Advanced Materials: Bioactive Glass and BMP Applications Report
VerifiedAdded on 2022/12/15
|7
|1840
|256
Report
AI Summary
This report delves into the realm of advanced materials, primarily focusing on bioactive glass and bone morphogenetic protein (BMP). Bioactive glass, a surface-reactive glass-ceramic biomaterial, is examined for its applications in bone repair and replacement, including its use in spinal fusion and dental clinics. The report highlights the material's properties, advantages, and disadvantages, such as its antibacterial qualities and potential influence on the body. The report also explores bone morphogenetic protein (BMP), a growth factor stimulating bone and cartilage development, discussing its functions, clinical applications, and advantages in spinal fusion surgery, alongside its associated risks. The report emphasizes the mechanical properties, clinical uses, and potential of these materials in orthopedic and trauma applications, supported by references to relevant research and studies.

ADVANCED MATERIALS 1
Advance Materials
Students name:
Instructors name:
University affiliated:
Date:
Advance Materials
Students name:
Instructors name:
University affiliated:
Date:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ADVANCED MATERIALS 2
BIOACTIVE GLASS
Bioactive glass is a collection of surface reactive glass-ceramic biomaterials (Pugely,
Petersen, DeVries-Watson, & Fredericks, 2017). These glasses are hard materials that have silicon
and other components which are mainly in solid state. In addition, these bioactive glasses are used
for implant in a human body that assists in repairing and replacing bones that are damaged. In
addition, these bioactive glasses have been discovered by scientist that they can be very significant
in long bone infection in the human body.
Solid-state NMR spectroscopy is very important in explaining the arrangement of
amorphous solids (Salinas, Vallet-Regi & Heikkilä, 2018). However, these glasses have been
considered by 29Si and 31P that are in concrete state MAS NMR spectroscopy. However, the
chemical shift converted from MAS NMR is a clear indicates form of chemical species that are
present in those glasses. 29Si MAS NMR spectroscopy indicates that Bioglass 45S5 before was Q2
form-structure that had a little amount of Q3. On the other hand, 31P MAS NMR discovered
predominately Q0 group. A consequent MAS NMR spectroscopy measure shows clearly that Si-O-
P bonds are below measurable points. The scientist has been investigating the essential method
which facilitates bioactive glasses that operates as one of the resources in repairing and replacing
bones in the human body.
Mechanical properties
In bioactive glass there is always a need of developing synthetic scaffolds that mainly assist
in repairing huge faults in load-bearing bones. In this material there is an attractive property where
scaffold material that repairs injuries in bones is limited. Contained fault bones can be repaired
with commercially-available.
APPLICATION
There is much selection of bone graft replacement that is now implemented in orthopaedic
surgery which allograft bones, bioactive ceramic granules, beta-tricalcium phosphate, coralline
hydro-xyapatite, and osteogenic protein-1, with changeable fusion success charge.
Bioactive glasses can be used in clinics by the dentist (Ke et al., 2018). They are silicate-
based which can create a tough chemical bond in the body with tissues. In addition, they might also
create a hydroxyapatite layer in case they are implanted or maybe soaked in the reproduce fluids in
the body.
BIOACTIVE GLASS
Bioactive glass is a collection of surface reactive glass-ceramic biomaterials (Pugely,
Petersen, DeVries-Watson, & Fredericks, 2017). These glasses are hard materials that have silicon
and other components which are mainly in solid state. In addition, these bioactive glasses are used
for implant in a human body that assists in repairing and replacing bones that are damaged. In
addition, these bioactive glasses have been discovered by scientist that they can be very significant
in long bone infection in the human body.
Solid-state NMR spectroscopy is very important in explaining the arrangement of
amorphous solids (Salinas, Vallet-Regi & Heikkilä, 2018). However, these glasses have been
considered by 29Si and 31P that are in concrete state MAS NMR spectroscopy. However, the
chemical shift converted from MAS NMR is a clear indicates form of chemical species that are
present in those glasses. 29Si MAS NMR spectroscopy indicates that Bioglass 45S5 before was Q2
form-structure that had a little amount of Q3. On the other hand, 31P MAS NMR discovered
predominately Q0 group. A consequent MAS NMR spectroscopy measure shows clearly that Si-O-
P bonds are below measurable points. The scientist has been investigating the essential method
which facilitates bioactive glasses that operates as one of the resources in repairing and replacing
bones in the human body.
Mechanical properties
In bioactive glass there is always a need of developing synthetic scaffolds that mainly assist
in repairing huge faults in load-bearing bones. In this material there is an attractive property where
scaffold material that repairs injuries in bones is limited. Contained fault bones can be repaired
with commercially-available.
APPLICATION
There is much selection of bone graft replacement that is now implemented in orthopaedic
surgery which allograft bones, bioactive ceramic granules, beta-tricalcium phosphate, coralline
hydro-xyapatite, and osteogenic protein-1, with changeable fusion success charge.
Bioactive glasses can be used in clinics by the dentist (Ke et al., 2018). They are silicate-
based which can create a tough chemical bond in the body with tissues. In addition, they might also
create a hydroxyapatite layer in case they are implanted or maybe soaked in the reproduce fluids in
the body.
ADVANCED MATERIALS 3
Lilac crest autograft is another material that is used in spinal fusion. These glasses use are
limited by other effective time, loss of blood increases and morbidity (Jones, Brauer, Hupa &
Greenspan, 2016).Both bioactive glass and iliac crest autograft are materials that perform the same
role in the human body. Bioactive glass assists in the treatment of thoracic adolescent idiopathic
scoliosis. When it is implanted in a patient’s body, numerous numbers of reactions might take
place.
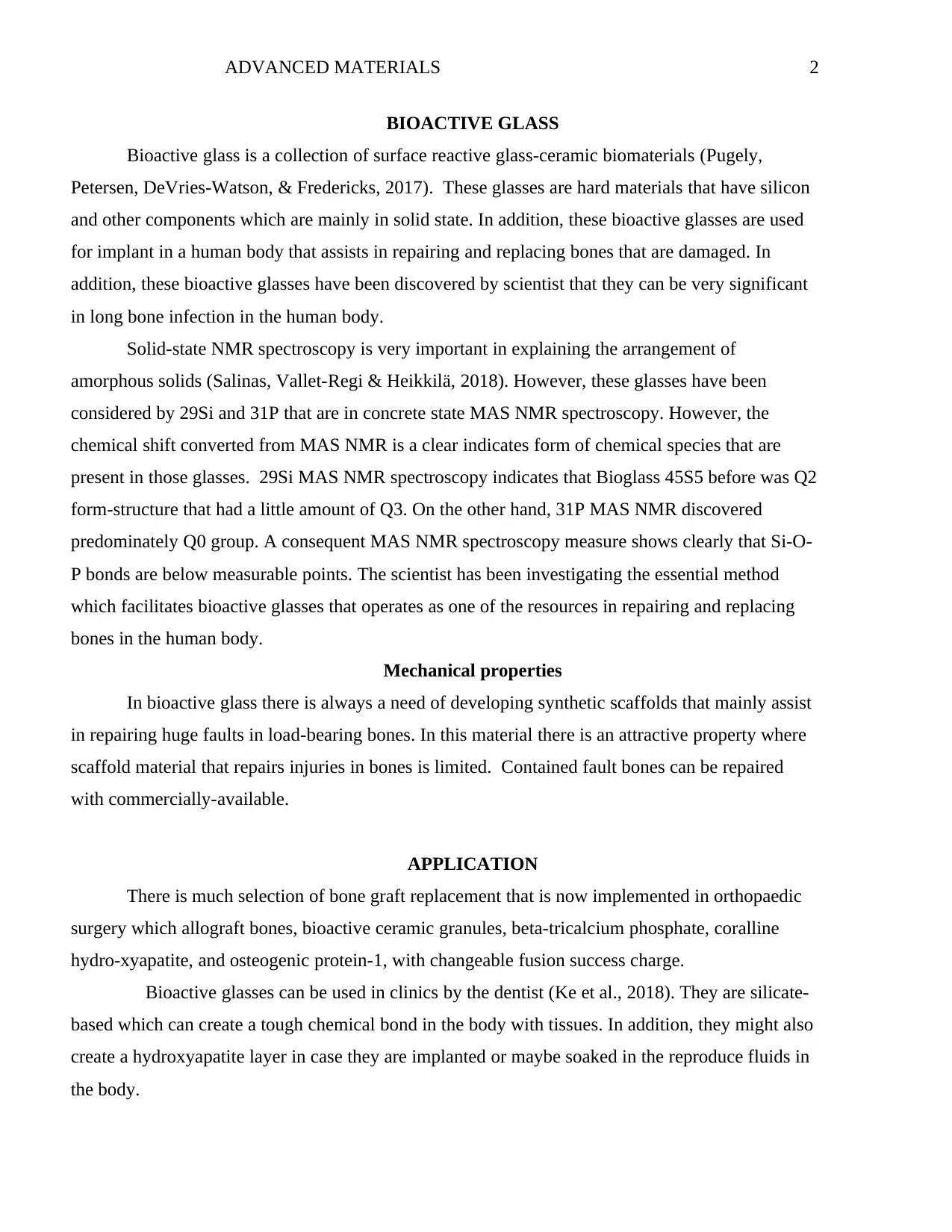
S53P4 bioactive glass has been specified as a bone graft replacement in many clinical
applications. This bone graft replacements are used commonly in replacement and regulating lost
bones to trauma and disease.
Figure 1
DISADVANTAGE AND ADVANTAGE
Bioactive glass S53P4 is a bone that is used in bonding that has verified antibac-terial
material goods (Saarenpää, Hirvonen, Rinne & Frantzén, 2018). This material is preferred in many
clinics because it is best when it comes in repairing cartilage and replacement of bones that are
damaged. It can be used in repairing or replacing long term bone damages. This bioactive glass has
effects on the human body when they are replaced. Additional of silver, aluminum, magnesium, and
others may influence the body system.
In conclusion, results in presentation study recommend that bioglasses are as helpful as iliac
crest grafts that assist in achieving fusion and in maintaining improvement in Adolescent Idiopathic
Scoliosis AIS. They can also be future in the treatment of AIS that might evade the morbidity of
iliac crest collection.
Lilac crest autograft is another material that is used in spinal fusion. These glasses use are
limited by other effective time, loss of blood increases and morbidity (Jones, Brauer, Hupa &
Greenspan, 2016).Both bioactive glass and iliac crest autograft are materials that perform the same
role in the human body. Bioactive glass assists in the treatment of thoracic adolescent idiopathic
scoliosis. When it is implanted in a patient’s body, numerous numbers of reactions might take
place.
S53P4 bioactive glass has been specified as a bone graft replacement in many clinical
applications. This bone graft replacements are used commonly in replacement and regulating lost
bones to trauma and disease.
Figure 1
DISADVANTAGE AND ADVANTAGE
Bioactive glass S53P4 is a bone that is used in bonding that has verified antibac-terial
material goods (Saarenpää, Hirvonen, Rinne & Frantzén, 2018). This material is preferred in many
clinics because it is best when it comes in repairing cartilage and replacement of bones that are
damaged. It can be used in repairing or replacing long term bone damages. This bioactive glass has
effects on the human body when they are replaced. Additional of silver, aluminum, magnesium, and
others may influence the body system.
In conclusion, results in presentation study recommend that bioglasses are as helpful as iliac
crest grafts that assist in achieving fusion and in maintaining improvement in Adolescent Idiopathic
Scoliosis AIS. They can also be future in the treatment of AIS that might evade the morbidity of
iliac crest collection.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
ADVANCED MATERIALS 4
BORNE MORPHOGENETIC PROTEIN (BMPs)
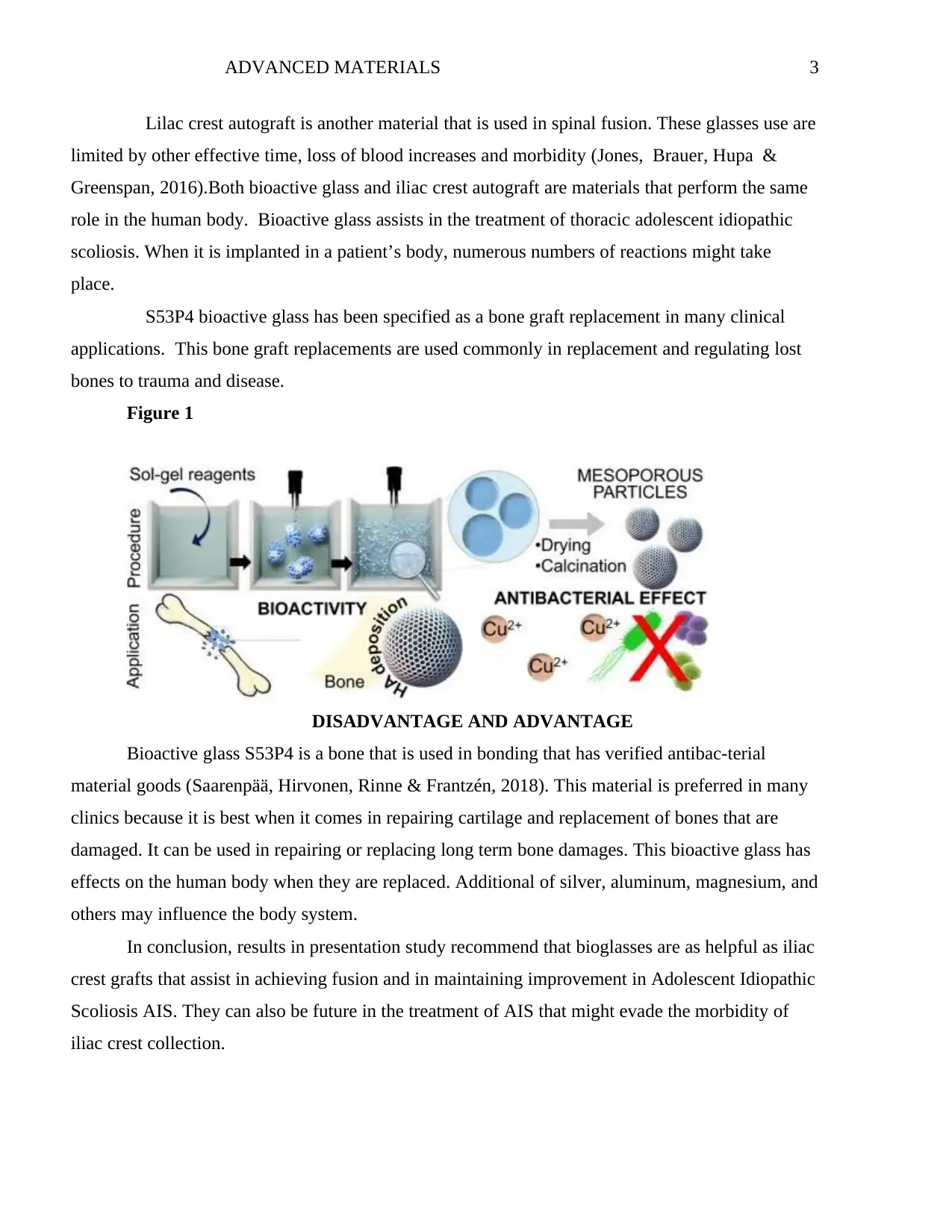
Figure 2
The figure below shows emerging roles of borne morphogenetic protein.
Bone morphogenetic protein (BMP) is also referred to as metabolites and cytokines that are
a collection of growth factors. BMPs were discovered to stimulate the development of cartilages
and bones (Bansal, Mukherjee, Horwitz & Mukherjee, 2019). In addition, they are now believed in
constituting a collection of pivotal morphogenetic indication and the orchestrating tissue planning
in the entire body system. The main function of the BMP signals in physiology is stressed by
numerous numbers of functions in dysregulated BMP indication in the pathological procedure.
Introduction of this material was mainly to replace the crest bone graft that is involved in spinal
fusion surgery.
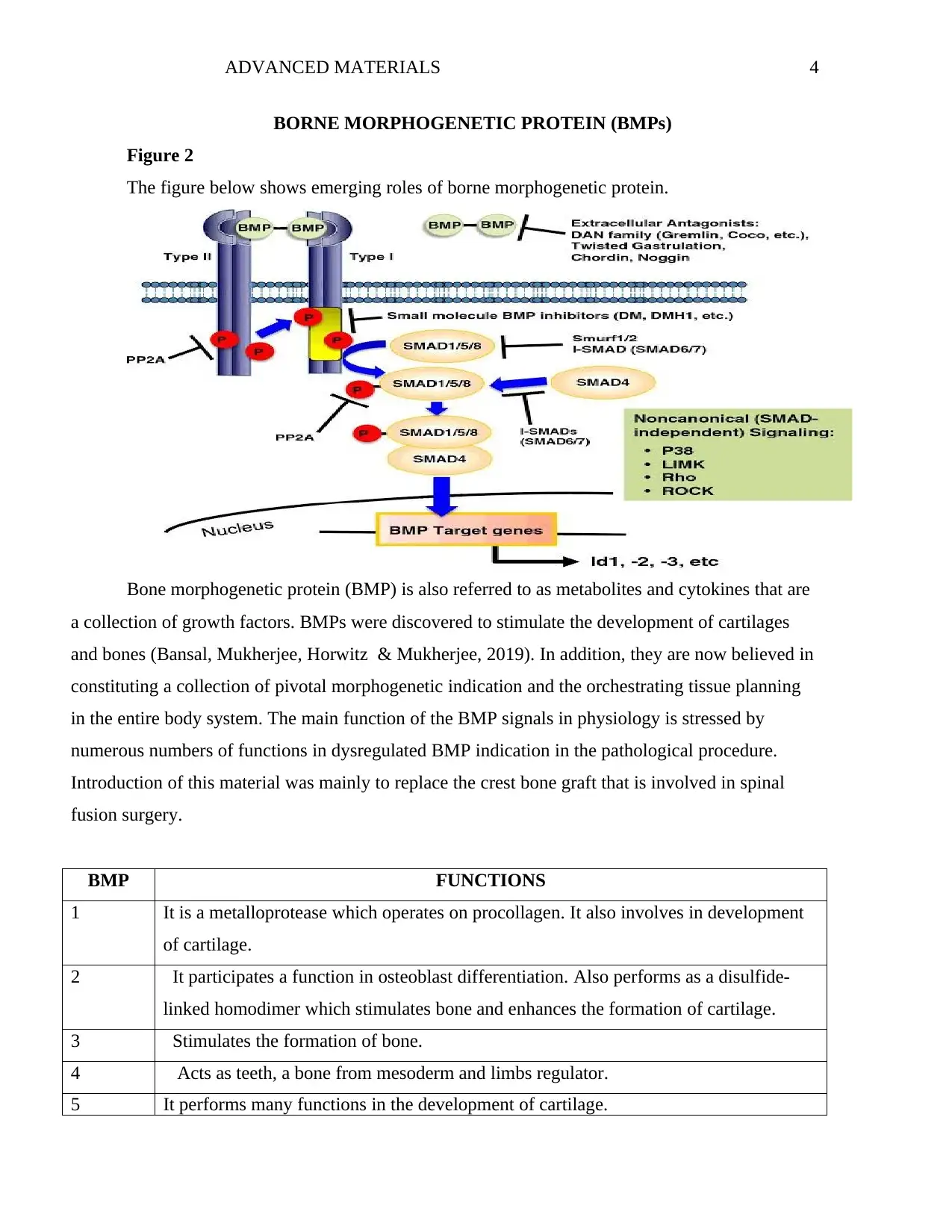
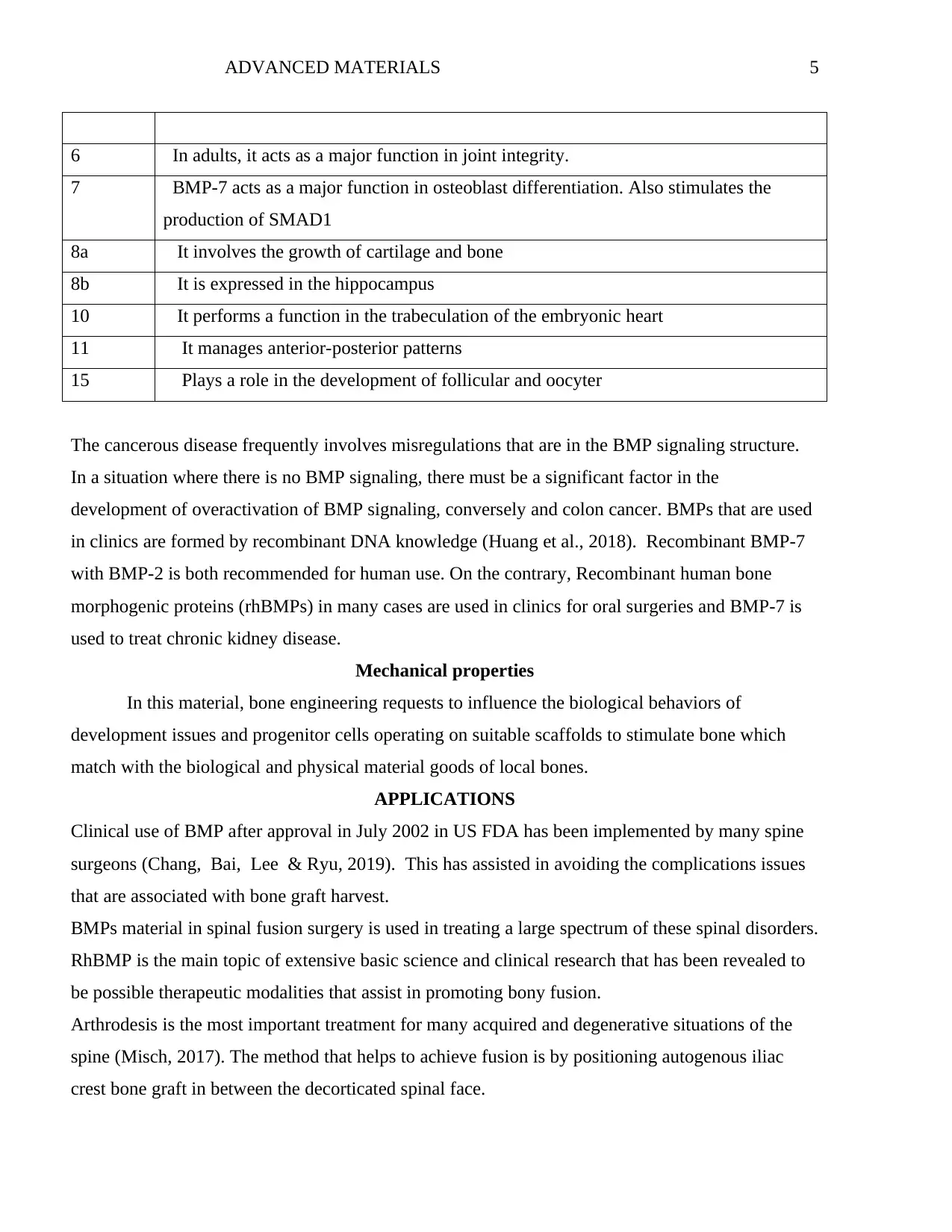
BMP FUNCTIONS
1 It is a metalloprotease which operates on procollagen. It also involves in development
of cartilage.
2 It participates a function in osteoblast differentiation. Also performs as a disulfide-
linked homodimer which stimulates bone and enhances the formation of cartilage.
3 Stimulates the formation of bone.
4 Acts as teeth, a bone from mesoderm and limbs regulator.
5 It performs many functions in the development of cartilage.
BORNE MORPHOGENETIC PROTEIN (BMPs)
Figure 2
The figure below shows emerging roles of borne morphogenetic protein.
Bone morphogenetic protein (BMP) is also referred to as metabolites and cytokines that are
a collection of growth factors. BMPs were discovered to stimulate the development of cartilages
and bones (Bansal, Mukherjee, Horwitz & Mukherjee, 2019). In addition, they are now believed in
constituting a collection of pivotal morphogenetic indication and the orchestrating tissue planning
in the entire body system. The main function of the BMP signals in physiology is stressed by
numerous numbers of functions in dysregulated BMP indication in the pathological procedure.
Introduction of this material was mainly to replace the crest bone graft that is involved in spinal
fusion surgery.
BMP FUNCTIONS
1 It is a metalloprotease which operates on procollagen. It also involves in development
of cartilage.
2 It participates a function in osteoblast differentiation. Also performs as a disulfide-
linked homodimer which stimulates bone and enhances the formation of cartilage.
3 Stimulates the formation of bone.
4 Acts as teeth, a bone from mesoderm and limbs regulator.
5 It performs many functions in the development of cartilage.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ADVANCED MATERIALS 5
6 In adults, it acts as a major function in joint integrity.
7 BMP-7 acts as a major function in osteoblast differentiation. Also stimulates the
production of SMAD1
8a It involves the growth of cartilage and bone
8b It is expressed in the hippocampus
10 It performs a function in the trabeculation of the embryonic heart
11 It manages anterior-posterior patterns
15 Plays a role in the development of follicular and oocyter
The cancerous disease frequently involves misregulations that are in the BMP signaling structure.
In a situation where there is no BMP signaling, there must be a significant factor in the
development of overactivation of BMP signaling, conversely and colon cancer. BMPs that are used
in clinics are formed by recombinant DNA knowledge (Huang et al., 2018). Recombinant BMP-7
with BMP-2 is both recommended for human use. On the contrary, Recombinant human bone
morphogenic proteins (rhBMPs) in many cases are used in clinics for oral surgeries and BMP-7 is
used to treat chronic kidney disease.
Mechanical properties
In this material, bone engineering requests to influence the biological behaviors of
development issues and progenitor cells operating on suitable scaffolds to stimulate bone which
match with the biological and physical material goods of local bones.
APPLICATIONS
Clinical use of BMP after approval in July 2002 in US FDA has been implemented by many spine
surgeons (Chang, Bai, Lee & Ryu, 2019). This has assisted in avoiding the complications issues
that are associated with bone graft harvest.
BMPs material in spinal fusion surgery is used in treating a large spectrum of these spinal disorders.
RhBMP is the main topic of extensive basic science and clinical research that has been revealed to
be possible therapeutic modalities that assist in promoting bony fusion.
Arthrodesis is the most important treatment for many acquired and degenerative situations of the
spine (Misch, 2017). The method that helps to achieve fusion is by positioning autogenous iliac
crest bone graft in between the decorticated spinal face.
6 In adults, it acts as a major function in joint integrity.
7 BMP-7 acts as a major function in osteoblast differentiation. Also stimulates the
production of SMAD1
8a It involves the growth of cartilage and bone
8b It is expressed in the hippocampus
10 It performs a function in the trabeculation of the embryonic heart
11 It manages anterior-posterior patterns
15 Plays a role in the development of follicular and oocyter
The cancerous disease frequently involves misregulations that are in the BMP signaling structure.
In a situation where there is no BMP signaling, there must be a significant factor in the
development of overactivation of BMP signaling, conversely and colon cancer. BMPs that are used
in clinics are formed by recombinant DNA knowledge (Huang et al., 2018). Recombinant BMP-7
with BMP-2 is both recommended for human use. On the contrary, Recombinant human bone
morphogenic proteins (rhBMPs) in many cases are used in clinics for oral surgeries and BMP-7 is
used to treat chronic kidney disease.
Mechanical properties
In this material, bone engineering requests to influence the biological behaviors of
development issues and progenitor cells operating on suitable scaffolds to stimulate bone which
match with the biological and physical material goods of local bones.
APPLICATIONS
Clinical use of BMP after approval in July 2002 in US FDA has been implemented by many spine
surgeons (Chang, Bai, Lee & Ryu, 2019). This has assisted in avoiding the complications issues
that are associated with bone graft harvest.
BMPs material in spinal fusion surgery is used in treating a large spectrum of these spinal disorders.
RhBMP is the main topic of extensive basic science and clinical research that has been revealed to
be possible therapeutic modalities that assist in promoting bony fusion.
Arthrodesis is the most important treatment for many acquired and degenerative situations of the
spine (Misch, 2017). The method that helps to achieve fusion is by positioning autogenous iliac
crest bone graft in between the decorticated spinal face.
ADVANCED MATERIALS 6
DISADVANTAGE AND ADVANTAGE
The main disadvantage of this material is that it increases the risks that are associated with utilizing
INFUSE that occurs in "off label" capacity for this surgery (Liu et al., 2018). This straight
contraindication includes allergy, infection, pregnancy, kidney disease HIV/AIDS.
The benefit of using this material is that it effectively reduces pain and improves the outcomes in
fusion surgery.
DISADVANTAGE AND ADVANTAGE
The main disadvantage of this material is that it increases the risks that are associated with utilizing
INFUSE that occurs in "off label" capacity for this surgery (Liu et al., 2018). This straight
contraindication includes allergy, infection, pregnancy, kidney disease HIV/AIDS.
The benefit of using this material is that it effectively reduces pain and improves the outcomes in
fusion surgery.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
ADVANCED MATERIALS 7
REFERENCES
Bansal, R., Mukherjee, M., Horwitz, B. A., & Mukherjee, P. K. (2019). Regulation of conidiation
and antagonistic properties of the soil-borne plant beneficial fungus Trichoderma virens by a novel
proline-, glycine-, tyrosine-rich protein and a GPI-anchored cell wall protein. Current genetics, 1-
12.
Bioglass and bioactive glasses and their impact on healthcare. International Journal of Applied
Glass Science, 7(4), 423-434.
Chang, Y., Bai, J., Lee, J. H., & Ryu, S. (2019). Mutation of a Staphylococcus aureus temperate
bacteriophage to a virulent one and evaluation of its application. Food Microbiology.
Huang, B., Lou, Y., Li, T., Lin, Z., Sun, S., Yuan, Y., ... & Gu, Y. (2018). Molecular dynamics
simulations of adsorption and desorption of bone morphogenetic protein-2 on textured
hydroxyapatite surfaces. Acta biomaterialia, 80, 121-130.
Ke, X., Zhang, L., Yang, X., Wang, J., Zhuang, C., Jin, Z., ... & Gou, Z. (2018). Low‐melt
bioactive glass‐reinforced 3D printing akermanite porous cages with highly improved mechanical
properties for lumbar spinal fusion. Journal of tissue engineering and regenerative medicine, 12(5),
1149-1162.
Liu, Y., Schouten, C., Boerman, O., Wu, G., Jansen, J. A., & Hunziker, E. B. (2018). The kinetics
and mechanism of bone morphogenetic protein 2 release from calcium phosphate‐based implant‐
coatings. Journal of Biomedical Materials Research Part A, 106(9), 2363-2371.
Misch, C. M. (2017). Bone augmentation using allogeneic bone blocks with recombinant bone
morphogenetic protein-2. Implant dentistry, 26(6), 826-831.
Pugely, A. J., Petersen, E. B., DeVries-Watson, N., & Fredericks, D. C. (2017). Influence of 45S5
bioactive glass in a standard calcium phosphate collagen bone graft substitute on the posterolateral
fusion of rabbit spine. The Iowa orthopaedic journal, 37, 193.
Saarenpää, I., Hirvonen, J., Rinne, J., & Frantzén, J. (2018). Novel bioactive glass putty (S53P4) as
bone graft expander in minimally invasive lumbosacral interbody fusion. Journal of Minimally
Invasive Spine Surgery and Technique, 3(2), 52-58.
Salinas, A. J., Vallet-Regi, M., & Heikkilä, J. (2018). Use of bioactive glasses as bone substitutes in
orthopedics and traumatology. In Bioactive Glasses (pp. 337-364). Woodhead Publishing.
REFERENCES
Bansal, R., Mukherjee, M., Horwitz, B. A., & Mukherjee, P. K. (2019). Regulation of conidiation
and antagonistic properties of the soil-borne plant beneficial fungus Trichoderma virens by a novel
proline-, glycine-, tyrosine-rich protein and a GPI-anchored cell wall protein. Current genetics, 1-
12.
Bioglass and bioactive glasses and their impact on healthcare. International Journal of Applied
Glass Science, 7(4), 423-434.
Chang, Y., Bai, J., Lee, J. H., & Ryu, S. (2019). Mutation of a Staphylococcus aureus temperate
bacteriophage to a virulent one and evaluation of its application. Food Microbiology.
Huang, B., Lou, Y., Li, T., Lin, Z., Sun, S., Yuan, Y., ... & Gu, Y. (2018). Molecular dynamics
simulations of adsorption and desorption of bone morphogenetic protein-2 on textured
hydroxyapatite surfaces. Acta biomaterialia, 80, 121-130.
Ke, X., Zhang, L., Yang, X., Wang, J., Zhuang, C., Jin, Z., ... & Gou, Z. (2018). Low‐melt
bioactive glass‐reinforced 3D printing akermanite porous cages with highly improved mechanical
properties for lumbar spinal fusion. Journal of tissue engineering and regenerative medicine, 12(5),
1149-1162.
Liu, Y., Schouten, C., Boerman, O., Wu, G., Jansen, J. A., & Hunziker, E. B. (2018). The kinetics
and mechanism of bone morphogenetic protein 2 release from calcium phosphate‐based implant‐
coatings. Journal of Biomedical Materials Research Part A, 106(9), 2363-2371.
Misch, C. M. (2017). Bone augmentation using allogeneic bone blocks with recombinant bone
morphogenetic protein-2. Implant dentistry, 26(6), 826-831.
Pugely, A. J., Petersen, E. B., DeVries-Watson, N., & Fredericks, D. C. (2017). Influence of 45S5
bioactive glass in a standard calcium phosphate collagen bone graft substitute on the posterolateral
fusion of rabbit spine. The Iowa orthopaedic journal, 37, 193.
Saarenpää, I., Hirvonen, J., Rinne, J., & Frantzén, J. (2018). Novel bioactive glass putty (S53P4) as
bone graft expander in minimally invasive lumbosacral interbody fusion. Journal of Minimally
Invasive Spine Surgery and Technique, 3(2), 52-58.
Salinas, A. J., Vallet-Regi, M., & Heikkilä, J. (2018). Use of bioactive glasses as bone substitutes in
orthopedics and traumatology. In Bioactive Glasses (pp. 337-364). Woodhead Publishing.
1 out of 7
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


