Aging and Mental Health
VerifiedAdded on 2020/06/06
|60
|18572
|66
AI Summary
This assignment delves into the complex relationship between aging and mental well-being. It examines prevalent mental health issues among older adults, including anxiety and depression, alongside age-related cognitive changes such as memory impairment and executive dysfunction. The assignment further analyzes risk factors contributing to these conditions in later life, drawing upon research findings and epidemiological data. Understanding this interplay is crucial for promoting healthy aging and supporting the mental health of the growing elderly population.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Anxiety In Ageing, Subjective And
Objective Cognitive Impairment
(Literature Review)
Objective Cognitive Impairment
(Literature Review)
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
TABLE OF CONTENTS
INTRODUCTION...........................................................................................................................1
1.1 ANXIETY..................................................................................................................................2
1.1.1 Definition and Types.....................................................................................................2
1.1.2 Anxiety Disorders..........................................................................................................4
1.1.3 Risk Factors/Assessment for Anxiety in Old Age.........................................................7
1.1.4 Co-Morbidities..............................................................................................................8
1.2 AGEING AND LATE LIFE....................................................................................................16
1.2.1 Cognitive Changes in Normal ageing..........................................................................20
1.2.2 Structural/Functional Brain Changes in Normal Ageing............................................28
1.2.3 Subjective and Objective cognitive impairment and Dementia .................................34
1.3 NEUROLOGY OF ANXIETY ...............................................................................................36
1.4 FUNCTIONAL ANATOMIC AND NEUROCHEMICAL CORRELATES IN ANXIETY
DISORDERS.................................................................................................................................40
1.5 NEUROPSYCHOLOGICAL RELATIONSHIP BETWEEN ANXIETY AND COGNITIVE
DECLINE......................................................................................................................................42
CONCLUSION..............................................................................................................................45
REFERENCES..............................................................................................................................47
INTRODUCTION...........................................................................................................................1
1.1 ANXIETY..................................................................................................................................2
1.1.1 Definition and Types.....................................................................................................2
1.1.2 Anxiety Disorders..........................................................................................................4
1.1.3 Risk Factors/Assessment for Anxiety in Old Age.........................................................7
1.1.4 Co-Morbidities..............................................................................................................8
1.2 AGEING AND LATE LIFE....................................................................................................16
1.2.1 Cognitive Changes in Normal ageing..........................................................................20
1.2.2 Structural/Functional Brain Changes in Normal Ageing............................................28
1.2.3 Subjective and Objective cognitive impairment and Dementia .................................34
1.3 NEUROLOGY OF ANXIETY ...............................................................................................36
1.4 FUNCTIONAL ANATOMIC AND NEUROCHEMICAL CORRELATES IN ANXIETY
DISORDERS.................................................................................................................................40
1.5 NEUROPSYCHOLOGICAL RELATIONSHIP BETWEEN ANXIETY AND COGNITIVE
DECLINE......................................................................................................................................42
CONCLUSION..............................................................................................................................45
REFERENCES..............................................................................................................................47
INTRODUCTION
In older people and the ones having objective and subjective cognitive impairment and
AD, there is a high probability of having various anxiety symptoms. According to empirical
literature, it has been observed that anxiety is considered as a very common issue in moreover of
the population which creates issues in the later life. It has been analysed from taking samples
from community and it was on an estimation of 1.2% to 15% and from 1 to 28% in case of older
adults. This can be related to the various reasons such as ageing, other medical conditions or
because of the comorbid mental disorders (Bryant and et al., 2009; Therrien and Hunsley, 2011).
It has been observed that the patients that have been geriatric from the hospital has a prevalence
of about 43% in case of the anxiety issues. After taking samples from older people in the
community samples, it ranged about 15 to 25% and checking for the anxiety symptoms, it was
observed as 15 to 56%. These factors have helped in investigating the factors of anxiety in both
the cases of anxiety and in inhibitory cognitive control (Castriotta and et al., 2010; Therrien &
Hunsley, 2011). There has been observed a change in the estimation of cognitive control and
anxiety by different age groups, for people more than the age group of 85 and above. Dementia
is classified as a class of serious mental illness under the National institutes of health (NIH). The
data and information on the prevalence of Alzheimer represents the increasing rate of prevalence
(Kvaal et al., 2001). From the age of 65, the rate of dementia starts increasing from every five
years.
The chapter determines the need of examining the potential relationship between anxiety
and inhibitory cognitive control with relation to the functioning of brain which includes various
factors such attention, information processing speed, reaction time, reaction time variability,
1
In older people and the ones having objective and subjective cognitive impairment and
AD, there is a high probability of having various anxiety symptoms. According to empirical
literature, it has been observed that anxiety is considered as a very common issue in moreover of
the population which creates issues in the later life. It has been analysed from taking samples
from community and it was on an estimation of 1.2% to 15% and from 1 to 28% in case of older
adults. This can be related to the various reasons such as ageing, other medical conditions or
because of the comorbid mental disorders (Bryant and et al., 2009; Therrien and Hunsley, 2011).
It has been observed that the patients that have been geriatric from the hospital has a prevalence
of about 43% in case of the anxiety issues. After taking samples from older people in the
community samples, it ranged about 15 to 25% and checking for the anxiety symptoms, it was
observed as 15 to 56%. These factors have helped in investigating the factors of anxiety in both
the cases of anxiety and in inhibitory cognitive control (Castriotta and et al., 2010; Therrien &
Hunsley, 2011). There has been observed a change in the estimation of cognitive control and
anxiety by different age groups, for people more than the age group of 85 and above. Dementia
is classified as a class of serious mental illness under the National institutes of health (NIH). The
data and information on the prevalence of Alzheimer represents the increasing rate of prevalence
(Kvaal et al., 2001). From the age of 65, the rate of dementia starts increasing from every five
years.
The chapter determines the need of examining the potential relationship between anxiety
and inhibitory cognitive control with relation to the functioning of brain which includes various
factors such attention, information processing speed, reaction time, reaction time variability,
1
quality of sleep and memory etc. As the person starts ageing, it starts affecting the individual as
well, both physically and mentally as well. The whole process of ageing may also result in
various disorders such as anxiety as well as cognitive control. So, it can affect the older ones and
the people with subjective or objective cognitive impairment and AD. For the people suffering
from dementia or Alzheimer, anxiety is considered as a sort of inability to remember even the
basic facts. The symptoms of anxiety throw an impact on the personal well being of an
individual as it includes sleeping issues, short term memory. Along with this, it also has an
impact on the visual attention as the person may face issues with the eyesight as well. For
conducting this study, anxiety levels of various people including the younger ones and the elders
will be considered. All these factors that have been used for the whole investigation and will be
helpful enough in analyzing the potential relationship between anxiety and inhibitory cognitive
control and also how it affects the various factors of an individual cognition.
1.1 ANXIETY
1.1.1 Definition and Types
Anxiety is considered as an abnormal sense of feeling which disturbs the whole way of
doing activities. It is an intense feeling or emotion of uneasiness and worry which causes some
sort of interruption in doing activities of daily life (Cassidy & Rector, 2008; Lindesay, Stewart,
and Bisla, 2012). It is a very common issue that is being faced almost half of the population. It
can be because of various factors such as excess load in the work place, any stress factors or in
case if the person is going through a tough time. It is because stress itself makes the person tired
enough. When some tough times come and the person has to make some important decisions, in
that case when the person seems unable to think and understand what should be done, in that
case as well, the person feels high anxiety levels.
2
well, both physically and mentally as well. The whole process of ageing may also result in
various disorders such as anxiety as well as cognitive control. So, it can affect the older ones and
the people with subjective or objective cognitive impairment and AD. For the people suffering
from dementia or Alzheimer, anxiety is considered as a sort of inability to remember even the
basic facts. The symptoms of anxiety throw an impact on the personal well being of an
individual as it includes sleeping issues, short term memory. Along with this, it also has an
impact on the visual attention as the person may face issues with the eyesight as well. For
conducting this study, anxiety levels of various people including the younger ones and the elders
will be considered. All these factors that have been used for the whole investigation and will be
helpful enough in analyzing the potential relationship between anxiety and inhibitory cognitive
control and also how it affects the various factors of an individual cognition.
1.1 ANXIETY
1.1.1 Definition and Types
Anxiety is considered as an abnormal sense of feeling which disturbs the whole way of
doing activities. It is an intense feeling or emotion of uneasiness and worry which causes some
sort of interruption in doing activities of daily life (Cassidy & Rector, 2008; Lindesay, Stewart,
and Bisla, 2012). It is a very common issue that is being faced almost half of the population. It
can be because of various factors such as excess load in the work place, any stress factors or in
case if the person is going through a tough time. It is because stress itself makes the person tired
enough. When some tough times come and the person has to make some important decisions, in
that case when the person seems unable to think and understand what should be done, in that
case as well, the person feels high anxiety levels.
2
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
It is not necessary that it would remain permanent only, it can be temporary as well.
Pathological anxiety is frequent and chronic and interferes with daily activities (Lindesay and et
al., 2012; Mah and et al., 2016). It has been observed that Sub-syndromal anxiety symptoms or
sub-clinical anxiety occurs more widely than pathological anxiety or anxiety disorders, with a
prevalence that ranges between 15 and 52% (Bryant and et al., 2008; Sherbourne, Sullivan and
et.al., 2010; Yochim and et.al, 2012). State anxiety describes temporarily experienced anxiety
which is considered as a very unpleasant emotion for facing any situation that seems threatening
and complicated. This type of anxiety is not related to the health or social status of the
individual, and passes as soon as the disturbing stimulus passes (Bryant et al., 2008; Eysenck &
Derakshan, 2011; Paulus & Stein, 2006). Trait anxiety is considered as a tendency which has
disturbing emotional arousal rather than a short-term event. This type of anxiety also lasts longer
than state anxiety. Trait anxiety is higher on the average among all the lower class individuals
but is termed lower among the middle and upper class (Bryant and et.al, 2008; Eysenck and
Derakshan, 2011; Paulus and Stein, 2006). State anxiety depends on the interaction between
situational stress and trait anxiety (Derakshan & Eysenck, 2009).
In general, anxiety is associated with a range of cognitive, physical, and effective
responses including muscle tension, apprehension, palpitations, sleep problems, restlessness,
poor concentration, and reassurance seeking behavior (Mah et al., 2016; Lindesay et al., 2012;
Goldin et al., 2009). Anxiety often coexists or is associated with various health issues such as
stroke, obesity, cancer, cardiovascular disease, diabetes, chronic physical illness, medical illness,
Alzheimer’s disease, pain, sleep issues, depression, and increasing frailty (Cassidy & Rector,
2008; Hek, Tiemeier, Newson, et al. 2011; Lindesay et al. 2012), and cognitive impairment and
decline (Derakshan & Eysenck, 2009).
3
Pathological anxiety is frequent and chronic and interferes with daily activities (Lindesay and et
al., 2012; Mah and et al., 2016). It has been observed that Sub-syndromal anxiety symptoms or
sub-clinical anxiety occurs more widely than pathological anxiety or anxiety disorders, with a
prevalence that ranges between 15 and 52% (Bryant and et al., 2008; Sherbourne, Sullivan and
et.al., 2010; Yochim and et.al, 2012). State anxiety describes temporarily experienced anxiety
which is considered as a very unpleasant emotion for facing any situation that seems threatening
and complicated. This type of anxiety is not related to the health or social status of the
individual, and passes as soon as the disturbing stimulus passes (Bryant et al., 2008; Eysenck &
Derakshan, 2011; Paulus & Stein, 2006). Trait anxiety is considered as a tendency which has
disturbing emotional arousal rather than a short-term event. This type of anxiety also lasts longer
than state anxiety. Trait anxiety is higher on the average among all the lower class individuals
but is termed lower among the middle and upper class (Bryant and et.al, 2008; Eysenck and
Derakshan, 2011; Paulus and Stein, 2006). State anxiety depends on the interaction between
situational stress and trait anxiety (Derakshan & Eysenck, 2009).
In general, anxiety is associated with a range of cognitive, physical, and effective
responses including muscle tension, apprehension, palpitations, sleep problems, restlessness,
poor concentration, and reassurance seeking behavior (Mah et al., 2016; Lindesay et al., 2012;
Goldin et al., 2009). Anxiety often coexists or is associated with various health issues such as
stroke, obesity, cancer, cardiovascular disease, diabetes, chronic physical illness, medical illness,
Alzheimer’s disease, pain, sleep issues, depression, and increasing frailty (Cassidy & Rector,
2008; Hek, Tiemeier, Newson, et al. 2011; Lindesay et al. 2012), and cognitive impairment and
decline (Derakshan & Eysenck, 2009).
3
1.1.2 Anxiety Disorders
Anxiety disorders are based on physical symptoms related to anxiety; most of such
disorders constitute psychiatric disorders (Yates, 2015). Anxiety disorders make people to avoid
and neglect situations that can turn complex or complicated further. Anxiety disorders can be
observed by a huge number of factors and these can be environmental, genetic, substance abuse
etc. The environmental factors can be considered as when the person plays outside or spends
some time outside like for various different purposes such as while shopping, playing etc.
Genetic factors may include the fact that anxiety can be observed because of genes as well. Like
in case if one of the parent or both has the issue of anxiety, then in that case, there are high
chances of the fact that the children may also suffer from the same issue (Copeland et al., 2014;
Yates, 2015). Doing substance abuse has also been considered as a factor because smoking and
drinking can be even tolerated to a level but doing substance abuse cannot. It is because these
drugs affect the brain in a way that the person loses its ability to think what is right and what is
not. So, it takes the person in a zone where the person does not feel any external behavior and
even if the person is observing it, it does not have any impact on the person (Katerndahl &
Talamantes, 2000; Yates, 2015). It is because these substances makes the person in such a way
that the person is not being affected by any other external factor, whether it is noise or anything.
Anxiety disorders are caused by an interaction between biopsychosocial and environmental
factors to produce clinical syndromes. An example of a biopsychosocial factor is classified as the
genetic vulnerability; stress and trauma constitute examples of environmental factors. An
individual may be resilient to stress while another is vulnerable, leading to a disorder.
4
Anxiety disorders are based on physical symptoms related to anxiety; most of such
disorders constitute psychiatric disorders (Yates, 2015). Anxiety disorders make people to avoid
and neglect situations that can turn complex or complicated further. Anxiety disorders can be
observed by a huge number of factors and these can be environmental, genetic, substance abuse
etc. The environmental factors can be considered as when the person plays outside or spends
some time outside like for various different purposes such as while shopping, playing etc.
Genetic factors may include the fact that anxiety can be observed because of genes as well. Like
in case if one of the parent or both has the issue of anxiety, then in that case, there are high
chances of the fact that the children may also suffer from the same issue (Copeland et al., 2014;
Yates, 2015). Doing substance abuse has also been considered as a factor because smoking and
drinking can be even tolerated to a level but doing substance abuse cannot. It is because these
drugs affect the brain in a way that the person loses its ability to think what is right and what is
not. So, it takes the person in a zone where the person does not feel any external behavior and
even if the person is observing it, it does not have any impact on the person (Katerndahl &
Talamantes, 2000; Yates, 2015). It is because these substances makes the person in such a way
that the person is not being affected by any other external factor, whether it is noise or anything.
Anxiety disorders are caused by an interaction between biopsychosocial and environmental
factors to produce clinical syndromes. An example of a biopsychosocial factor is classified as the
genetic vulnerability; stress and trauma constitute examples of environmental factors. An
individual may be resilient to stress while another is vulnerable, leading to a disorder.
4
Unrecognized medical conditions or use of substances such as herbal preparations and over-the-
counter medications may also lead to a disorder.
There are several types of anxiety disorders such as general anxiety disorder, panic disorder,
social anxiety disorder, late-life anxiety, as well as specific phobias (Cassidy & Rector, 2008).
General anxiety disorder (GAD) is described as a condition marked by feelings of fear, dread,
excessive worry and uneasiness lasting six months or longer (National Institutes for Health
[NIH], 2017). The persistent and exaggerated fears in GAD not a response to any threats or
related to concrete situations, rather the feeling of anxiety may be associated with anything. The
temporary physical state of alertness in which the body release's
Adrenaline in response to some stress, lasts much longer in people with GAD, causing
nervousness, muscle tension, lightheaded ness, increasing rate of the heartbeat or stomach
problems. This in turn can lead to exhaustion, poor concentration, and potentially other sleeps
problems (NIH, 2017). There are various risk factors as well as all the causes of the anxiety
disorders are not observed completely till now. In case of the anxiety disorders because of
various environmental, genetic factors, the person can take help of a medical practitioner.
Usually, the people who suffer from these disabilities and anxiety, does not seek for any help
because in that situation, they are themselves unaware of their own situation. They do not realize
that they are doing something wrong and are unable to take any specific measures against it as
well.
There is a quite difference between the GAD and various other panic disorders. Panic
disorder is triggered only by specific conditions and is a genetically inherited condition. Panic
can be triggered by injury, use of drugs such as cannabis, use of stimulants like decongestants,
interpersonal conflict, loss, illness, caffeine and other addictive substances, hyperventilation,
5
counter medications may also lead to a disorder.
There are several types of anxiety disorders such as general anxiety disorder, panic disorder,
social anxiety disorder, late-life anxiety, as well as specific phobias (Cassidy & Rector, 2008).
General anxiety disorder (GAD) is described as a condition marked by feelings of fear, dread,
excessive worry and uneasiness lasting six months or longer (National Institutes for Health
[NIH], 2017). The persistent and exaggerated fears in GAD not a response to any threats or
related to concrete situations, rather the feeling of anxiety may be associated with anything. The
temporary physical state of alertness in which the body release's
Adrenaline in response to some stress, lasts much longer in people with GAD, causing
nervousness, muscle tension, lightheaded ness, increasing rate of the heartbeat or stomach
problems. This in turn can lead to exhaustion, poor concentration, and potentially other sleeps
problems (NIH, 2017). There are various risk factors as well as all the causes of the anxiety
disorders are not observed completely till now. In case of the anxiety disorders because of
various environmental, genetic factors, the person can take help of a medical practitioner.
Usually, the people who suffer from these disabilities and anxiety, does not seek for any help
because in that situation, they are themselves unaware of their own situation. They do not realize
that they are doing something wrong and are unable to take any specific measures against it as
well.
There is a quite difference between the GAD and various other panic disorders. Panic
disorder is triggered only by specific conditions and is a genetically inherited condition. Panic
can be triggered by injury, use of drugs such as cannabis, use of stimulants like decongestants,
interpersonal conflict, loss, illness, caffeine and other addictive substances, hyperventilation,
5
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
public settings (in cases of agoraphobia), and inhalation of carbon dioxide (Dowden and Allen,
1997; Johnson and et.al., 1995; Yates, 2015). Social anxiety disorder or social phobia, is a type
of phobia with risks that are moderately heritable (Yates, 2015). Social phobia is based on the
interaction between genetic make-up and environmental events (Katerndahl & Talamantes,
2000). This phobia is triggered by events such as recurring negative experiences based on a
deficit of social skills or else traumatic social experiences such as embarrassment (Liebman &
Allen, 1995). This phobia is conceptualized in the psychoanalytic model as a symptom of a
deeper conflict such as low self-esteem. Social phobia is construed as a conditioned response due
to past associations in which negative emotional valence had occurred (Katerndahl &
Talamantes, 2000, Yates. 2015). Treatment is based on attempting to weaken and separate such
responses from the causative stimulus (Yates, 2015). Specific phobia such as blood-injury
phobia may also be acquired through modeling, conditioning, or trauma (Copeland et al., 2014).
Late-life anxiety also occurs in older adults. This type of anxiety may be difficult to diagnose as
older adults may have multiple medical and psychiatric issues. They may also be on medication
that affects the physiological pathways in anxiety such as the medication used for treating
Asthma, Depression, and High Blood Pressure (Cassidy & Rector, 2008; Liebman & Allen,
1995). Late-life anxiety will be discussed in detail in the subsequent chapter of this study.
The disorder of anxiety and cognitive decline are defined in both research and clinical settings.
With respect to ageing, it also affects the facial expressions of an individual because when a
person starts to age, the flexibility of the muscles starts decreasing as well (Lindesay, Stewart, &
Bisla, 2012; Lezak, Howieson, Bigler, et al., 2012). It is because the muscles of the skin and its
cells are very delicate and after a few times, it starts losing its capability to hold all the cells
together. So, when these cells moves apart, wrinkles start to appear on the face. So, it also
6
1997; Johnson and et.al., 1995; Yates, 2015). Social anxiety disorder or social phobia, is a type
of phobia with risks that are moderately heritable (Yates, 2015). Social phobia is based on the
interaction between genetic make-up and environmental events (Katerndahl & Talamantes,
2000). This phobia is triggered by events such as recurring negative experiences based on a
deficit of social skills or else traumatic social experiences such as embarrassment (Liebman &
Allen, 1995). This phobia is conceptualized in the psychoanalytic model as a symptom of a
deeper conflict such as low self-esteem. Social phobia is construed as a conditioned response due
to past associations in which negative emotional valence had occurred (Katerndahl &
Talamantes, 2000, Yates. 2015). Treatment is based on attempting to weaken and separate such
responses from the causative stimulus (Yates, 2015). Specific phobia such as blood-injury
phobia may also be acquired through modeling, conditioning, or trauma (Copeland et al., 2014).
Late-life anxiety also occurs in older adults. This type of anxiety may be difficult to diagnose as
older adults may have multiple medical and psychiatric issues. They may also be on medication
that affects the physiological pathways in anxiety such as the medication used for treating
Asthma, Depression, and High Blood Pressure (Cassidy & Rector, 2008; Liebman & Allen,
1995). Late-life anxiety will be discussed in detail in the subsequent chapter of this study.
The disorder of anxiety and cognitive decline are defined in both research and clinical settings.
With respect to ageing, it also affects the facial expressions of an individual because when a
person starts to age, the flexibility of the muscles starts decreasing as well (Lindesay, Stewart, &
Bisla, 2012; Lezak, Howieson, Bigler, et al., 2012). It is because the muscles of the skin and its
cells are very delicate and after a few times, it starts losing its capability to hold all the cells
together. So, when these cells moves apart, wrinkles start to appear on the face. So, it also
6
affects the emotional expressions as well (American Psychiatric Association, 2013). According
to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), various
factors of the anxiety disorders were classified as fear, anxiety and other external disturbing
factors.
1.1.3 Risk Factors/Assessment for Anxiety in Old Age
There are three classes of factors that affects the risk of developing anxiety symptoms -
premorbid vulnerability factors, destabilization factors (triggering the onset of particular
episodes), and restitution factors (Lindesay and et al., 2012). Exposure to specific risk factors
varies across the lifespan (Acierno and et.al, 2006). Another way of classifying risk factors
related to anxiety is as - biological, psychological, or social. The primary biological factors
associated with the risk for anxiety symptoms and disorders includes poor self-perceived health,
functional limitation, and number of chronic health problems (Lindesay and et al., 2012; Vink,
Aartsen and Schovers, 2008). The psychological risk factors for anxiety includes variety of
factors such as neuroticism, poor coping strategies, external locus of control, and
psychopathology (Vink and et al., 2008).
Some identified social risk factors for anxiety in late life involve social demographic associations
like lower educational level, female gender (Vink et al., 2008), size and quality of social
networks (Lindesay et al., 2012). Infrequent social contacts, low income, childlessness, and
adverse life events have also been associated with anxiety. There is little evidence on difference
in prevalence rates of anxiety disorders among different racial and ethnic ageing groups
(Lindesay et al., 2012).
There are enormous number of anxiety assessment scales that are being used for adults
who come under the age of 65 and over, out of all those, only a few of them have sufficient
7
to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), various
factors of the anxiety disorders were classified as fear, anxiety and other external disturbing
factors.
1.1.3 Risk Factors/Assessment for Anxiety in Old Age
There are three classes of factors that affects the risk of developing anxiety symptoms -
premorbid vulnerability factors, destabilization factors (triggering the onset of particular
episodes), and restitution factors (Lindesay and et al., 2012). Exposure to specific risk factors
varies across the lifespan (Acierno and et.al, 2006). Another way of classifying risk factors
related to anxiety is as - biological, psychological, or social. The primary biological factors
associated with the risk for anxiety symptoms and disorders includes poor self-perceived health,
functional limitation, and number of chronic health problems (Lindesay and et al., 2012; Vink,
Aartsen and Schovers, 2008). The psychological risk factors for anxiety includes variety of
factors such as neuroticism, poor coping strategies, external locus of control, and
psychopathology (Vink and et al., 2008).
Some identified social risk factors for anxiety in late life involve social demographic associations
like lower educational level, female gender (Vink et al., 2008), size and quality of social
networks (Lindesay et al., 2012). Infrequent social contacts, low income, childlessness, and
adverse life events have also been associated with anxiety. There is little evidence on difference
in prevalence rates of anxiety disorders among different racial and ethnic ageing groups
(Lindesay et al., 2012).
There are enormous number of anxiety assessment scales that are being used for adults
who come under the age of 65 and over, out of all those, only a few of them have sufficient
7
psychometric evidence that can provide a sort of support to make use of it for this age group: the
Penn State Worry Questionnaire (PSWQ14), the Beck Anxiety Inventory (BAI13), and the
Geriatric Mental Status Examination (GMSE15) (Lindesay et al., 2012). In recent years,
however, more instruments can be developed to identify and for the measure anxiety or validated
specifically for older adults. Such recent instruments include the RAID (rating anxiety in
dementia) tool, Short Anxiety Screening Test (SAST) for medical in-patients and out-patients,
FEAR tool for older adults in primary care, the Worry Scale (WS), and the Geriatric Anxiety
Inventory (GAI20) tools (Lindesay et al., 2012). This study make use of the State-Trait Anxiety
Inventory (STAI) and Beck Anxiety Inventory (BAI). STAI is a validated tool that has been
observed that it is commonly used in clinical settings to diagnose anxiety, and while the
distinguishment of the anxiety from other depressive syndromes. In research, it is often used to
identify caregiver distress. The Beck Anxiety Inventory (BAI) is a 21-item validated self-report
inventory that is used to assess levels of anxiety in both adults and adolescents.
1.1.4 Co-Morbidities
Co morbidity is considered as the condition in which the person is suffering from two or
more than two diseases. The diseases sometimes overlaps with a few complications as well. The
issue can be any primary disorder or diseases. In this, both the diseases or all ones occur at the
same time. There is very less chance of the one occurring before or after the other one. The
diseases in a person occur each other. Co morbidity of various syndromes such as the
psychiatric syndrome are very common. Several conditions co-exist with anxiety. These
conditions are important in differential diagnosis. They are discussed following. It has been
observed that more than 50% of the older adults on an overall population, face this issue. The
prevalence of co morbid anxiety disorder along with the major depressive disorder (MDD), the
8
Penn State Worry Questionnaire (PSWQ14), the Beck Anxiety Inventory (BAI13), and the
Geriatric Mental Status Examination (GMSE15) (Lindesay et al., 2012). In recent years,
however, more instruments can be developed to identify and for the measure anxiety or validated
specifically for older adults. Such recent instruments include the RAID (rating anxiety in
dementia) tool, Short Anxiety Screening Test (SAST) for medical in-patients and out-patients,
FEAR tool for older adults in primary care, the Worry Scale (WS), and the Geriatric Anxiety
Inventory (GAI20) tools (Lindesay et al., 2012). This study make use of the State-Trait Anxiety
Inventory (STAI) and Beck Anxiety Inventory (BAI). STAI is a validated tool that has been
observed that it is commonly used in clinical settings to diagnose anxiety, and while the
distinguishment of the anxiety from other depressive syndromes. In research, it is often used to
identify caregiver distress. The Beck Anxiety Inventory (BAI) is a 21-item validated self-report
inventory that is used to assess levels of anxiety in both adults and adolescents.
1.1.4 Co-Morbidities
Co morbidity is considered as the condition in which the person is suffering from two or
more than two diseases. The diseases sometimes overlaps with a few complications as well. The
issue can be any primary disorder or diseases. In this, both the diseases or all ones occur at the
same time. There is very less chance of the one occurring before or after the other one. The
diseases in a person occur each other. Co morbidity of various syndromes such as the
psychiatric syndrome are very common. Several conditions co-exist with anxiety. These
conditions are important in differential diagnosis. They are discussed following. It has been
observed that more than 50% of the older adults on an overall population, face this issue. The
prevalence of co morbid anxiety disorder along with the major depressive disorder (MDD), the
8
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
average rate is estimated as high as 60%. Co morbidity refers to the situation when the same
person is facing two or more than two disorders. The occurrence of the both disorders is not
necessary to happen at some specific time. Anyone can occur before, so does the second one
following the first one. Various interactions are also being seen which can even make the whole
condition worst. According to GAD, the co morbidity rates have been evaluated as equal or in
some case, more than that of the anxiety disorders.
Fear
Both fear and anxiety act as signals of threat, danger, or motivational conflict. The two
emotions trigger appropriate adaptive responses to the stimuli or stress. However, they are
distinct emotions. Fear is a motivational state that is caused by specific stimuli or known external
danger, and leads to defensive behavior or escape (Steimer, 2002). Avoidance behavior may be
shown to fear situations that have been learned through previous exposure to pain or stress.
Sense of fear in a person can be because of various factors such as the person might have
experienced some bad experience, because of which the fear has been involved in the mental
status of the person that they are unable to forget it. Being afraid because of any such situation,
whether of past or current situation is called as fear. There are various ways as well which can
help in excluding out all the fear. It is important to compete with the fear, avoiding it can make
the person weaker and a looser as well. So, it is important to compete with the fear and do that
thing only from which the person is afraid from. It is because when once the person will face that
situation, in that case, they get more familiar to that thing, so they will stop being afraid of the
same. Doing that things again and again can help in increasing the rate of confidence so that the
person can be able to compete with it and in any part of the life, it does not act as a barrier or
9
person is facing two or more than two disorders. The occurrence of the both disorders is not
necessary to happen at some specific time. Anyone can occur before, so does the second one
following the first one. Various interactions are also being seen which can even make the whole
condition worst. According to GAD, the co morbidity rates have been evaluated as equal or in
some case, more than that of the anxiety disorders.
Fear
Both fear and anxiety act as signals of threat, danger, or motivational conflict. The two
emotions trigger appropriate adaptive responses to the stimuli or stress. However, they are
distinct emotions. Fear is a motivational state that is caused by specific stimuli or known external
danger, and leads to defensive behavior or escape (Steimer, 2002). Avoidance behavior may be
shown to fear situations that have been learned through previous exposure to pain or stress.
Sense of fear in a person can be because of various factors such as the person might have
experienced some bad experience, because of which the fear has been involved in the mental
status of the person that they are unable to forget it. Being afraid because of any such situation,
whether of past or current situation is called as fear. There are various ways as well which can
help in excluding out all the fear. It is important to compete with the fear, avoiding it can make
the person weaker and a looser as well. So, it is important to compete with the fear and do that
thing only from which the person is afraid from. It is because when once the person will face that
situation, in that case, they get more familiar to that thing, so they will stop being afraid of the
same. Doing that things again and again can help in increasing the rate of confidence so that the
person can be able to compete with it and in any part of the life, it does not act as a barrier or
9
challenge. Anxiety on the other hand, is a generalized response to internal conflict or an
unknown threat (Steimer, 2002). The same brain structures are involves in the neurology of fear
and anxiety and these are discussed below.
Depression
Depression is a mood disorder characterized by loss of interest and persistent feeling of
sadness. Depression can be caused by various number of reasons such as because of family
issues, relationship issues or because of any other personal issues. Often when people go through
depression, various negative thoughts come in mind such as suicidal factors etc. It is because at
this time, the person feels demotivated because of their own life (Corna, Cairney, Herrmann et
al., 2007; Lindesay et al., 2012). It largely affects the lifestyle of the person as well because
somewhere it affects the mental stability of the person, so the person is not able to think and act
properly. In such situations, the person wants to stay alone, out of all the external world. There
are various symptoms of depression by which it is easy to ensure that the person is facing
depression or not. Some of very common and well known examples of it are considered as
tearfulness, in which the person feels sensitive enough that they are being affected by very small
things and starts crying on every small factors. Another symptom can be considered as
hopelessness in which the person is depressed to an extent that they have lost all its hopes that
they can do something in the future. Also, the person observes less appetite and lack of sleep as
well because in their mind, they have been thinking the same things and considerations only
which are bothering the person in actual, which is their main issue. Comorbidity is considered as
the situation when the person is suffering from one or more diseases or dis orders. It is also
termed as an additional source.
10
unknown threat (Steimer, 2002). The same brain structures are involves in the neurology of fear
and anxiety and these are discussed below.
Depression
Depression is a mood disorder characterized by loss of interest and persistent feeling of
sadness. Depression can be caused by various number of reasons such as because of family
issues, relationship issues or because of any other personal issues. Often when people go through
depression, various negative thoughts come in mind such as suicidal factors etc. It is because at
this time, the person feels demotivated because of their own life (Corna, Cairney, Herrmann et
al., 2007; Lindesay et al., 2012). It largely affects the lifestyle of the person as well because
somewhere it affects the mental stability of the person, so the person is not able to think and act
properly. In such situations, the person wants to stay alone, out of all the external world. There
are various symptoms of depression by which it is easy to ensure that the person is facing
depression or not. Some of very common and well known examples of it are considered as
tearfulness, in which the person feels sensitive enough that they are being affected by very small
things and starts crying on every small factors. Another symptom can be considered as
hopelessness in which the person is depressed to an extent that they have lost all its hopes that
they can do something in the future. Also, the person observes less appetite and lack of sleep as
well because in their mind, they have been thinking the same things and considerations only
which are bothering the person in actual, which is their main issue. Comorbidity is considered as
the situation when the person is suffering from one or more diseases or dis orders. It is also
termed as an additional source.
10
An overlap may occur in between the situation when a person is suffering from two or
more diseases, because of evidence for shared genes in their biological pathways, shared brain
mechanisms, and often, shared treatment effects (Goodwin, 2015). There is co-morbidity
between the two conditions at case levels (Lindesay et al., 2012); about 85% of patients who
suffer with depression have significant anxiety, while 90% of patients with anxiety disorder have
depression. Diagnostic criteria designed to distinguish between the disorders exclude clinical
features common to more than one, although many common somatic symptoms occur in the two
disorders (Tiller, 2012). The high comorbidity rates for depression in anxiety cases (Lindesay et
al., 2012), the ability of depression to disrupt day-to-day functioning (Goodwin, 2015; Tiller,
2012), combined with the fact that depression on its own is one of the most common mental
health problems (Tiller, 2012) may be responsible for the tendency to focus on depression
compared to anxiety.
There is also co-morbidity between bipolar disorder [a condition that involves mania and
depression] and anxiety disorders across all ages, including older adulthood (Lindesay et al.,
2012). There is extensive co-morbidity between depression in old age and GAD (Hopko,
Bourland, Stanley et al. 2000). This co-morbidity is associated with greater severity of GAD
severity, impaired response to treatment, as well as increased suicidal ideation (Hopko et al.,
2000; Lindesay et al., 2012). There is also a co-morbidity between depression and many other
anxiety disorders in old age such as panic disorder, social phobia, and agoraphobia (Bartels,
Coakley, Oxman et al., 2002; Corna et al., 2007; Lindesay et al., 2012).
11
more diseases, because of evidence for shared genes in their biological pathways, shared brain
mechanisms, and often, shared treatment effects (Goodwin, 2015). There is co-morbidity
between the two conditions at case levels (Lindesay et al., 2012); about 85% of patients who
suffer with depression have significant anxiety, while 90% of patients with anxiety disorder have
depression. Diagnostic criteria designed to distinguish between the disorders exclude clinical
features common to more than one, although many common somatic symptoms occur in the two
disorders (Tiller, 2012). The high comorbidity rates for depression in anxiety cases (Lindesay et
al., 2012), the ability of depression to disrupt day-to-day functioning (Goodwin, 2015; Tiller,
2012), combined with the fact that depression on its own is one of the most common mental
health problems (Tiller, 2012) may be responsible for the tendency to focus on depression
compared to anxiety.
There is also co-morbidity between bipolar disorder [a condition that involves mania and
depression] and anxiety disorders across all ages, including older adulthood (Lindesay et al.,
2012). There is extensive co-morbidity between depression in old age and GAD (Hopko,
Bourland, Stanley et al. 2000). This co-morbidity is associated with greater severity of GAD
severity, impaired response to treatment, as well as increased suicidal ideation (Hopko et al.,
2000; Lindesay et al., 2012). There is also a co-morbidity between depression and many other
anxiety disorders in old age such as panic disorder, social phobia, and agoraphobia (Bartels,
Coakley, Oxman et al., 2002; Corna et al., 2007; Lindesay et al., 2012).
11
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Physical illness
Physical health is considered as a health issue that has very fewer chances of going away.
There are various common and well known examples of the physical illness and some of them
involves asthma, diabetes, cancer etc. These are considered as such diseases that have very less
or no chance of getting prevented. Once the person has been got any of these, then it is difficult
to exclude completely. Although, medicines are been taken in order to have a sort of relief from
the symptoms of these diseases but the proper and the ultimate cure has not been yet found.
Anxiety has its important role as well in this because these symptoms only cause pain, weakness,
dizziness etc in a person. The issue of anxiety may also cause less appetite in an individual. It has
also been observed that anxiety also results in various complications in the physical life, so it
affects the relationship as well because it makes decreased level of interest.
The constant state of anxiety can lead to a person getting in depression and that too in a
huge extent. Anxieties also cause phobias as well in which the person goes through an irrational
fear of any specific thing. It can be smaller as ant or can be bigger as well. In this, the person
feels afraid of from what they have phobias with such as some does not want to go to a crowded
place. It may be because of various factors such as the person may feel insecure or the person is
afraid to face the crowd. So, this is considered as a very common disorder of anxiety. Another
very important disorder of anxiety is that the person wants to stay alone and does not want to
interact with others and wants to stay in enclosed spaces. Generalized anxiety disorder is one of
the very basic and well known disorder of anxiety in which the person feels worried about their
selves, their health, money, security, safety. Because of overthinking, the person often feels
muscle pain, headaches, breathlessness, insomnia etc. These happen because of the overthinking
12
Physical health is considered as a health issue that has very fewer chances of going away.
There are various common and well known examples of the physical illness and some of them
involves asthma, diabetes, cancer etc. These are considered as such diseases that have very less
or no chance of getting prevented. Once the person has been got any of these, then it is difficult
to exclude completely. Although, medicines are been taken in order to have a sort of relief from
the symptoms of these diseases but the proper and the ultimate cure has not been yet found.
Anxiety has its important role as well in this because these symptoms only cause pain, weakness,
dizziness etc in a person. The issue of anxiety may also cause less appetite in an individual. It has
also been observed that anxiety also results in various complications in the physical life, so it
affects the relationship as well because it makes decreased level of interest.
The constant state of anxiety can lead to a person getting in depression and that too in a
huge extent. Anxieties also cause phobias as well in which the person goes through an irrational
fear of any specific thing. It can be smaller as ant or can be bigger as well. In this, the person
feels afraid of from what they have phobias with such as some does not want to go to a crowded
place. It may be because of various factors such as the person may feel insecure or the person is
afraid to face the crowd. So, this is considered as a very common disorder of anxiety. Another
very important disorder of anxiety is that the person wants to stay alone and does not want to
interact with others and wants to stay in enclosed spaces. Generalized anxiety disorder is one of
the very basic and well known disorder of anxiety in which the person feels worried about their
selves, their health, money, security, safety. Because of overthinking, the person often feels
muscle pain, headaches, breathlessness, insomnia etc. These happen because of the overthinking
12
about themselves and their body. So this worried ness makes them more tired and it results in
affecting different parts of the body.
Physical illness and various disabilities are common across the life span. However, some
risk factors (premorbid vulnerability factors that trigger anxiety episodes and restitution factors
that determine duration of the episode) and some disability may be more prevalent in old age,
making it highly probable that a degree of co-occurrence will occur with psychiatric disorders
such as anxiety and depression (Lindesay et al., 2012). However, higher rates of co-morbidity
have been observed for anxiety and some medical conditions such as respiratory and cardiac
disorders, indicating that there is some causality. Studies shows that approximately one-third of
older patients with cardiac conditions have an anxiety disorder. Similarly, half of older patients
with chronic obstructive pulmonary disease (COPD) have an anxiety disorder (Vogele & von
Leupoldt, 2008). Other physical illnesses associated with anxiety and anxiety disorders in older
adults include Parkinson’s disease, Alzheimer’s disease, postural disturbance, and vestibular
disease (Lindesay et al., 2012; Mehta Yaffe, Brenes et al., 2007).
Mild/Severe Cognitive impairment
Cognitive impairment is considered as an intermediate stage within the two factors which
involves the expected cognitive decline for ageing normally and serious decline of dementia as
well. It can include various issues with languages, memory, making judgments, understanding
things etc. There are various causes of cognitive disorder, some of which includes some physical
injuries, substance abuse etc. Substance abuse can prove every harmful for a person because in
this, the drugs make the person in a way that they lose their capability of thinking and
understanding facts. They are not even in their senses as well for a few amounts of time after
13
affecting different parts of the body.
Physical illness and various disabilities are common across the life span. However, some
risk factors (premorbid vulnerability factors that trigger anxiety episodes and restitution factors
that determine duration of the episode) and some disability may be more prevalent in old age,
making it highly probable that a degree of co-occurrence will occur with psychiatric disorders
such as anxiety and depression (Lindesay et al., 2012). However, higher rates of co-morbidity
have been observed for anxiety and some medical conditions such as respiratory and cardiac
disorders, indicating that there is some causality. Studies shows that approximately one-third of
older patients with cardiac conditions have an anxiety disorder. Similarly, half of older patients
with chronic obstructive pulmonary disease (COPD) have an anxiety disorder (Vogele & von
Leupoldt, 2008). Other physical illnesses associated with anxiety and anxiety disorders in older
adults include Parkinson’s disease, Alzheimer’s disease, postural disturbance, and vestibular
disease (Lindesay et al., 2012; Mehta Yaffe, Brenes et al., 2007).
Mild/Severe Cognitive impairment
Cognitive impairment is considered as an intermediate stage within the two factors which
involves the expected cognitive decline for ageing normally and serious decline of dementia as
well. It can include various issues with languages, memory, making judgments, understanding
things etc. There are various causes of cognitive disorder, some of which includes some physical
injuries, substance abuse etc. Substance abuse can prove every harmful for a person because in
this, the drugs make the person in a way that they lose their capability of thinking and
understanding facts. They are not even in their senses as well for a few amounts of time after
13
doing substance abuse. Because if considering these factors, smoking and drinking are two that
habits which can be even controlled by some specific measures but controlling substance abuse
is quite hard as compared to two of these. It is a tough job to exclude from these things once
attached to (Beaudreau & Hara, 2008). There can be various reasons why people do this. Some
do it for passing time, some because of any mental pressure, some because of the fact of not
achieving anything in their life. There are enormous number of reasons why people do substance
abuse.
Some people also do it because of the peer pressure. It is because when the surrounding
people, friends etc are doing substance abuse, so the person just because in sake of maintaining
their respect in front of them also gets involved with them and does substance abuse. Although
while taking it, they do not realize that they can get addicted to it but after a few times, they get
to understand that it is difficult for them to stay without it (Beaudreau & Hara, 2008). It is
because when they do not take it, they observe some sort of changes in their body such as some
feel like nausea, some feels like sleeping the whole day etc. They do not feel good if they do not
do substance abuse. Even some people when do not get these drugs, they do various such
activities to purchase it. It has been observed that many people who get addicted to it and does
not get it sometimes because of some issue like money etc., they even steal money just because
to take it. In order to do the substance abuse, they do not realize what they are doing and how it
can result. At that time, they just want to do substance abuse, nothing else matters for them at
that time. Cognitive impairment may range from mild to severe.
Mild impairment involves changes in cognitive functions that does not prevent the
affected person from carrying out their day-to-day activities. Severe levels of cognitive
impairment may result in loss of the ability to talk, write, comprehend important issues, and
14
habits which can be even controlled by some specific measures but controlling substance abuse
is quite hard as compared to two of these. It is a tough job to exclude from these things once
attached to (Beaudreau & Hara, 2008). There can be various reasons why people do this. Some
do it for passing time, some because of any mental pressure, some because of the fact of not
achieving anything in their life. There are enormous number of reasons why people do substance
abuse.
Some people also do it because of the peer pressure. It is because when the surrounding
people, friends etc are doing substance abuse, so the person just because in sake of maintaining
their respect in front of them also gets involved with them and does substance abuse. Although
while taking it, they do not realize that they can get addicted to it but after a few times, they get
to understand that it is difficult for them to stay without it (Beaudreau & Hara, 2008). It is
because when they do not take it, they observe some sort of changes in their body such as some
feel like nausea, some feels like sleeping the whole day etc. They do not feel good if they do not
do substance abuse. Even some people when do not get these drugs, they do various such
activities to purchase it. It has been observed that many people who get addicted to it and does
not get it sometimes because of some issue like money etc., they even steal money just because
to take it. In order to do the substance abuse, they do not realize what they are doing and how it
can result. At that time, they just want to do substance abuse, nothing else matters for them at
that time. Cognitive impairment may range from mild to severe.
Mild impairment involves changes in cognitive functions that does not prevent the
affected person from carrying out their day-to-day activities. Severe levels of cognitive
impairment may result in loss of the ability to talk, write, comprehend important issues, and
14
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
ultimately, inability to live independently. Both anxiety and cognitive impairment are common in
the ageing adult population (Beaudreau & Hara, 2008; Lindesay et al., 2012). In many cases,
there is evidence suggesting a causal relationship. Baseline anxiety symptoms or disorders for
example, have been shown to predict cognitive decline in prospective studies (Lindesay et al.,
2012). Studies also show that veterans with PTSD have higher chances of developing dementia
compared to those without PTSD (Cooper, Bebbington, Lindesay et al 2011). Research shows
that there is a reciprocal relationship between late-life anxiety and cognition in the sense that the
presence of one condition generates the symptoms of the other and vice versa (Beaudreau &
Hara, 2008).
The relationship between cognitive performance and anxiety is quite complicated because
there are various complications in the cognitive impairment and anxiety. On a significant scale, it
has been observed that the clinical anxiety has a large and negative impact on the normal and
basic cognitive abilities (Cooper et al., 2011; Lindesay et al., 2012). Anxiety has also been
associated with lower levels of cognitive performance in case of older adults. Because of anxiety,
the effective cognitive functioning can get affected such as sleep disorders, poor level of
concentration and understanding and useless worries and stress factors as well (Castaneda et al.,
2008).
Studies have found that cognitive impairments depend on level of anxiety; high level
anxiety is associated with more agitation, depression, and sleep disorders. High state anxiety was
also associated with more compromise in their instrumental daily functions and executive
functioning (Rozzini et al., 2009). In terms of the sequence of effects, anxiety may develop after
the individual becomes aware of cognitive decline as a response to the decline and its possible
implications. In people with dementia, for example, epidemiological evidence seems to suggest
15
the ageing adult population (Beaudreau & Hara, 2008; Lindesay et al., 2012). In many cases,
there is evidence suggesting a causal relationship. Baseline anxiety symptoms or disorders for
example, have been shown to predict cognitive decline in prospective studies (Lindesay et al.,
2012). Studies also show that veterans with PTSD have higher chances of developing dementia
compared to those without PTSD (Cooper, Bebbington, Lindesay et al 2011). Research shows
that there is a reciprocal relationship between late-life anxiety and cognition in the sense that the
presence of one condition generates the symptoms of the other and vice versa (Beaudreau &
Hara, 2008).
The relationship between cognitive performance and anxiety is quite complicated because
there are various complications in the cognitive impairment and anxiety. On a significant scale, it
has been observed that the clinical anxiety has a large and negative impact on the normal and
basic cognitive abilities (Cooper et al., 2011; Lindesay et al., 2012). Anxiety has also been
associated with lower levels of cognitive performance in case of older adults. Because of anxiety,
the effective cognitive functioning can get affected such as sleep disorders, poor level of
concentration and understanding and useless worries and stress factors as well (Castaneda et al.,
2008).
Studies have found that cognitive impairments depend on level of anxiety; high level
anxiety is associated with more agitation, depression, and sleep disorders. High state anxiety was
also associated with more compromise in their instrumental daily functions and executive
functioning (Rozzini et al., 2009). In terms of the sequence of effects, anxiety may develop after
the individual becomes aware of cognitive decline as a response to the decline and its possible
implications. In people with dementia, for example, epidemiological evidence seems to suggest
15
an association with anxiety symptoms, rather than with anxiety disorders (Schaub and et al.,
2012). Anxiety may also manifest in different ways as cognitive impairment progresses, for
instance as agitation. Such symptoms may lead to under-diagnosis of anxiety or a disorder. The
rate of anxiety also appears to vary in different types of dementia; for instance anxiety rates
appear to be higher in vascular dementia compared to Alzheimer’s disease (Lindesay and et al.,
2012).
Subjective cognitive impairment is also considered as the disorder of subjective memory
in which there has been observed some worst cases of the person (Derakshan & Eysenck, 2009;
Stern, 2012; Shadlen & Larson, 2010). It has also been observed that subjective cognitive decline
(SCD) acts as a precursor for the mild cognitive impairment (MCI) but along with it, it is also
considered as an early sign of the Alzheimer's diseases. As per the statistics of 2015, Alzheimer's
association of international conference (AAIC) has evaluated that on analyzing various studies
on SCD, it may act as the first consideration factor for conceptualizing that what are the other
factors and operations that the investigators are looking for (Derakshan and Eysenck, 2009;
Stern, 2012). Subjective cognitive impairment may also constitute a risk factor for dementia,
although it can also have a treatable cause.
1.2 AGEING AND LATE LIFE
Ageing is simply considered as a process of getting older. The term, ageing can refer to
human beings, animals etc. After some time, every living being on the earth goes through this.
When a person starts ageing, the flexibility of skin of a person starts decreasing. It is because
after some time, the cells inside starts losing its flexibility and they start moving apart from each
other, so in that case, it starts reflecting its results and they are visible enough such as the
16
2012). Anxiety may also manifest in different ways as cognitive impairment progresses, for
instance as agitation. Such symptoms may lead to under-diagnosis of anxiety or a disorder. The
rate of anxiety also appears to vary in different types of dementia; for instance anxiety rates
appear to be higher in vascular dementia compared to Alzheimer’s disease (Lindesay and et al.,
2012).
Subjective cognitive impairment is also considered as the disorder of subjective memory
in which there has been observed some worst cases of the person (Derakshan & Eysenck, 2009;
Stern, 2012; Shadlen & Larson, 2010). It has also been observed that subjective cognitive decline
(SCD) acts as a precursor for the mild cognitive impairment (MCI) but along with it, it is also
considered as an early sign of the Alzheimer's diseases. As per the statistics of 2015, Alzheimer's
association of international conference (AAIC) has evaluated that on analyzing various studies
on SCD, it may act as the first consideration factor for conceptualizing that what are the other
factors and operations that the investigators are looking for (Derakshan and Eysenck, 2009;
Stern, 2012). Subjective cognitive impairment may also constitute a risk factor for dementia,
although it can also have a treatable cause.
1.2 AGEING AND LATE LIFE
Ageing is simply considered as a process of getting older. The term, ageing can refer to
human beings, animals etc. After some time, every living being on the earth goes through this.
When a person starts ageing, the flexibility of skin of a person starts decreasing. It is because
after some time, the cells inside starts losing its flexibility and they start moving apart from each
other, so in that case, it starts reflecting its results and they are visible enough such as the
16
wrinkles many people have in their old age (Besdine, 2017). That is considered as the fact that
the person has start getting old. There are various effects of ageing. Very common and well
known examples of it can be considered as that in case of teenagers, the normal range of hearing
comes within 20 to 20,000 Hz which means if a person listens to a voice greater than this
frequency, it may damage their ear and hearing power because there have been different range
for every living being. Such as for dogs, cats, it is different, for human beings, it is different. So
any living being if goes through a very high frequency of more than the normal level, in that case
it can directly affect the hearing range of the person. It has also been observed that in the middle
of 20's, the cognitive decline of a person starts (Besdine, 2017; Vincent & Victoria, 2010).
Another important factor of ageing is that wrinkles also happen because of photo ageing and
moreover, it affects those areas that are exposed of the sun rays. Age matters a lot, specially in
case of women as when a girl goes mature, she got to know about mensuration which engages
four to five days of a woman. After a long time period of this, in the late forty's, i.e. from 49 –
52 years, the women goes under a situation called menopause. It is the stopping of the
mensuration period after which the women cannot fertile further. From the age of 50, the hair
starts getting Grey. Ageing can also be described in various ways such as chronologically,
biologically, and psychologically. Chronological age is based on the passage of time and
represents a person’s age in years. Since the likelihood of health problems developing increases
as people age, chronological age helps to predict many health problems and as a result, it is used
for certain legal and financial purposes (Besdine, 2017). Biological age describes the changes
that occur in the body as people age. This change differs for different people and some people
may be biologically old at 40 while others get old at later ages. Psychological age refers to how
people act and feel. A person may be chronologically old but participates in many activities and
17
the person has start getting old. There are various effects of ageing. Very common and well
known examples of it can be considered as that in case of teenagers, the normal range of hearing
comes within 20 to 20,000 Hz which means if a person listens to a voice greater than this
frequency, it may damage their ear and hearing power because there have been different range
for every living being. Such as for dogs, cats, it is different, for human beings, it is different. So
any living being if goes through a very high frequency of more than the normal level, in that case
it can directly affect the hearing range of the person. It has also been observed that in the middle
of 20's, the cognitive decline of a person starts (Besdine, 2017; Vincent & Victoria, 2010).
Another important factor of ageing is that wrinkles also happen because of photo ageing and
moreover, it affects those areas that are exposed of the sun rays. Age matters a lot, specially in
case of women as when a girl goes mature, she got to know about mensuration which engages
four to five days of a woman. After a long time period of this, in the late forty's, i.e. from 49 –
52 years, the women goes under a situation called menopause. It is the stopping of the
mensuration period after which the women cannot fertile further. From the age of 50, the hair
starts getting Grey. Ageing can also be described in various ways such as chronologically,
biologically, and psychologically. Chronological age is based on the passage of time and
represents a person’s age in years. Since the likelihood of health problems developing increases
as people age, chronological age helps to predict many health problems and as a result, it is used
for certain legal and financial purposes (Besdine, 2017). Biological age describes the changes
that occur in the body as people age. This change differs for different people and some people
may be biologically old at 40 while others get old at later ages. Psychological age refers to how
people act and feel. A person may be chronologically old but participates in many activities and
17
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
have a youthful attitude to life. Such a person is considered psychologically young (Besdine,
2017). In the context of this study, the focus is on chronological ageing and related effects with
regard to anxiety.
Although people may age differently, there are biological changes that occur from the
ageing process itself, a process termed normal ageing (Besdine, 2017; Salthouse, 2009). Such
normal ageing processes are expected and may be unavoidable. For example, presbyopia occurs
in older people – a condition in which the lens of the eye stiffens, thickens, becoming less able to
focus on objects that are close, such as reading materials (Salthouse, 2012). Functional decline
also occurs as part of the normal ageing process. This decline may include increased difficulty in
learning new languages or increased forgetfulness. In normal ageing, people may misplace
objects or forget certain details. Blood sugar levels may also increase more after carbohydrates
are eaten in ageing people compared to younger people. However, where these changes exceed
certain levels or limits, they constitute a pathological condition. For example, people who have
dementia have difficulty understanding their environment, forget entire events, and may have
difficulty doing normal tasks like cooking and driving. Similarly, where blood sugar levels
exceed certain levels, a diagnosis of diabetes will be made (Besdine, 2017)
Healthy ageing refers to the reduction or postponement of the undesired effects
associated with ageing. In healthy ageing, the goals are to maintain physical and mental health,
avoid disorders, and remain independent and active. Developing healthy habits such as
exercising regularly, nutritious diet, and staying mentally active can contribute to healthy ageing.
Similarly, people can also take certain actions to compensate for changes in normal ageing
(Besdine, 2017). The concept of ageing is related to life expectancy in the sense that life
expectancy is influenced by heredity, life style, exposure to environmental toxins, and
18
2017). In the context of this study, the focus is on chronological ageing and related effects with
regard to anxiety.
Although people may age differently, there are biological changes that occur from the
ageing process itself, a process termed normal ageing (Besdine, 2017; Salthouse, 2009). Such
normal ageing processes are expected and may be unavoidable. For example, presbyopia occurs
in older people – a condition in which the lens of the eye stiffens, thickens, becoming less able to
focus on objects that are close, such as reading materials (Salthouse, 2012). Functional decline
also occurs as part of the normal ageing process. This decline may include increased difficulty in
learning new languages or increased forgetfulness. In normal ageing, people may misplace
objects or forget certain details. Blood sugar levels may also increase more after carbohydrates
are eaten in ageing people compared to younger people. However, where these changes exceed
certain levels or limits, they constitute a pathological condition. For example, people who have
dementia have difficulty understanding their environment, forget entire events, and may have
difficulty doing normal tasks like cooking and driving. Similarly, where blood sugar levels
exceed certain levels, a diagnosis of diabetes will be made (Besdine, 2017)
Healthy ageing refers to the reduction or postponement of the undesired effects
associated with ageing. In healthy ageing, the goals are to maintain physical and mental health,
avoid disorders, and remain independent and active. Developing healthy habits such as
exercising regularly, nutritious diet, and staying mentally active can contribute to healthy ageing.
Similarly, people can also take certain actions to compensate for changes in normal ageing
(Besdine, 2017). The concept of ageing is related to life expectancy in the sense that life
expectancy is influenced by heredity, life style, exposure to environmental toxins, and
18
healthcare. Heredity influences the possibility of developing certain disorders as well as the
possibility of living to very old age. Healthy lifestyles such as avoiding smoking, healthy diet
and exercising improve body functions and help people avoid disorders. Exposure to toxins can
be dangerous and shorten life expectancy despite the best genetic makeup. Preventing or treating
disorders helps increase life expectancy (Besdine, 2017).
While people do not become elderly at a specific age, 65 has been traditionally designated as
when old age begins as evident in retirement programs (Besdine, 2017; Vincent & Victoria,
2010). As already mentioned above, subtle cognitive changes are associated with ageing
(Salthouse, 2010).
There are various pathological conditions as well which involves cognitive impairment
and dementia and refers to the fact that these are common in old age. It is because as the person
ages, the stability of the person starts decreasing and the body also starts lowering its rate of
metabolism and doing activities (Salthouse, 2010; Salthouse, 2012). The number of persons over
the age of 65 and it is then projected to double across the next forty years (Harada, Love &
Triebeld, 2013; Vincent & Victoria, 2010). Considering this feature, it also helps in
understanding and analyzing better the cognitive and normal changes that can occur in ageing
and it is being done because these changes affect the daily operations and functioning of life. It is
better if one understands the general and normal cognitive changes and it is so because these
changes may affect the daily function of the older adult (Salthouse, 2009). In addition, making
the difference between the normal and the abnormal diseases is considered as a simple and easy
task (Harada et al., 2013). The neurocognitive changes in ageing are discussed in detail
following, as well as the structural and functional changes in ageing. Such structural and
functional alterations may explain observed cognitive changes.
19
possibility of living to very old age. Healthy lifestyles such as avoiding smoking, healthy diet
and exercising improve body functions and help people avoid disorders. Exposure to toxins can
be dangerous and shorten life expectancy despite the best genetic makeup. Preventing or treating
disorders helps increase life expectancy (Besdine, 2017).
While people do not become elderly at a specific age, 65 has been traditionally designated as
when old age begins as evident in retirement programs (Besdine, 2017; Vincent & Victoria,
2010). As already mentioned above, subtle cognitive changes are associated with ageing
(Salthouse, 2010).
There are various pathological conditions as well which involves cognitive impairment
and dementia and refers to the fact that these are common in old age. It is because as the person
ages, the stability of the person starts decreasing and the body also starts lowering its rate of
metabolism and doing activities (Salthouse, 2010; Salthouse, 2012). The number of persons over
the age of 65 and it is then projected to double across the next forty years (Harada, Love &
Triebeld, 2013; Vincent & Victoria, 2010). Considering this feature, it also helps in
understanding and analyzing better the cognitive and normal changes that can occur in ageing
and it is being done because these changes affect the daily operations and functioning of life. It is
better if one understands the general and normal cognitive changes and it is so because these
changes may affect the daily function of the older adult (Salthouse, 2009). In addition, making
the difference between the normal and the abnormal diseases is considered as a simple and easy
task (Harada et al., 2013). The neurocognitive changes in ageing are discussed in detail
following, as well as the structural and functional changes in ageing. Such structural and
functional alterations may explain observed cognitive changes.
19
1.2.1 Cognitive Changes in Normal ageing
Usually people have a misunderstanding of the fact that because of the process of ageing,
there is also observed a loss in the cognitive abilities. However, it has not yet proved true.
Although there are some areas that have observed to a bit change because of ageing but not all
factors come in the same category. All the interventions with their functions are discussed as
following:
Intelligence
Crystallized intelligence describes the abilities, skills, and knowledge that is familiar and
well-practiced such as vocabulary and general knowledge. Such abilities either remain stable or
else gradually improve through the sixth and seventh life decades an annual rate of 0.02 to 0.003
standard deviations (Harada et al., 2013; Salthouse, 2012). Adults usually perform better in tasks
requiring crystallized intelligence compared to young people since crystallized intelligence is
based on information accumulated based on one’s life experiences (Elias & Saucier, 2006).
Fluid intelligence, on the other hand, is considered as the capability by which the issues
and problems can get resolved. The resolving of the issues can be done in any way that seems the
best suitable and relevant. The methods for solving the issue can include using logic or use
techniques so that the patterns can be identified etc. If comparing the same with the crystallized
intelligence, it makes use of the knowledge that has been already created. In this, no new
knowledge is being analyzed, the whole process is being evaluated from the old and previous
knowledge as well. It can also be described as the abilities involving reasoning and problem-
20
Usually people have a misunderstanding of the fact that because of the process of ageing,
there is also observed a loss in the cognitive abilities. However, it has not yet proved true.
Although there are some areas that have observed to a bit change because of ageing but not all
factors come in the same category. All the interventions with their functions are discussed as
following:
Intelligence
Crystallized intelligence describes the abilities, skills, and knowledge that is familiar and
well-practiced such as vocabulary and general knowledge. Such abilities either remain stable or
else gradually improve through the sixth and seventh life decades an annual rate of 0.02 to 0.003
standard deviations (Harada et al., 2013; Salthouse, 2012). Adults usually perform better in tasks
requiring crystallized intelligence compared to young people since crystallized intelligence is
based on information accumulated based on one’s life experiences (Elias & Saucier, 2006).
Fluid intelligence, on the other hand, is considered as the capability by which the issues
and problems can get resolved. The resolving of the issues can be done in any way that seems the
best suitable and relevant. The methods for solving the issue can include using logic or use
techniques so that the patterns can be identified etc. If comparing the same with the crystallized
intelligence, it makes use of the knowledge that has been already created. In this, no new
knowledge is being analyzed, the whole process is being evaluated from the old and previous
knowledge as well. It can also be described as the abilities involving reasoning and problem-
20
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
solving concerning things that are independent of lie experiences and less familiar (Elias &
Saucier, 2006; Salthouse, 2012).
Memory
Anxiety throws a huge impact on the memory status of a person. It is because as
discussed earlier, it affects the brain and various reasons why this happened can be consider as
the environmental, genetic factors or because of the involvement of some habits such as
substance abuse etc. The overall intelligence quotient (IQ) level of a person is also related to the
genetic factor as DNA affects a lot, so the features and characteristics of parents reflect on the
child. It can be reflected in any factor (Harada and et. al., 2013). Brain changes and anxiety can
cause problems with memory. At the same time, change in memory represents one of the most
common cognitive changes that occur in older adulthood (Harada and et al., 2013; West & Alain,
2000). This group in general does not perform as well as younger adults on learning and memory
tests (Harada et al., 2013). There can be various changes occur in the memory and usually, these
changes in memory can be considered with the slow processing speed, decreased use of learning
strategies, and the reduced ability to ignore information that is relevant, that occurs with ageing
(Harada and et al., 2013; Schnitzspahn, Stahl, Zeintl, et al., 2012).
Memory can be classified in two ways, either the declarative and the non declarative one.
Declarative or explicit memory must involve conscious gathering of the events and facts (Harada
and et al., 2013). Two types of declarative memory are considered as episodic and semantic
memory (Harada and et al., 2013; Isingrini & Taconnat, 2008). Episodic memory is considered
as the memory that can be used and associated for events that are to be personally experienced
and that events which has an occurrence at a specific time and place. The measurement of
21
Saucier, 2006; Salthouse, 2012).
Memory
Anxiety throws a huge impact on the memory status of a person. It is because as
discussed earlier, it affects the brain and various reasons why this happened can be consider as
the environmental, genetic factors or because of the involvement of some habits such as
substance abuse etc. The overall intelligence quotient (IQ) level of a person is also related to the
genetic factor as DNA affects a lot, so the features and characteristics of parents reflect on the
child. It can be reflected in any factor (Harada and et. al., 2013). Brain changes and anxiety can
cause problems with memory. At the same time, change in memory represents one of the most
common cognitive changes that occur in older adulthood (Harada and et al., 2013; West & Alain,
2000). This group in general does not perform as well as younger adults on learning and memory
tests (Harada et al., 2013). There can be various changes occur in the memory and usually, these
changes in memory can be considered with the slow processing speed, decreased use of learning
strategies, and the reduced ability to ignore information that is relevant, that occurs with ageing
(Harada and et al., 2013; Schnitzspahn, Stahl, Zeintl, et al., 2012).
Memory can be classified in two ways, either the declarative and the non declarative one.
Declarative or explicit memory must involve conscious gathering of the events and facts (Harada
and et al., 2013). Two types of declarative memory are considered as episodic and semantic
memory (Harada and et al., 2013; Isingrini & Taconnat, 2008). Episodic memory is considered
as the memory that can be used and associated for events that are to be personally experienced
and that events which has an occurrence at a specific time and place. The measurement of
21
memory can be done by various factors such as by using the memory of figures, word lists, and
stories, word lists, or figures (Isingrini & Taconnat, 2008). Episodic memory can also be
considered as autobiographical memory. Semantic memory involves various types of
information such as language usage (the meaning of words), and practical knowledge. Both
episodic and semantic memory decline with normal ageing; however, the timing of such decline
is different (Salthouse, 2009). While episodic memory reveals lifelong decline, semantic
memory shows decline in late life (Harada and et al., 2013). Nondeclarative or implicit memory
is outside of an individual’s awareness, for instance how to sing familiar songs. Procedural
memory is a form of nondeclarative memory involving memory for cognitive and motor skills;
for instance, riding a bicycle. Nondeclarative memory does not change across the lifespan
(Harada et al., 2013; Lezak, Howieson, Bigler et al., 2012).
Changes in memory is also another concept which can also be discussed and is based on
various stages of memory. Memory acquisition stage involves the ability to encode new
information into memory (Harada and et al., 2013; Haaland and et al., 2003. It can also be
considered as a process in which all the new data and information is being included in the
memory. The rate of acquisition gets minimized or also can even get declined across the
individual’s lifespan (Delis, Kramer, Kaplan, et al., 2000; Haaland, Price & Larue, 2003). A very
common and well known stage, that is the memory retention state which involves retaining the
data and information successfully. There has been observed a successful rate of adults who are
considered healthy. It also gives a sort of decline in the memory retrieval and along with it, also
in the capability by which it can become more easy that the changes can occur in the memory
and along with it, also in the subjective cognitive impairment (Stern, 2012; Shadlen & Larson,
2010). Memory types and various changes will be discussed in detail in the chapter following.
22
stories, word lists, or figures (Isingrini & Taconnat, 2008). Episodic memory can also be
considered as autobiographical memory. Semantic memory involves various types of
information such as language usage (the meaning of words), and practical knowledge. Both
episodic and semantic memory decline with normal ageing; however, the timing of such decline
is different (Salthouse, 2009). While episodic memory reveals lifelong decline, semantic
memory shows decline in late life (Harada and et al., 2013). Nondeclarative or implicit memory
is outside of an individual’s awareness, for instance how to sing familiar songs. Procedural
memory is a form of nondeclarative memory involving memory for cognitive and motor skills;
for instance, riding a bicycle. Nondeclarative memory does not change across the lifespan
(Harada et al., 2013; Lezak, Howieson, Bigler et al., 2012).
Changes in memory is also another concept which can also be discussed and is based on
various stages of memory. Memory acquisition stage involves the ability to encode new
information into memory (Harada and et al., 2013; Haaland and et al., 2003. It can also be
considered as a process in which all the new data and information is being included in the
memory. The rate of acquisition gets minimized or also can even get declined across the
individual’s lifespan (Delis, Kramer, Kaplan, et al., 2000; Haaland, Price & Larue, 2003). A very
common and well known stage, that is the memory retention state which involves retaining the
data and information successfully. There has been observed a successful rate of adults who are
considered healthy. It also gives a sort of decline in the memory retrieval and along with it, also
in the capability by which it can become more easy that the changes can occur in the memory
and along with it, also in the subjective cognitive impairment (Stern, 2012; Shadlen & Larson,
2010). Memory types and various changes will be discussed in detail in the chapter following.
22
Processing speed
Processing speed describes the speed at which cognitive activities are carried out as well
as speed of motor responses .The process of ageing impacts the speed as it minimizes it to an
extent. Also, it decreases the speed of the motor operations that are being performed. It does not
mean that all the processes and procedures cannot be performed, instead can take a much more
time (Harada et al., 2013; Salthouse, 2010). This decline negatively affects the older adult’s
performance on many neuropsychological tests used in measuring other cognitive domains such
as verbal fluency (Harada et al., 2013).
Reaction time, speed, and variability are related to the integrity of white matter in the
brain, but, they may also have cognitive components. White matter pathways mediate the long-
range information transmission across distributed brain networks. These pathways also support
integration of operations across individual brain areas (Mesulam, 2000; Turken, Whitfield-
Gabrieli, Bammer et al., 2008). Information flows across the brain is regulated by major white
matter tracts and the patterns of interactions created by these tracts account to a large extent for
distributed patterns of cortical activity (Schmahmann & Pandya, 2006; Turken et al., 2008).
Structural variations in these pathways impact on individual differences in cognitive processing
speed (Turken et al., 2008). The degree of myelination and thickness of long myelinated axons in
the CNS impacts on the speed of conduct for neural signals. Thus, White matter diseases, that
lead to demyelination and damage across fiber systems, result to slowing of cognitive processes
(Turken et al., 2008). It is hypothesized that the people who have higher levels of anxiety are
slower and more variable (Harada et al., 2013; Salthouse, 2009; Salthouse, 2010).
23
Processing speed describes the speed at which cognitive activities are carried out as well
as speed of motor responses .The process of ageing impacts the speed as it minimizes it to an
extent. Also, it decreases the speed of the motor operations that are being performed. It does not
mean that all the processes and procedures cannot be performed, instead can take a much more
time (Harada et al., 2013; Salthouse, 2010). This decline negatively affects the older adult’s
performance on many neuropsychological tests used in measuring other cognitive domains such
as verbal fluency (Harada et al., 2013).
Reaction time, speed, and variability are related to the integrity of white matter in the
brain, but, they may also have cognitive components. White matter pathways mediate the long-
range information transmission across distributed brain networks. These pathways also support
integration of operations across individual brain areas (Mesulam, 2000; Turken, Whitfield-
Gabrieli, Bammer et al., 2008). Information flows across the brain is regulated by major white
matter tracts and the patterns of interactions created by these tracts account to a large extent for
distributed patterns of cortical activity (Schmahmann & Pandya, 2006; Turken et al., 2008).
Structural variations in these pathways impact on individual differences in cognitive processing
speed (Turken et al., 2008). The degree of myelination and thickness of long myelinated axons in
the CNS impacts on the speed of conduct for neural signals. Thus, White matter diseases, that
lead to demyelination and damage across fiber systems, result to slowing of cognitive processes
(Turken et al., 2008). It is hypothesized that the people who have higher levels of anxiety are
slower and more variable (Harada et al., 2013; Salthouse, 2009; Salthouse, 2010).
23
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Cognitive inhibition
Cognitive inhibition describes ability of the mind to tune out irrelevant stimuli regarding
tasks or processes at hand. It can be done partially, wholly, intentionally or otherwise (Peter,
Hertwig & Hoffrage, 2004). Cognitive inhibition may be an extension of neural inhibition, the
ability of individual neurons to regulate or stop elements of thought. Lateral inhibition, involving
an excited neuron reducing the activity of its neighbors’ activities, is integral in the biological
framework for cognitive inhibition (Davidson, Dima, Loren, et al., 2006). Inhibitory
neurotransmitters such as GABA, Serotonin and dopamine, have the ability to block
transmissions between neurons, ultimately resulting in cognitive inhibition (Peter et al., 2004).
Also, inhibitory connections are also present in the CNS. Cognitive inhibition is responsible for
determining relevant information with regard to working memory and shutting out the irrelevant,
thus freeing up the mental capacity for more pressing matters (Davidson et al., 2006; Peter et al.,
2004). Conversely, inefficient inhibition may also occur where cognitive inhibition is not fully
functional and a shortage of mental resources results to inefficiency in certain tasks. For
instance, inefficient inhibition can occur in mild cognitive impairment (Peter et al., 2004).
Colin MacLeod (2007) suggested that the cognitive and neural inhibition are two
distinctly separate realms, however, in spite of this, there are distinct links between the neural
levels of inhibition, those that are identified through the use of reaction time speed, and its
variabilities and the associated cognitive inhibitions, which serve to affect, or, are linked to the
anxiety level of the individual. The aim of this study includes to determine whether the levels of
anxiety are correlated to RT, as well as to determine the relationship between anxiety and sleep
and RT. A detailed discussion on reaction time, reaction time variability, and processing speed
will be done in a subsequent chapter.
24
Cognitive inhibition describes ability of the mind to tune out irrelevant stimuli regarding
tasks or processes at hand. It can be done partially, wholly, intentionally or otherwise (Peter,
Hertwig & Hoffrage, 2004). Cognitive inhibition may be an extension of neural inhibition, the
ability of individual neurons to regulate or stop elements of thought. Lateral inhibition, involving
an excited neuron reducing the activity of its neighbors’ activities, is integral in the biological
framework for cognitive inhibition (Davidson, Dima, Loren, et al., 2006). Inhibitory
neurotransmitters such as GABA, Serotonin and dopamine, have the ability to block
transmissions between neurons, ultimately resulting in cognitive inhibition (Peter et al., 2004).
Also, inhibitory connections are also present in the CNS. Cognitive inhibition is responsible for
determining relevant information with regard to working memory and shutting out the irrelevant,
thus freeing up the mental capacity for more pressing matters (Davidson et al., 2006; Peter et al.,
2004). Conversely, inefficient inhibition may also occur where cognitive inhibition is not fully
functional and a shortage of mental resources results to inefficiency in certain tasks. For
instance, inefficient inhibition can occur in mild cognitive impairment (Peter et al., 2004).
Colin MacLeod (2007) suggested that the cognitive and neural inhibition are two
distinctly separate realms, however, in spite of this, there are distinct links between the neural
levels of inhibition, those that are identified through the use of reaction time speed, and its
variabilities and the associated cognitive inhibitions, which serve to affect, or, are linked to the
anxiety level of the individual. The aim of this study includes to determine whether the levels of
anxiety are correlated to RT, as well as to determine the relationship between anxiety and sleep
and RT. A detailed discussion on reaction time, reaction time variability, and processing speed
will be done in a subsequent chapter.
24
Attention
Attention is the ability to concentrate on specific stimuli. Immediate memory or simple
auditory attention span shows a slight decline in late life as measured by repeating a string of
digits (Harada et al., 2013; Salthouse, 2009). Selective and divided attention which are more
complex tasks show a noticeable age effect (Harada et al., 2013; Salthouse, 2012; West & Alain,
2000). In selective attention, the individual has the ability to focus on specific information
within the environment while irrelevant information is ignored. This ability is important for
tasks such as carrying out conversation in car or in a noisy environment. Divided attention
involves the ability to focus simultaneously on multiple tasks such as holding conversations on a
phone while working on meal preparation Harada et al., 2013.
Older adults tend to perform worse compared to younger adults on tasks that involve working
memory or the ability to hold information momentarily in memory while at the same time
manipulating that information (Singh-Manoux, Kivimaki, Glymour et al., 2009; West & Alain,
2000). For instance, older adults may find it difficult to order a string of letters in the proper
alphanumerical sequence or calculate a tip on a bill (Harada et al., 2013; Singh-Manoux et al.,
2009). A detailed discussion attention and visual attention and anxiety will be done in a
subsequent chapter.
Language
Memory and language are prominent domains in attempts to understand human cognition
(Burke & Mackay, 1997). Language is a cognitive domain that involves both crystallized and
fluid cognitive abilities. An individual’s overall language ability does not change with age.
Vocabulary for instance, not only remains stable, it improves with age (Harada et al., 2013;
25
Attention is the ability to concentrate on specific stimuli. Immediate memory or simple
auditory attention span shows a slight decline in late life as measured by repeating a string of
digits (Harada et al., 2013; Salthouse, 2009). Selective and divided attention which are more
complex tasks show a noticeable age effect (Harada et al., 2013; Salthouse, 2012; West & Alain,
2000). In selective attention, the individual has the ability to focus on specific information
within the environment while irrelevant information is ignored. This ability is important for
tasks such as carrying out conversation in car or in a noisy environment. Divided attention
involves the ability to focus simultaneously on multiple tasks such as holding conversations on a
phone while working on meal preparation Harada et al., 2013.
Older adults tend to perform worse compared to younger adults on tasks that involve working
memory or the ability to hold information momentarily in memory while at the same time
manipulating that information (Singh-Manoux, Kivimaki, Glymour et al., 2009; West & Alain,
2000). For instance, older adults may find it difficult to order a string of letters in the proper
alphanumerical sequence or calculate a tip on a bill (Harada et al., 2013; Singh-Manoux et al.,
2009). A detailed discussion attention and visual attention and anxiety will be done in a
subsequent chapter.
Language
Memory and language are prominent domains in attempts to understand human cognition
(Burke & Mackay, 1997). Language is a cognitive domain that involves both crystallized and
fluid cognitive abilities. An individual’s overall language ability does not change with age.
Vocabulary for instance, not only remains stable, it improves with age (Harada et al., 2013;
25
Hayden & Welsh-Bohmer, 2010). Input in language involves perception of speech sounds and
letters that make up words and comprehending the meaning of sentences and words. Input
processes are stable in ageing and are independent of sensory deficits or decline in the
individual’s ability to encode new information (Burke & Mackay, 1997). Other abilities such as
visual confrontation naming, involving the ability to see and name a common object, stays the
same until 70 years of age and subsequently declines in subsequent years (Salthouse, 2009; Zec,
Markwell, Burkett, et al., 2005). Language production however, is affected by ageing and
aspects of written and spoken language may show age –related effects. Older adults may find it
difficult to produce words they know (Burke & Mackay, 1997). Verbal fluency, the ability to
carry out a word search and generate specific words within a certain amount of time, declines
with age as well (Harada et al., 2013; West & Alain, 2000).
Visuospatial Abilities/Construction
Visuospatial and visual construction abilities are a group of cognitive functions that
involve the ability to understand space two- and three-dimensional space (Harada et al., 2013;
West & Alain, 2000). Visual construction involves the ability to connect individual parts and
produce a coherent whole such as assembling furniture from separate parts. This ability declines
with time. Visuospatial abilities involves the ability to perceive objects, recognize familiar
objects such as faces, and the ability to appreciate an object’s location in relation to others or
alone. This ability on the other hand, remains intact (Harada and et al., 2013; West and Alain,
2000). Visual attention is that cognitive function that is being affected by ageing. The person
loses its ability to see clearly though as the person starts ageing. However, it may be corrected by
26
letters that make up words and comprehending the meaning of sentences and words. Input
processes are stable in ageing and are independent of sensory deficits or decline in the
individual’s ability to encode new information (Burke & Mackay, 1997). Other abilities such as
visual confrontation naming, involving the ability to see and name a common object, stays the
same until 70 years of age and subsequently declines in subsequent years (Salthouse, 2009; Zec,
Markwell, Burkett, et al., 2005). Language production however, is affected by ageing and
aspects of written and spoken language may show age –related effects. Older adults may find it
difficult to produce words they know (Burke & Mackay, 1997). Verbal fluency, the ability to
carry out a word search and generate specific words within a certain amount of time, declines
with age as well (Harada et al., 2013; West & Alain, 2000).
Visuospatial Abilities/Construction
Visuospatial and visual construction abilities are a group of cognitive functions that
involve the ability to understand space two- and three-dimensional space (Harada et al., 2013;
West & Alain, 2000). Visual construction involves the ability to connect individual parts and
produce a coherent whole such as assembling furniture from separate parts. This ability declines
with time. Visuospatial abilities involves the ability to perceive objects, recognize familiar
objects such as faces, and the ability to appreciate an object’s location in relation to others or
alone. This ability on the other hand, remains intact (Harada and et al., 2013; West and Alain,
2000). Visual attention is that cognitive function that is being affected by ageing. The person
loses its ability to see clearly though as the person starts ageing. However, it may be corrected by
26
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
using various methods. Such as the person can use spectacles of the particular number, means
how much correction in the eyesight is required.
Executive Functioning
Executive functions are considered as a set of cognitive methods that has an essential role
in the cognitive control. Also, they are responsible for selecting and then manageing the
behaviors which makes it easy to achieve the targets and goals (West & Alain, 2000). The
executive functioning involves various cognitive process such as inhibitory control, cognitive
flexibility etc. Although there are various cognitive processes that gets affected by ageing but not
all executive functions are sensitive to age. There are some executive functions that do not get
affected at all by the age factor. The process is also known as the focus switching. There are
some age related deficits that are responsible for maintaining the specific representations outside
the attention or its whole focus (Salthouse, 2010; Oosterman, Vogels van Harten, et al., 2010).
Executive abilities that require speed motor components are especially susceptible and
affected by the increasing age (Oosterman et al. 2010; Hayden & Welsh-Bohmer, 2012). For
instance, ageing affects the response inhibition negatively. Response inhibition is the ability to
control an automatic response and to produce a novel response instead. Inductive reasoning and
reasoning using unfamiliar material also reduces with age (Wecker et al., 2000). Some executive
functions, however, remain stable throughout the life span such as the ability to describe the
meanings of proverbs, appreciate similarities, reason about familiar materials (Harada et al.,
2013).
27
how much correction in the eyesight is required.
Executive Functioning
Executive functions are considered as a set of cognitive methods that has an essential role
in the cognitive control. Also, they are responsible for selecting and then manageing the
behaviors which makes it easy to achieve the targets and goals (West & Alain, 2000). The
executive functioning involves various cognitive process such as inhibitory control, cognitive
flexibility etc. Although there are various cognitive processes that gets affected by ageing but not
all executive functions are sensitive to age. There are some executive functions that do not get
affected at all by the age factor. The process is also known as the focus switching. There are
some age related deficits that are responsible for maintaining the specific representations outside
the attention or its whole focus (Salthouse, 2010; Oosterman, Vogels van Harten, et al., 2010).
Executive abilities that require speed motor components are especially susceptible and
affected by the increasing age (Oosterman et al. 2010; Hayden & Welsh-Bohmer, 2012). For
instance, ageing affects the response inhibition negatively. Response inhibition is the ability to
control an automatic response and to produce a novel response instead. Inductive reasoning and
reasoning using unfamiliar material also reduces with age (Wecker et al., 2000). Some executive
functions, however, remain stable throughout the life span such as the ability to describe the
meanings of proverbs, appreciate similarities, reason about familiar materials (Harada et al.,
2013).
27
Sleep Quality
With respect to the sleep quality, sleep patterns tends to change with ageing. Ageing
starts impacting the sleep quality which further impacts the cognitive performance as well as the
memory. As the person starts ageing, it affects the quality of their sleep as the person goes
through sleep deprivation. The people in their older ages find it hard to sleep comfortably. They
do not be able to sleep properly and the sleep deprivation often results in making the skin to age
faster as well (Minaker, 2011).
Emotional processing
As the person starts ageing, they start getting bound by various limitations as their life
goes under a lot of changes. It is obvious that ageing makes the person weak to a smaller level. It
is because their social life decreases and various factors like this becomes limited. So, the people
after ageing often feel lonely and hopeless. There can be various reasons as well for staying
lonely and hopeless such as most of the people are suffering from some sort of diseases.
1.2.2 Structural/Functional Brain Changes in Normal Ageing
Ageing affects the whole body, so does the brain as well. It has an impact on the cells,
molecules, cognition etc. As the person ages, the volume of the brain starts to shrink. Mostly, the
change is being observed in the frontal cortex. As the vasculature of the person ages, the blood
pressure of a person starts increasing the possibility of various issues such as the person may get
stoke or the level of ischemia maximizes. The whole structure of the brain changes initially from
the birth. Although it is being affected by various other factors in between such as dementia,
stress or any mental pressures etc., the changes in the brain is a normal process and starts from
28
With respect to the sleep quality, sleep patterns tends to change with ageing. Ageing
starts impacting the sleep quality which further impacts the cognitive performance as well as the
memory. As the person starts ageing, it affects the quality of their sleep as the person goes
through sleep deprivation. The people in their older ages find it hard to sleep comfortably. They
do not be able to sleep properly and the sleep deprivation often results in making the skin to age
faster as well (Minaker, 2011).
Emotional processing
As the person starts ageing, they start getting bound by various limitations as their life
goes under a lot of changes. It is obvious that ageing makes the person weak to a smaller level. It
is because their social life decreases and various factors like this becomes limited. So, the people
after ageing often feel lonely and hopeless. There can be various reasons as well for staying
lonely and hopeless such as most of the people are suffering from some sort of diseases.
1.2.2 Structural/Functional Brain Changes in Normal Ageing
Ageing affects the whole body, so does the brain as well. It has an impact on the cells,
molecules, cognition etc. As the person ages, the volume of the brain starts to shrink. Mostly, the
change is being observed in the frontal cortex. As the vasculature of the person ages, the blood
pressure of a person starts increasing the possibility of various issues such as the person may get
stoke or the level of ischemia maximizes. The whole structure of the brain changes initially from
the birth. Although it is being affected by various other factors in between such as dementia,
stress or any mental pressures etc., the changes in the brain is a normal process and starts from
28
the birth only. It is important to understand the brain structure and function as well as normative
brain development as the foundation for both normative and pathological cognitive processes.
The brain is made up of gray matter consisting of cell bodies and synaptic connections, and
white matter consisting of axons that have a characteristic white color due to myelin sheaths
(Braun, 2011). Gray matter functions in the low-level processing of sensory and motor
information (Braun, 2011; Heitman, 2003). The cerebral cortex has four lobes – frontal, parietal,
occipital, and temporal. The frontal lobe controls several functions including emotions,
personality, morality, language, judgment, intellect, planning, abstract thought, olfaction, short-
term memory, attention, voluntary movement, perseverance, and impulse control (Heitman,
2003). The parietal lobe affects the experience of pain, sensory functions, motor functions,
perception, spatial relationships, proprioception, abstract reasoning, body image, and the ability
to read. The temporal lobe is affects hearing, receptive language, emotional memories, general
awareness, sound discrimination, smell, ability to understand speech, as well as is involved in
memory processing (Braun, 2011; Heitman, 2003). The occipital lobe coordinates visual stimuli
in conjunction with other areas of the brain (Heitman, 2003). In general, brain cells undergo
atrophy at a rate of -0.23% annually across the lifespan, [compared to individuals who have a
diagnoses of dementia and experience at least twice the normative atrophy rate for the brain ]
(Braun, 2011; Marcus, Fotenos, Csernansky, et al., 2010). This would indicate that there would
be a higher rate of decline in cognitive functions where there are detrimental effects from anxiety
on the brain, as is being investigated in this study.
The emotional-processing brain structure is the limbic system and includes the insular
cortex and cingulate cortex. The hippocampus is also a limbic system structure that has
inhibitory control over the stress-response system and contributes to negative feedback for the
29
brain development as the foundation for both normative and pathological cognitive processes.
The brain is made up of gray matter consisting of cell bodies and synaptic connections, and
white matter consisting of axons that have a characteristic white color due to myelin sheaths
(Braun, 2011). Gray matter functions in the low-level processing of sensory and motor
information (Braun, 2011; Heitman, 2003). The cerebral cortex has four lobes – frontal, parietal,
occipital, and temporal. The frontal lobe controls several functions including emotions,
personality, morality, language, judgment, intellect, planning, abstract thought, olfaction, short-
term memory, attention, voluntary movement, perseverance, and impulse control (Heitman,
2003). The parietal lobe affects the experience of pain, sensory functions, motor functions,
perception, spatial relationships, proprioception, abstract reasoning, body image, and the ability
to read. The temporal lobe is affects hearing, receptive language, emotional memories, general
awareness, sound discrimination, smell, ability to understand speech, as well as is involved in
memory processing (Braun, 2011; Heitman, 2003). The occipital lobe coordinates visual stimuli
in conjunction with other areas of the brain (Heitman, 2003). In general, brain cells undergo
atrophy at a rate of -0.23% annually across the lifespan, [compared to individuals who have a
diagnoses of dementia and experience at least twice the normative atrophy rate for the brain ]
(Braun, 2011; Marcus, Fotenos, Csernansky, et al., 2010). This would indicate that there would
be a higher rate of decline in cognitive functions where there are detrimental effects from anxiety
on the brain, as is being investigated in this study.
The emotional-processing brain structure is the limbic system and includes the insular
cortex and cingulate cortex. The hippocampus is also a limbic system structure that has
inhibitory control over the stress-response system and contributes to negative feedback for the
29
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
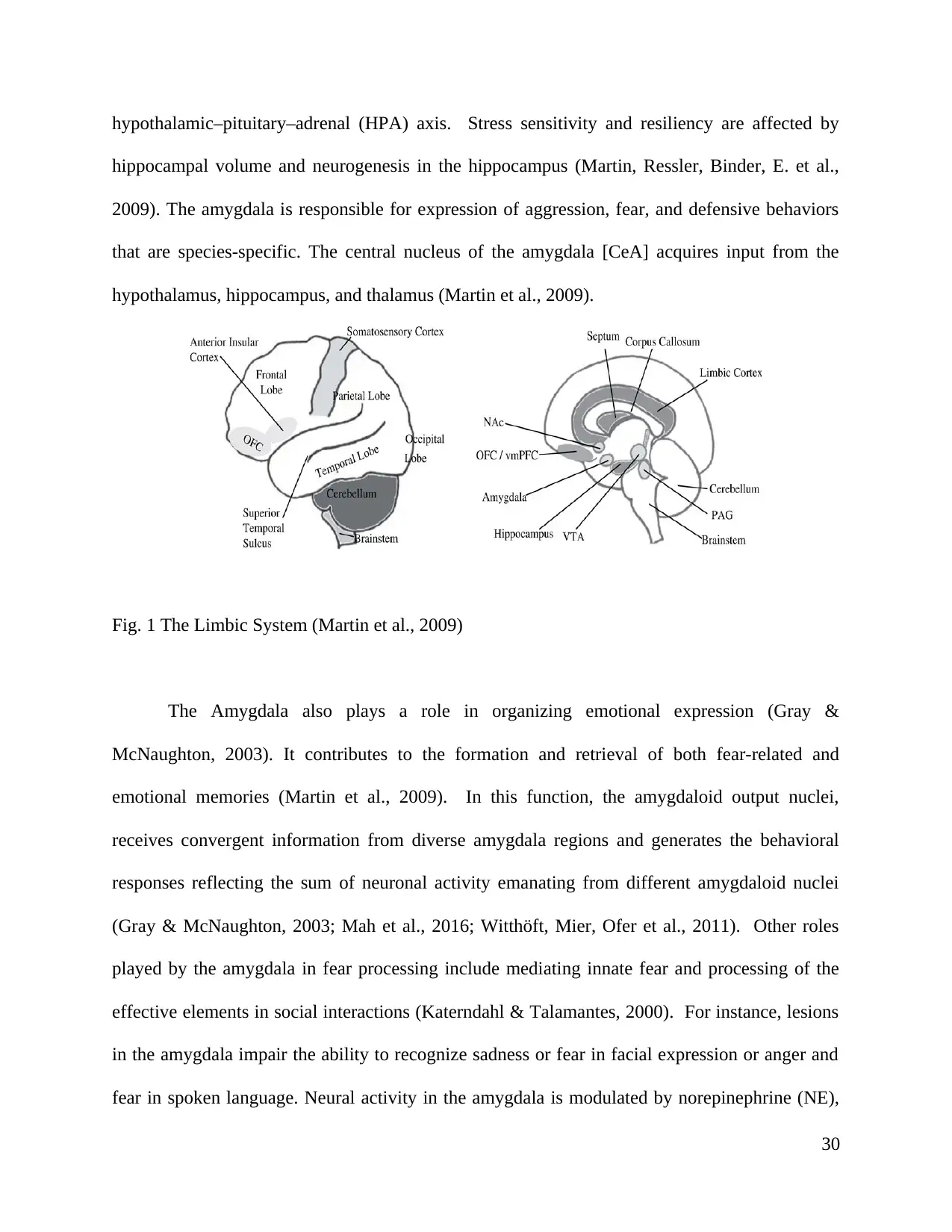
hypothalamic–pituitary–adrenal (HPA) axis. Stress sensitivity and resiliency are affected by
hippocampal volume and neurogenesis in the hippocampus (Martin, Ressler, Binder, E. et al.,
2009). The amygdala is responsible for expression of aggression, fear, and defensive behaviors
that are species-specific. The central nucleus of the amygdala [CeA] acquires input from the
hypothalamus, hippocampus, and thalamus (Martin et al., 2009).
Fig. 1 The Limbic System (Martin et al., 2009)
The Amygdala also plays a role in organizing emotional expression (Gray &
McNaughton, 2003). It contributes to the formation and retrieval of both fear-related and
emotional memories (Martin et al., 2009). In this function, the amygdaloid output nuclei,
receives convergent information from diverse amygdala regions and generates the behavioral
responses reflecting the sum of neuronal activity emanating from different amygdaloid nuclei
(Gray & McNaughton, 2003; Mah et al., 2016; Witthöft, Mier, Ofer et al., 2011). Other roles
played by the amygdala in fear processing include mediating innate fear and processing of the
effective elements in social interactions (Katerndahl & Talamantes, 2000). For instance, lesions
in the amygdala impair the ability to recognize sadness or fear in facial expression or anger and
fear in spoken language. Neural activity in the amygdala is modulated by norepinephrine (NE),
30
hippocampal volume and neurogenesis in the hippocampus (Martin, Ressler, Binder, E. et al.,
2009). The amygdala is responsible for expression of aggression, fear, and defensive behaviors
that are species-specific. The central nucleus of the amygdala [CeA] acquires input from the
hypothalamus, hippocampus, and thalamus (Martin et al., 2009).
Fig. 1 The Limbic System (Martin et al., 2009)
The Amygdala also plays a role in organizing emotional expression (Gray &
McNaughton, 2003). It contributes to the formation and retrieval of both fear-related and
emotional memories (Martin et al., 2009). In this function, the amygdaloid output nuclei,
receives convergent information from diverse amygdala regions and generates the behavioral
responses reflecting the sum of neuronal activity emanating from different amygdaloid nuclei
(Gray & McNaughton, 2003; Mah et al., 2016; Witthöft, Mier, Ofer et al., 2011). Other roles
played by the amygdala in fear processing include mediating innate fear and processing of the
effective elements in social interactions (Katerndahl & Talamantes, 2000). For instance, lesions
in the amygdala impair the ability to recognize sadness or fear in facial expression or anger and
fear in spoken language. Neural activity in the amygdala is modulated by norepinephrine (NE),
30
cortisol, and other neurotransmitters (Mah et al., 2016), as well as by mnemonic input based on
previous conditioning and reinforcement experiences. Such previous experiences are projected
from the mesiotemporal and prefrontal cortical structures (Charney & Drevets, 2002; Gray &
McNaughton, 2003; Phelps & LeDoux, 2005; Witthöft, Mier, Ofer et al., 2011).
Grey Matter Volume Decline
Grey matter is considered as one of the major and essential components of the central
nervous system (CNS). It includes the composition of neuronal cell bodies, dendrites, glial cells
and the capillaries. These are also considered as the neural tissues which are considered as an
important part of the spinal cord and the brain. Ageing causes various changes to the brain, so as
to the Grey matter as well. The brain is said to get shrink when a person starts ageing. The
effects of ageing on the brain as well as on cognition are being observed to a huge extent. The
volume of Grey matter in the brain begins to decrease after the age of 20 (Harada et al., 2013).
This atrophy occurs most prominently at the prefrontal cortex. Moderate age-related change
occurs in the temporal lobes, involving reduction in the hippocampal volume (Harada et al.,
2013; Rodrigue, Kennedy & Park, 2009). Several factors may be responsible for decline in the
grey matter such as the death of brain cells or neurons themselves, the contribution of beta-
amyloid to grey matter volume, and decrease in neuronal size and synaptic density (Harada et al.,
2013).
Beta-amyloid is a protein that has been found to accumulate in the brains of individuals
with Alzheimer’s dementia (AD). This protein is proposed to cause AD through neuronal death
(Harada et al., 2013). In patients with cognitive impairments, the elevated presence this protein is
a predictor for conversion to AD (Harada et al., 2013). Associations have also been found
31
previous conditioning and reinforcement experiences. Such previous experiences are projected
from the mesiotemporal and prefrontal cortical structures (Charney & Drevets, 2002; Gray &
McNaughton, 2003; Phelps & LeDoux, 2005; Witthöft, Mier, Ofer et al., 2011).
Grey Matter Volume Decline
Grey matter is considered as one of the major and essential components of the central
nervous system (CNS). It includes the composition of neuronal cell bodies, dendrites, glial cells
and the capillaries. These are also considered as the neural tissues which are considered as an
important part of the spinal cord and the brain. Ageing causes various changes to the brain, so as
to the Grey matter as well. The brain is said to get shrink when a person starts ageing. The
effects of ageing on the brain as well as on cognition are being observed to a huge extent. The
volume of Grey matter in the brain begins to decrease after the age of 20 (Harada et al., 2013).
This atrophy occurs most prominently at the prefrontal cortex. Moderate age-related change
occurs in the temporal lobes, involving reduction in the hippocampal volume (Harada et al.,
2013; Rodrigue, Kennedy & Park, 2009). Several factors may be responsible for decline in the
grey matter such as the death of brain cells or neurons themselves, the contribution of beta-
amyloid to grey matter volume, and decrease in neuronal size and synaptic density (Harada et al.,
2013).
Beta-amyloid is a protein that has been found to accumulate in the brains of individuals
with Alzheimer’s dementia (AD). This protein is proposed to cause AD through neuronal death
(Harada et al., 2013). In patients with cognitive impairments, the elevated presence this protein is
a predictor for conversion to AD (Harada et al., 2013). Associations have also been found
31
between high levels of beta-amyloid and decreased episodic memory, as well as between high
levels of beta-amyloid and hippocampal volumes in cognitively normal individuals (Dickstein et
al., 2007; Rodrigue et al., 2009). Beta-amyloid is also found in the cortex of 20–30% of
cognitively normal adults, a factor that is postulated to be a predictor for eventual development
of AD (Harada et al., 2013; Rodrigue et al., 2009).
Decrease in neuronal size and synaptic density may also explain grey matter decline
(Dickstein, Kabaso, Rocher et al., 2007; Harada et al., 2013). Reduction in synaptic density
among older adults is well documented (Harada et al., 2013). Reduction in synaptic density may
be caused by the morphologic changes in the neuron that occur with ageing (Dickstein et al.,
2007). Such morphologic changes include decrease in dendrite lengths, decrease in dendrite
arborization complexity, as well as decreased neuritic spines which are the main sites for
excitatory synapses (Dickstein et al., 2007; Harada et al., 2013).
Older adults have been shown from studies using functional MRI (fMRI) to have reduced
capacities for metalizing or the ability to infer other person’s mental state (Harada et al., 2013)
This decline is associated with reduction in BOLD response, a marker for metabolic activity
located in the dorsomedial prefrontal cortex. This raises the possibility that the dorsomedial
prefrontal cortex area of the brain may be important for mentalizing and that it may also become
less active with ageing (Harada et al., 2013).
32
levels of beta-amyloid and hippocampal volumes in cognitively normal individuals (Dickstein et
al., 2007; Rodrigue et al., 2009). Beta-amyloid is also found in the cortex of 20–30% of
cognitively normal adults, a factor that is postulated to be a predictor for eventual development
of AD (Harada et al., 2013; Rodrigue et al., 2009).
Decrease in neuronal size and synaptic density may also explain grey matter decline
(Dickstein, Kabaso, Rocher et al., 2007; Harada et al., 2013). Reduction in synaptic density
among older adults is well documented (Harada et al., 2013). Reduction in synaptic density may
be caused by the morphologic changes in the neuron that occur with ageing (Dickstein et al.,
2007). Such morphologic changes include decrease in dendrite lengths, decrease in dendrite
arborization complexity, as well as decreased neuritic spines which are the main sites for
excitatory synapses (Dickstein et al., 2007; Harada et al., 2013).
Older adults have been shown from studies using functional MRI (fMRI) to have reduced
capacities for metalizing or the ability to infer other person’s mental state (Harada et al., 2013)
This decline is associated with reduction in BOLD response, a marker for metabolic activity
located in the dorsomedial prefrontal cortex. This raises the possibility that the dorsomedial
prefrontal cortex area of the brain may be important for mentalizing and that it may also become
less active with ageing (Harada et al., 2013).
32
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

Fig. 2 Key Brain Structures in the Neurocuitry of Emotion (Mah et al. 2016)
Changes in White Matter
White matter is considered as the matter that is made up of the composition of various
bundles. It makes a sort of connection between various different areas of the gray matter.
Along with this, it also carries the nerve impulses within the neurons. When there have been
observed some changes in the white matter, it can cause various complex and complicated
situations. It has been observed that the changes in the white matter takes place faster as
compared to the adults. An important factor which is to be considered here is that the dormant
oligodendrocytes have the potential to get activated at the time when some one is suffering from
any demyelinating disease. Also, the whole mechanism of the white matter requires repeated
activation. There occur some changes as well in the white matter but only in the case in which
the memory has involved various sort of connections within the parietal as well as lateral frontal
areas. Various symptoms of this can be classified as the person feeling weakness or the person
may also feel numb. Grey matter diseases also cause various diseases such as the person can
suffer from memory loss as in case of people with dementia, the person feels quite hard to recall
the previous details. Along with it, the person forgets even the basic operations such as where the
33
Changes in White Matter
White matter is considered as the matter that is made up of the composition of various
bundles. It makes a sort of connection between various different areas of the gray matter.
Along with this, it also carries the nerve impulses within the neurons. When there have been
observed some changes in the white matter, it can cause various complex and complicated
situations. It has been observed that the changes in the white matter takes place faster as
compared to the adults. An important factor which is to be considered here is that the dormant
oligodendrocytes have the potential to get activated at the time when some one is suffering from
any demyelinating disease. Also, the whole mechanism of the white matter requires repeated
activation. There occur some changes as well in the white matter but only in the case in which
the memory has involved various sort of connections within the parietal as well as lateral frontal
areas. Various symptoms of this can be classified as the person feeling weakness or the person
may also feel numb. Grey matter diseases also cause various diseases such as the person can
suffer from memory loss as in case of people with dementia, the person feels quite hard to recall
the previous details. Along with it, the person forgets even the basic operations such as where the
33
keys of the vehicle or home is placed etc. Reduction in the volume of White matter with ageing
is greater than that of grey matter (Harada et al., 2013; Rogalski, Stebbins, Barnes et al., 2012).
Studies have found a reduction of between 16 and 20% in white matter volume in individuals
over age 70 compared to younger subjects (Harada et al., 2013). The decline was noted in the
corpus callosum, precentral gyrus and gyrus rectus. In the grey matter, these areas constitute less
than 6% of the areas of decline (Harada et al., 2013). With regard to white matter function,
white matter integrity has also been found to decline with increasing age (O’Sullivan, Summers,
Jones et al. 2001). Such age-related declines are most vivid in the anterior white matter and the
declines are associated with deficits in the individual’s executive function and reaction time as
discussed previously (Harada and et al., 2013)
1.2.3 Subjective and Objective cognitive impairment and Dementia
Dementia refers to a clinical syndrome (a cluster of co-occurring signs and symptoms)
involving progressive deterioration in intellectual function (Davis, 2015; Korolev, 2014).
Dementia is a broad term used to describe conditions involving loss of reasoning, memory, and
loss of mental abilities or cognitive functions such as judgment, behavior, language, and
thinking. Such cognitive decline impacts negatively on the ability of the affected person to
successfully or independently carry out activities of daily living (Davis, 2015). Dementia is most
common among elderly adults and is often termed senility (Korolev, 2014).
Alzheimer’s Disease (AD) is a type of dementia, as well as the most common cause of
irreversible dementia; in the United States, this condition accounts for an estimated 70% of all
dementia cases (Thies and Bleiler, 2013; Korolev, 2014). It is estimated that about 35 million
people worldwide have AD or some types of dementia, while another 65 million people are
34
is greater than that of grey matter (Harada et al., 2013; Rogalski, Stebbins, Barnes et al., 2012).
Studies have found a reduction of between 16 and 20% in white matter volume in individuals
over age 70 compared to younger subjects (Harada et al., 2013). The decline was noted in the
corpus callosum, precentral gyrus and gyrus rectus. In the grey matter, these areas constitute less
than 6% of the areas of decline (Harada et al., 2013). With regard to white matter function,
white matter integrity has also been found to decline with increasing age (O’Sullivan, Summers,
Jones et al. 2001). Such age-related declines are most vivid in the anterior white matter and the
declines are associated with deficits in the individual’s executive function and reaction time as
discussed previously (Harada and et al., 2013)
1.2.3 Subjective and Objective cognitive impairment and Dementia
Dementia refers to a clinical syndrome (a cluster of co-occurring signs and symptoms)
involving progressive deterioration in intellectual function (Davis, 2015; Korolev, 2014).
Dementia is a broad term used to describe conditions involving loss of reasoning, memory, and
loss of mental abilities or cognitive functions such as judgment, behavior, language, and
thinking. Such cognitive decline impacts negatively on the ability of the affected person to
successfully or independently carry out activities of daily living (Davis, 2015). Dementia is most
common among elderly adults and is often termed senility (Korolev, 2014).
Alzheimer’s Disease (AD) is a type of dementia, as well as the most common cause of
irreversible dementia; in the United States, this condition accounts for an estimated 70% of all
dementia cases (Thies and Bleiler, 2013; Korolev, 2014). It is estimated that about 35 million
people worldwide have AD or some types of dementia, while another 65 million people are
34
expected to develop dementia by 2030 . AD is described as a multi factorial disease. While there
is no single known cause for the disease, there are several modifiable and non-modifiable risk
factors associated with its onset and progression.
Dementia is not a part of the normal ageing process but rather has underlying medical
conditions in both younger and older adults. Dementia is different from age-related memory loss
or benign senescent forgetfulness. Normal ageing and slowing of mental processes with age
does not impair the individual’s ability to solve problems, learn new things, or carry out daily
activities of living as occurs in dementia (Bouhuys et al., 1997; Yates, 2015). Dementia
symptoms depend on both the underlying cause and on the individual. Most affected people have
some symptoms (Braun, 2011; Davis, 2015).
The first sign of dementia is usually the loss of short-term memory. The affected person
may forget what he or she had just said. In early dementia, the affected individual has difficulty
with finding words and names. Appointments may be forgotten, and there is difficulty with tasks
daily tasks such as cooking, driving, or managing finances. Other symptoms of dementia include
poor judgment, confusion, paranoia, mood swings, and other uncharacteristic behavior (Braun,
2011; Davis, 2015). There are some stages of dementia such as MCI and SCI which are
considered as the initial stages of dementia. In the mild cognitive impairment (MCI), the
problems start becoming visible in the third stage, in which one can guess through a variety of
symptoms such as getting lost from the outside world, which means not understanding and
feeling what is going around, observing poor performance at work or in academic level etc. Also,
the person feels difficult to concentrate. SCI stands for subjective cognitive impairment is that
phase when the person goes through various issues that are related to memory and
35
is no single known cause for the disease, there are several modifiable and non-modifiable risk
factors associated with its onset and progression.
Dementia is not a part of the normal ageing process but rather has underlying medical
conditions in both younger and older adults. Dementia is different from age-related memory loss
or benign senescent forgetfulness. Normal ageing and slowing of mental processes with age
does not impair the individual’s ability to solve problems, learn new things, or carry out daily
activities of living as occurs in dementia (Bouhuys et al., 1997; Yates, 2015). Dementia
symptoms depend on both the underlying cause and on the individual. Most affected people have
some symptoms (Braun, 2011; Davis, 2015).
The first sign of dementia is usually the loss of short-term memory. The affected person
may forget what he or she had just said. In early dementia, the affected individual has difficulty
with finding words and names. Appointments may be forgotten, and there is difficulty with tasks
daily tasks such as cooking, driving, or managing finances. Other symptoms of dementia include
poor judgment, confusion, paranoia, mood swings, and other uncharacteristic behavior (Braun,
2011; Davis, 2015). There are some stages of dementia such as MCI and SCI which are
considered as the initial stages of dementia. In the mild cognitive impairment (MCI), the
problems start becoming visible in the third stage, in which one can guess through a variety of
symptoms such as getting lost from the outside world, which means not understanding and
feeling what is going around, observing poor performance at work or in academic level etc. Also,
the person feels difficult to concentrate. SCI stands for subjective cognitive impairment is that
phase when the person goes through various issues that are related to memory and
35
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
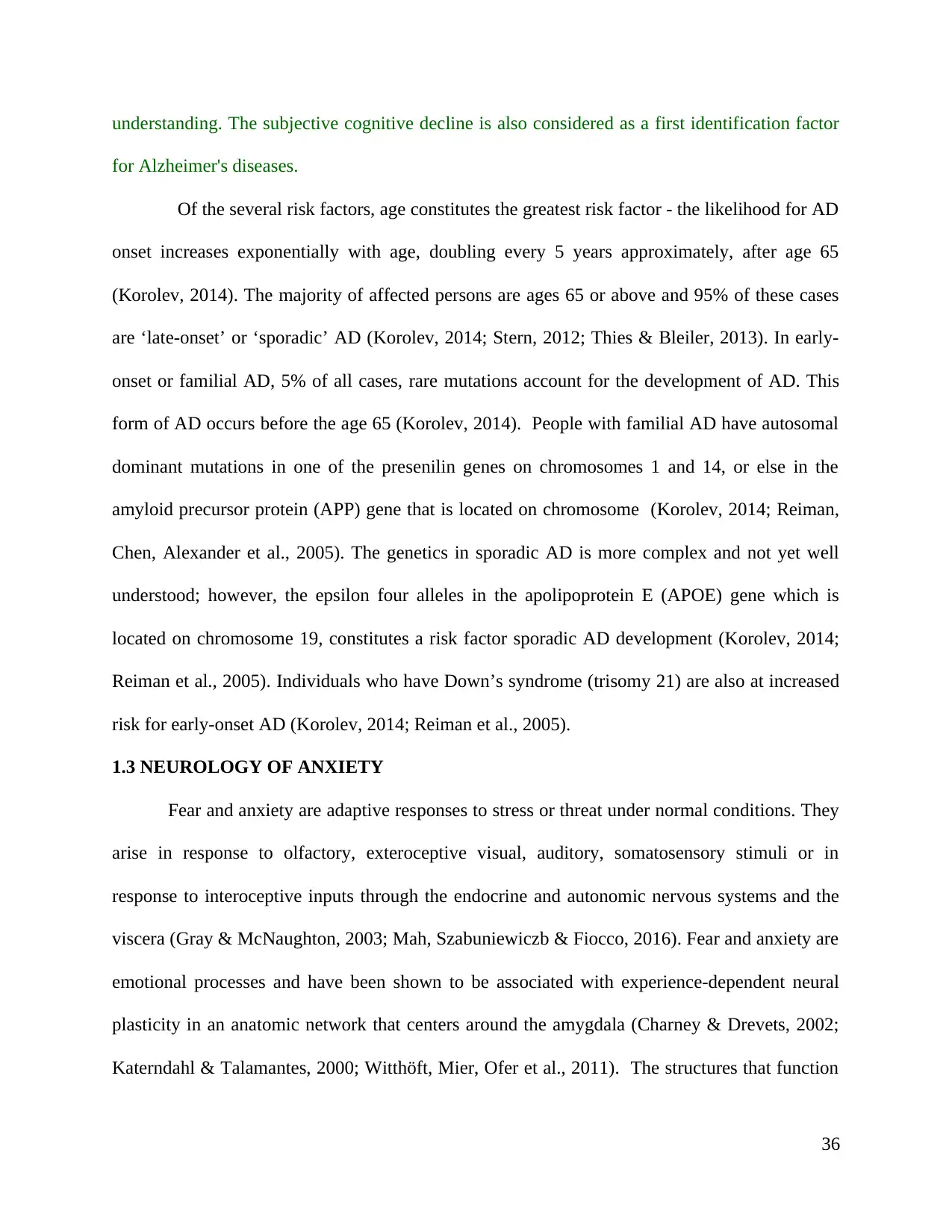
understanding. The subjective cognitive decline is also considered as a first identification factor
for Alzheimer's diseases.
Of the several risk factors, age constitutes the greatest risk factor - the likelihood for AD
onset increases exponentially with age, doubling every 5 years approximately, after age 65
(Korolev, 2014). The majority of affected persons are ages 65 or above and 95% of these cases
are ‘late-onset’ or ‘sporadic’ AD (Korolev, 2014; Stern, 2012; Thies & Bleiler, 2013). In early-
onset or familial AD, 5% of all cases, rare mutations account for the development of AD. This
form of AD occurs before the age 65 (Korolev, 2014). People with familial AD have autosomal
dominant mutations in one of the presenilin genes on chromosomes 1 and 14, or else in the
amyloid precursor protein (APP) gene that is located on chromosome (Korolev, 2014; Reiman,
Chen, Alexander et al., 2005). The genetics in sporadic AD is more complex and not yet well
understood; however, the epsilon four alleles in the apolipoprotein E (APOE) gene which is
located on chromosome 19, constitutes a risk factor sporadic AD development (Korolev, 2014;
Reiman et al., 2005). Individuals who have Down’s syndrome (trisomy 21) are also at increased
risk for early-onset AD (Korolev, 2014; Reiman et al., 2005).
1.3 NEUROLOGY OF ANXIETY
Fear and anxiety are adaptive responses to stress or threat under normal conditions. They
arise in response to olfactory, exteroceptive visual, auditory, somatosensory stimuli or in
response to interoceptive inputs through the endocrine and autonomic nervous systems and the
viscera (Gray & McNaughton, 2003; Mah, Szabuniewiczb & Fiocco, 2016). Fear and anxiety are
emotional processes and have been shown to be associated with experience-dependent neural
plasticity in an anatomic network that centers around the amygdala (Charney & Drevets, 2002;
Katerndahl & Talamantes, 2000; Witthöft, Mier, Ofer et al., 2011). The structures that function
36
for Alzheimer's diseases.
Of the several risk factors, age constitutes the greatest risk factor - the likelihood for AD
onset increases exponentially with age, doubling every 5 years approximately, after age 65
(Korolev, 2014). The majority of affected persons are ages 65 or above and 95% of these cases
are ‘late-onset’ or ‘sporadic’ AD (Korolev, 2014; Stern, 2012; Thies & Bleiler, 2013). In early-
onset or familial AD, 5% of all cases, rare mutations account for the development of AD. This
form of AD occurs before the age 65 (Korolev, 2014). People with familial AD have autosomal
dominant mutations in one of the presenilin genes on chromosomes 1 and 14, or else in the
amyloid precursor protein (APP) gene that is located on chromosome (Korolev, 2014; Reiman,
Chen, Alexander et al., 2005). The genetics in sporadic AD is more complex and not yet well
understood; however, the epsilon four alleles in the apolipoprotein E (APOE) gene which is
located on chromosome 19, constitutes a risk factor sporadic AD development (Korolev, 2014;
Reiman et al., 2005). Individuals who have Down’s syndrome (trisomy 21) are also at increased
risk for early-onset AD (Korolev, 2014; Reiman et al., 2005).
1.3 NEUROLOGY OF ANXIETY
Fear and anxiety are adaptive responses to stress or threat under normal conditions. They
arise in response to olfactory, exteroceptive visual, auditory, somatosensory stimuli or in
response to interoceptive inputs through the endocrine and autonomic nervous systems and the
viscera (Gray & McNaughton, 2003; Mah, Szabuniewiczb & Fiocco, 2016). Fear and anxiety are
emotional processes and have been shown to be associated with experience-dependent neural
plasticity in an anatomic network that centers around the amygdala (Charney & Drevets, 2002;
Katerndahl & Talamantes, 2000; Witthöft, Mier, Ofer et al., 2011). The structures that function
36
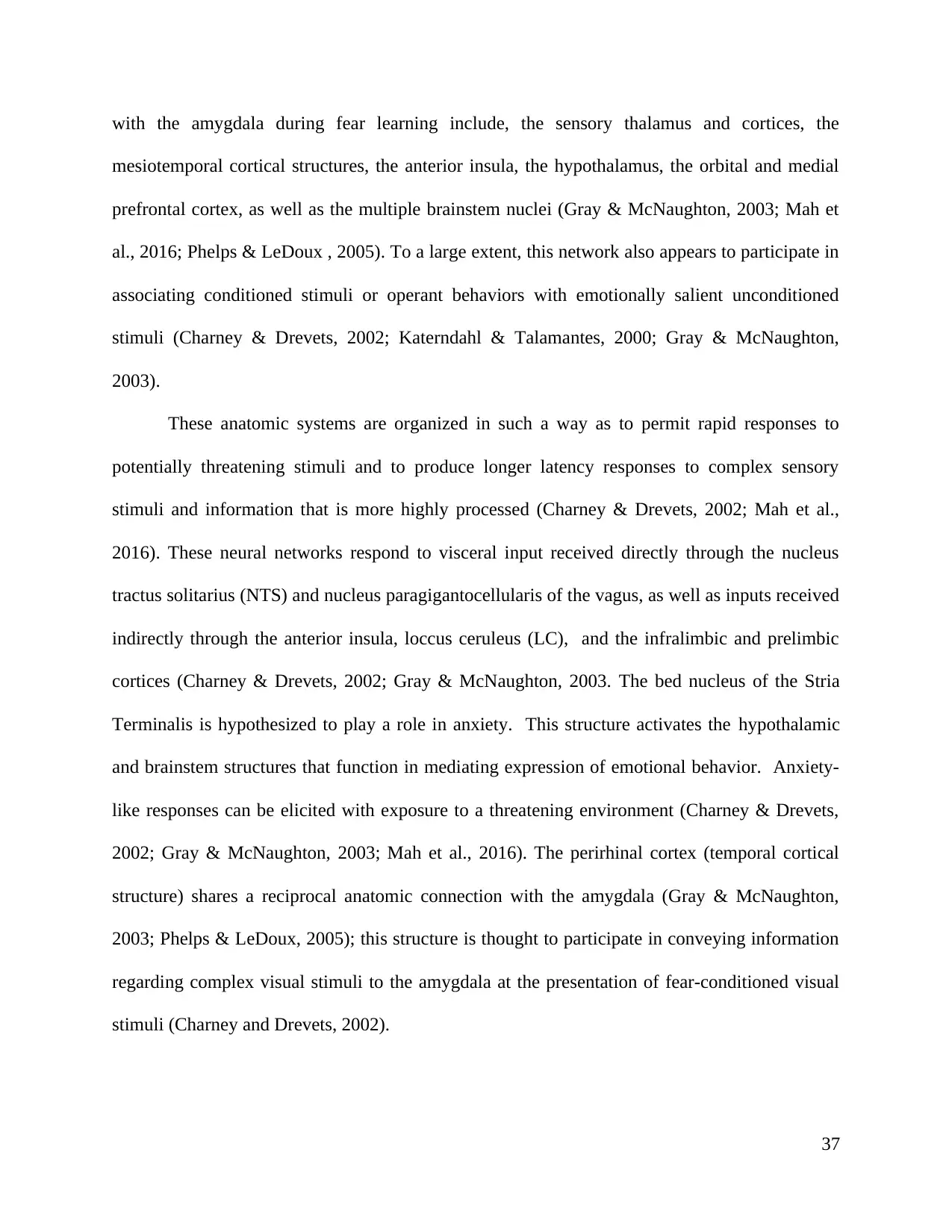
with the amygdala during fear learning include, the sensory thalamus and cortices, the
mesiotemporal cortical structures, the anterior insula, the hypothalamus, the orbital and medial
prefrontal cortex, as well as the multiple brainstem nuclei (Gray & McNaughton, 2003; Mah et
al., 2016; Phelps & LeDoux , 2005). To a large extent, this network also appears to participate in
associating conditioned stimuli or operant behaviors with emotionally salient unconditioned
stimuli (Charney & Drevets, 2002; Katerndahl & Talamantes, 2000; Gray & McNaughton,
2003).
These anatomic systems are organized in such a way as to permit rapid responses to
potentially threatening stimuli and to produce longer latency responses to complex sensory
stimuli and information that is more highly processed (Charney & Drevets, 2002; Mah et al.,
2016). These neural networks respond to visceral input received directly through the nucleus
tractus solitarius (NTS) and nucleus paragigantocellularis of the vagus, as well as inputs received
indirectly through the anterior insula, loccus ceruleus (LC), and the infralimbic and prelimbic
cortices (Charney & Drevets, 2002; Gray & McNaughton, 2003. The bed nucleus of the Stria
Terminalis is hypothesized to play a role in anxiety. This structure activates the hypothalamic
and brainstem structures that function in mediating expression of emotional behavior. Anxiety-
like responses can be elicited with exposure to a threatening environment (Charney & Drevets,
2002; Gray & McNaughton, 2003; Mah et al., 2016). The perirhinal cortex (temporal cortical
structure) shares a reciprocal anatomic connection with the amygdala (Gray & McNaughton,
2003; Phelps & LeDoux, 2005); this structure is thought to participate in conveying information
regarding complex visual stimuli to the amygdala at the presentation of fear-conditioned visual
stimuli (Charney and Drevets, 2002).
37
mesiotemporal cortical structures, the anterior insula, the hypothalamus, the orbital and medial
prefrontal cortex, as well as the multiple brainstem nuclei (Gray & McNaughton, 2003; Mah et
al., 2016; Phelps & LeDoux , 2005). To a large extent, this network also appears to participate in
associating conditioned stimuli or operant behaviors with emotionally salient unconditioned
stimuli (Charney & Drevets, 2002; Katerndahl & Talamantes, 2000; Gray & McNaughton,
2003).
These anatomic systems are organized in such a way as to permit rapid responses to
potentially threatening stimuli and to produce longer latency responses to complex sensory
stimuli and information that is more highly processed (Charney & Drevets, 2002; Mah et al.,
2016). These neural networks respond to visceral input received directly through the nucleus
tractus solitarius (NTS) and nucleus paragigantocellularis of the vagus, as well as inputs received
indirectly through the anterior insula, loccus ceruleus (LC), and the infralimbic and prelimbic
cortices (Charney & Drevets, 2002; Gray & McNaughton, 2003. The bed nucleus of the Stria
Terminalis is hypothesized to play a role in anxiety. This structure activates the hypothalamic
and brainstem structures that function in mediating expression of emotional behavior. Anxiety-
like responses can be elicited with exposure to a threatening environment (Charney & Drevets,
2002; Gray & McNaughton, 2003; Mah et al., 2016). The perirhinal cortex (temporal cortical
structure) shares a reciprocal anatomic connection with the amygdala (Gray & McNaughton,
2003; Phelps & LeDoux, 2005); this structure is thought to participate in conveying information
regarding complex visual stimuli to the amygdala at the presentation of fear-conditioned visual
stimuli (Charney and Drevets, 2002).
37
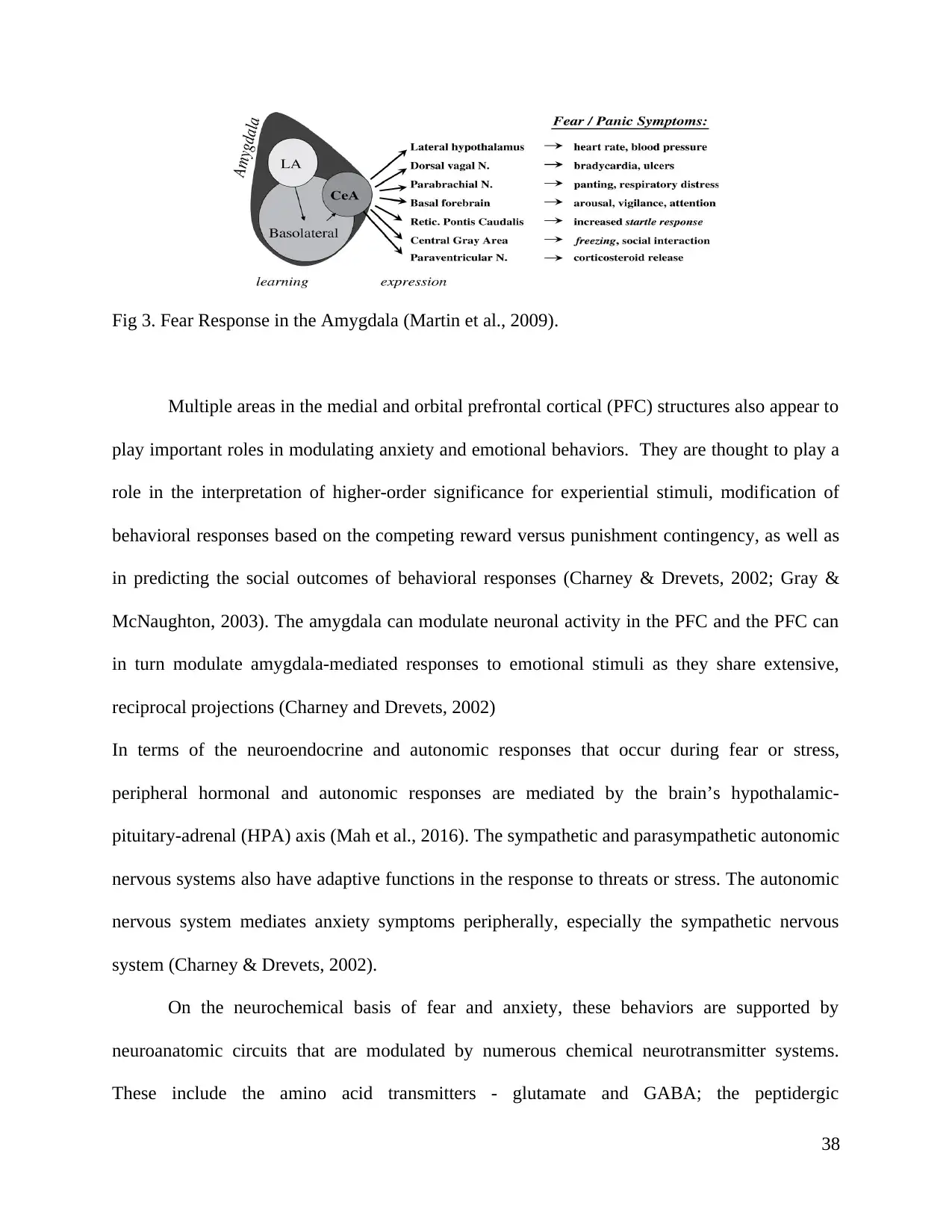
Fig 3. Fear Response in the Amygdala (Martin et al., 2009).
Multiple areas in the medial and orbital prefrontal cortical (PFC) structures also appear to
play important roles in modulating anxiety and emotional behaviors. They are thought to play a
role in the interpretation of higher-order significance for experiential stimuli, modification of
behavioral responses based on the competing reward versus punishment contingency, as well as
in predicting the social outcomes of behavioral responses (Charney & Drevets, 2002; Gray &
McNaughton, 2003). The amygdala can modulate neuronal activity in the PFC and the PFC can
in turn modulate amygdala-mediated responses to emotional stimuli as they share extensive,
reciprocal projections (Charney and Drevets, 2002)
In terms of the neuroendocrine and autonomic responses that occur during fear or stress,
peripheral hormonal and autonomic responses are mediated by the brain’s hypothalamic-
pituitary-adrenal (HPA) axis (Mah et al., 2016). The sympathetic and parasympathetic autonomic
nervous systems also have adaptive functions in the response to threats or stress. The autonomic
nervous system mediates anxiety symptoms peripherally, especially the sympathetic nervous
system (Charney & Drevets, 2002).
On the neurochemical basis of fear and anxiety, these behaviors are supported by
neuroanatomic circuits that are modulated by numerous chemical neurotransmitter systems.
These include the amino acid transmitters - glutamate and GABA; the peptidergic
38
Multiple areas in the medial and orbital prefrontal cortical (PFC) structures also appear to
play important roles in modulating anxiety and emotional behaviors. They are thought to play a
role in the interpretation of higher-order significance for experiential stimuli, modification of
behavioral responses based on the competing reward versus punishment contingency, as well as
in predicting the social outcomes of behavioral responses (Charney & Drevets, 2002; Gray &
McNaughton, 2003). The amygdala can modulate neuronal activity in the PFC and the PFC can
in turn modulate amygdala-mediated responses to emotional stimuli as they share extensive,
reciprocal projections (Charney and Drevets, 2002)
In terms of the neuroendocrine and autonomic responses that occur during fear or stress,
peripheral hormonal and autonomic responses are mediated by the brain’s hypothalamic-
pituitary-adrenal (HPA) axis (Mah et al., 2016). The sympathetic and parasympathetic autonomic
nervous systems also have adaptive functions in the response to threats or stress. The autonomic
nervous system mediates anxiety symptoms peripherally, especially the sympathetic nervous
system (Charney & Drevets, 2002).
On the neurochemical basis of fear and anxiety, these behaviors are supported by
neuroanatomic circuits that are modulated by numerous chemical neurotransmitter systems.
These include the amino acid transmitters - glutamate and GABA; the peptidergic
38
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
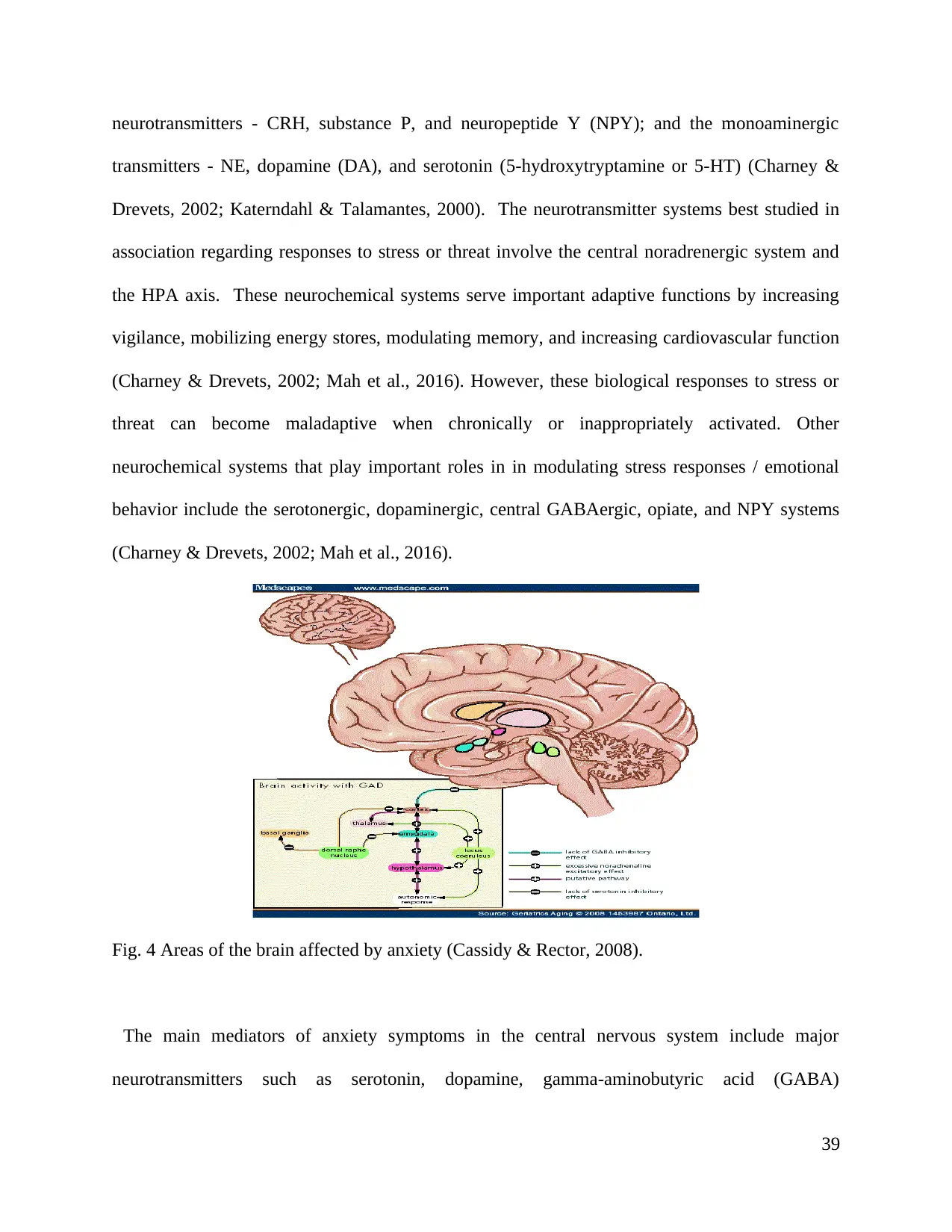
neurotransmitters - CRH, substance P, and neuropeptide Y (NPY); and the monoaminergic
transmitters - NE, dopamine (DA), and serotonin (5-hydroxytryptamine or 5-HT) (Charney &
Drevets, 2002; Katerndahl & Talamantes, 2000). The neurotransmitter systems best studied in
association regarding responses to stress or threat involve the central noradrenergic system and
the HPA axis. These neurochemical systems serve important adaptive functions by increasing
vigilance, mobilizing energy stores, modulating memory, and increasing cardiovascular function
(Charney & Drevets, 2002; Mah et al., 2016). However, these biological responses to stress or
threat can become maladaptive when chronically or inappropriately activated. Other
neurochemical systems that play important roles in in modulating stress responses / emotional
behavior include the serotonergic, dopaminergic, central GABAergic, opiate, and NPY systems
(Charney & Drevets, 2002; Mah et al., 2016).
Fig. 4 Areas of the brain affected by anxiety (Cassidy & Rector, 2008).
The main mediators of anxiety symptoms in the central nervous system include major
neurotransmitters such as serotonin, dopamine, gamma-aminobutyric acid (GABA)
39
transmitters - NE, dopamine (DA), and serotonin (5-hydroxytryptamine or 5-HT) (Charney &
Drevets, 2002; Katerndahl & Talamantes, 2000). The neurotransmitter systems best studied in
association regarding responses to stress or threat involve the central noradrenergic system and
the HPA axis. These neurochemical systems serve important adaptive functions by increasing
vigilance, mobilizing energy stores, modulating memory, and increasing cardiovascular function
(Charney & Drevets, 2002; Mah et al., 2016). However, these biological responses to stress or
threat can become maladaptive when chronically or inappropriately activated. Other
neurochemical systems that play important roles in in modulating stress responses / emotional
behavior include the serotonergic, dopaminergic, central GABAergic, opiate, and NPY systems
(Charney & Drevets, 2002; Mah et al., 2016).
Fig. 4 Areas of the brain affected by anxiety (Cassidy & Rector, 2008).
The main mediators of anxiety symptoms in the central nervous system include major
neurotransmitters such as serotonin, dopamine, gamma-aminobutyric acid (GABA)
39
andnorepinephrine (Katerndahl & Talamantes, 2000; Gray & McNaughton, 2003; Mah et al.,
2016). Exposure to stressful stimuli increases central noradrenergic function. Patients with PTSD
for instance, show evidence of increased peripheral sympathetic nervous system arousal.
Exposure to acute stress of different types also results in the release of cortisol and ACTH.
Glucocorticoid levels decrease after stress termination, and glucocorticoid-receptor density
increases while feedback sensitivity normalizes (Charney & Drevets, 2002). Acute stress
increases dopamine release and turnover across multiple brain areas (Charney & Drevets, 2002;
Mah et al., 2016). Maladaptive biological responses to stress or threat due to chronic or
inappropriate activation of neurochemical systems may occur in AD since there is neuronal
damage in AD associated with the deposition of abnormal proteins in and around the neurons
that can also disrupt neurotransmitter activity (Korolev, 2014; Norfray & Provenzale, 2004;
Reiman et al., 2005; Querfurth & LaFerla, 2010).
1.4 FUNCTIONAL ANATOMIC AND NEUROCHEMICAL CORRELATES IN
ANXIETY DISORDERS
There are functional anatomic and neurochemical correlates for specific anxiety
disorders. Studies implicate limbic, paralimbic, and sensory associations in the functional
anatomy for emotional behavior (Charney & Drevets, 2002). Anxiety disorders are characterized
by an impaired ability in regulating emotional responses to stress or perceived threat. This
impairment may be as a result of a reduction in threshold for amygdala activation or the
activation of limbic/subcortical regions in the ventral neural system, false or exaggerated activity
in these regions, or else the failure of top-down processes that are responsible for downregulating
the ventral neural system (Gray & McNaughton, 2003; Mah et al., 2016). The ventral neural
40
2016). Exposure to stressful stimuli increases central noradrenergic function. Patients with PTSD
for instance, show evidence of increased peripheral sympathetic nervous system arousal.
Exposure to acute stress of different types also results in the release of cortisol and ACTH.
Glucocorticoid levels decrease after stress termination, and glucocorticoid-receptor density
increases while feedback sensitivity normalizes (Charney & Drevets, 2002). Acute stress
increases dopamine release and turnover across multiple brain areas (Charney & Drevets, 2002;
Mah et al., 2016). Maladaptive biological responses to stress or threat due to chronic or
inappropriate activation of neurochemical systems may occur in AD since there is neuronal
damage in AD associated with the deposition of abnormal proteins in and around the neurons
that can also disrupt neurotransmitter activity (Korolev, 2014; Norfray & Provenzale, 2004;
Reiman et al., 2005; Querfurth & LaFerla, 2010).
1.4 FUNCTIONAL ANATOMIC AND NEUROCHEMICAL CORRELATES IN
ANXIETY DISORDERS
There are functional anatomic and neurochemical correlates for specific anxiety
disorders. Studies implicate limbic, paralimbic, and sensory associations in the functional
anatomy for emotional behavior (Charney & Drevets, 2002). Anxiety disorders are characterized
by an impaired ability in regulating emotional responses to stress or perceived threat. This
impairment may be as a result of a reduction in threshold for amygdala activation or the
activation of limbic/subcortical regions in the ventral neural system, false or exaggerated activity
in these regions, or else the failure of top-down processes that are responsible for downregulating
the ventral neural system (Gray & McNaughton, 2003; Mah et al., 2016). The ventral neural
40
system (amygdala) which responds to threat may be hyperactive while the dorsal neural system
(PFC and hippocampus) may be hypoactive (Mah et al., 2016).
Evidence also suggests that anxiety disorders are associated with heightened sensitivity to
negative information or threat in the external environment, with the result that attention is
selective for threat. Exposure to threat is in turn associated with heightened or enhanced
amygdala activity (Charney & Drevets, 2002; Gray & McNaughton, 2003). This association has
been shown in social anxiety disorder (SAD), panic disorder, simple phobias, GAD, and PTSD
(Mah et al., 2016). Anxiety disorders are associated with over generalization of fear across
stimuli or contexts since there is impaired ability to discriminate between safety cues and threats.
This impaired discriminative conditioning or deficits in discriminative conditioning are seen in
GAD, social phobia, and panic disorder (Mah et al., 2016).
Evidence also shows that there is impaired extinction learning, reduced mPFC activity, as well as
decoupling of the amygdala and mPFC in anxiety disorders (Mah et al., 2016). This would
suggest that there is decreased control over the amygdala and associated regions in the ventral
neural system, by the PFC (Charney & Drevets, 2002; Gray & McNaughton, 2003; Mah et al.,
2016). PTSD for instance, is hypothesized to involve an emotional-learning circuitry linked to
the amygdala since the traumatic event is a fear-conditioning experience. Subsequent exposure to
contextual, sensory, or mnemonic stimuli that recalls the event leads to psychological distress
and sympathetic system arousal (Mah et al., 2016).
Looking at neurobiological correlates in anxiety disorders, panic disorder, for instance, is a
neurochemical dysfunction that is genetically inherited. Evidence suggests that the chromosomal
regions 13q, 4q31-q34, 14q, 22q, and 9q31 may be associated with heritability for the phenotype
in this disorder type (Johnson, Lydiard & Ballenger, 1995; Yates, 2015). Panic disorder may also
41
(PFC and hippocampus) may be hypoactive (Mah et al., 2016).
Evidence also suggests that anxiety disorders are associated with heightened sensitivity to
negative information or threat in the external environment, with the result that attention is
selective for threat. Exposure to threat is in turn associated with heightened or enhanced
amygdala activity (Charney & Drevets, 2002; Gray & McNaughton, 2003). This association has
been shown in social anxiety disorder (SAD), panic disorder, simple phobias, GAD, and PTSD
(Mah et al., 2016). Anxiety disorders are associated with over generalization of fear across
stimuli or contexts since there is impaired ability to discriminate between safety cues and threats.
This impaired discriminative conditioning or deficits in discriminative conditioning are seen in
GAD, social phobia, and panic disorder (Mah et al., 2016).
Evidence also shows that there is impaired extinction learning, reduced mPFC activity, as well as
decoupling of the amygdala and mPFC in anxiety disorders (Mah et al., 2016). This would
suggest that there is decreased control over the amygdala and associated regions in the ventral
neural system, by the PFC (Charney & Drevets, 2002; Gray & McNaughton, 2003; Mah et al.,
2016). PTSD for instance, is hypothesized to involve an emotional-learning circuitry linked to
the amygdala since the traumatic event is a fear-conditioning experience. Subsequent exposure to
contextual, sensory, or mnemonic stimuli that recalls the event leads to psychological distress
and sympathetic system arousal (Mah et al., 2016).
Looking at neurobiological correlates in anxiety disorders, panic disorder, for instance, is a
neurochemical dysfunction that is genetically inherited. Evidence suggests that the chromosomal
regions 13q, 4q31-q34, 14q, 22q, and 9q31 may be associated with heritability for the phenotype
in this disorder type (Johnson, Lydiard & Ballenger, 1995; Yates, 2015). Panic disorder may also
41
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
involve decrease in GABA-ergic tone, polymorphism of the catechol-O-methyltransferase gene
(allelic), autonomic imbalance, increase in adenosine receptor function, increased cortisol,
reduced function of the benzodiazepine receptor, as well as disturbances in serotonin transporter
(5-HTTLPR)[17], serotonin, and promoter (SLC6A4) genes (Cassidy & Rector, 2008). Other
theories about panic disorder include that the disorder represents a state of chronic
hyperventilation and hypersensitivity in the carbon dioxide receptors (Johnson et al., 1995;
Yates, 2015). MRI results reveal reduced temporal lobe volume in patients diagnosed with panic
disorder although their hippocampal volume is normal. Positron emission tomography (PET)
scanning also reveals reduced binding of serotonin type 1A receptor in the raphe and anterior and
posterior cingulate, and additionally, increased flow in the right parahippocampal region
(Cassidy & Rector, 2008).
1.5 NEUROPSYCHOLOGICAL RELATIONSHIP BETWEEN ANXIETY AND
COGNITIVE DECLINE
There is a quite different relationship between the cognitive processing and anxiety. For
assessing the cognitive development, various methods can be used, from which one of the most
well known and common method is to test with a Piagetian conversation along with a theory of
mind test (TOM). According to Piagetian conversation, it can be considered as the ability for
thinking logically. As per Piaget, cognitive development, it can be classified in four types such as
sensorimeter, period of formal operational, concrete operational and the pre operational.
However, anxiety is considered as a risk factor for various diseases including dementia as well as
cognitive decline. It has also been observed that anxiety is being termed with the maximized risk
of the cognitive impairment as well as dementia. These factors and its risk can be increased by a
42
(allelic), autonomic imbalance, increase in adenosine receptor function, increased cortisol,
reduced function of the benzodiazepine receptor, as well as disturbances in serotonin transporter
(5-HTTLPR)[17], serotonin, and promoter (SLC6A4) genes (Cassidy & Rector, 2008). Other
theories about panic disorder include that the disorder represents a state of chronic
hyperventilation and hypersensitivity in the carbon dioxide receptors (Johnson et al., 1995;
Yates, 2015). MRI results reveal reduced temporal lobe volume in patients diagnosed with panic
disorder although their hippocampal volume is normal. Positron emission tomography (PET)
scanning also reveals reduced binding of serotonin type 1A receptor in the raphe and anterior and
posterior cingulate, and additionally, increased flow in the right parahippocampal region
(Cassidy & Rector, 2008).
1.5 NEUROPSYCHOLOGICAL RELATIONSHIP BETWEEN ANXIETY AND
COGNITIVE DECLINE
There is a quite different relationship between the cognitive processing and anxiety. For
assessing the cognitive development, various methods can be used, from which one of the most
well known and common method is to test with a Piagetian conversation along with a theory of
mind test (TOM). According to Piagetian conversation, it can be considered as the ability for
thinking logically. As per Piaget, cognitive development, it can be classified in four types such as
sensorimeter, period of formal operational, concrete operational and the pre operational.
However, anxiety is considered as a risk factor for various diseases including dementia as well as
cognitive decline. It has also been observed that anxiety is being termed with the maximized risk
of the cognitive impairment as well as dementia. These factors and its risk can be increased by a
42
maximized age and other related factors. Often, anxiety is being associated with the dementia
and cognitive decline, as a major factor of risk. After enormous number of observations, it has
been observed by the people in which they analyzed that MCI is considered as a very essential
factor for dementia and other various diseases as well such as for depression and anxiety.
Although more number has been presented on depression because in today's world, everyone is
having tensions, whether some must be having lesser and probably, some may be having bigger
ones. Depression can be evolved in a person because of various reasons such as there may be
some issues in the relationship, or with the family members etc. Such factors act as the main
reasons for depression and further, if these are not being sorted for a longer period, the person
might be involved in various other acts such as thinking of suicide, doing substance abuse etc.
Both of these factors have become common nowadays. So, it is important for the authorities to
ensure and stay aware of anxiety that it is considered as a very essential symptom for dementia.
Specially, it is being considered at the time when people have to face anxiety at later stages of
life.
Anxiety is considered as a very common symptom in patients that suffer from dementia
with an estimated prevalence of anxiety symptoms in dementia ranging from 8% to 71%, and
10% to 74% in patients with mild cognitive impairment (MCI) (Yates, 2015). Mild cognitive
impairment (MCI) is considered as an impairment that is responsible for making a slight decline
in the abilities which also involves the skills of a person about their abilities and intelligence as
well. The important factor which is to be note here is that although these changes are slight and
very smooth, but these are noticeable enough and cannot be avoided. So, these can be considered
as that impairment in which the change is small and in a way that the people are able to notice it
(Fauzan & Amran, 2015; Boudreaux & Hara, 2008). Persons with MCI are not impaired but they
43
and cognitive decline, as a major factor of risk. After enormous number of observations, it has
been observed by the people in which they analyzed that MCI is considered as a very essential
factor for dementia and other various diseases as well such as for depression and anxiety.
Although more number has been presented on depression because in today's world, everyone is
having tensions, whether some must be having lesser and probably, some may be having bigger
ones. Depression can be evolved in a person because of various reasons such as there may be
some issues in the relationship, or with the family members etc. Such factors act as the main
reasons for depression and further, if these are not being sorted for a longer period, the person
might be involved in various other acts such as thinking of suicide, doing substance abuse etc.
Both of these factors have become common nowadays. So, it is important for the authorities to
ensure and stay aware of anxiety that it is considered as a very essential symptom for dementia.
Specially, it is being considered at the time when people have to face anxiety at later stages of
life.
Anxiety is considered as a very common symptom in patients that suffer from dementia
with an estimated prevalence of anxiety symptoms in dementia ranging from 8% to 71%, and
10% to 74% in patients with mild cognitive impairment (MCI) (Yates, 2015). Mild cognitive
impairment (MCI) is considered as an impairment that is responsible for making a slight decline
in the abilities which also involves the skills of a person about their abilities and intelligence as
well. The important factor which is to be note here is that although these changes are slight and
very smooth, but these are noticeable enough and cannot be avoided. So, these can be considered
as that impairment in which the change is small and in a way that the people are able to notice it
(Fauzan & Amran, 2015; Boudreaux & Hara, 2008). Persons with MCI are not impaired but they
43
exhibit a typical sort of functioning (Braun, 2011). As noted previously, SCI, on the other hand,
may be an age-related process of cognitive decline in which there are perceptions that some
aspects of functioning such as memory is not quite as functional or effective (Fauzan & Amran,
2015; Boudreaux & Hara, 2008; Tales, 2015). The prevalence for anxiety disorders in MCI is
estimated at about 49%. Anxiety can also coexist in patients with dementia and MCI, exhibiting
common symptoms across the two effective states, and complicating diagnosis (Ortega, Qazi, &
Orrell, 2015). At the same time, there is some lack of consensus as to how anxiety in dementia
should be defined; for instance, there is a question whether anxiety and agitation are different
concepts (Ortega and et al., 2015).
Some answers may be found to such questions when anxiety is examined in the context
of contemporary neuropsychological theories. There are several neuropsychological theories of
anxiety. The two process theories of learning are the classical “stimulus–stimulus” or
“respondent” theory and the instrumental (“stimulus–response” or “operant” conditioning (Gray
& McNaughton, 2003). In the first theory, behaviors are acquired through conditioning, where
the subject learns associative relationships between stimulus events. In instrumental
conditioning, the subject acquires behavior patterns that can alter the frequency of exposure to
stimulus events (Gray & McNaughton, 2003; McNaughton, & Corr, 2004). Another theory, the
behavioral inhibition system theory, is more commonly accepted as being central to anxiety. The
premise for this theory is that a fight–flight–freezing system that controls behavior whenever the
primary purpose of the subject is to remove itself from danger or to reach safety. The behavioral
inhibition system on the other hand controls behavior whenever the primary purpose of the
subject conflicting. For instance, the subject wants to achieve a goal that requires moving
towards the source of danger, a conflicting goal of satisfying the appetite and reaching safety at
44
may be an age-related process of cognitive decline in which there are perceptions that some
aspects of functioning such as memory is not quite as functional or effective (Fauzan & Amran,
2015; Boudreaux & Hara, 2008; Tales, 2015). The prevalence for anxiety disorders in MCI is
estimated at about 49%. Anxiety can also coexist in patients with dementia and MCI, exhibiting
common symptoms across the two effective states, and complicating diagnosis (Ortega, Qazi, &
Orrell, 2015). At the same time, there is some lack of consensus as to how anxiety in dementia
should be defined; for instance, there is a question whether anxiety and agitation are different
concepts (Ortega and et al., 2015).
Some answers may be found to such questions when anxiety is examined in the context
of contemporary neuropsychological theories. There are several neuropsychological theories of
anxiety. The two process theories of learning are the classical “stimulus–stimulus” or
“respondent” theory and the instrumental (“stimulus–response” or “operant” conditioning (Gray
& McNaughton, 2003). In the first theory, behaviors are acquired through conditioning, where
the subject learns associative relationships between stimulus events. In instrumental
conditioning, the subject acquires behavior patterns that can alter the frequency of exposure to
stimulus events (Gray & McNaughton, 2003; McNaughton, & Corr, 2004). Another theory, the
behavioral inhibition system theory, is more commonly accepted as being central to anxiety. The
premise for this theory is that a fight–flight–freezing system that controls behavior whenever the
primary purpose of the subject is to remove itself from danger or to reach safety. The behavioral
inhibition system on the other hand controls behavior whenever the primary purpose of the
subject conflicting. For instance, the subject wants to achieve a goal that requires moving
towards the source of danger, a conflicting goal of satisfying the appetite and reaching safety at
44
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
the same time. Anxiety is identified with activity in the behavior (Gray & McNaughton, 2003;
McNaughton, & Corr, 2004).
Conceptualizing the relationship between anxiety and dementia is a complex task as there
are overlaps between the symptoms of anxiety and dementia. GAD for instance, has symptoms
such as fatigue, restlessness and difficult concentrating (National Institutes for Health [NIH],
2017). These symptoms also occur in dementia even in the absence of an anxiety disorder
(Davis, 2015; Korolev, 2014). However, several factors suggest a direct relationship between
dementia and anxiety. First, the neural degeneration that occurs in dementia can also affect the
limbic structures which are associated with the regulation of emotions (Seignourel, Kunik, Snow,
et al., 2008). Secondly, individuals with dementia tend to have more anxiety, with the levels of
anxiety varying based on the type of dementia (Seignourel et al., 2008). Thirdly, anxiety
symptoms overlap with those of dementia. With regard to the effects of anxiety on the brain and
its implications for dementia, pathological anxiety and chronic stress can increase risk of
neuropsychiatric disorders, including dementia and depression (Mah et al., 2016). Chronic stress
increases amygdala function while leading to deficits in emotion regulation due to stress-induced
impaired hippocampal neurogenesis and the structural degeneration of the PFC. Such stress-
induced changes can contribute to the development of effective and cognitive disorders (Mah
and et.al., 2016).
CONCLUSION
It can be concluded from the literature review that there is a potential relationship with
the anxiety and the inhibitory cognitive control and for understanding the relationship in
between, various cognitive changes have been analyzed along with a wide range of factors that
45
McNaughton, & Corr, 2004).
Conceptualizing the relationship between anxiety and dementia is a complex task as there
are overlaps between the symptoms of anxiety and dementia. GAD for instance, has symptoms
such as fatigue, restlessness and difficult concentrating (National Institutes for Health [NIH],
2017). These symptoms also occur in dementia even in the absence of an anxiety disorder
(Davis, 2015; Korolev, 2014). However, several factors suggest a direct relationship between
dementia and anxiety. First, the neural degeneration that occurs in dementia can also affect the
limbic structures which are associated with the regulation of emotions (Seignourel, Kunik, Snow,
et al., 2008). Secondly, individuals with dementia tend to have more anxiety, with the levels of
anxiety varying based on the type of dementia (Seignourel et al., 2008). Thirdly, anxiety
symptoms overlap with those of dementia. With regard to the effects of anxiety on the brain and
its implications for dementia, pathological anxiety and chronic stress can increase risk of
neuropsychiatric disorders, including dementia and depression (Mah et al., 2016). Chronic stress
increases amygdala function while leading to deficits in emotion regulation due to stress-induced
impaired hippocampal neurogenesis and the structural degeneration of the PFC. Such stress-
induced changes can contribute to the development of effective and cognitive disorders (Mah
and et.al., 2016).
CONCLUSION
It can be concluded from the literature review that there is a potential relationship with
the anxiety and the inhibitory cognitive control and for understanding the relationship in
between, various cognitive changes have been analyzed along with a wide range of factors that
45
are directly or indirectly related to the cognitive change and anxiety. It also included the effect of
ageing on various functions of the body such as the visual attention, ability to think etc. As the
person ages, there have been observed various changes in the human body. There are various
disorders as well that are related to anxiety and the cognitive control and both of them have
different impacts on the human body.
46
ageing on various functions of the body such as the visual attention, ability to think etc. As the
person ages, there have been observed various changes in the human body. There are various
disorders as well that are related to anxiety and the cognitive control and both of them have
different impacts on the human body.
46
REFERENCES
Books and Journals
Acierno, R., Ruggiers, J., Kilpatrick, G. et al (2006). Risk and protective factors for
psychopathology among older versus younger adults after the 2004 Florida hurricanes.
Am J Geriatr Psychiatry 2006; 14: 1051–59.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders.
5th ed. Arlington, VA: APA Press; 2013.
Braun, K. (2011). Behavioral interventions in elderly populations with Dementia: A
review of relevant factors. Illinois State University.
Beaudreau, S. & Hara, R. (2008). Late-life anxiety and cognitive impairment: A review.
Am J Geriatr Psychiatry, 16(10):790-803
Bryant, C., Jackson, H. & Ames, D. (2008). The prevalence of anxiety in older adults:
methodological issues and a review of the literature. J. Aflect. Disord 109(3), 233-250.
Bartels SJ, Coakley E, Oxman TE, Constantino G, et al. (2002). Suicidal ideation and
death ideation in older primary care patients with depression, anxiety, and at-risk alcohol
use. Am J Geriatr Psychiatry 10: 417–27.
47
Books and Journals
Acierno, R., Ruggiers, J., Kilpatrick, G. et al (2006). Risk and protective factors for
psychopathology among older versus younger adults after the 2004 Florida hurricanes.
Am J Geriatr Psychiatry 2006; 14: 1051–59.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders.
5th ed. Arlington, VA: APA Press; 2013.
Braun, K. (2011). Behavioral interventions in elderly populations with Dementia: A
review of relevant factors. Illinois State University.
Beaudreau, S. & Hara, R. (2008). Late-life anxiety and cognitive impairment: A review.
Am J Geriatr Psychiatry, 16(10):790-803
Bryant, C., Jackson, H. & Ames, D. (2008). The prevalence of anxiety in older adults:
methodological issues and a review of the literature. J. Aflect. Disord 109(3), 233-250.
Bartels SJ, Coakley E, Oxman TE, Constantino G, et al. (2002). Suicidal ideation and
death ideation in older primary care patients with depression, anxiety, and at-risk alcohol
use. Am J Geriatr Psychiatry 10: 417–27.
47
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Bouhuys, A., Geerts, E. & Mersch, P. (1997). Relationship between perception of facial
emotions and anxiety in clinical depression: does anxiety-related perception predict
persistence of depression? Journal of Affective Disorders, 43: 213-223.
Burke, D. & Mackay, D. (1997). Memory, language, and ageing. Phil. Trans. R. Soc.
Lond. 352:1845-1856
Cassidy, K. & Rector, N. (2008). The silent geriatric giant: anxiety disorders in late life.
Geriatrics and ageing. 11(3):150-156.
Charney & Drevets (2002). Neurobiological basis of anxiety disorders. In
Neuropsychopharmacology: The Fifth Generation of Progress.
Kenneth L. Davis, Dennis Charney, Joseph T. Coyle, and Charles Nemeroff (Eds).
American College of Neuropsychopharmacology.
Cooper C, Bebbington P, Lindesay J, Meltzer H, McManus S, Jenkins R, Livingston G.
(2011). The meaning of reporting forgetfulness: a cross-sectional study of adults in the
English 2007 Adult Psychiatric Morbidity Survey. Age Ageing 40: 711–17.
Castaneda, A., Tuulio-Henriksson, A., Marttunen, M., Suvisaari, J. & Lonnqvist, J.
(2008). A review on cognitive impairments in depressive and anxiety disorders with a
focus on young adults. Journal of Affective Disorders, 108: 1-27
48
emotions and anxiety in clinical depression: does anxiety-related perception predict
persistence of depression? Journal of Affective Disorders, 43: 213-223.
Burke, D. & Mackay, D. (1997). Memory, language, and ageing. Phil. Trans. R. Soc.
Lond. 352:1845-1856
Cassidy, K. & Rector, N. (2008). The silent geriatric giant: anxiety disorders in late life.
Geriatrics and ageing. 11(3):150-156.
Charney & Drevets (2002). Neurobiological basis of anxiety disorders. In
Neuropsychopharmacology: The Fifth Generation of Progress.
Kenneth L. Davis, Dennis Charney, Joseph T. Coyle, and Charles Nemeroff (Eds).
American College of Neuropsychopharmacology.
Cooper C, Bebbington P, Lindesay J, Meltzer H, McManus S, Jenkins R, Livingston G.
(2011). The meaning of reporting forgetfulness: a cross-sectional study of adults in the
English 2007 Adult Psychiatric Morbidity Survey. Age Ageing 40: 711–17.
Castaneda, A., Tuulio-Henriksson, A., Marttunen, M., Suvisaari, J. & Lonnqvist, J.
(2008). A review on cognitive impairments in depressive and anxiety disorders with a
focus on young adults. Journal of Affective Disorders, 108: 1-27
48
Corbett. A., Williams, G. & Ballard, C.(2013). Drug repositioning: an opportunity to
develop novel treatments for Alzheimer’s disease. Pharmaceuticals 6: 1304-21. doi:
10.3390/ph6101304.
Corna LM, Cairney J, Herrmann N, Veldhuizen S, McCabe L, Streiner D. (2007). Panic
disorder in later life: results from a national survey of Canadians. Int Psychogeriatr 2007;
19: 1084–96.
Davis, C. (2015) Dementia. Emedicine. WebMD.
http://www.emedicinehealth.com/dementia_overview/article_em.htm
Delis, D., Kramer, J., Kaplan, E. & Ober, B. (2000). CVLT-II California verbal learning
test. San Antonio, TX: The Psychological Corporation.
Derakshan, N. & Eysenck, M. (2009). Anxiety, processing efficiency, and cognitive
performance. New developments from attentional control theory. European Psychologist
14(2): 168-176
Davidson, M., Dima, A. Loren, A. et al. (2006). Development of cognitive control and
executive functions from 4 to 13 years: Evidence from manipulations of memory,
inhibition, and task switching. Neuropsychologia 44 (11): 2037–2078
49
develop novel treatments for Alzheimer’s disease. Pharmaceuticals 6: 1304-21. doi:
10.3390/ph6101304.
Corna LM, Cairney J, Herrmann N, Veldhuizen S, McCabe L, Streiner D. (2007). Panic
disorder in later life: results from a national survey of Canadians. Int Psychogeriatr 2007;
19: 1084–96.
Davis, C. (2015) Dementia. Emedicine. WebMD.
http://www.emedicinehealth.com/dementia_overview/article_em.htm
Delis, D., Kramer, J., Kaplan, E. & Ober, B. (2000). CVLT-II California verbal learning
test. San Antonio, TX: The Psychological Corporation.
Derakshan, N. & Eysenck, M. (2009). Anxiety, processing efficiency, and cognitive
performance. New developments from attentional control theory. European Psychologist
14(2): 168-176
Davidson, M., Dima, A. Loren, A. et al. (2006). Development of cognitive control and
executive functions from 4 to 13 years: Evidence from manipulations of memory,
inhibition, and task switching. Neuropsychologia 44 (11): 2037–2078
49
Dickstein, L., Kabaso, D., Roche, B. et al., (2007). Changes in the structural complexity
of the aged brain. ageing cell. 2007; 6:275–84.
Dowden, S. & Allen, G. (1997). Relationships between anxiety sensitivity,
hyperventilation, and emotional reactivity to displays of facial emotions. Journal of
Anxiety Disorders, 11, 63-75
Elias, L. & Saucier, D. (2006). Neuropsychology: Clinical and experimental foundations.
Boston: Pearson Education, Inc.
Fauzan, N. & Amran, N. (2015). Brain dynamics of mild cognitive impairment (MCI)
from EEG features. Procedia – Social and behavioral Sciences, 165: 284-290
Gray, J. & McNaughton, N. (2003). The Neuropsychology of Anxiety: An Enquiry into
the Functions of the Septo-Hippocampal System, Second Edition. Oxford University
Press.
Goodwin, G. (2015). The overlap between anxiety, depression, and obsessive-compulsive
disorder. Dialogues Clin Neurosci. 17(3): 249–260.
Harada, C., Love, M. &Triebeld, K. (2013). Normal cognitive ageing. Clin Geriatr Med.
29(4): 737–752. doi: 10.1016/j.cger.2013.07.002
50
of the aged brain. ageing cell. 2007; 6:275–84.
Dowden, S. & Allen, G. (1997). Relationships between anxiety sensitivity,
hyperventilation, and emotional reactivity to displays of facial emotions. Journal of
Anxiety Disorders, 11, 63-75
Elias, L. & Saucier, D. (2006). Neuropsychology: Clinical and experimental foundations.
Boston: Pearson Education, Inc.
Fauzan, N. & Amran, N. (2015). Brain dynamics of mild cognitive impairment (MCI)
from EEG features. Procedia – Social and behavioral Sciences, 165: 284-290
Gray, J. & McNaughton, N. (2003). The Neuropsychology of Anxiety: An Enquiry into
the Functions of the Septo-Hippocampal System, Second Edition. Oxford University
Press.
Goodwin, G. (2015). The overlap between anxiety, depression, and obsessive-compulsive
disorder. Dialogues Clin Neurosci. 17(3): 249–260.
Harada, C., Love, M. &Triebeld, K. (2013). Normal cognitive ageing. Clin Geriatr Med.
29(4): 737–752. doi: 10.1016/j.cger.2013.07.002
50
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Haaland, Y., Price, L. & Larue, A. (2003). What does the WMS-III tell us about memory
changes with normal ageing? Journal of the International Neuropsychological Society:
JINS. 9:89–96.
Hek, K., Tiemeier, H., Newson, S., et al. (2011). Anxiety disorders and comorbid
depression in community dwelling older adults. Int. J. Methods. Psychiatr. Res 20(3),
157-168.
Hebert, E., Scherr, A., McCann, J. et al. (2001). Is the risk of developing Alzheimer’s
disease greater for women than for men? Am J Epidemiol 153: 132 6. doi: 10.1093/
/153.2.132.
Hopko DR, Bourland SL, Stanley MA, et al. (2000). Generalized anxiety disorder in
older adults: examining the relationship between clinician severity ratings and patient
self-report measures. Depress Anxiety 12: 17–25.
Johnson MR, Lydiard RB, Ballenger JC. (1995). Panic disorder. Pathophysiology and
drug treatment. Drugs. 49(3):328-44.
Katerndahl DA, Talamantes M. A comparison of persons with early-versus late-onset
panic attacks. J Clin Psychiatry. 2000 Jun. 61(6):422-7
51
changes with normal ageing? Journal of the International Neuropsychological Society:
JINS. 9:89–96.
Hek, K., Tiemeier, H., Newson, S., et al. (2011). Anxiety disorders and comorbid
depression in community dwelling older adults. Int. J. Methods. Psychiatr. Res 20(3),
157-168.
Hebert, E., Scherr, A., McCann, J. et al. (2001). Is the risk of developing Alzheimer’s
disease greater for women than for men? Am J Epidemiol 153: 132 6. doi: 10.1093/
/153.2.132.
Hopko DR, Bourland SL, Stanley MA, et al. (2000). Generalized anxiety disorder in
older adults: examining the relationship between clinician severity ratings and patient
self-report measures. Depress Anxiety 12: 17–25.
Johnson MR, Lydiard RB, Ballenger JC. (1995). Panic disorder. Pathophysiology and
drug treatment. Drugs. 49(3):328-44.
Katerndahl DA, Talamantes M. A comparison of persons with early-versus late-onset
panic attacks. J Clin Psychiatry. 2000 Jun. 61(6):422-7
51
Lindesay, J., Stewart, R. & Bisla, J. (2012). Anxiety disorders in older people. Rev. Clin.
Geront 22(1), 204-217
Liebman, S. & Allen, G. (1995). Anxiety sensitivity, state anxiety and perceptions of
facial emotions. Journal of Anxiety Disorders, 9(4): 257-267.
Lezak, M., Howieson, D, Bigler, E. & Tranel, D. (2012). Neuropsychological assessment.
5. New York: Oxford University Press.
Mah, L., Binnus, M. & Steffens, D. (2016). Can anxiety damage the brain? Curr Opin
Psychiatry 29:56–63
McKhann, G., Drachman, D., Folstein, M. et al (1984). Clinical diagnosis of
Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of
Department of Health and Human Services Task Force on Alzheimer’s disease.
Neurology 1984; 34: 93944.
Mehta, M., Yaffe, K., Brenes, A. (2007). Anxiety symptoms and decline in
physical function over 5 years in the health, ageing and the body composition study. J Am
Geriatr Soc 55: 265–70.
Minaker, L. (2011). Common clinical sequelae of ageing. In: Goldman L, Schafer AI,
eds Goldman's Cecil Medicine. 24th ed. Philadelphia, PA: Elsevier Saunders.
52
Geront 22(1), 204-217
Liebman, S. & Allen, G. (1995). Anxiety sensitivity, state anxiety and perceptions of
facial emotions. Journal of Anxiety Disorders, 9(4): 257-267.
Lezak, M., Howieson, D, Bigler, E. & Tranel, D. (2012). Neuropsychological assessment.
5. New York: Oxford University Press.
Mah, L., Binnus, M. & Steffens, D. (2016). Can anxiety damage the brain? Curr Opin
Psychiatry 29:56–63
McKhann, G., Drachman, D., Folstein, M. et al (1984). Clinical diagnosis of
Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of
Department of Health and Human Services Task Force on Alzheimer’s disease.
Neurology 1984; 34: 93944.
Mehta, M., Yaffe, K., Brenes, A. (2007). Anxiety symptoms and decline in
physical function over 5 years in the health, ageing and the body composition study. J Am
Geriatr Soc 55: 265–70.
Minaker, L. (2011). Common clinical sequelae of ageing. In: Goldman L, Schafer AI,
eds Goldman's Cecil Medicine. 24th ed. Philadelphia, PA: Elsevier Saunders.
52
Martin, E., Ressler, K., Binder, E. et al. (2009). The neurobiology of anxiety disorders:
Brain Imageing, Genetics, and Psychoneuroendocrinology. Psychiatr Clin North Am.
32(3): 549–575. doi: 10.1016/j.psc.2009.05.004
McNaughton, N. & Corr, J. (2004). A two-dimensional neuropsychology of defense:
fear/anxiety and defensive distance. Neuroscience and Biobehavioral Reviews, 28, 285–
305
Mesulam M. Brain, mind, and the evolution of connectivity. Brain Cogn. 2000;42:4–6.
Norfray, F. & Provenzale, M. (2004). Alzheimer’s disease: neuropathologic findings and
recent advances in imageing. AJR Am J Roentgenol 2004; 182: 313. doi:
10.2214/ajr.182.1.1820003
O’Sullivan M, Summers PE, Jones DK, Jarosz JM, Williams SC, Markus HS. Normal-
appearing white matter in ischemic leukoaraiosis: a diffusion tensor MRI study.
Neurology. 2001; 57:2307–10.
Phelps, A. & LeDoux, E. (2005). Contributions of the amygdala to emotion processing:
from animal models to human behavior. Neuron 48:175–187.
Peter, T., Hertwig, R. & Hoffrage, U. (2004). Evolutionary cognitive psychology.
Handbook of Evolutionary Psychology.
53
Brain Imageing, Genetics, and Psychoneuroendocrinology. Psychiatr Clin North Am.
32(3): 549–575. doi: 10.1016/j.psc.2009.05.004
McNaughton, N. & Corr, J. (2004). A two-dimensional neuropsychology of defense:
fear/anxiety and defensive distance. Neuroscience and Biobehavioral Reviews, 28, 285–
305
Mesulam M. Brain, mind, and the evolution of connectivity. Brain Cogn. 2000;42:4–6.
Norfray, F. & Provenzale, M. (2004). Alzheimer’s disease: neuropathologic findings and
recent advances in imageing. AJR Am J Roentgenol 2004; 182: 313. doi:
10.2214/ajr.182.1.1820003
O’Sullivan M, Summers PE, Jones DK, Jarosz JM, Williams SC, Markus HS. Normal-
appearing white matter in ischemic leukoaraiosis: a diffusion tensor MRI study.
Neurology. 2001; 57:2307–10.
Phelps, A. & LeDoux, E. (2005). Contributions of the amygdala to emotion processing:
from animal models to human behavior. Neuron 48:175–187.
Peter, T., Hertwig, R. & Hoffrage, U. (2004). Evolutionary cognitive psychology.
Handbook of Evolutionary Psychology.
53
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Querfurth, W. & LaFerla, M. (2010). Alzheimer’s disease. N Engl J Med 2010; 362:
32944. doi: 10.1056/NEJMra0909142
Reiman, M., Chen, K., Alexander, G. et al. (2005). Correlations between apolipoprotein
Eepsilon4 gene dose and brain-imageing measurements of regional hypometabolism.
Proc Natl Acad Sci U S A 102:8299 -302. doi: 10.1073/pnas.0500579102
Rozzini, L., Chilovi, V., Peli, M., Conti, M., Rozzini, R., Trabucchi, M. et al. (2009)
Anxiety symptoms in mild cognitive impairment. Int J Geriatr Psychiatry. 24(3):300-5.
doi: 10.1002/gps.2106.
Rodrigue, M., Kennedy, M. & Park, C. (2009). Beta-amyloid deposition and the ageing
brain.Neuropsychology review. 19:436–50.
Salthouse, A. (2010). Selective review of cognitive ageing. Journal of the International
Neuropsychological Society: JINS. 16:754–60.
Salthouse T. (2012). Consequences of age-related cognitive declines. Annual review of
psychology. 63:201–26.
Salthouse TA. Decomposing age correlations on neuropsychological and cognitive
variables. Journal of the International Neuropsychological Society. 2009; 15:650–61.
54
32944. doi: 10.1056/NEJMra0909142
Reiman, M., Chen, K., Alexander, G. et al. (2005). Correlations between apolipoprotein
Eepsilon4 gene dose and brain-imageing measurements of regional hypometabolism.
Proc Natl Acad Sci U S A 102:8299 -302. doi: 10.1073/pnas.0500579102
Rozzini, L., Chilovi, V., Peli, M., Conti, M., Rozzini, R., Trabucchi, M. et al. (2009)
Anxiety symptoms in mild cognitive impairment. Int J Geriatr Psychiatry. 24(3):300-5.
doi: 10.1002/gps.2106.
Rodrigue, M., Kennedy, M. & Park, C. (2009). Beta-amyloid deposition and the ageing
brain.Neuropsychology review. 19:436–50.
Salthouse, A. (2010). Selective review of cognitive ageing. Journal of the International
Neuropsychological Society: JINS. 16:754–60.
Salthouse T. (2012). Consequences of age-related cognitive declines. Annual review of
psychology. 63:201–26.
Salthouse TA. Decomposing age correlations on neuropsychological and cognitive
variables. Journal of the International Neuropsychological Society. 2009; 15:650–61.
54
Singh-Manoux A, Kivimaki M, Glymour MM, et al. (2012). Timing of onset of cognitive
decline: results from Whitehall II prospective cohort study. Bmj. 344:d7622.
Seignourel, P., Kunik, M., Snow, L., Wilson, N. & Stanley. M. (2008). Anxiety in
dementia: A critical review. Clin Psychol Rev, 28(7):1071-1082
Schnitzspahn, M., Stahl, C., Zeintl, M., Kaller, P. & Kliegel, M. (2012). The role of
shifting, updating, and inhibition in prospective memory performance in young and older
adults. Developmental psychology. 2012.
Stern, Y. (2012). Cognitive reserve in ageing and Alzheimer’s disease. Lancet Neurol
11: 1006 12. doi: 10.1016/S1474-4422(12)70191-6
Schaub, T. & Linden, M. (2001). Anxiety and anxiety disorders in the old and very old –
results from the Berlin ageing Study. Comp Psychiatry 41: 48–54.
Shadlen, M. & Larson, E. (2010). Evaluation of cognitive impairment and dementia. In:
Basow D, ed. Waltham, MA: Steimer, T. (2002). The biology of fear- and anxiety-related
behaviors. Dialogues Clin Neurosci. 4(3): 231–249.
Schmahmann, D. & Pandya, N. (2006). Fiber pathways of the brain. New York: Oxford
University Press, Oxford.
55
decline: results from Whitehall II prospective cohort study. Bmj. 344:d7622.
Seignourel, P., Kunik, M., Snow, L., Wilson, N. & Stanley. M. (2008). Anxiety in
dementia: A critical review. Clin Psychol Rev, 28(7):1071-1082
Schnitzspahn, M., Stahl, C., Zeintl, M., Kaller, P. & Kliegel, M. (2012). The role of
shifting, updating, and inhibition in prospective memory performance in young and older
adults. Developmental psychology. 2012.
Stern, Y. (2012). Cognitive reserve in ageing and Alzheimer’s disease. Lancet Neurol
11: 1006 12. doi: 10.1016/S1474-4422(12)70191-6
Schaub, T. & Linden, M. (2001). Anxiety and anxiety disorders in the old and very old –
results from the Berlin ageing Study. Comp Psychiatry 41: 48–54.
Shadlen, M. & Larson, E. (2010). Evaluation of cognitive impairment and dementia. In:
Basow D, ed. Waltham, MA: Steimer, T. (2002). The biology of fear- and anxiety-related
behaviors. Dialogues Clin Neurosci. 4(3): 231–249.
Schmahmann, D. & Pandya, N. (2006). Fiber pathways of the brain. New York: Oxford
University Press, Oxford.
55
Tiller, G. (2012). Depression and anxiety. MJA Open 2012; 1 Suppl 4: 28-31.
Thies, W. & Bleiler, L. (2013). Alzheimer’s disease facts and figures. Alzheimers Dement
9: 20845. doi: 10.1016/ j.jalz.2013.02.003
Therrien, Z. & Hunsley, J. (2011). Assessment of anxiety in older adults: A systematic
review of commonly used measures. Ageing & Mental Health 16(1): 1-6.
Turken, A., Whitfield-Gabrieli, S., Bammer, R. et al. (2008). Cognitive processing speed
and the structure of white matter pathways: convergent evidence from normal variation
and lesion studies. Neuroimage. 42(2): 1032–1044.
doi:10.1016/j.neuroimage.2008.03.057
Vincent, G. & Victoria, A. (2010). The next four decades, the older population in the
United States: 2010 to 2050. Washington, DC: U.S. Census Bureau; 2010.
Vink, D., Aartsen, M. & Schovers, A. (2008). Risk factors for anxiety and depression in
the elderly: A review. J AffDisord 106: 29–44.
Vogele C, von Leupoldt A. (2008). Mental disorders inchronic obstructive pulmonary
disease. Respir Med 102: 764–73.
56
Thies, W. & Bleiler, L. (2013). Alzheimer’s disease facts and figures. Alzheimers Dement
9: 20845. doi: 10.1016/ j.jalz.2013.02.003
Therrien, Z. & Hunsley, J. (2011). Assessment of anxiety in older adults: A systematic
review of commonly used measures. Ageing & Mental Health 16(1): 1-6.
Turken, A., Whitfield-Gabrieli, S., Bammer, R. et al. (2008). Cognitive processing speed
and the structure of white matter pathways: convergent evidence from normal variation
and lesion studies. Neuroimage. 42(2): 1032–1044.
doi:10.1016/j.neuroimage.2008.03.057
Vincent, G. & Victoria, A. (2010). The next four decades, the older population in the
United States: 2010 to 2050. Washington, DC: U.S. Census Bureau; 2010.
Vink, D., Aartsen, M. & Schovers, A. (2008). Risk factors for anxiety and depression in
the elderly: A review. J AffDisord 106: 29–44.
Vogele C, von Leupoldt A. (2008). Mental disorders inchronic obstructive pulmonary
disease. Respir Med 102: 764–73.
56
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Wecker, S., Kramer, H., Wisniewski, A., Delis, C. & Kaplan, E. (2000). Age effects on
executive ability. Neuropsychology. 14:409–14.
Witthöft, M., Mie, D., Ofer, J. et al. (2013). Neuronal and behavioral correlates of health
anxiety: results of an illness-related emotional stroop task. Neuropsychobiology 67:93–
102
Yates, W. (2015). Anxiety disorders. Medscape Reference.
http://emedicine.medscape.com/article/286227-overview#a2
Yochim, P., Mueller, A. & Segal, L. (2013). Late life anxiety is associated with
decreased memory and executive functioning in community dwelling older adults. J.
Anxiety. Disord 27(6), 567-575.
Zec, F., Markwell, J., Burkett, R. &, Larsen, L. (2005). A longitudinal study of
confrontation naming in the “normal” elderly. Journal of the International
Neuropsychological Society: JINS. 11:716–26.
Osterman, M., Vogels, L., van Harten, B. et al. (2010). Assessing mental flexibility:
neuroanatomical and neuropsychological correlates of the Trail Making Test in elderly
people. The Clinical Neuropsychologist.24:203–19.
57
executive ability. Neuropsychology. 14:409–14.
Witthöft, M., Mie, D., Ofer, J. et al. (2013). Neuronal and behavioral correlates of health
anxiety: results of an illness-related emotional stroop task. Neuropsychobiology 67:93–
102
Yates, W. (2015). Anxiety disorders. Medscape Reference.
http://emedicine.medscape.com/article/286227-overview#a2
Yochim, P., Mueller, A. & Segal, L. (2013). Late life anxiety is associated with
decreased memory and executive functioning in community dwelling older adults. J.
Anxiety. Disord 27(6), 567-575.
Zec, F., Markwell, J., Burkett, R. &, Larsen, L. (2005). A longitudinal study of
confrontation naming in the “normal” elderly. Journal of the International
Neuropsychological Society: JINS. 11:716–26.
Osterman, M., Vogels, L., van Harten, B. et al. (2010). Assessing mental flexibility:
neuroanatomical and neuropsychological correlates of the Trail Making Test in elderly
people. The Clinical Neuropsychologist.24:203–19.
57
Online
Besdine, R. (2017). Overview of ageing. Merck Manual: Consumer Version.
http://www.merckmanuals.com/home/older-people%E2%80%99s-health-issues/the-
ageing-body/overview-of-ageing
Korolev, I. (2014). Alzheimer’s disease: A clinical and basic science review
http://msrj.chm.msu.edu/wp-content/uploads/2014/12/Fall-2014-Alzheimers-Disease.pdf
National Institutes of Health (2016). Alzheimer's disease fact sheet.
https://www.nia.nih.gov/alzheimers/publication/alzheimers-disease-fact-sheet
58
Besdine, R. (2017). Overview of ageing. Merck Manual: Consumer Version.
http://www.merckmanuals.com/home/older-people%E2%80%99s-health-issues/the-
ageing-body/overview-of-ageing
Korolev, I. (2014). Alzheimer’s disease: A clinical and basic science review
http://msrj.chm.msu.edu/wp-content/uploads/2014/12/Fall-2014-Alzheimers-Disease.pdf
National Institutes of Health (2016). Alzheimer's disease fact sheet.
https://www.nia.nih.gov/alzheimers/publication/alzheimers-disease-fact-sheet
58
1 out of 60
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





