ACUTE CORONARY SYNDROME
VerifiedAdded on 2023/01/16
|12
|3546
|1
AI Summary
This document provides information on ACUTE CORONARY SYNDROME, including the rationale for ECG request, pathophysiology of angina, risk factors of ACS, ECG interpretation, central findings for diagnosis, and discussion of drugs. It also discusses the mechanism of action and use of Ticagrelor and Aspirin in cardiac patients, as well as the use of Morphine in ACS.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Running head: ACUTE CORONARY SYNDROME 1
Introduction
The paper will answer the given questions with regard to the case scenario of Betsy
Blogger with a previous medical history of Coronary Heart Disease (CHD), Type 2 Diabetes
Mellitus, hypertension, Chronic Obstructive Pulmonary Disease (COPD), and Coronary
Artery Bypass Graft. The paper will provide the rationale and interpretation for Betsy’s
request for ECG and the pathophysiology of angina including the two primary risk factors of
Acute Coronary Syndrome (ACS). The paper will discuss some of the medication regimens,
three central findings for the diagnosis of ACS, and the connection between high risk of
depression and Coronary Heart Disease.
Question 1: Rationale for Betsy’s ECG request
The Electrocardiogram was meant to record the electrical activity of the patient’s
heart when at rest. This EG was used to obtain the information about the patient's heart
rhythm and heart and any heart enlargement due to hypertension or signs of past myocardial
infarction. It was necessary to test if the patient had risk factors of heart disease like chest
pain, shortness of breath, and elevated blood pressure. With regard to the case scenario, the
patient presented to the surgical ward with complaints of shortness of breath and nausea
(Amsterdam et al., 2014).
Question 2a: Pathophysiology and progress of Angina
Angina is the chest discomfort, chest pain, or tightness which typically last for about
one to fifteen minutes. Angina is divided into stable, unstable, nonSTEMI, and STEMI based
on the pattern of attacks. The chest discomfort primarily results from insufficient oxygen
supply to the heart muscles which results in cardiac ischemia. The primary process associated
with the inadequate flow of oxygenated blood to the heart is atherosclerosis. Atherosclerosis
refers to the buildup or accumulation of plaque at the arteries thus reducing the blood flow to
the heart. The gradual deposition of fats leads to the narrowing and stiffening of the arteries
Introduction
The paper will answer the given questions with regard to the case scenario of Betsy
Blogger with a previous medical history of Coronary Heart Disease (CHD), Type 2 Diabetes
Mellitus, hypertension, Chronic Obstructive Pulmonary Disease (COPD), and Coronary
Artery Bypass Graft. The paper will provide the rationale and interpretation for Betsy’s
request for ECG and the pathophysiology of angina including the two primary risk factors of
Acute Coronary Syndrome (ACS). The paper will discuss some of the medication regimens,
three central findings for the diagnosis of ACS, and the connection between high risk of
depression and Coronary Heart Disease.
Question 1: Rationale for Betsy’s ECG request
The Electrocardiogram was meant to record the electrical activity of the patient’s
heart when at rest. This EG was used to obtain the information about the patient's heart
rhythm and heart and any heart enlargement due to hypertension or signs of past myocardial
infarction. It was necessary to test if the patient had risk factors of heart disease like chest
pain, shortness of breath, and elevated blood pressure. With regard to the case scenario, the
patient presented to the surgical ward with complaints of shortness of breath and nausea
(Amsterdam et al., 2014).
Question 2a: Pathophysiology and progress of Angina
Angina is the chest discomfort, chest pain, or tightness which typically last for about
one to fifteen minutes. Angina is divided into stable, unstable, nonSTEMI, and STEMI based
on the pattern of attacks. The chest discomfort primarily results from insufficient oxygen
supply to the heart muscles which results in cardiac ischemia. The primary process associated
with the inadequate flow of oxygenated blood to the heart is atherosclerosis. Atherosclerosis
refers to the buildup or accumulation of plaque at the arteries thus reducing the blood flow to
the heart. The gradual deposition of fats leads to the narrowing and stiffening of the arteries
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
ACUTE CORONARY SYNDROME 2
thus minimizing the supply of oxygen to the heart (Santos-Gallego, Picatoste, & Badimon,
2014).
Coronary arteries are the vessels responsible for the delivery of oxygenated blood to
the cardiac muscles to ensues continuous and effective functioning of the heart. The blockage
of one of the three vessels by blood clots or fat deposits results in angina. There are other risk
factors which increase the possibility of recurrence of angina in a patient. These factors
include tobacco use, hypertension, Type 2 diabetes, high levels of blood cholesterol or
triglycerides, older age, and family, past medical or surgical history of heart diseases
(Giustino et al., 2015).
Smoking, chewing tobacco and long-time exposure to a passive form of smoking
damages the interior walls of the coronary arteries thus allowing the collection of cholesterol
deposits which consequently results in blockage of the flow of blood to the heart.
Additionally, smoking acts as a booster for atherosclerosis by maximizing the pulse rate and
blood pressure. Increased pulse rate and blood pressure increase the demand for myocardial
oxygen by the heart thus. Smoking also results in the hardening and narrowing of the arteries
thus lowering their oxygen-carrying capacity and increasing the possibility of recurrence of
angina in a patient (Niccoli, Montone, Lanza, & Crea, 2017).
Diabetes results from the inability of the patient’s body to produce or regulate the
levels of insulin properly. Diabetes is associated with the increased risk of development of
Coronary Artery Disease which results in angina and cardiac attacks by increasing the levels
of cholesterol in the blood and speeding up the rate of atherosclerosis (Radico, Cicchitti,
Zimarino, & De Caterina, 2014). Elevated blood pressure damages the arteries through the
acceleration of the hardening of arteries which results in reduced and insufficient flow of
blood to the cardiac muscles.
thus minimizing the supply of oxygen to the heart (Santos-Gallego, Picatoste, & Badimon,
2014).
Coronary arteries are the vessels responsible for the delivery of oxygenated blood to
the cardiac muscles to ensues continuous and effective functioning of the heart. The blockage
of one of the three vessels by blood clots or fat deposits results in angina. There are other risk
factors which increase the possibility of recurrence of angina in a patient. These factors
include tobacco use, hypertension, Type 2 diabetes, high levels of blood cholesterol or
triglycerides, older age, and family, past medical or surgical history of heart diseases
(Giustino et al., 2015).
Smoking, chewing tobacco and long-time exposure to a passive form of smoking
damages the interior walls of the coronary arteries thus allowing the collection of cholesterol
deposits which consequently results in blockage of the flow of blood to the heart.
Additionally, smoking acts as a booster for atherosclerosis by maximizing the pulse rate and
blood pressure. Increased pulse rate and blood pressure increase the demand for myocardial
oxygen by the heart thus. Smoking also results in the hardening and narrowing of the arteries
thus lowering their oxygen-carrying capacity and increasing the possibility of recurrence of
angina in a patient (Niccoli, Montone, Lanza, & Crea, 2017).
Diabetes results from the inability of the patient’s body to produce or regulate the
levels of insulin properly. Diabetes is associated with the increased risk of development of
Coronary Artery Disease which results in angina and cardiac attacks by increasing the levels
of cholesterol in the blood and speeding up the rate of atherosclerosis (Radico, Cicchitti,
Zimarino, & De Caterina, 2014). Elevated blood pressure damages the arteries through the
acceleration of the hardening of arteries which results in reduced and insufficient flow of
blood to the cardiac muscles.
ACUTE CORONARY SYNDROME 3
High levels of triglycerides or cholesterol in the body form the major components of
the arterial deposits which result in the narrowing of the arteries in the body including the
ones supplying the heart. High levels of cholesterol especially, the Low-Density Lipoprotein
(LDL) which increases the risk of development angina and cardiac attacks. Family history of
cardiac diseases such as heart attack or Coronary Artery Disease increases the risk of
development of angina (Lewis, Collier, & Heitkemper, 2017).
There are multiple signs and symptoms which act as an indication of angina. One of
them is the expression of the feeling of pressure, tightness, burning or squeezing in the chest
region. The patient experience attacks like central chest pain radiating to the neck, arms,
shoulders, throat, jaw, back, or upper abdomen. Also, the patient may encounter other things
like shortness of breath, especially when involved in a physical activity associated with
fatigue, nausea, light-headedness, sweating, or weakness (Fors et al., 2015).
Stable angina lasts for approximately 10 minutes and usually relieves when the patient
is resting or on medication. The patient experiences an episode of chest pain radiating to the
back, arms, or other body areas making it more predictable. Stable angina is usually
stimulated by physical activity which activates the sympathetic system thus resulting in
increased pulse rate, high blood pressure, and contractions which increase the oxygen
demand by the cardiac muscles (Ford, Corcoran, & Berry, 2018).
Stable angina progresses to unstable angina which is dangerous and should be
managed as an emergency. In unstable angina, the patient may experience unexpected
discomfort or pain lasting longer and is not relieved by medication or resting. This results in
an increased risk of other chronic conditions such as myocardial ischemia, cardiac failure,
severe cardiac arrhythmias, and sudden death. If not well managed, unstable angina may
progress to non-STEMI which results from partial occlusion of the supply blood supply to the
High levels of triglycerides or cholesterol in the body form the major components of
the arterial deposits which result in the narrowing of the arteries in the body including the
ones supplying the heart. High levels of cholesterol especially, the Low-Density Lipoprotein
(LDL) which increases the risk of development angina and cardiac attacks. Family history of
cardiac diseases such as heart attack or Coronary Artery Disease increases the risk of
development of angina (Lewis, Collier, & Heitkemper, 2017).
There are multiple signs and symptoms which act as an indication of angina. One of
them is the expression of the feeling of pressure, tightness, burning or squeezing in the chest
region. The patient experience attacks like central chest pain radiating to the neck, arms,
shoulders, throat, jaw, back, or upper abdomen. Also, the patient may encounter other things
like shortness of breath, especially when involved in a physical activity associated with
fatigue, nausea, light-headedness, sweating, or weakness (Fors et al., 2015).
Stable angina lasts for approximately 10 minutes and usually relieves when the patient
is resting or on medication. The patient experiences an episode of chest pain radiating to the
back, arms, or other body areas making it more predictable. Stable angina is usually
stimulated by physical activity which activates the sympathetic system thus resulting in
increased pulse rate, high blood pressure, and contractions which increase the oxygen
demand by the cardiac muscles (Ford, Corcoran, & Berry, 2018).
Stable angina progresses to unstable angina which is dangerous and should be
managed as an emergency. In unstable angina, the patient may experience unexpected
discomfort or pain lasting longer and is not relieved by medication or resting. This results in
an increased risk of other chronic conditions such as myocardial ischemia, cardiac failure,
severe cardiac arrhythmias, and sudden death. If not well managed, unstable angina may
progress to non-STEMI which results from partial occlusion of the supply blood supply to the
ACUTE CORONARY SYNDROME 4
heart. STEMI is the most severe heart attack which is caused by total occlusion of the arteries
by a thrombus thus blocking the blood flow to the heart. This results in extensive damage of
areas around the heart compared to the non-STEMI which damages a small area of the heart
(Dong et al., 2015).
Question 2b: Two risk factors of Acute Coronary Syndrome
1. Past medical history of Coronary Heart Disease
2. History of Type 2 Diabetes Mellitus and hypertension
Question 3: ECG interpretation
The ECG is irregular and has a slow rate. The ECG shows transient elevation of the
T-segment, depression of the ST segment, and inversion of the T wave. P waves are present,
but they are irregular. The presence of the ST depression and elevation of the T segment are
an indication of the possibility of myocardial infarction and cardiac ischemia. The STEMI is
referred to as current injury which is indicated by the occurrence of presumed or new
elevation of the ST segment as shown in the ECG in more than two continuous leads.
In the ECG, the ST elevation is greater than 0.2 mV in the leads V1, V2, and V3 and
its greater than 0.1 mV in the subsequent leads. As per the ECG, the patient has usually an
ongoing occlusion of the epicardial Coronary Artery which requires consideration for an
urgent immediate therapy for reperfusion. The presence of the significant Q waves which are
greater than 0.04 seconds and a quarter of the height of the R wavs is an indication of
myocardial infarction. The small and isolated Q waves in the leads II, aVF, and III and the
leads aVL and I are normal. Due to the origin of the first vector in the ventricular
depolarization, the small Q waves are referred to as “Septal Q waves”. Regarding rhythm, the
ECG has various abnormalities which are termed as arrhythmias due to the presence of
heart. STEMI is the most severe heart attack which is caused by total occlusion of the arteries
by a thrombus thus blocking the blood flow to the heart. This results in extensive damage of
areas around the heart compared to the non-STEMI which damages a small area of the heart
(Dong et al., 2015).
Question 2b: Two risk factors of Acute Coronary Syndrome
1. Past medical history of Coronary Heart Disease
2. History of Type 2 Diabetes Mellitus and hypertension
Question 3: ECG interpretation
The ECG is irregular and has a slow rate. The ECG shows transient elevation of the
T-segment, depression of the ST segment, and inversion of the T wave. P waves are present,
but they are irregular. The presence of the ST depression and elevation of the T segment are
an indication of the possibility of myocardial infarction and cardiac ischemia. The STEMI is
referred to as current injury which is indicated by the occurrence of presumed or new
elevation of the ST segment as shown in the ECG in more than two continuous leads.
In the ECG, the ST elevation is greater than 0.2 mV in the leads V1, V2, and V3 and
its greater than 0.1 mV in the subsequent leads. As per the ECG, the patient has usually an
ongoing occlusion of the epicardial Coronary Artery which requires consideration for an
urgent immediate therapy for reperfusion. The presence of the significant Q waves which are
greater than 0.04 seconds and a quarter of the height of the R wavs is an indication of
myocardial infarction. The small and isolated Q waves in the leads II, aVF, and III and the
leads aVL and I are normal. Due to the origin of the first vector in the ventricular
depolarization, the small Q waves are referred to as “Septal Q waves”. Regarding rhythm, the
ECG has various abnormalities which are termed as arrhythmias due to the presence of
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
ACUTE CORONARY SYNDROME 5
transient elevation of the T-segment, inversion of the T wave, depression of the ST segment,
and presence of irregular P waves.
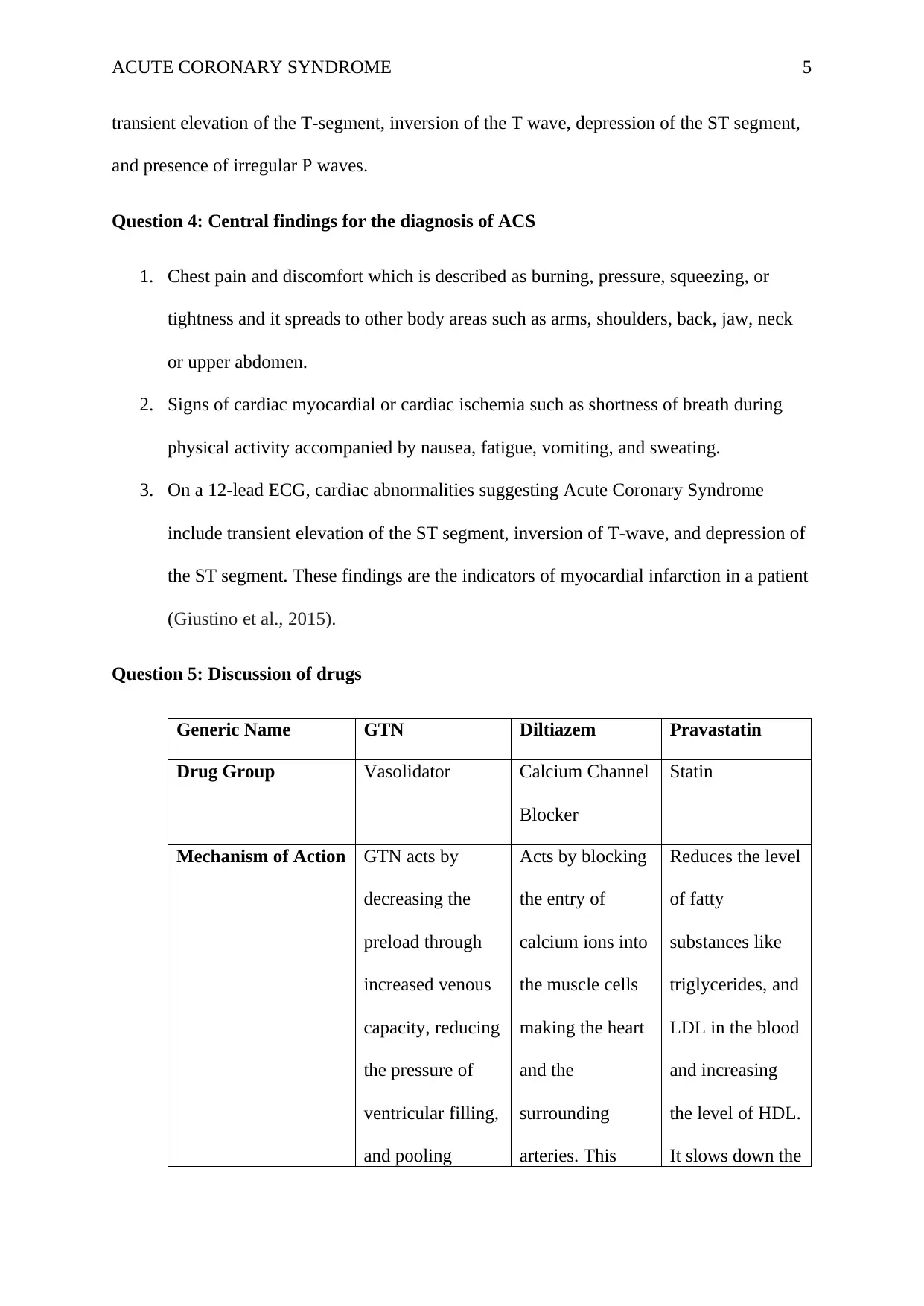
Question 4: Central findings for the diagnosis of ACS
1. Chest pain and discomfort which is described as burning, pressure, squeezing, or
tightness and it spreads to other body areas such as arms, shoulders, back, jaw, neck
or upper abdomen.
2. Signs of cardiac myocardial or cardiac ischemia such as shortness of breath during
physical activity accompanied by nausea, fatigue, vomiting, and sweating.
3. On a 12-lead ECG, cardiac abnormalities suggesting Acute Coronary Syndrome
include transient elevation of the ST segment, inversion of T-wave, and depression of
the ST segment. These findings are the indicators of myocardial infarction in a patient
(Giustino et al., 2015).
Question 5: Discussion of drugs
Generic Name GTN Diltiazem Pravastatin
Drug Group Vasolidator Calcium Channel
Blocker
Statin
Mechanism of Action GTN acts by
decreasing the
preload through
increased venous
capacity, reducing
the pressure of
ventricular filling,
and pooling
Acts by blocking
the entry of
calcium ions into
the muscle cells
making the heart
and the
surrounding
arteries. This
Reduces the level
of fatty
substances like
triglycerides, and
LDL in the blood
and increasing
the level of HDL.
It slows down the
transient elevation of the T-segment, inversion of the T wave, depression of the ST segment,
and presence of irregular P waves.
Question 4: Central findings for the diagnosis of ACS
1. Chest pain and discomfort which is described as burning, pressure, squeezing, or
tightness and it spreads to other body areas such as arms, shoulders, back, jaw, neck
or upper abdomen.
2. Signs of cardiac myocardial or cardiac ischemia such as shortness of breath during
physical activity accompanied by nausea, fatigue, vomiting, and sweating.
3. On a 12-lead ECG, cardiac abnormalities suggesting Acute Coronary Syndrome
include transient elevation of the ST segment, inversion of T-wave, and depression of
the ST segment. These findings are the indicators of myocardial infarction in a patient
(Giustino et al., 2015).
Question 5: Discussion of drugs
Generic Name GTN Diltiazem Pravastatin
Drug Group Vasolidator Calcium Channel
Blocker
Statin
Mechanism of Action GTN acts by
decreasing the
preload through
increased venous
capacity, reducing
the pressure of
ventricular filling,
and pooling
Acts by blocking
the entry of
calcium ions into
the muscle cells
making the heart
and the
surrounding
arteries. This
Reduces the level
of fatty
substances like
triglycerides, and
LDL in the blood
and increasing
the level of HDL.
It slows down the
ACUTE CORONARY SYNDROME 6
venous of the
peripheral veins,
and decreasing
afterload. GTN
also results in the
vasodilation of the
coronary arteries
and redistributing
the flow of blood
in the collateral
channels located
in the heart
(Kaddurah‐Daouk
& Weinshilboum,
2014).
decreases the rate
and force of
contraction of the
heart. Diltiazem
also facilitates
the relaxation of
the surrounding
arteries thus
allowing
dilatation and
reducing the
pressure on the
arteries for
pumping.
Consequently,
this reduces the
oxygen demand
for the heart
since it is
performing less
work (Kaddurah‐
Daouk &
Weinshilboum,
2014).
production of
cholesterol by the
liver to prevent
deposition and
accumulation of
fatty substances
in the walls of
the arteries thus
reducing the risk
of blockage
which may cause
cardiac ischemia
and angina
(Katzung, 2017).
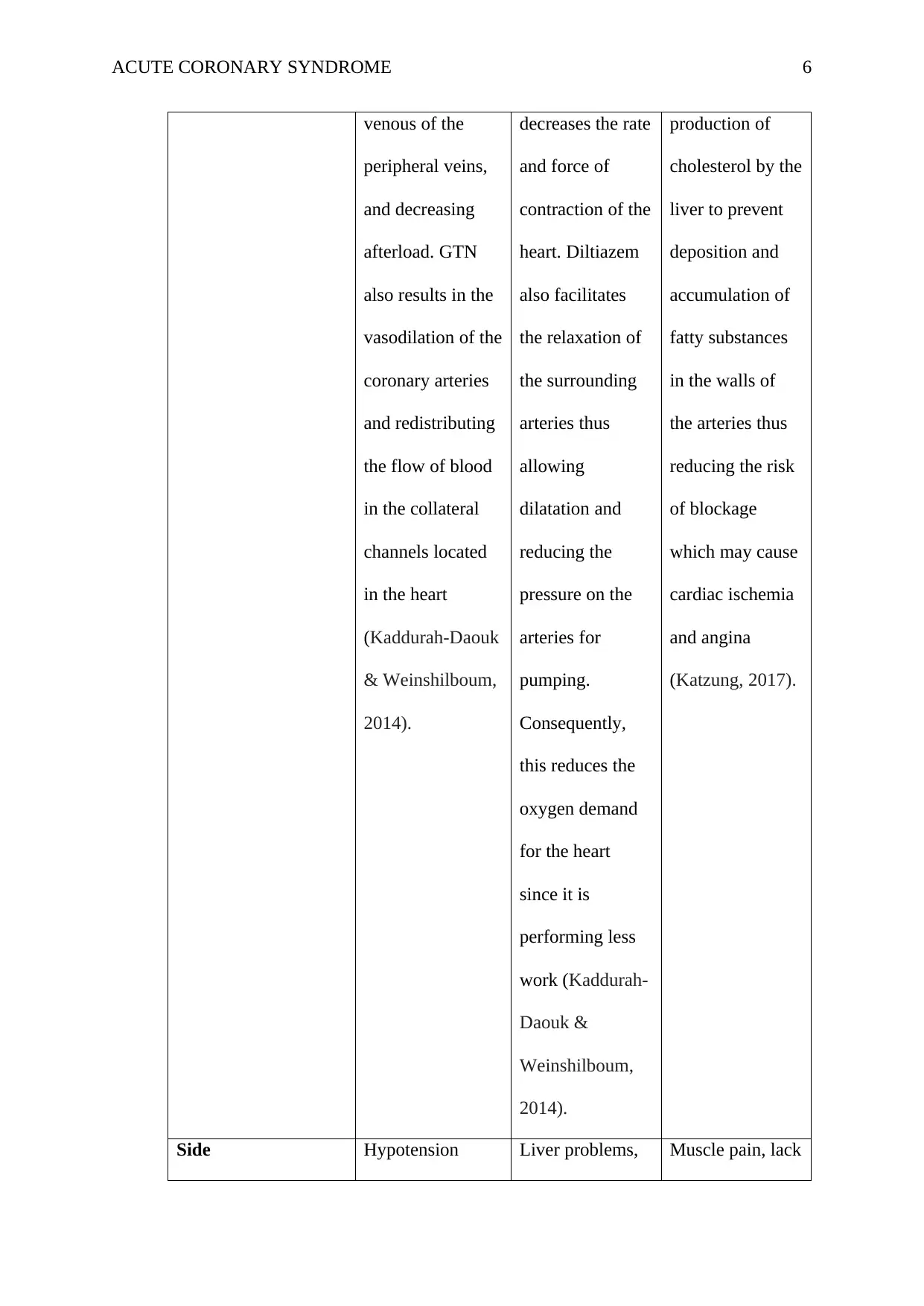
Side Hypotension Liver problems, Muscle pain, lack
venous of the
peripheral veins,
and decreasing
afterload. GTN
also results in the
vasodilation of the
coronary arteries
and redistributing
the flow of blood
in the collateral
channels located
in the heart
(Kaddurah‐Daouk
& Weinshilboum,
2014).
decreases the rate
and force of
contraction of the
heart. Diltiazem
also facilitates
the relaxation of
the surrounding
arteries thus
allowing
dilatation and
reducing the
pressure on the
arteries for
pumping.
Consequently,
this reduces the
oxygen demand
for the heart
since it is
performing less
work (Kaddurah‐
Daouk &
Weinshilboum,
2014).
production of
cholesterol by the
liver to prevent
deposition and
accumulation of
fatty substances
in the walls of
the arteries thus
reducing the risk
of blockage
which may cause
cardiac ischemia
and angina
(Katzung, 2017).
Side Hypotension Liver problems, Muscle pain, lack
ACUTE CORONARY SYNDROME 7
effects/Complication
s
Circulatory
collapse
Reflex
tachycardia
Vascular
headaches
slow pulse rate of energy,
yellowing of the
eyes or the skin,
difficulty
swallowing and
breathing
Nursing
Considerations
Close monitoring
of the blood
pressure
Assessing the
patient for other
contraindications
like intoxication,
cerebral vascular
disease, and risk
of hypotension
(Roffi et al.,
2016).
Monitoring the
patient for
reduced pulse
rate
Assessing and
taking the
patient's history
before
administration to
rule out the
hypersensitivity
reactions
(Katzung, 2017).
The nurse should
monitor the
patient for
hypersensitivity
reactions
The nurse should
ensure proper
administer the
drug using the
right dose, route,
and time to
ensure efficiency
(Bos-Touwen et
al.,2015).
Question 6: Mechanism of Action and Use of Ticagrelor and Aspirin in cardiac patients.
The aspirin has antithrombotic action which is essential in the inhibition of the
activation and aggregation of the platelets thus preventing blood clotting. It prevents the
formation of the thrombi which may partially or entirely occlude the coronary arteries
effects/Complication
s
Circulatory
collapse
Reflex
tachycardia
Vascular
headaches
slow pulse rate of energy,
yellowing of the
eyes or the skin,
difficulty
swallowing and
breathing
Nursing
Considerations
Close monitoring
of the blood
pressure
Assessing the
patient for other
contraindications
like intoxication,
cerebral vascular
disease, and risk
of hypotension
(Roffi et al.,
2016).
Monitoring the
patient for
reduced pulse
rate
Assessing and
taking the
patient's history
before
administration to
rule out the
hypersensitivity
reactions
(Katzung, 2017).
The nurse should
monitor the
patient for
hypersensitivity
reactions
The nurse should
ensure proper
administer the
drug using the
right dose, route,
and time to
ensure efficiency
(Bos-Touwen et
al.,2015).
Question 6: Mechanism of Action and Use of Ticagrelor and Aspirin in cardiac patients.
The aspirin has antithrombotic action which is essential in the inhibition of the
activation and aggregation of the platelets thus preventing blood clotting. It prevents the
formation of the thrombi which may partially or entirely occlude the coronary arteries
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ACUTE CORONARY SYNDROME 8
resulting in STEMI or non-STEMI myocardial infarction which are the principal causes of
Coronary Heart Disease and ACS. Ticagrelor is regarded as an antiplatelet drug that is used
in the reduction of the rate of the thrombotic cardiovascular instances in a patient with ACS.
It is used in reducing the rates of stent thrombosis in a patient who has been stented for the
treatment of ACS. Both aspirin and ticagrelor can be effectively used to prevent the
formation of blood clots and the thrombotic events in the patient with cardiac problems for a
reasonable prognosis of the disease (Katzung, 2017).
Question 7: Use of Morphine in ACS
Morphine has an analgesic effect which makes it a beneficial drug in the management
of chest in patients with STEMI. This ensures the comfort of the patient through pain relief.
Despite this, morphine has controversies associated with its use in cardiac patients. The
current controversies are concerned with the routine use of the drug due to the potential
concerns of patient safety (McCarthy, Bhambhani, Pomerantsev, & Wasfy, 2018). The
routine use of morphine has been associated with a high risk of an in-hospital type of
mortality, platelet reactivity, and Major Adverse Cardiovascular events like heart failure,
cardiovascular mortality, myocardial infarction, cardiogenic shock, bleeding, stroke, and
unstable angina. Morphine is also associated with the reduction of the antiplatelet effect of
the platelet inhibitors. Other safety concerns include the adverse events induced by morphine
such as nausea, bleeding, emesis, hypotension, bradycardia, and respiratory insufficiency
(Bonin et al., 2018).
Question 8: Depression and Coronary Heart Disease
In accordance with the case scenario, Betsy shows an increased risk of depression.
CHD impacts mainly on the patient's state of health due to its manifestations, medication
regimens, and outcomes (Sanchis-Gomar, Perez-Quilis, Leischik, & Lucia, 2016). The patient
resulting in STEMI or non-STEMI myocardial infarction which are the principal causes of
Coronary Heart Disease and ACS. Ticagrelor is regarded as an antiplatelet drug that is used
in the reduction of the rate of the thrombotic cardiovascular instances in a patient with ACS.
It is used in reducing the rates of stent thrombosis in a patient who has been stented for the
treatment of ACS. Both aspirin and ticagrelor can be effectively used to prevent the
formation of blood clots and the thrombotic events in the patient with cardiac problems for a
reasonable prognosis of the disease (Katzung, 2017).
Question 7: Use of Morphine in ACS
Morphine has an analgesic effect which makes it a beneficial drug in the management
of chest in patients with STEMI. This ensures the comfort of the patient through pain relief.
Despite this, morphine has controversies associated with its use in cardiac patients. The
current controversies are concerned with the routine use of the drug due to the potential
concerns of patient safety (McCarthy, Bhambhani, Pomerantsev, & Wasfy, 2018). The
routine use of morphine has been associated with a high risk of an in-hospital type of
mortality, platelet reactivity, and Major Adverse Cardiovascular events like heart failure,
cardiovascular mortality, myocardial infarction, cardiogenic shock, bleeding, stroke, and
unstable angina. Morphine is also associated with the reduction of the antiplatelet effect of
the platelet inhibitors. Other safety concerns include the adverse events induced by morphine
such as nausea, bleeding, emesis, hypotension, bradycardia, and respiratory insufficiency
(Bonin et al., 2018).
Question 8: Depression and Coronary Heart Disease
In accordance with the case scenario, Betsy shows an increased risk of depression.
CHD impacts mainly on the patient's state of health due to its manifestations, medication
regimens, and outcomes (Sanchis-Gomar, Perez-Quilis, Leischik, & Lucia, 2016). The patient
ACUTE CORONARY SYNDROME 9
may develop feelings of hopelessness, worthlessness, and unhappiness due to her health
condition thus increasing the risk of development of depression. Medical conditions such as
CHD have emotional and psychological trauma to the patient due to its manifestations such
as chest pain, shortness of breath, nausea, fatigue, sweating, and heart attack. The medication
regimens and anxiety may make the patient develop depression since she may not be able to
tolerate them (Lichtman et al., 2014).
Conclusion
The paper has provided an interpretation of Betsy’s ECG and the pathophysiology of
angina and two major risk factors for the development of ACS concerning the case scenario.
The paper has provided three central findings which are useful in the differential diagnosis of
ACS and the mechanisms of action, side effects, and nursing considerations for GTN,
Diltiazem, and Pravastatin. The paper has discussed, the use of Ticagrelor, Aspirin, and
Morphine in cardiac patients including the controversies associated with the use of morphine.
Lastly, the paper has addressed the linkage between CHD and increased risk for the
development of depression.
References
may develop feelings of hopelessness, worthlessness, and unhappiness due to her health
condition thus increasing the risk of development of depression. Medical conditions such as
CHD have emotional and psychological trauma to the patient due to its manifestations such
as chest pain, shortness of breath, nausea, fatigue, sweating, and heart attack. The medication
regimens and anxiety may make the patient develop depression since she may not be able to
tolerate them (Lichtman et al., 2014).
Conclusion
The paper has provided an interpretation of Betsy’s ECG and the pathophysiology of
angina and two major risk factors for the development of ACS concerning the case scenario.
The paper has provided three central findings which are useful in the differential diagnosis of
ACS and the mechanisms of action, side effects, and nursing considerations for GTN,
Diltiazem, and Pravastatin. The paper has discussed, the use of Ticagrelor, Aspirin, and
Morphine in cardiac patients including the controversies associated with the use of morphine.
Lastly, the paper has addressed the linkage between CHD and increased risk for the
development of depression.
References
ACUTE CORONARY SYNDROME 10
Amsterdam, E. A., Wenger, N. K., Brindis, R. G., Casey, D. E., Ganiats, T. G., Holmes, D.
R., ... & Levine, G. N. (2014). 2014 AHA/ACC guideline for the management of
patients with non–ST-elevation acute coronary syndromes: a report of the American
College of Cardiology/American Heart Association Task Force on Practice
Guidelines. Journal of the American College of Cardiology, 64(24), e139-e228.
Bonin, M., Mewton, N., Roubille, F., Morel, O., Cayla, G., Angoulvant, D., ... & Rioufol, G.
(2018). Effect and Safety of Morphine Use in Acute Anterior ST‐Segment Elevation
Myocardial Infarction. Journal of the American Heart Association, 7(4), e006833.
Bos-Touwen, I., Schuurmans, M., Monninkhof, E. M., Korpershoek, Y., Spruit-Bentvelzen,
L., Ertugrul-van der Graaf, I., ... & Trappenburg, J. (2015). Patient and disease
characteristics associated with activation for self-management in patients with
diabetes, chronic obstructive pulmonary disease, chronic heart failure, and chronic
renal disease: a cross-sectional survey study. PloS one, 10(5), e0126400.
Dong, L., Mintz, G. S., Witzenbichler, B., Metzger, D. C., Rinaldi, M. J., Duffy, P. L., ... &
Xu, K. (2015). Comparison of plaque characteristics in narrowings with ST-elevation
myocardial infarction (STEMI), non-STEMI/unstable angina pectoris and stable
coronary artery disease (from the ADAPT-DES IVUS Substudy). The American
journal of cardiology, 115(7), 860-866.
Ford, T. J., Corcoran, D., & Berry, C. (2018). Stable coronary syndromes: pathophysiology,
diagnostic advances, and therapeutic need. Heart, 104(4), 284-292.
Fors, A., Ekman, I., Taft, C., Bjorkelund, C., Frid, K., Larsson, M. E., ... & Swedberg, K.
(2015). Person-centered care after acute coronary syndrome, from hospital to primary
care—a randomized controlled trial. International journal of cardiology, 187, 693-
699.
Amsterdam, E. A., Wenger, N. K., Brindis, R. G., Casey, D. E., Ganiats, T. G., Holmes, D.
R., ... & Levine, G. N. (2014). 2014 AHA/ACC guideline for the management of
patients with non–ST-elevation acute coronary syndromes: a report of the American
College of Cardiology/American Heart Association Task Force on Practice
Guidelines. Journal of the American College of Cardiology, 64(24), e139-e228.
Bonin, M., Mewton, N., Roubille, F., Morel, O., Cayla, G., Angoulvant, D., ... & Rioufol, G.
(2018). Effect and Safety of Morphine Use in Acute Anterior ST‐Segment Elevation
Myocardial Infarction. Journal of the American Heart Association, 7(4), e006833.
Bos-Touwen, I., Schuurmans, M., Monninkhof, E. M., Korpershoek, Y., Spruit-Bentvelzen,
L., Ertugrul-van der Graaf, I., ... & Trappenburg, J. (2015). Patient and disease
characteristics associated with activation for self-management in patients with
diabetes, chronic obstructive pulmonary disease, chronic heart failure, and chronic
renal disease: a cross-sectional survey study. PloS one, 10(5), e0126400.
Dong, L., Mintz, G. S., Witzenbichler, B., Metzger, D. C., Rinaldi, M. J., Duffy, P. L., ... &
Xu, K. (2015). Comparison of plaque characteristics in narrowings with ST-elevation
myocardial infarction (STEMI), non-STEMI/unstable angina pectoris and stable
coronary artery disease (from the ADAPT-DES IVUS Substudy). The American
journal of cardiology, 115(7), 860-866.
Ford, T. J., Corcoran, D., & Berry, C. (2018). Stable coronary syndromes: pathophysiology,
diagnostic advances, and therapeutic need. Heart, 104(4), 284-292.
Fors, A., Ekman, I., Taft, C., Bjorkelund, C., Frid, K., Larsson, M. E., ... & Swedberg, K.
(2015). Person-centered care after acute coronary syndrome, from hospital to primary
care—a randomized controlled trial. International journal of cardiology, 187, 693-
699.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
ACUTE CORONARY SYNDROME 11
Giustino, G., Baber, U., Stefanini, G. G., Aquino, M., Stone, G. W., Sartori, S., ... & Leon,
M. B. (2015). Impact of Clinical Presentation (Stable Angina Pectoris vs. Unstable
Angina Pectoris or Non–ST-Elevation Myocardial Infarction vs. ST-Elevation
Myocardial Infarction) on Long-Term Outcomes in Women Undergoing Percutaneous
Coronary Intervention With Drug-Eluting Stents. The American journal of
cardiology, 116(6), 845-852.
Kaddurah‐Daouk, R., & Weinshilboum, R. M. (2014). Pharmacometabolomics: implications
for clinical pharmacology and systems pharmacology. Clinical Pharmacology &
Therapeutics, 95(2), 154-167.
Katzung, B. G. (2017). Basic and clinical pharmacology. McGraw-Hill Education.
Lewis, S. M., Collier, I. C., & Heitkemper, M. M. (2017). Medical-surgical nursing:
assessment and management of clinical problems. Elsevier, Incorporated.
Lichtman, J. H., Froelicher, E. S., Blumenthal, J. A., Carney, R. M., Doering, L. V., Frasure-
Smith, N., ... & Vaccarino, V. (2014). Depression as a risk factor for poor prognosis
among patients with acute coronary syndrome: systematic review and
recommendations: a scientific statement from the American Heart
Association. Circulation, 129(12), 1350-1369.
McCarthy, C. P., Bhambhani, V., Pomerantsev, E., & Wasfy, J. H. (2018). In‐hospital
outcomes in invasively managed acute myocardial infarction patients who receive
morphine. Journal of interventional cardiology, 31(2), 150-158.
Niccoli, G., Montone, R. A., Lanza, G. A., & Crea, F. (2017). Angina after percutaneous
coronary intervention: The need for precision medicine. International journal of
cardiology, 248, 14-19.
Giustino, G., Baber, U., Stefanini, G. G., Aquino, M., Stone, G. W., Sartori, S., ... & Leon,
M. B. (2015). Impact of Clinical Presentation (Stable Angina Pectoris vs. Unstable
Angina Pectoris or Non–ST-Elevation Myocardial Infarction vs. ST-Elevation
Myocardial Infarction) on Long-Term Outcomes in Women Undergoing Percutaneous
Coronary Intervention With Drug-Eluting Stents. The American journal of
cardiology, 116(6), 845-852.
Kaddurah‐Daouk, R., & Weinshilboum, R. M. (2014). Pharmacometabolomics: implications
for clinical pharmacology and systems pharmacology. Clinical Pharmacology &
Therapeutics, 95(2), 154-167.
Katzung, B. G. (2017). Basic and clinical pharmacology. McGraw-Hill Education.
Lewis, S. M., Collier, I. C., & Heitkemper, M. M. (2017). Medical-surgical nursing:
assessment and management of clinical problems. Elsevier, Incorporated.
Lichtman, J. H., Froelicher, E. S., Blumenthal, J. A., Carney, R. M., Doering, L. V., Frasure-
Smith, N., ... & Vaccarino, V. (2014). Depression as a risk factor for poor prognosis
among patients with acute coronary syndrome: systematic review and
recommendations: a scientific statement from the American Heart
Association. Circulation, 129(12), 1350-1369.
McCarthy, C. P., Bhambhani, V., Pomerantsev, E., & Wasfy, J. H. (2018). In‐hospital
outcomes in invasively managed acute myocardial infarction patients who receive
morphine. Journal of interventional cardiology, 31(2), 150-158.
Niccoli, G., Montone, R. A., Lanza, G. A., & Crea, F. (2017). Angina after percutaneous
coronary intervention: The need for precision medicine. International journal of
cardiology, 248, 14-19.
ACUTE CORONARY SYNDROME 12
Radico, F., Cicchitti, V., Zimarino, M., & De Caterina, R. (2014). Angina pectoris and
myocardial ischemia in the absence of obstructive coronary artery disease: practical
considerations for diagnostic tests. JACC: Cardiovascular Interventions, 7(5), 453-
463.
Roffi, M., Patrono, C., Collet, J. P., Mueller, C., Valgimigli, M., Andreotti, F., ... & Gencer,
B. (2016). 2015 ESC Guidelines for the management of acute coronary syndromes in
patients presenting without persistent ST-segment elevation: Task Force for the
Management of Acute Coronary Syndromes in Patients Presenting without Persistent
ST-Segment Elevation of the European Society of Cardiology (ESC). European heart
journal, 37(3), 267-315.
Sanchis-Gomar, F., Perez-Quilis, C., Leischik, R., & Lucia, A. (2016). Epidemiology of
coronary heart disease and acute coronary syndrome. Annals of translational
medicine, 4(13).
Santos-Gallego, C. G., Picatoste, B., & Badimon, J. J. (2014). Pathophysiology of the acute
coronary syndrome. Current atherosclerosis reports, 16(4), 401.
Radico, F., Cicchitti, V., Zimarino, M., & De Caterina, R. (2014). Angina pectoris and
myocardial ischemia in the absence of obstructive coronary artery disease: practical
considerations for diagnostic tests. JACC: Cardiovascular Interventions, 7(5), 453-
463.
Roffi, M., Patrono, C., Collet, J. P., Mueller, C., Valgimigli, M., Andreotti, F., ... & Gencer,
B. (2016). 2015 ESC Guidelines for the management of acute coronary syndromes in
patients presenting without persistent ST-segment elevation: Task Force for the
Management of Acute Coronary Syndromes in Patients Presenting without Persistent
ST-Segment Elevation of the European Society of Cardiology (ESC). European heart
journal, 37(3), 267-315.
Sanchis-Gomar, F., Perez-Quilis, C., Leischik, R., & Lucia, A. (2016). Epidemiology of
coronary heart disease and acute coronary syndrome. Annals of translational
medicine, 4(13).
Santos-Gallego, C. G., Picatoste, B., & Badimon, J. J. (2014). Pathophysiology of the acute
coronary syndrome. Current atherosclerosis reports, 16(4), 401.
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





