Comprehensive Nursing Care Plan: Dementia, Ageing & Health Services
VerifiedAdded on 2023/06/08
|12
|3368
|434
Report
AI Summary
This nursing assignment presents a comprehensive nursing care plan for an 89-year-old female patient, Miss Alice Jones, residing in an aged care facility and diagnosed with Alzheimer’s Dementia, urinary incontinence, hypertension, osteoarthritis, anxiety, depression and a past episode of Myocardial Infarction. The plan includes a review of her medical history, application of the neuroendocrine theory of ageing, and an analysis of the physiological effects of ageing relevant to her conditions. It identifies primary health services needed, such as neurological assessment and heart monitoring, and proposes strategies for managing challenging behaviors associated with dementia, including wandering, refusal to eat, and expressions of pain. Interventions include medication, nutritional support, physiotherapy, psychological counseling, and meticulous oral hygiene practices. The plan also suggests complementary therapies like cognitive behavioral therapy, occupational therapy, and mindfulness techniques to improve the patient's quality of life. The document is available on Desklib, a platform offering a wide range of study resources for students.

Running head: NURSING ASSIGNMENT
NURSING ASSIGNMENT
Name of the Student:
Name of the University:
Author Note:
NURSING ASSIGNMENT
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1NURSING ASSIGNMENT
Nursing Care Plan
Part A:
Medical Diagnosis:
The patient Miss Alice Jones who is eighty nine years old, has been residing
at the Minnows aged care facility for a period of one year. Initially, the patient stayed
with her sister and her family, but after the demise of her sister she found it
extremely difficult to manage her living at home. Miss Jones also has a brother who
visits her sometimes. She does not have a wife or children. Her previous medical
history states that she was diagnosed with an episode of Myocardial Infarction 10
years ago. Also, she had been diagnosed with hypertension, osteoarthritis in her
right knee and anxiety and depression. On account of the problem of Osteoarthritis it
can be said that she frequently experiences the sensation of pain in her right knee.
Also, Miss Jones has been recently diagnosed with Alzheimer’s Dementia and
Urinary incontinence. It can be mentioned that the symptoms of Alzheimer’s
Dementia is causing symptoms of confusion in her. She has already experienced
two falls and has also lost weight due to the symptoms of Dementia.
Theory of ageing:
The neuroendocrine theory was proposed by Dilman and Dean and the theory
critically sheds lights on the process of wear and tear of tissues and the role of the
neuroendocrine system on the process (Kuh et al., 2013). It should be noted that the
system operates by the functioning of a complex network of biochemical synthesis
produced by the pituitary gland. The hypothalamus, which is also known as the
master gland directs the synthesis of the hormones which maintain the normal
metabolic processes of the body (Naismith et al., 2013). As the body ages, the
capacity of the hormone regulation deteriorates and the receptors that are
responsible for the uptake of the hormones loses their specificity and the
effectiveness of the hormones in maintaining the normal body functions declines. It
can therefore be stated that the Neuroendocrine ageing theory appropriately
explains the ageing process of the patient. It is primarily because of the deteriorating
mechanism of the hypothalamus that the patient is experiencing symptoms of the
Alzheimer’s Dementia and depression.
Nursing Care Plan
Part A:
Medical Diagnosis:
The patient Miss Alice Jones who is eighty nine years old, has been residing
at the Minnows aged care facility for a period of one year. Initially, the patient stayed
with her sister and her family, but after the demise of her sister she found it
extremely difficult to manage her living at home. Miss Jones also has a brother who
visits her sometimes. She does not have a wife or children. Her previous medical
history states that she was diagnosed with an episode of Myocardial Infarction 10
years ago. Also, she had been diagnosed with hypertension, osteoarthritis in her
right knee and anxiety and depression. On account of the problem of Osteoarthritis it
can be said that she frequently experiences the sensation of pain in her right knee.
Also, Miss Jones has been recently diagnosed with Alzheimer’s Dementia and
Urinary incontinence. It can be mentioned that the symptoms of Alzheimer’s
Dementia is causing symptoms of confusion in her. She has already experienced
two falls and has also lost weight due to the symptoms of Dementia.
Theory of ageing:
The neuroendocrine theory was proposed by Dilman and Dean and the theory
critically sheds lights on the process of wear and tear of tissues and the role of the
neuroendocrine system on the process (Kuh et al., 2013). It should be noted that the
system operates by the functioning of a complex network of biochemical synthesis
produced by the pituitary gland. The hypothalamus, which is also known as the
master gland directs the synthesis of the hormones which maintain the normal
metabolic processes of the body (Naismith et al., 2013). As the body ages, the
capacity of the hormone regulation deteriorates and the receptors that are
responsible for the uptake of the hormones loses their specificity and the
effectiveness of the hormones in maintaining the normal body functions declines. It
can therefore be stated that the Neuroendocrine ageing theory appropriately
explains the ageing process of the patient. It is primarily because of the deteriorating
mechanism of the hypothalamus that the patient is experiencing symptoms of the
Alzheimer’s Dementia and depression.
2NURSING ASSIGNMENT
Physiology of ageing:
The process of ageing in unavoidable and starts at conception and continues
till the end of life. The genetic component and the environmental experience is
reflected by the body at any age. The bodies critically reflect the genetic capability of
the body to respond to tissue wear and tear and diseases. Ageing reduces the
thickness of the dermis by 20% and the skin loses the properties of vascularity,
cellularity and sensitivity (Vernooij-Dassen & Moniz-Cook, 2014). The skin loses the
ability to retain internal heat and becomes fragile. Ageing also reduces the size,
elasticity and muscular strength of the muscles mass. The muscle fibres diminish in
diameter due to reduction of ATP, glycogen, myoglobin and myofibrils (Abereen &
Bye, 2013). This makes the body susceptible to injuries and persisting pain. Ageing
also leads to diminishing lung function and stiffness of the chest wall. This makes the
process of gaseous exchange difficult. In addition to this, ageing also leads to the
declining of cardiovascular functions, endocrine metabolism and neurosensory
functions. It can hence be mentioned that the physiology of ageing relates with the
symptoms of depression, dementia and poor muscular strength in the patient.
Primary health services:
On closely assessing the medical history of the patient, it can be stated that
the two primary health services that must be immediately provided to the patient
would include, conducting a comprehensive neurological assessment of the patient
and monitoring the pulse rate and heart-beat of the patient. The rationale for the
recommendation of neurological assessment can be explained as the diagnosed
disease condition of Dementia. As has already been reported that the patient is
suffering from Dementia, conducting a neurological assessment would help in
understanding the pattern of neurological tremors (Jung, 2015). The results would
help in prescribing medication and modifying the dose of the medication. The
rationale for the recommendation of the continued monitoring of pulse rate and heart
beat through pulse oximetry can be explained as the increased susceptibility of the
patient to suffer from a cardiac arrest or brain stroke due to advancing age. In
addition to this, regular monitoring of the vital; signs and frequent blood test analysis
would help in understanding the functioning of the body. It would help in detecting
Physiology of ageing:
The process of ageing in unavoidable and starts at conception and continues
till the end of life. The genetic component and the environmental experience is
reflected by the body at any age. The bodies critically reflect the genetic capability of
the body to respond to tissue wear and tear and diseases. Ageing reduces the
thickness of the dermis by 20% and the skin loses the properties of vascularity,
cellularity and sensitivity (Vernooij-Dassen & Moniz-Cook, 2014). The skin loses the
ability to retain internal heat and becomes fragile. Ageing also reduces the size,
elasticity and muscular strength of the muscles mass. The muscle fibres diminish in
diameter due to reduction of ATP, glycogen, myoglobin and myofibrils (Abereen &
Bye, 2013). This makes the body susceptible to injuries and persisting pain. Ageing
also leads to diminishing lung function and stiffness of the chest wall. This makes the
process of gaseous exchange difficult. In addition to this, ageing also leads to the
declining of cardiovascular functions, endocrine metabolism and neurosensory
functions. It can hence be mentioned that the physiology of ageing relates with the
symptoms of depression, dementia and poor muscular strength in the patient.
Primary health services:
On closely assessing the medical history of the patient, it can be stated that
the two primary health services that must be immediately provided to the patient
would include, conducting a comprehensive neurological assessment of the patient
and monitoring the pulse rate and heart-beat of the patient. The rationale for the
recommendation of neurological assessment can be explained as the diagnosed
disease condition of Dementia. As has already been reported that the patient is
suffering from Dementia, conducting a neurological assessment would help in
understanding the pattern of neurological tremors (Jung, 2015). The results would
help in prescribing medication and modifying the dose of the medication. The
rationale for the recommendation of the continued monitoring of pulse rate and heart
beat through pulse oximetry can be explained as the increased susceptibility of the
patient to suffer from a cardiac arrest or brain stroke due to advancing age. In
addition to this, regular monitoring of the vital; signs and frequent blood test analysis
would help in understanding the functioning of the body. It would help in detecting
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3NURSING ASSIGNMENT
the slightest abnormality and accordingly appropriate measures could be undertaken
to control the condition (Borson et al., 2013).
Strategies and Interventions for dementia/challenging behaviours:
Alzheimer’s Dementia is accompanied with a number of challenging
behaviours which becomes extremely difficult to manage for care professionals.
Studies have reported that Dementia might present symptoms of a different
personality which is separate from the natural trait of the patient and this makes
managing the disease, all the more difficult. It should be mentioned here the
common challenging behaviours include behavioural problems, behavioural as well
as psychological symptoms of Dementia, behaviour transitions, difficult behaviours,
disruptive behaviours, inappropriate behaviours, behavioural symptoms and acting
out (Prince et al., 2013).
While caring for the patient in the case-study, the application of the following
strategies can help in effectively managing the patient. The patient has been
reported to be roaming aimlessly during the night hours within the residential care
facility. Wandering without assistance would make the patient susceptible to
accidental fall and injuries which would cause substantial wear and tear of tissues. In
order to avoid the tendency of the patient to wander during the night hours, it is
critically important to ensure that the patient sleeps peacefully through the night. To
assure the same, administration of mild dosage of Diazepam could help in inducing
peaceful sleep to the patient. Diazepam comprises of the chemical ingredient
benzodiazepine which comprises of sedative properties and helps in inducing sleep
to the patient. Studies suggest that Diazepam is an effective sedative drug that can
be prescribed to Dementia patients in order to induce peaceful sleep (Van De Glind
et al., 2013). Also, the previous medical history of the patient does not report the
presence of any allergies and that makes the drug safe for administration.
The second challenging behaviour identified in relation to the patient includes
the refusal to consume meals. The case study suggests that the on account of
memory impairment, a number of times, the meals of the patient are returned intact.
Research studies on the physiology of ageing suggest that with the progression of
age the body becomes susceptible to a number of infections and weakened immune
responses (Borson et al., 2013). The consumption of an optimal diet enriched with
the slightest abnormality and accordingly appropriate measures could be undertaken
to control the condition (Borson et al., 2013).
Strategies and Interventions for dementia/challenging behaviours:
Alzheimer’s Dementia is accompanied with a number of challenging
behaviours which becomes extremely difficult to manage for care professionals.
Studies have reported that Dementia might present symptoms of a different
personality which is separate from the natural trait of the patient and this makes
managing the disease, all the more difficult. It should be mentioned here the
common challenging behaviours include behavioural problems, behavioural as well
as psychological symptoms of Dementia, behaviour transitions, difficult behaviours,
disruptive behaviours, inappropriate behaviours, behavioural symptoms and acting
out (Prince et al., 2013).
While caring for the patient in the case-study, the application of the following
strategies can help in effectively managing the patient. The patient has been
reported to be roaming aimlessly during the night hours within the residential care
facility. Wandering without assistance would make the patient susceptible to
accidental fall and injuries which would cause substantial wear and tear of tissues. In
order to avoid the tendency of the patient to wander during the night hours, it is
critically important to ensure that the patient sleeps peacefully through the night. To
assure the same, administration of mild dosage of Diazepam could help in inducing
peaceful sleep to the patient. Diazepam comprises of the chemical ingredient
benzodiazepine which comprises of sedative properties and helps in inducing sleep
to the patient. Studies suggest that Diazepam is an effective sedative drug that can
be prescribed to Dementia patients in order to induce peaceful sleep (Van De Glind
et al., 2013). Also, the previous medical history of the patient does not report the
presence of any allergies and that makes the drug safe for administration.
The second challenging behaviour identified in relation to the patient includes
the refusal to consume meals. The case study suggests that the on account of
memory impairment, a number of times, the meals of the patient are returned intact.
Research studies on the physiology of ageing suggest that with the progression of
age the body becomes susceptible to a number of infections and weakened immune
responses (Borson et al., 2013). The consumption of an optimal diet enriched with
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

4NURSING ASSIGNMENT
adequate nourishment helps in supplying nutrients to the body that helps in
maintaining normal metabolic functions. The intervention strategy for monitoring the
nutritional intake of the patient would include the referral to a nutritionist. The
nutritionist would closely monitor the dietary and water intake of the patient by
keeping a track on the meal consumption pattern. Further, the nutritionist would also
customise a diet plan aligned to the nutritious need of the patient so as to ensure
proper diet intake of the patient.
The third challenging behaviour identified in relation to the patient mentioned
in the case study includes her confused comment on experiencing pain. The case
study suggests that the patient complains of an intense sensation of pain in her right
knee, however on asking her to describe about the pain, she is confused and is not
able to provide correct information. This suggests that the patient is experiencing
symptoms of confusion pertaining to Dementia but that does not rule out her feeling
of pain. The intervention strategy would include, frequently conducting a pain
assessment of the patient and the referral of a physiotherapist. The rationale for the
referral of a physiotherapist can be explained as the assistance offered to the patient
by imparting mild physical exercise training which could help in bringing relief to the
patient (Forbes et al., 2015; Livingston et al., 2017). Further, the physiotherapist
would also impart training about energy saving techniques which could help the
patient acquire relief from the pertinent sensation of pain.
The fourth challenging behaviour that can be identified in close association to
the case study would include controlling the symptoms of depression of the patient.
The case study suggests that the patient has recently been looking for her sister who
is no more alive. It is important to take note of the emotional bond that the patient
had shared with her sister. The symptoms of impaired memory can be attributed as
the cause that has made her forget about the major life events. Studies suggest that
Dementia patients within residential care facilities are susceptible to develop feelings
of loneliness and depression (Aberdeen & Bye, 2013). It is therefore important to
foster an emotionally safe care environment for the patient, where the patient would
be treated with empathy (Prorok et al., 2013; Tranvag et al., 2013). The intervention
strategy to ensure the same would include the referral of the patient to a
psychological counsellor. The rationale for the same can be explained as the
administration of counselling to effectively help the patient deal with the feelings of
adequate nourishment helps in supplying nutrients to the body that helps in
maintaining normal metabolic functions. The intervention strategy for monitoring the
nutritional intake of the patient would include the referral to a nutritionist. The
nutritionist would closely monitor the dietary and water intake of the patient by
keeping a track on the meal consumption pattern. Further, the nutritionist would also
customise a diet plan aligned to the nutritious need of the patient so as to ensure
proper diet intake of the patient.
The third challenging behaviour identified in relation to the patient mentioned
in the case study includes her confused comment on experiencing pain. The case
study suggests that the patient complains of an intense sensation of pain in her right
knee, however on asking her to describe about the pain, she is confused and is not
able to provide correct information. This suggests that the patient is experiencing
symptoms of confusion pertaining to Dementia but that does not rule out her feeling
of pain. The intervention strategy would include, frequently conducting a pain
assessment of the patient and the referral of a physiotherapist. The rationale for the
referral of a physiotherapist can be explained as the assistance offered to the patient
by imparting mild physical exercise training which could help in bringing relief to the
patient (Forbes et al., 2015; Livingston et al., 2017). Further, the physiotherapist
would also impart training about energy saving techniques which could help the
patient acquire relief from the pertinent sensation of pain.
The fourth challenging behaviour that can be identified in close association to
the case study would include controlling the symptoms of depression of the patient.
The case study suggests that the patient has recently been looking for her sister who
is no more alive. It is important to take note of the emotional bond that the patient
had shared with her sister. The symptoms of impaired memory can be attributed as
the cause that has made her forget about the major life events. Studies suggest that
Dementia patients within residential care facilities are susceptible to develop feelings
of loneliness and depression (Aberdeen & Bye, 2013). It is therefore important to
foster an emotionally safe care environment for the patient, where the patient would
be treated with empathy (Prorok et al., 2013; Tranvag et al., 2013). The intervention
strategy to ensure the same would include the referral of the patient to a
psychological counsellor. The rationale for the same can be explained as the
administration of counselling to effectively help the patient deal with the feelings of
5NURSING ASSIGNMENT
loneliness and reinforce an optimistic approach towards recovery (Sjogren et al.,
2013).
Oral hygiene:
The information provided in the case study suggests that the patient requires
complete assistance with dental care. The patient contains complete lower dentures
and partial upper dentures. It has also been reported that the patient is often
confused and this makes it likely that she would compromise with her personal
hygiene. Poor oral hygiene could lead to infection in her oral cavity and also cause
dental cavities and mouth ulcers. Therefore, it is extremely important to ensure that
the oral hygiene of the patient is maintained. The strategies that could help in the
maintenance of oral hygiene would include the appointment of a care professional
who would maintain the oral hygiene of the patient and also offer assistance with
activities of daily living (ADLs). In addition to a tracker sheet would be maintained
with the care professional who would document the timing and material used to
maintain oral hygiene of the patient twice a day, during the morning, prior to
breakfast as well as after dinner during the night. The tracker would help in ensuring
that the oral hygiene routine has been followed for the patient.
Pain:
The case-study already suggests that the patient is already prescribed
medication for the treatment of pain. The prescribed medications Prn Panadol 1grm
tds, Voltaren Emulgen to right knee and Tramadol 50 mg PRN is ideally prescribed
for the management of the symptom of pain. However, it is difficult to identify that
whether or not the patient is experiencing pain as the patient is confused and is
unable to provide correct information about the type of pain. In order to effectively
manage the symptom of pain, the patient would be referred to a physiotherapist. The
physiotherapist would conduct pain assessments to assess the quality of pain and
also administer mild physical exercise training to the patient which could help the
patient in dealing with the symptom of pain.
Complementary Therapies:
The complementary therapies that could potentially benefit the patient and
promote accelerated recovery would include, administration of cognitive behavioural
loneliness and reinforce an optimistic approach towards recovery (Sjogren et al.,
2013).
Oral hygiene:
The information provided in the case study suggests that the patient requires
complete assistance with dental care. The patient contains complete lower dentures
and partial upper dentures. It has also been reported that the patient is often
confused and this makes it likely that she would compromise with her personal
hygiene. Poor oral hygiene could lead to infection in her oral cavity and also cause
dental cavities and mouth ulcers. Therefore, it is extremely important to ensure that
the oral hygiene of the patient is maintained. The strategies that could help in the
maintenance of oral hygiene would include the appointment of a care professional
who would maintain the oral hygiene of the patient and also offer assistance with
activities of daily living (ADLs). In addition to a tracker sheet would be maintained
with the care professional who would document the timing and material used to
maintain oral hygiene of the patient twice a day, during the morning, prior to
breakfast as well as after dinner during the night. The tracker would help in ensuring
that the oral hygiene routine has been followed for the patient.
Pain:
The case-study already suggests that the patient is already prescribed
medication for the treatment of pain. The prescribed medications Prn Panadol 1grm
tds, Voltaren Emulgen to right knee and Tramadol 50 mg PRN is ideally prescribed
for the management of the symptom of pain. However, it is difficult to identify that
whether or not the patient is experiencing pain as the patient is confused and is
unable to provide correct information about the type of pain. In order to effectively
manage the symptom of pain, the patient would be referred to a physiotherapist. The
physiotherapist would conduct pain assessments to assess the quality of pain and
also administer mild physical exercise training to the patient which could help the
patient in dealing with the symptom of pain.
Complementary Therapies:
The complementary therapies that could potentially benefit the patient and
promote accelerated recovery would include, administration of cognitive behavioural
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6NURSING ASSIGNMENT
therapies and referral to an occupational therapist. In addition to this, administration
of mindfulness based therapies such as yoga and meditation and using the
reminiscence and life story therapy can help in effectively treating the symptoms of
Dementia. The rationale for the recommendation of the complementary therapies
include the success rate in the evidence bases that suggest that the administration
of the mentioned therapies could help in managing the challenging symptoms. The
cognitive stimulation therapy makes use of group activities as well as exercises to
substantially improve memory skills, problem solving skills and also improves the
language ability (Prince et al., 2013). Also, as has been mentioned that the patient
does not like to involve herself in social gatherings, the administration of mindfulness
based therapies such as yoga and meditation can help in fostering peace and
optimism in her which would improve her symptoms (Naismith et al., 2013). The
reminiscence or the life story therapy is comparatively a new approach that makes
use of past life events, music or photographs to evoke a good feeling among the
patient (Forbes et al., 2015). Research studies indicate that the use of the
reminiscence therapy helps in improving the quality of mood in Dementia patients
(Livingston et al., 2017).
Part B:
Nursing
Diagnosis
Patient
Goals
Intervention
Rationale
Implementation
(Yes/No)
Evaluation
Outcome
therapies and referral to an occupational therapist. In addition to this, administration
of mindfulness based therapies such as yoga and meditation and using the
reminiscence and life story therapy can help in effectively treating the symptoms of
Dementia. The rationale for the recommendation of the complementary therapies
include the success rate in the evidence bases that suggest that the administration
of the mentioned therapies could help in managing the challenging symptoms. The
cognitive stimulation therapy makes use of group activities as well as exercises to
substantially improve memory skills, problem solving skills and also improves the
language ability (Prince et al., 2013). Also, as has been mentioned that the patient
does not like to involve herself in social gatherings, the administration of mindfulness
based therapies such as yoga and meditation can help in fostering peace and
optimism in her which would improve her symptoms (Naismith et al., 2013). The
reminiscence or the life story therapy is comparatively a new approach that makes
use of past life events, music or photographs to evoke a good feeling among the
patient (Forbes et al., 2015). Research studies indicate that the use of the
reminiscence therapy helps in improving the quality of mood in Dementia patients
(Livingston et al., 2017).
Part B:
Nursing
Diagnosis
Patient
Goals
Intervention
Rationale
Implementation
(Yes/No)
Evaluation
Outcome
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURSING ASSIGNMENT
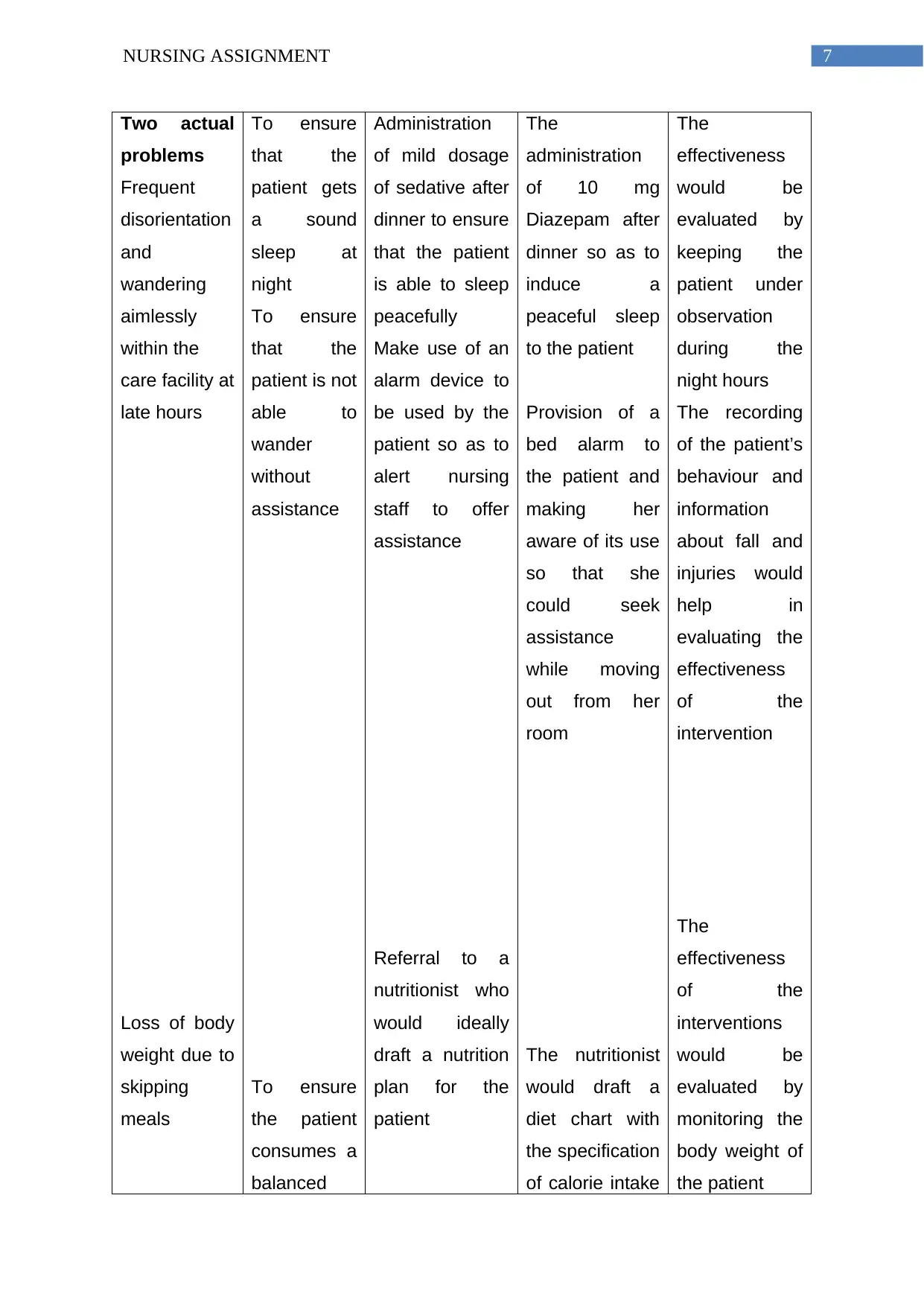
Two actual
problems
Frequent
disorientation
and
wandering
aimlessly
within the
care facility at
late hours
Loss of body
weight due to
skipping
meals
To ensure
that the
patient gets
a sound
sleep at
night
To ensure
that the
patient is not
able to
wander
without
assistance
To ensure
the patient
consumes a
balanced
Administration
of mild dosage
of sedative after
dinner to ensure
that the patient
is able to sleep
peacefully
Make use of an
alarm device to
be used by the
patient so as to
alert nursing
staff to offer
assistance
Referral to a
nutritionist who
would ideally
draft a nutrition
plan for the
patient
The
administration
of 10 mg
Diazepam after
dinner so as to
induce a
peaceful sleep
to the patient
Provision of a
bed alarm to
the patient and
making her
aware of its use
so that she
could seek
assistance
while moving
out from her
room
The nutritionist
would draft a
diet chart with
the specification
of calorie intake
The
effectiveness
would be
evaluated by
keeping the
patient under
observation
during the
night hours
The recording
of the patient’s
behaviour and
information
about fall and
injuries would
help in
evaluating the
effectiveness
of the
intervention
The
effectiveness
of the
interventions
would be
evaluated by
monitoring the
body weight of
the patient
Two actual
problems
Frequent
disorientation
and
wandering
aimlessly
within the
care facility at
late hours
Loss of body
weight due to
skipping
meals
To ensure
that the
patient gets
a sound
sleep at
night
To ensure
that the
patient is not
able to
wander
without
assistance
To ensure
the patient
consumes a
balanced
Administration
of mild dosage
of sedative after
dinner to ensure
that the patient
is able to sleep
peacefully
Make use of an
alarm device to
be used by the
patient so as to
alert nursing
staff to offer
assistance
Referral to a
nutritionist who
would ideally
draft a nutrition
plan for the
patient
The
administration
of 10 mg
Diazepam after
dinner so as to
induce a
peaceful sleep
to the patient
Provision of a
bed alarm to
the patient and
making her
aware of its use
so that she
could seek
assistance
while moving
out from her
room
The nutritionist
would draft a
diet chart with
the specification
of calorie intake
The
effectiveness
would be
evaluated by
keeping the
patient under
observation
during the
night hours
The recording
of the patient’s
behaviour and
information
about fall and
injuries would
help in
evaluating the
effectiveness
of the
intervention
The
effectiveness
of the
interventions
would be
evaluated by
monitoring the
body weight of
the patient
8NURSING ASSIGNMENT
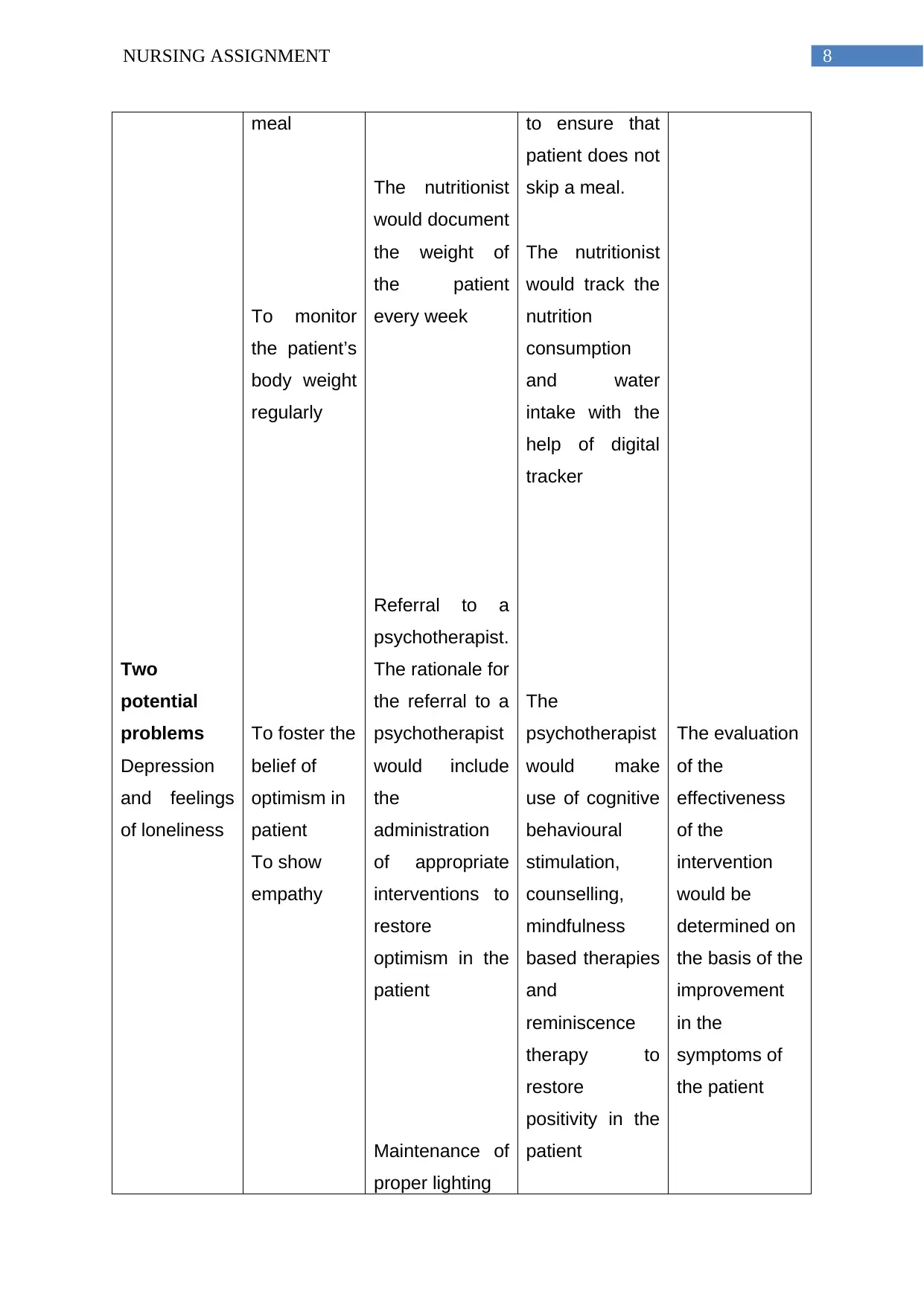
Two
potential
problems
Depression
and feelings
of loneliness
meal
To monitor
the patient’s
body weight
regularly
To foster the
belief of
optimism in
patient
To show
empathy
The nutritionist
would document
the weight of
the patient
every week
Referral to a
psychotherapist.
The rationale for
the referral to a
psychotherapist
would include
the
administration
of appropriate
interventions to
restore
optimism in the
patient
Maintenance of
proper lighting
to ensure that
patient does not
skip a meal.
The nutritionist
would track the
nutrition
consumption
and water
intake with the
help of digital
tracker
The
psychotherapist
would make
use of cognitive
behavioural
stimulation,
counselling,
mindfulness
based therapies
and
reminiscence
therapy to
restore
positivity in the
patient
The evaluation
of the
effectiveness
of the
intervention
would be
determined on
the basis of the
improvement
in the
symptoms of
the patient
Two
potential
problems
Depression
and feelings
of loneliness
meal
To monitor
the patient’s
body weight
regularly
To foster the
belief of
optimism in
patient
To show
empathy
The nutritionist
would document
the weight of
the patient
every week
Referral to a
psychotherapist.
The rationale for
the referral to a
psychotherapist
would include
the
administration
of appropriate
interventions to
restore
optimism in the
patient
Maintenance of
proper lighting
to ensure that
patient does not
skip a meal.
The nutritionist
would track the
nutrition
consumption
and water
intake with the
help of digital
tracker
The
psychotherapist
would make
use of cognitive
behavioural
stimulation,
counselling,
mindfulness
based therapies
and
reminiscence
therapy to
restore
positivity in the
patient
The evaluation
of the
effectiveness
of the
intervention
would be
determined on
the basis of the
improvement
in the
symptoms of
the patient
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9NURSING ASSIGNMENT
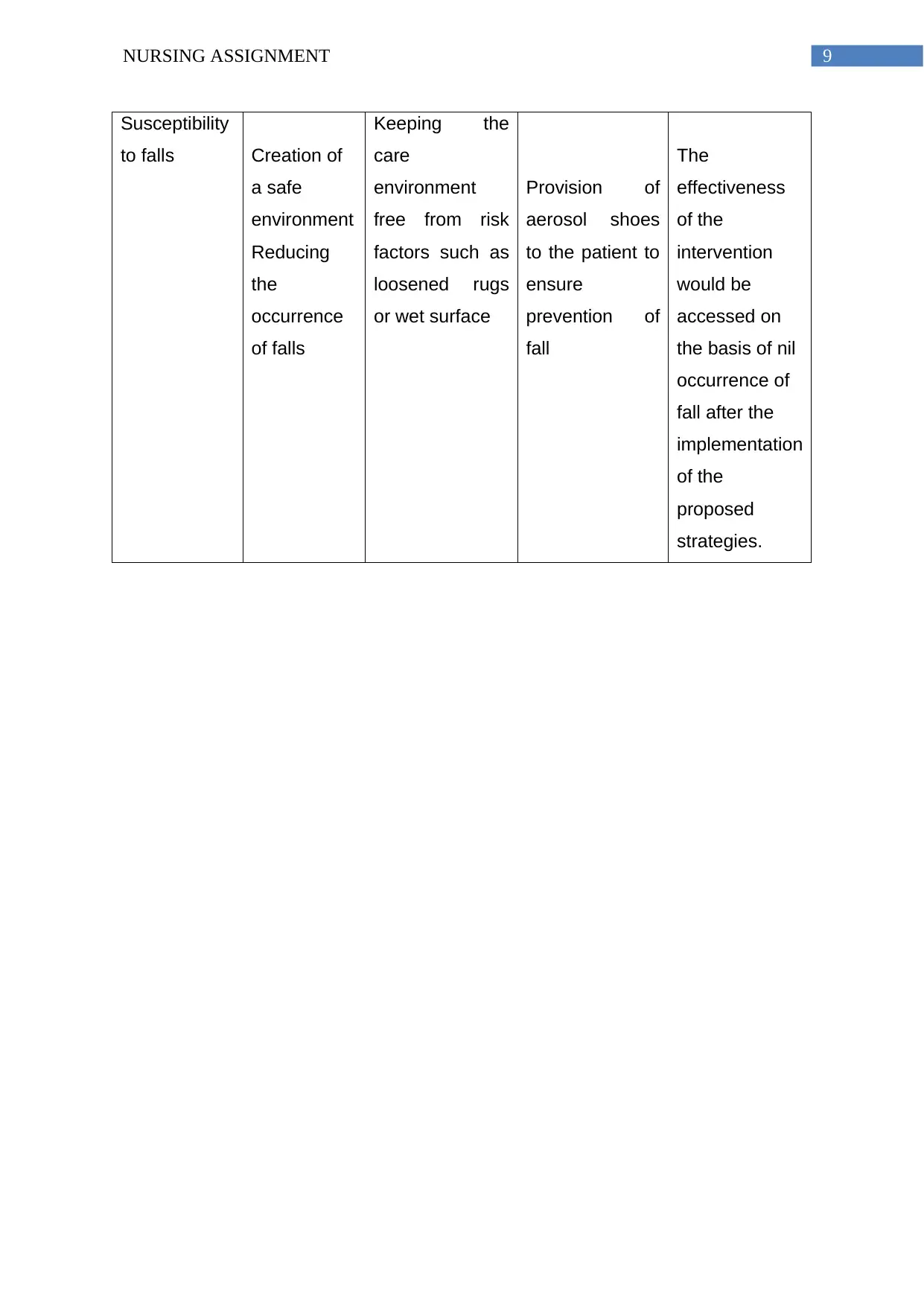
Susceptibility
to falls Creation of
a safe
environment
Reducing
the
occurrence
of falls
Keeping the
care
environment
free from risk
factors such as
loosened rugs
or wet surface
Provision of
aerosol shoes
to the patient to
ensure
prevention of
fall
The
effectiveness
of the
intervention
would be
accessed on
the basis of nil
occurrence of
fall after the
implementation
of the
proposed
strategies.
Susceptibility
to falls Creation of
a safe
environment
Reducing
the
occurrence
of falls
Keeping the
care
environment
free from risk
factors such as
loosened rugs
or wet surface
Provision of
aerosol shoes
to the patient to
ensure
prevention of
fall
The
effectiveness
of the
intervention
would be
accessed on
the basis of nil
occurrence of
fall after the
implementation
of the
proposed
strategies.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10NURSING ASSIGNMENT
References:
Aberdeen, L., & Bye, L. A. (2013). Challenges for Australian sociology: Critical
ageing research–ageing well?. Journal of Sociology, 49(1), 3-21.
Borson, S., Frank, L., Bayley, P. J., Boustani, M., Dean, M., Lin, P. J., ... &
Stefanacci, R. G. (2013). Improving dementia care: the role of screening and
detection of cognitive impairment. Alzheimer's & Dementia, 9(2), 151-159.
Forbes, D., Forbes, S. C., Blake, C. M., Thiessen, E. J., & Forbes, S. (2015).
Exercise programs for people with dementia. Cochrane Database of
Systematic Reviews, (4).
Jung, C. G. (2015). Psychology of dementia praecox (Vol. 1294). Princeton
University Press.
Kuh, D., Cooper, R., Hardy, R., Richards, M., & Ben-Shlomo, Y. (Eds.). (2013). A life
course approach to healthy ageing. OUP Oxford.
Livingston, G., Sommerlad, A., Orgeta, V., Costafreda, S. G., Huntley, J., Ames,
D., ... & Cooper, C. (2017). Dementia prevention, intervention, and care. The
Lancet, 390(10113), 2673-2734.
Naismith, S. L., Mowszowski, L., Diamond, K., & Lewis, S. J. (2013). Improving
memory in Parkinson's disease: a healthy brain ageing cognitive training
program. Movement Disorders, 28(8), 1097-1103.
Prince, M., Bryce, R., Albanese, E., Wimo, A., Ribeiro, W., & Ferri, C. P. (2013). The
global prevalence of dementia: a systematic review and
metaanalysis. Alzheimer's & dementia, 9(1), 63-75.
Prorok, J. C., Horgan, S., & Seitz, D. P. (2013). Health care experiences of people
with dementia and their caregivers: a meta-ethnographic analysis of
qualitative studies. Cmaj, 185(14), E669-E680.
Sjögren, K., Lindkvist, M., Sandman, P. O., Zingmark, K., & Edvardsson, D. (2013).
Person‐centredness and its association with resident well‐being in dementia
care units. Journal of Advanced Nursing, 69(10), 2196-2206.
References:
Aberdeen, L., & Bye, L. A. (2013). Challenges for Australian sociology: Critical
ageing research–ageing well?. Journal of Sociology, 49(1), 3-21.
Borson, S., Frank, L., Bayley, P. J., Boustani, M., Dean, M., Lin, P. J., ... &
Stefanacci, R. G. (2013). Improving dementia care: the role of screening and
detection of cognitive impairment. Alzheimer's & Dementia, 9(2), 151-159.
Forbes, D., Forbes, S. C., Blake, C. M., Thiessen, E. J., & Forbes, S. (2015).
Exercise programs for people with dementia. Cochrane Database of
Systematic Reviews, (4).
Jung, C. G. (2015). Psychology of dementia praecox (Vol. 1294). Princeton
University Press.
Kuh, D., Cooper, R., Hardy, R., Richards, M., & Ben-Shlomo, Y. (Eds.). (2013). A life
course approach to healthy ageing. OUP Oxford.
Livingston, G., Sommerlad, A., Orgeta, V., Costafreda, S. G., Huntley, J., Ames,
D., ... & Cooper, C. (2017). Dementia prevention, intervention, and care. The
Lancet, 390(10113), 2673-2734.
Naismith, S. L., Mowszowski, L., Diamond, K., & Lewis, S. J. (2013). Improving
memory in Parkinson's disease: a healthy brain ageing cognitive training
program. Movement Disorders, 28(8), 1097-1103.
Prince, M., Bryce, R., Albanese, E., Wimo, A., Ribeiro, W., & Ferri, C. P. (2013). The
global prevalence of dementia: a systematic review and
metaanalysis. Alzheimer's & dementia, 9(1), 63-75.
Prorok, J. C., Horgan, S., & Seitz, D. P. (2013). Health care experiences of people
with dementia and their caregivers: a meta-ethnographic analysis of
qualitative studies. Cmaj, 185(14), E669-E680.
Sjögren, K., Lindkvist, M., Sandman, P. O., Zingmark, K., & Edvardsson, D. (2013).
Person‐centredness and its association with resident well‐being in dementia
care units. Journal of Advanced Nursing, 69(10), 2196-2206.

11NURSING ASSIGNMENT
Tranvåg, O., Petersen, K. A., & Nåden, D. (2013). Dignity-preserving dementia care:
a metasynthesis. Nursing Ethics, 20(8), 861-880.
Van De Glind, E. M., Van Enst, W. A., Van Munster, B. C., Rikkert, M. G. O.,
Scheltens, P., Scholten, R. J., & Hooft, L. (2013). Pharmacological treatment
of dementia: a scoping review of systematic reviews. Dementia and geriatric
cognitive disorders, 36(3-4), 211-228.
Vernooij-Dassen, M., & Moniz-Cook, E. (2014). Raising the standard of applied
dementia care research: addressing the implementation error.
Tranvåg, O., Petersen, K. A., & Nåden, D. (2013). Dignity-preserving dementia care:
a metasynthesis. Nursing Ethics, 20(8), 861-880.
Van De Glind, E. M., Van Enst, W. A., Van Munster, B. C., Rikkert, M. G. O.,
Scheltens, P., Scholten, R. J., & Hooft, L. (2013). Pharmacological treatment
of dementia: a scoping review of systematic reviews. Dementia and geriatric
cognitive disorders, 36(3-4), 211-228.
Vernooij-Dassen, M., & Moniz-Cook, E. (2014). Raising the standard of applied
dementia care research: addressing the implementation error.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



