Mrs. Brown's Case Study: Acute Exacerbation of Chronic Conditions
VerifiedAdded on 2022/10/02
|10
|1944
|88
Report
AI Summary
This report presents a case study of Mrs. Brown, who experienced an acute exacerbation of chronic heart failure. The report details her symptoms, including severe dyspnea, increased respiratory and pulse rates, low oxygen saturation, and high blood pressure. Through analysis of her vital signs, ECG readings (atrial fibrillation), and auscultation findings (bilateral crackles), the report diagnoses systolic dysfunction and acute decompensated heart failure (ADHF). It explores the pathogenesis of her condition, highlighting the role of increased afterload, reduced cardiac contractility, and tachycardia. The report also examines the patient's journey through the emergency department, emphasizing the importance of nurses in assessing and managing the condition. Finally, it discusses the administered treatments, including sublingual Glyceryl Trinitrate (GTN) and Furosemide (Lasix), and their mechanisms of action in managing the patient's condition.

Running Head: Acute excerbation of chronic conditions 1
Student Name:
Student ID:
Lecturer:
Unit Coordinator:
University:
Acute excerbation of
chronic conditions
HRM
Date: 16/08/2019
Reference Style: APA
Student Name:
Student ID:
Lecturer:
Unit Coordinator:
University:
Acute excerbation of
chronic conditions
HRM
Date: 16/08/2019
Reference Style: APA
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Acute excerbation of chronic conditions 2
Answers to guided questions
Answer 1
To understand the disease of Mrs. Brown, it is important to study and deduce her signs
and symptoms. Mrs. Brown when admitted to the emergency was complaining of severe
dyspnoea. Dyspnoea is the medical term for shortness of breath and can be caused by heart
failure (Zannad, McMurray, Krum, van Veldhuisen, et al., 2011). She also had respiratory rate of
24 breaths per minute. For a normal person the respiration rate is 12-20 breaths per minute. An
increased respiratory rate can be an indication of heart failure. The oxyhaemoglobin saturation as
noted through the reading of pulse oximeter is 85%. However, for a normal human being the
SPO2 is between 97% and 99% (WHO, 2011). Therefore a value under 90% is considered too
low and can result in hypoxia. The BP reading of the patient is 170/95 mm Hg. In a normal
human being the reading above 140/90 mm Hg is considered as a case of hyper tension. The
pulse rate which remains between 60 to 80 beats per minute is at 120 beats per minute in Mrs.
Brown. This means that the heart is working extra hard to compensate for the lack of cardiac
output. This is an indication of heart failure. Additionally, auscultation of lungs found bilateral
crackles. Crackles are the medical term of popping open sound of small alveolis and airways that
were collapsed by fluid. Crackles might be caused due to left sided congestive heart failure or
pulmonary edema. Additionally ECG readings demonstrated atrial fibrillation which is
characterised by abnormal beatings of heart and can increase the risk of stroke.
Given the finding of arterial fibrillation along with a history of heart failure in Mrs.
Brown, it is clear that she is suffering from heart failure caused by systolic dysfunction. The fact
that she is getting repeatedly admitted with heart failure along with the feeling of dyspnoea
suggests that her heart performance has been severely impaired. The rapid onset or escalation of
2
Answers to guided questions
Answer 1
To understand the disease of Mrs. Brown, it is important to study and deduce her signs
and symptoms. Mrs. Brown when admitted to the emergency was complaining of severe
dyspnoea. Dyspnoea is the medical term for shortness of breath and can be caused by heart
failure (Zannad, McMurray, Krum, van Veldhuisen, et al., 2011). She also had respiratory rate of
24 breaths per minute. For a normal person the respiration rate is 12-20 breaths per minute. An
increased respiratory rate can be an indication of heart failure. The oxyhaemoglobin saturation as
noted through the reading of pulse oximeter is 85%. However, for a normal human being the
SPO2 is between 97% and 99% (WHO, 2011). Therefore a value under 90% is considered too
low and can result in hypoxia. The BP reading of the patient is 170/95 mm Hg. In a normal
human being the reading above 140/90 mm Hg is considered as a case of hyper tension. The
pulse rate which remains between 60 to 80 beats per minute is at 120 beats per minute in Mrs.
Brown. This means that the heart is working extra hard to compensate for the lack of cardiac
output. This is an indication of heart failure. Additionally, auscultation of lungs found bilateral
crackles. Crackles are the medical term of popping open sound of small alveolis and airways that
were collapsed by fluid. Crackles might be caused due to left sided congestive heart failure or
pulmonary edema. Additionally ECG readings demonstrated atrial fibrillation which is
characterised by abnormal beatings of heart and can increase the risk of stroke.
Given the finding of arterial fibrillation along with a history of heart failure in Mrs.
Brown, it is clear that she is suffering from heart failure caused by systolic dysfunction. The fact
that she is getting repeatedly admitted with heart failure along with the feeling of dyspnoea
suggests that her heart performance has been severely impaired. The rapid onset or escalation of
2
Acute excerbation of chronic conditions 3
the symptoms related to heart failure in Mrs. Brown indicates that she is presented with acute
decompensated HF (ADHF). The pathogenesis of her condition is presented below-
Mrs. Brown’s Bp readings indicated that her systolic pressure was 170 as against the
normal range of systolic pressure between 120-139. Thus she can be said to be suffering from
systolic dysfunction. Systole is referred to as the contraction of the ventricle. In order to
understand the underlying condition of Mrs. Brown that has led to her current condition it is
important to consider afterload.
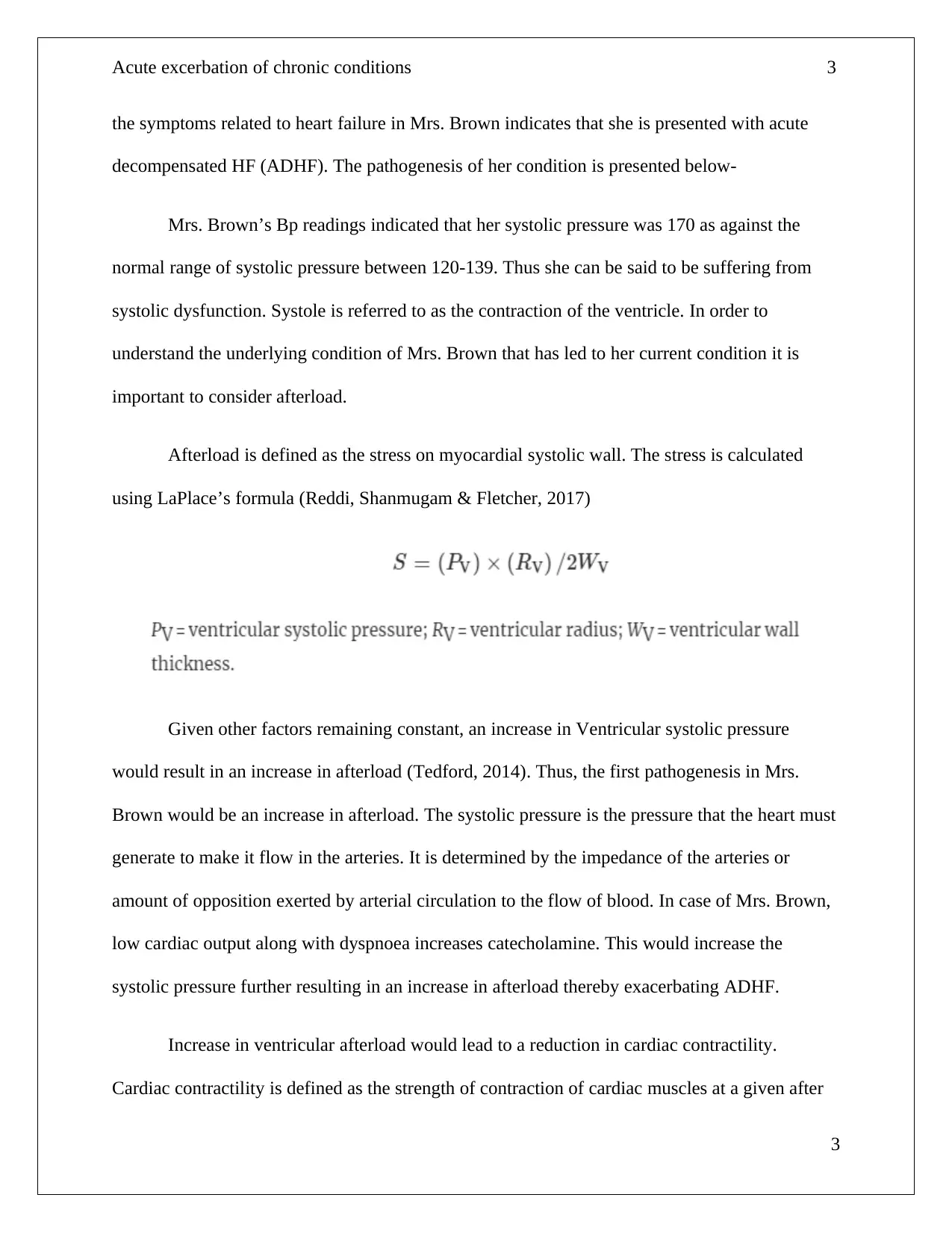
Afterload is defined as the stress on myocardial systolic wall. The stress is calculated
using LaPlace’s formula (Reddi, Shanmugam & Fletcher, 2017)
Given other factors remaining constant, an increase in Ventricular systolic pressure
would result in an increase in afterload (Tedford, 2014). Thus, the first pathogenesis in Mrs.
Brown would be an increase in afterload. The systolic pressure is the pressure that the heart must
generate to make it flow in the arteries. It is determined by the impedance of the arteries or
amount of opposition exerted by arterial circulation to the flow of blood. In case of Mrs. Brown,
low cardiac output along with dyspnoea increases catecholamine. This would increase the
systolic pressure further resulting in an increase in afterload thereby exacerbating ADHF.
Increase in ventricular afterload would lead to a reduction in cardiac contractility.
Cardiac contractility is defined as the strength of contraction of cardiac muscles at a given after
3
the symptoms related to heart failure in Mrs. Brown indicates that she is presented with acute
decompensated HF (ADHF). The pathogenesis of her condition is presented below-
Mrs. Brown’s Bp readings indicated that her systolic pressure was 170 as against the
normal range of systolic pressure between 120-139. Thus she can be said to be suffering from
systolic dysfunction. Systole is referred to as the contraction of the ventricle. In order to
understand the underlying condition of Mrs. Brown that has led to her current condition it is
important to consider afterload.
Afterload is defined as the stress on myocardial systolic wall. The stress is calculated
using LaPlace’s formula (Reddi, Shanmugam & Fletcher, 2017)
Given other factors remaining constant, an increase in Ventricular systolic pressure
would result in an increase in afterload (Tedford, 2014). Thus, the first pathogenesis in Mrs.
Brown would be an increase in afterload. The systolic pressure is the pressure that the heart must
generate to make it flow in the arteries. It is determined by the impedance of the arteries or
amount of opposition exerted by arterial circulation to the flow of blood. In case of Mrs. Brown,
low cardiac output along with dyspnoea increases catecholamine. This would increase the
systolic pressure further resulting in an increase in afterload thereby exacerbating ADHF.
Increase in ventricular afterload would lead to a reduction in cardiac contractility.
Cardiac contractility is defined as the strength of contraction of cardiac muscles at a given after
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Acute excerbation of chronic conditions 4
load and preload. Diminishing contractility would reduce the maximal ventricular pressure
attained and also lead to a reduction in the velocity of myocardial contraction. The patient also
has demonstrated an increase in heart rate, a symptom referred to as tachycardia. Tachycardia
can lead to an increase in myocardial demand of oxygen. Reduction in forward flow and
subsequent activation of neurohormones can lead to haemorrhage of the alveoli and oedema.
After the collapsed alveoli gets opened due to flow of blood there is a poping sound referred to
as crackles which is heard through auscultation of lungs. As the Right ventricle has been dilated
due to increase in arterial impediment and consequent increase in RV after load, the left ventricle
preload would decrease thus increasing the risk of diastolic dysfunction as well.
Answer 2
The journey of acute heart failure for the patient starts with an increase in shortness of
breath. As noticed in case of Mrs. Brown, this was accompanied by other symptoms like an
increase in pulse rate, blood pressure, symptoms of oedema etc. The family of Mrs. Brown
referred her to the emergency department after they failed to help her. The onset of the different
symptoms is rapid as was in the case of Mrs. Brown. After being brought into the emergency
department of the hospital, the feeling of shortness of breath worsened for Mrs. Brown.
The emergency department of the hospital normally do not have a nurse who specialises
in care delivery to a acute heart failure patient. Therefore the initial nurse who attends the patient
in emergency department determines the patient history and has to access the severity of the
patient before referring the case to the relevant team.
4
load and preload. Diminishing contractility would reduce the maximal ventricular pressure
attained and also lead to a reduction in the velocity of myocardial contraction. The patient also
has demonstrated an increase in heart rate, a symptom referred to as tachycardia. Tachycardia
can lead to an increase in myocardial demand of oxygen. Reduction in forward flow and
subsequent activation of neurohormones can lead to haemorrhage of the alveoli and oedema.
After the collapsed alveoli gets opened due to flow of blood there is a poping sound referred to
as crackles which is heard through auscultation of lungs. As the Right ventricle has been dilated
due to increase in arterial impediment and consequent increase in RV after load, the left ventricle
preload would decrease thus increasing the risk of diastolic dysfunction as well.
Answer 2
The journey of acute heart failure for the patient starts with an increase in shortness of
breath. As noticed in case of Mrs. Brown, this was accompanied by other symptoms like an
increase in pulse rate, blood pressure, symptoms of oedema etc. The family of Mrs. Brown
referred her to the emergency department after they failed to help her. The onset of the different
symptoms is rapid as was in the case of Mrs. Brown. After being brought into the emergency
department of the hospital, the feeling of shortness of breath worsened for Mrs. Brown.
The emergency department of the hospital normally do not have a nurse who specialises
in care delivery to a acute heart failure patient. Therefore the initial nurse who attends the patient
in emergency department determines the patient history and has to access the severity of the
patient before referring the case to the relevant team.
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Acute excerbation of chronic conditions 5
Such nurses therefore perform an important function of determining the cause of
breathlessness and prompt initiation of therapy that can provide relief to the patient. The key
issues in assessing the heart failure condition in case of Mrs. Brown were
1. Monitoring the respiratory rate to provide an objective measurement of the severity of
dyspnoea
2. Monitoring the systolic and diastolic blood pressure to monitor the haemodynamic
status.
3. Monitoring the heart rate and rhythm through ECG
4. Performing auscultation of lungs to determine Clinical signs of congestion
Thus the first step in taking care of the patient suffering from heart failure would be
determining the underlying cause (Riley, 2015). Identification of the clinical stability of the
patient therefore firms an important initial step in the treatment of the patient and his or her
transfer to appropriate care that he requires.
However, if there is high risk of clinical deterioration in case of the patient, he should
ideally be transferred to the resuscitation area of the emergency care. In the resuscitation area
there is a lower patient to nurse ratio and closer monitoring of the patients. There is more
medical staff to support the decision making on patients in resuscitation area.
The nurses have the duty to manage acute breathlessness or instability of heart with the
diagnosis of the same. After diagnosis of the patient with heart failure the first drugs to be
administered are diuretics. Diuretics help in relieving dyspnoea. The patient should also be made
5
Such nurses therefore perform an important function of determining the cause of
breathlessness and prompt initiation of therapy that can provide relief to the patient. The key
issues in assessing the heart failure condition in case of Mrs. Brown were
1. Monitoring the respiratory rate to provide an objective measurement of the severity of
dyspnoea
2. Monitoring the systolic and diastolic blood pressure to monitor the haemodynamic
status.
3. Monitoring the heart rate and rhythm through ECG
4. Performing auscultation of lungs to determine Clinical signs of congestion
Thus the first step in taking care of the patient suffering from heart failure would be
determining the underlying cause (Riley, 2015). Identification of the clinical stability of the
patient therefore firms an important initial step in the treatment of the patient and his or her
transfer to appropriate care that he requires.
However, if there is high risk of clinical deterioration in case of the patient, he should
ideally be transferred to the resuscitation area of the emergency care. In the resuscitation area
there is a lower patient to nurse ratio and closer monitoring of the patients. There is more
medical staff to support the decision making on patients in resuscitation area.
The nurses have the duty to manage acute breathlessness or instability of heart with the
diagnosis of the same. After diagnosis of the patient with heart failure the first drugs to be
administered are diuretics. Diuretics help in relieving dyspnoea. The patient should also be made
5
Acute excerbation of chronic conditions 6
to sit in a upright position with the legs suspended from the bed. This will lead to a reduction in
preload and gradually alleviate the condition.
Answer 3
The drug that was administered to Mrs. Brown was sublingual Glyceryl Trinitrate (GTN)
and Furosemide (Lasix).
Lasix is a diuretic that helps to eliminate excess fluid which cannot be accommodated by
the heart (Felker, Lee, Bull, Redfield, Stevenson, Goldsmith, et al., 2011). This helps in
improving the stroke volume and decreases the peripheral and pulmonary edema.
Diuretics can help in relieving dyspnoea. However, the dose of a diuretic should the
lowest and sufficient to just remove the congestion. This will help in balancing the negative
effect on renal function with the benefits of the positive action. Administration of diuretic is
followed by close monitoring of fluid balance, renal function and urine output. Sometimes
catheter is inserted to monitor urine output with the administration of diuretic. However, the
insertion of catheter can also lead to infection and therefore care should be taken to ensure that
there is limited risk of infection while insertion of catheter.
Similarly, Glyceryl Trinitrate functions by decreasing preload through venodilation and
thus help in improving the delivery of oxygen to blood. This reduces the heart fatigue and
reduces the chances of a stroke or heart attack.
6
to sit in a upright position with the legs suspended from the bed. This will lead to a reduction in
preload and gradually alleviate the condition.
Answer 3
The drug that was administered to Mrs. Brown was sublingual Glyceryl Trinitrate (GTN)
and Furosemide (Lasix).
Lasix is a diuretic that helps to eliminate excess fluid which cannot be accommodated by
the heart (Felker, Lee, Bull, Redfield, Stevenson, Goldsmith, et al., 2011). This helps in
improving the stroke volume and decreases the peripheral and pulmonary edema.
Diuretics can help in relieving dyspnoea. However, the dose of a diuretic should the
lowest and sufficient to just remove the congestion. This will help in balancing the negative
effect on renal function with the benefits of the positive action. Administration of diuretic is
followed by close monitoring of fluid balance, renal function and urine output. Sometimes
catheter is inserted to monitor urine output with the administration of diuretic. However, the
insertion of catheter can also lead to infection and therefore care should be taken to ensure that
there is limited risk of infection while insertion of catheter.
Similarly, Glyceryl Trinitrate functions by decreasing preload through venodilation and
thus help in improving the delivery of oxygen to blood. This reduces the heart fatigue and
reduces the chances of a stroke or heart attack.
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Acute excerbation of chronic conditions 7
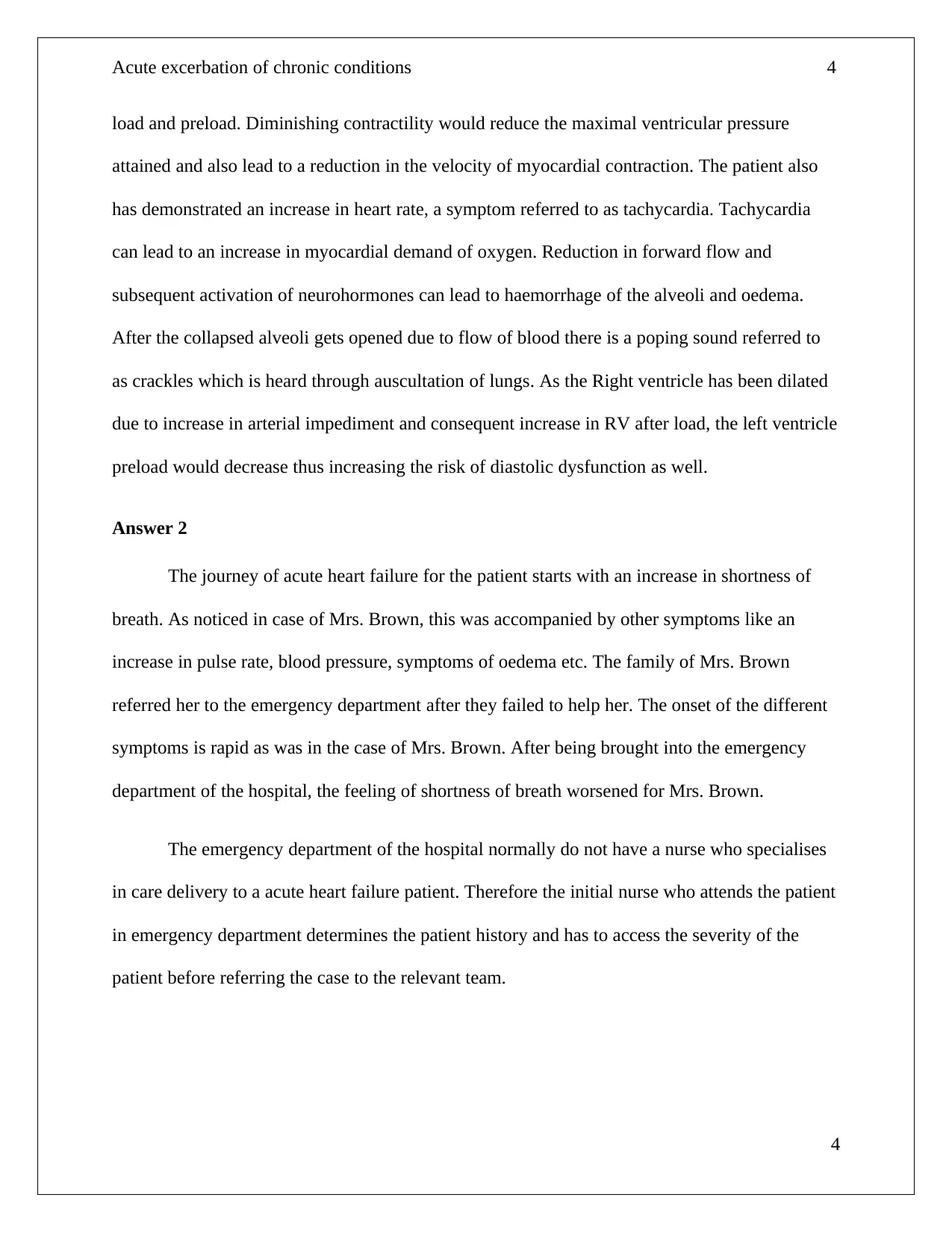
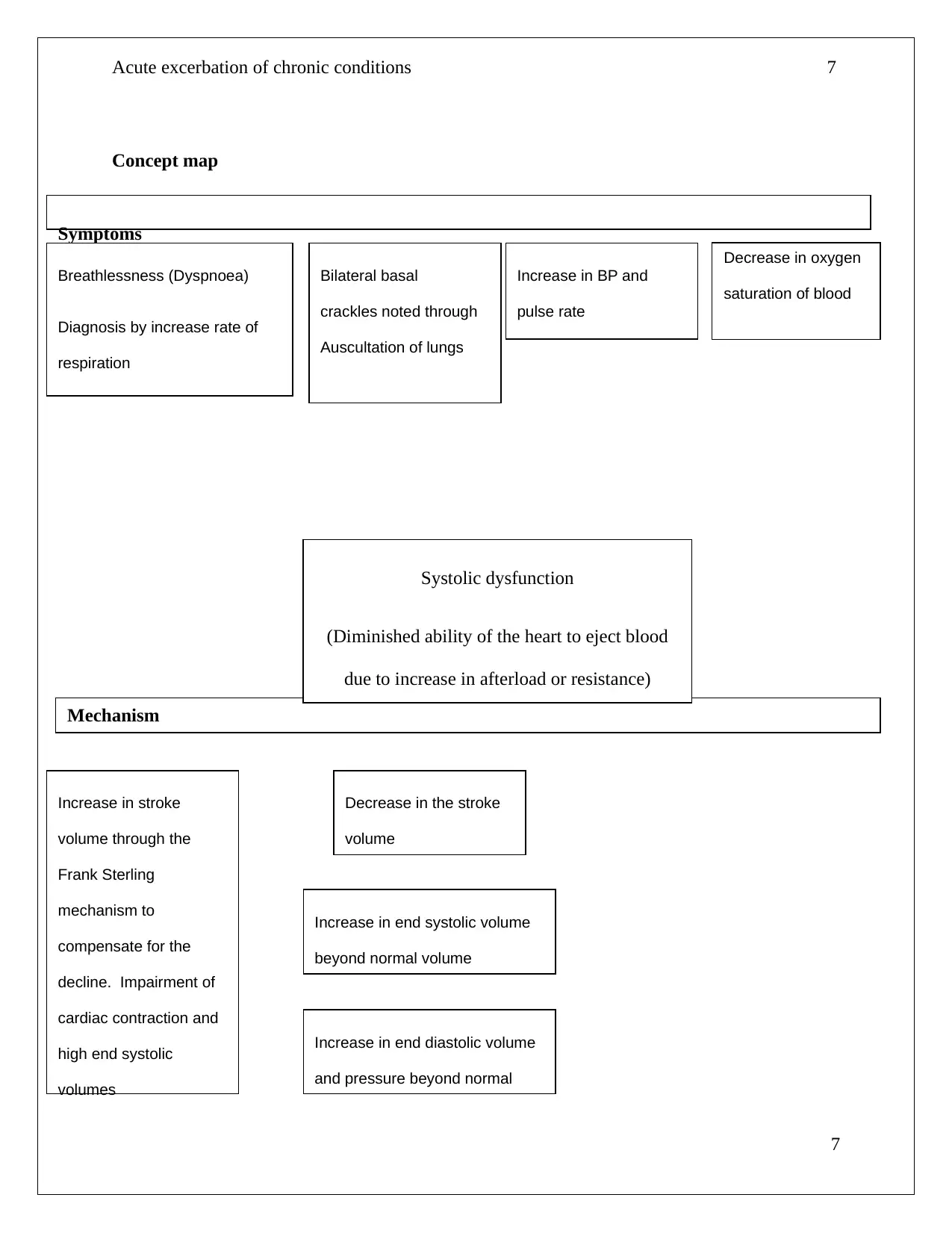
Concept map
7
Decrease in oxygen
saturation of blood
Mechanism
Symptoms
Systolic dysfunction
(Diminished ability of the heart to eject blood
due to increase in afterload or resistance)
Breathlessness (Dyspnoea)
Diagnosis by increase rate of
respiration
Bilateral basal
crackles noted through
Auscultation of lungs
Increase in BP and
pulse rate
Decrease in the stroke
volume
Increase in end systolic volume
beyond normal volume
Increase in end diastolic volume
and pressure beyond normal
Increase in stroke
volume through the
Frank Sterling
mechanism to
compensate for the
decline. Impairment of
cardiac contraction and
high end systolic
volumes
Concept map
7
Decrease in oxygen
saturation of blood
Mechanism
Symptoms
Systolic dysfunction
(Diminished ability of the heart to eject blood
due to increase in afterload or resistance)
Breathlessness (Dyspnoea)
Diagnosis by increase rate of
respiration
Bilateral basal
crackles noted through
Auscultation of lungs
Increase in BP and
pulse rate
Decrease in the stroke
volume
Increase in end systolic volume
beyond normal volume
Increase in end diastolic volume
and pressure beyond normal
Increase in stroke
volume through the
Frank Sterling
mechanism to
compensate for the
decline. Impairment of
cardiac contraction and
high end systolic
volumes
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
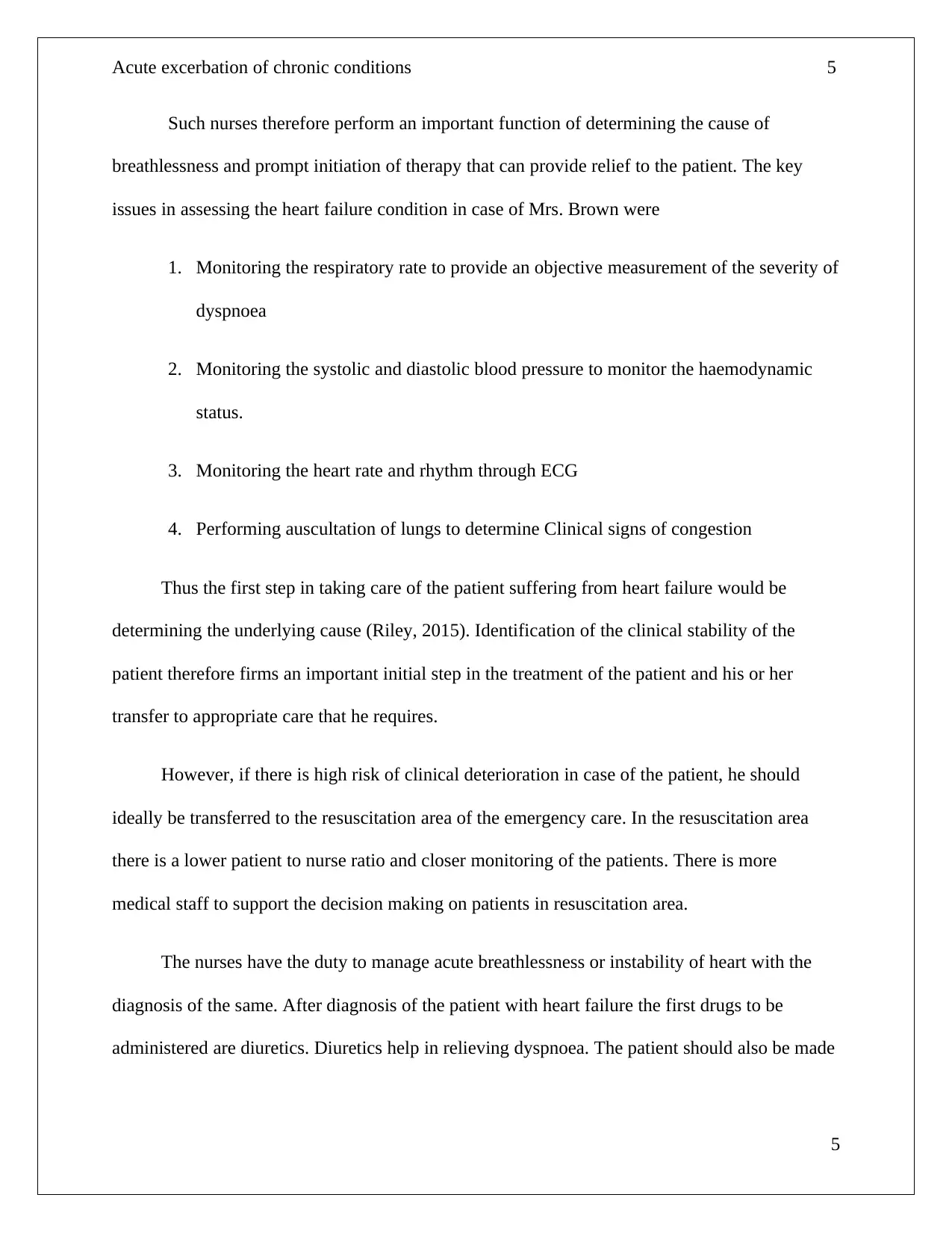
Acute excerbation of chronic conditions 8
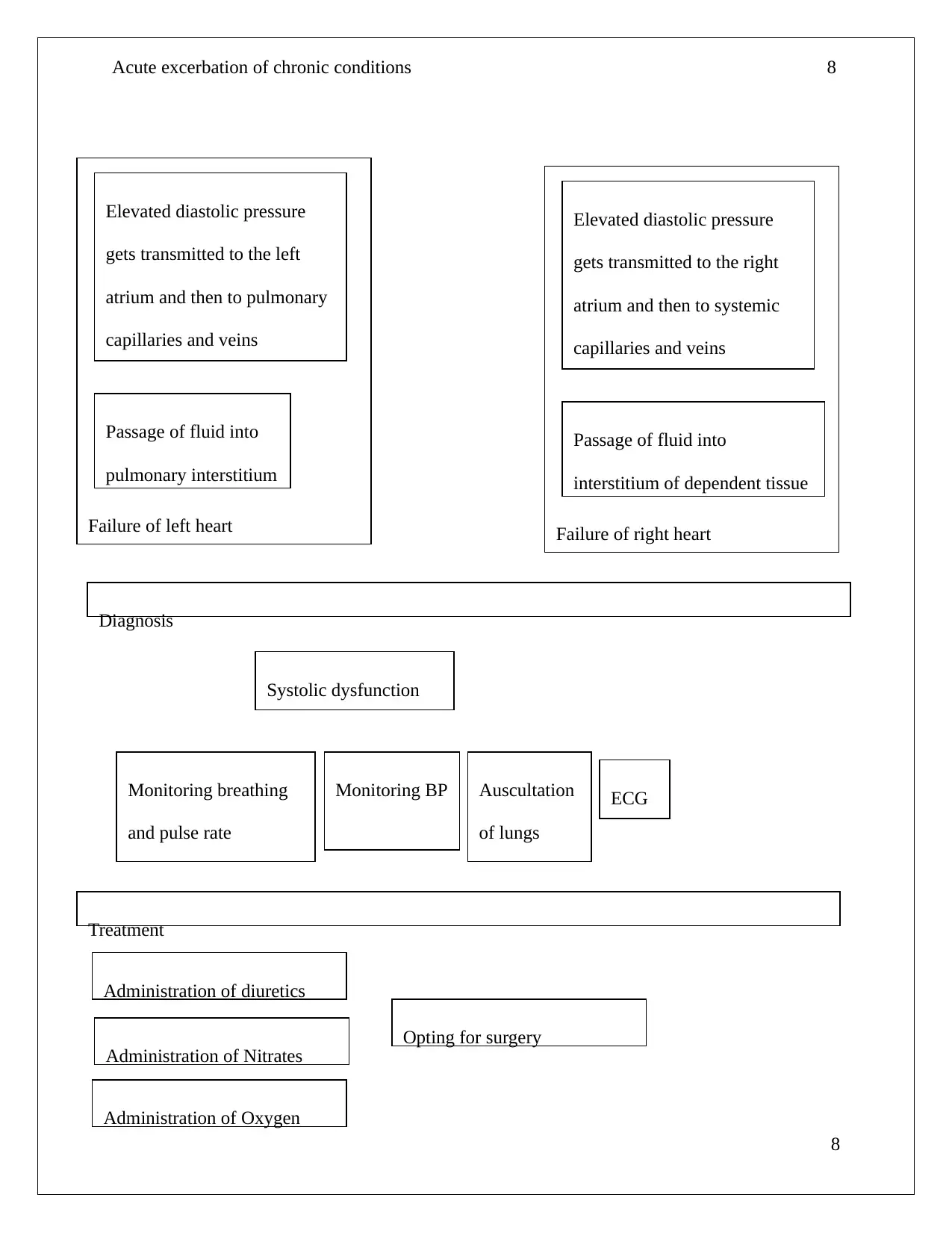
8
Failure of left heart
Elevated diastolic pressure
gets transmitted to the left
atrium and then to pulmonary
capillaries and veins
Passage of fluid into
pulmonary interstitium
Failure of right heart
Elevated diastolic pressure
gets transmitted to the right
atrium and then to systemic
capillaries and veins
Passage of fluid into
interstitium of dependent tissue
Diagnosis
Systolic dysfunction
Monitoring breathing
and pulse rate
Monitoring BP Auscultation
of lungs
ECG
Treatment
Administration of diuretics
Administration of Nitrates
Administration of Oxygen
Opting for surgery
8
Failure of left heart
Elevated diastolic pressure
gets transmitted to the left
atrium and then to pulmonary
capillaries and veins
Passage of fluid into
pulmonary interstitium
Failure of right heart
Elevated diastolic pressure
gets transmitted to the right
atrium and then to systemic
capillaries and veins
Passage of fluid into
interstitium of dependent tissue
Diagnosis
Systolic dysfunction
Monitoring breathing
and pulse rate
Monitoring BP Auscultation
of lungs
ECG
Treatment
Administration of diuretics
Administration of Nitrates
Administration of Oxygen
Opting for surgery
Acute excerbation of chronic conditions 9
9
Prevention
Reducing weight
Minimising intake of sodium
Reducing or ceasing smoking and drinking
Opting for a cholesterol free diet
9
Prevention
Reducing weight
Minimising intake of sodium
Reducing or ceasing smoking and drinking
Opting for a cholesterol free diet
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Acute excerbation of chronic conditions
10
References
Felker, G. M., Lee, K. L., Bull, D. A., Redfield, M. M., Stevenson, L. W., Goldsmith, S. R., ... &
Anstrom, K. J. (2011). Diuretic strategies in patients with acute decompensated heart
failure. New England Journal of Medicine, 364(9), 797-805.
Reddi, B. A. J., Shanmugam, N., & Fletcher, N. (2017). Heart failure—pathophysiology and
inpatient management. Bja Education, 17(5), 151-160.
Riley, J. (2015). The key roles for the nurse in acute heart failure management. Cardiac failure
review, 1(2), 123-127.
Tedford, R. J. (2014). Determinants of right ventricular afterload (2013 Grover Conference
series). Pulmonary circulation, 4(2), 211-219.
WHO. (2011). Pulse Oximetry Training Manual. Retrieved from
https://www.who.int/patientsafety/safesurgery/pulse_oximetry/who_ps_pulse_oxymetry_
training_manual_en.pdf
Zannad, F., McMurray, J. J., Krum, H., van Veldhuisen, D. J., Swedberg, K., Shi, H., ... & Pitt,
B. (2011). Eplerenone in patients with systolic heart failure and mild symptoms. New
England Journal of Medicine, 364(1), 11-21.
10
10
References
Felker, G. M., Lee, K. L., Bull, D. A., Redfield, M. M., Stevenson, L. W., Goldsmith, S. R., ... &
Anstrom, K. J. (2011). Diuretic strategies in patients with acute decompensated heart
failure. New England Journal of Medicine, 364(9), 797-805.
Reddi, B. A. J., Shanmugam, N., & Fletcher, N. (2017). Heart failure—pathophysiology and
inpatient management. Bja Education, 17(5), 151-160.
Riley, J. (2015). The key roles for the nurse in acute heart failure management. Cardiac failure
review, 1(2), 123-127.
Tedford, R. J. (2014). Determinants of right ventricular afterload (2013 Grover Conference
series). Pulmonary circulation, 4(2), 211-219.
WHO. (2011). Pulse Oximetry Training Manual. Retrieved from
https://www.who.int/patientsafety/safesurgery/pulse_oximetry/who_ps_pulse_oxymetry_
training_manual_en.pdf
Zannad, F., McMurray, J. J., Krum, H., van Veldhuisen, D. J., Swedberg, K., Shi, H., ... & Pitt,
B. (2011). Eplerenone in patients with systolic heart failure and mild symptoms. New
England Journal of Medicine, 364(1), 11-21.
10
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





