Nursing & Aboriginal Clients: Cultural Competence in Palliative Care
VerifiedAdded on 2023/06/12
|14
|3164
|174
Report
AI Summary
This report examines the crucial role of cultural competence for nurses providing palliative and end-of-life care to Aboriginal clients. It discusses the impact of colonization and residential schools on the health and communication needs of Aboriginal communities, highlighting the importance of integrating traditional practices into medical care. The report defines cultural competence, emphasizing the need for nurses to respect cultural differences, avoid personal biases, and engage in effective communication with patients and their families. It also addresses cultural barriers such as language differences, stereotyping, and lack of cultural safety, and suggests solutions like strengthening cultural competency training for healthcare professionals and fostering collaboration between healthcare providers and Aboriginal communities. A questionnaire provides insights into the experiences and perceptions of Aboriginal individuals regarding healthcare access and cultural sensitivity. Ultimately, the report underscores the significance of cultural competence in improving healthcare outcomes and ensuring equitable access to care for Aboriginal clients.

Running Head: PROFFESIONAL COMMUNICATION 1
The Role Cultural Competencies Play for a Nurse Caring For Aboriginal Clients
Name
Institutional Affiliation
The Role Cultural Competencies Play for a Nurse Caring For Aboriginal Clients
Name
Institutional Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PROFESSIONAL COMMUNICATION 2
Introduction
Question 1
According to WHO, Palliative care refers to the improved care and management of the
quality of life patients approaching end of life, and also providing psychological support to the
families throughout the course of illness into bereavement (Land, et al 2016). Nurses are
increasingly becoming involved in the palliative care and are source of significant information
and much needed support for families and patients at the end of life. Health professionals
responsible for patients with terminal illness should develop skills that enable effective
communication with patients, and their respective families.
Different communities of Aboriginal people have different and unique languages, beliefs,
healing cultural practices(Mobula et al. 2015). It is noted that all patients are distinctively unique
and cultural differences do arise while providing terminally ill aboriginal patients palliative care.
Some of these patients value individual respect and involvement of family and their community
during important decision making processes. The Aboriginal cultures usually have distinct
approaches to revealing bad information to the patients, and also a way of encouraging the
family members.
Culture refers to the lifestyles, learned and commonly shared beliefs and values, learned
knowledge, customized symbols, rules and regulations that guide behavior and create shared
meanings within a given group of people (Driscoll, 2017). Vast cultural differences exist
between the aboriginal patients and healthcare givers. Different presumptions and expectations
on how communications should occur, who can participate, and the measures to be taken during
decision making processes are some of the differences that are more apparent.
Introduction
Question 1
According to WHO, Palliative care refers to the improved care and management of the
quality of life patients approaching end of life, and also providing psychological support to the
families throughout the course of illness into bereavement (Land, et al 2016). Nurses are
increasingly becoming involved in the palliative care and are source of significant information
and much needed support for families and patients at the end of life. Health professionals
responsible for patients with terminal illness should develop skills that enable effective
communication with patients, and their respective families.
Different communities of Aboriginal people have different and unique languages, beliefs,
healing cultural practices(Mobula et al. 2015). It is noted that all patients are distinctively unique
and cultural differences do arise while providing terminally ill aboriginal patients palliative care.
Some of these patients value individual respect and involvement of family and their community
during important decision making processes. The Aboriginal cultures usually have distinct
approaches to revealing bad information to the patients, and also a way of encouraging the
family members.
Culture refers to the lifestyles, learned and commonly shared beliefs and values, learned
knowledge, customized symbols, rules and regulations that guide behavior and create shared
meanings within a given group of people (Driscoll, 2017). Vast cultural differences exist
between the aboriginal patients and healthcare givers. Different presumptions and expectations
on how communications should occur, who can participate, and the measures to be taken during
decision making processes are some of the differences that are more apparent.
PROFESSIONAL COMMUNICATION 3
Some aboriginal patient values indirect communication, speechlessness, and sharing of critical
information and decision making with the family members.According to Alesi et al, (2011),
terminally ill patients and their family members face difficult challenges when medical
caregivers come from different cultural background as the patient. Difficulty on communication
and decision making becomes a big challenge.
Question 2
The policy instrument of the residential system during the colonization process
contributed to the poor state of the health sector in the aboriginal communities. Before
colonization, the indigenous population was organized into groups of hunting and gathering
communities with less inactivity and diseases were uncommon. Colonization process and
establishments of residential schools lead to mistrust and trauma in medical practices among the
indigenous people. The health of the aboriginals declined after contact with colonizers where
there was an increase on the transmission of new diseases, loss of traditional lifestyle, change to
a less nutritious diet, and depletion of natural food resource due to overhunting, fishing and also
confinement of the reserve system and development of the residential schools (Pilcher, Charles&
Lancaster, 2008). There is need to integrate the aboriginals way of life into the medical practices
to make it safe for the aboriginal people to access medical care. It will enhance the
communication and acceptance of the medical services among the aboriginal people.
Question 3
Catalanotto et al. (2017) describe cultural competence as the process of accepting and
respecting differences and not letting one’s personal beliefs have an undue influence on those
with a different beliefs, values, and lifestyles as of one’s own. To the health care givers such as
nurses, cultural competency involves having general cultural-specific information about other
Some aboriginal patient values indirect communication, speechlessness, and sharing of critical
information and decision making with the family members.According to Alesi et al, (2011),
terminally ill patients and their family members face difficult challenges when medical
caregivers come from different cultural background as the patient. Difficulty on communication
and decision making becomes a big challenge.
Question 2
The policy instrument of the residential system during the colonization process
contributed to the poor state of the health sector in the aboriginal communities. Before
colonization, the indigenous population was organized into groups of hunting and gathering
communities with less inactivity and diseases were uncommon. Colonization process and
establishments of residential schools lead to mistrust and trauma in medical practices among the
indigenous people. The health of the aboriginals declined after contact with colonizers where
there was an increase on the transmission of new diseases, loss of traditional lifestyle, change to
a less nutritious diet, and depletion of natural food resource due to overhunting, fishing and also
confinement of the reserve system and development of the residential schools (Pilcher, Charles&
Lancaster, 2008). There is need to integrate the aboriginals way of life into the medical practices
to make it safe for the aboriginal people to access medical care. It will enhance the
communication and acceptance of the medical services among the aboriginal people.
Question 3
Catalanotto et al. (2017) describe cultural competence as the process of accepting and
respecting differences and not letting one’s personal beliefs have an undue influence on those
with a different beliefs, values, and lifestyles as of one’s own. To the health care givers such as
nurses, cultural competency involves having general cultural-specific information about other
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

PROFESSIONAL COMMUNICATION 4
cultures and knowing what kind of questions to ask to avoid discomfort by the aboriginal
patients. For nurses caring for aboriginal patients, achieving cultural competency is essential in
helping handling different types of cultural barriers they might face. Cultural competency means
learning, assessing, sharing, communicating and demonstrate skills within and outside one’s
culture is a key strength (Pilcher, Charles& Lancaster, 2008). Through cultural awareness and
sensitivity, nurses began to learn differences incultures leading to cultural safety which predicts
the understanding of the power differentials deep-rooted in health services delivery and
redressing the inequalities through the process of education.
Failure to understand and appreciate the different cultural practices of Aboriginal people
leads to inappropriate and poor health care service. Communication between the nurses and the
aboriginals would improve if the nurses/caregivers are keenlistening to aboriginals and the
healthcare givers let the communication shape their perceptions. Both the nurses and aboriginals
needs to recognize that their cultural understandings come from their own individual
backgrounds and therefore are saturated in their own beliefs and values development.
Collaboration also plays a crucial role in building the cultural competency between the
aboriginal and the nurses during the palliative and end of life care services received and
delivered during terminal illnesses. Collaboration is not only expected from the aboriginals and
nurses, but also from their families, health workers, interpreters and other staff members. It is
vital in building up the trust between the parties involved. It is vital in planning and
implementing strategies for change to produce optimum outcomes.
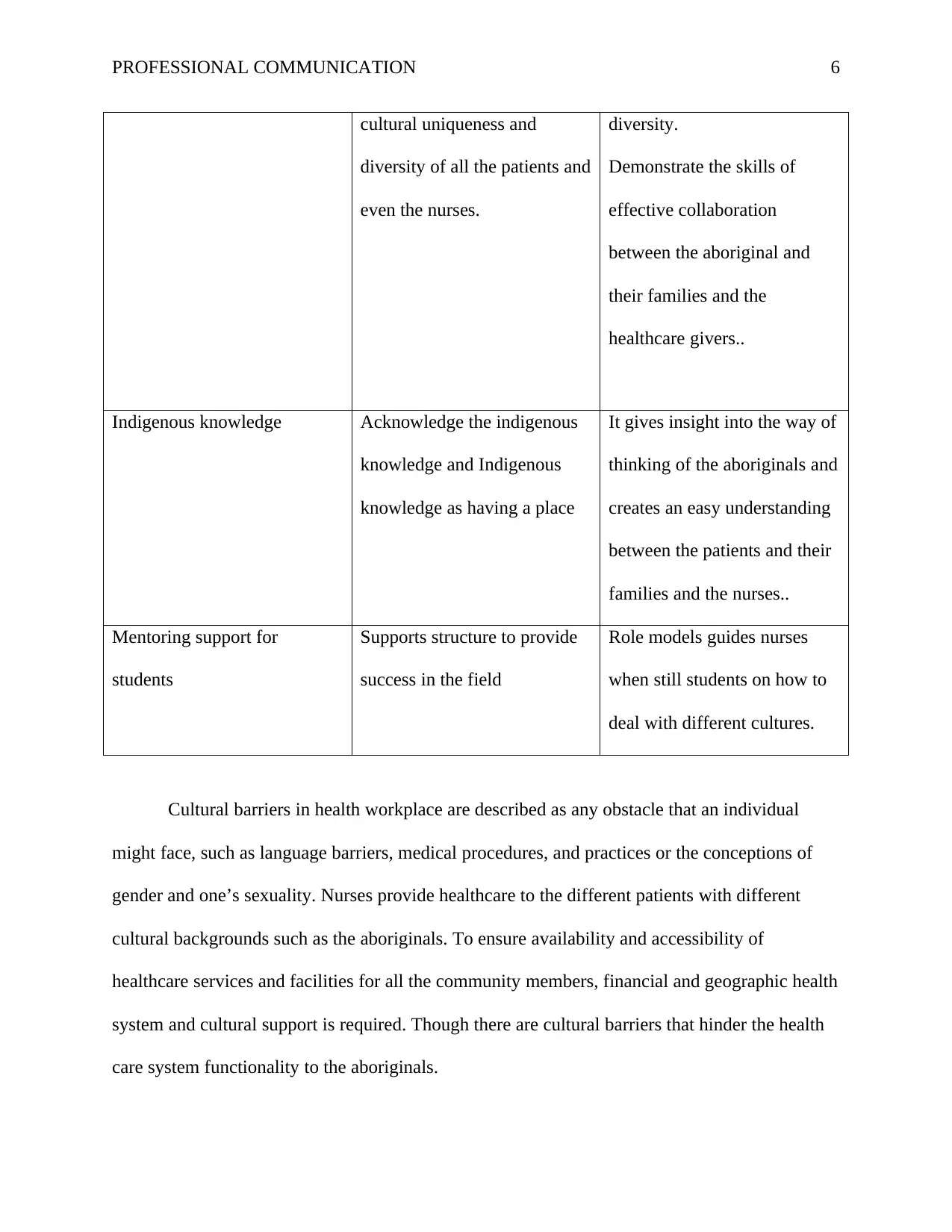
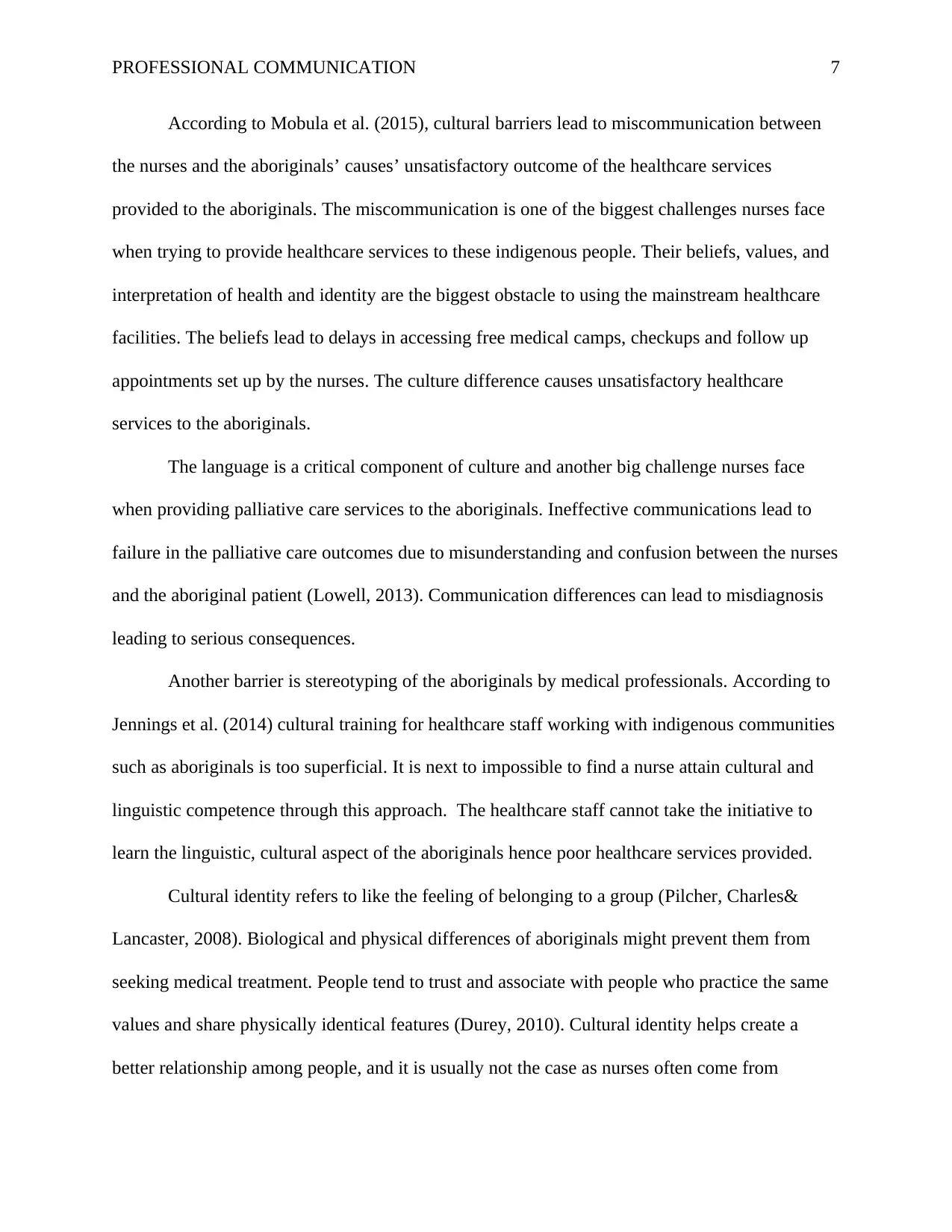
Table 1: The core competencies of culture in the biomedical field
Core Competency Key Concepts Role of the competency
cultures and knowing what kind of questions to ask to avoid discomfort by the aboriginal
patients. For nurses caring for aboriginal patients, achieving cultural competency is essential in
helping handling different types of cultural barriers they might face. Cultural competency means
learning, assessing, sharing, communicating and demonstrate skills within and outside one’s
culture is a key strength (Pilcher, Charles& Lancaster, 2008). Through cultural awareness and
sensitivity, nurses began to learn differences incultures leading to cultural safety which predicts
the understanding of the power differentials deep-rooted in health services delivery and
redressing the inequalities through the process of education.
Failure to understand and appreciate the different cultural practices of Aboriginal people
leads to inappropriate and poor health care service. Communication between the nurses and the
aboriginals would improve if the nurses/caregivers are keenlistening to aboriginals and the
healthcare givers let the communication shape their perceptions. Both the nurses and aboriginals
needs to recognize that their cultural understandings come from their own individual
backgrounds and therefore are saturated in their own beliefs and values development.
Collaboration also plays a crucial role in building the cultural competency between the
aboriginal and the nurses during the palliative and end of life care services received and
delivered during terminal illnesses. Collaboration is not only expected from the aboriginals and
nurses, but also from their families, health workers, interpreters and other staff members. It is
vital in building up the trust between the parties involved. It is vital in planning and
implementing strategies for change to produce optimum outcomes.
Table 1: The core competencies of culture in the biomedical field
Core Competency Key Concepts Role of the competency
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

PROFESSIONAL COMMUNICATION 5
Postcolonial understanding The effect of colonization on
Aboriginal people
The nurses can provide
culturally safe care, build
relationships and give care to
aboriginals in a compassionate
manner.
Also, identify the determinants
of health of aboriginals and
use the information to promote
health among the aboriginals..
Communication Effective and culturally safe
communication among in
nurses and improved
interactions with Aboriginal
people.
Establish an effective and
culturally safe communication
with the aboriginal patients
and the families.
Inclusivity To increase awareness and
sensitivity among the involved
parties.
Engage in dialogues and build
a relationship with the
aboriginals. It creates culture
awareness and sensitivity
between the health practices
and the aboriginals.
Respect Respect for aboriginals
cultural integrity. Consider the
Identify and put in place
measures that uphold cultural
Postcolonial understanding The effect of colonization on
Aboriginal people
The nurses can provide
culturally safe care, build
relationships and give care to
aboriginals in a compassionate
manner.
Also, identify the determinants
of health of aboriginals and
use the information to promote
health among the aboriginals..
Communication Effective and culturally safe
communication among in
nurses and improved
interactions with Aboriginal
people.
Establish an effective and
culturally safe communication
with the aboriginal patients
and the families.
Inclusivity To increase awareness and
sensitivity among the involved
parties.
Engage in dialogues and build
a relationship with the
aboriginals. It creates culture
awareness and sensitivity
between the health practices
and the aboriginals.
Respect Respect for aboriginals
cultural integrity. Consider the
Identify and put in place
measures that uphold cultural
PROFESSIONAL COMMUNICATION 6
cultural uniqueness and
diversity of all the patients and
even the nurses.
diversity.
Demonstrate the skills of
effective collaboration
between the aboriginal and
their families and the
healthcare givers..
Indigenous knowledge Acknowledge the indigenous
knowledge and Indigenous
knowledge as having a place
It gives insight into the way of
thinking of the aboriginals and
creates an easy understanding
between the patients and their
families and the nurses..
Mentoring support for
students
Supports structure to provide
success in the field
Role models guides nurses
when still students on how to
deal with different cultures.
Cultural barriers in health workplace are described as any obstacle that an individual
might face, such as language barriers, medical procedures, and practices or the conceptions of
gender and one’s sexuality. Nurses provide healthcare to the different patients with different
cultural backgrounds such as the aboriginals. To ensure availability and accessibility of
healthcare services and facilities for all the community members, financial and geographic health
system and cultural support is required. Though there are cultural barriers that hinder the health
care system functionality to the aboriginals.
cultural uniqueness and
diversity of all the patients and
even the nurses.
diversity.
Demonstrate the skills of
effective collaboration
between the aboriginal and
their families and the
healthcare givers..
Indigenous knowledge Acknowledge the indigenous
knowledge and Indigenous
knowledge as having a place
It gives insight into the way of
thinking of the aboriginals and
creates an easy understanding
between the patients and their
families and the nurses..
Mentoring support for
students
Supports structure to provide
success in the field
Role models guides nurses
when still students on how to
deal with different cultures.
Cultural barriers in health workplace are described as any obstacle that an individual
might face, such as language barriers, medical procedures, and practices or the conceptions of
gender and one’s sexuality. Nurses provide healthcare to the different patients with different
cultural backgrounds such as the aboriginals. To ensure availability and accessibility of
healthcare services and facilities for all the community members, financial and geographic health
system and cultural support is required. Though there are cultural barriers that hinder the health
care system functionality to the aboriginals.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
PROFESSIONAL COMMUNICATION 7
According to Mobula et al. (2015), cultural barriers lead to miscommunication between
the nurses and the aboriginals’ causes’ unsatisfactory outcome of the healthcare services
provided to the aboriginals. The miscommunication is one of the biggest challenges nurses face
when trying to provide healthcare services to these indigenous people. Their beliefs, values, and
interpretation of health and identity are the biggest obstacle to using the mainstream healthcare
facilities. The beliefs lead to delays in accessing free medical camps, checkups and follow up
appointments set up by the nurses. The culture difference causes unsatisfactory healthcare
services to the aboriginals.
The language is a critical component of culture and another big challenge nurses face
when providing palliative care services to the aboriginals. Ineffective communications lead to
failure in the palliative care outcomes due to misunderstanding and confusion between the nurses
and the aboriginal patient (Lowell, 2013). Communication differences can lead to misdiagnosis
leading to serious consequences.
Another barrier is stereotyping of the aboriginals by medical professionals. According to
Jennings et al. (2014) cultural training for healthcare staff working with indigenous communities
such as aboriginals is too superficial. It is next to impossible to find a nurse attain cultural and
linguistic competence through this approach. The healthcare staff cannot take the initiative to
learn the linguistic, cultural aspect of the aboriginals hence poor healthcare services provided.
Cultural identity refers to like the feeling of belonging to a group (Pilcher, Charles&
Lancaster, 2008). Biological and physical differences of aboriginals might prevent them from
seeking medical treatment. People tend to trust and associate with people who practice the same
values and share physically identical features (Durey, 2010). Cultural identity helps create a
better relationship among people, and it is usually not the case as nurses often come from
According to Mobula et al. (2015), cultural barriers lead to miscommunication between
the nurses and the aboriginals’ causes’ unsatisfactory outcome of the healthcare services
provided to the aboriginals. The miscommunication is one of the biggest challenges nurses face
when trying to provide healthcare services to these indigenous people. Their beliefs, values, and
interpretation of health and identity are the biggest obstacle to using the mainstream healthcare
facilities. The beliefs lead to delays in accessing free medical camps, checkups and follow up
appointments set up by the nurses. The culture difference causes unsatisfactory healthcare
services to the aboriginals.
The language is a critical component of culture and another big challenge nurses face
when providing palliative care services to the aboriginals. Ineffective communications lead to
failure in the palliative care outcomes due to misunderstanding and confusion between the nurses
and the aboriginal patient (Lowell, 2013). Communication differences can lead to misdiagnosis
leading to serious consequences.
Another barrier is stereotyping of the aboriginals by medical professionals. According to
Jennings et al. (2014) cultural training for healthcare staff working with indigenous communities
such as aboriginals is too superficial. It is next to impossible to find a nurse attain cultural and
linguistic competence through this approach. The healthcare staff cannot take the initiative to
learn the linguistic, cultural aspect of the aboriginals hence poor healthcare services provided.
Cultural identity refers to like the feeling of belonging to a group (Pilcher, Charles&
Lancaster, 2008). Biological and physical differences of aboriginals might prevent them from
seeking medical treatment. People tend to trust and associate with people who practice the same
values and share physically identical features (Durey, 2010). Cultural identity helps create a
better relationship among people, and it is usually not the case as nurses often come from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

PROFESSIONAL COMMUNICATION 8
different cultural backgrounds. Cultural identity prevents indigenous people from seeking health
services due to lack of cultural safety. Hence, terminally ill patients do not seek medical
attention.
Question 4
Strengthening cultural competency of healthcare professional can be an effective solution
to the communicative challenges and reduce disparities in the healthcare system. According to
Mobula et al. (2015), nurses who are culturally aware and competent can reduce the
communication barriers. Including the cultural competency in the service delivery and
understanding other cultures beliefs and practices of other communities and inclusion in the
medical school, practices can also be another solution.
Also, research institutions and healthcare provider’s organizations can work together and
come up with innovative ideas to reduce the cultural barriers in the healthcare systems. Wylie et
al., 2013 suggests that it is recommended for institutions to adopt cultural competency
measurement tools to provide self-assessments for healthcare staffs
For future practices, strategies and policies need to be put in place to improve access and
incorporate cultural protocols that would address the healthcare issues for the indigenous
families. Institutions should provide the basis for the achievement of the set strategies.
Aboriginals’ challenges in the healthcare system are the key to ensure cultural respect and equal
healthcare access in the future.
different cultural backgrounds. Cultural identity prevents indigenous people from seeking health
services due to lack of cultural safety. Hence, terminally ill patients do not seek medical
attention.
Question 4
Strengthening cultural competency of healthcare professional can be an effective solution
to the communicative challenges and reduce disparities in the healthcare system. According to
Mobula et al. (2015), nurses who are culturally aware and competent can reduce the
communication barriers. Including the cultural competency in the service delivery and
understanding other cultures beliefs and practices of other communities and inclusion in the
medical school, practices can also be another solution.
Also, research institutions and healthcare provider’s organizations can work together and
come up with innovative ideas to reduce the cultural barriers in the healthcare systems. Wylie et
al., 2013 suggests that it is recommended for institutions to adopt cultural competency
measurement tools to provide self-assessments for healthcare staffs
For future practices, strategies and policies need to be put in place to improve access and
incorporate cultural protocols that would address the healthcare issues for the indigenous
families. Institutions should provide the basis for the achievement of the set strategies.
Aboriginals’ challenges in the healthcare system are the key to ensure cultural respect and equal
healthcare access in the future.
PROFESSIONAL COMMUNICATION 9
Questionnaire to the Aboriginal
1. Do you identify as:
Do you consider yourself an aboriginal or non-aboriginal?
I identify as an Aboriginal.
2. What city do you live in?
Currently, residing in Katherine
3. What’s your gender?
Female
4. What’s your age group?
Between 40-50
5. When accessing health care services, do you identify as an Aboriginal or not?
No, initially I would identify as an aboriginal but the discrimination from the nurses was too
much, and I stopped Identifying myself as an aboriginal to receive good services and treated
with no discrimination.
6. Share your reasons for identifying or not identifying as aboriginal when seeking
healthcare services?
I identify with the aboriginal due to the cultural aspects involved.
7. Do you think aboriginals have access to palliative care services?
Some do, while a good percentage of aboriginals do not have access to health facilities.
8. Who do you go for if you need support with someone who is dying or terminally ill?
The family and community play an important role when someone is terminally ill. There is
support from the community. Decisions are usually made in a group, and the community is
Questionnaire to the Aboriginal
1. Do you identify as:
Do you consider yourself an aboriginal or non-aboriginal?
I identify as an Aboriginal.
2. What city do you live in?
Currently, residing in Katherine
3. What’s your gender?
Female
4. What’s your age group?
Between 40-50
5. When accessing health care services, do you identify as an Aboriginal or not?
No, initially I would identify as an aboriginal but the discrimination from the nurses was too
much, and I stopped Identifying myself as an aboriginal to receive good services and treated
with no discrimination.
6. Share your reasons for identifying or not identifying as aboriginal when seeking
healthcare services?
I identify with the aboriginal due to the cultural aspects involved.
7. Do you think aboriginals have access to palliative care services?
Some do, while a good percentage of aboriginals do not have access to health facilities.
8. Who do you go for if you need support with someone who is dying or terminally ill?
The family and community play an important role when someone is terminally ill. There is
support from the community. Decisions are usually made in a group, and the community is
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
PROFESSIONAL COMMUNICATION 10
usually alerted when someone is dying. They prefer to be with the family members before
during terminal illnesses.
9. Who provides end of life care services to members of your community?
There are health care providers proving health care services. Though it is hard for the
community members to accept the western/modern way of health practices, the cultural
belief and values make it difficult for members of my community to attend the health
facilities. Family members sometimes take care of the terminally ill and sometimes they are
taken to the healthcare facility. Previous experiences from the medical field also make it very
difficult for them as they had poor services causing fear of hospitalization for our community
people.
10. How was your experience in seeking health care services? Were the providers
respectful of your community beliefs?
The healthcare facility I visited was not so welcoming, they did not want to attend to me at
the beginning, and I had to go and come back a few times for me to access the medical
treatment I required. There was lack of empathy from their side and they claimed I was not ill
yet I knew I had anxiety problems. I was attended to when the illness had advanced. They
stereotyped a lot and assumed we do not understand the medical services.
The experience was ok, though there were difficulty in communication and stereotyping from
the healthcare providers. There was also difficulty in developing positive relationship with
the healthcare service provider.
11. What do you think could be improved in the palliative care services?
The healthcare service providers taking care our people need to be aware and how important
the culture is to our people. They need to be understood and respect the aboriginal culture in
usually alerted when someone is dying. They prefer to be with the family members before
during terminal illnesses.
9. Who provides end of life care services to members of your community?
There are health care providers proving health care services. Though it is hard for the
community members to accept the western/modern way of health practices, the cultural
belief and values make it difficult for members of my community to attend the health
facilities. Family members sometimes take care of the terminally ill and sometimes they are
taken to the healthcare facility. Previous experiences from the medical field also make it very
difficult for them as they had poor services causing fear of hospitalization for our community
people.
10. How was your experience in seeking health care services? Were the providers
respectful of your community beliefs?
The healthcare facility I visited was not so welcoming, they did not want to attend to me at
the beginning, and I had to go and come back a few times for me to access the medical
treatment I required. There was lack of empathy from their side and they claimed I was not ill
yet I knew I had anxiety problems. I was attended to when the illness had advanced. They
stereotyped a lot and assumed we do not understand the medical services.
The experience was ok, though there were difficulty in communication and stereotyping from
the healthcare providers. There was also difficulty in developing positive relationship with
the healthcare service provider.
11. What do you think could be improved in the palliative care services?
The healthcare service providers taking care our people need to be aware and how important
the culture is to our people. They need to be understood and respect the aboriginal culture in
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PROFESSIONAL COMMUNICATION 11
order to build trust and good rapport with patients. Stereotyping and racism are some of the
issues they need to work on as they instill fear in patients hence not seeking help when ill.
The rooms where patients are should be able to accommodate large number of people. Also,
construction of roads in rural areas would provide access to the medical facilities as some of
the aboriginals do not seek medical support due to lack of transportation.
12. What do you think is important to the palliative life care for the aboriginal
people?
The aboriginals value their families and having centered family care in the health care’s
facilities would empower patients and families to seek medical service. The support from
health care providers and sense of acceptance would enable the terminally ill to develop trust
in the medical facility.
13. What are your thoughts about the role of Traditional Aboriginal Medicine at the end
of life care for Aboriginal people living in your town?
Some people still believe in the traditional medicine provides spiritual support to the
members of our community, and they are still used. They provide a sense of hope to the ill.
14. What do you recommend can be improved in the provision of healthcare services to
improve the experience of users?
The healthcare service providers need to be more culturally aware of the aboriginal needs and
culturally safe. The mistrust and fear of accessing the medical facilities are due to the
stereotyping and lack of appreciation for their cultures.
order to build trust and good rapport with patients. Stereotyping and racism are some of the
issues they need to work on as they instill fear in patients hence not seeking help when ill.
The rooms where patients are should be able to accommodate large number of people. Also,
construction of roads in rural areas would provide access to the medical facilities as some of
the aboriginals do not seek medical support due to lack of transportation.
12. What do you think is important to the palliative life care for the aboriginal
people?
The aboriginals value their families and having centered family care in the health care’s
facilities would empower patients and families to seek medical service. The support from
health care providers and sense of acceptance would enable the terminally ill to develop trust
in the medical facility.
13. What are your thoughts about the role of Traditional Aboriginal Medicine at the end
of life care for Aboriginal people living in your town?
Some people still believe in the traditional medicine provides spiritual support to the
members of our community, and they are still used. They provide a sense of hope to the ill.
14. What do you recommend can be improved in the provision of healthcare services to
improve the experience of users?
The healthcare service providers need to be more culturally aware of the aboriginal needs and
culturally safe. The mistrust and fear of accessing the medical facilities are due to the
stereotyping and lack of appreciation for their cultures.

PROFESSIONAL COMMUNICATION 12
Conclusion
Health equity is the core value and a basic human right for all human beings. Strategies
and interventions should be put in place to protect and assist the indigenous groups such as the
aboriginals. Cultural barriers should not prevent the communities from accessing the healthcare
services provided worldwide. Nurses and healthcare providers need to research and come up
with better solutions to enable aboriginals’ access healthcare services and do away with the
cultural barriers. It can only be achieved by ensuring cultural safety communities such as
aboriginals and winning their trust in the modern healthcare systems.
Conclusion
Health equity is the core value and a basic human right for all human beings. Strategies
and interventions should be put in place to protect and assist the indigenous groups such as the
aboriginals. Cultural barriers should not prevent the communities from accessing the healthcare
services provided worldwide. Nurses and healthcare providers need to research and come up
with better solutions to enable aboriginals’ access healthcare services and do away with the
cultural barriers. It can only be achieved by ensuring cultural safety communities such as
aboriginals and winning their trust in the modern healthcare systems.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





