Mental Health Assessment and Recovery Models
VerifiedAdded on 2021/04/24
|13
|4089
|95
AI Summary
This assignment involves a thorough examination of mental health assessments and recovery models. It covers various sources, including books, journals, and online resources, that provide insights into the topic. The assignment requires careful analysis and understanding of the subject matter, making it an excellent resource for students looking to improve their knowledge in this area.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: ASSESSMENT ANALYSIS IN MENTAL HEALTH NURSING
Assessment analysis in mental health nursing
Name of the student:
Name of the University:
Author’s note
Assessment analysis in mental health nursing
Name of the student:
Name of the University:
Author’s note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1ASSESSMENT ANALYSIS IN MENTAL HEALTH NURSING
Task 1: Mental health assessment and recovery focussed care plan
Introduction:
Mental health assessment is a systematic approach to assess the overall psychological
functioning of an individual based on different parameters like appearance, behaviour, mental
appearance and many others. This paper provides detail on mental state assessment done for a
client named Mr. A, a 35 year old man (hypothetical client) who came to a primary care clinic
complaining about symptoms of low mood and irritation since the last three months. The mental
state examination was done in an enclosed room and no other family members accompanied the
client during the assessment. The assessment was done based on single interactions. The paper
describes the results of the mental status assessment and the recovery focused care plan made for
the client based on assessment.
Mental status assessment:
Level of consciousness:
Clinical assessment: The level of consciousness was determined using the Glasgow coma scale. Verbal
response, eye opening and motor response of the client were assessed (Teasdale et al., 2014). Patient was
found in a confused fstate and he seemed lethargic too. The client also reported about not getting sound
sleep (Ma et al., 2015). Evidence suggests that sleep deprivation can have negative impact on behaviour
and it can reverse periods of consciousness (Cologan et al., 2010).
Assessment question:
1. Is the patient lethargic during the interaction?
2. Was the patient found to be in a confused state?
References:
Task 1: Mental health assessment and recovery focussed care plan
Introduction:
Mental health assessment is a systematic approach to assess the overall psychological
functioning of an individual based on different parameters like appearance, behaviour, mental
appearance and many others. This paper provides detail on mental state assessment done for a
client named Mr. A, a 35 year old man (hypothetical client) who came to a primary care clinic
complaining about symptoms of low mood and irritation since the last three months. The mental
state examination was done in an enclosed room and no other family members accompanied the
client during the assessment. The assessment was done based on single interactions. The paper
describes the results of the mental status assessment and the recovery focused care plan made for
the client based on assessment.
Mental status assessment:
Level of consciousness:
Clinical assessment: The level of consciousness was determined using the Glasgow coma scale. Verbal
response, eye opening and motor response of the client were assessed (Teasdale et al., 2014). Patient was
found in a confused fstate and he seemed lethargic too. The client also reported about not getting sound
sleep (Ma et al., 2015). Evidence suggests that sleep deprivation can have negative impact on behaviour
and it can reverse periods of consciousness (Cologan et al., 2010).
Assessment question:
1. Is the patient lethargic during the interaction?
2. Was the patient found to be in a confused state?
References:

2ASSESSMENT ANALYSIS IN MENTAL HEALTH NURSING
Cologan, V., Schabus, M., Ledoux, D., Moonen, G., Maquet, P., & Laureys, S. (2010). Sleep in disorders
of consciousness. Sleep Medicine Reviews, 14(2), 97–105.
http://doi.org/10.1016/j.smrv.2009.04.003
Ma, N., Dinges, D. F., Basner, M., & Rao, H. (2015). How acute total sleep loss affects the attending
brain: a meta-analysis of neuroimaging studies. Sleep, 38(2), 233-240.
Teasdale, G., Maas, A., Lecky, F., Manley, G., Stocchetti, N., & Murray, G. (2014). The Glasgow Coma
Scale at 40 years: standing the test of time. The Lancet Neurology, 13(8), 844-854.
General appearance:
Clinical assessment:
While going ahead with formal introduction process with the client, the gait, postures, clothing and
grooming status of client was observed (Finney, Minagar & Heilman, 2016). Although the client’s cloth
was appropriate for the occasion, however it was very dirty and not pressed. His gait was normal, but he
was not very well-groomed which became evident from his entangled hairs and sweaty shirt. Research
studies on psychiatric assessment states that looking at abnormalities of general appearance is important
to make sense of the mental state of client (Townsend & Morgan, 2017).
Assessment question:
1. Is the client’s clothing appropriate for the situation and weather?
2. Is the client well-groomed or his appearance reflects signs of mental disturbance?
References:
Finney, G. R., Minagar, A., & Heilman, K. M. (2016). Assessment of mental status. Neurologic
clinics, 34(1), 1-16.
Townsend, M. C., & Morgan, K. I. (2017). Psychiatric mental health nursing: Concepts of care in
evidence-based practice. FA Davis.
Cologan, V., Schabus, M., Ledoux, D., Moonen, G., Maquet, P., & Laureys, S. (2010). Sleep in disorders
of consciousness. Sleep Medicine Reviews, 14(2), 97–105.
http://doi.org/10.1016/j.smrv.2009.04.003
Ma, N., Dinges, D. F., Basner, M., & Rao, H. (2015). How acute total sleep loss affects the attending
brain: a meta-analysis of neuroimaging studies. Sleep, 38(2), 233-240.
Teasdale, G., Maas, A., Lecky, F., Manley, G., Stocchetti, N., & Murray, G. (2014). The Glasgow Coma
Scale at 40 years: standing the test of time. The Lancet Neurology, 13(8), 844-854.
General appearance:
Clinical assessment:
While going ahead with formal introduction process with the client, the gait, postures, clothing and
grooming status of client was observed (Finney, Minagar & Heilman, 2016). Although the client’s cloth
was appropriate for the occasion, however it was very dirty and not pressed. His gait was normal, but he
was not very well-groomed which became evident from his entangled hairs and sweaty shirt. Research
studies on psychiatric assessment states that looking at abnormalities of general appearance is important
to make sense of the mental state of client (Townsend & Morgan, 2017).
Assessment question:
1. Is the client’s clothing appropriate for the situation and weather?
2. Is the client well-groomed or his appearance reflects signs of mental disturbance?
References:
Finney, G. R., Minagar, A., & Heilman, K. M. (2016). Assessment of mental status. Neurologic
clinics, 34(1), 1-16.
Townsend, M. C., & Morgan, K. I. (2017). Psychiatric mental health nursing: Concepts of care in
evidence-based practice. FA Davis.

3ASSESSMENT ANALYSIS IN MENTAL HEALTH NURSING
Behaviour:
Clinical assessment:
Assessment of abnormal behaviour in client was done by observing client’s expression, mannerism,
gestures, eye contact and ability to follow commands during the interaction ( Pollard, 2018). Throughout
the interaction, his tone of voice and body language was observed. Although he was comfortable and
displayed good manners, however he was not making eye contact. He was not cooperative throughout the
interaction and he seemed to be in a lost state several times (Finney, Minagar & Heilman, 2016).
Assessment question:
1. Is the client cooperative or is he becoming irritated in between interactions?
2. Does the client display good manners and ability to follow commands during the
interaction?
References:
Finney, G. R., Minagar, A., & Heilman, K. M. (2016). Assessment of mental status. Neurologic
clinics, 34(1), 1-16.
Pollard, C. W. (2018). Fundamentals of the Psychiatric Mental Status Examination: A Workbook.
Canadian Scholars.
Mood and affect:
Clinical assessment:
Signs of irritation and tone of voice indicated mood and affect (Forbes & Watt, 2015). When asked about
his current mood, the client reported that he feels good currently however he remains in a poor mood
most of the time. He is not satisfied with what he does and he reports being in a low mood most of the
time. His unstable mental state was also understood from the fact that he went out of control in one social
Behaviour:
Clinical assessment:
Assessment of abnormal behaviour in client was done by observing client’s expression, mannerism,
gestures, eye contact and ability to follow commands during the interaction ( Pollard, 2018). Throughout
the interaction, his tone of voice and body language was observed. Although he was comfortable and
displayed good manners, however he was not making eye contact. He was not cooperative throughout the
interaction and he seemed to be in a lost state several times (Finney, Minagar & Heilman, 2016).
Assessment question:
1. Is the client cooperative or is he becoming irritated in between interactions?
2. Does the client display good manners and ability to follow commands during the
interaction?
References:
Finney, G. R., Minagar, A., & Heilman, K. M. (2016). Assessment of mental status. Neurologic
clinics, 34(1), 1-16.
Pollard, C. W. (2018). Fundamentals of the Psychiatric Mental Status Examination: A Workbook.
Canadian Scholars.
Mood and affect:
Clinical assessment:
Signs of irritation and tone of voice indicated mood and affect (Forbes & Watt, 2015). When asked about
his current mood, the client reported that he feels good currently however he remains in a poor mood
most of the time. He is not satisfied with what he does and he reports being in a low mood most of the
time. His unstable mental state was also understood from the fact that he went out of control in one social
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4ASSESSMENT ANALYSIS IN MENTAL HEALTH NURSING
gathering as he wanted to stay alone, however the social gathering wanted him to join in a game ( Pollard,
2018).
Assessment question:
1. How are you feeling currently?
2. Have you experienced situations when you were out of control? Do you feel guilty for it
now?
References:
Forbes, H., & Watt, E. (2015). Jarvis's Physical Examination and Health Assessment. Elsevier Health
Sciences.
Pollard, C. W. (2018). Fundamentals of the Psychiatric Mental Status Examination: A Workbook.
Canadian Scholars.
Speech:
Clinical assessment:
Clinical assessment of speech was done by assessment of quantity, rate, volume and fluency of speech.
The parameters used for quantity of speech included talkative, spontaneous, expansive or paucity of
speech (Finney, Minagar & Heilman, 2016). The rate of speech was determined by evaluating whether
the rate of speech was fast or slow. Tone of voice during speaking and fluency of rhythm was determined
too. He has a soft tone and the rate of speech was little slow. However, took time to open up and was
hesitant throughout the interaction. The pressured speech and elevated mood of the client gave an
indication of a mental state consistent with a diagnosis of depression (Fernando & Carter, 2016).
Assessment question:
1. Is the client’s tone of voice normal?
gathering as he wanted to stay alone, however the social gathering wanted him to join in a game ( Pollard,
2018).
Assessment question:
1. How are you feeling currently?
2. Have you experienced situations when you were out of control? Do you feel guilty for it
now?
References:
Forbes, H., & Watt, E. (2015). Jarvis's Physical Examination and Health Assessment. Elsevier Health
Sciences.
Pollard, C. W. (2018). Fundamentals of the Psychiatric Mental Status Examination: A Workbook.
Canadian Scholars.
Speech:
Clinical assessment:
Clinical assessment of speech was done by assessment of quantity, rate, volume and fluency of speech.
The parameters used for quantity of speech included talkative, spontaneous, expansive or paucity of
speech (Finney, Minagar & Heilman, 2016). The rate of speech was determined by evaluating whether
the rate of speech was fast or slow. Tone of voice during speaking and fluency of rhythm was determined
too. He has a soft tone and the rate of speech was little slow. However, took time to open up and was
hesitant throughout the interaction. The pressured speech and elevated mood of the client gave an
indication of a mental state consistent with a diagnosis of depression (Fernando & Carter, 2016).
Assessment question:
1. Is the client’s tone of voice normal?
5ASSESSMENT ANALYSIS IN MENTAL HEALTH NURSING
2. Was the rhythm of speech clear or slurred?
References:
Fernando, I., & Carter, G. (2016). A case report using the mental state examination scale (MSES): a tool
for measuring change in mental state. Australasian Psychiatry, 24(1), 76-80.
Finney, G. R., Minagar, A., & Heilman, K. M. (2016). Assessment of mental status. Neurologic
clinics, 34(1), 1-16.
Thought (content/stream:
Clinical assessment:
The clinical assessment for thought was done by questioning regarding his plans for life and analysing his
aspirations in life (Grover & Kate, 2017). He was also asked regarding the things he regret or the
strategies that he uses to deal with stressors in life. The client’s response revealed that he was dissatisfied
with almost everything he had done till now. He was not satisfied with his job and left many jobs on his
own. The client also reported about an occasion when he developed the urge of committing suicide.
However, he did not attempt it, suicidal ideation existed. This indicated that he was slowing moving
towards a disorders mental state where treatment became necessary for him. Self-injurious thoughts are
harmful as it is a risk factor for future suicide attempts and death (Ribeiro et al. 2016).
Assessment question:
1. Does the client experience any delusion?
2. Did the person attempted to do suicide or did he developed suicidal thoughts ever?
References:
Grover, S., & Kate, N. (2017). Unit-2 Steps In Mental Health (Status) Assessment. IGNOU.
Ribeiro, J. D., Franklin, J. C., Fox, K. R., Bentley, K. H., Kleiman, E. M., Chang, B. P., & Nock, M. K.
(2016). Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts,
and death: a meta-analysis of longitudinal studies. Psychological Medicine, 46(2), 225–236.
2. Was the rhythm of speech clear or slurred?
References:
Fernando, I., & Carter, G. (2016). A case report using the mental state examination scale (MSES): a tool
for measuring change in mental state. Australasian Psychiatry, 24(1), 76-80.
Finney, G. R., Minagar, A., & Heilman, K. M. (2016). Assessment of mental status. Neurologic
clinics, 34(1), 1-16.
Thought (content/stream:
Clinical assessment:
The clinical assessment for thought was done by questioning regarding his plans for life and analysing his
aspirations in life (Grover & Kate, 2017). He was also asked regarding the things he regret or the
strategies that he uses to deal with stressors in life. The client’s response revealed that he was dissatisfied
with almost everything he had done till now. He was not satisfied with his job and left many jobs on his
own. The client also reported about an occasion when he developed the urge of committing suicide.
However, he did not attempt it, suicidal ideation existed. This indicated that he was slowing moving
towards a disorders mental state where treatment became necessary for him. Self-injurious thoughts are
harmful as it is a risk factor for future suicide attempts and death (Ribeiro et al. 2016).
Assessment question:
1. Does the client experience any delusion?
2. Did the person attempted to do suicide or did he developed suicidal thoughts ever?
References:
Grover, S., & Kate, N. (2017). Unit-2 Steps In Mental Health (Status) Assessment. IGNOU.
Ribeiro, J. D., Franklin, J. C., Fox, K. R., Bentley, K. H., Kleiman, E. M., Chang, B. P., & Nock, M. K.
(2016). Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts,
and death: a meta-analysis of longitudinal studies. Psychological Medicine, 46(2), 225–236.
6ASSESSMENT ANALYSIS IN MENTAL HEALTH NURSING
http://doi.org/10.1017/S0033291715001804
Intellectual performance:
Clinical assessment:
Assessment of intellectual performance is done to evaluate whether client have good knowledge about
information or not (Parlar et al., 2016). It is also done to evaluate abstract thinking of client and their
interest or awareness about current events (Finney, Minagar & Heilman, 2016). Being aware about
current event can suggest that client is not isolated and he takes interest in other current events and social
affairs too. In the context of assessment for Mr. A, he was found to have good intellectual knowledge and
good awareness about recent events too.
Assessment question:
The client was asked questions like-
1. Name the current president of your country?
2. How are the items like apple and orange similar?
References:
Finney, G. R., Minagar, A., & Heilman, K. M. (2016). Assessment of mental status. Neurologic
clinics, 34(1), 1-16.
Parlar, M., Frewen, P. A., Oremus, C., Lanius, R. A., & McKinnon, M. C. (2016). Dissociative symptoms
are associated with reduced neuropsychological performance in patients with recurrent depression
and a history of trauma exposure. European journal of psychotraumatology, 7(1), 29061.
Perception:
Clinical assessment:
Assessment of perception is done to evaluate thinking patterns of client and see how much effort the
client has done to understand his problem and take control over his life ( Townsend & Morgan, 2017).
Based on client’s response to the below mentioned question, it was found that he took negative measures
http://doi.org/10.1017/S0033291715001804
Intellectual performance:
Clinical assessment:
Assessment of intellectual performance is done to evaluate whether client have good knowledge about
information or not (Parlar et al., 2016). It is also done to evaluate abstract thinking of client and their
interest or awareness about current events (Finney, Minagar & Heilman, 2016). Being aware about
current event can suggest that client is not isolated and he takes interest in other current events and social
affairs too. In the context of assessment for Mr. A, he was found to have good intellectual knowledge and
good awareness about recent events too.
Assessment question:
The client was asked questions like-
1. Name the current president of your country?
2. How are the items like apple and orange similar?
References:
Finney, G. R., Minagar, A., & Heilman, K. M. (2016). Assessment of mental status. Neurologic
clinics, 34(1), 1-16.
Parlar, M., Frewen, P. A., Oremus, C., Lanius, R. A., & McKinnon, M. C. (2016). Dissociative symptoms
are associated with reduced neuropsychological performance in patients with recurrent depression
and a history of trauma exposure. European journal of psychotraumatology, 7(1), 29061.
Perception:
Clinical assessment:
Assessment of perception is done to evaluate thinking patterns of client and see how much effort the
client has done to understand his problem and take control over his life ( Townsend & Morgan, 2017).
Based on client’s response to the below mentioned question, it was found that he took negative measures
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
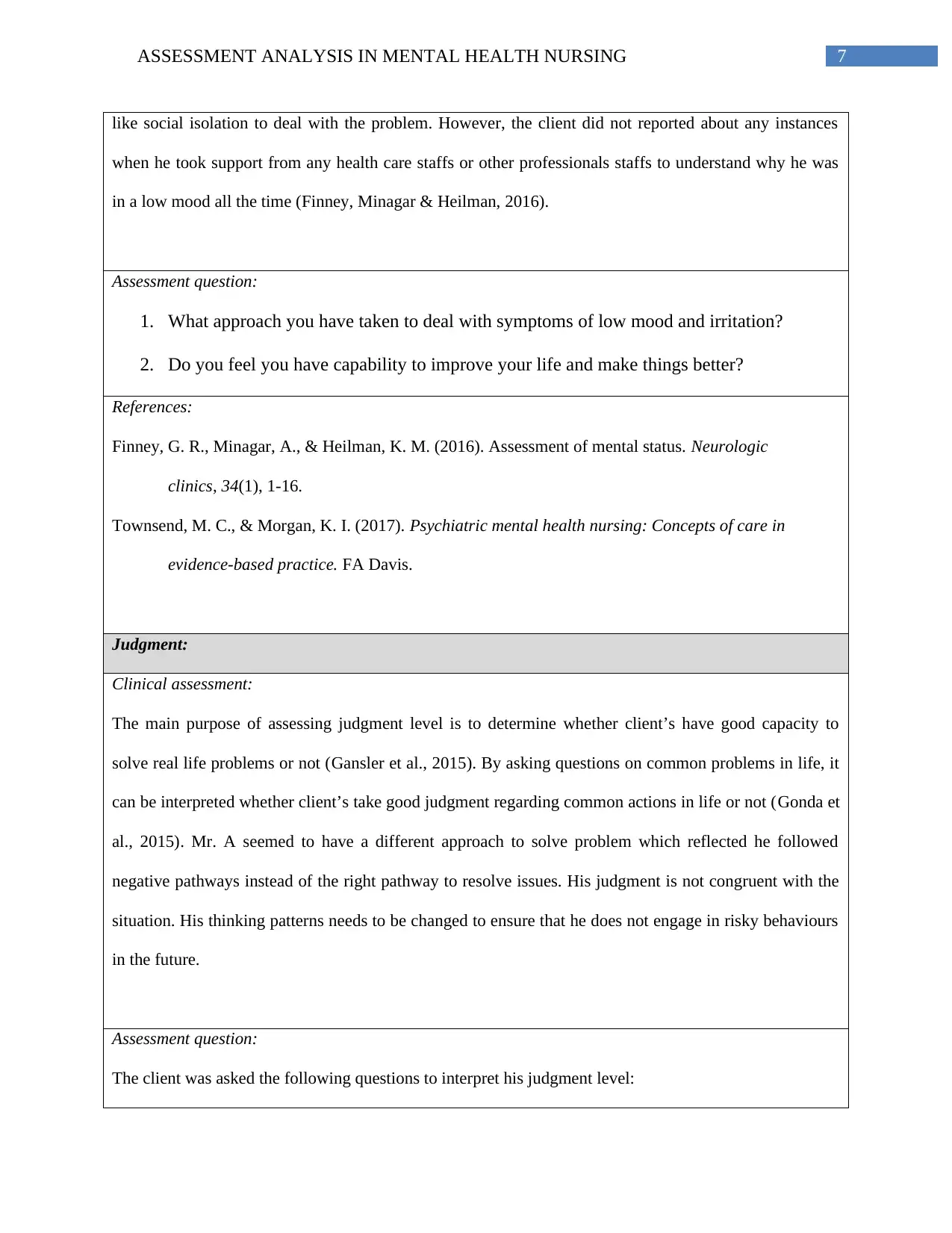
7ASSESSMENT ANALYSIS IN MENTAL HEALTH NURSING
like social isolation to deal with the problem. However, the client did not reported about any instances
when he took support from any health care staffs or other professionals staffs to understand why he was
in a low mood all the time (Finney, Minagar & Heilman, 2016).
Assessment question:
1. What approach you have taken to deal with symptoms of low mood and irritation?
2. Do you feel you have capability to improve your life and make things better?
References:
Finney, G. R., Minagar, A., & Heilman, K. M. (2016). Assessment of mental status. Neurologic
clinics, 34(1), 1-16.
Townsend, M. C., & Morgan, K. I. (2017). Psychiatric mental health nursing: Concepts of care in
evidence-based practice. FA Davis.
Judgment:
Clinical assessment:
The main purpose of assessing judgment level is to determine whether client’s have good capacity to
solve real life problems or not (Gansler et al., 2015). By asking questions on common problems in life, it
can be interpreted whether client’s take good judgment regarding common actions in life or not (Gonda et
al., 2015). Mr. A seemed to have a different approach to solve problem which reflected he followed
negative pathways instead of the right pathway to resolve issues. His judgment is not congruent with the
situation. His thinking patterns needs to be changed to ensure that he does not engage in risky behaviours
in the future.
Assessment question:
The client was asked the following questions to interpret his judgment level:
like social isolation to deal with the problem. However, the client did not reported about any instances
when he took support from any health care staffs or other professionals staffs to understand why he was
in a low mood all the time (Finney, Minagar & Heilman, 2016).
Assessment question:
1. What approach you have taken to deal with symptoms of low mood and irritation?
2. Do you feel you have capability to improve your life and make things better?
References:
Finney, G. R., Minagar, A., & Heilman, K. M. (2016). Assessment of mental status. Neurologic
clinics, 34(1), 1-16.
Townsend, M. C., & Morgan, K. I. (2017). Psychiatric mental health nursing: Concepts of care in
evidence-based practice. FA Davis.
Judgment:
Clinical assessment:
The main purpose of assessing judgment level is to determine whether client’s have good capacity to
solve real life problems or not (Gansler et al., 2015). By asking questions on common problems in life, it
can be interpreted whether client’s take good judgment regarding common actions in life or not (Gonda et
al., 2015). Mr. A seemed to have a different approach to solve problem which reflected he followed
negative pathways instead of the right pathway to resolve issues. His judgment is not congruent with the
situation. His thinking patterns needs to be changed to ensure that he does not engage in risky behaviours
in the future.
Assessment question:
The client was asked the following questions to interpret his judgment level:
8ASSESSMENT ANALYSIS IN MENTAL HEALTH NURSING
1. What will you do if you were in a movie theatre and you smelled smoke?
2. What will you do if you find an addressed envelope on the street?
References:
Gansler, D. A., Suvak, M., Arean, P., & Alexopoulos, G. S. (2015). Role of executive dysfunction and
dysexecutive behavior in late-life depression and disability. The American Journal of Geriatric
Psychiatry, 23(10), 1038-1045.
Gonda, X., Pompili, M., Serafini, G., Carvalho, A. F., Rihmer, Z., & Dome, P. (2015). The role of
cognitive dysfunction in the symptoms and remission from depression. Annals of general
psychiatry, 14(1), 27.
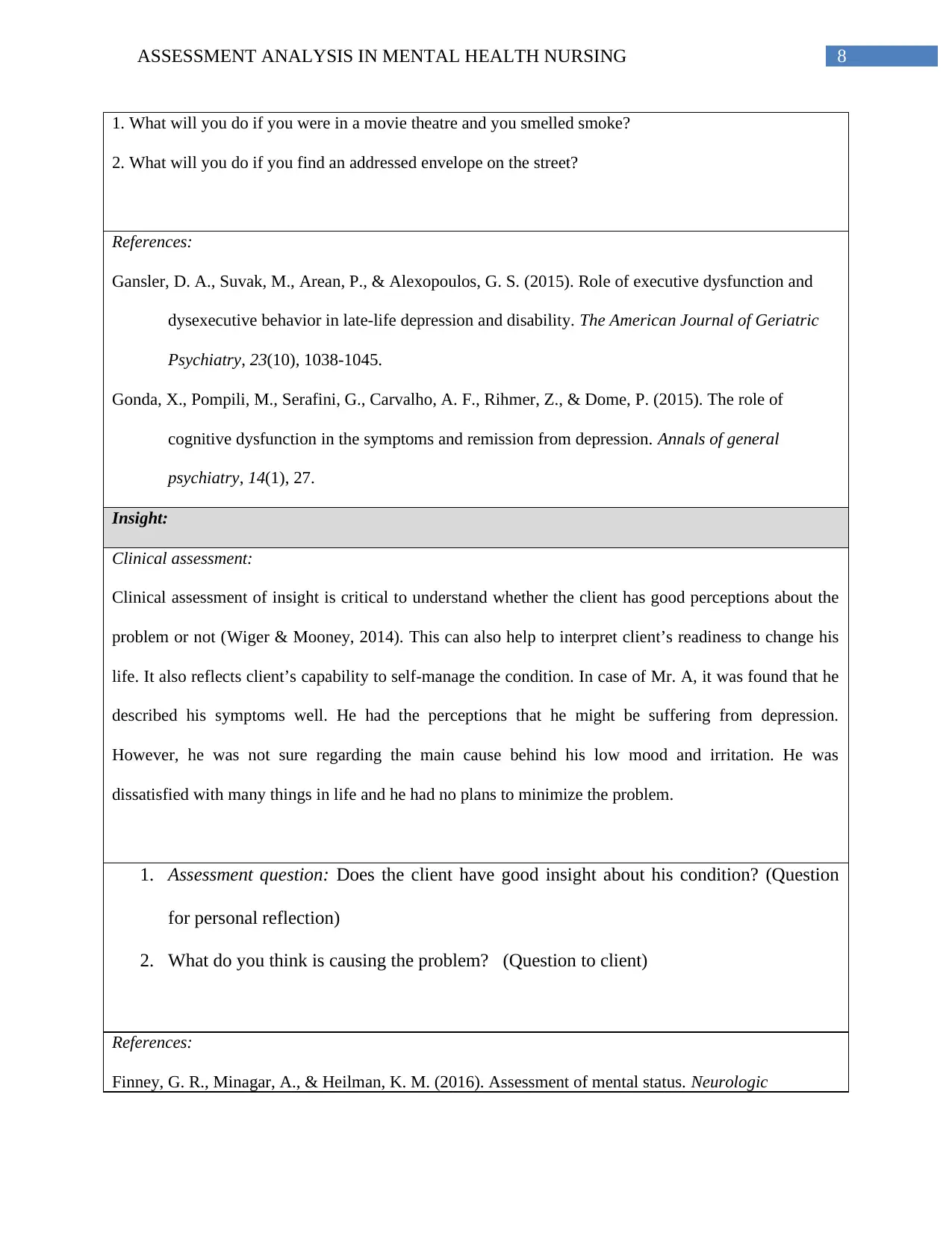
Insight:
Clinical assessment:
Clinical assessment of insight is critical to understand whether the client has good perceptions about the
problem or not (Wiger & Mooney, 2014). This can also help to interpret client’s readiness to change his
life. It also reflects client’s capability to self-manage the condition. In case of Mr. A, it was found that he
described his symptoms well. He had the perceptions that he might be suffering from depression.
However, he was not sure regarding the main cause behind his low mood and irritation. He was
dissatisfied with many things in life and he had no plans to minimize the problem.
1. Assessment question: Does the client have good insight about his condition? (Question
for personal reflection)
2. What do you think is causing the problem? (Question to client)
References:
Finney, G. R., Minagar, A., & Heilman, K. M. (2016). Assessment of mental status. Neurologic
1. What will you do if you were in a movie theatre and you smelled smoke?
2. What will you do if you find an addressed envelope on the street?
References:
Gansler, D. A., Suvak, M., Arean, P., & Alexopoulos, G. S. (2015). Role of executive dysfunction and
dysexecutive behavior in late-life depression and disability. The American Journal of Geriatric
Psychiatry, 23(10), 1038-1045.
Gonda, X., Pompili, M., Serafini, G., Carvalho, A. F., Rihmer, Z., & Dome, P. (2015). The role of
cognitive dysfunction in the symptoms and remission from depression. Annals of general
psychiatry, 14(1), 27.
Insight:
Clinical assessment:
Clinical assessment of insight is critical to understand whether the client has good perceptions about the
problem or not (Wiger & Mooney, 2014). This can also help to interpret client’s readiness to change his
life. It also reflects client’s capability to self-manage the condition. In case of Mr. A, it was found that he
described his symptoms well. He had the perceptions that he might be suffering from depression.
However, he was not sure regarding the main cause behind his low mood and irritation. He was
dissatisfied with many things in life and he had no plans to minimize the problem.
1. Assessment question: Does the client have good insight about his condition? (Question
for personal reflection)
2. What do you think is causing the problem? (Question to client)
References:
Finney, G. R., Minagar, A., & Heilman, K. M. (2016). Assessment of mental status. Neurologic
9ASSESSMENT ANALYSIS IN MENTAL HEALTH NURSING
clinics, 34(1), 1-16.
Wiger, D. E., & Mooney, N. B. (2014). Mental Status Exam. The Encyclopedia of Clinical Psychology, 1-
5.
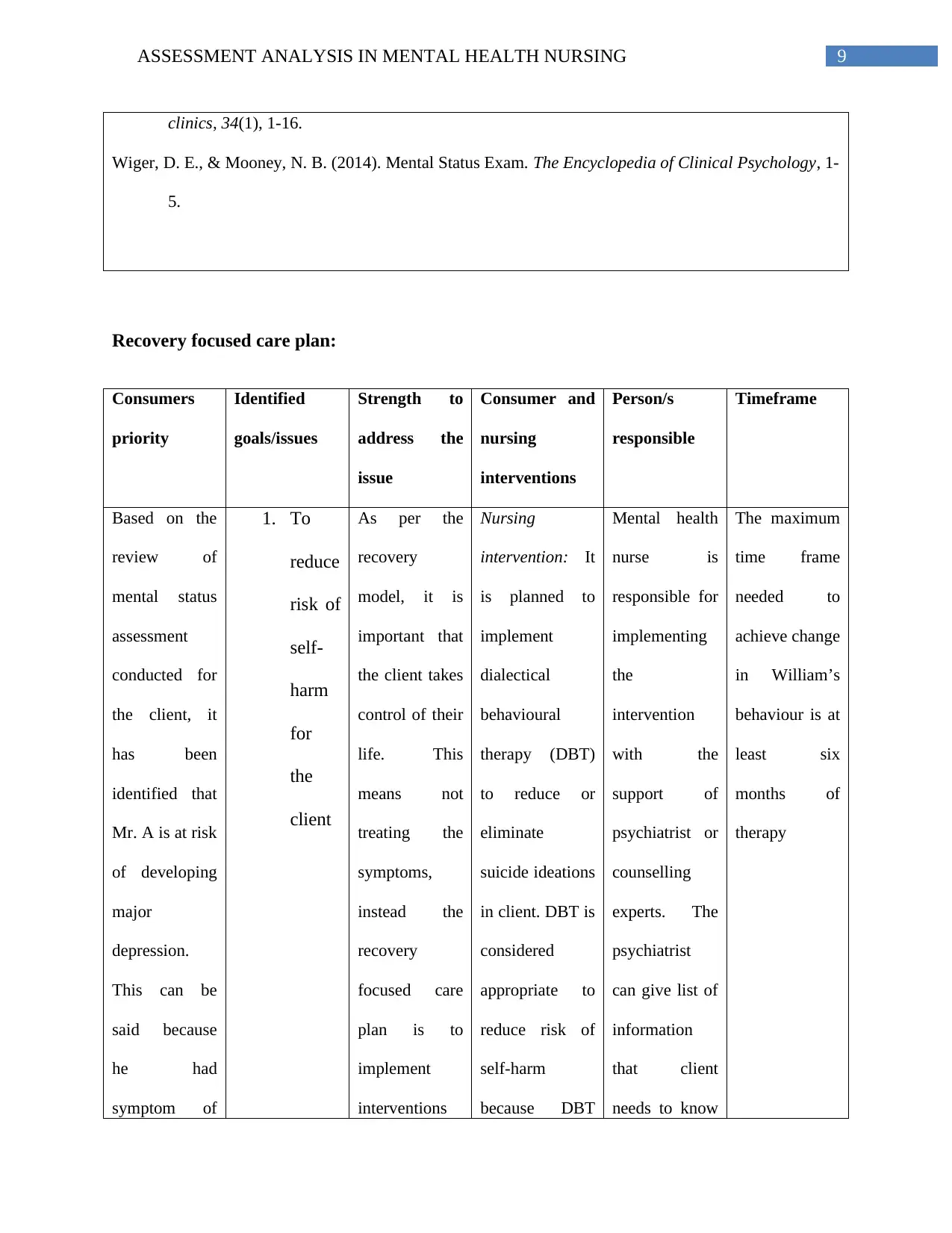
Recovery focused care plan:
Consumers
priority
Identified
goals/issues
Strength to
address the
issue
Consumer and
nursing
interventions
Person/s
responsible
Timeframe
Based on the
review of
mental status
assessment
conducted for
the client, it
has been
identified that
Mr. A is at risk
of developing
major
depression.
This can be
said because
he had
symptom of
1. To
reduce
risk of
self-
harm
for
the
client
As per the
recovery
model, it is
important that
the client takes
control of their
life. This
means not
treating the
symptoms,
instead the
recovery
focused care
plan is to
implement
interventions
Nursing
intervention: It
is planned to
implement
dialectical
behavioural
therapy (DBT)
to reduce or
eliminate
suicide ideations
in client. DBT is
considered
appropriate to
reduce risk of
self-harm
because DBT
Mental health
nurse is
responsible for
implementing
the
intervention
with the
support of
psychiatrist or
counselling
experts. The
psychiatrist
can give list of
information
that client
needs to know
The maximum
time frame
needed to
achieve change
in William’s
behaviour is at
least six
months of
therapy
clinics, 34(1), 1-16.
Wiger, D. E., & Mooney, N. B. (2014). Mental Status Exam. The Encyclopedia of Clinical Psychology, 1-
5.
Recovery focused care plan:
Consumers
priority
Identified
goals/issues
Strength to
address the
issue
Consumer and
nursing
interventions
Person/s
responsible
Timeframe
Based on the
review of
mental status
assessment
conducted for
the client, it
has been
identified that
Mr. A is at risk
of developing
major
depression.
This can be
said because
he had
symptom of
1. To
reduce
risk of
self-
harm
for
the
client
As per the
recovery
model, it is
important that
the client takes
control of their
life. This
means not
treating the
symptoms,
instead the
recovery
focused care
plan is to
implement
interventions
Nursing
intervention: It
is planned to
implement
dialectical
behavioural
therapy (DBT)
to reduce or
eliminate
suicide ideations
in client. DBT is
considered
appropriate to
reduce risk of
self-harm
because DBT
Mental health
nurse is
responsible for
implementing
the
intervention
with the
support of
psychiatrist or
counselling
experts. The
psychiatrist
can give list of
information
that client
needs to know
The maximum
time frame
needed to
achieve change
in William’s
behaviour is at
least six
months of
therapy
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10ASSESSMENT ANALYSIS IN MENTAL HEALTH NURSING
depressed
mood, little
interest in
daily life
activities,
insomnia,
fatigue, suicide
ideation and
feelings of
guilt for more
than 2 weeks.
This
conclusion has
been made
because his
conditions
matches with
the symptoms
provided as
per the DSM-
V criteria for
diagnostic
disorder
(Koukopoulos
& Sani, 2014).
that can build
resilience of
people with
mental
problems. Self-
management
skills have
been
prioritized to
promote
control, hope
and optimism
as part of the
recovery
focussed care
plan (Jacob,
2015).
was developed
to treat para-
suicidal
behaviour and
difficulty in
tolerating
emotional
distress
(Mehlum et al.,
2016). These
conditions were
found in Mr. A
too.
Consumer
intervention:
Consumer can
search for
information in
the internet to
understand ways
to engage in
activities that
relaxes mind
(Chen et al.,
2015)
to avoid
suicidal
behaviour and
lead a life that
is worth living.
depressed
mood, little
interest in
daily life
activities,
insomnia,
fatigue, suicide
ideation and
feelings of
guilt for more
than 2 weeks.
This
conclusion has
been made
because his
conditions
matches with
the symptoms
provided as
per the DSM-
V criteria for
diagnostic
disorder
(Koukopoulos
& Sani, 2014).
that can build
resilience of
people with
mental
problems. Self-
management
skills have
been
prioritized to
promote
control, hope
and optimism
as part of the
recovery
focussed care
plan (Jacob,
2015).
was developed
to treat para-
suicidal
behaviour and
difficulty in
tolerating
emotional
distress
(Mehlum et al.,
2016). These
conditions were
found in Mr. A
too.
Consumer
intervention:
Consumer can
search for
information in
the internet to
understand ways
to engage in
activities that
relaxes mind
(Chen et al.,
2015)
to avoid
suicidal
behaviour and
lead a life that
is worth living.
11ASSESSMENT ANALYSIS IN MENTAL HEALTH NURSING
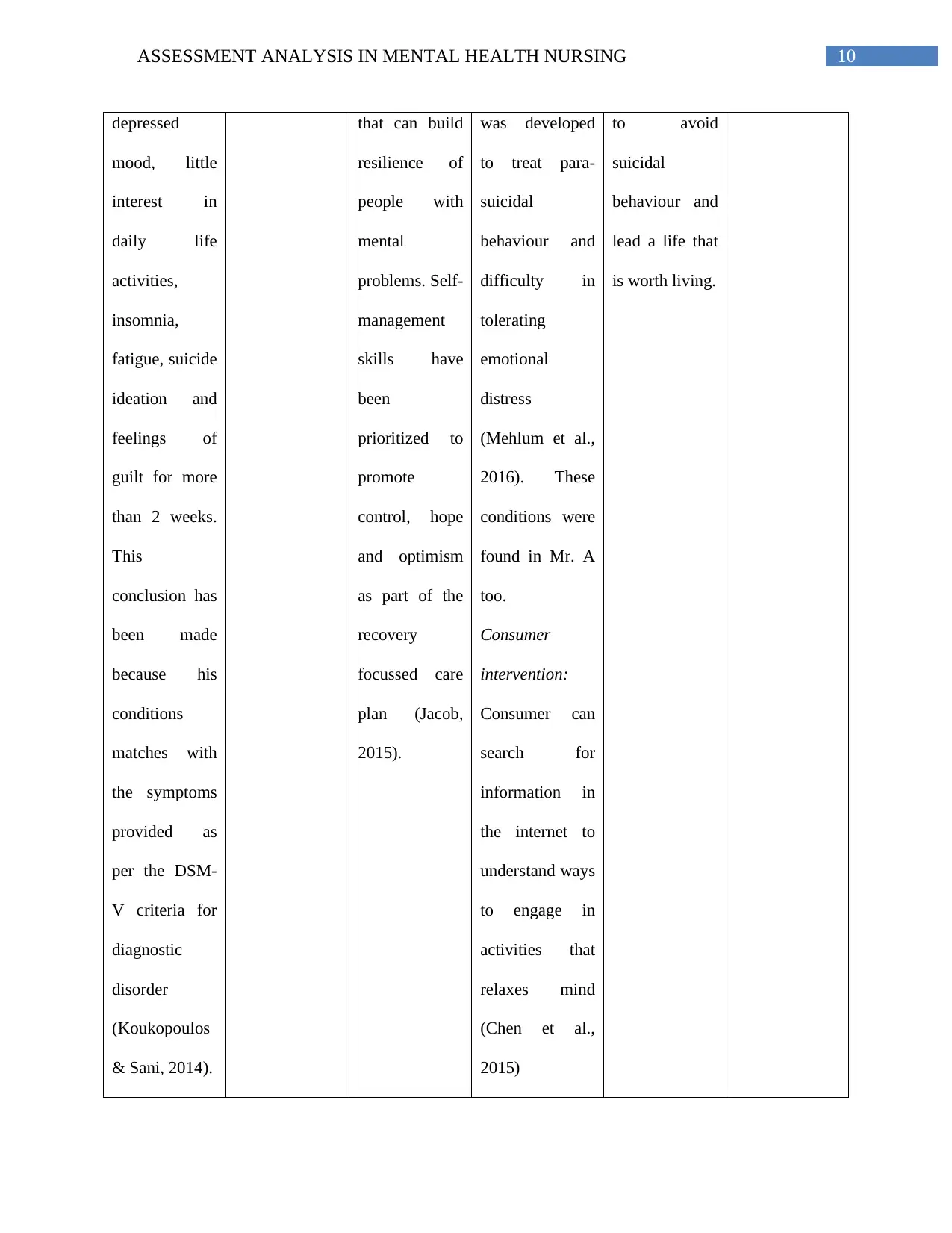
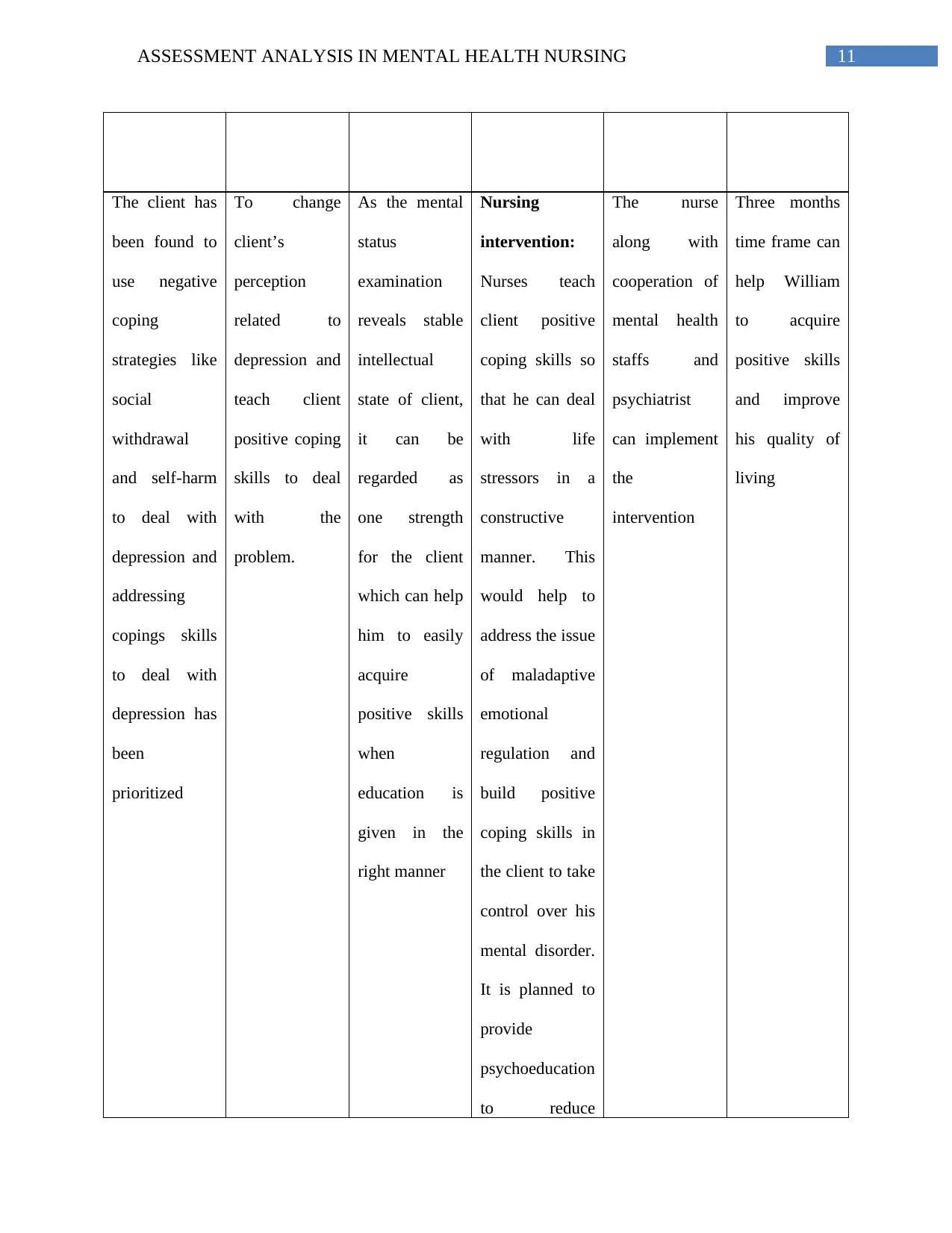
The client has
been found to
use negative
coping
strategies like
social
withdrawal
and self-harm
to deal with
depression and
addressing
copings skills
to deal with
depression has
been
prioritized
To change
client’s
perception
related to
depression and
teach client
positive coping
skills to deal
with the
problem.
As the mental
status
examination
reveals stable
intellectual
state of client,
it can be
regarded as
one strength
for the client
which can help
him to easily
acquire
positive skills
when
education is
given in the
right manner
Nursing
intervention:
Nurses teach
client positive
coping skills so
that he can deal
with life
stressors in a
constructive
manner. This
would help to
address the issue
of maladaptive
emotional
regulation and
build positive
coping skills in
the client to take
control over his
mental disorder.
It is planned to
provide
psychoeducation
to reduce
The nurse
along with
cooperation of
mental health
staffs and
psychiatrist
can implement
the
intervention
Three months
time frame can
help William
to acquire
positive skills
and improve
his quality of
living
The client has
been found to
use negative
coping
strategies like
social
withdrawal
and self-harm
to deal with
depression and
addressing
copings skills
to deal with
depression has
been
prioritized
To change
client’s
perception
related to
depression and
teach client
positive coping
skills to deal
with the
problem.
As the mental
status
examination
reveals stable
intellectual
state of client,
it can be
regarded as
one strength
for the client
which can help
him to easily
acquire
positive skills
when
education is
given in the
right manner
Nursing
intervention:
Nurses teach
client positive
coping skills so
that he can deal
with life
stressors in a
constructive
manner. This
would help to
address the issue
of maladaptive
emotional
regulation and
build positive
coping skills in
the client to take
control over his
mental disorder.
It is planned to
provide
psychoeducation
to reduce
The nurse
along with
cooperation of
mental health
staffs and
psychiatrist
can implement
the
intervention
Three months
time frame can
help William
to acquire
positive skills
and improve
his quality of
living
12ASSESSMENT ANALYSIS IN MENTAL HEALTH NURSING
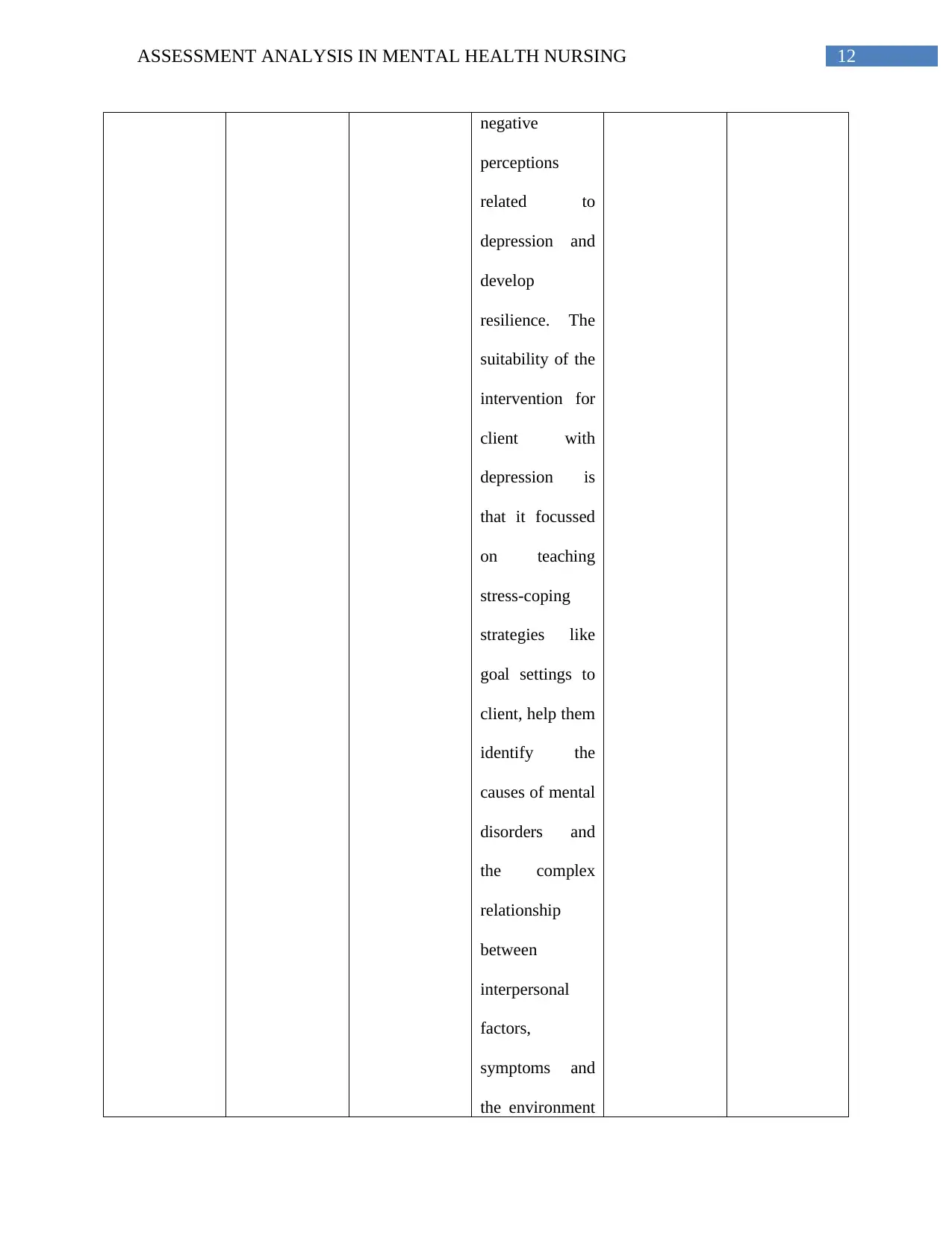
negative
perceptions
related to
depression and
develop
resilience. The
suitability of the
intervention for
client with
depression is
that it focussed
on teaching
stress-coping
strategies like
goal settings to
client, help them
identify the
causes of mental
disorders and
the complex
relationship
between
interpersonal
factors,
symptoms and
the environment
negative
perceptions
related to
depression and
develop
resilience. The
suitability of the
intervention for
client with
depression is
that it focussed
on teaching
stress-coping
strategies like
goal settings to
client, help them
identify the
causes of mental
disorders and
the complex
relationship
between
interpersonal
factors,
symptoms and
the environment
1 out of 13
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.
