell et al., 2017). From the general population, it has been
observed that the Indigenous Australian population who are living in the remote regions, has
been found to have a high diabetes prevalence in the communities with a 10 fold higher value
than the general population. The prevalence associated with the age adjustments for the self-
reported diabetes cases for the Indigenous and non-Indigenous people from Australia has been
found to be 44% and 12% respectively (Simmons et al, 2019). Reasons for these values or a high
prevalence among the indigenous Australians will be discussed in detail in the following
sections.
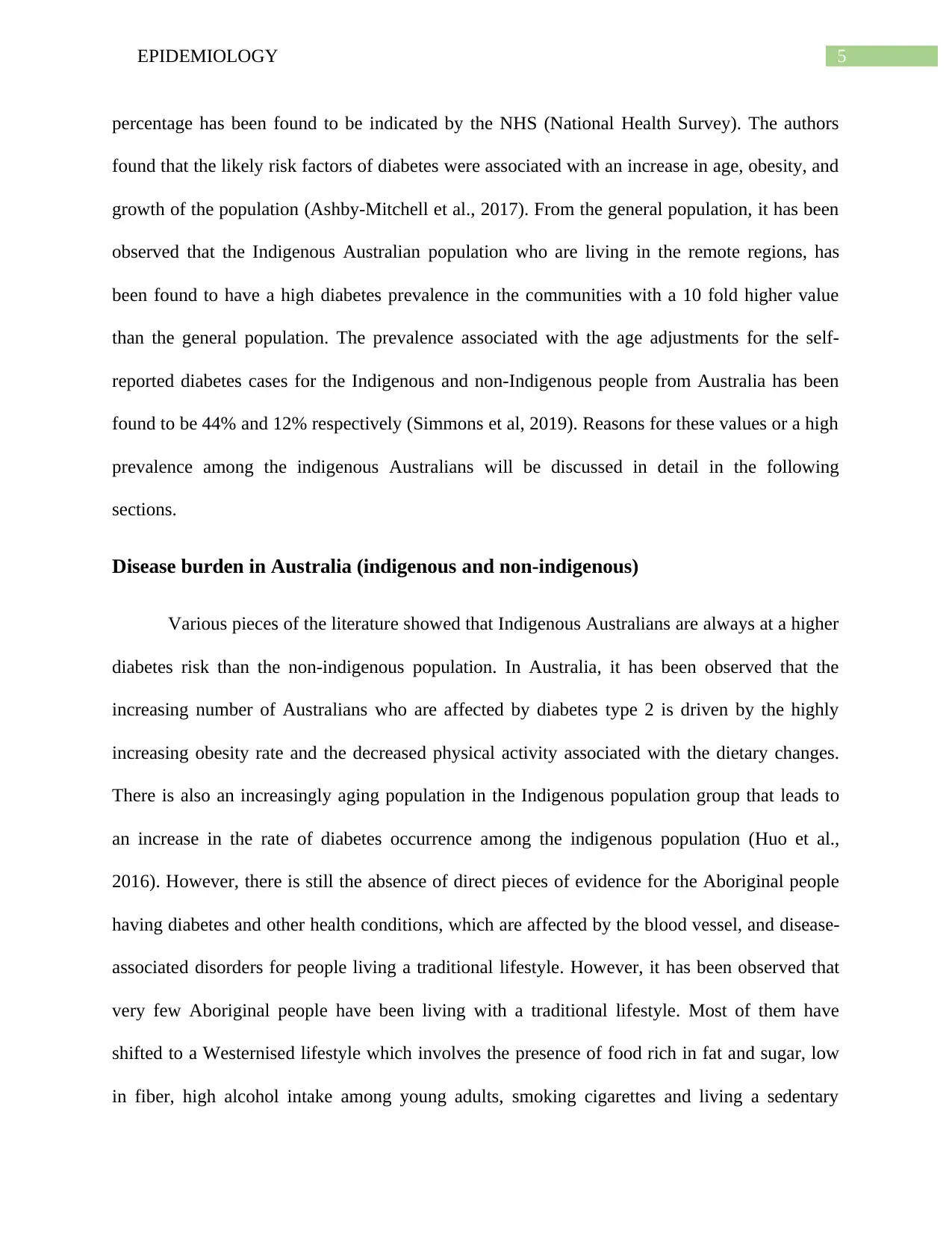
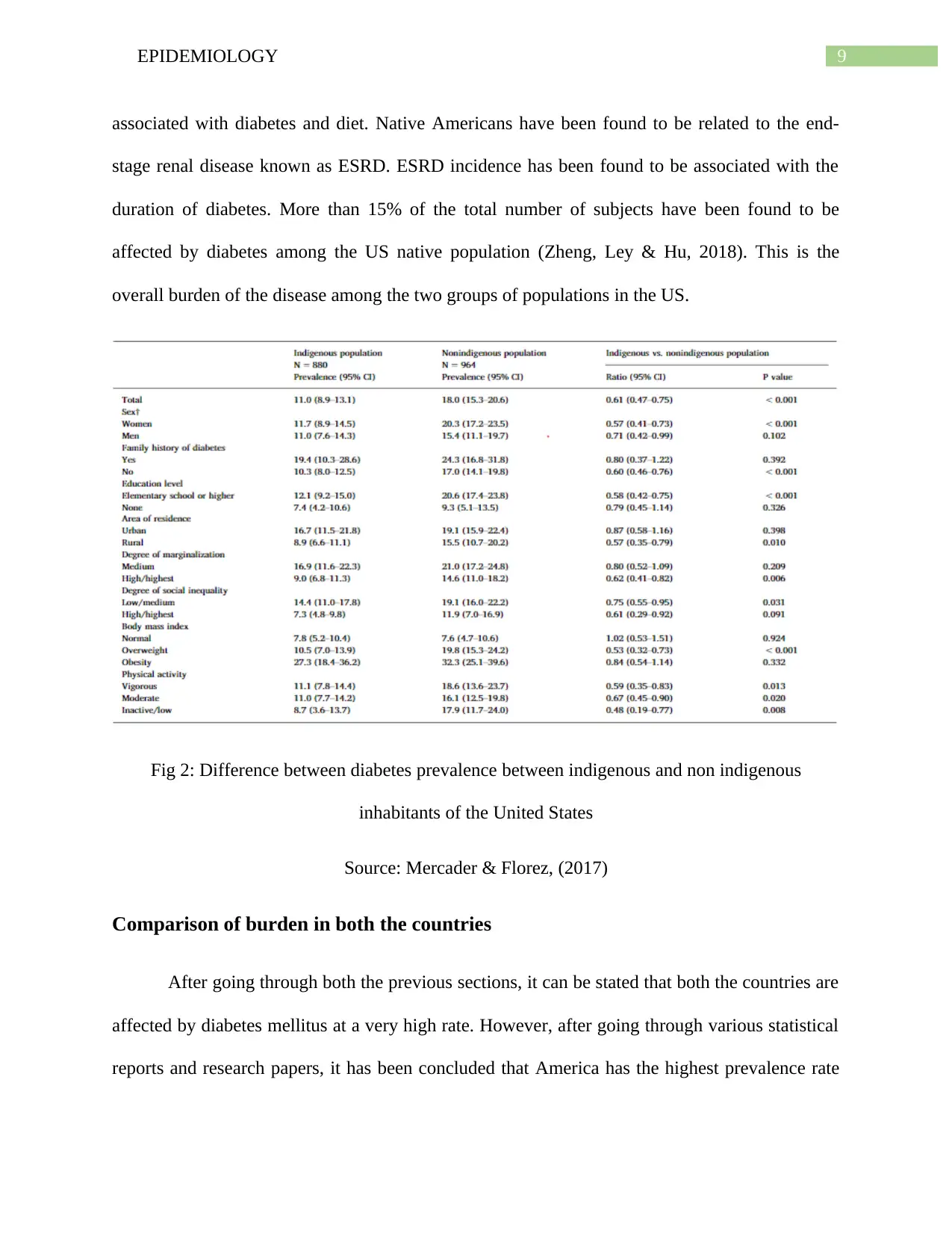
Disease burden in Australia (indigenous and non-indigenous)
Various pieces of the literature showed that Indigenous Australians are always at a higher
diabetes risk than the non-indigenous population. In Australia, it has been observed that the
increasing number of Australians who are affected by diabetes type 2 is driven by the highly
increasing obesity rate and the decreased physical activity associated with the dietary changes.
There is also an increasingly aging population in the Indigenous population group that leads to
an increase in the rate of diabetes occurrence among the indigenous population (Huo et al.,
2016). However, there is still the absence of direct pieces of evidence for the Aboriginal people
having diabetes and other health conditions, which are affected by the blood vessel, and disease-
associated disorders for people living a traditional lifestyle. However, it has been observed that
very few Aboriginal people have been living with a traditional lifestyle. Most of them have
shifted to a Westernised lifestyle which involves the presence of food rich in fat and sugar, low
in fiber, high alcohol intake among young adults, smoking cigarettes and living a sedentary
percentage has been found to be indicated by the NHS (National Health Survey). The authors
found that the likely risk factors of diabetes were associated with an increase in age, obesity, and
growth of the population (Ashby-Mitchell et al., 2017). From the general population, it has been
observed that the Indigenous Australian population who are living in the remote regions, has
been found to have a high diabetes prevalence in the communities with a 10 fold higher value
than the general population. The prevalence associated with the age adjustments for the self-
reported diabetes cases for the Indigenous and non-Indigenous people from Australia has been
found to be 44% and 12% respectively (Simmons et al, 2019). Reasons for these values or a high
prevalence among the indigenous Australians will be discussed in detail in the following
sections.
Disease burden in Australia (indigenous and non-indigenous)
Various pieces of the literature showed that Indigenous Australians are always at a higher
diabetes risk than the non-indigenous population. In Australia, it has been observed that the
increasing number of Australians who are affected by diabetes type 2 is driven by the highly
increasing obesity rate and the decreased physical activity associated with the dietary changes.
There is also an increasingly aging population in the Indigenous population group that leads to
an increase in the rate of diabetes occurrence among the indigenous population (Huo et al.,
2016). However, there is still the absence of direct pieces of evidence for the Aboriginal people
having diabetes and other health conditions, which are affected by the blood vessel, and disease-
associated disorders for people living a traditional lifestyle. However, it has been observed that
very few Aboriginal people have been living with a traditional lifestyle. Most of them have
shifted to a Westernised lifestyle which involves the presence of food rich in fat and sugar, low
in fiber, high alcohol intake among young adults, smoking cigarettes and living a sedentary
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6EPIDEMIOLOGY
lifestyle. Many research studies have shown that the Aboriginal people have lived in a
Westernised lifestyle having a high obesity rate with impaired glucose tolerance and high
triglyceride level in their blood with excessively high levels of insulin (Estevez et al., 2019).
There is a combination of genetic predisposition associated with an unhealthy lifestyle which
contributes to a higher type 2 diabetes rate among Indigenous Australians. This is the main
reason for the Indigenous Australians being highly affected by Diabetes type II Mellitus.
Fig 1: Diabetes prevalence between indigenous and non-indigenous Australians
Source: (Estevez et al., 2019)
Disease burden in the United States (indigenous and non-indigenous)
lifestyle. Many research studies have shown that the Aboriginal people have lived in a
Westernised lifestyle having a high obesity rate with impaired glucose tolerance and high
triglyceride level in their blood with excessively high levels of insulin (Estevez et al., 2019).
There is a combination of genetic predisposition associated with an unhealthy lifestyle which
contributes to a higher type 2 diabetes rate among Indigenous Australians. This is the main
reason for the Indigenous Australians being highly affected by Diabetes type II Mellitus.
Fig 1: Diabetes prevalence between indigenous and non-indigenous Australians
Source: (Estevez et al., 2019)
Disease burden in the United States (indigenous and non-indigenous)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7EPIDEMIOLOGY
Various pieces of literature have found the fact that Non-native Americans (whites) are
less affected by the prevalence of diabetes that the Native Americans. The Native American
population consists of American Indian/African American/Alaska Native adults and the non-
native group includes people belonging to the population of non-Hispanic whites. During the
1940s, diabetes mellitus has been found to be rare among the native Americans unless the middle
part of the 20th century arrived (Leung et al., 2017). However, according to the recent reports it
has been observed that diabetes mellitus has become the most common disease among the Native
Americans after World War 2. There are seven major determinants for the high prevalence of
diabetes in the indigenous population of Australia. Aboriginals have been found to have been
living since 60,000 years which has occurred before colonization. This study found that, after
colonisation, Aboriginal people have been found to experience a large number of socio-
economic disruptions which has given rise to a rapid decline in their health condition. Diet
change has been found to be one of the most significant factors affecting the high prevalence of
diabetes among the indigenous Australian population. This disease has become one of the serious
causes of morbidity among Native Americans. In the world, the highest recorded prevalence of
non-insulin-dependent diabetes mellitus has been found to be the Pima Indians. This is because
of the fact that Native Americans have been found to show the highest rates of diabetes in the
world. According to various literature pieces, it can be said that the increased frequency among
the Native Americans is due to a genetic predisposition to NIDDM associated with the
environmental factors (Stokes & Preston, 2017). Diabetes complications have been found to
account for a significant increase in morbidity and mortality among the subjects affected by
diabetes which can also be delayed or prevented by various preventive strategies. However, it
has been observed that it is still not clear how the frequency of diabetes has increased among the
Various pieces of literature have found the fact that Non-native Americans (whites) are
less affected by the prevalence of diabetes that the Native Americans. The Native American
population consists of American Indian/African American/Alaska Native adults and the non-
native group includes people belonging to the population of non-Hispanic whites. During the
1940s, diabetes mellitus has been found to be rare among the native Americans unless the middle
part of the 20th century arrived (Leung et al., 2017). However, according to the recent reports it
has been observed that diabetes mellitus has become the most common disease among the Native
Americans after World War 2. There are seven major determinants for the high prevalence of
diabetes in the indigenous population of Australia. Aboriginals have been found to have been
living since 60,000 years which has occurred before colonization. This study found that, after
colonisation, Aboriginal people have been found to experience a large number of socio-
economic disruptions which has given rise to a rapid decline in their health condition. Diet
change has been found to be one of the most significant factors affecting the high prevalence of
diabetes among the indigenous Australian population. This disease has become one of the serious
causes of morbidity among Native Americans. In the world, the highest recorded prevalence of
non-insulin-dependent diabetes mellitus has been found to be the Pima Indians. This is because
of the fact that Native Americans have been found to show the highest rates of diabetes in the
world. According to various literature pieces, it can be said that the increased frequency among
the Native Americans is due to a genetic predisposition to NIDDM associated with the
environmental factors (Stokes & Preston, 2017). Diabetes complications have been found to
account for a significant increase in morbidity and mortality among the subjects affected by
diabetes which can also be delayed or prevented by various preventive strategies. However, it
has been observed that it is still not clear how the frequency of diabetes has increased among the
8EPIDEMIOLOGY
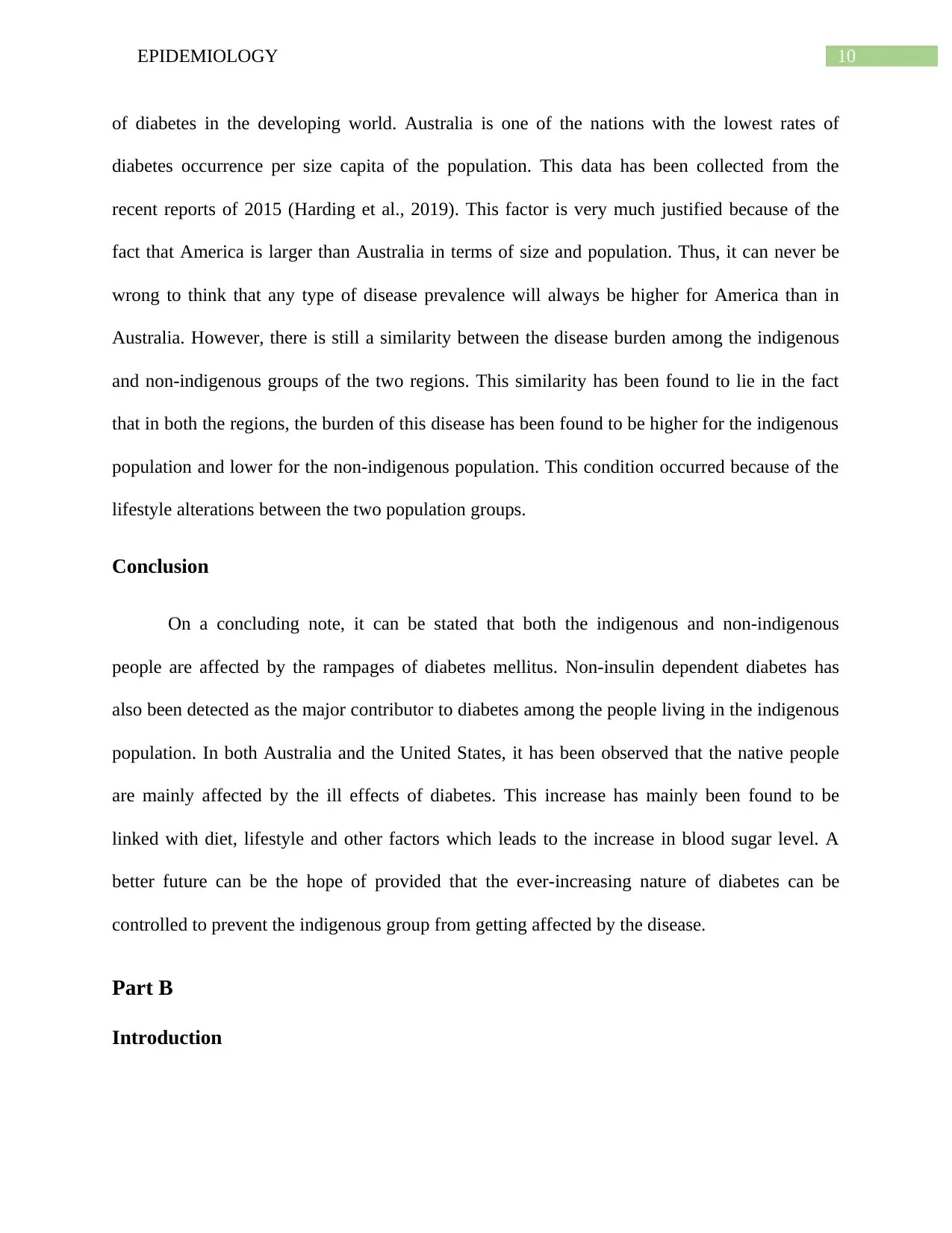
Native Americans (Gray et al., 2017). Fifty per cent of diabetes have been found to remain
undiagnosed in the Native American populations (NA). NA tribes have been found to show a
high prevalence of diabetes and have been found to be higher for women than for men. For all
the US populations, it has been stated that the overall prevalence percentage is 6.6% higher for
the NA populations (Dalal et al., 2017). Many epidemiological studies have been reviewed and it
can be concluded that NA is affected by a high prevalence of diabetes than the non-native group
of population. The Pimas have been found to have an age-sex standardized diabetes prevalence
rate 13 times higher than Caucasians (Ganesh & Sripriya, (2019). The biggest question to be
answered in this section is the reason for the high diabetes prevalence among the Native
Americans. This prevalence has been found to have increased for two main reasons. The first
reason is the improvement in survival or the increase in the developmental rate of new cases.
Since the rates of survival with diabetes have increased due to a better treatment option, the total
number of people living with diabetes accounts for most of the percentages in the prevalence rate
amount (Aminov et al., 2016). Diabetes has also been found to contribute very little to the rates
of mortality among the people who are under the age of 55 years and has been found to
contribute less to the prevalence of diabetes. According to various pieces of literature, it can be
stated that Pimas are associated with the HLA-A2 phenotype and two genetic markers on
chromosome 4q and 7q which are linked to insulin resistance. The prevalence of obesity was
found to be higher among the Native Americans in both females and males of all ages. High-
calorie diet has also been found to be linked with Native Americans which is further related to
the high prevalence of diabetes among them (Mercader & Florez, 2017). The overall fat content
of their diet has been found to dramatically increase which is the main reason for diabetes
occurrence among the Native Americans. Pimas are the biggest examples of the above statement
Native Americans (Gray et al., 2017). Fifty per cent of diabetes have been found to remain
undiagnosed in the Native American populations (NA). NA tribes have been found to show a
high prevalence of diabetes and have been found to be higher for women than for men. For all
the US populations, it has been stated that the overall prevalence percentage is 6.6% higher for
the NA populations (Dalal et al., 2017). Many epidemiological studies have been reviewed and it
can be concluded that NA is affected by a high prevalence of diabetes than the non-native group
of population. The Pimas have been found to have an age-sex standardized diabetes prevalence
rate 13 times higher than Caucasians (Ganesh & Sripriya, (2019). The biggest question to be
answered in this section is the reason for the high diabetes prevalence among the Native
Americans. This prevalence has been found to have increased for two main reasons. The first
reason is the improvement in survival or the increase in the developmental rate of new cases.
Since the rates of survival with diabetes have increased due to a better treatment option, the total
number of people living with diabetes accounts for most of the percentages in the prevalence rate
amount (Aminov et al., 2016). Diabetes has also been found to contribute very little to the rates
of mortality among the people who are under the age of 55 years and has been found to
contribute less to the prevalence of diabetes. According to various pieces of literature, it can be
stated that Pimas are associated with the HLA-A2 phenotype and two genetic markers on
chromosome 4q and 7q which are linked to insulin resistance. The prevalence of obesity was
found to be higher among the Native Americans in both females and males of all ages. High-
calorie diet has also been found to be linked with Native Americans which is further related to
the high prevalence of diabetes among them (Mercader & Florez, 2017). The overall fat content
of their diet has been found to dramatically increase which is the main reason for diabetes
occurrence among the Native Americans. Pimas are the biggest examples of the above statement
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9EPIDEMIOLOGY
associated with diabetes and diet. Native Americans have been found to be related to the end-
stage renal disease known as ESRD. ESRD incidence has been found to be associated with the
duration of diabetes. More than 15% of the total number of subjects have been found to be
affected by diabetes among the US native population (Zheng, Ley & Hu, 2018). This is the
overall burden of the disease among the two groups of populations in the US.
Fig 2: Difference between diabetes prevalence between indigenous and non indigenous
inhabitants of the United States
Source: Mercader & Florez, (2017)
Comparison of burden in both the countries
After going through both the previous sections, it can be stated that both the countries are
affected by diabetes mellitus at a very high rate. However, after going through various statistical
reports and research papers, it has been concluded that America has the highest prevalence rate
associated with diabetes and diet. Native Americans have been found to be related to the end-
stage renal disease known as ESRD. ESRD incidence has been found to be associated with the
duration of diabetes. More than 15% of the total number of subjects have been found to be
affected by diabetes among the US native population (Zheng, Ley & Hu, 2018). This is the
overall burden of the disease among the two groups of populations in the US.
Fig 2: Difference between diabetes prevalence between indigenous and non indigenous
inhabitants of the United States
Source: Mercader & Florez, (2017)
Comparison of burden in both the countries
After going through both the previous sections, it can be stated that both the countries are
affected by diabetes mellitus at a very high rate. However, after going through various statistical
reports and research papers, it has been concluded that America has the highest prevalence rate
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10EPIDEMIOLOGY
of diabetes in the developing world. Australia is one of the nations with the lowest rates of
diabetes occurrence per size capita of the population. This data has been collected from the
recent reports of 2015 (Harding et al., 2019). This factor is very much justified because of the
fact that America is larger than Australia in terms of size and population. Thus, it can never be
wrong to think that any type of disease prevalence will always be higher for America than in
Australia. However, there is still a similarity between the disease burden among the indigenous
and non-indigenous groups of the two regions. This similarity has been found to lie in the fact
that in both the regions, the burden of this disease has been found to be higher for the indigenous
population and lower for the non-indigenous population. This condition occurred because of the
lifestyle alterations between the two population groups.
Conclusion
On a concluding note, it can be stated that both the indigenous and non-indigenous
people are affected by the rampages of diabetes mellitus. Non-insulin dependent diabetes has
also been detected as the major contributor to diabetes among the people living in the indigenous
population. In both Australia and the United States, it has been observed that the native people
are mainly affected by the ill effects of diabetes. This increase has mainly been found to be
linked with diet, lifestyle and other factors which leads to the increase in blood sugar level. A
better future can be the hope of provided that the ever-increasing nature of diabetes can be
controlled to prevent the indigenous group from getting affected by the disease.
Part B
Introduction
of diabetes in the developing world. Australia is one of the nations with the lowest rates of
diabetes occurrence per size capita of the population. This data has been collected from the
recent reports of 2015 (Harding et al., 2019). This factor is very much justified because of the
fact that America is larger than Australia in terms of size and population. Thus, it can never be
wrong to think that any type of disease prevalence will always be higher for America than in
Australia. However, there is still a similarity between the disease burden among the indigenous
and non-indigenous groups of the two regions. This similarity has been found to lie in the fact
that in both the regions, the burden of this disease has been found to be higher for the indigenous
population and lower for the non-indigenous population. This condition occurred because of the
lifestyle alterations between the two population groups.
Conclusion
On a concluding note, it can be stated that both the indigenous and non-indigenous
people are affected by the rampages of diabetes mellitus. Non-insulin dependent diabetes has
also been detected as the major contributor to diabetes among the people living in the indigenous
population. In both Australia and the United States, it has been observed that the native people
are mainly affected by the ill effects of diabetes. This increase has mainly been found to be
linked with diet, lifestyle and other factors which leads to the increase in blood sugar level. A
better future can be the hope of provided that the ever-increasing nature of diabetes can be
controlled to prevent the indigenous group from getting affected by the disease.
Part B
Introduction
11EPIDEMIOLOGY
Aboriginal and Torres Strait Islanders have been found to be affected by non-insulin
dependent diabetes in Australia. This local population has been selected within Australia for the
discussion of common determinants of diabetes in this section. There are seven major
determinants for the high prevalence of diabetes in the indigenous population of Australia.
Aboriginals have been found to have been living since 60,000 years which has occurred before
colonization (Price & Rogers, 2019). After colonization, Aboriginal people have been found to
experience a large number of socio-economic disruptions which has given rise to a rapid decline
in their health condition (Taylor et al., 2017). These people have been found to migrate to
different lands because of the force from the white Europeans society. During this time, the
introduction of refined foods and sugar in the diet of Aboriginal Australians increased to a high
level. Their former diet consisted of land animals, shellfish and fishes including plant food and
birds (Lee & Ride, 2018). Thus, it can be stated that Aboriginal people have become highly
vulnerable to diabetes, which has become one of the most significant causes of high mortality
and high morbidity among the community. The next section will discuss the area of the highest
prevalence of the disease and the determinants responsible for the high prevalence.
Area of the highest prevalence
In the Aboriginal community, it has been found that the prevalence of diabetes has been
highest. This is because of a large number of social determinants which are named European
influence, Remoteness, Unutilised resources, Health inequalities, Low birth weights, Pregnancy,
and Lifestyle. The overall prevalence of type 2 diabetes and obesity has been found to be
associated with European influences at the colonization time. According to various pieces of
literature, it can be stated that sugar and refined foods replaced the normal diet of Aboriginal
people when they were detached from their own habitats (Gwynn et al., 2019). As a result, it has
Aboriginal and Torres Strait Islanders have been found to be affected by non-insulin
dependent diabetes in Australia. This local population has been selected within Australia for the
discussion of common determinants of diabetes in this section. There are seven major
determinants for the high prevalence of diabetes in the indigenous population of Australia.
Aboriginals have been found to have been living since 60,000 years which has occurred before
colonization (Price & Rogers, 2019). After colonization, Aboriginal people have been found to
experience a large number of socio-economic disruptions which has given rise to a rapid decline
in their health condition (Taylor et al., 2017). These people have been found to migrate to
different lands because of the force from the white Europeans society. During this time, the
introduction of refined foods and sugar in the diet of Aboriginal Australians increased to a high
level. Their former diet consisted of land animals, shellfish and fishes including plant food and
birds (Lee & Ride, 2018). Thus, it can be stated that Aboriginal people have become highly
vulnerable to diabetes, which has become one of the most significant causes of high mortality
and high morbidity among the community. The next section will discuss the area of the highest
prevalence of the disease and the determinants responsible for the high prevalence.
Area of the highest prevalence
In the Aboriginal community, it has been found that the prevalence of diabetes has been
highest. This is because of a large number of social determinants which are named European
influence, Remoteness, Unutilised resources, Health inequalities, Low birth weights, Pregnancy,
and Lifestyle. The overall prevalence of type 2 diabetes and obesity has been found to be
associated with European influences at the colonization time. According to various pieces of
literature, it can be stated that sugar and refined foods replaced the normal diet of Aboriginal
people when they were detached from their own habitats (Gwynn et al., 2019). As a result, it has
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 22
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





