EBP Report: Antibiotic Therapy Effects on Necrotizing Enterocolitis
VerifiedAdded on 2023/04/11
|14
|1493
|282
Report
AI Summary
This report summarizes the evidence regarding the effects of antibiotic therapy on necrotizing enterocolitis (NEC) in neonates. It includes a table summarizing individual evidence from various studies, including systematic reviews, meta-analyses, retrospective cohort studies, and case reports. The studies examine the impact of antibiotic usage, the role of probiotics, and other interventions like pentoxifylline on NEC incidence, mortality, and associated complications. Limitations of the included studies, such as methodological issues, sample size limitations, and potential biases, are also discussed. The report also touches upon the current perspectives on antibiotic administration and the importance of considering anaerobic coverage. The report concludes by addressing the PICO question regarding the effectiveness of different parenteral antibiotics in preventing NEC progression and sequelae, emphasizing the importance of this issue due to the potential for severe outcomes like perforation, sepsis, and neonatal death if NEC is left untreated. Desklib provides access to similar solved assignments.

Running head: APPENDIX
Summary table
Name of the Student
Name of the University
Author Note
Summary table
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1APPENDIX
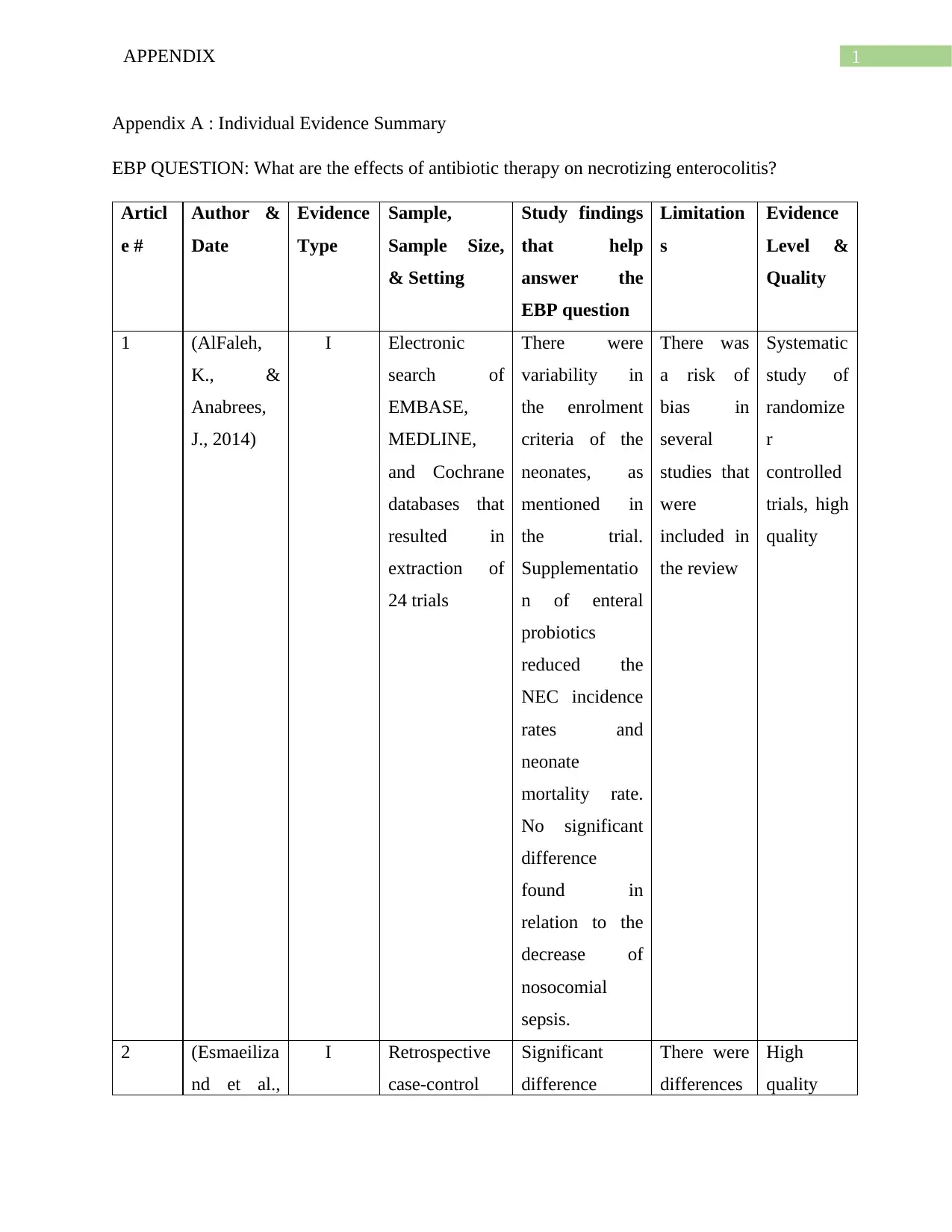
Appendix A : Individual Evidence Summary
EBP QUESTION: What are the effects of antibiotic therapy on necrotizing enterocolitis?
Articl
e #
Author &
Date
Evidence
Type
Sample,
Sample Size,
& Setting
Study findings
that help
answer the
EBP question
Limitation
s
Evidence
Level &
Quality
1 (AlFaleh,
K., &
Anabrees,
J., 2014)
I Electronic
search of
EMBASE,
MEDLINE,
and Cochrane
databases that
resulted in
extraction of
24 trials
There were
variability in
the enrolment
criteria of the
neonates, as
mentioned in
the trial.
Supplementatio
n of enteral
probiotics
reduced the
NEC incidence
rates and
neonate
mortality rate.
No significant
difference
found in
relation to the
decrease of
nosocomial
sepsis.
There was
a risk of
bias in
several
studies that
were
included in
the review
Systematic
study of
randomize
r
controlled
trials, high
quality
2 (Esmaeiliza
nd et al.,
I Retrospective
case-control
Significant
difference
There were
differences
High
quality
Appendix A : Individual Evidence Summary
EBP QUESTION: What are the effects of antibiotic therapy on necrotizing enterocolitis?
Articl
e #
Author &
Date
Evidence
Type
Sample,
Sample Size,
& Setting
Study findings
that help
answer the
EBP question
Limitation
s
Evidence
Level &
Quality
1 (AlFaleh,
K., &
Anabrees,
J., 2014)
I Electronic
search of
EMBASE,
MEDLINE,
and Cochrane
databases that
resulted in
extraction of
24 trials
There were
variability in
the enrolment
criteria of the
neonates, as
mentioned in
the trial.
Supplementatio
n of enteral
probiotics
reduced the
NEC incidence
rates and
neonate
mortality rate.
No significant
difference
found in
relation to the
decrease of
nosocomial
sepsis.
There was
a risk of
bias in
several
studies that
were
included in
the review
Systematic
study of
randomize
r
controlled
trials, high
quality
2 (Esmaeiliza
nd et al.,
I Retrospective
case-control
Significant
difference
There were
differences
High
quality
2APPENDIX
2017) study
conducted
among preterm
neonates born
prior to 29
week gestation
period. 447
controls and
224 cases.
observed in the
incidence rates
of antibiotic
day number
before NEC
onset, antenatal
steroid
administration,.
High duration
of antibiotic
usage found
among NEC
cases, in
comparison to
control.
Significant
increase in
NEC odds, in
relation to
empiric
treatment of
antibiotics for 5
days or more.
in clinical
practice
modalities
within and
between
centres.
The
researchers
failed to
obtain
detailed
information
on the kind
of feeding
and number
or type of
antibiotics
used.
since this
was an
experimen
tal study
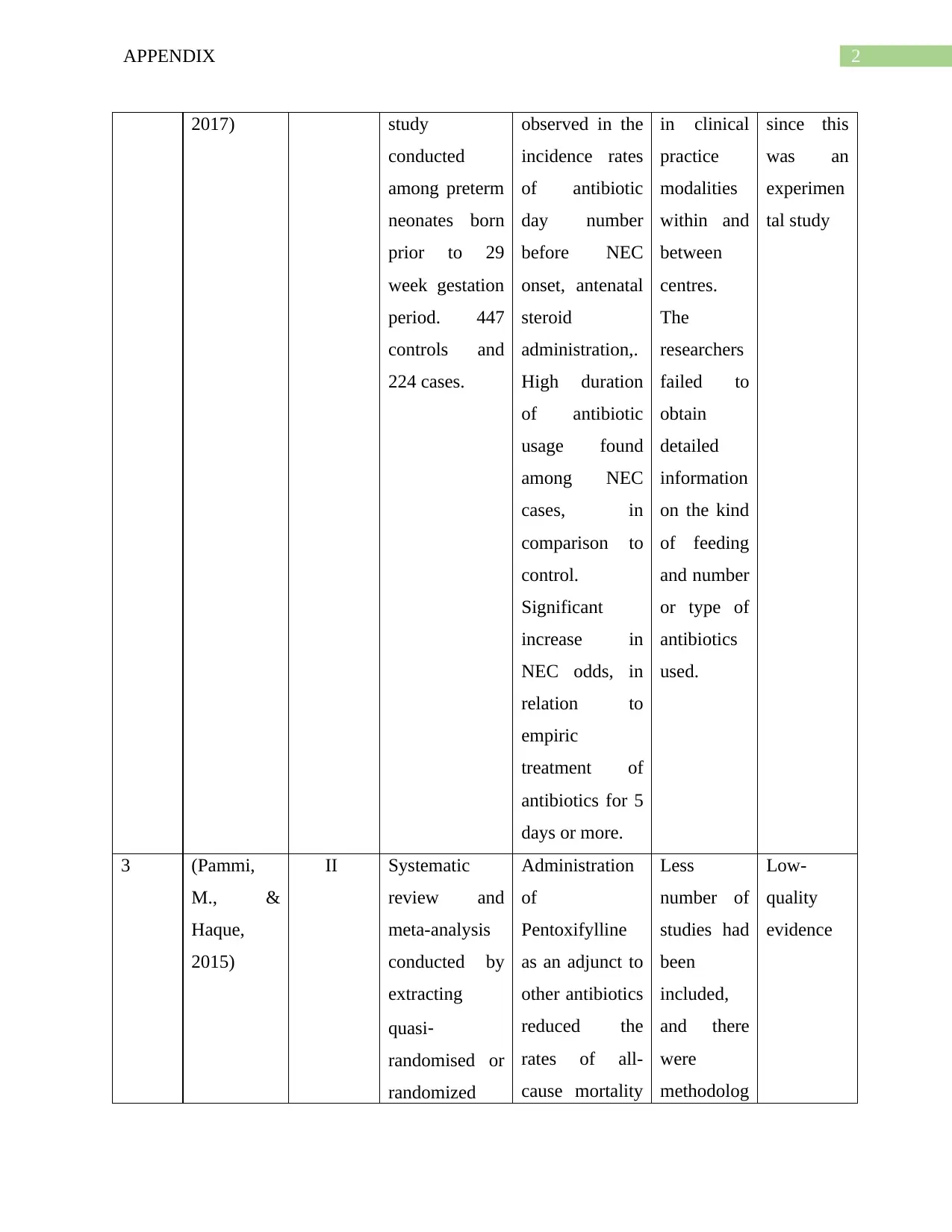
3 (Pammi,
M., &
Haque,
2015)
II Systematic
review and
meta-analysis
conducted by
extracting
quasi‐
randomised or
randomized
Administration
of
Pentoxifylline
as an adjunct to
other antibiotics
reduced the
rates of all-
cause mortality
Less
number of
studies had
been
included,
and there
were
methodolog
Low-
quality
evidence
2017) study
conducted
among preterm
neonates born
prior to 29
week gestation
period. 447
controls and
224 cases.
observed in the
incidence rates
of antibiotic
day number
before NEC
onset, antenatal
steroid
administration,.
High duration
of antibiotic
usage found
among NEC
cases, in
comparison to
control.
Significant
increase in
NEC odds, in
relation to
empiric
treatment of
antibiotics for 5
days or more.
in clinical
practice
modalities
within and
between
centres.
The
researchers
failed to
obtain
detailed
information
on the kind
of feeding
and number
or type of
antibiotics
used.
since this
was an
experimen
tal study
3 (Pammi,
M., &
Haque,
2015)
II Systematic
review and
meta-analysis
conducted by
extracting
quasi‐
randomised or
randomized
Administration
of
Pentoxifylline
as an adjunct to
other antibiotics
reduced the
rates of all-
cause mortality
Less
number of
studies had
been
included,
and there
were
methodolog
Low-
quality
evidence
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3APPENDIX
trials from
electronic
databases such
as, Pubmed,
EMBASE,
CINAHL,
CENTRAL,
and Cochrane
Neonatal
Review Group
Specialized
Register.
among
neonates,
during their
length of
hospitalization.
Pentoxifylline
also decreased
hospital stay.
However, it did
not have any
significant
impact on
retinopathy of
prematurity,
chronic lung
disease,
development of
NEC, or
periventricular
leukomalacia or
severe
intraventricular
haemorrhag, in
neonates
ical
limitations
in each of
them.
4 (Samuels et
al., 2016)
II A quasi-
experimental
study was
performed
among level IV
NICU located
in Rotterdam
Interrupted time
series logistic
regression
analysis failed
to demonstrate
any noteworthy
difference
Observatio
nal design
prevented
random
allocation
of infants.
Confidence
Good
quality
evidence
trials from
electronic
databases such
as, Pubmed,
EMBASE,
CINAHL,
CENTRAL,
and Cochrane
Neonatal
Review Group
Specialized
Register.
among
neonates,
during their
length of
hospitalization.
Pentoxifylline
also decreased
hospital stay.
However, it did
not have any
significant
impact on
retinopathy of
prematurity,
chronic lung
disease,
development of
NEC, or
periventricular
leukomalacia or
severe
intraventricular
haemorrhag, in
neonates
ical
limitations
in each of
them.
4 (Samuels et
al., 2016)
II A quasi-
experimental
study was
performed
among level IV
NICU located
in Rotterdam
Interrupted time
series logistic
regression
analysis failed
to demonstrate
any noteworthy
difference
Observatio
nal design
prevented
random
allocation
of infants.
Confidence
Good
quality
evidence
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4APPENDIX
and comprised
of two groups,
based on
probiotic
introduction
before birth
(October 1,
2012-January
1, 2015) and
after birth
(January 1,
2008-October
1, 2012)
between the
death rates or
NEC rates
among the two
infant groups.
General
incidence of
NEC showed a
reduction from
7.8-5.1% (OR
0.63, 95% CI
0.42–0.93, p =
0.02) that was
not statistically
prominent to
the adjusted
models used.
Probiotic
introduction
was allied with
decline in the
NEC or death
or sepsis
adjusted odds
among infant
who were fed
breast milk
(OR 0.43, 95%
CI 0.21–0.93, p
= 0.03)
interval
could have
been
narrowed
using a
large
sample
size.
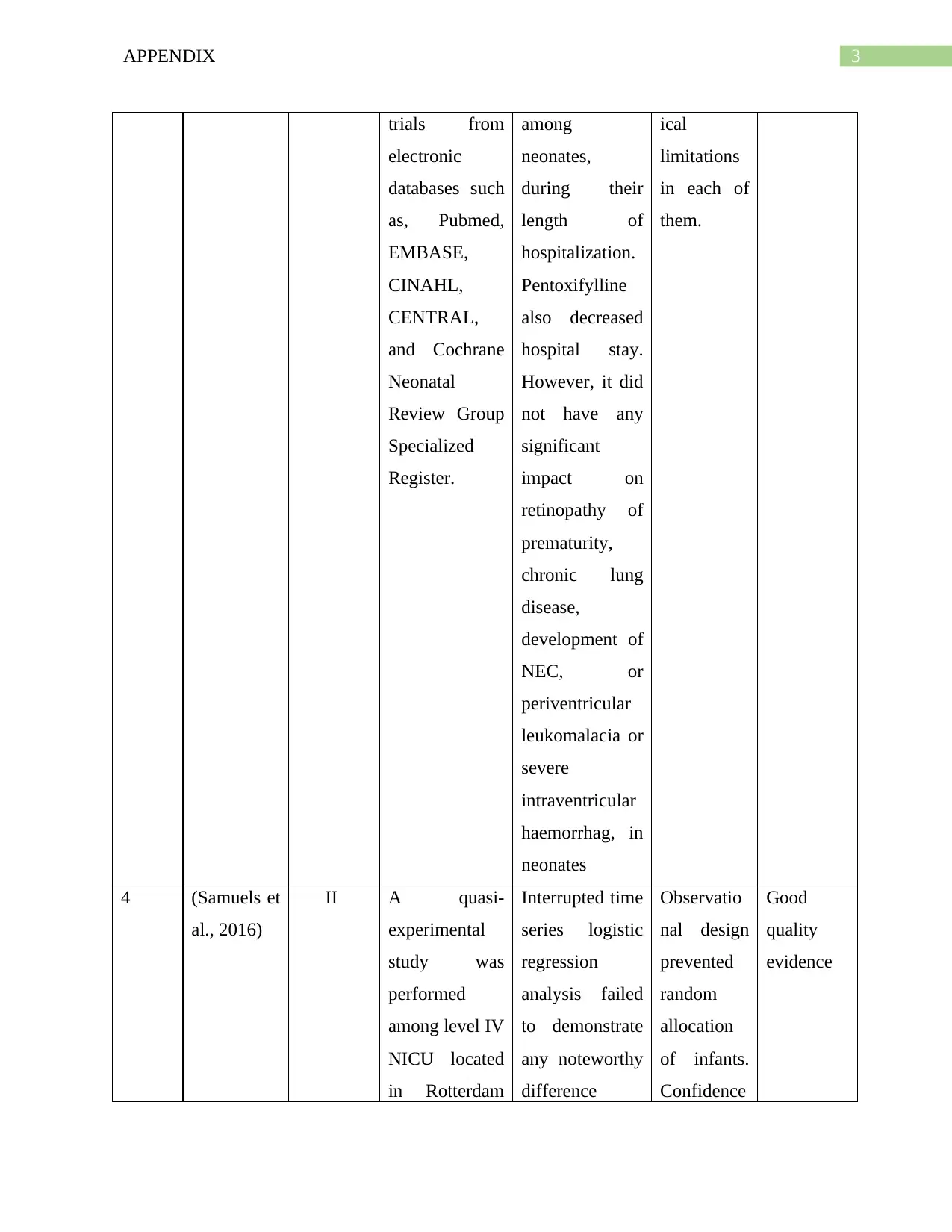
5 (Ting et al., III Retrospective 11 669 Researcher Non-
and comprised
of two groups,
based on
probiotic
introduction
before birth
(October 1,
2012-January
1, 2015) and
after birth
(January 1,
2008-October
1, 2012)
between the
death rates or
NEC rates
among the two
infant groups.
General
incidence of
NEC showed a
reduction from
7.8-5.1% (OR
0.63, 95% CI
0.42–0.93, p =
0.02) that was
not statistically
prominent to
the adjusted
models used.
Probiotic
introduction
was allied with
decline in the
NEC or death
or sepsis
adjusted odds
among infant
who were fed
breast milk
(OR 0.43, 95%
CI 0.21–0.93, p
= 0.03)
interval
could have
been
narrowed
using a
large
sample
size.
5 (Ting et al., III Retrospective 11 669 Researcher Non-
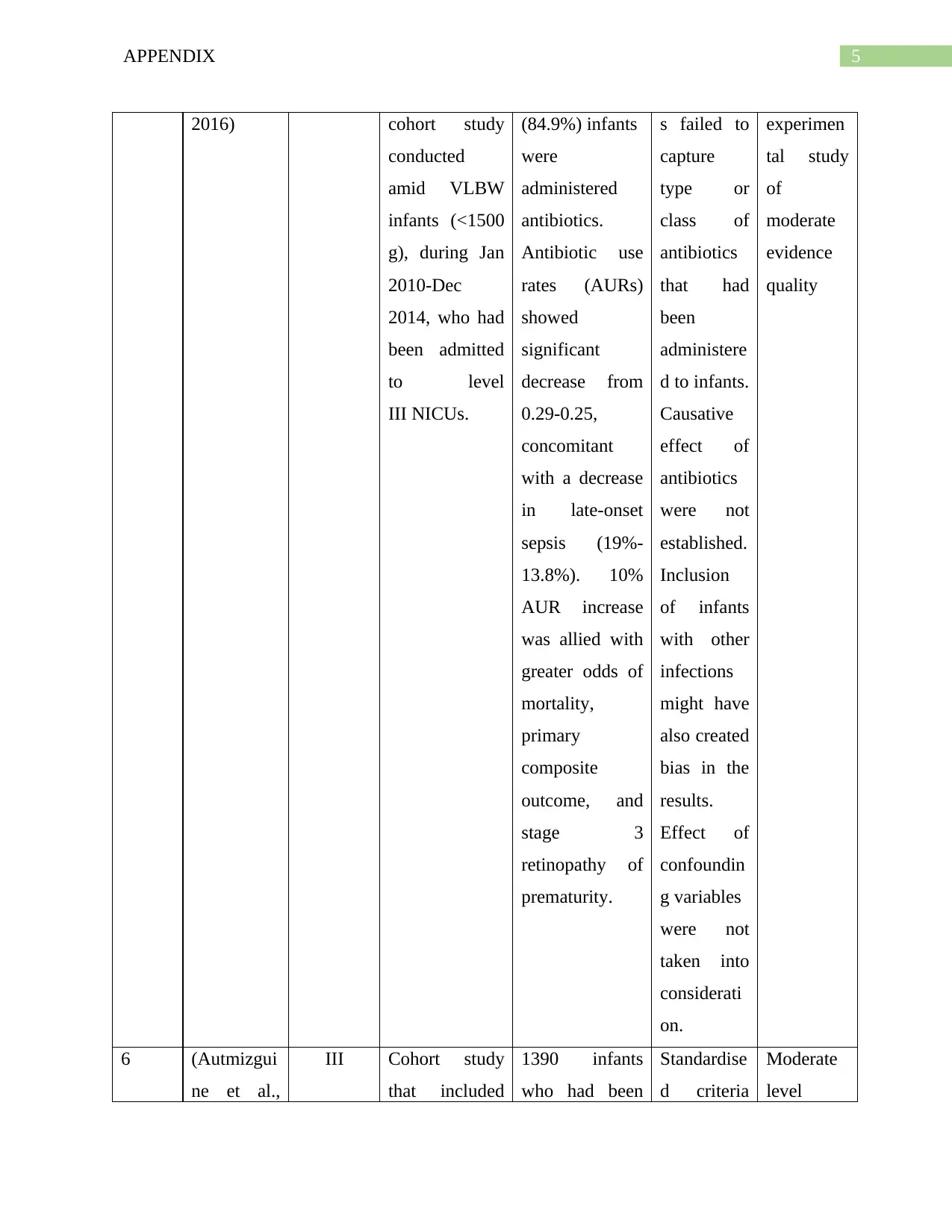
5APPENDIX
2016) cohort study
conducted
amid VLBW
infants (<1500
g), during Jan
2010-Dec
2014, who had
been admitted
to level
III NICUs.
(84.9%) infants
were
administered
antibiotics.
Antibiotic use
rates (AURs)
showed
significant
decrease from
0.29-0.25,
concomitant
with a decrease
in late-onset
sepsis (19%-
13.8%). 10%
AUR increase
was allied with
greater odds of
mortality,
primary
composite
outcome, and
stage 3
retinopathy of
prematurity.
s failed to
capture
type or
class of
antibiotics
that had
been
administere
d to infants.
Causative
effect of
antibiotics
were not
established.
Inclusion
of infants
with other
infections
might have
also created
bias in the
results.
Effect of
confoundin
g variables
were not
taken into
considerati
on.
experimen
tal study
of
moderate
evidence
quality
6 (Autmizgui
ne et al.,
III Cohort study
that included
1390 infants
who had been
Standardise
d criteria
Moderate
level
2016) cohort study
conducted
amid VLBW
infants (<1500
g), during Jan
2010-Dec
2014, who had
been admitted
to level
III NICUs.
(84.9%) infants
were
administered
antibiotics.
Antibiotic use
rates (AURs)
showed
significant
decrease from
0.29-0.25,
concomitant
with a decrease
in late-onset
sepsis (19%-
13.8%). 10%
AUR increase
was allied with
greater odds of
mortality,
primary
composite
outcome, and
stage 3
retinopathy of
prematurity.
s failed to
capture
type or
class of
antibiotics
that had
been
administere
d to infants.
Causative
effect of
antibiotics
were not
established.
Inclusion
of infants
with other
infections
might have
also created
bias in the
results.
Effect of
confoundin
g variables
were not
taken into
considerati
on.
experimen
tal study
of
moderate
evidence
quality
6 (Autmizgui
ne et al.,
III Cohort study
that included
1390 infants
who had been
Standardise
d criteria
Moderate
level
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
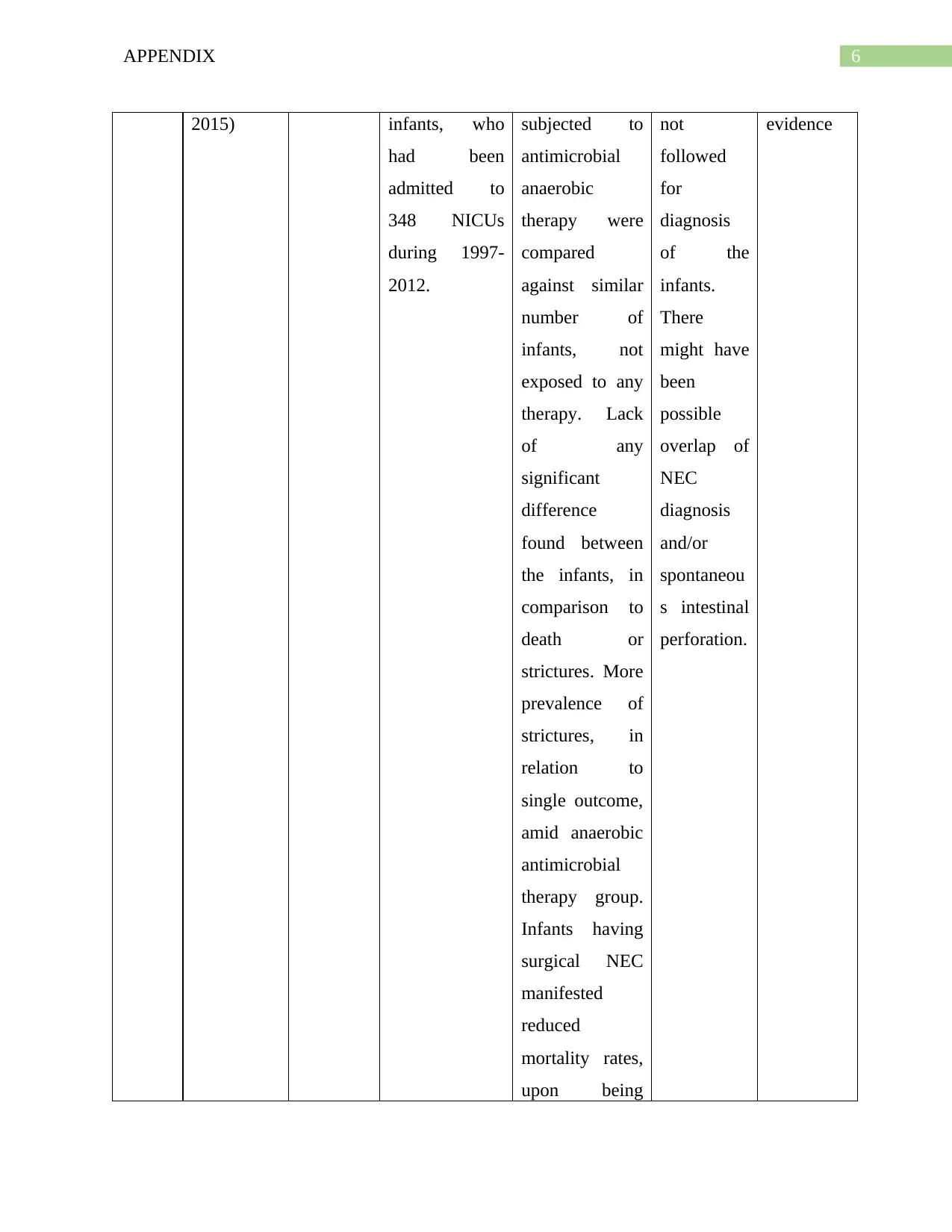
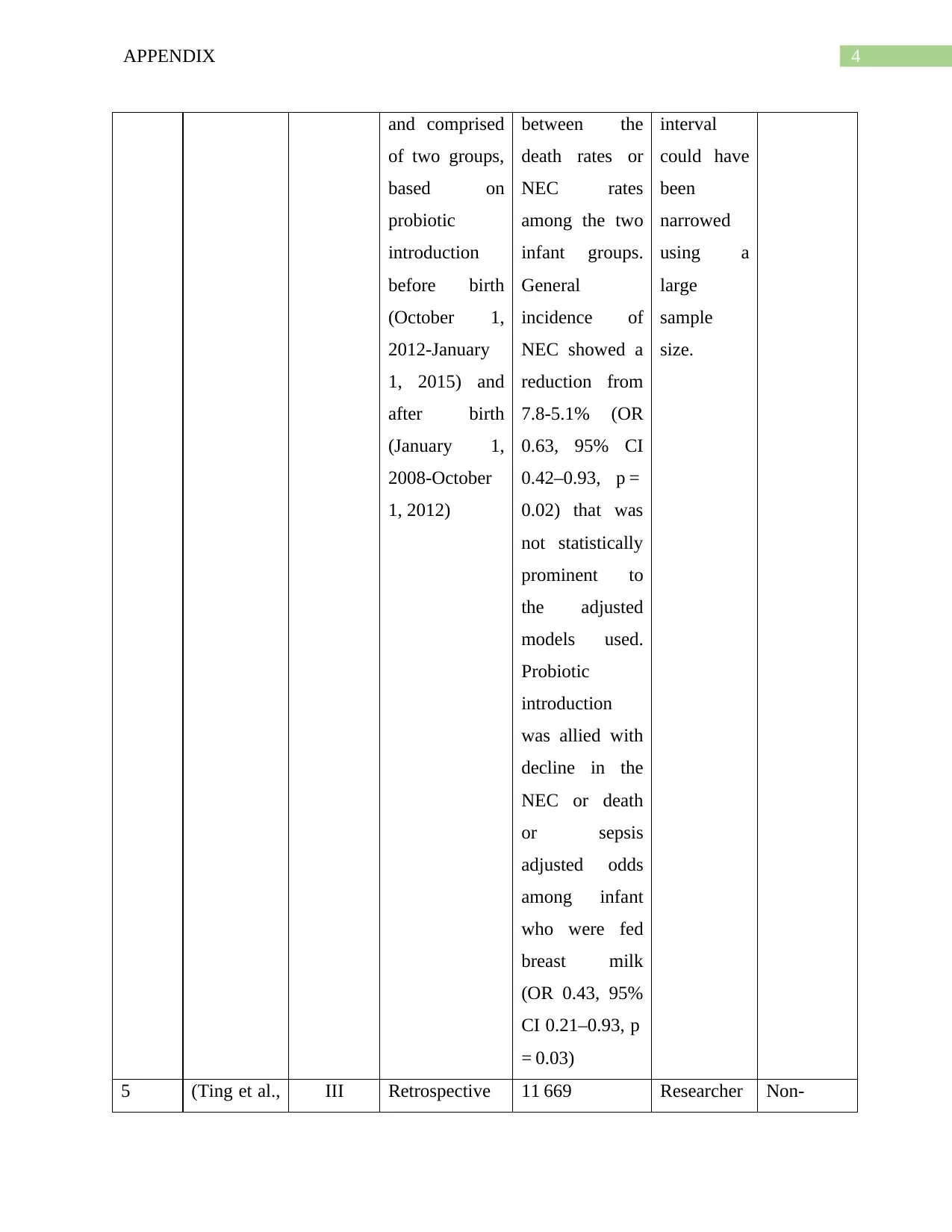
6APPENDIX
2015) infants, who
had been
admitted to
348 NICUs
during 1997-
2012.
subjected to
antimicrobial
anaerobic
therapy were
compared
against similar
number of
infants, not
exposed to any
therapy. Lack
of any
significant
difference
found between
the infants, in
comparison to
death or
strictures. More
prevalence of
strictures, in
relation to
single outcome,
amid anaerobic
antimicrobial
therapy group.
Infants having
surgical NEC
manifested
reduced
mortality rates,
upon being
not
followed
for
diagnosis
of the
infants.
There
might have
been
possible
overlap of
NEC
diagnosis
and/or
spontaneou
s intestinal
perforation.
evidence
2015) infants, who
had been
admitted to
348 NICUs
during 1997-
2012.
subjected to
antimicrobial
anaerobic
therapy were
compared
against similar
number of
infants, not
exposed to any
therapy. Lack
of any
significant
difference
found between
the infants, in
comparison to
death or
strictures. More
prevalence of
strictures, in
relation to
single outcome,
amid anaerobic
antimicrobial
therapy group.
Infants having
surgical NEC
manifested
reduced
mortality rates,
upon being
not
followed
for
diagnosis
of the
infants.
There
might have
been
possible
overlap of
NEC
diagnosis
and/or
spontaneou
s intestinal
perforation.
evidence
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7APPENDIX
subjected to
antimicrobial
therapy.
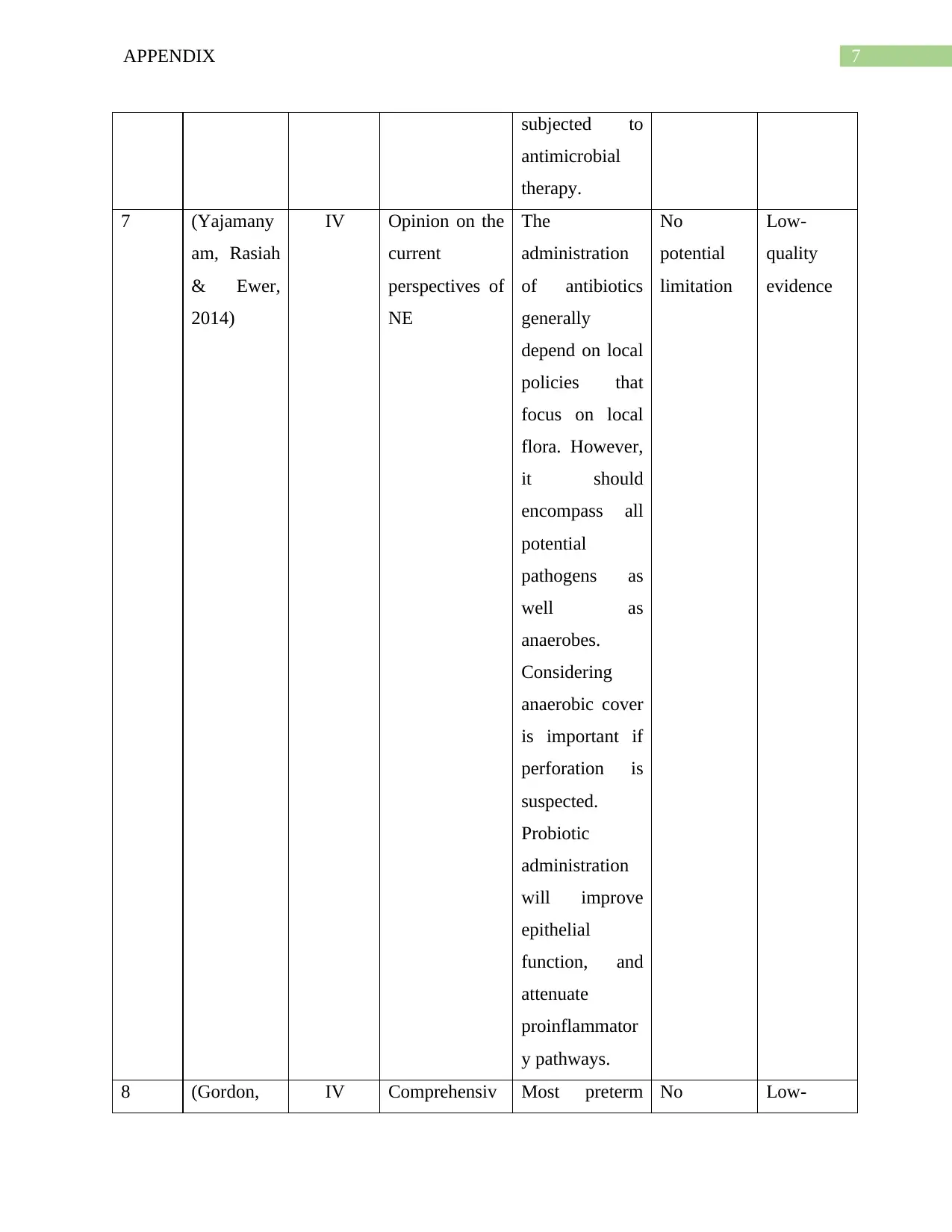
7 (Yajamany
am, Rasiah
& Ewer,
2014)
IV Opinion on the
current
perspectives of
NE
The
administration
of antibiotics
generally
depend on local
policies that
focus on local
flora. However,
it should
encompass all
potential
pathogens as
well as
anaerobes.
Considering
anaerobic cover
is important if
perforation is
suspected.
Probiotic
administration
will improve
epithelial
function, and
attenuate
proinflammator
y pathways.
No
potential
limitation
Low-
quality
evidence
8 (Gordon, IV Comprehensiv Most preterm No Low-
subjected to
antimicrobial
therapy.
7 (Yajamany
am, Rasiah
& Ewer,
2014)
IV Opinion on the
current
perspectives of
NE
The
administration
of antibiotics
generally
depend on local
policies that
focus on local
flora. However,
it should
encompass all
potential
pathogens as
well as
anaerobes.
Considering
anaerobic cover
is important if
perforation is
suspected.
Probiotic
administration
will improve
epithelial
function, and
attenuate
proinflammator
y pathways.
No
potential
limitation
Low-
quality
evidence
8 (Gordon, IV Comprehensiv Most preterm No Low-
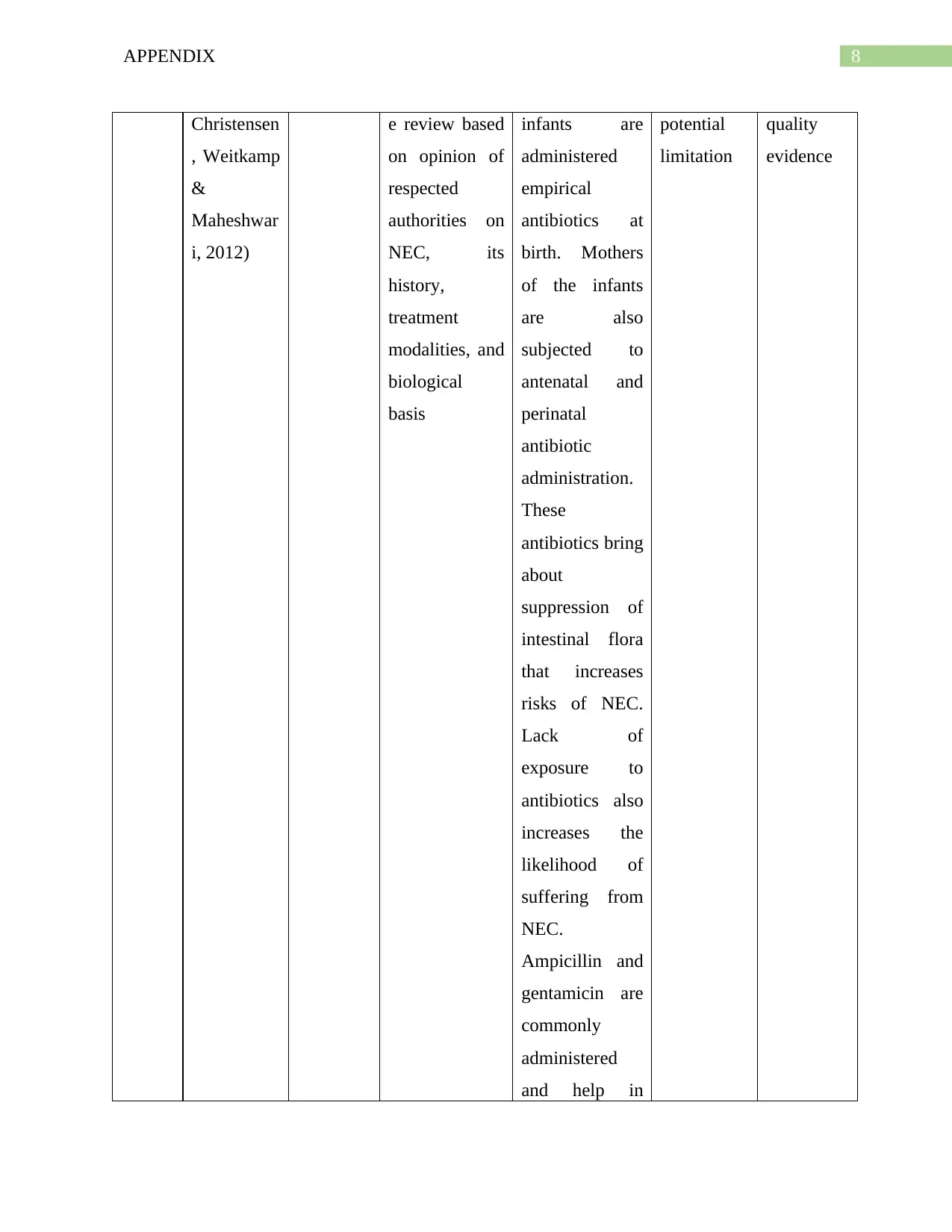
8APPENDIX
Christensen
, Weitkamp
&
Maheshwar
i, 2012)
e review based
on opinion of
respected
authorities on
NEC, its
history,
treatment
modalities, and
biological
basis
infants are
administered
empirical
antibiotics at
birth. Mothers
of the infants
are also
subjected to
antenatal and
perinatal
antibiotic
administration.
These
antibiotics bring
about
suppression of
intestinal flora
that increases
risks of NEC.
Lack of
exposure to
antibiotics also
increases the
likelihood of
suffering from
NEC.
Ampicillin and
gentamicin are
commonly
administered
and help in
potential
limitation
quality
evidence
Christensen
, Weitkamp
&
Maheshwar
i, 2012)
e review based
on opinion of
respected
authorities on
NEC, its
history,
treatment
modalities, and
biological
basis
infants are
administered
empirical
antibiotics at
birth. Mothers
of the infants
are also
subjected to
antenatal and
perinatal
antibiotic
administration.
These
antibiotics bring
about
suppression of
intestinal flora
that increases
risks of NEC.
Lack of
exposure to
antibiotics also
increases the
likelihood of
suffering from
NEC.
Ampicillin and
gentamicin are
commonly
administered
and help in
potential
limitation
quality
evidence
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9APPENDIX
reducing NEC
by as much as
10 times.
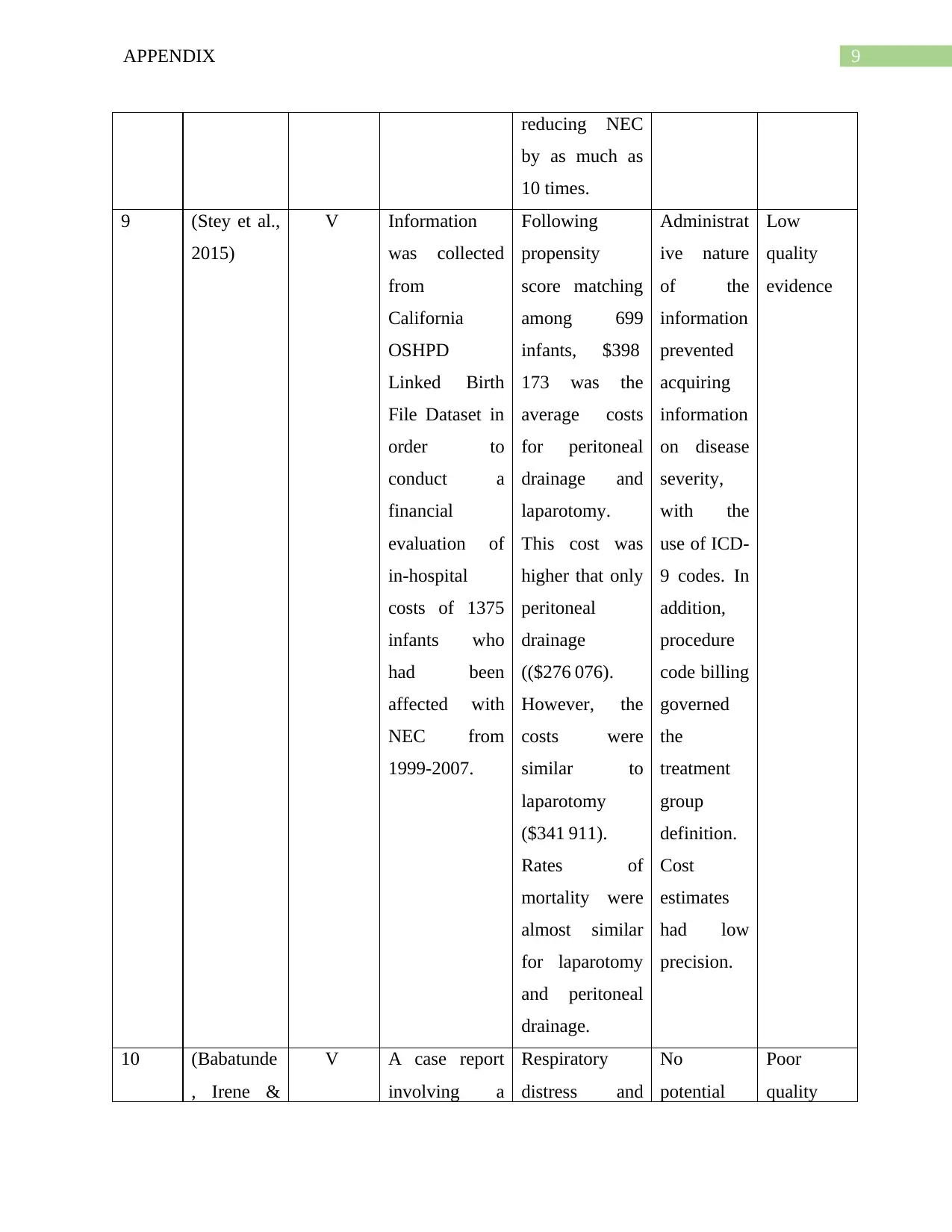
9 (Stey et al.,
2015)
V Information
was collected
from
California
OSHPD
Linked Birth
File Dataset in
order to
conduct a
financial
evaluation of
in-hospital
costs of 1375
infants who
had been
affected with
NEC from
1999-2007.
Following
propensity
score matching
among 699
infants, $398
173 was the
average costs
for peritoneal
drainage and
laparotomy.
This cost was
higher that only
peritoneal
drainage
(($276 076).
However, the
costs were
similar to
laparotomy
($341 911).
Rates of
mortality were
almost similar
for laparotomy
and peritoneal
drainage.
Administrat
ive nature
of the
information
prevented
acquiring
information
on disease
severity,
with the
use of ICD-
9 codes. In
addition,
procedure
code billing
governed
the
treatment
group
definition.
Cost
estimates
had low
precision.
Low
quality
evidence
10 (Babatunde
, Irene &
V A case report
involving a
Respiratory
distress and
No
potential
Poor
quality
reducing NEC
by as much as
10 times.
9 (Stey et al.,
2015)
V Information
was collected
from
California
OSHPD
Linked Birth
File Dataset in
order to
conduct a
financial
evaluation of
in-hospital
costs of 1375
infants who
had been
affected with
NEC from
1999-2007.
Following
propensity
score matching
among 699
infants, $398
173 was the
average costs
for peritoneal
drainage and
laparotomy.
This cost was
higher that only
peritoneal
drainage
(($276 076).
However, the
costs were
similar to
laparotomy
($341 911).
Rates of
mortality were
almost similar
for laparotomy
and peritoneal
drainage.
Administrat
ive nature
of the
information
prevented
acquiring
information
on disease
severity,
with the
use of ICD-
9 codes. In
addition,
procedure
code billing
governed
the
treatment
group
definition.
Cost
estimates
had low
precision.
Low
quality
evidence
10 (Babatunde
, Irene &
V A case report
involving a
Respiratory
distress and
No
potential
Poor
quality
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
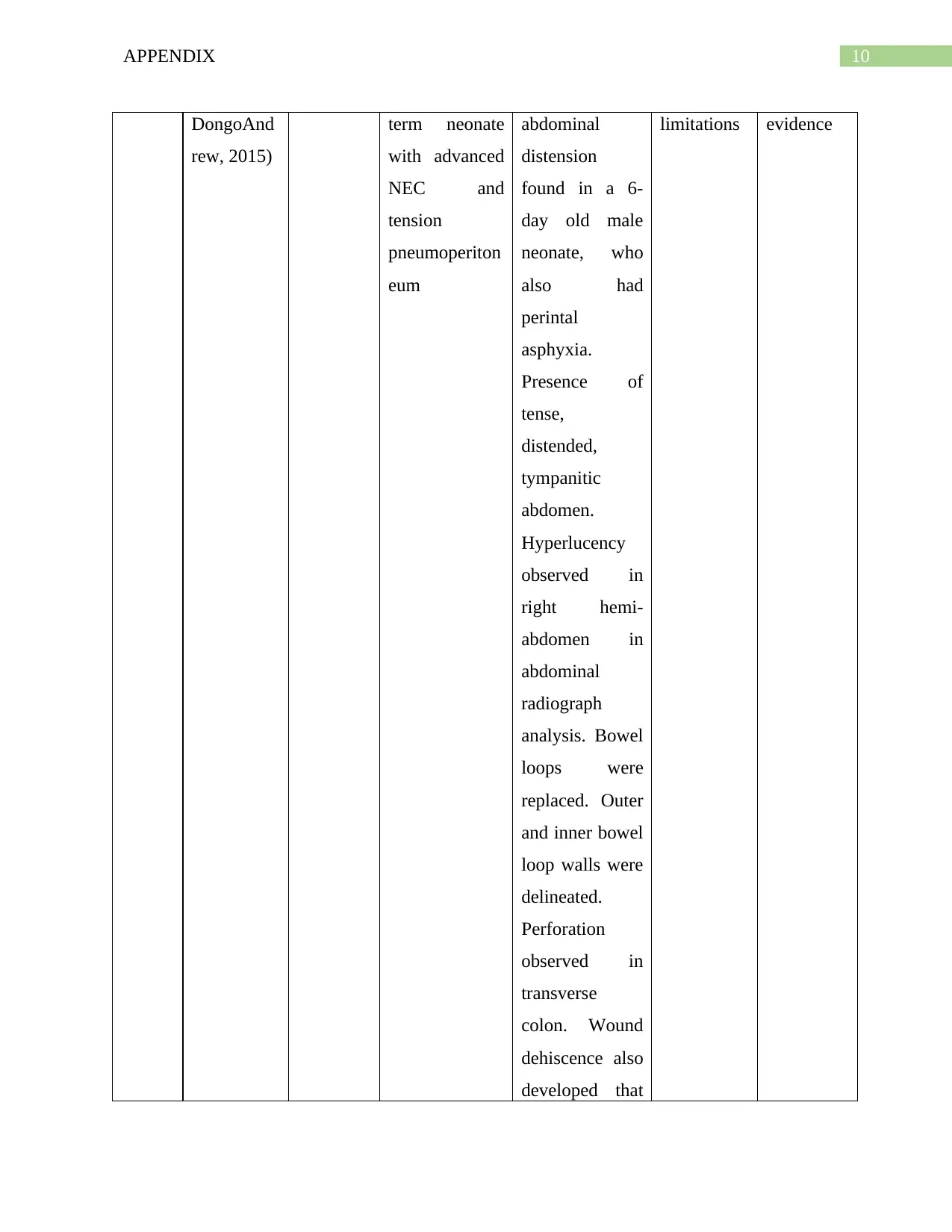
10APPENDIX
DongoAnd
rew, 2015)
term neonate
with advanced
NEC and
tension
pneumoperiton
eum
abdominal
distension
found in a 6-
day old male
neonate, who
also had
perintal
asphyxia.
Presence of
tense,
distended,
tympanitic
abdomen.
Hyperlucency
observed in
right hemi-
abdomen in
abdominal
radiograph
analysis. Bowel
loops were
replaced. Outer
and inner bowel
loop walls were
delineated.
Perforation
observed in
transverse
colon. Wound
dehiscence also
developed that
limitations evidence
DongoAnd
rew, 2015)
term neonate
with advanced
NEC and
tension
pneumoperiton
eum
abdominal
distension
found in a 6-
day old male
neonate, who
also had
perintal
asphyxia.
Presence of
tense,
distended,
tympanitic
abdomen.
Hyperlucency
observed in
right hemi-
abdomen in
abdominal
radiograph
analysis. Bowel
loops were
replaced. Outer
and inner bowel
loop walls were
delineated.
Perforation
observed in
transverse
colon. Wound
dehiscence also
developed that
limitations evidence
11APPENDIX
needed
secondary
closure
needed
secondary
closure
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





