CNA156 Reflective Essay: Improving Indigenous Healthcare Access
VerifiedAdded on 2023/06/03
|8
|2027
|360
Essay
AI Summary
This essay reflects on the critical role of cultural safety, self-determination, and collaboration in enhancing the health of Aboriginal and Torres Strait Islander peoples in Australia. It addresses the historical and ongoing impacts of colonization on their health and wellbeing, highlighting issues like social exclusion, poor sanitation, and lack of access to resources. The essay explores how personal beliefs and values can influence healthcare practices with Indigenous patients and their families, emphasizing the importance of patient-centered care and involving Indigenous healthcare providers. Furthermore, it proposes advocacy strategies for improving health service delivery to bridge the gap in healthcare equality, including partnerships with Indigenous communities, support for Aboriginal community-controlled health services, cultural safety training, and the abolition of discriminatory policies. The essay concludes by underscoring the need for healthcare providers to advocate for the rights of Indigenous people to ensure equitable access to vital services.

Running Head: HEALTHCARE FOR THE ABORIGINAL AND TORRES STRAIT ISLANDER
PEOPLE
Healthcare for The Aboriginal and Torres Strait Islander People
Students Name
University Affiliation
Date
PEOPLE
Healthcare for The Aboriginal and Torres Strait Islander People
Students Name
University Affiliation
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTHCARE FOR THE ABORIGINAL AND TORRES STRAIT ISLANDER 2
Introduction
According to the National Aboriginal Community Controlled Health Organization
(2018), health is defined as not just a person’s physical wellbeing but the cultural emotional as
well as the social wellbeing of an entire society whereby every person is able to fully attain their
capability as a human being, thus, creating the whole wellbeing of their society. Enhancing the
health status of the Aboriginal and the Torres Strait Islander people has been considered as a
longstanding problem affecting Australian government yet is it one of the fundamental rights of
the people. Even though there have been steadfast improvements and development registered in
certain areas since the 1960s, overall the development has been viewed as inconsistent as well as
slow. The gap of inequality between other people of Australia and the Aboriginal and the Torres
Strait Islander people has remained wide and has not been bridged (DeSilva-Ranasinghe, 2014).
Unless bold and sustainable steps are taken by the government of the country, there is real and
actual prospect the of the Aboriginal and the Torres Strait Islander medical health status may
worsen in the years to come.
This paper will discuss in depth how the cultural safety, self-determination and the
collaboration are key to ensuring the health of the Aboriginal and the Torres Strait Islander
peoples. The paper will address how colonization has and continues to affect medical and
wellbeing of the indigenous Australian, how in my own cultural and Social location including
attitudes, beliefs and values, may influence my future health care practice with the Aboriginal
parents, their families and Aboriginal health workers. Lastly, the paper will discuss how as a
future health provider I will come up with advocacy strategies for health service delivery which
will contribute to the bridging the gap for the indigenous people.
Introduction
According to the National Aboriginal Community Controlled Health Organization
(2018), health is defined as not just a person’s physical wellbeing but the cultural emotional as
well as the social wellbeing of an entire society whereby every person is able to fully attain their
capability as a human being, thus, creating the whole wellbeing of their society. Enhancing the
health status of the Aboriginal and the Torres Strait Islander people has been considered as a
longstanding problem affecting Australian government yet is it one of the fundamental rights of
the people. Even though there have been steadfast improvements and development registered in
certain areas since the 1960s, overall the development has been viewed as inconsistent as well as
slow. The gap of inequality between other people of Australia and the Aboriginal and the Torres
Strait Islander people has remained wide and has not been bridged (DeSilva-Ranasinghe, 2014).
Unless bold and sustainable steps are taken by the government of the country, there is real and
actual prospect the of the Aboriginal and the Torres Strait Islander medical health status may
worsen in the years to come.
This paper will discuss in depth how the cultural safety, self-determination and the
collaboration are key to ensuring the health of the Aboriginal and the Torres Strait Islander
peoples. The paper will address how colonization has and continues to affect medical and
wellbeing of the indigenous Australian, how in my own cultural and Social location including
attitudes, beliefs and values, may influence my future health care practice with the Aboriginal
parents, their families and Aboriginal health workers. Lastly, the paper will discuss how as a
future health provider I will come up with advocacy strategies for health service delivery which
will contribute to the bridging the gap for the indigenous people.
HEALTHCARE FOR THE ABORIGINAL AND TORRES STRAIT ISLANDER 3
How Colonization Has and Continues to affect the Health as well as the Wellbeing of The
Aboriginal and Torres Islander Australian?
The current crisis in indigenous health is because of the generations of neglect,
inadequate cohesive and unifying public policy as well as the failure to offer adequate resources
and ensure that such resources reach individual in Australia. The major problems affecting the
delivery of health services to the indigenous people is due to colonization policies like economic
and social exclusion, poor sanitation and housing, lack of sufficient nutrition, low income,
unemployment and poor education. Historically, the Aboriginal and Strait Islander people have
had very little influence and power to these challenging factors and the decisions in public policy
which affect their health as well as lives. Due to Australian colonization, racism was rife (Dwyer
et al, 2016). The indigenous people were compelled to reside on reserves as well as on missions
where their freedom to live their normal lives were highly limited. Assimilation as well as
segregation policies were established coupled with geographical and institutionalization
limitations.
According to Fedele (2018), moreover, the indigenous people were not allowed to speak
their native language, practicing their traditions and educating their children on their cultures and
history. These limitations resulted to loss of life and liberty and irreparably changed the
indigenous people’s social as well as cultural behavior. Historical atrocities as well as the
continued segregation have established a longstanding psychological and physical impacts on the
indigenous people which are usually transgenerational. This is normally mirrored in several
psychological situations which show that racism and segregation towards indigenous people still
impacts their lives. For instance, rates of unemployment indicate a disparity with about 18%
unemployment for the indigenous people as compared to the 6% for the non-indigenous people
How Colonization Has and Continues to affect the Health as well as the Wellbeing of The
Aboriginal and Torres Islander Australian?
The current crisis in indigenous health is because of the generations of neglect,
inadequate cohesive and unifying public policy as well as the failure to offer adequate resources
and ensure that such resources reach individual in Australia. The major problems affecting the
delivery of health services to the indigenous people is due to colonization policies like economic
and social exclusion, poor sanitation and housing, lack of sufficient nutrition, low income,
unemployment and poor education. Historically, the Aboriginal and Strait Islander people have
had very little influence and power to these challenging factors and the decisions in public policy
which affect their health as well as lives. Due to Australian colonization, racism was rife (Dwyer
et al, 2016). The indigenous people were compelled to reside on reserves as well as on missions
where their freedom to live their normal lives were highly limited. Assimilation as well as
segregation policies were established coupled with geographical and institutionalization
limitations.
According to Fedele (2018), moreover, the indigenous people were not allowed to speak
their native language, practicing their traditions and educating their children on their cultures and
history. These limitations resulted to loss of life and liberty and irreparably changed the
indigenous people’s social as well as cultural behavior. Historical atrocities as well as the
continued segregation have established a longstanding psychological and physical impacts on the
indigenous people which are usually transgenerational. This is normally mirrored in several
psychological situations which show that racism and segregation towards indigenous people still
impacts their lives. For instance, rates of unemployment indicate a disparity with about 18%
unemployment for the indigenous people as compared to the 6% for the non-indigenous people
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HEALTHCARE FOR THE ABORIGINAL AND TORRES STRAIT ISLANDER 4
(Davy et al, 2016). These disparities and the discrimination have affected the indigenous people
access to adequate and sufficient health services that they highly require. It should be noted that
the disparities between the indigenous people and non-indigenous people have been recorded by
the World Health Organization as the highest in the world (Thomas et al, 2017). The current
government assimilation and discrimination policies have ensured that the indigenous people do
not adequately access healthcare services.
How My Own Cultural and Social Locations, Including My Beliefs, Attitudes and Values, May
Influence My Future Health Care Practice with The indigenous Patients, Their Families and
Their Health Workers?
As a non-indigenous individual in Australia practicing health care, my beliefs, attitudes
and values towards the indigenous people will be to equitably and professionally provide them
with the necessary healthcare services. the location of the indigenous people has always been in
the remote areas where access to healthcare services are limited and restricted, however, as a
professional health care provider, I will strive ant attempt to reach every part of the country
especially the areas that are neglected by the government. This will ensure that the indigenous
people receive equal health care services just like their indigenous people. As a professional
healthcare provider in the country, I will relate professionally with the health care providers from
the indigenous people. Families of the patients as well as their relatives will also be treated
equally and their lived experiences in managing and treating certain diseases will be taken into
consideration. It should be noted that there has been discrimination and bias in involving the
lived experiences of the indigenous people in the management of health care practice in the
country. I will, therefore, ensure that I practice patient-centred care in which the patient and their
families are incorporated into the treatment process (Wilson, Ewen & Mazel, 2018).
(Davy et al, 2016). These disparities and the discrimination have affected the indigenous people
access to adequate and sufficient health services that they highly require. It should be noted that
the disparities between the indigenous people and non-indigenous people have been recorded by
the World Health Organization as the highest in the world (Thomas et al, 2017). The current
government assimilation and discrimination policies have ensured that the indigenous people do
not adequately access healthcare services.
How My Own Cultural and Social Locations, Including My Beliefs, Attitudes and Values, May
Influence My Future Health Care Practice with The indigenous Patients, Their Families and
Their Health Workers?
As a non-indigenous individual in Australia practicing health care, my beliefs, attitudes
and values towards the indigenous people will be to equitably and professionally provide them
with the necessary healthcare services. the location of the indigenous people has always been in
the remote areas where access to healthcare services are limited and restricted, however, as a
professional health care provider, I will strive ant attempt to reach every part of the country
especially the areas that are neglected by the government. This will ensure that the indigenous
people receive equal health care services just like their indigenous people. As a professional
healthcare provider in the country, I will relate professionally with the health care providers from
the indigenous people. Families of the patients as well as their relatives will also be treated
equally and their lived experiences in managing and treating certain diseases will be taken into
consideration. It should be noted that there has been discrimination and bias in involving the
lived experiences of the indigenous people in the management of health care practice in the
country. I will, therefore, ensure that I practice patient-centred care in which the patient and their
families are incorporated into the treatment process (Wilson, Ewen & Mazel, 2018).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTHCARE FOR THE ABORIGINAL AND TORRES STRAIT ISLANDER 5
How as A Future Health Service Provider, I Will Develop Advocacy Strategies for Health
Service Delivery Which Will Contribute to Bridging the Gap for the indigenous Islander
Peoples?
Over the last decades the health of the people of Australia has improved steadily due to
the main advantages in health care and the developing prosperity. However, the indigenous
people have not enjoyed the same benefits in health services. The neglect by the government to
the indigenous people is not a normal state of affairs and should be condemned by all and
sundry. The major problem facing indigenous people is the relatively inadequate access basic
healthcare. As a professional health care provider, I will ensure that a partnership is created with
the indigenous people as well as their representatives (Campbell et al, 2018). I will also ensure
that I support the Aboriginal community-controlled healthcare services. Thus, I will make sure
that a considerable number of health care professionals particularly the indigenous people, are
trained so as to deliver basic health care and other medical care services to the Aboriginal and
Torres Strait Islander people. I will also champion through establishment or implementation of
the existing policies on the housing, water and waste systems so as to support the enhancement
of health equality (Clifford, Shakeshaft & Deans, 2013). I will also ensure training in cultural
safety with the aim of enhancing the health care sector’s capacity to develop design in policy
programs and the delivery of culturally adequate and safe services to the indigenous people. I
will also ensure that the discriminatory policies that affect the lives of the indigenous people and
which prevent them from accessing adequate healthcare are abolished.
How as A Future Health Service Provider, I Will Develop Advocacy Strategies for Health
Service Delivery Which Will Contribute to Bridging the Gap for the indigenous Islander
Peoples?
Over the last decades the health of the people of Australia has improved steadily due to
the main advantages in health care and the developing prosperity. However, the indigenous
people have not enjoyed the same benefits in health services. The neglect by the government to
the indigenous people is not a normal state of affairs and should be condemned by all and
sundry. The major problem facing indigenous people is the relatively inadequate access basic
healthcare. As a professional health care provider, I will ensure that a partnership is created with
the indigenous people as well as their representatives (Campbell et al, 2018). I will also ensure
that I support the Aboriginal community-controlled healthcare services. Thus, I will make sure
that a considerable number of health care professionals particularly the indigenous people, are
trained so as to deliver basic health care and other medical care services to the Aboriginal and
Torres Strait Islander people. I will also champion through establishment or implementation of
the existing policies on the housing, water and waste systems so as to support the enhancement
of health equality (Clifford, Shakeshaft & Deans, 2013). I will also ensure training in cultural
safety with the aim of enhancing the health care sector’s capacity to develop design in policy
programs and the delivery of culturally adequate and safe services to the indigenous people. I
will also ensure that the discriminatory policies that affect the lives of the indigenous people and
which prevent them from accessing adequate healthcare are abolished.
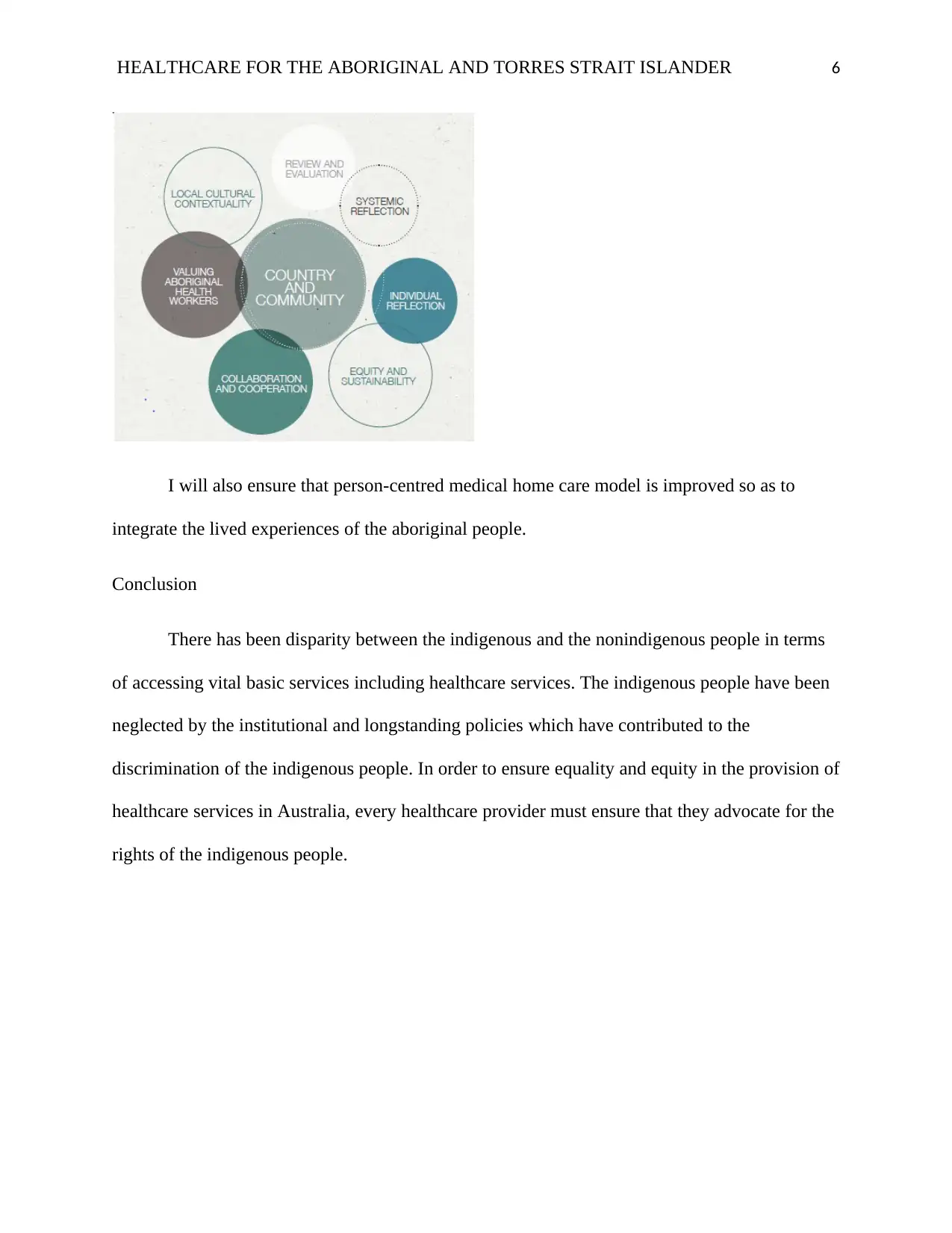
HEALTHCARE FOR THE ABORIGINAL AND TORRES STRAIT ISLANDER 6
I will also ensure that person-centred medical home care model is improved so as to
integrate the lived experiences of the aboriginal people.
Conclusion
There has been disparity between the indigenous and the nonindigenous people in terms
of accessing vital basic services including healthcare services. The indigenous people have been
neglected by the institutional and longstanding policies which have contributed to the
discrimination of the indigenous people. In order to ensure equality and equity in the provision of
healthcare services in Australia, every healthcare provider must ensure that they advocate for the
rights of the indigenous people.
I will also ensure that person-centred medical home care model is improved so as to
integrate the lived experiences of the aboriginal people.
Conclusion
There has been disparity between the indigenous and the nonindigenous people in terms
of accessing vital basic services including healthcare services. The indigenous people have been
neglected by the institutional and longstanding policies which have contributed to the
discrimination of the indigenous people. In order to ensure equality and equity in the provision of
healthcare services in Australia, every healthcare provider must ensure that they advocate for the
rights of the indigenous people.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HEALTHCARE FOR THE ABORIGINAL AND TORRES STRAIT ISLANDER 7
References
Campbell, MA, Hunt, J, Scrimgeour, DJ, Davey, M & Jones, V 2018, ‘Contribution of
Aboriginal Community-Controlled Health Services to improving Aboriginal health: an evidence
review’, Australian Health Review, vol. 42, no. 2, pp. 218–226,
Clifford, A, Shakeshaft, A & Deans, C 2013, ‘Training and tailored outreach support to
improve alcohol screening and brief intervention in Aboriginal Community Controlled Health
Services’, Drug & Alcohol Review, vol. 32, no. 1, pp. 72–79,
Davy, C, Cass, A, Brady, J, DeVries, J, Fewquandie, B, Ingram, S, Mentha, R, Simon, P,
Rickards, B, Togni, S, Liu, H, Peiris, D, Askew, D, Kite, E, Sivak, L, Hackett, M, Lavoie, J &
Brown, A 2016, ‘Facilitating engagement through strong relationships between primary
healthcare and Aboriginal and Torres Strait Islander peoples’, Australian & New Zealand
Journal of Public Health, vol. 40, no. 6, pp. 535–541,
DeSilva-Ranasinghe, S 2014, ‘Indigenous Nation Building: The Army Aboriginal Community
Assistance Program’, Policy, vol. 30, no. 4, pp. 29–35,
Dwyer, J, O’Donnell, K, Willis, E & Kelly, J 2016, ‘Equitable Care for Indigenous People:
every health service can do it’, Asia Pacific Journal of Health Management, vol. 11, no. 3, pp.
11–17,
Fedele, R 2018, ‘END OF AN ERA: AN INSPIRING ABORIGINAL LEADER. (Cover
story)’, Australian Nursing & Midwifery Journal, vol. 26, no. 4, pp. 10–12,
Markwick, A., Ansari, Z., Sullivan, M., Parsons, L. and McNeil, J 2014, Inequalities in the social
determinants of health of Aboriginal and Torres Strait Islander People: a cross-sectional
References
Campbell, MA, Hunt, J, Scrimgeour, DJ, Davey, M & Jones, V 2018, ‘Contribution of
Aboriginal Community-Controlled Health Services to improving Aboriginal health: an evidence
review’, Australian Health Review, vol. 42, no. 2, pp. 218–226,
Clifford, A, Shakeshaft, A & Deans, C 2013, ‘Training and tailored outreach support to
improve alcohol screening and brief intervention in Aboriginal Community Controlled Health
Services’, Drug & Alcohol Review, vol. 32, no. 1, pp. 72–79,
Davy, C, Cass, A, Brady, J, DeVries, J, Fewquandie, B, Ingram, S, Mentha, R, Simon, P,
Rickards, B, Togni, S, Liu, H, Peiris, D, Askew, D, Kite, E, Sivak, L, Hackett, M, Lavoie, J &
Brown, A 2016, ‘Facilitating engagement through strong relationships between primary
healthcare and Aboriginal and Torres Strait Islander peoples’, Australian & New Zealand
Journal of Public Health, vol. 40, no. 6, pp. 535–541,
DeSilva-Ranasinghe, S 2014, ‘Indigenous Nation Building: The Army Aboriginal Community
Assistance Program’, Policy, vol. 30, no. 4, pp. 29–35,
Dwyer, J, O’Donnell, K, Willis, E & Kelly, J 2016, ‘Equitable Care for Indigenous People:
every health service can do it’, Asia Pacific Journal of Health Management, vol. 11, no. 3, pp.
11–17,
Fedele, R 2018, ‘END OF AN ERA: AN INSPIRING ABORIGINAL LEADER. (Cover
story)’, Australian Nursing & Midwifery Journal, vol. 26, no. 4, pp. 10–12,
Markwick, A., Ansari, Z., Sullivan, M., Parsons, L. and McNeil, J 2014, Inequalities in the social
determinants of health of Aboriginal and Torres Strait Islander People: a cross-sectional
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTHCARE FOR THE ABORIGINAL AND TORRES STRAIT ISLANDER 8
population-based study in the Australian state of Victoria. International Journal for Equity in
HealthThe official journal of the International Society for Equity in Health201413:91.
https://doi.org/10.1186/s12939-014-0091-5
NACCHO, 2018, Aboriginal health, https://www.naccho.org.au/about/aboriginal-health/
Thomas, DP, Panaretto, KS, Davey, M, Briggs, V & Borland, R 2017, ‘The social determinants
and starting and sustaining quit attempts in a national sample of Aboriginal and Torres Strait
Islander smokers’, Australian & New Zealand Journal of Public Health, vol. 41, no. 3, pp. 230–
236,
Wilson, N, Ewen, S & Mazel, O 2018, ‘Medical students in Aboriginal Community Controlled
Health Services: identifying the factors involved in successful placements for staff and
students’, Australian Medical Student Journal, vol. 8, no. 2, pp. 26–29,
population-based study in the Australian state of Victoria. International Journal for Equity in
HealthThe official journal of the International Society for Equity in Health201413:91.
https://doi.org/10.1186/s12939-014-0091-5
NACCHO, 2018, Aboriginal health, https://www.naccho.org.au/about/aboriginal-health/
Thomas, DP, Panaretto, KS, Davey, M, Briggs, V & Borland, R 2017, ‘The social determinants
and starting and sustaining quit attempts in a national sample of Aboriginal and Torres Strait
Islander smokers’, Australian & New Zealand Journal of Public Health, vol. 41, no. 3, pp. 230–
236,
Wilson, N, Ewen, S & Mazel, O 2018, ‘Medical students in Aboriginal Community Controlled
Health Services: identifying the factors involved in successful placements for staff and
students’, Australian Medical Student Journal, vol. 8, no. 2, pp. 26–29,
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




