Applied Pathophysiology Assignment Report
VerifiedAdded on 2022/08/14
|10
|2490
|13
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running Head: APPLIED PATHOPHYSIOLOGY
APPLIED PATHOPHYSIOLOGY
Name of the Student
Name of the University
Author’s Note
APPLIED PATHOPHYSIOLOGY
Name of the Student
Name of the University
Author’s Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1APPLIED PATHOPHYSIOLOGY
Introduction
Carly is a 12 year old girl suffering from diabetic ketoacidosis (DKA) and is going to be
discussed in detail in this paper. She was taken to the emergency ward for her health condition as
she had symptoms of fever, polydipsia and polyuria. Her complaints were that she was suffering
from nausea and abdominal pain during the time of admission. She was diagnosed after her
admission, which gave the result that she had tachycardia. She also has orthostatic hypotension.
During her stay she was observed for three to four hours, which showed her gradual biochemical
and clinical improvement. Her neurological deterioration was noticed after six hours to her
treatment and resuscitation (Cameron et al., 2014). After a while she was given Mannitol. Her
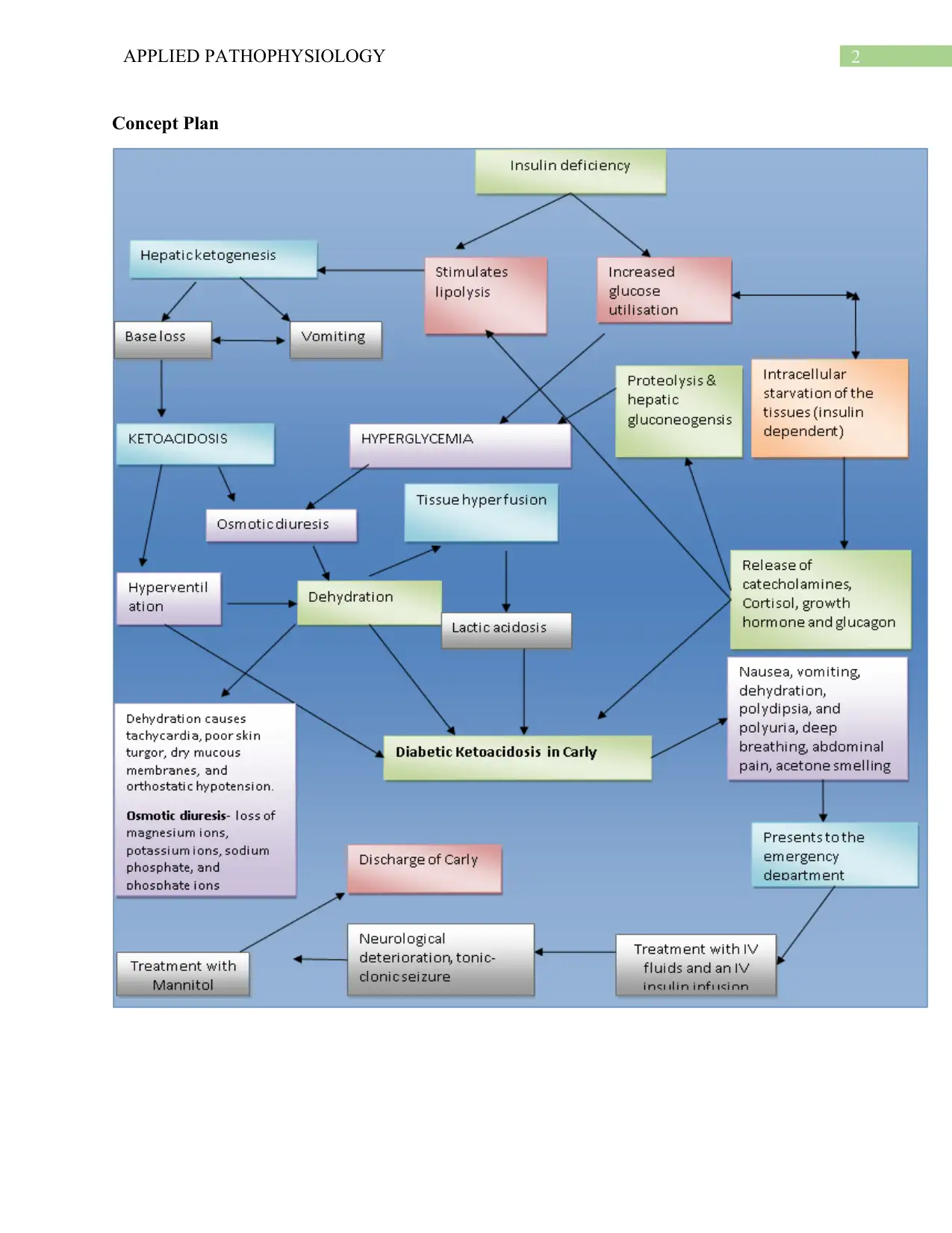
improvement in GCS was observed, which was the reason for her discharge. This paper has a
concept map that is linked to case study and it consists of the processes of the pathophysiology
of the disease Carly is suffering from. The paper also explains the disease in detail including its
pathophysiology and gives reasons for the alterations in the vital signs of the patient when she
was taken to the emergency department.
Introduction
Carly is a 12 year old girl suffering from diabetic ketoacidosis (DKA) and is going to be
discussed in detail in this paper. She was taken to the emergency ward for her health condition as
she had symptoms of fever, polydipsia and polyuria. Her complaints were that she was suffering
from nausea and abdominal pain during the time of admission. She was diagnosed after her
admission, which gave the result that she had tachycardia. She also has orthostatic hypotension.
During her stay she was observed for three to four hours, which showed her gradual biochemical
and clinical improvement. Her neurological deterioration was noticed after six hours to her
treatment and resuscitation (Cameron et al., 2014). After a while she was given Mannitol. Her
improvement in GCS was observed, which was the reason for her discharge. This paper has a
concept map that is linked to case study and it consists of the processes of the pathophysiology
of the disease Carly is suffering from. The paper also explains the disease in detail including its
pathophysiology and gives reasons for the alterations in the vital signs of the patient when she
was taken to the emergency department.
2APPLIED PATHOPHYSIOLOGY
Concept Plan
Concept Plan
3APPLIED PATHOPHYSIOLOGY
Pathophysiology
DKA is a health complication in which the bicarbonate serum has a concentration of less
than 15 mmol/L, including blood glucose that is more than 200 mg/dl, venous pH is more than
7.3, same with ketonemia, glucosuria and ketonuria. The study of pathophysiology has
disorganized physiological events happening inside the body because of any acute or chronic
disease. It is a collaboration of pathology and physiology that supports in explaining the
complications seen during the disease. This part of the paper will deal with the pathophysiology
of DKA as Carly is suffering from the same.
The major reason for diabetic ketoacidosis is insulin deficiency that leads to intracellular
starvation of the tissues that are insulin dependent. Growth hormones like glucagon,
catecholamines, and cortisol are released to increase the secretion of lipolysis, ketone bodies,
glucose and proteolysis. However, these bodies are only processed during physiologic fasting
(Nyenwe & Kitabchi, 2016).
The blood glucose regulation is due to the outcome of the above process as it mostly
happens with the help of insulin. The renal glucose and hepatic production is increased during
the absence of insulin, which leads to decrease in the level of peripheral glucose and the
peripheral fat character is prevented by this action. The glycogen synthesis is stimulated in the
presence of insulin when the hepatic gluconeogenesis is turned off. This happens during normal
fasting to some extent. However, the usual response to fasting is exaggerated in the case of
insulin depletion and it also increases glucose production in the liver (Srinivas, 2016).
Gluconeogenesis is the process that occurs when the same thing happens with protein and fat.
Glycogenolysis is the process in which liver glycogen breakdown occurs. Thus, inhibition of
peripheral glucose release happens and it is followed by different metabolic issues.
Pathophysiology
DKA is a health complication in which the bicarbonate serum has a concentration of less
than 15 mmol/L, including blood glucose that is more than 200 mg/dl, venous pH is more than
7.3, same with ketonemia, glucosuria and ketonuria. The study of pathophysiology has
disorganized physiological events happening inside the body because of any acute or chronic
disease. It is a collaboration of pathology and physiology that supports in explaining the
complications seen during the disease. This part of the paper will deal with the pathophysiology
of DKA as Carly is suffering from the same.
The major reason for diabetic ketoacidosis is insulin deficiency that leads to intracellular
starvation of the tissues that are insulin dependent. Growth hormones like glucagon,
catecholamines, and cortisol are released to increase the secretion of lipolysis, ketone bodies,
glucose and proteolysis. However, these bodies are only processed during physiologic fasting
(Nyenwe & Kitabchi, 2016).
The blood glucose regulation is due to the outcome of the above process as it mostly
happens with the help of insulin. The renal glucose and hepatic production is increased during
the absence of insulin, which leads to decrease in the level of peripheral glucose and the
peripheral fat character is prevented by this action. The glycogen synthesis is stimulated in the
presence of insulin when the hepatic gluconeogenesis is turned off. This happens during normal
fasting to some extent. However, the usual response to fasting is exaggerated in the case of
insulin depletion and it also increases glucose production in the liver (Srinivas, 2016).
Gluconeogenesis is the process that occurs when the same thing happens with protein and fat.
Glycogenolysis is the process in which liver glycogen breakdown occurs. Thus, inhibition of
peripheral glucose release happens and it is followed by different metabolic issues.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4APPLIED PATHOPHYSIOLOGY
Hepatic ketogenesis occurs due to lipolysis that happens due to insulin deficiency and it
is the reason for base loss that is the deficit of sodium and potassium, acidosis and vomiting.
Ketoacidosis is accelerated because of base loss, which happens due to the increase in ketone
bodies. Ketoacidosis has two outcomes that is hyperventilation and osmotic diuresis, which
causes lactic acidosis, dehydration and tissue perfusion. Hyperglycemia is caused due to insulin
deficiency that causes glucose utilization, and hormone production such as catecholamines,
cortisol, glucagon and growth hormones is the reason for the increase of hepatic gluconeogenesis
and proteolysis. The uptake of peripheral glucose gets impaired because of osmotic diuresis due
to the process of hyperglycemia. The residual insulin synthesis gets hampers due to this process
as well (Watts & Edge, 2014).
The whole phenomena explained above is the reason for the serum glucose to be 48
mmol/L in Carly’s vital signs as she had increased levels of β-hydroxybutyrate (β-HBO), which
were 1.9 mmol/L. Diabetic Ketoacidosis treatment makes the CSF show some changes in the
acid-base status (Kamel & Halperin, 2015). The pH of CSF decreases without the administration
of bicarbonate. The result of the respiratory responses takes a fall and the decrease in CSF pH
happens due to the increase in Pco2. The pH of arterial blood gas is 7.06 and 10 mmHg of
PaCO2 occurred due to this phenomena.
Diabetic ketoacidosis has few symptoms such as vomiting, nausea, polydipsia, and
polyuria. Polydipsia is a complication in which excessive thirst is seen with polyuria as
dehydration is the major reason for this complication. Vomiting and hyperventilation also
contributes to this condition. Carly has complains of polydipsia and hyperventilation, which
occurred due to ketoacidosis. Decreased kidney perfusion causes polyuria that increases the
stimulation of angiotensin and rennin that signals the brain for excessive thirst. Eventually,
Hepatic ketogenesis occurs due to lipolysis that happens due to insulin deficiency and it
is the reason for base loss that is the deficit of sodium and potassium, acidosis and vomiting.
Ketoacidosis is accelerated because of base loss, which happens due to the increase in ketone
bodies. Ketoacidosis has two outcomes that is hyperventilation and osmotic diuresis, which
causes lactic acidosis, dehydration and tissue perfusion. Hyperglycemia is caused due to insulin
deficiency that causes glucose utilization, and hormone production such as catecholamines,
cortisol, glucagon and growth hormones is the reason for the increase of hepatic gluconeogenesis
and proteolysis. The uptake of peripheral glucose gets impaired because of osmotic diuresis due
to the process of hyperglycemia. The residual insulin synthesis gets hampers due to this process
as well (Watts & Edge, 2014).
The whole phenomena explained above is the reason for the serum glucose to be 48
mmol/L in Carly’s vital signs as she had increased levels of β-hydroxybutyrate (β-HBO), which
were 1.9 mmol/L. Diabetic Ketoacidosis treatment makes the CSF show some changes in the
acid-base status (Kamel & Halperin, 2015). The pH of CSF decreases without the administration
of bicarbonate. The result of the respiratory responses takes a fall and the decrease in CSF pH
happens due to the increase in Pco2. The pH of arterial blood gas is 7.06 and 10 mmHg of
PaCO2 occurred due to this phenomena.
Diabetic ketoacidosis has few symptoms such as vomiting, nausea, polydipsia, and
polyuria. Polydipsia is a complication in which excessive thirst is seen with polyuria as
dehydration is the major reason for this complication. Vomiting and hyperventilation also
contributes to this condition. Carly has complains of polydipsia and hyperventilation, which
occurred due to ketoacidosis. Decreased kidney perfusion causes polyuria that increases the
stimulation of angiotensin and rennin that signals the brain for excessive thirst. Eventually,
5APPLIED PATHOPHYSIOLOGY
osmotic diuresis occurs when the glucose increases to a threshold of the renal glucose absorption
and due to osmotic diuresis an excess amount of water is lost (Shah et al., 2017). Dehydration
due to osmotic diuresis results to a loss of potassium ions, phosphate ions, magnesium ions and
sodium phosphate. However, sodium serum can be increased in patients who has a rise in
osmotic diuresis including poor fluid compensation. Carly’s condition with serum sodium being
128 mmol/L, serum potassium being 6.3 m, which indicated high levels suggested that she was
having insulin depletion that led to the increase in potassium levels by protein catabolism. People
with diabetic ketoacidosis have alterations in their sodium and potassium levels initially but a
normal potassium content in diabetic ketoacidosis shows potassium deficit in a large amount
(Wolfsdorf et al., 2014).
Carly’s condition is due to insulin depletion and after a consistency of this issue for two
weeks she was taken to the hospital. After she was admitted she complained of vomiting, nausea
and abdominal pain. Lipolysis and hepatic ketogenesis is the reason for her vomiting tendencies
and due to the loss in the base, the patient went through weight loss in the last few months. The
deep labored breathing is caused due to diabetic ketoacidosis that is seen in Carly. This condition
decreases carbon dioxide in the blood that also causes hyperventilation and increasing deepness
of respiration (Wolfsdorf, 2014).
Carly had a breath that smelled like acetone that was due to ketoacidosis. It is a
complication that is mixed with an acetone like smell and an increased level of acetone in the
body, which is a dangerous amount. The circulation of fatty acid level increases due to
ketoacidosis and inhibiting lipolytic action in the growth hormones and the cortisol of insulin is
stopped by its depletion. The accumulation of fatty acids causes the acceleration of beta-
oxidation produces excess amount of ketone bodies. Acetone is formed with acetoacetate and
osmotic diuresis occurs when the glucose increases to a threshold of the renal glucose absorption
and due to osmotic diuresis an excess amount of water is lost (Shah et al., 2017). Dehydration
due to osmotic diuresis results to a loss of potassium ions, phosphate ions, magnesium ions and
sodium phosphate. However, sodium serum can be increased in patients who has a rise in
osmotic diuresis including poor fluid compensation. Carly’s condition with serum sodium being
128 mmol/L, serum potassium being 6.3 m, which indicated high levels suggested that she was
having insulin depletion that led to the increase in potassium levels by protein catabolism. People
with diabetic ketoacidosis have alterations in their sodium and potassium levels initially but a
normal potassium content in diabetic ketoacidosis shows potassium deficit in a large amount
(Wolfsdorf et al., 2014).
Carly’s condition is due to insulin depletion and after a consistency of this issue for two
weeks she was taken to the hospital. After she was admitted she complained of vomiting, nausea
and abdominal pain. Lipolysis and hepatic ketogenesis is the reason for her vomiting tendencies
and due to the loss in the base, the patient went through weight loss in the last few months. The
deep labored breathing is caused due to diabetic ketoacidosis that is seen in Carly. This condition
decreases carbon dioxide in the blood that also causes hyperventilation and increasing deepness
of respiration (Wolfsdorf, 2014).
Carly had a breath that smelled like acetone that was due to ketoacidosis. It is a
complication that is mixed with an acetone like smell and an increased level of acetone in the
body, which is a dangerous amount. The circulation of fatty acid level increases due to
ketoacidosis and inhibiting lipolytic action in the growth hormones and the cortisol of insulin is
stopped by its depletion. The accumulation of fatty acids causes the acceleration of beta-
oxidation produces excess amount of ketone bodies. Acetone is formed with acetoacetate and
6APPLIED PATHOPHYSIOLOGY
hydroxybutyrate that is the reason for acetone like smell. Lactic acidosis and poor tissue
perfusion is another factor that contributes to acetone formation. The above condition is the
reason for Carly’s positive result of urinalysis for ketones and glucose (Tasker & Acerini, 2014).
Orthostatic hypotension has symptoms like tachycardia and dehydration, which is seen in
Carly. Dehydration is the reason for tachycardia. It is also the cause of poor skin turgor,
orthostatic hypotension and dry mucous membrane as it was the reason for Carly’s pale and dry
skin. If the treatment of this condition is delayed then it can result to dehydration and acidosis.
This was seen in Carly’s case as she was admitted after 2 weeks after issues of polyuria,
polydipsia and fever. Diabetic acidosis is another reason for fever, which made Carly’s body hot
and a reason for increasing infection. Her WCC and CRP levels had an elevation that shows
immature band cells that occurs due to no infection (Singh et al., 2016). The reason for their
elevation might be due to systematic inflammatory response syndrome (SIRS) and in some
patients the CRP is increased including immature band cells of WCC due to the critical level of
diabetic ketoacidosis and its treatment, which is seen in Carly. Thus, the tendency of fever in
Carly occurs due to SIRS and not sepsis. It is also known as non-infectious form of SIRS due to
the increased levels of CRP and it is not because of infection but it is the result due to the
complications found in an aggressive treatment of diabetic ketoacidosis. Diabetic ketoacidosis
has a marker that happens due to fever, which is seen in Carly’s case.
The bodily energy gets drained due to decreased glucose and ketoacidosis and Carly is
the young child so she tends to get weak due to dehydration, weight loss, rapid deep sighing,
vomiting and abdominal pain, polydipsia and polyuria, and fever. This makes a person feel
sleepy because of lack of food, which is a compensation for low energy. This process explains
the drowsiness in Carly. Cerebral edema is another issue faced during diabetic ketoacidosis, but
hydroxybutyrate that is the reason for acetone like smell. Lactic acidosis and poor tissue
perfusion is another factor that contributes to acetone formation. The above condition is the
reason for Carly’s positive result of urinalysis for ketones and glucose (Tasker & Acerini, 2014).
Orthostatic hypotension has symptoms like tachycardia and dehydration, which is seen in
Carly. Dehydration is the reason for tachycardia. It is also the cause of poor skin turgor,
orthostatic hypotension and dry mucous membrane as it was the reason for Carly’s pale and dry
skin. If the treatment of this condition is delayed then it can result to dehydration and acidosis.
This was seen in Carly’s case as she was admitted after 2 weeks after issues of polyuria,
polydipsia and fever. Diabetic acidosis is another reason for fever, which made Carly’s body hot
and a reason for increasing infection. Her WCC and CRP levels had an elevation that shows
immature band cells that occurs due to no infection (Singh et al., 2016). The reason for their
elevation might be due to systematic inflammatory response syndrome (SIRS) and in some
patients the CRP is increased including immature band cells of WCC due to the critical level of
diabetic ketoacidosis and its treatment, which is seen in Carly. Thus, the tendency of fever in
Carly occurs due to SIRS and not sepsis. It is also known as non-infectious form of SIRS due to
the increased levels of CRP and it is not because of infection but it is the result due to the
complications found in an aggressive treatment of diabetic ketoacidosis. Diabetic ketoacidosis
has a marker that happens due to fever, which is seen in Carly’s case.
The bodily energy gets drained due to decreased glucose and ketoacidosis and Carly is
the young child so she tends to get weak due to dehydration, weight loss, rapid deep sighing,
vomiting and abdominal pain, polydipsia and polyuria, and fever. This makes a person feel
sleepy because of lack of food, which is a compensation for low energy. This process explains
the drowsiness in Carly. Cerebral edema is another issue faced during diabetic ketoacidosis, but
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7APPLIED PATHOPHYSIOLOGY
the mechanism is unclear (Gee, 2015). The contributing factors is delay in treatment and severe
level of diabetic ketoacidosis as seen in Carly’s case. Cerebral edema also occurs after intense
fluid replacement and insulin therapy and it also continues after severe condition of
hyperglycemia. It has a short span of time when the treatment is started. The symptoms of this
disease is urinary incontinence, headache, slow progress to neurological deterioration and
behavioral changes. The mechanism explained above shows the reason for noticeable
neurological degradation in Carly and one of them is aggressive behaviour. However, the
treatment of IV insulin infusion and IV fluids provide enhancement of biochemical functions and
relief in health condition. Diabetic ketoacidosis commonly leads to cerebral edema in children
below the age of 12 years (Boling & Pravikoff, 2016). Tonic-clonic convulsion occurs in this
treatment and that was observed in Carly including non-arousing tendencies. The GCS on her
assessment is marked as 6 and her pupils are reactive but dilated. A good treatment for cerebral
edema is Mannitol, and it occurs due to DKA. Another treatment is hypotonic solution that helps
in reducing the effects of cerebral edema. Carly‘s condition was improved and she was
discharged after she was treated with Mannitol, which enhanced her GCS.
Conclusion
Carly’s issue of diabetic ketoacidosis and its pathophysiological processes are explained
in the concept map. The reason her illness was caused and continuous degradation of her health
after admission is highlighted in the paper. This paper also gives a detail about the diseases of
diabetic ketoacidosis through significant literature review. The change in Carly’s vital signs,
symptoms and neurological conditions were clearly discussed by linking it to her health
condition and the disease she is suffering from.
the mechanism is unclear (Gee, 2015). The contributing factors is delay in treatment and severe
level of diabetic ketoacidosis as seen in Carly’s case. Cerebral edema also occurs after intense
fluid replacement and insulin therapy and it also continues after severe condition of
hyperglycemia. It has a short span of time when the treatment is started. The symptoms of this
disease is urinary incontinence, headache, slow progress to neurological deterioration and
behavioral changes. The mechanism explained above shows the reason for noticeable
neurological degradation in Carly and one of them is aggressive behaviour. However, the
treatment of IV insulin infusion and IV fluids provide enhancement of biochemical functions and
relief in health condition. Diabetic ketoacidosis commonly leads to cerebral edema in children
below the age of 12 years (Boling & Pravikoff, 2016). Tonic-clonic convulsion occurs in this
treatment and that was observed in Carly including non-arousing tendencies. The GCS on her
assessment is marked as 6 and her pupils are reactive but dilated. A good treatment for cerebral
edema is Mannitol, and it occurs due to DKA. Another treatment is hypotonic solution that helps
in reducing the effects of cerebral edema. Carly‘s condition was improved and she was
discharged after she was treated with Mannitol, which enhanced her GCS.
Conclusion
Carly’s issue of diabetic ketoacidosis and its pathophysiological processes are explained
in the concept map. The reason her illness was caused and continuous degradation of her health
after admission is highlighted in the paper. This paper also gives a detail about the diseases of
diabetic ketoacidosis through significant literature review. The change in Carly’s vital signs,
symptoms and neurological conditions were clearly discussed by linking it to her health
condition and the disease she is suffering from.
8APPLIED PATHOPHYSIOLOGY
References
Boling, B., & Pravikoff, D. (2016). Diabetic Ketoacidosis in Children.
Cameron, F. J., Scratch, S. E., Nadebaum, C., Northam, E. A., Koves, I., Jennings, J., ... & Inder,
T. E. (2014). Neurological consequences of diabetic ketoacidosis at initial presentation of
type 1 diabetes in a prospective cohort study of children. Diabetes care, 37(6), 1554-
1562.
Gee, S. W. (2015). The lethargic diabetic: cerebral edema in pediatric patients in diabetic
ketoacidosis. Air medical journal, 34(2), 109-112.
Kamel, K. S., & Halperin, M. L. (2015). Acid–base problems in diabetic ketoacidosis. New
England Journal of Medicine, 372(6), 546-554.
Nyenwe, E. A., & Kitabchi, A. E. (2016). The evolution of diabetic ketoacidosis: an update of its
etiology, pathogenesis and management. Metabolism, 65(4), 507-521.
Shah, I., Hoffman, G. F., Nyhan, W. L., Zschocke, J., Kahler, S. A., Mayatepek, E., ... & Chen,
Y. T. (2017). Lactic Acidosis in Children–A Varied Presentation. Journal of Pediatric
Intensive Care, 6(03), 206-208.
Singh, D., Cantu, M., Marx, M. H., & Akingbola, O. (2016). Diabetic Ketoacidosis and Fluid
Refractory Hypotension. Clinical pediatrics, 55(2), 182-184.
Srinivas, M. (2016). Diabetic Ketoacidosis in Children: A Systematic Review. Journal of
Chalmeda Anand Rao Institute of Medical Sciences Vol, 11(1), 31.
Tasker, R. C., & Acerini, C. L. (2014). Cerebral edema in children with diabetic ketoacidosis:
vasogenic rather than cellular?. Pediatric diabetes, 15(4), 261-270.
References
Boling, B., & Pravikoff, D. (2016). Diabetic Ketoacidosis in Children.
Cameron, F. J., Scratch, S. E., Nadebaum, C., Northam, E. A., Koves, I., Jennings, J., ... & Inder,
T. E. (2014). Neurological consequences of diabetic ketoacidosis at initial presentation of
type 1 diabetes in a prospective cohort study of children. Diabetes care, 37(6), 1554-
1562.
Gee, S. W. (2015). The lethargic diabetic: cerebral edema in pediatric patients in diabetic
ketoacidosis. Air medical journal, 34(2), 109-112.
Kamel, K. S., & Halperin, M. L. (2015). Acid–base problems in diabetic ketoacidosis. New
England Journal of Medicine, 372(6), 546-554.
Nyenwe, E. A., & Kitabchi, A. E. (2016). The evolution of diabetic ketoacidosis: an update of its
etiology, pathogenesis and management. Metabolism, 65(4), 507-521.
Shah, I., Hoffman, G. F., Nyhan, W. L., Zschocke, J., Kahler, S. A., Mayatepek, E., ... & Chen,
Y. T. (2017). Lactic Acidosis in Children–A Varied Presentation. Journal of Pediatric
Intensive Care, 6(03), 206-208.
Singh, D., Cantu, M., Marx, M. H., & Akingbola, O. (2016). Diabetic Ketoacidosis and Fluid
Refractory Hypotension. Clinical pediatrics, 55(2), 182-184.
Srinivas, M. (2016). Diabetic Ketoacidosis in Children: A Systematic Review. Journal of
Chalmeda Anand Rao Institute of Medical Sciences Vol, 11(1), 31.
Tasker, R. C., & Acerini, C. L. (2014). Cerebral edema in children with diabetic ketoacidosis:
vasogenic rather than cellular?. Pediatric diabetes, 15(4), 261-270.
9APPLIED PATHOPHYSIOLOGY
Watts, W., & Edge, J. A. (2014). How can cerebral edema during treatment of diabetic
ketoacidosis be avoided?. Pediatric diabetes, 15(4), 271-276.
Wolfsdorf, J. I. (2014). The International Society of Pediatric and Adolescent Diabetes
guidelines for management of diabetic ketoacidosis: do the guidelines need to be
modified?. Pediatric diabetes, 15(4), 277-286.
Wolfsdorf, J. I., Allgrove, J., Craig, M. E., Edge, J., Glaser, N., Jain, V., ... & Hanas, R. (2014).
Diabetic ketoacidosis and hyperglycemic hyperosmolar state. Pediatric
diabetes, 15(S20), 154-179.
Watts, W., & Edge, J. A. (2014). How can cerebral edema during treatment of diabetic
ketoacidosis be avoided?. Pediatric diabetes, 15(4), 271-276.
Wolfsdorf, J. I. (2014). The International Society of Pediatric and Adolescent Diabetes
guidelines for management of diabetic ketoacidosis: do the guidelines need to be
modified?. Pediatric diabetes, 15(4), 277-286.
Wolfsdorf, J. I., Allgrove, J., Craig, M. E., Edge, J., Glaser, N., Jain, V., ... & Hanas, R. (2014).
Diabetic ketoacidosis and hyperglycemic hyperosmolar state. Pediatric
diabetes, 15(S20), 154-179.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





