Acute Care Nursing Report: Patient Care After Laparotomy Surgery
VerifiedAdded on 2019/10/31
|7
|1684
|180
Report
AI Summary
This acute care nursing report focuses on the care of a patient, Mr. Jones, who underwent a laparotomy for a recto-sigmoid tumor and subsequently received a colostomy. The report addresses key learning triggers related to intestinal obstruction, surgical goals, pre-operative preparation, and the types and management of ostomies. It includes a detailed patient and family teaching guide on ostomy self-care, along with a discussion of the effects of food on stoma output. The report further outlines a comprehensive nursing care plan, encompassing nursing diagnoses such as risk of constipation, acute pain, and impaired skin/tissue integrity. Each diagnosis includes specific goals, nursing interventions, rationales, and expected outcomes. The report concludes with a list of relevant references supporting the presented information. This assignment is designed to provide a thorough understanding of post-operative care following abdominal surgery and colostomy creation.

Acute care
Name of the student:
Name of the university:
Author note:
Name of the student:
Name of the university:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PART A
Laparotomy is a type of incision in the abdominal cavity. This type of operation is generally for
the examination of the abdominal organs and for the diagnosis of any type of problem which
includes abdominal pain. After the laparotomy had been done it can cause to various problems.
Here in this care plan there has been described the top three priority problems are risk of
constipation, acute pain and skin/tissue integrity, impaired (Ackley & Makic, 2016).
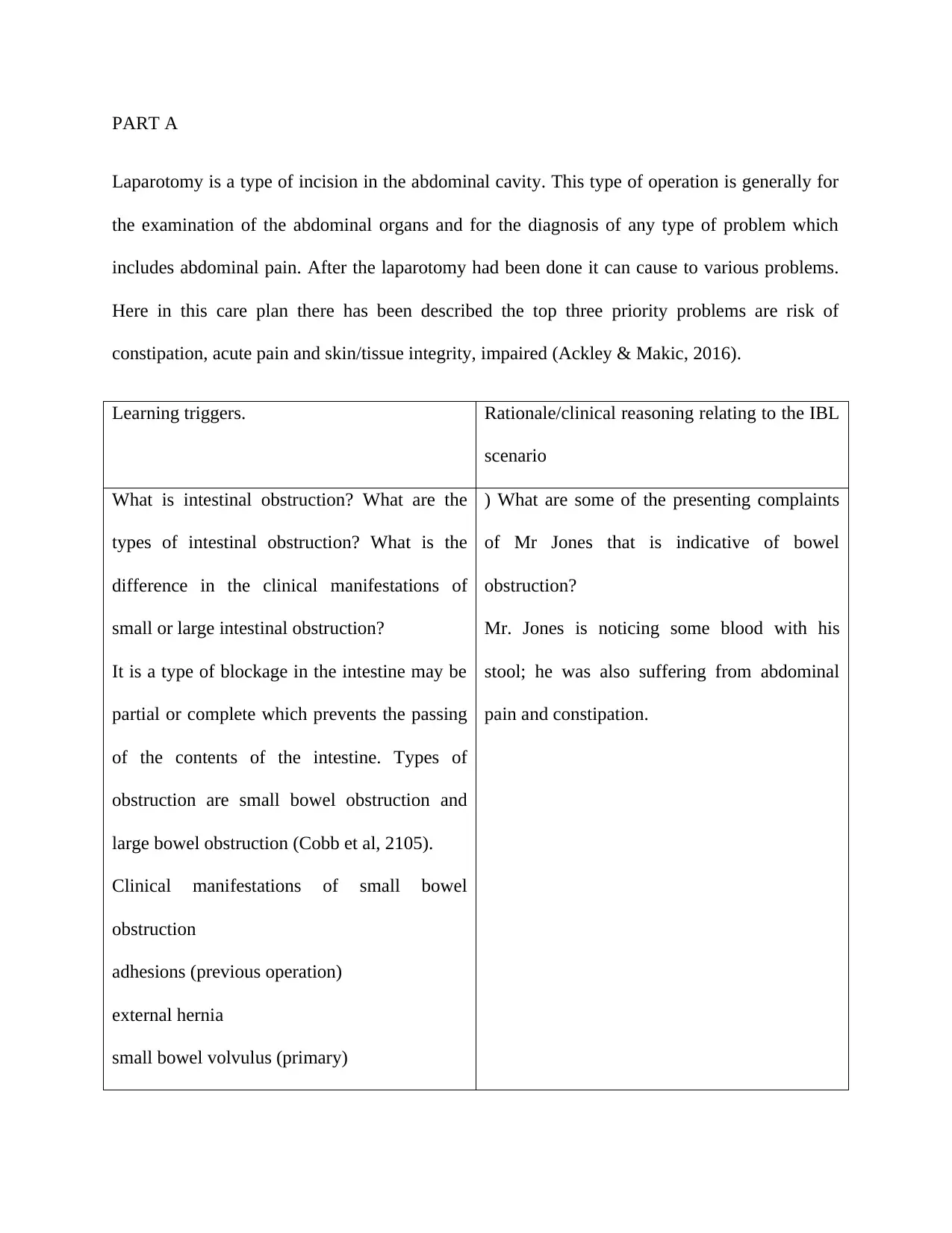
Learning triggers. Rationale/clinical reasoning relating to the IBL
scenario
What is intestinal obstruction? What are the
types of intestinal obstruction? What is the
difference in the clinical manifestations of
small or large intestinal obstruction?
It is a type of blockage in the intestine may be
partial or complete which prevents the passing
of the contents of the intestine. Types of
obstruction are small bowel obstruction and
large bowel obstruction (Cobb et al, 2105).
Clinical manifestations of small bowel
obstruction
adhesions (previous operation)
external hernia
small bowel volvulus (primary)
) What are some of the presenting complaints
of Mr Jones that is indicative of bowel
obstruction?
Mr. Jones is noticing some blood with his
stool; he was also suffering from abdominal
pain and constipation.
Laparotomy is a type of incision in the abdominal cavity. This type of operation is generally for
the examination of the abdominal organs and for the diagnosis of any type of problem which
includes abdominal pain. After the laparotomy had been done it can cause to various problems.
Here in this care plan there has been described the top three priority problems are risk of
constipation, acute pain and skin/tissue integrity, impaired (Ackley & Makic, 2016).
Learning triggers. Rationale/clinical reasoning relating to the IBL
scenario
What is intestinal obstruction? What are the
types of intestinal obstruction? What is the
difference in the clinical manifestations of
small or large intestinal obstruction?
It is a type of blockage in the intestine may be
partial or complete which prevents the passing
of the contents of the intestine. Types of
obstruction are small bowel obstruction and
large bowel obstruction (Cobb et al, 2105).
Clinical manifestations of small bowel
obstruction
adhesions (previous operation)
external hernia
small bowel volvulus (primary)
) What are some of the presenting complaints
of Mr Jones that is indicative of bowel
obstruction?
Mr. Jones is noticing some blood with his
stool; he was also suffering from abdominal
pain and constipation.

neoplasms
Clinical manifestations of large bowel
obstruction
carcinoma of colon
volvulus (sigmoid)
diverticular disease
What are the surgical goals and the pre-
operative preparation for a patient going for
colorectal surgery?
The patient starts preparing for the surgery few
days before the surgery (Doenges & Murr,
2014). The doctor may prescribe the oral
antibiotics to start days before the surgery. The
patient is asked to keep the colon as empty as
possible to keep the risk of infection at bay.
2) The operation has a stoma and a large
dressing covering his laparotomy wound.
The basic principle of the surgery is to remove
the vascular pedicle along with the lymphatics
which feeds the tumor. This procedure is done
to obtain a tumor free margin.
What type of surgery does Mr Jones need for
his recto sigmoid tumour? Why is a colostomy
performed in Mr Jones’ case?
An emergency laparotomy was done on Mr.
Jones for the resection of the recto-sigmoid
tumor. After the surgery he has a stoma and a
large dressing covering his laparotomy wound
Clinical manifestations of large bowel
obstruction
carcinoma of colon
volvulus (sigmoid)
diverticular disease
What are the surgical goals and the pre-
operative preparation for a patient going for
colorectal surgery?
The patient starts preparing for the surgery few
days before the surgery (Doenges & Murr,
2014). The doctor may prescribe the oral
antibiotics to start days before the surgery. The
patient is asked to keep the colon as empty as
possible to keep the risk of infection at bay.
2) The operation has a stoma and a large
dressing covering his laparotomy wound.
The basic principle of the surgery is to remove
the vascular pedicle along with the lymphatics
which feeds the tumor. This procedure is done
to obtain a tumor free margin.
What type of surgery does Mr Jones need for
his recto sigmoid tumour? Why is a colostomy
performed in Mr Jones’ case?
An emergency laparotomy was done on Mr.
Jones for the resection of the recto-sigmoid
tumor. After the surgery he has a stoma and a
large dressing covering his laparotomy wound
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

(Lambrecht et al., 2015).
4) What are the types of ostomies? What are
the specific nursing management after ostomy
surgery? Two types of ostomies are ilieostomy
and colostomy. Nursing care management plan
after surgery are:
Assessment on the stoma location and the
colostomy.
Position a collection bag or drainable pouch
over the stoma.
Empty a drainable pouch or replace the
colostomy bag according to the need or when it
is one-third full.
Provide stomal and skin care for the client with
a colostomy (Zhang & Zheng, 2017).
How long will it take for Mr Jones’s colostomy
to be active? What are some of the possible
areas of concerns of Mr Jones going home with
a colostomy?
Post operative care for Mr. Jones are:
Mr. Jones has to strictly follow a balanced diet
which comprises a lot of fresh fruits ans
vegetables.
Eating yogurt or drinking buttermilk may help
reduce gas.
Mr Jones must change his pouch. Empty the
pouch when it is one-third full.
Mr Jones must stop eating such foods like
cabbage, broccoli, onions, garlic and fish in to
reduce the odour of the bowel.
Every time while emptying the pouch, very
carefully clean the pouch opening. Never
forget to clean both inside and outside of the
pouch with a wet toilet paper.
He must rinse his pouch 1 or 2 times daily after
you empty it (Di Gesaro, 2012)
5) Identify some of the general post-operative 5) Prepare a patient & family teaching guide
4) What are the types of ostomies? What are
the specific nursing management after ostomy
surgery? Two types of ostomies are ilieostomy
and colostomy. Nursing care management plan
after surgery are:
Assessment on the stoma location and the
colostomy.
Position a collection bag or drainable pouch
over the stoma.
Empty a drainable pouch or replace the
colostomy bag according to the need or when it
is one-third full.
Provide stomal and skin care for the client with
a colostomy (Zhang & Zheng, 2017).
How long will it take for Mr Jones’s colostomy
to be active? What are some of the possible
areas of concerns of Mr Jones going home with
a colostomy?
Post operative care for Mr. Jones are:
Mr. Jones has to strictly follow a balanced diet
which comprises a lot of fresh fruits ans
vegetables.
Eating yogurt or drinking buttermilk may help
reduce gas.
Mr Jones must change his pouch. Empty the
pouch when it is one-third full.
Mr Jones must stop eating such foods like
cabbage, broccoli, onions, garlic and fish in to
reduce the odour of the bowel.
Every time while emptying the pouch, very
carefully clean the pouch opening. Never
forget to clean both inside and outside of the
pouch with a wet toilet paper.
He must rinse his pouch 1 or 2 times daily after
you empty it (Di Gesaro, 2012)
5) Identify some of the general post-operative 5) Prepare a patient & family teaching guide
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
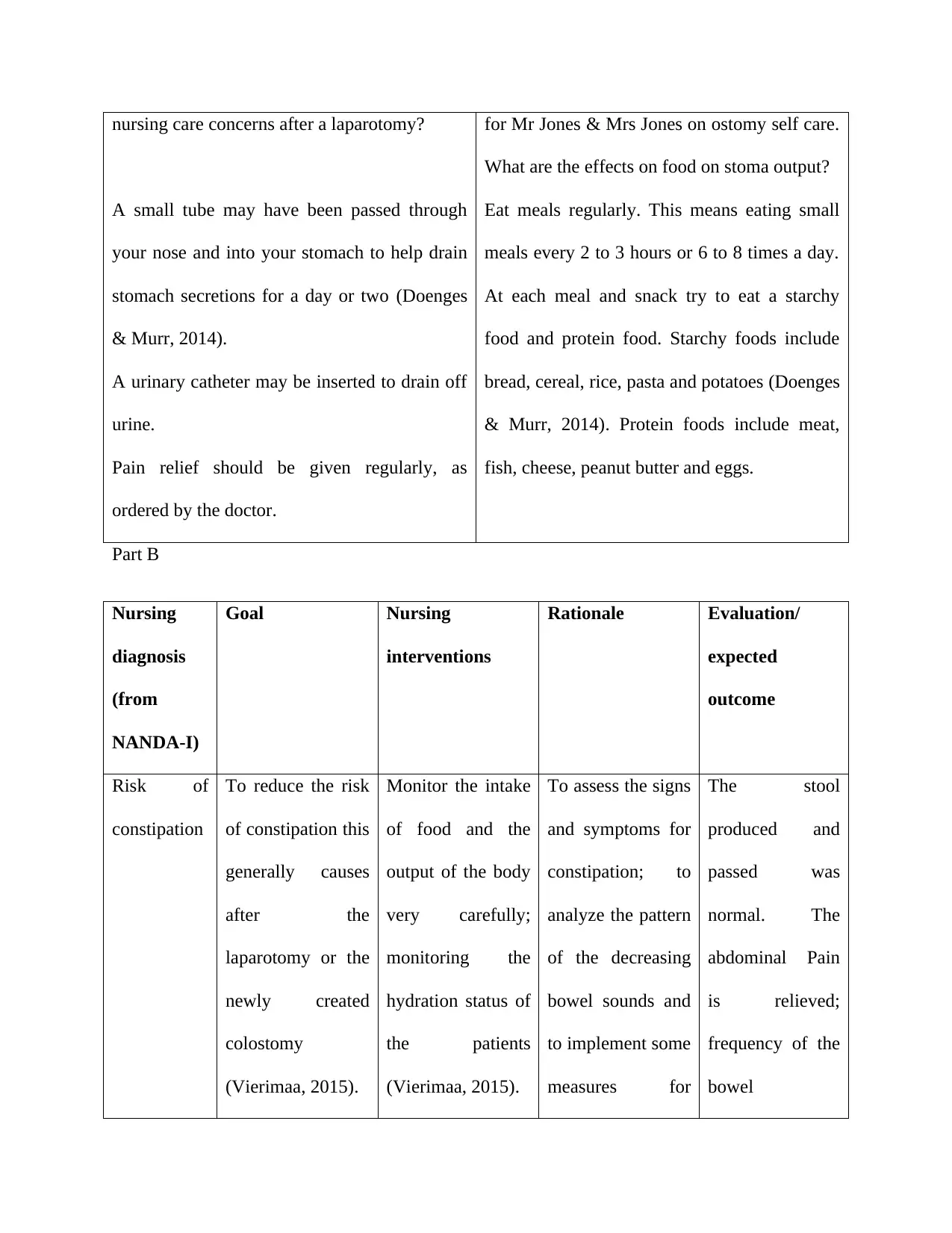
nursing care concerns after a laparotomy?
A small tube may have been passed through
your nose and into your stomach to help drain
stomach secretions for a day or two (Doenges
& Murr, 2014).
A urinary catheter may be inserted to drain off
urine.
Pain relief should be given regularly, as
ordered by the doctor.
for Mr Jones & Mrs Jones on ostomy self care.
What are the effects on food on stoma output?
Eat meals regularly. This means eating small
meals every 2 to 3 hours or 6 to 8 times a day.
At each meal and snack try to eat a starchy
food and protein food. Starchy foods include
bread, cereal, rice, pasta and potatoes (Doenges
& Murr, 2014). Protein foods include meat,
fish, cheese, peanut butter and eggs.
Part B
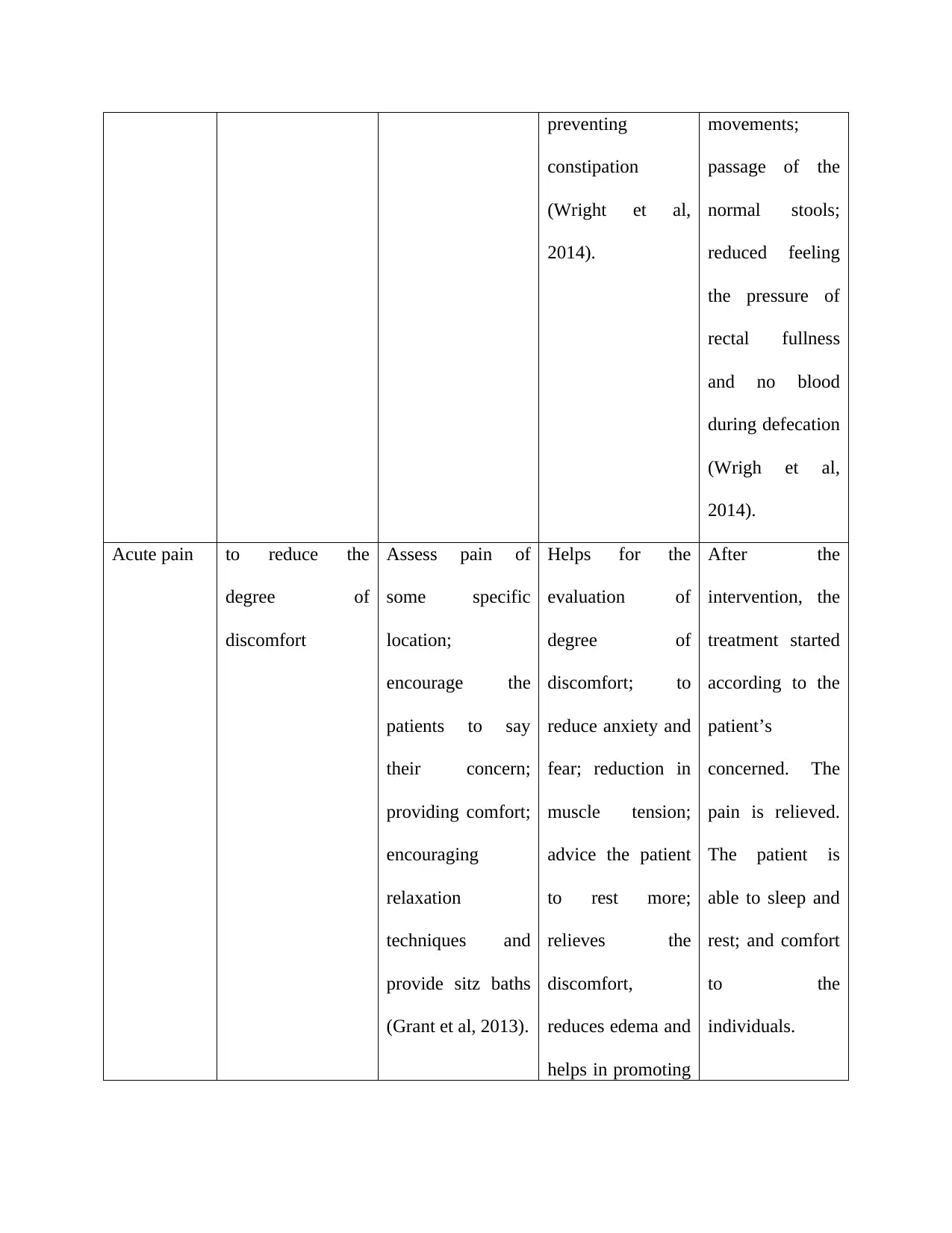
Nursing
diagnosis
(from
NANDA-I)
Goal Nursing
interventions
Rationale Evaluation/
expected
outcome
Risk of
constipation
To reduce the risk
of constipation this
generally causes
after the
laparotomy or the
newly created
colostomy
(Vierimaa, 2015).
Monitor the intake
of food and the
output of the body
very carefully;
monitoring the
hydration status of
the patients
(Vierimaa, 2015).
To assess the signs
and symptoms for
constipation; to
analyze the pattern
of the decreasing
bowel sounds and
to implement some
measures for
The stool
produced and
passed was
normal. The
abdominal Pain
is relieved;
frequency of the
bowel
A small tube may have been passed through
your nose and into your stomach to help drain
stomach secretions for a day or two (Doenges
& Murr, 2014).
A urinary catheter may be inserted to drain off
urine.
Pain relief should be given regularly, as
ordered by the doctor.
for Mr Jones & Mrs Jones on ostomy self care.
What are the effects on food on stoma output?
Eat meals regularly. This means eating small
meals every 2 to 3 hours or 6 to 8 times a day.
At each meal and snack try to eat a starchy
food and protein food. Starchy foods include
bread, cereal, rice, pasta and potatoes (Doenges
& Murr, 2014). Protein foods include meat,
fish, cheese, peanut butter and eggs.
Part B
Nursing
diagnosis
(from
NANDA-I)
Goal Nursing
interventions
Rationale Evaluation/
expected
outcome
Risk of
constipation
To reduce the risk
of constipation this
generally causes
after the
laparotomy or the
newly created
colostomy
(Vierimaa, 2015).
Monitor the intake
of food and the
output of the body
very carefully;
monitoring the
hydration status of
the patients
(Vierimaa, 2015).
To assess the signs
and symptoms for
constipation; to
analyze the pattern
of the decreasing
bowel sounds and
to implement some
measures for
The stool
produced and
passed was
normal. The
abdominal Pain
is relieved;
frequency of the
bowel
preventing
constipation
(Wright et al,
2014).
movements;
passage of the
normal stools;
reduced feeling
the pressure of
rectal fullness
and no blood
during defecation
(Wrigh et al,
2014).
Acute pain to reduce the
degree of
discomfort
Assess pain of
some specific
location;
encourage the
patients to say
their concern;
providing comfort;
encouraging
relaxation
techniques and
provide sitz baths
(Grant et al, 2013).
Helps for the
evaluation of
degree of
discomfort; to
reduce anxiety and
fear; reduction in
muscle tension;
advice the patient
to rest more;
relieves the
discomfort,
reduces edema and
helps in promoting
After the
intervention, the
treatment started
according to the
patient’s
concerned. The
pain is relieved.
The patient is
able to sleep and
rest; and comfort
to the
individuals.
constipation
(Wright et al,
2014).
movements;
passage of the
normal stools;
reduced feeling
the pressure of
rectal fullness
and no blood
during defecation
(Wrigh et al,
2014).
Acute pain to reduce the
degree of
discomfort
Assess pain of
some specific
location;
encourage the
patients to say
their concern;
providing comfort;
encouraging
relaxation
techniques and
provide sitz baths
(Grant et al, 2013).
Helps for the
evaluation of
degree of
discomfort; to
reduce anxiety and
fear; reduction in
muscle tension;
advice the patient
to rest more;
relieves the
discomfort,
reduces edema and
helps in promoting
After the
intervention, the
treatment started
according to the
patient’s
concerned. The
pain is relieved.
The patient is
able to sleep and
rest; and comfort
to the
individuals.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
healing (Grant et
al., 2013).
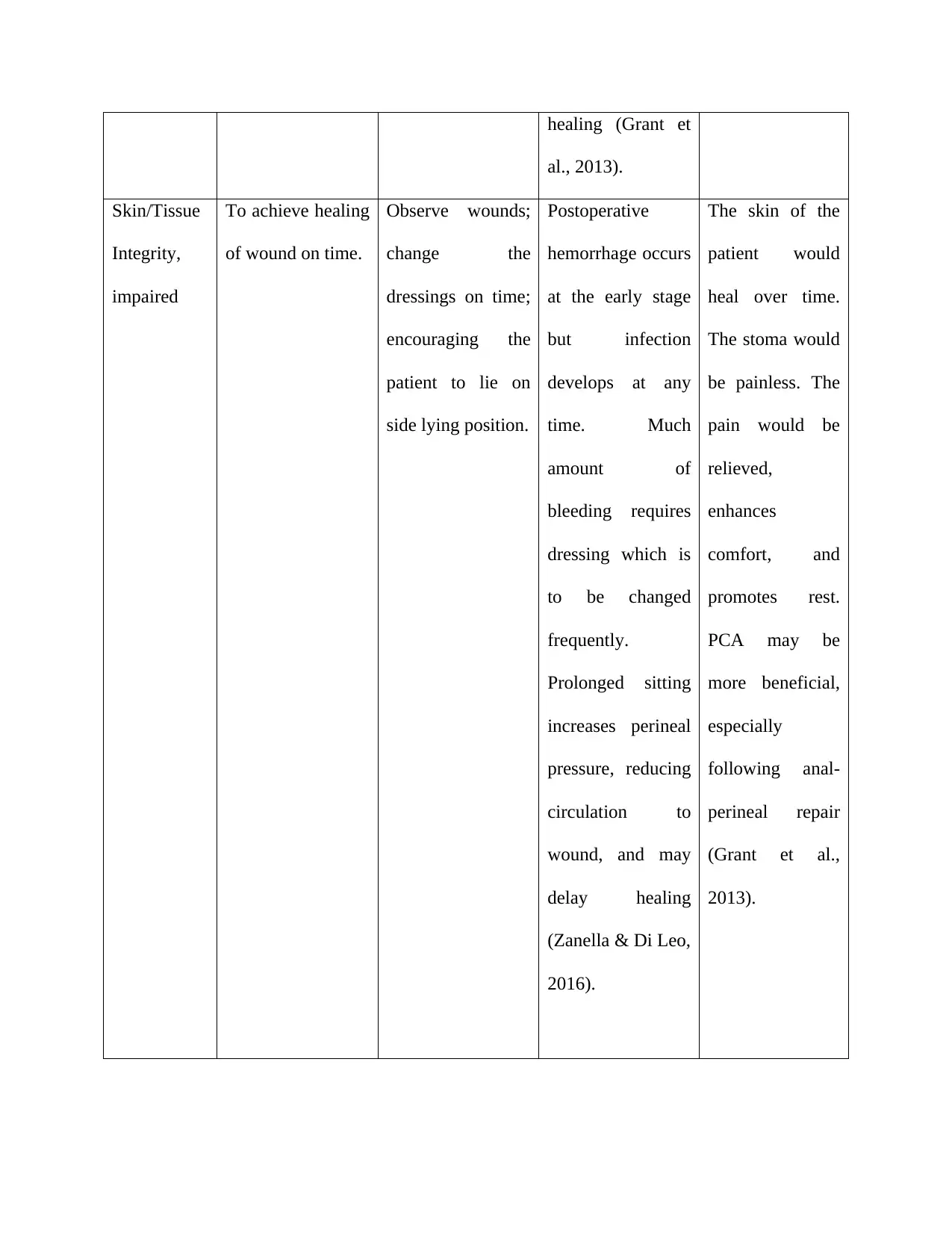
Skin/Tissue
Integrity,
impaired
To achieve healing
of wound on time.
Observe wounds;
change the
dressings on time;
encouraging the
patient to lie on
side lying position.
Postoperative
hemorrhage occurs
at the early stage
but infection
develops at any
time. Much
amount of
bleeding requires
dressing which is
to be changed
frequently.
Prolonged sitting
increases perineal
pressure, reducing
circulation to
wound, and may
delay healing
(Zanella & Di Leo,
2016).
The skin of the
patient would
heal over time.
The stoma would
be painless. The
pain would be
relieved,
enhances
comfort, and
promotes rest.
PCA may be
more beneficial,
especially
following anal-
perineal repair
(Grant et al.,
2013).
al., 2013).
Skin/Tissue
Integrity,
impaired
To achieve healing
of wound on time.
Observe wounds;
change the
dressings on time;
encouraging the
patient to lie on
side lying position.
Postoperative
hemorrhage occurs
at the early stage
but infection
develops at any
time. Much
amount of
bleeding requires
dressing which is
to be changed
frequently.
Prolonged sitting
increases perineal
pressure, reducing
circulation to
wound, and may
delay healing
(Zanella & Di Leo,
2016).
The skin of the
patient would
heal over time.
The stoma would
be painless. The
pain would be
relieved,
enhances
comfort, and
promotes rest.
PCA may be
more beneficial,
especially
following anal-
perineal repair
(Grant et al.,
2013).
1 out of 7
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.