Alzheimer’s Disease | Presentation
Identification of a disease from a case study and production of a Narrated Microsoft PowerPoint Poster.
1 Pages1591 Words29 Views
Added on 2022-09-18
Alzheimer’s Disease | Presentation
Identification of a disease from a case study and production of a Narrated Microsoft PowerPoint Poster.
Added on 2022-09-18
ShareRelated Documents
`
In order to diagnose Alzheimer's dementia, a doctor trained in brain
conditions (neurologist) or a doctor trained to treat older adults
(geriatrician) will examine the patient's medical history, history of
medication and symptoms. Assessments may be performed as such, as
mental status tests to evaluate reasoning (cognitive) and memory skills.
Doctors use scores on these tests to assess the degree of cognitive
impairment. Neuropsychological tests are performed to determine the
patient's remembrance and (cognitive) reasoning skills. Doctors are also
found to be interviewing a family member or friend with questions about
the patient and their impaired behaviour. Diagonistic tests, such as brain
imaging tests, are performed which show a variety of brain scans that
may show the degeneration caused by brain cells. Magnetic resonance
imaging (MRI) (Sabuncu, Konukoglu and Alzheimer’s Disease
Neuroimaging Initiative, 2015) uses powerful radio waves and magnets to
give a detailed view of your brain. CT scan uses x-rays to obtain cross-
section images of your brain. Positron emission tomography (PET) scan
utilizes a radioactive substance called a tracer to identify compounds in
the body. There are different kinds of PET scans. The most commonly
used PET scan is a PET scan of fluorodeoxyglucose (FDG) which can
identify brain regions with decreased glucose metabolism. Metabolism
patterns can differentiate between different types of degenerative brain
disease. PET scans have recently been developed to locate clumps of
amyloid proteins (plaques) correlated with Alzheimer's dementia.
ALZHEIMER’S DISEASE
Name:
Student ID:
Module Code:
Alzheimer’s Disease:
Pathophysiology:
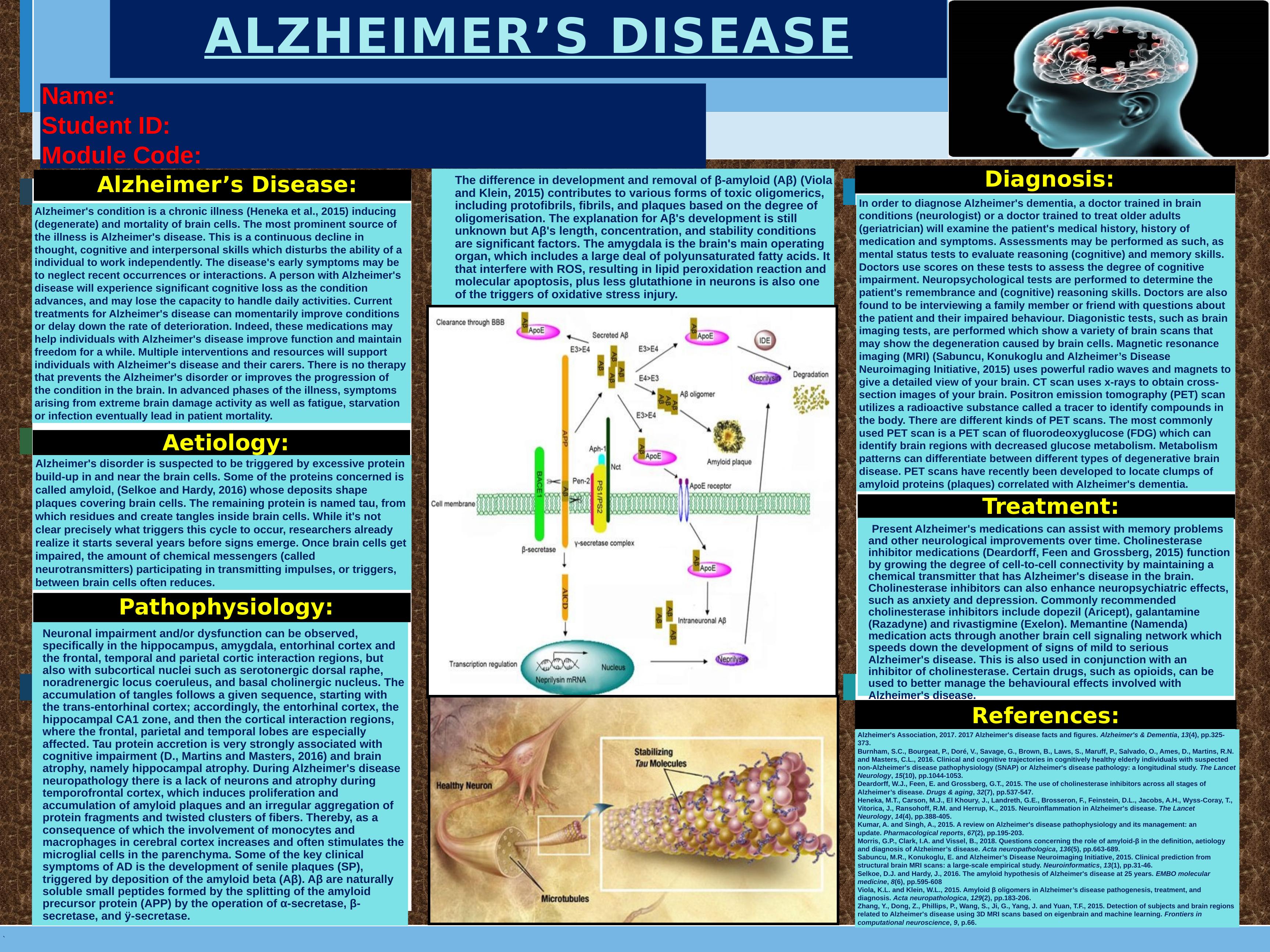
Neuronal impairment and/or dysfunction can be observed,
specifically in the hippocampus, amygdala, entorhinal cortex and
the frontal, temporal and parietal cortic interaction regions, but
also with subcortical nuclei such as serotonergic dorsal raphe,
noradrenergic locus coeruleus, and basal cholinergic nucleus. The
accumulation of tangles follows a given sequence, starting with
the trans-entorhinal cortex; accordingly, the entorhinal cortex, the
hippocampal CA1 zone, and then the cortical interaction regions,
where the frontal, parietal and temporal lobes are especially
affected. Tau protein accretion is very strongly associated with
cognitive impairment (D., Martins and Masters, 2016) and brain
atrophy, namely hippocampal atrophy. During Alzheimer's disease
neuropathology there is a lack of neurons and atrophy during
temporofrontal cortex, which induces proliferation and
accumulation of amyloid plaques and an irregular aggregation of
protein fragments and twisted clusters of fibers. Thereby, as a
consequence of which the involvement of monocytes and
macrophages in cerebral cortex increases and often stimulates the
microglial cells in the parenchyma. Some of the key clinical
symptoms of AD is the development of senile plaques (SP),
triggered by deposition of the amyloid beta (Aβ). Aβ are naturally
soluble small peptides formed by the splitting of the amyloid
precursor protein (APP) by the operation of α-secretase, β-
secretase, and ÿ-secretase.
The difference in development and removal of β-amyloid (Aβ) (Viola
and Klein, 2015) contributes to various forms of toxic oligomerics,
including protofibrils, fibrils, and plaques based on the degree of
oligomerisation. The explanation for Aβ's development is still
unknown but Aβ's length, concentration, and stability conditions
are significant factors. The amygdala is the brain's main operating
organ, which includes a large deal of polyunsaturated fatty acids. It
that interfere with ROS, resulting in lipid peroxidation reaction and
molecular apoptosis, plus less glutathione in neurons is also one
of the triggers of oxidative stress injury.
Diagnosis:
Treatment:
Present Alzheimer's medications can assist with memory problems
and other neurological improvements over time. Cholinesterase
inhibitor medications (Deardorff, Feen and Grossberg, 2015) function
by growing the degree of cell-to-cell connectivity by maintaining a
chemical transmitter that has Alzheimer's disease in the brain.
Cholinesterase inhibitors can also enhance neuropsychiatric effects,
such as anxiety and depression. Commonly recommended
cholinesterase inhibitors include dopezil (Aricept), galantamine
(Razadyne) and rivastigmine (Exelon). Memantine (Namenda)
medication acts through another brain cell signaling network which
speeds down the development of signs of mild to serious
Alzheimer's disease. This is also used in conjunction with an
inhibitor of cholinesterase. Certain drugs, such as opioids, can be
used to better manage the behavioural effects involved with
Alzheimer's disease.
Alzheimer's condition is a chronic illness (Heneka et al., 2015) inducing
(degenerate) and mortality of brain cells. The most prominent source of
the illness is Alzheimer's disease. This is a continuous decline in
thought, cognitive and interpersonal skills which disturbs the ability of a
individual to work independently. The disease's early symptoms may be
to neglect recent occurrences or interactions. A person with Alzheimer's
disease will experience significant cognitive loss as the condition
advances, and may lose the capacity to handle daily activities. Current
treatments for Alzheimer's disease can momentarily improve conditions
or delay down the rate of deterioration. Indeed, these medications may
help individuals with Alzheimer's disease improve function and maintain
freedom for a while. Multiple interventions and resources will support
individuals with Alzheimer's disease and their carers. There is no therapy
that prevents the Alzheimer's disorder or improves the progression of
the condition in the brain. In advanced phases of the illness, symptoms
arising from extreme brain damage activity as well as fatigue, starvation
or infection eventually lead in patient mortality.
The graph above
References:
Alzheimer's Association, 2017. 2017 Alzheimer's disease facts and figures. Alzheimer's & Dementia, 13(4), pp.325-
373.
Burnham, S.C., Bourgeat, P., Doré, V., Savage, G., Brown, B., Laws, S., Maruff, P., Salvado, O., Ames, D., Martins, R.N.
and Masters, C.L., 2016. Clinical and cognitive trajectories in cognitively healthy elderly individuals with suspected
non-Alzheimer's disease pathophysiology (SNAP) or Alzheimer's disease pathology: a longitudinal study. The Lancet
Neurology, 15(10), pp.1044-1053.
Deardorff, W.J., Feen, E. and Grossberg, G.T., 2015. The use of cholinesterase inhibitors across all stages of
Alzheimer’s disease. Drugs & aging, 32(7), pp.537-547.
Heneka, M.T., Carson, M.J., El Khoury, J., Landreth, G.E., Brosseron, F., Feinstein, D.L., Jacobs, A.H., Wyss-Coray, T.,
Vitorica, J., Ransohoff, R.M. and Herrup, K., 2015. Neuroinflammation in Alzheimer's disease. The Lancet
Neurology, 14(4), pp.388-405.
Kumar, A. and Singh, A., 2015. A review on Alzheimer's disease pathophysiology and its management: an
update. Pharmacological reports, 67(2), pp.195-203.
Morris, G.P., Clark, I.A. and Vissel, B., 2018. Questions concerning the role of amyloid-β in the definition, aetiology
and diagnosis of Alzheimer’s disease. Acta neuropathologica, 136(5), pp.663-689.
Sabuncu, M.R., Konukoglu, E. and Alzheimer’s Disease Neuroimaging Initiative, 2015. Clinical prediction from
structural brain MRI scans: a large-scale empirical study. Neuroinformatics, 13(1), pp.31-46.
Selkoe, D.J. and Hardy, J., 2016. The amyloid hypothesis of Alzheimer's disease at 25 years. EMBO molecular
medicine, 8(6), pp.595-608
Viola, K.L. and Klein, W.L., 2015. Amyloid β oligomers in Alzheimer’s disease pathogenesis, treatment, and
diagnosis. Acta neuropathologica, 129(2), pp.183-206.
Zhang, Y., Dong, Z., Phillips, P., Wang, S., Ji, G., Yang, J. and Yuan, T.F., 2015. Detection of subjects and brain regions
related to Alzheimer's disease using 3D MRI scans based on eigenbrain and machine learning. Frontiers in
computational neuroscience, 9, p.66.
Aetiology:
Alzheimer's disorder is suspected to be triggered by excessive protein
build-up in and near the brain cells. Some of the proteins concerned is
called amyloid, (Selkoe and Hardy, 2016) whose deposits shape
plaques covering brain cells. The remaining protein is named tau, from
which residues and create tangles inside brain cells. While it's not
clear precisely what triggers this cycle to occur, researchers already
realize it starts several years before signs emerge. Once brain cells get
impaired, the amount of chemical messengers (called
neurotransmitters) participating in transmitting impulses, or triggers,
between brain cells often reduces.
In order to diagnose Alzheimer's dementia, a doctor trained in brain
conditions (neurologist) or a doctor trained to treat older adults
(geriatrician) will examine the patient's medical history, history of
medication and symptoms. Assessments may be performed as such, as
mental status tests to evaluate reasoning (cognitive) and memory skills.
Doctors use scores on these tests to assess the degree of cognitive
impairment. Neuropsychological tests are performed to determine the
patient's remembrance and (cognitive) reasoning skills. Doctors are also
found to be interviewing a family member or friend with questions about
the patient and their impaired behaviour. Diagonistic tests, such as brain
imaging tests, are performed which show a variety of brain scans that
may show the degeneration caused by brain cells. Magnetic resonance
imaging (MRI) (Sabuncu, Konukoglu and Alzheimer’s Disease
Neuroimaging Initiative, 2015) uses powerful radio waves and magnets to
give a detailed view of your brain. CT scan uses x-rays to obtain cross-
section images of your brain. Positron emission tomography (PET) scan
utilizes a radioactive substance called a tracer to identify compounds in
the body. There are different kinds of PET scans. The most commonly
used PET scan is a PET scan of fluorodeoxyglucose (FDG) which can
identify brain regions with decreased glucose metabolism. Metabolism
patterns can differentiate between different types of degenerative brain
disease. PET scans have recently been developed to locate clumps of
amyloid proteins (plaques) correlated with Alzheimer's dementia.
ALZHEIMER’S DISEASE
Name:
Student ID:
Module Code:
Alzheimer’s Disease:
Pathophysiology:
Neuronal impairment and/or dysfunction can be observed,
specifically in the hippocampus, amygdala, entorhinal cortex and
the frontal, temporal and parietal cortic interaction regions, but
also with subcortical nuclei such as serotonergic dorsal raphe,
noradrenergic locus coeruleus, and basal cholinergic nucleus. The
accumulation of tangles follows a given sequence, starting with
the trans-entorhinal cortex; accordingly, the entorhinal cortex, the
hippocampal CA1 zone, and then the cortical interaction regions,
where the frontal, parietal and temporal lobes are especially
affected. Tau protein accretion is very strongly associated with
cognitive impairment (D., Martins and Masters, 2016) and brain
atrophy, namely hippocampal atrophy. During Alzheimer's disease
neuropathology there is a lack of neurons and atrophy during
temporofrontal cortex, which induces proliferation and
accumulation of amyloid plaques and an irregular aggregation of
protein fragments and twisted clusters of fibers. Thereby, as a
consequence of which the involvement of monocytes and
macrophages in cerebral cortex increases and often stimulates the
microglial cells in the parenchyma. Some of the key clinical
symptoms of AD is the development of senile plaques (SP),
triggered by deposition of the amyloid beta (Aβ). Aβ are naturally
soluble small peptides formed by the splitting of the amyloid
precursor protein (APP) by the operation of α-secretase, β-
secretase, and ÿ-secretase.
The difference in development and removal of β-amyloid (Aβ) (Viola
and Klein, 2015) contributes to various forms of toxic oligomerics,
including protofibrils, fibrils, and plaques based on the degree of
oligomerisation. The explanation for Aβ's development is still
unknown but Aβ's length, concentration, and stability conditions
are significant factors. The amygdala is the brain's main operating
organ, which includes a large deal of polyunsaturated fatty acids. It
that interfere with ROS, resulting in lipid peroxidation reaction and
molecular apoptosis, plus less glutathione in neurons is also one
of the triggers of oxidative stress injury.
Diagnosis:
Treatment:
Present Alzheimer's medications can assist with memory problems
and other neurological improvements over time. Cholinesterase
inhibitor medications (Deardorff, Feen and Grossberg, 2015) function
by growing the degree of cell-to-cell connectivity by maintaining a
chemical transmitter that has Alzheimer's disease in the brain.
Cholinesterase inhibitors can also enhance neuropsychiatric effects,
such as anxiety and depression. Commonly recommended
cholinesterase inhibitors include dopezil (Aricept), galantamine
(Razadyne) and rivastigmine (Exelon). Memantine (Namenda)
medication acts through another brain cell signaling network which
speeds down the development of signs of mild to serious
Alzheimer's disease. This is also used in conjunction with an
inhibitor of cholinesterase. Certain drugs, such as opioids, can be
used to better manage the behavioural effects involved with
Alzheimer's disease.
Alzheimer's condition is a chronic illness (Heneka et al., 2015) inducing
(degenerate) and mortality of brain cells. The most prominent source of
the illness is Alzheimer's disease. This is a continuous decline in
thought, cognitive and interpersonal skills which disturbs the ability of a
individual to work independently. The disease's early symptoms may be
to neglect recent occurrences or interactions. A person with Alzheimer's
disease will experience significant cognitive loss as the condition
advances, and may lose the capacity to handle daily activities. Current
treatments for Alzheimer's disease can momentarily improve conditions
or delay down the rate of deterioration. Indeed, these medications may
help individuals with Alzheimer's disease improve function and maintain
freedom for a while. Multiple interventions and resources will support
individuals with Alzheimer's disease and their carers. There is no therapy
that prevents the Alzheimer's disorder or improves the progression of
the condition in the brain. In advanced phases of the illness, symptoms
arising from extreme brain damage activity as well as fatigue, starvation
or infection eventually lead in patient mortality.
The graph above
References:
Alzheimer's Association, 2017. 2017 Alzheimer's disease facts and figures. Alzheimer's & Dementia, 13(4), pp.325-
373.
Burnham, S.C., Bourgeat, P., Doré, V., Savage, G., Brown, B., Laws, S., Maruff, P., Salvado, O., Ames, D., Martins, R.N.
and Masters, C.L., 2016. Clinical and cognitive trajectories in cognitively healthy elderly individuals with suspected
non-Alzheimer's disease pathophysiology (SNAP) or Alzheimer's disease pathology: a longitudinal study. The Lancet
Neurology, 15(10), pp.1044-1053.
Deardorff, W.J., Feen, E. and Grossberg, G.T., 2015. The use of cholinesterase inhibitors across all stages of
Alzheimer’s disease. Drugs & aging, 32(7), pp.537-547.
Heneka, M.T., Carson, M.J., El Khoury, J., Landreth, G.E., Brosseron, F., Feinstein, D.L., Jacobs, A.H., Wyss-Coray, T.,
Vitorica, J., Ransohoff, R.M. and Herrup, K., 2015. Neuroinflammation in Alzheimer's disease. The Lancet
Neurology, 14(4), pp.388-405.
Kumar, A. and Singh, A., 2015. A review on Alzheimer's disease pathophysiology and its management: an
update. Pharmacological reports, 67(2), pp.195-203.
Morris, G.P., Clark, I.A. and Vissel, B., 2018. Questions concerning the role of amyloid-β in the definition, aetiology
and diagnosis of Alzheimer’s disease. Acta neuropathologica, 136(5), pp.663-689.
Sabuncu, M.R., Konukoglu, E. and Alzheimer’s Disease Neuroimaging Initiative, 2015. Clinical prediction from
structural brain MRI scans: a large-scale empirical study. Neuroinformatics, 13(1), pp.31-46.
Selkoe, D.J. and Hardy, J., 2016. The amyloid hypothesis of Alzheimer's disease at 25 years. EMBO molecular
medicine, 8(6), pp.595-608
Viola, K.L. and Klein, W.L., 2015. Amyloid β oligomers in Alzheimer’s disease pathogenesis, treatment, and
diagnosis. Acta neuropathologica, 129(2), pp.183-206.
Zhang, Y., Dong, Z., Phillips, P., Wang, S., Ji, G., Yang, J. and Yuan, T.F., 2015. Detection of subjects and brain regions
related to Alzheimer's disease using 3D MRI scans based on eigenbrain and machine learning. Frontiers in
computational neuroscience, 9, p.66.
Aetiology:
Alzheimer's disorder is suspected to be triggered by excessive protein
build-up in and near the brain cells. Some of the proteins concerned is
called amyloid, (Selkoe and Hardy, 2016) whose deposits shape
plaques covering brain cells. The remaining protein is named tau, from
which residues and create tangles inside brain cells. While it's not
clear precisely what triggers this cycle to occur, researchers already
realize it starts several years before signs emerge. Once brain cells get
impaired, the amount of chemical messengers (called
neurotransmitters) participating in transmitting impulses, or triggers,
between brain cells often reduces.
End of preview
Want to access all the pages? Upload your documents or become a member.
Related Documents
Care for Older People - Case Studylg...
|11
|3312
|26
NUR104 Assessment Task 3: Case Study Analysislg...
|7
|3269
|273
Alzheimer Disease Project PDFlg...
|14
|3441
|143
Pathophysiology Flow Guide for Alzheimers Diseaselg...
|2
|200
|332
Systematic Review in Neurosciencelg...
|19
|4643
|30
Herpes Simplex Virus: Researchlg...
|5
|1590
|202
