Palliative Care Approaches and Issues in Aged Care Facilities
VerifiedAdded on 2022/11/17
|16
|4778
|483
Essay
AI Summary
This essay examines palliative care within the context of aged care, focusing on improving the lives of elderly patients and their families facing life-threatening illnesses. It details palliative measures such as pain management, psychosocial support, and bereavement care, highlighting the benefits of palliative home care and residential health care. The essay discusses the Aged Care Funding Instrument (ACFI) data, the palliative approach, and its application in enhancing the quality of life for elderly residents. It also addresses challenges, including comorbidities, dementia, and the need for advanced care planning. Furthermore, the essay explores complementary therapies, the importance of family involvement, and the impact of social and cultural considerations in providing effective palliative care, emphasizing the need for a multidisciplinary approach to support the elderly and their families.

AGED CARE 1
AGED CARE
Student’s Name
Institutional Affiliation
AGED CARE
Student’s Name
Institutional Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
AGED CARE 2
Aged Care
World health organization (WHO) defines palliative care as a methodology that aims at
improving the lives of aged patients and their families at large facing the complications that
are linked to illness that is life-threatening. These can be made possible through the
mitigation and respite of grief through early recognition and impeccable appraisal by
management of the pain. The symptoms that are experienced by the patient and submitted to
treatment include psychosocial, physical, and spiritual illness. Aged patient’s symptoms may
need better palliation as death approaches (Burkett & Scott, 2015). Support should be
provided to the dying patient’s family as comfort measures are being intensified. This essay
illustrates the palliative measures that are being taken to the relieve suffering of elderly
patients together with their families.
Palliative Care Provision
In cases of the worst scenario the elderly patient dies, the palliative care will shift its entire
focus on bereavement and providing support to the family that has lost its love one (Fitch,
Fliedner, & O’Connor, 2015). Palliative upkeep has proven to be more beneficial in various
ways. Therefore, it aids the family to make significant medical decisions. Moreover, it aims
at anticipating, preventing, diagnosing, and treating signs and symptoms that the patients may
have experienced. The focal target of the palliative care system is to improve the quality of
life of both the patient and the family as well regardless of the patient’s diagnosis (Martin,
Hayes, Gregorevic & Lim, 2016). Palliative care reduces pain, fatigue, nausea in the aged
patients that suffer from chronic illness as well progresses quality of patient’s life, which is a
long term beneficiary effect.
The palliative home care measure is fundamental to the aged since it gives them the
chance to stay at home in a more familiar environment as compared to the hospital
environment (Frey, Boyd, Foster, Robinson & Gott, 2016). This type of environment reduces
Aged Care
World health organization (WHO) defines palliative care as a methodology that aims at
improving the lives of aged patients and their families at large facing the complications that
are linked to illness that is life-threatening. These can be made possible through the
mitigation and respite of grief through early recognition and impeccable appraisal by
management of the pain. The symptoms that are experienced by the patient and submitted to
treatment include psychosocial, physical, and spiritual illness. Aged patient’s symptoms may
need better palliation as death approaches (Burkett & Scott, 2015). Support should be
provided to the dying patient’s family as comfort measures are being intensified. This essay
illustrates the palliative measures that are being taken to the relieve suffering of elderly
patients together with their families.
Palliative Care Provision
In cases of the worst scenario the elderly patient dies, the palliative care will shift its entire
focus on bereavement and providing support to the family that has lost its love one (Fitch,
Fliedner, & O’Connor, 2015). Palliative upkeep has proven to be more beneficial in various
ways. Therefore, it aids the family to make significant medical decisions. Moreover, it aims
at anticipating, preventing, diagnosing, and treating signs and symptoms that the patients may
have experienced. The focal target of the palliative care system is to improve the quality of
life of both the patient and the family as well regardless of the patient’s diagnosis (Martin,
Hayes, Gregorevic & Lim, 2016). Palliative care reduces pain, fatigue, nausea in the aged
patients that suffer from chronic illness as well progresses quality of patient’s life, which is a
long term beneficiary effect.
The palliative home care measure is fundamental to the aged since it gives them the
chance to stay at home in a more familiar environment as compared to the hospital
environment (Frey, Boyd, Foster, Robinson & Gott, 2016). This type of environment reduces
AGED CARE 3
their rate of depression; as a result, they will visit the emergency rooms a few times.
Families, at times, find it challenging to take care of the elder members of their families who
have chronic illness due to commitments and engagements. Thus, professional caregiving can
relieve them from that duty and pressure for their loved ones during the final month.
Research has proven that the majority of elderly patients who are nearing the end of their
lives spend their last moments in the hospital, which makes them feel lonely and helpless.
Palliative home care provides them emotional and physical support to prolong their lives
(Smedbäck et al., 2017).
Residential Health Care
Residential health care is a type of care that has been established to take care of the aged
people who can no longer take shelter at their homes and are always regarded as a vulnerable
group. This facility provides them progressive support care that comprises of aid with routine
activities and individual care to 24 hours of treatment care. The residential aged services in
Victoria are being overseen by the Commonwealth Government. The Aged Care Act 1997
(the Act) governs the residential aged care in Australia. An approximate of 200 000
Australians stay or live in residential aged care due to the growing population of older people.
In Australia, there is an estimate of 2,672 residential aged care facilities (Broad et al., 2015).
Residential care services can be provided under respite or permanent basis. The residential
respite is short care that is provided to the elderly during emergencies in aged care facilities,
and approval has to be made before the services are offered to them.
The residential elderly care provides accommodation and amenities to the aged population
that require continuing nursing and health care as a result of lack of self- independence in
daily activities and critical impairments (Chapman, Johnston, Lovell & Liu, 2018). These
facilities offer a variety of services that constitute supervision, nursing, or any other
additional care that the patient may be in need.
their rate of depression; as a result, they will visit the emergency rooms a few times.
Families, at times, find it challenging to take care of the elder members of their families who
have chronic illness due to commitments and engagements. Thus, professional caregiving can
relieve them from that duty and pressure for their loved ones during the final month.
Research has proven that the majority of elderly patients who are nearing the end of their
lives spend their last moments in the hospital, which makes them feel lonely and helpless.
Palliative home care provides them emotional and physical support to prolong their lives
(Smedbäck et al., 2017).
Residential Health Care
Residential health care is a type of care that has been established to take care of the aged
people who can no longer take shelter at their homes and are always regarded as a vulnerable
group. This facility provides them progressive support care that comprises of aid with routine
activities and individual care to 24 hours of treatment care. The residential aged services in
Victoria are being overseen by the Commonwealth Government. The Aged Care Act 1997
(the Act) governs the residential aged care in Australia. An approximate of 200 000
Australians stay or live in residential aged care due to the growing population of older people.
In Australia, there is an estimate of 2,672 residential aged care facilities (Broad et al., 2015).
Residential care services can be provided under respite or permanent basis. The residential
respite is short care that is provided to the elderly during emergencies in aged care facilities,
and approval has to be made before the services are offered to them.
The residential elderly care provides accommodation and amenities to the aged population
that require continuing nursing and health care as a result of lack of self- independence in
daily activities and critical impairments (Chapman, Johnston, Lovell & Liu, 2018). These
facilities offer a variety of services that constitute supervision, nursing, or any other
additional care that the patient may be in need.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
AGED CARE 4
They are some of the challenges that the residential elderly care faces during the
administration of palliative care. Therefore, the permanent inhabitants occasionally have
difficulty during communication or dementia and comorbidities (AIHW 2015). Majority of
the permanent residents diagnose chronic degenerative diseases as compared to patients in
hospice that often diagnose cancer (Gribich et al. 2005).
Discussion
The Aged Care Funding Instrument (ACFI) facilitates in the data collection that is utilised
to establish the quantity of subventions of perpetual residents in Australia. The data below
encompass a section that was recorded in 2016, which indicates the perpetual residents that
require palliative care under (ACFI). The percentage that results in palliative care in elderly
individuals rises with the age of the residents. 23.2% of the permanent residents that receive
palliative care are often analysed with cancer. The type of cancer majorly affects the people is
lung cancer (17.4%) and prostate cancer (21.9%). On the other hand, the inner local areas
have the maximum rate of the palliative upkeep amid the permanent residents (69%) while
majority cities and outer region comprise of (32.2%) and (38.8%) of the simultaneously per
100, 000 population.
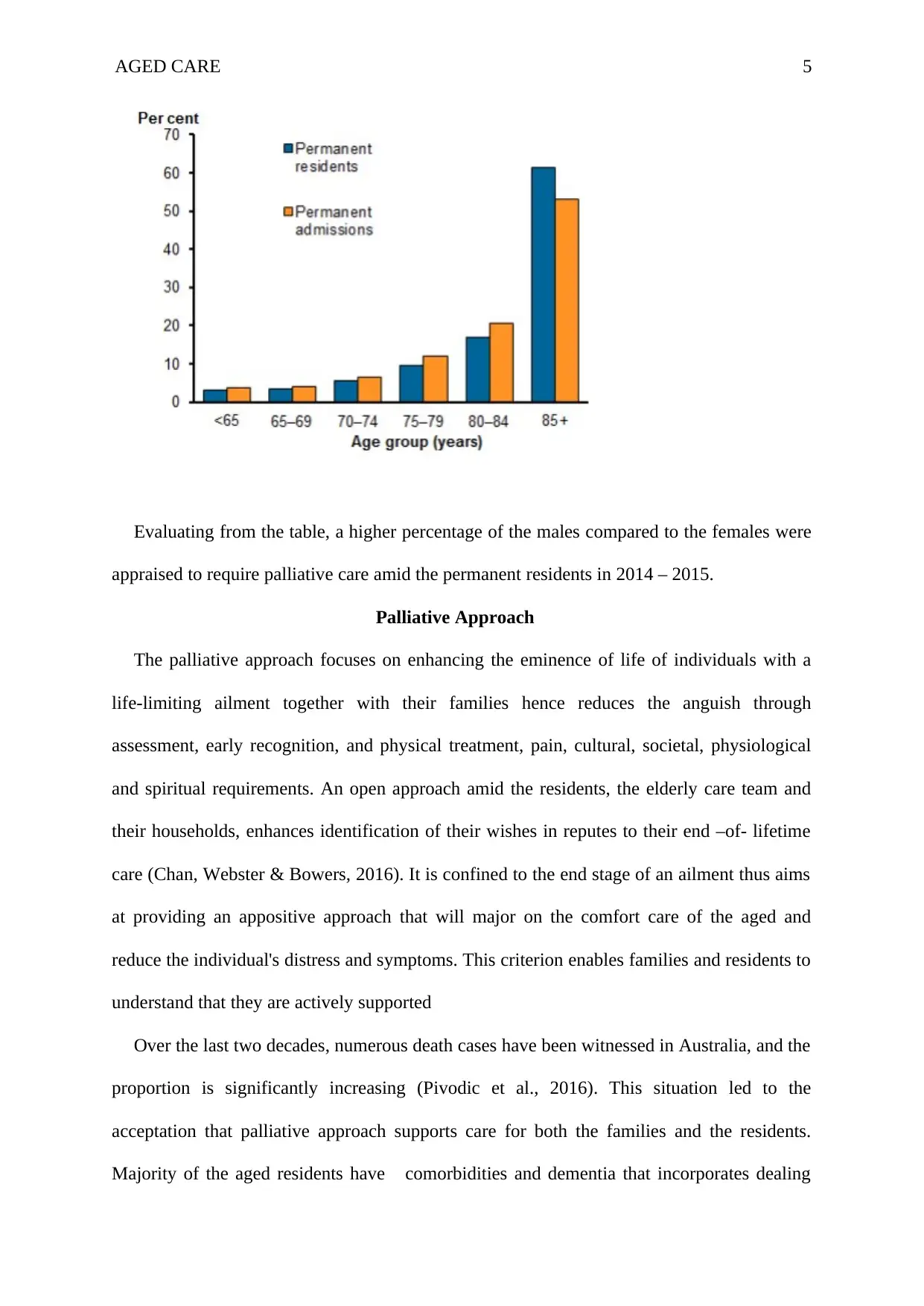
There was a similarity that was noted in the age profile of the permanent resident that
requires palliative care during 2014- 2015. A typical example is that one- quarter of the
people ranged between 75-84 and 60% of the aged population was 85 years and above.
Permanent admissions are regarded as the permanent residents who joined the care facility
between 2014 -2015 and were acquainted with entail palliative care. The figure below
indicates a perpetual residential elderly care and permanent admittances reviewed as
demanding palliative care between 2014 -2015 (AIHW, 2015).
They are some of the challenges that the residential elderly care faces during the
administration of palliative care. Therefore, the permanent inhabitants occasionally have
difficulty during communication or dementia and comorbidities (AIHW 2015). Majority of
the permanent residents diagnose chronic degenerative diseases as compared to patients in
hospice that often diagnose cancer (Gribich et al. 2005).
Discussion
The Aged Care Funding Instrument (ACFI) facilitates in the data collection that is utilised
to establish the quantity of subventions of perpetual residents in Australia. The data below
encompass a section that was recorded in 2016, which indicates the perpetual residents that
require palliative care under (ACFI). The percentage that results in palliative care in elderly
individuals rises with the age of the residents. 23.2% of the permanent residents that receive
palliative care are often analysed with cancer. The type of cancer majorly affects the people is
lung cancer (17.4%) and prostate cancer (21.9%). On the other hand, the inner local areas
have the maximum rate of the palliative upkeep amid the permanent residents (69%) while
majority cities and outer region comprise of (32.2%) and (38.8%) of the simultaneously per
100, 000 population.
There was a similarity that was noted in the age profile of the permanent resident that
requires palliative care during 2014- 2015. A typical example is that one- quarter of the
people ranged between 75-84 and 60% of the aged population was 85 years and above.
Permanent admissions are regarded as the permanent residents who joined the care facility
between 2014 -2015 and were acquainted with entail palliative care. The figure below
indicates a perpetual residential elderly care and permanent admittances reviewed as
demanding palliative care between 2014 -2015 (AIHW, 2015).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
AGED CARE 5
Evaluating from the table, a higher percentage of the males compared to the females were
appraised to require palliative care amid the permanent residents in 2014 – 2015.
Palliative Approach
The palliative approach focuses on enhancing the eminence of life of individuals with a
life-limiting ailment together with their families hence reduces the anguish through
assessment, early recognition, and physical treatment, pain, cultural, societal, physiological
and spiritual requirements. An open approach amid the residents, the elderly care team and
their households, enhances identification of their wishes in reputes to their end –of- lifetime
care (Chan, Webster & Bowers, 2016). It is confined to the end stage of an ailment thus aims
at providing an appositive approach that will major on the comfort care of the aged and
reduce the individual's distress and symptoms. This criterion enables families and residents to
understand that they are actively supported
Over the last two decades, numerous death cases have been witnessed in Australia, and the
proportion is significantly increasing (Pivodic et al., 2016). This situation led to the
acceptation that palliative approach supports care for both the families and the residents.
Majority of the aged residents have comorbidities and dementia that incorporates dealing
Evaluating from the table, a higher percentage of the males compared to the females were
appraised to require palliative care amid the permanent residents in 2014 – 2015.
Palliative Approach
The palliative approach focuses on enhancing the eminence of life of individuals with a
life-limiting ailment together with their families hence reduces the anguish through
assessment, early recognition, and physical treatment, pain, cultural, societal, physiological
and spiritual requirements. An open approach amid the residents, the elderly care team and
their households, enhances identification of their wishes in reputes to their end –of- lifetime
care (Chan, Webster & Bowers, 2016). It is confined to the end stage of an ailment thus aims
at providing an appositive approach that will major on the comfort care of the aged and
reduce the individual's distress and symptoms. This criterion enables families and residents to
understand that they are actively supported
Over the last two decades, numerous death cases have been witnessed in Australia, and the
proportion is significantly increasing (Pivodic et al., 2016). This situation led to the
acceptation that palliative approach supports care for both the families and the residents.
Majority of the aged residents have comorbidities and dementia that incorporates dealing
AGED CARE 6
with emotional, psychological, physical, and social complications. Highly dependency on
medication complicates the process, thus compromising the delivery of the palliative
approach. A palliative approach is essential during the aging process since an individual is
approaching death and may be vulnerable to cardiovascular diseases. The aged people who
are at the verge of dying have varying palliative needs as contrasted to the individuals that
have been diagnosed with cancer. They comprise of: lack of family support, dementia,
confusion or communication difficulties, several clinical diagnoses that need numerous
medications and need end of life care for a shorter duration (Frey et al., 2017). Therefore, it is
significant that the older people who are dying to be put under a palliative approach to
prolong their life span.
In palliative approach, their methods that are utilized in the identification of the survival
time such as clinical predicament by the specialist may have some shortcomings such as
precision and accuracy that result to overestimating of the survival duration. It is therefore
not recommended to rely on these methods in determination of the time to commence a
palliative approach. It is crucial for the members of the aged care group to be aware of the
tendency of their patients to avoid overestimating of survival time in order to reduce the
families and the resident’s distress.
On the other hand, the resident's transition from the active curative care to palliative care
requires team members of the aged care to provide the families and residents of the aged with
the equitable information in regards to the transition process to aid in decision making.
Access to information can reduce concerns of the families and aged residents, thus enhance
their satisfaction in regards to the efficiency of the palliative approach.
A palliative approach can be administered in an environment that is familiar to the aged
patient when skilled care is adequately available (Street, Ottmann, Johnstone, Considine &
Livingston, 2015). Hence, it will reduce the need to translocate to an intensive care setting,
with emotional, psychological, physical, and social complications. Highly dependency on
medication complicates the process, thus compromising the delivery of the palliative
approach. A palliative approach is essential during the aging process since an individual is
approaching death and may be vulnerable to cardiovascular diseases. The aged people who
are at the verge of dying have varying palliative needs as contrasted to the individuals that
have been diagnosed with cancer. They comprise of: lack of family support, dementia,
confusion or communication difficulties, several clinical diagnoses that need numerous
medications and need end of life care for a shorter duration (Frey et al., 2017). Therefore, it is
significant that the older people who are dying to be put under a palliative approach to
prolong their life span.
In palliative approach, their methods that are utilized in the identification of the survival
time such as clinical predicament by the specialist may have some shortcomings such as
precision and accuracy that result to overestimating of the survival duration. It is therefore
not recommended to rely on these methods in determination of the time to commence a
palliative approach. It is crucial for the members of the aged care group to be aware of the
tendency of their patients to avoid overestimating of survival time in order to reduce the
families and the resident’s distress.
On the other hand, the resident's transition from the active curative care to palliative care
requires team members of the aged care to provide the families and residents of the aged with
the equitable information in regards to the transition process to aid in decision making.
Access to information can reduce concerns of the families and aged residents, thus enhance
their satisfaction in regards to the efficiency of the palliative approach.
A palliative approach can be administered in an environment that is familiar to the aged
patient when skilled care is adequately available (Street, Ottmann, Johnstone, Considine &
Livingston, 2015). Hence, it will reduce the need to translocate to an intensive care setting,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
AGED CARE 7
which will avoid potential distress to their families and residents. The multidisciplinary team
is efficient in proving the palliative approach.
The aged care team addresses several factors during the implementation of the palliative
methodology that enhances the eminence of life and dignity of the residents. These factors
encompass reinforced affection with he loved ones, recognition of family members and
friends, being continent, symptom, and intensive pain management, ability to communicate,
and sense of control. The dignity maintenance care helps to reduce the elderly desire for
speed up death.
Aged Care Issues
They are complementary therapy that is part of the palliative approach and may be
beneficial to the individuals who are unable to tolerate medications. These therapies improve
the aged resident's sense of control because they fit their cultural preferences and
specifications. On that note, a combination of the traditional palliative medication, with
relaxation, acupuncture, and imagery may be beneficial in symptom management since they
reduce obstinate pain, thus refining the quality of life. Aromatherapy bodywork for patients
with radical dementia may diminish the level of anxiety, disturbance behavior problems, and
boost the quality of life (Gilissen et al., 2017).
Suicidal attempts are often a signal of clinical misery, and dynamic responses address the
state of hopelessness and depression amid the aged patients. Family member's involvement in
the treatment in a palliative approach is crucial. Thus, the death and the health deterioration
of the patient can be triggered by the family member’s inability to communicate and support
the specialist in the monitoring and administration of an appropriate palliative approach. The
social challenges due to the aged care involve the inability of the Australian administration to
release funds for the development of palliative care.
which will avoid potential distress to their families and residents. The multidisciplinary team
is efficient in proving the palliative approach.
The aged care team addresses several factors during the implementation of the palliative
methodology that enhances the eminence of life and dignity of the residents. These factors
encompass reinforced affection with he loved ones, recognition of family members and
friends, being continent, symptom, and intensive pain management, ability to communicate,
and sense of control. The dignity maintenance care helps to reduce the elderly desire for
speed up death.
Aged Care Issues
They are complementary therapy that is part of the palliative approach and may be
beneficial to the individuals who are unable to tolerate medications. These therapies improve
the aged resident's sense of control because they fit their cultural preferences and
specifications. On that note, a combination of the traditional palliative medication, with
relaxation, acupuncture, and imagery may be beneficial in symptom management since they
reduce obstinate pain, thus refining the quality of life. Aromatherapy bodywork for patients
with radical dementia may diminish the level of anxiety, disturbance behavior problems, and
boost the quality of life (Gilissen et al., 2017).
Suicidal attempts are often a signal of clinical misery, and dynamic responses address the
state of hopelessness and depression amid the aged patients. Family member's involvement in
the treatment in a palliative approach is crucial. Thus, the death and the health deterioration
of the patient can be triggered by the family member’s inability to communicate and support
the specialist in the monitoring and administration of an appropriate palliative approach. The
social challenges due to the aged care involve the inability of the Australian administration to
release funds for the development of palliative care.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
AGED CARE 8
Additionally, inadequate social provision may result in diminished functional health
depression, depression, and deterioration of the psychological health of the aged residents.
The practical framework can be implemented to enhance the resident’s condition when
proper evaluation of the resident’s societal network is done.
Knowledge of cultural miscellany is commended for the aged care groups to facilitate in
the considerate of the care choice and preference of inhabitants in different ethnic
dimensions. The palliative approach being able to accommodate residents and families
preference will facilitate the improvement of quality of life. Providing information
concerning palliative care approach to residents from linguistically and cultural backgrounds
by use of their native languages will improve cultural sensitivity for families and residents,
ensuring appropriate and adequate care plan.
Advanced Care Planning
Advanced care planning (ACP) is a step or process that an individual may take to plan for
the future health care (Martin, Hayes, Gregorevic & Lim, 2016). This is a state where a
person decides the type of care he wants in the eventuality that he will not be able to speak in
the future. The decisions that are made are occasionally based on the preferences, personal
values, and discussion with the family members. The primary focus of the ACP is to enable
the aged to be able to make appropriate future care for their health. The family and the aged
patient can decide on the type of medication or care to be utilized. ACP is regarded to be
beneficial to the aged community; thus it enhances them to discuss and reflect their
preferences and values on an individual health care plan in the state where they are unable to
communicate or make decisions. ACP is an appropriate care plan for the elderly, especially
with chronic diseases, and their health seems to be deteriorating.
ACP can be utilized to reduce family depression, stress, and anxiety. The programs that
have have been enhanced by ACP tend to minimize the chances of aged patients dying in
Additionally, inadequate social provision may result in diminished functional health
depression, depression, and deterioration of the psychological health of the aged residents.
The practical framework can be implemented to enhance the resident’s condition when
proper evaluation of the resident’s societal network is done.
Knowledge of cultural miscellany is commended for the aged care groups to facilitate in
the considerate of the care choice and preference of inhabitants in different ethnic
dimensions. The palliative approach being able to accommodate residents and families
preference will facilitate the improvement of quality of life. Providing information
concerning palliative care approach to residents from linguistically and cultural backgrounds
by use of their native languages will improve cultural sensitivity for families and residents,
ensuring appropriate and adequate care plan.
Advanced Care Planning
Advanced care planning (ACP) is a step or process that an individual may take to plan for
the future health care (Martin, Hayes, Gregorevic & Lim, 2016). This is a state where a
person decides the type of care he wants in the eventuality that he will not be able to speak in
the future. The decisions that are made are occasionally based on the preferences, personal
values, and discussion with the family members. The primary focus of the ACP is to enable
the aged to be able to make appropriate future care for their health. The family and the aged
patient can decide on the type of medication or care to be utilized. ACP is regarded to be
beneficial to the aged community; thus it enhances them to discuss and reflect their
preferences and values on an individual health care plan in the state where they are unable to
communicate or make decisions. ACP is an appropriate care plan for the elderly, especially
with chronic diseases, and their health seems to be deteriorating.
ACP can be utilized to reduce family depression, stress, and anxiety. The programs that
have have been enhanced by ACP tend to minimize the chances of aged patients dying in
AGED CARE 9
their residential care facilities. ACP seems to be affiliated with healthcare cost reduction that
ay comprises of the people that are living with dementia in the society.
Advanced Care Directives
The emergence of the advanced care directives (ACD) is as a result of ACP. ACD is the
type of document that contains legitimate channels where an individual can select and
instruct one or more alternative decision makers to note their choices and preferences for
their future projects in regards to individual health care. The strategies of ACD constitute of
the advanced personal project, advanced health care directives, living will, medical
directions, refusal of treatment certificate, specialist orders for life-sustaining medication, do
not resuscitate and do not hospitalize (Sellars, Silvester, Masso & Johnson, 2015). The state
and territory government laws in Australia differ in regards to ACD and ACP.
Nevertheless, they are some of the challenges that are affiliated with ACDs (Lund,
Richardson & May 2015). They constitute the inability of clinicians not to be able to follow
directives in the ACD and instances where individuals change their preferences after a certain
period and are unable to revise their ACD.
Discussion and Critique
The palliative health upkeep for the elderly is steered by doctrines that will promulgate
palliative, rehabilitative, preventive, supportive and curative care (Leslie et al., 2016).
Palliative health care for the aged facilitates the provision of health services that constitute of
management of health diagnosis, condition, and sustenance in the supervision of long term
healthcare that can be a chronic infection like diabetes or hypertension (Stokoe et al., 2016).
The old need to see the health professionals regularly for checks ups and health advises
maintaining their good health condition. It is crucial for aged people to be attached to a
medical expert who can attend to their emergencies.
their residential care facilities. ACP seems to be affiliated with healthcare cost reduction that
ay comprises of the people that are living with dementia in the society.
Advanced Care Directives
The emergence of the advanced care directives (ACD) is as a result of ACP. ACD is the
type of document that contains legitimate channels where an individual can select and
instruct one or more alternative decision makers to note their choices and preferences for
their future projects in regards to individual health care. The strategies of ACD constitute of
the advanced personal project, advanced health care directives, living will, medical
directions, refusal of treatment certificate, specialist orders for life-sustaining medication, do
not resuscitate and do not hospitalize (Sellars, Silvester, Masso & Johnson, 2015). The state
and territory government laws in Australia differ in regards to ACD and ACP.
Nevertheless, they are some of the challenges that are affiliated with ACDs (Lund,
Richardson & May 2015). They constitute the inability of clinicians not to be able to follow
directives in the ACD and instances where individuals change their preferences after a certain
period and are unable to revise their ACD.
Discussion and Critique
The palliative health upkeep for the elderly is steered by doctrines that will promulgate
palliative, rehabilitative, preventive, supportive and curative care (Leslie et al., 2016).
Palliative health care for the aged facilitates the provision of health services that constitute of
management of health diagnosis, condition, and sustenance in the supervision of long term
healthcare that can be a chronic infection like diabetes or hypertension (Stokoe et al., 2016).
The old need to see the health professionals regularly for checks ups and health advises
maintaining their good health condition. It is crucial for aged people to be attached to a
medical expert who can attend to their emergencies.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
AGED CARE
10
However, the community health facilities for the aged can be provided in a community
setting; thus, the residential healthcare provider can perform their duties in community health
centers, allied health practices, and medical clinics. Seemingly, the palliative health care
seeks to advise the aged be able to manage depression and stress, stop smoking, to be
physically active and take balance diet to prolong their life span.
Lack of modern technology has been a challenge to the developing states, thus leading to
reduced medical service delivery. Unequal resource distribution has enhanced the level of
poverty in the developing nations; thus, they lack machines like the body scanners and heart-
lung machines. Therefore, it is the responsibility of the administration to enhance the quality
of upkeep for the aged community. The old community contributes to a more significant
percentage of the population in the country; thus, the government needs to put more emphasis
on their treatment plan (Wakerman et al., 2017).
Contrary, the increased demand for health care by the aged can lead to a burden on the
health care systems. It is essential when the care insurance system that is determined by the
adoption of the national health care scheme as well as the aid from the commercial insurance
in sharing the financial burden. Due to high health care requirements by the aged community
in the residential has led to the service delivery to be a challenging process (Willis, Reynolds
& Keleher, 2016). Insufficient aged care training, education, and inadequate health care
providers are some of the restrictions that are faced during the process of service delivery.
Strategies
The state and the federal government are responsible for the formulation of effective
strategies and guidelines to enhance service delivery for the aged population. The workforce
for the care provider also needs to be improved to attract more professionals and nurses to
work in that sector. It is essential for the government to establish palliative care facilities that
10
However, the community health facilities for the aged can be provided in a community
setting; thus, the residential healthcare provider can perform their duties in community health
centers, allied health practices, and medical clinics. Seemingly, the palliative health care
seeks to advise the aged be able to manage depression and stress, stop smoking, to be
physically active and take balance diet to prolong their life span.
Lack of modern technology has been a challenge to the developing states, thus leading to
reduced medical service delivery. Unequal resource distribution has enhanced the level of
poverty in the developing nations; thus, they lack machines like the body scanners and heart-
lung machines. Therefore, it is the responsibility of the administration to enhance the quality
of upkeep for the aged community. The old community contributes to a more significant
percentage of the population in the country; thus, the government needs to put more emphasis
on their treatment plan (Wakerman et al., 2017).
Contrary, the increased demand for health care by the aged can lead to a burden on the
health care systems. It is essential when the care insurance system that is determined by the
adoption of the national health care scheme as well as the aid from the commercial insurance
in sharing the financial burden. Due to high health care requirements by the aged community
in the residential has led to the service delivery to be a challenging process (Willis, Reynolds
& Keleher, 2016). Insufficient aged care training, education, and inadequate health care
providers are some of the restrictions that are faced during the process of service delivery.
Strategies
The state and the federal government are responsible for the formulation of effective
strategies and guidelines to enhance service delivery for the aged population. The workforce
for the care provider also needs to be improved to attract more professionals and nurses to
work in that sector. It is essential for the government to establish palliative care facilities that
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
AGED CARE
11
will aid in taking care of the aged that comprise of their medical needs. (Rosenwax,
Spilsbury, Arendts, McNamara, & Semmens, 2015).
Extensive evaluation of the resident’s agony and the utilization of evidenced-based
palliative decision-making offer heightened pain administration, thus enhancing their value of
life. Some of the aged patients may be unable to verbalize the pain that they endure; as a
result, a specialist can use accurate report based evidence from behavioral cues in
determining the pain. The use of a useful evaluation tool increases the tendency in which
illness is diagnosed as being contrasted by physical inquiring from the patients where the pain
is generating from.
In addition, the regular education programs for the elderly and their families on the
concerns about advanced care and end -life -care enhances the tendency of plans that are
being implemented and completed to improve the family satisfaction with the end- life -care.
Furthermore, comprehensive advance care plan for the aged include assessment of the change
and response of the resident's health to enhance the families or residents satisfaction with the
care (Street, Ottmann, Johnstone, Considine & Livingston, 2015). The implementation of the
systemic advance care plan comprises of communication amid family, residents, and
specialist to enhance the gratification that has been provided to the family and the residents.
Conclusion
In summary, the care for the dying has been abandoned in the majority of the residential
aged care facilities and where death is an ordinary aspect. The Australian government has,
therefore, published guidelines to provide acquaintance and understanding in the current
context to address the problems affiliated to end of life care to family members, specialist,
and residents. The palliative care is pragmatic to be vital at the end of life since it gets rid of
the misery that the patient and the family may be going through a complete assessment and
treatment. Thus, it provides comfort to the dying patient and the family as well. This paper
11
will aid in taking care of the aged that comprise of their medical needs. (Rosenwax,
Spilsbury, Arendts, McNamara, & Semmens, 2015).
Extensive evaluation of the resident’s agony and the utilization of evidenced-based
palliative decision-making offer heightened pain administration, thus enhancing their value of
life. Some of the aged patients may be unable to verbalize the pain that they endure; as a
result, a specialist can use accurate report based evidence from behavioral cues in
determining the pain. The use of a useful evaluation tool increases the tendency in which
illness is diagnosed as being contrasted by physical inquiring from the patients where the pain
is generating from.
In addition, the regular education programs for the elderly and their families on the
concerns about advanced care and end -life -care enhances the tendency of plans that are
being implemented and completed to improve the family satisfaction with the end- life -care.
Furthermore, comprehensive advance care plan for the aged include assessment of the change
and response of the resident's health to enhance the families or residents satisfaction with the
care (Street, Ottmann, Johnstone, Considine & Livingston, 2015). The implementation of the
systemic advance care plan comprises of communication amid family, residents, and
specialist to enhance the gratification that has been provided to the family and the residents.
Conclusion
In summary, the care for the dying has been abandoned in the majority of the residential
aged care facilities and where death is an ordinary aspect. The Australian government has,
therefore, published guidelines to provide acquaintance and understanding in the current
context to address the problems affiliated to end of life care to family members, specialist,
and residents. The palliative care is pragmatic to be vital at the end of life since it gets rid of
the misery that the patient and the family may be going through a complete assessment and
treatment. Thus, it provides comfort to the dying patient and the family as well. This paper
AGED CARE
12
has concentrated on the need for the palliative care of the aged since the population of the
aged is progressively growing (O’Loughlin & Kendig, 2017). The aging population has been
a growing trend due to the low fertility rate, increased longevity, technological advances, and
migration. Nonetheless, partisan and social dynamics can impact the service provision of
aged people. Therefore, the future directions to cope with those challenges have been shifted
on the government efforts to develop an active community care service and workforce for the
aged
12
has concentrated on the need for the palliative care of the aged since the population of the
aged is progressively growing (O’Loughlin & Kendig, 2017). The aging population has been
a growing trend due to the low fertility rate, increased longevity, technological advances, and
migration. Nonetheless, partisan and social dynamics can impact the service provision of
aged people. Therefore, the future directions to cope with those challenges have been shifted
on the government efforts to develop an active community care service and workforce for the
aged
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 16
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





