Critical Evaluation of Schizophrenia Treatment: A Biopsychosocial Lens
VerifiedAdded on 2023/01/18
|8
|1775
|88
Essay
AI Summary
This essay provides a critical evaluation of a research article focusing on a mindfulness-based psychoeducation program for schizophrenia patients. It examines the effectiveness of the intervention in reducing psychiatric symptoms, improving psychosocial functioning, and increasing insight into the illness. The evaluation incorporates Engel's biopsychosocial model, assessing how the treatment addresses biological, psychological, and social factors. While acknowledging the positive outcomes reported in the article, the essay also identifies gaps, such as the lack of consideration for cultural, familial, and socioeconomic aspects. It concludes by suggesting relevant referrals and resources for schizophrenia patients in Ontario, Canada, highlighting the importance of comprehensive support and treatment approaches. The essay emphasizes that while the intervention shows promise, a more holistic understanding of the patient's context is crucial for effective management of schizophrenia.

Running head: ARTICLE EVALUATION
Psychology
Name of the Student
Name of the University
Author note
Psychology
Name of the Student
Name of the University
Author note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1ARTICLE EVALUATION
Introduction
Psychological disorder is an umbrella term that refers to several psychiatric or mental
disorders that are primarily characterized by a range of behavioral patterns and symptoms,
creating an impact on several domains of life (Caspi et al., 2014). Common psychological
disorders are anxiety, depression, schizophrenia, PTSD, and bipolar disorder. These disorders
have been found to create a significant impact on the daily life experiences of the affected
person, thus affecting their health and quality of life. This essay will elaborate on an article
that focuses on an intervention for schizophrenia.
Article summary
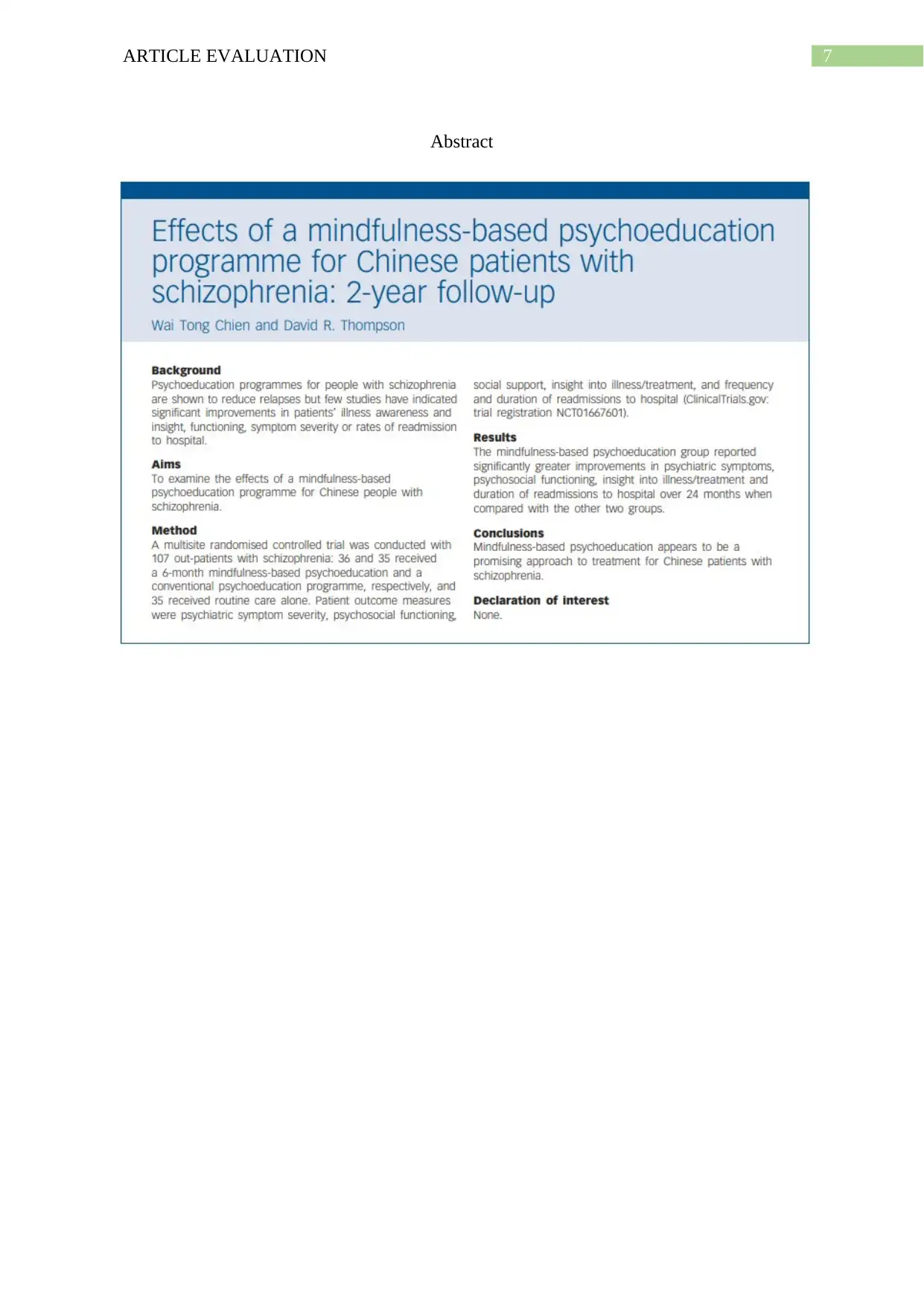
The researchers conducted their investigation based on the fact that there is mounting
evidence for the efficacy of psychoeducation programmes in lowering symptom severity
among people, affected with schizophrenia. The researchers stated that despite the
effectiveness of the intervention in schizophrenia treatment, there was lack of adequate
evidence for its effectiveness in enhancing awareness among patients, and helping them gain
an insight into the mental disorder they are suffering from (Chien & Thompson, 2014). With
the aim of examining the impacts of mindfulness-based psychoeducation programme, the
researchers recruited 107 Chinese outpatients who were categorised into the intervention
(n=36) and conventional psychoeducation (n=35) groups. Determination of the outcome
measures suggested that greater improvements were reported by patients who were present in
the intervention group, in relation to reduction of psychiatric symptoms, improvement of
psychosocial functioning, reduction in readmission rates, and increased insight into the
disease and its treatment, in comparison to the control counterparts, thus highlighting the
effectiveness of mindfulness-based psychoeducation in schizophrenia treatment.
Introduction
Psychological disorder is an umbrella term that refers to several psychiatric or mental
disorders that are primarily characterized by a range of behavioral patterns and symptoms,
creating an impact on several domains of life (Caspi et al., 2014). Common psychological
disorders are anxiety, depression, schizophrenia, PTSD, and bipolar disorder. These disorders
have been found to create a significant impact on the daily life experiences of the affected
person, thus affecting their health and quality of life. This essay will elaborate on an article
that focuses on an intervention for schizophrenia.
Article summary
The researchers conducted their investigation based on the fact that there is mounting
evidence for the efficacy of psychoeducation programmes in lowering symptom severity
among people, affected with schizophrenia. The researchers stated that despite the
effectiveness of the intervention in schizophrenia treatment, there was lack of adequate
evidence for its effectiveness in enhancing awareness among patients, and helping them gain
an insight into the mental disorder they are suffering from (Chien & Thompson, 2014). With
the aim of examining the impacts of mindfulness-based psychoeducation programme, the
researchers recruited 107 Chinese outpatients who were categorised into the intervention
(n=36) and conventional psychoeducation (n=35) groups. Determination of the outcome
measures suggested that greater improvements were reported by patients who were present in
the intervention group, in relation to reduction of psychiatric symptoms, improvement of
psychosocial functioning, reduction in readmission rates, and increased insight into the
disease and its treatment, in comparison to the control counterparts, thus highlighting the
effectiveness of mindfulness-based psychoeducation in schizophrenia treatment.
2ARTICLE EVALUATION
Critical Examination of the Biopsychosocial Factors
Proposed by Engel, the primary aim of the biopsychosocial model of health is to
reflect disease development, through the multifaceted and complex interactions between
biological factors (biochemical, genetic), social factors (familial, socioeconomic, cultural,
medical), and psychological factors (personality, mood, behaviour) (Pilgrim, 2015). Thus,
gaining a sound understanding of the biopsychosocial factors acts in the form of an
integrative and comprehensive framework that facilitates increasing awareness on human
functioning, development and health. Therefore, while taking these biopsychosocial factors
into consideration, it is imperative for placing an emphasis on the need for attaining positive
functioning and health, across several domains of the lives of patients, besides lowering
psychological distress and treating symptomatology. The outcomes that had been measured
by the researchers in the article discussed above were namely, social support, psychosocial
functioning, insight into treatment and disease, psychiatric indication severity, and incidence
and length of hospital readmissions. Thus, it can be stated that apart from measuring the
effects of mindfulness-based psychoeducation programme on the symptoms that are
manifested by schizophrenia patients, the researchers addressed biopsychosocial factors
namely, psychosocial functioning, mood, behaviour and social support.
Time and again it has been proved that the psychosocial approaches consider
individuals in the light of joint impact that the surrounding social circumstances and
psychological factors create on the mental and physical wellness of people (Thomas et al.,
2017). In addition, psychosocial functioning has also been identified as significant in the
revised tool of Diagnostic and Statistical Manual of Mental Disorders (DSM) that is
considered as the mainstay for recognising the signs and symptoms of mental illnesses.
Furthermore, despite the most characteristic signs of schizophrenia involving hallucinations
and delusions, functional insufficiencies are an essential aspect of the disorder, and the
Critical Examination of the Biopsychosocial Factors
Proposed by Engel, the primary aim of the biopsychosocial model of health is to
reflect disease development, through the multifaceted and complex interactions between
biological factors (biochemical, genetic), social factors (familial, socioeconomic, cultural,
medical), and psychological factors (personality, mood, behaviour) (Pilgrim, 2015). Thus,
gaining a sound understanding of the biopsychosocial factors acts in the form of an
integrative and comprehensive framework that facilitates increasing awareness on human
functioning, development and health. Therefore, while taking these biopsychosocial factors
into consideration, it is imperative for placing an emphasis on the need for attaining positive
functioning and health, across several domains of the lives of patients, besides lowering
psychological distress and treating symptomatology. The outcomes that had been measured
by the researchers in the article discussed above were namely, social support, psychosocial
functioning, insight into treatment and disease, psychiatric indication severity, and incidence
and length of hospital readmissions. Thus, it can be stated that apart from measuring the
effects of mindfulness-based psychoeducation programme on the symptoms that are
manifested by schizophrenia patients, the researchers addressed biopsychosocial factors
namely, psychosocial functioning, mood, behaviour and social support.
Time and again it has been proved that the psychosocial approaches consider
individuals in the light of joint impact that the surrounding social circumstances and
psychological factors create on the mental and physical wellness of people (Thomas et al.,
2017). In addition, psychosocial functioning has also been identified as significant in the
revised tool of Diagnostic and Statistical Manual of Mental Disorders (DSM) that is
considered as the mainstay for recognising the signs and symptoms of mental illnesses.
Furthermore, despite the most characteristic signs of schizophrenia involving hallucinations
and delusions, functional insufficiencies are an essential aspect of the disorder, and the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3ARTICLE EVALUATION
decline in patient’s social functioning acts in the form of a major predictor for poor health
outcomes (Carra et al., 2016). The researchers had used the Specific Level of Functioning
(SLOF) scale for determining the real life functioning of the Chinese schizophrenia patients
and assessed three major functional domains namely, self-maintenance, community living
skills, and social functioning. In addition, social support provides necessary psychological
and physical advantages for individuals who faced numerous stressful psychosocial and
physical events (Applebaum et al., 2014). Furthermore, Naslund et al. (2016) proposed that
emotional support from family members, co-workers and friends helps in relieving
psychological distress and also enhances the health-related quality of life. However, taking
into consideration the fact that mental disorders are associated with negative beliefs and
attitudes towards the patients, which results in discrimination, the researchers were accurate
in assessing the impact of the intervention on social support.
Nonetheless, some of the major gaps in the research can be accredited to the fact that
they did not form any association between the mindfulness based psycho-educational
approach with the cultural, familial, and socioeconomic aspects. Religious teachings and
cultural values often impact beliefs about the roots and nature of mental disorder, and also
shape approaches towards people who are mentally affected (Jenkins, 2015). This calls for
the need of understanding the effects that mindfulness breathing exercise, dealing with
barriers, body scan meditation, and dealing with attitudes will modify the ethno-cultural
beliefs of the patients, as well the society. In addition, high rates of mental illness have been
found among people belonging to poor socioeconomic status (Burns, 2015). Therefore, the
researchers should have recruited patients from poor socioeconomic background in order to
understand the effects that the intervention creates on their approach towards life and their
health, in addition to promoting employment seeking opportunities.
decline in patient’s social functioning acts in the form of a major predictor for poor health
outcomes (Carra et al., 2016). The researchers had used the Specific Level of Functioning
(SLOF) scale for determining the real life functioning of the Chinese schizophrenia patients
and assessed three major functional domains namely, self-maintenance, community living
skills, and social functioning. In addition, social support provides necessary psychological
and physical advantages for individuals who faced numerous stressful psychosocial and
physical events (Applebaum et al., 2014). Furthermore, Naslund et al. (2016) proposed that
emotional support from family members, co-workers and friends helps in relieving
psychological distress and also enhances the health-related quality of life. However, taking
into consideration the fact that mental disorders are associated with negative beliefs and
attitudes towards the patients, which results in discrimination, the researchers were accurate
in assessing the impact of the intervention on social support.
Nonetheless, some of the major gaps in the research can be accredited to the fact that
they did not form any association between the mindfulness based psycho-educational
approach with the cultural, familial, and socioeconomic aspects. Religious teachings and
cultural values often impact beliefs about the roots and nature of mental disorder, and also
shape approaches towards people who are mentally affected (Jenkins, 2015). This calls for
the need of understanding the effects that mindfulness breathing exercise, dealing with
barriers, body scan meditation, and dealing with attitudes will modify the ethno-cultural
beliefs of the patients, as well the society. In addition, high rates of mental illness have been
found among people belonging to poor socioeconomic status (Burns, 2015). Therefore, the
researchers should have recruited patients from poor socioeconomic background in order to
understand the effects that the intervention creates on their approach towards life and their
health, in addition to promoting employment seeking opportunities.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4ARTICLE EVALUATION
Referral and Resources
Seeking out support from different organisations and referral services present in the
community helps in educating the patient and their family members on the signs and
symptoms, and the appropriate interventions for the mental disease of interest. A person who
suffers from schizophrenia and currently resides in Ontario, Canada can be referred to the
Schizophrenia Society of Ontario since it comprises of a team of experts who offer telephone,
in-person, and online support and customised counselling to patients on their first episodes,
new diagnosis, justice, employment, advocacy, symptom management, housing and
medications (SSO, 2019). Such patients can also seek services from the Hamilton Program
for Schizophrenia owing to the fact that it facilitates personalised recovery from mental
illness by promoting choice, hope and wellness, with the aim of accomplishing personal
growth (HPS, 2019). Additional referral would also be made to the Ontario Shores Centre for
Mental Health Sciences where patients would obtain prompt services from an inter-
professional team of healthcare workers, who would collaboratively work with the medical
staff for schizophrenia treatment (Ontario Shores, 2019).
Conclusion
To conclude, schizophrenia is a severe and chronic mental disorder that creates an
impact on the mood, behaviour, and functioning of the affected people. The article discussed
was successful in illustrating the impacts of an intervention on several domains of the
disease, however it did not take into consideration numerous biopsychosocial aspects of
mental health and illness.
Referral and Resources
Seeking out support from different organisations and referral services present in the
community helps in educating the patient and their family members on the signs and
symptoms, and the appropriate interventions for the mental disease of interest. A person who
suffers from schizophrenia and currently resides in Ontario, Canada can be referred to the
Schizophrenia Society of Ontario since it comprises of a team of experts who offer telephone,
in-person, and online support and customised counselling to patients on their first episodes,
new diagnosis, justice, employment, advocacy, symptom management, housing and
medications (SSO, 2019). Such patients can also seek services from the Hamilton Program
for Schizophrenia owing to the fact that it facilitates personalised recovery from mental
illness by promoting choice, hope and wellness, with the aim of accomplishing personal
growth (HPS, 2019). Additional referral would also be made to the Ontario Shores Centre for
Mental Health Sciences where patients would obtain prompt services from an inter-
professional team of healthcare workers, who would collaboratively work with the medical
staff for schizophrenia treatment (Ontario Shores, 2019).
Conclusion
To conclude, schizophrenia is a severe and chronic mental disorder that creates an
impact on the mood, behaviour, and functioning of the affected people. The article discussed
was successful in illustrating the impacts of an intervention on several domains of the
disease, however it did not take into consideration numerous biopsychosocial aspects of
mental health and illness.
5ARTICLE EVALUATION
References
Applebaum, A. J., Stein, E. M., Lord‐Bessen, J., Pessin, H., Rosenfeld, B., & Breitbart, W.
(2014). Optimism, social support, and mental health outcomes in patients with
advanced cancer. Psycho
‐Oncology, 23(3), 299-306.
Burns, J. K. (2015). Poverty, inequality and a political economy of mental
health. Epidemiology and psychiatric sciences, 24(2), 107-113.
Carra, G., Johnson, S., Crocamo, C., Angermeyer, M. C., Brugha, T., Azorin, J. M., ... &
Bebbington, P. E. (2016). Psychosocial functioning, quality of life and clinical
correlates of comorbid alcohol and drug dependence syndromes in people with
schizophrenia across Europe. Psychiatry research, 239, 301-307.
Caspi, A., Houts, R. M., Belsky, D. W., Goldman-Mellor, S. J., Harrington, H., Israel, S., ...
& Moffitt, T. E. (2014). The p factor: one general psychopathology factor in the
structure of psychiatric disorders?. Clinical Psychological Science, 2(2), 119-137.
Chien, W. T., & Thompson, D. R. (2014). Effects of a mindfulness-based psychoeducation
programme for Chinese patients with schizophrenia: 2-year follow-up. The British
Journal of Psychiatry, 205(1), 52-59.
Hamilton Program for Schizophrenia. (2019). Get in touch. Retrieved from
http://www.hpfs.on.ca/
Jenkins, J. H. (2015). Extraordinary conditions: Culture and experience in mental illness.
University of California Press.
Naslund, J. A., Aschbrenner, K. A., Marsch, L. A., & Bartels, S. J. (2016). The future of
mental health care: peer-to-peer support and social media. Epidemiology and
psychiatric sciences, 25(2), 113-122.
References
Applebaum, A. J., Stein, E. M., Lord‐Bessen, J., Pessin, H., Rosenfeld, B., & Breitbart, W.
(2014). Optimism, social support, and mental health outcomes in patients with
advanced cancer. Psycho
‐Oncology, 23(3), 299-306.
Burns, J. K. (2015). Poverty, inequality and a political economy of mental
health. Epidemiology and psychiatric sciences, 24(2), 107-113.
Carra, G., Johnson, S., Crocamo, C., Angermeyer, M. C., Brugha, T., Azorin, J. M., ... &
Bebbington, P. E. (2016). Psychosocial functioning, quality of life and clinical
correlates of comorbid alcohol and drug dependence syndromes in people with
schizophrenia across Europe. Psychiatry research, 239, 301-307.
Caspi, A., Houts, R. M., Belsky, D. W., Goldman-Mellor, S. J., Harrington, H., Israel, S., ...
& Moffitt, T. E. (2014). The p factor: one general psychopathology factor in the
structure of psychiatric disorders?. Clinical Psychological Science, 2(2), 119-137.
Chien, W. T., & Thompson, D. R. (2014). Effects of a mindfulness-based psychoeducation
programme for Chinese patients with schizophrenia: 2-year follow-up. The British
Journal of Psychiatry, 205(1), 52-59.
Hamilton Program for Schizophrenia. (2019). Get in touch. Retrieved from
http://www.hpfs.on.ca/
Jenkins, J. H. (2015). Extraordinary conditions: Culture and experience in mental illness.
University of California Press.
Naslund, J. A., Aschbrenner, K. A., Marsch, L. A., & Bartels, S. J. (2016). The future of
mental health care: peer-to-peer support and social media. Epidemiology and
psychiatric sciences, 25(2), 113-122.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6ARTICLE EVALUATION
Ontario Shores Centre for Mental Health Sciences. (2019). How to make a referral. Retrieved
from https://www.ontarioshores.ca/finding_help/how_to_make_a_referral
Pilgrim, D. (2015). The biopsychosocial model in health research: its strengths and
limitations for critical realists. Journal of Critical Realism, 14(2), 164-180.
Schizophrenia Society of Ontario. (2019). Ask The Expert - Web and Telephone Support.
Retrieved from https://www.schizophrenia.on.ca/Get-Help/Services/Families
Thomas, M. L., Green, M. F., Hellemann, G., Sugar, C. A., Tarasenko, M., Calkins, M. E., ...
& Nuechterlein, K. H. (2017). Modeling deficits from early auditory information
processing to psychosocial functioning in schizophrenia. JAMA psychiatry, 74(1), 37-
46.
Ontario Shores Centre for Mental Health Sciences. (2019). How to make a referral. Retrieved
from https://www.ontarioshores.ca/finding_help/how_to_make_a_referral
Pilgrim, D. (2015). The biopsychosocial model in health research: its strengths and
limitations for critical realists. Journal of Critical Realism, 14(2), 164-180.
Schizophrenia Society of Ontario. (2019). Ask The Expert - Web and Telephone Support.
Retrieved from https://www.schizophrenia.on.ca/Get-Help/Services/Families
Thomas, M. L., Green, M. F., Hellemann, G., Sugar, C. A., Tarasenko, M., Calkins, M. E., ...
& Nuechterlein, K. H. (2017). Modeling deficits from early auditory information
processing to psychosocial functioning in schizophrenia. JAMA psychiatry, 74(1), 37-
46.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7ARTICLE EVALUATION
Abstract
Abstract
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





