Article Analysis 1: Analysis of Research Articles on Bipolar Disorder
VerifiedAdded on 2022/10/14
|5
|1614
|326
Homework Assignment
AI Summary
This assignment presents an analysis of three research articles related to bipolar disorder. The first article investigates the impact of recovery-focused cognitive-behavioral therapy (CBT) on patients with recent-onset bipolar disorder, examining independent and dependent variables, and employing a randomized sampling method with 67 patients. The second article is a cohort study determining the mortality gap for individuals with bipolar disorder and schizophrenia, utilizing a nationally representative cohort and analyzing data from primary care electronic health records. The third article is a case-control study exploring the correlation between bipolar disorder and rheumatoid arthritis (RA), using data from a CHS database. The assignment requires the identification of independent and dependent variables, the population of interest, sampling methods, and examples of both descriptive and inferential statistics from each article. The analysis reveals insights into treatment effectiveness, mortality risks, and potential associations between bipolar disorder and RA, as well as the application of various statistical methods in healthcare research.
Article Analysis 1
Article
Citatio
n and
Permali
nk
(APA
format)
Article 1
Jones, S. H., Smith, G.,
Mulligan, L. D., Lobban,
F., Law, H., Dunn, G., ...
& Morrison, A. P. (2015).
Recovery-focused
cognitive–behavioural
therapy for recent-onset
bipolar disorder:
randomised controlled
pilot trial. The British
Journal of Psychiatry,
206(1), 58-66.
https://doi.org/10.1192/bjp
.bp.113.141259
Article 2
Hayes, J. F., Marston, L.,
Walters, K., King, M. B.,
& Osborn, D. P. (2017).
Mortality gap for people
with bipolar disorder and
schizophrenia: UK-based
cohort study 2000–2014.
The British Journal of
Psychiatry, 211(3), 175-
181.
https://doi.org/10.1192/bjp
.bp.117.202606
Article 3
Farhi, A., Cohen, A. D.,
Shovman, O.,
Comaneshter, D., Amital,
H., & Amital, D. (2016).
Bipolar disorder
associated with
rheumatoid arthritis: a
case-control study.
Journal of affective
disorders, 189, 287-289.
https://doi.org/10.1016/j.j
ad.2015.09.058
Point Description Description Description
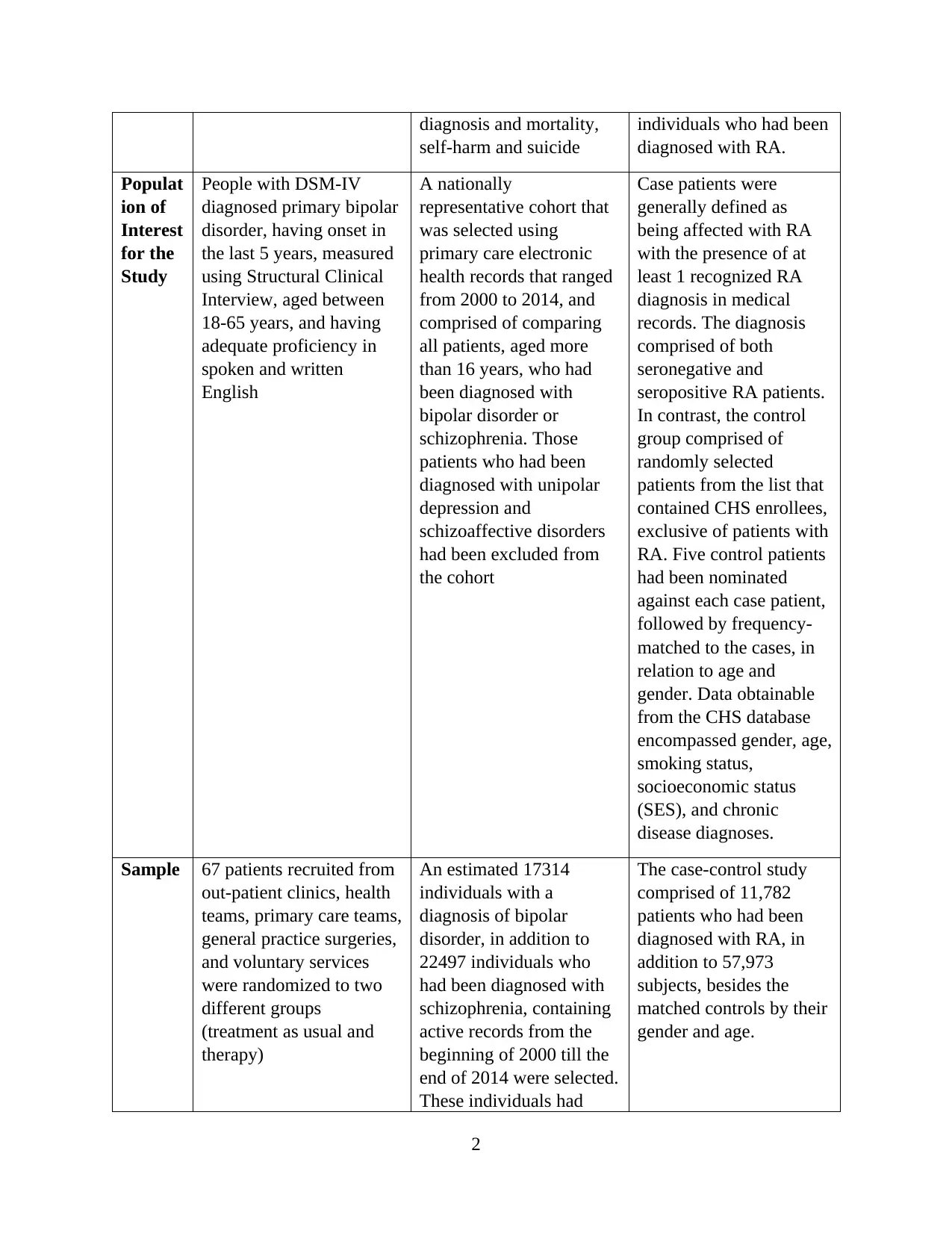
Broad
Topic
Area/Ti
tle
The impact of recovery-
focused cognitive-
behavioural therapy
(CBT) on patients who
have been diagnosed with
recent-onset bipolar
disorder
Cohort study for
determining the mortality
gap for individuals
suffering from
schizophrenia and bipolar
disorder from 2000-2014
A case-control study to
determine the correlation
of rheumatoid arthritis
with bipolar disorder
Identify
Indepe
ndent
and
Depend
ent
Variabl
es and
Type of
Data
for the
Variabl
es
Independent variable-
treatment (recovery-
focused cognitive-
behavioural therapy
(CBT) that had been
developed in collaboration
with patients
Dependent variable-
Personal and clinical
recovery outcomes (amid
patients with recent-onset
bipolar disorder)
Independent variable-
Primary care practices,
medication prescription,
symptom, referral,
examination finding, test
results, attendance at
hospital for people who
had received diagnosis for
schizophrenia or bipolar
disorder
Dependent variable- All-
cause mortality,
cardiovascular disease
Independent variable-
CHS database records
were used for collecting
retrospective information
for both bipolar disorder
and rheumatoid arthritis
(RA), depending on
information obtained
from reports of primary
physicians and hospitals.
Dependent variable-
Prevalence of bipolar
disorder among
© 2019. Grand Canyon University. All Rights Reserved.
Article
Citatio
n and
Permali
nk
(APA
format)
Article 1
Jones, S. H., Smith, G.,
Mulligan, L. D., Lobban,
F., Law, H., Dunn, G., ...
& Morrison, A. P. (2015).
Recovery-focused
cognitive–behavioural
therapy for recent-onset
bipolar disorder:
randomised controlled
pilot trial. The British
Journal of Psychiatry,
206(1), 58-66.
https://doi.org/10.1192/bjp
.bp.113.141259
Article 2
Hayes, J. F., Marston, L.,
Walters, K., King, M. B.,
& Osborn, D. P. (2017).
Mortality gap for people
with bipolar disorder and
schizophrenia: UK-based
cohort study 2000–2014.
The British Journal of
Psychiatry, 211(3), 175-
181.
https://doi.org/10.1192/bjp
.bp.117.202606
Article 3
Farhi, A., Cohen, A. D.,
Shovman, O.,
Comaneshter, D., Amital,
H., & Amital, D. (2016).
Bipolar disorder
associated with
rheumatoid arthritis: a
case-control study.
Journal of affective
disorders, 189, 287-289.
https://doi.org/10.1016/j.j
ad.2015.09.058
Point Description Description Description
Broad
Topic
Area/Ti
tle
The impact of recovery-
focused cognitive-
behavioural therapy
(CBT) on patients who
have been diagnosed with
recent-onset bipolar
disorder
Cohort study for
determining the mortality
gap for individuals
suffering from
schizophrenia and bipolar
disorder from 2000-2014
A case-control study to
determine the correlation
of rheumatoid arthritis
with bipolar disorder
Identify
Indepe
ndent
and
Depend
ent
Variabl
es and
Type of
Data
for the
Variabl
es
Independent variable-
treatment (recovery-
focused cognitive-
behavioural therapy
(CBT) that had been
developed in collaboration
with patients
Dependent variable-
Personal and clinical
recovery outcomes (amid
patients with recent-onset
bipolar disorder)
Independent variable-
Primary care practices,
medication prescription,
symptom, referral,
examination finding, test
results, attendance at
hospital for people who
had received diagnosis for
schizophrenia or bipolar
disorder
Dependent variable- All-
cause mortality,
cardiovascular disease
Independent variable-
CHS database records
were used for collecting
retrospective information
for both bipolar disorder
and rheumatoid arthritis
(RA), depending on
information obtained
from reports of primary
physicians and hospitals.
Dependent variable-
Prevalence of bipolar
disorder among
© 2019. Grand Canyon University. All Rights Reserved.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
diagnosis and mortality,
self-harm and suicide
individuals who had been
diagnosed with RA.
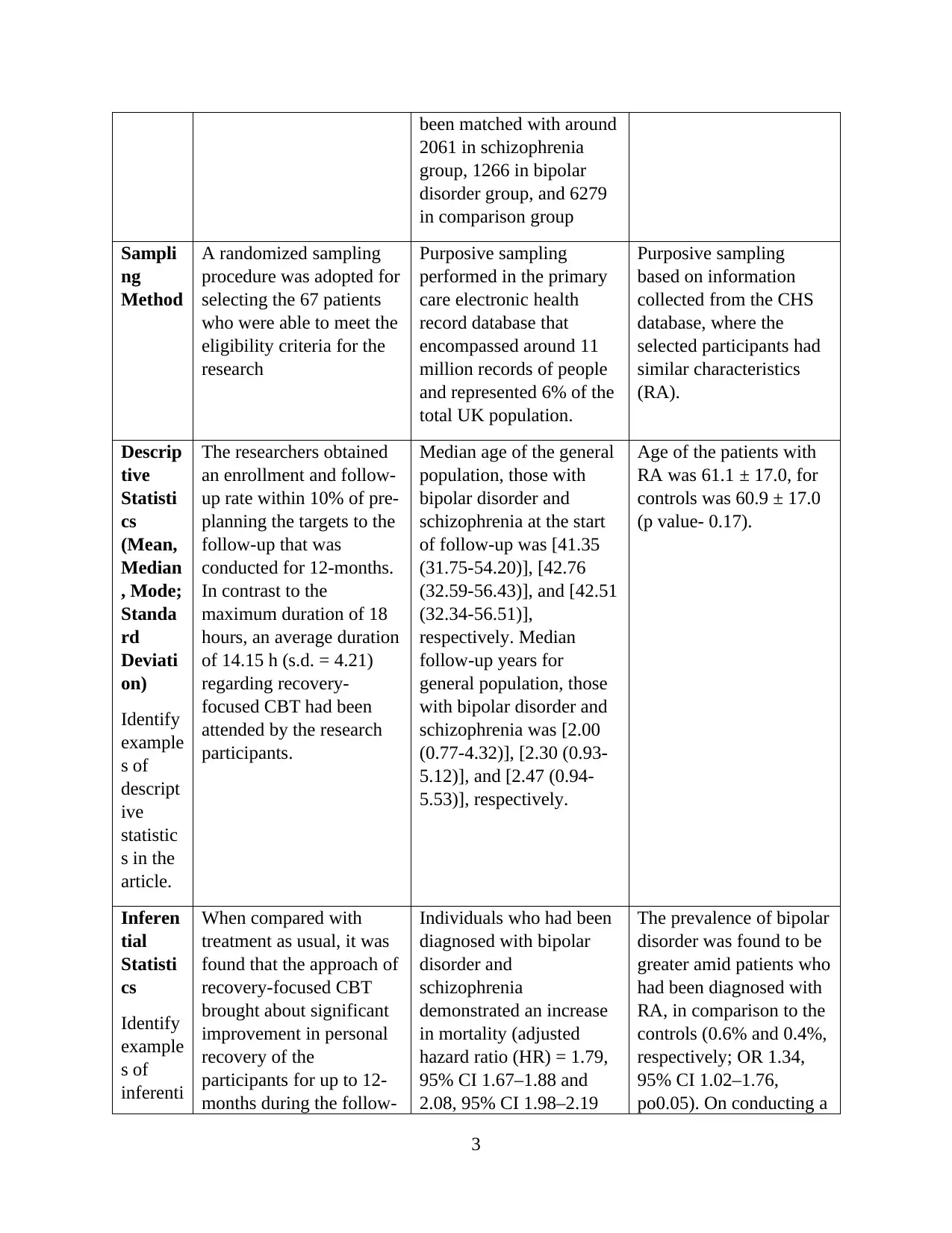
Populat
ion of
Interest
for the
Study
People with DSM-IV
diagnosed primary bipolar
disorder, having onset in
the last 5 years, measured
using Structural Clinical
Interview, aged between
18-65 years, and having
adequate proficiency in
spoken and written
English
A nationally
representative cohort that
was selected using
primary care electronic
health records that ranged
from 2000 to 2014, and
comprised of comparing
all patients, aged more
than 16 years, who had
been diagnosed with
bipolar disorder or
schizophrenia. Those
patients who had been
diagnosed with unipolar
depression and
schizoaffective disorders
had been excluded from
the cohort
Case patients were
generally defined as
being affected with RA
with the presence of at
least 1 recognized RA
diagnosis in medical
records. The diagnosis
comprised of both
seronegative and
seropositive RA patients.
In contrast, the control
group comprised of
randomly selected
patients from the list that
contained CHS enrollees,
exclusive of patients with
RA. Five control patients
had been nominated
against each case patient,
followed by frequency-
matched to the cases, in
relation to age and
gender. Data obtainable
from the CHS database
encompassed gender, age,
smoking status,
socioeconomic status
(SES), and chronic
disease diagnoses.
Sample 67 patients recruited from
out-patient clinics, health
teams, primary care teams,
general practice surgeries,
and voluntary services
were randomized to two
different groups
(treatment as usual and
therapy)
An estimated 17314
individuals with a
diagnosis of bipolar
disorder, in addition to
22497 individuals who
had been diagnosed with
schizophrenia, containing
active records from the
beginning of 2000 till the
end of 2014 were selected.
These individuals had
The case-control study
comprised of 11,782
patients who had been
diagnosed with RA, in
addition to 57,973
subjects, besides the
matched controls by their
gender and age.
2
self-harm and suicide
individuals who had been
diagnosed with RA.
Populat
ion of
Interest
for the
Study
People with DSM-IV
diagnosed primary bipolar
disorder, having onset in
the last 5 years, measured
using Structural Clinical
Interview, aged between
18-65 years, and having
adequate proficiency in
spoken and written
English
A nationally
representative cohort that
was selected using
primary care electronic
health records that ranged
from 2000 to 2014, and
comprised of comparing
all patients, aged more
than 16 years, who had
been diagnosed with
bipolar disorder or
schizophrenia. Those
patients who had been
diagnosed with unipolar
depression and
schizoaffective disorders
had been excluded from
the cohort
Case patients were
generally defined as
being affected with RA
with the presence of at
least 1 recognized RA
diagnosis in medical
records. The diagnosis
comprised of both
seronegative and
seropositive RA patients.
In contrast, the control
group comprised of
randomly selected
patients from the list that
contained CHS enrollees,
exclusive of patients with
RA. Five control patients
had been nominated
against each case patient,
followed by frequency-
matched to the cases, in
relation to age and
gender. Data obtainable
from the CHS database
encompassed gender, age,
smoking status,
socioeconomic status
(SES), and chronic
disease diagnoses.
Sample 67 patients recruited from
out-patient clinics, health
teams, primary care teams,
general practice surgeries,
and voluntary services
were randomized to two
different groups
(treatment as usual and
therapy)
An estimated 17314
individuals with a
diagnosis of bipolar
disorder, in addition to
22497 individuals who
had been diagnosed with
schizophrenia, containing
active records from the
beginning of 2000 till the
end of 2014 were selected.
These individuals had
The case-control study
comprised of 11,782
patients who had been
diagnosed with RA, in
addition to 57,973
subjects, besides the
matched controls by their
gender and age.
2
been matched with around
2061 in schizophrenia
group, 1266 in bipolar
disorder group, and 6279
in comparison group
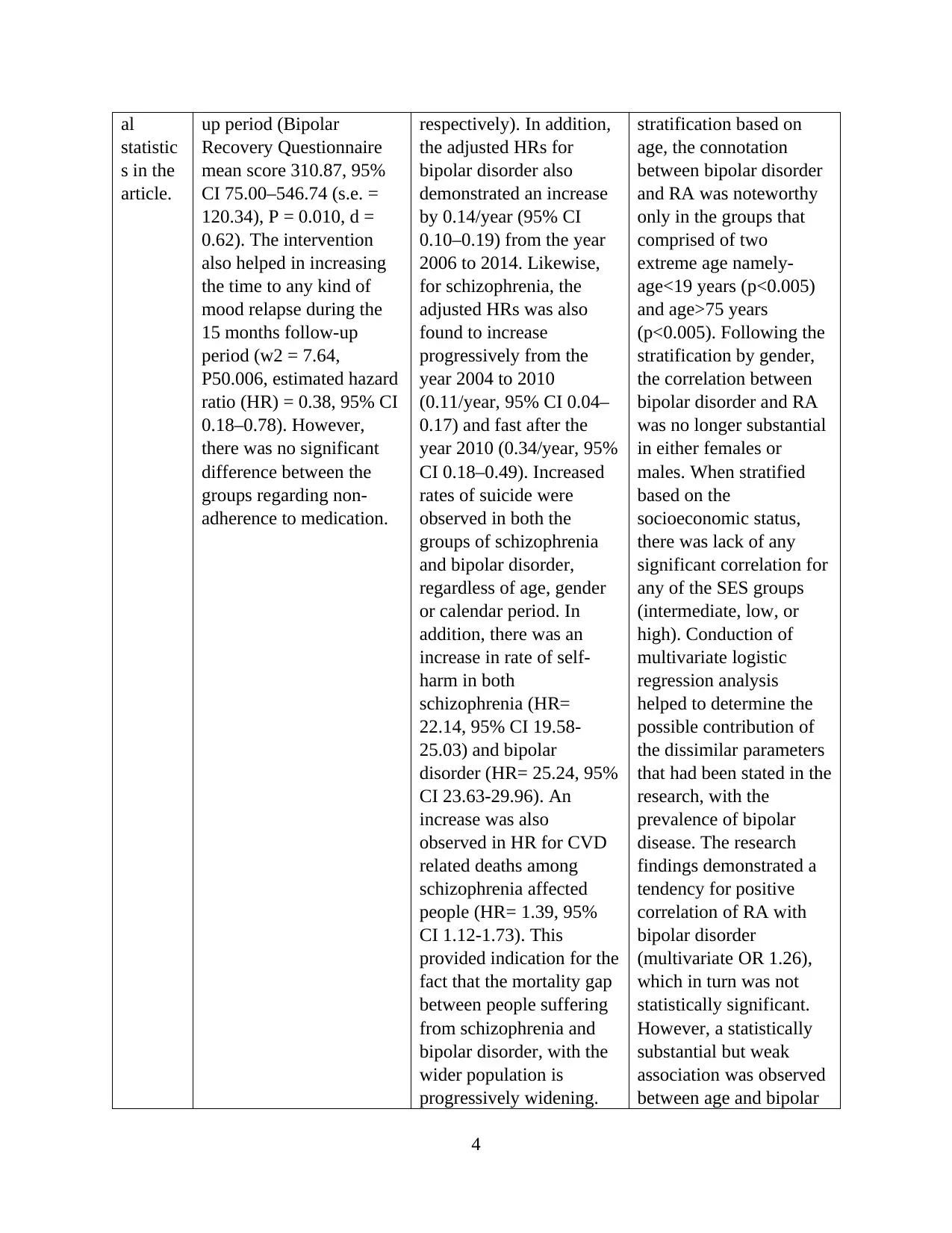
Sampli
ng
Method
A randomized sampling
procedure was adopted for
selecting the 67 patients
who were able to meet the
eligibility criteria for the
research
Purposive sampling
performed in the primary
care electronic health
record database that
encompassed around 11
million records of people
and represented 6% of the
total UK population.
Purposive sampling
based on information
collected from the CHS
database, where the
selected participants had
similar characteristics
(RA).
Descrip
tive
Statisti
cs
(Mean,
Median
, Mode;
Standa
rd
Deviati
on)
Identify
example
s of
descript
ive
statistic
s in the
article.
The researchers obtained
an enrollment and follow-
up rate within 10% of pre-
planning the targets to the
follow-up that was
conducted for 12-months.
In contrast to the
maximum duration of 18
hours, an average duration
of 14.15 h (s.d. = 4.21)
regarding recovery-
focused CBT had been
attended by the research
participants.
Median age of the general
population, those with
bipolar disorder and
schizophrenia at the start
of follow-up was [41.35
(31.75-54.20)], [42.76
(32.59-56.43)], and [42.51
(32.34-56.51)],
respectively. Median
follow-up years for
general population, those
with bipolar disorder and
schizophrenia was [2.00
(0.77-4.32)], [2.30 (0.93-
5.12)], and [2.47 (0.94-
5.53)], respectively.
Age of the patients with
RA was 61.1 ± 17.0, for
controls was 60.9 ± 17.0
(p value- 0.17).
Inferen
tial
Statisti
cs
Identify
example
s of
inferenti
When compared with
treatment as usual, it was
found that the approach of
recovery-focused CBT
brought about significant
improvement in personal
recovery of the
participants for up to 12-
months during the follow-
Individuals who had been
diagnosed with bipolar
disorder and
schizophrenia
demonstrated an increase
in mortality (adjusted
hazard ratio (HR) = 1.79,
95% CI 1.67–1.88 and
2.08, 95% CI 1.98–2.19
The prevalence of bipolar
disorder was found to be
greater amid patients who
had been diagnosed with
RA, in comparison to the
controls (0.6% and 0.4%,
respectively; OR 1.34,
95% CI 1.02–1.76,
po0.05). On conducting a
3
2061 in schizophrenia
group, 1266 in bipolar
disorder group, and 6279
in comparison group
Sampli
ng
Method
A randomized sampling
procedure was adopted for
selecting the 67 patients
who were able to meet the
eligibility criteria for the
research
Purposive sampling
performed in the primary
care electronic health
record database that
encompassed around 11
million records of people
and represented 6% of the
total UK population.
Purposive sampling
based on information
collected from the CHS
database, where the
selected participants had
similar characteristics
(RA).
Descrip
tive
Statisti
cs
(Mean,
Median
, Mode;
Standa
rd
Deviati
on)
Identify
example
s of
descript
ive
statistic
s in the
article.
The researchers obtained
an enrollment and follow-
up rate within 10% of pre-
planning the targets to the
follow-up that was
conducted for 12-months.
In contrast to the
maximum duration of 18
hours, an average duration
of 14.15 h (s.d. = 4.21)
regarding recovery-
focused CBT had been
attended by the research
participants.
Median age of the general
population, those with
bipolar disorder and
schizophrenia at the start
of follow-up was [41.35
(31.75-54.20)], [42.76
(32.59-56.43)], and [42.51
(32.34-56.51)],
respectively. Median
follow-up years for
general population, those
with bipolar disorder and
schizophrenia was [2.00
(0.77-4.32)], [2.30 (0.93-
5.12)], and [2.47 (0.94-
5.53)], respectively.
Age of the patients with
RA was 61.1 ± 17.0, for
controls was 60.9 ± 17.0
(p value- 0.17).
Inferen
tial
Statisti
cs
Identify
example
s of
inferenti
When compared with
treatment as usual, it was
found that the approach of
recovery-focused CBT
brought about significant
improvement in personal
recovery of the
participants for up to 12-
months during the follow-
Individuals who had been
diagnosed with bipolar
disorder and
schizophrenia
demonstrated an increase
in mortality (adjusted
hazard ratio (HR) = 1.79,
95% CI 1.67–1.88 and
2.08, 95% CI 1.98–2.19
The prevalence of bipolar
disorder was found to be
greater amid patients who
had been diagnosed with
RA, in comparison to the
controls (0.6% and 0.4%,
respectively; OR 1.34,
95% CI 1.02–1.76,
po0.05). On conducting a
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
al
statistic
s in the
article.
up period (Bipolar
Recovery Questionnaire
mean score 310.87, 95%
CI 75.00–546.74 (s.e. =
120.34), P = 0.010, d =
0.62). The intervention
also helped in increasing
the time to any kind of
mood relapse during the
15 months follow-up
period (w2 = 7.64,
P50.006, estimated hazard
ratio (HR) = 0.38, 95% CI
0.18–0.78). However,
there was no significant
difference between the
groups regarding non-
adherence to medication.
respectively). In addition,
the adjusted HRs for
bipolar disorder also
demonstrated an increase
by 0.14/year (95% CI
0.10–0.19) from the year
2006 to 2014. Likewise,
for schizophrenia, the
adjusted HRs was also
found to increase
progressively from the
year 2004 to 2010
(0.11/year, 95% CI 0.04–
0.17) and fast after the
year 2010 (0.34/year, 95%
CI 0.18–0.49). Increased
rates of suicide were
observed in both the
groups of schizophrenia
and bipolar disorder,
regardless of age, gender
or calendar period. In
addition, there was an
increase in rate of self-
harm in both
schizophrenia (HR=
22.14, 95% CI 19.58-
25.03) and bipolar
disorder (HR= 25.24, 95%
CI 23.63-29.96). An
increase was also
observed in HR for CVD
related deaths among
schizophrenia affected
people (HR= 1.39, 95%
CI 1.12-1.73). This
provided indication for the
fact that the mortality gap
between people suffering
from schizophrenia and
bipolar disorder, with the
wider population is
progressively widening.
stratification based on
age, the connotation
between bipolar disorder
and RA was noteworthy
only in the groups that
comprised of two
extreme age namely-
age<19 years (p<0.005)
and age>75 years
(p<0.005). Following the
stratification by gender,
the correlation between
bipolar disorder and RA
was no longer substantial
in either females or
males. When stratified
based on the
socioeconomic status,
there was lack of any
significant correlation for
any of the SES groups
(intermediate, low, or
high). Conduction of
multivariate logistic
regression analysis
helped to determine the
possible contribution of
the dissimilar parameters
that had been stated in the
research, with the
prevalence of bipolar
disease. The research
findings demonstrated a
tendency for positive
correlation of RA with
bipolar disorder
(multivariate OR 1.26),
which in turn was not
statistically significant.
However, a statistically
substantial but weak
association was observed
between age and bipolar
4
statistic
s in the
article.
up period (Bipolar
Recovery Questionnaire
mean score 310.87, 95%
CI 75.00–546.74 (s.e. =
120.34), P = 0.010, d =
0.62). The intervention
also helped in increasing
the time to any kind of
mood relapse during the
15 months follow-up
period (w2 = 7.64,
P50.006, estimated hazard
ratio (HR) = 0.38, 95% CI
0.18–0.78). However,
there was no significant
difference between the
groups regarding non-
adherence to medication.
respectively). In addition,
the adjusted HRs for
bipolar disorder also
demonstrated an increase
by 0.14/year (95% CI
0.10–0.19) from the year
2006 to 2014. Likewise,
for schizophrenia, the
adjusted HRs was also
found to increase
progressively from the
year 2004 to 2010
(0.11/year, 95% CI 0.04–
0.17) and fast after the
year 2010 (0.34/year, 95%
CI 0.18–0.49). Increased
rates of suicide were
observed in both the
groups of schizophrenia
and bipolar disorder,
regardless of age, gender
or calendar period. In
addition, there was an
increase in rate of self-
harm in both
schizophrenia (HR=
22.14, 95% CI 19.58-
25.03) and bipolar
disorder (HR= 25.24, 95%
CI 23.63-29.96). An
increase was also
observed in HR for CVD
related deaths among
schizophrenia affected
people (HR= 1.39, 95%
CI 1.12-1.73). This
provided indication for the
fact that the mortality gap
between people suffering
from schizophrenia and
bipolar disorder, with the
wider population is
progressively widening.
stratification based on
age, the connotation
between bipolar disorder
and RA was noteworthy
only in the groups that
comprised of two
extreme age namely-
age<19 years (p<0.005)
and age>75 years
(p<0.005). Following the
stratification by gender,
the correlation between
bipolar disorder and RA
was no longer substantial
in either females or
males. When stratified
based on the
socioeconomic status,
there was lack of any
significant correlation for
any of the SES groups
(intermediate, low, or
high). Conduction of
multivariate logistic
regression analysis
helped to determine the
possible contribution of
the dissimilar parameters
that had been stated in the
research, with the
prevalence of bipolar
disease. The research
findings demonstrated a
tendency for positive
correlation of RA with
bipolar disorder
(multivariate OR 1.26),
which in turn was not
statistically significant.
However, a statistically
substantial but weak
association was observed
between age and bipolar
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
disorder (multivariate OR
1.02, 95% CI 1.01–1.03,
po0.001). SES and
gender were not
individually related to
bipolar disorder.
However, there existed a
positive correlation
between smoking and
bipolar disorder
(multivariate OR 1.66,
95% CI 1.31–2.11,
po0.001)
5
1.02, 95% CI 1.01–1.03,
po0.001). SES and
gender were not
individually related to
bipolar disorder.
However, there existed a
positive correlation
between smoking and
bipolar disorder
(multivariate OR 1.66,
95% CI 1.31–2.11,
po0.001)
5
1 out of 5
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.