Chronic Kidney Disease Assignment 2022
VerifiedAdded on 2022/10/11
|7
|1598
|16
Assignment
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: NURSING
Nursing:
Name of the student:
Name of the University:
Author’s note
Nursing:
Name of the student:
Name of the University:
Author’s note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1NURSING
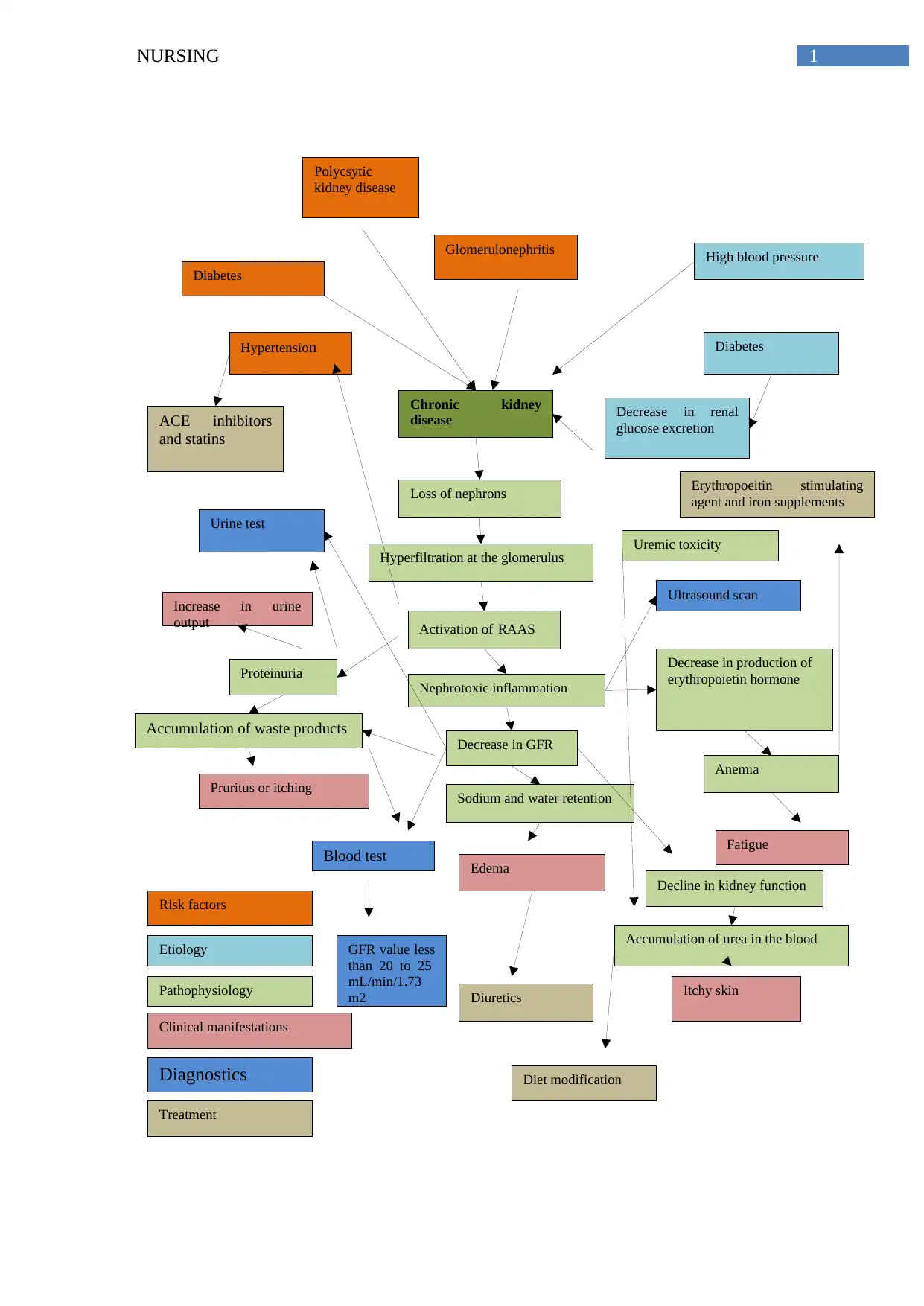
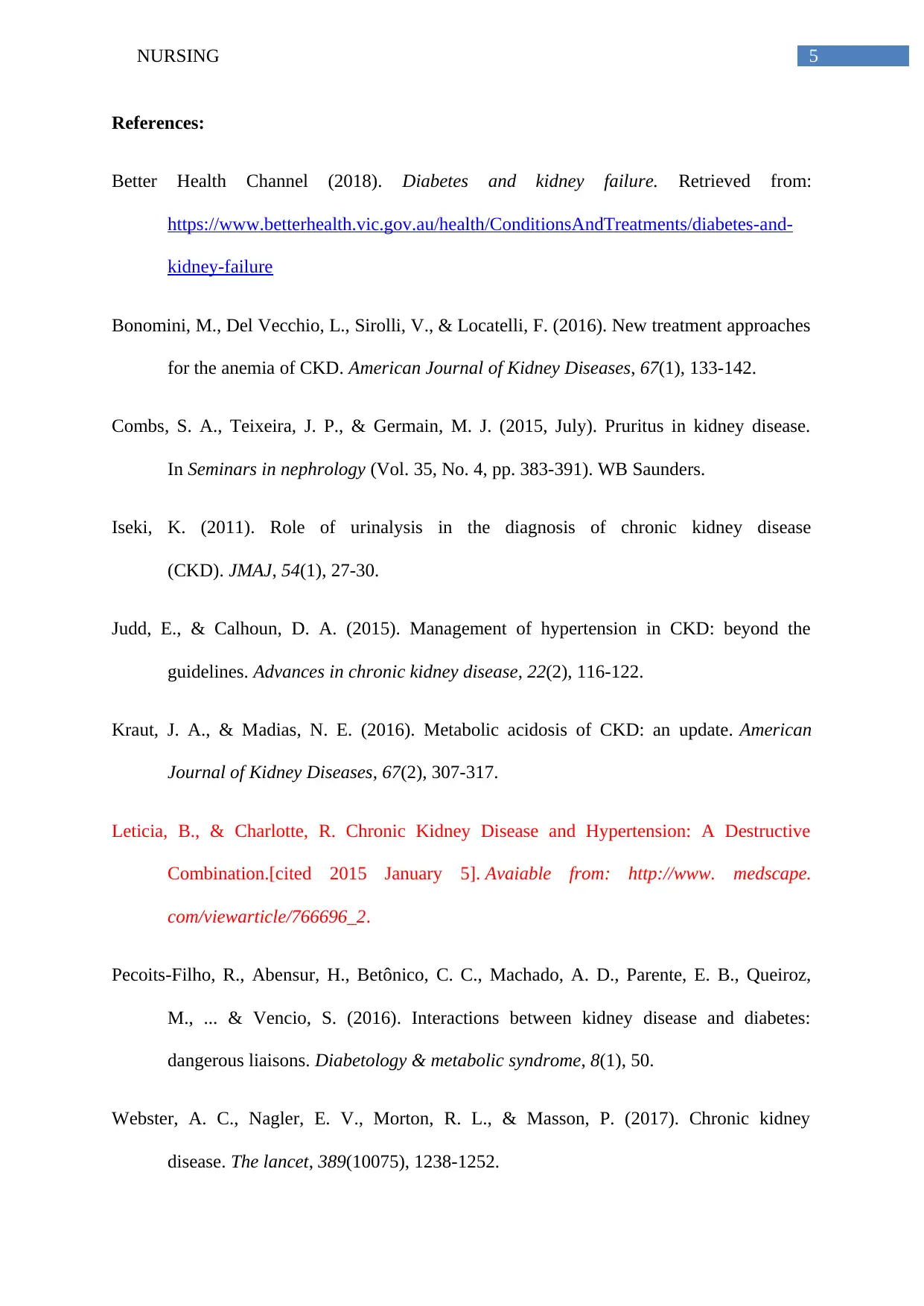
Chronic kidney
disease
Risk factors
Etiology
Pathophysiology
Clinical manifestations
Diagnostics
Treatment
Diabetes
Polycsytic
kidney disease
Glomerulonephritis High blood pressure
Diabetes
Decrease in renal
glucose excretion
Loss of nephrons
Hyperfiltration at the glomerulus
Activation of RAAS
Proteinuria
Nephrotoxic inflammation
Decrease in GFR
Pruritus or itching
Accumulation of waste products
Sodium and water retention
Edema
Decrease in production of
erythropoietin hormone
Anemia
Fatigue
Increase in urine
output
Urine test
Blood test
Ultrasound scan
Diuretics Itchy skin
Decline in kidney function
Accumulation of urea in the blood
Uremic toxicity
GFR value less
than 20 to 25
mL/min/1.73
m2
ACE inhibitors
and statins
Hypertension
Erythropoeitin stimulating
agent and iron supplements
Diet modification
Chronic kidney
disease
Risk factors
Etiology
Pathophysiology
Clinical manifestations
Diagnostics
Treatment
Diabetes
Polycsytic
kidney disease
Glomerulonephritis High blood pressure
Diabetes
Decrease in renal
glucose excretion
Loss of nephrons
Hyperfiltration at the glomerulus
Activation of RAAS
Proteinuria
Nephrotoxic inflammation
Decrease in GFR
Pruritus or itching
Accumulation of waste products
Sodium and water retention
Edema
Decrease in production of
erythropoietin hormone
Anemia
Fatigue
Increase in urine
output
Urine test
Blood test
Ultrasound scan
Diuretics Itchy skin
Decline in kidney function
Accumulation of urea in the blood
Uremic toxicity
GFR value less
than 20 to 25
mL/min/1.73
m2
ACE inhibitors
and statins
Hypertension
Erythropoeitin stimulating
agent and iron supplements
Diet modification
2NURSING
Relation between the disease risk factors and aetiology to the disease pathophysiology:
The case study is about Steve McManus who came to the GP with symptoms of
fatigue and itchy skin. He has been diagnosed with chronic kidney disease due to diffuse
nephron loss. Chronic kidney disease (CKD) is a clinical condition caused by long term
progressive and permanent loss of nephrons. In Steve’s case too, the risk of chronic kidney
disease increased because of long standing history of type 2 diabetes and hypertension. As
diabetes cause damage to the nerves and small blood vessels, it damages the small blood
vessels of the kidney resulting in water retention and swelling. Diabetic nephropathy or
diagnosis of kidney disease in patients with diabetes occurs because of interaction between
the metabolic and the hemodynamic pathways. The alteration of metabolic and hemodynamic
abnormalities and hemodynamic pathways result in inhibition of the various pathways and
various functional and structural changes contributing to albuminuria and renal function
decline. In addition, chronic kidney disease is often linked to presence of hypertension in an
individual because uncontrolled hypertension is associated with rapid progression of chronic
kidney disease and exacerbation of renal function because of volume expanasion and increase
in systemic vascular resistance. High blood pressure lead to intraglomerular pressure and
increase in protein filtration contributing to albuminaria. In many patient, proteinuria
develops due to progression of CKD and it contributes to poor prognosis of kidney disease
(Leticia & Charlotte, 2015). For this reason, blood pressure is prioritized in treatment of
patients with CKD (Judd & Calhoun, 2015). Hyperlipidemia is one of the risk factor of CKD
and patients with hypelipidemia are highly likely to suffer from CKD because of decrease in
HDL level. Therefore, history of diabetes, hyperlipidemia and hypertension has been
identified as a major risk factor of CKD in Steve’s case.
Relation between the disease risk factors and aetiology to the disease pathophysiology:
The case study is about Steve McManus who came to the GP with symptoms of
fatigue and itchy skin. He has been diagnosed with chronic kidney disease due to diffuse
nephron loss. Chronic kidney disease (CKD) is a clinical condition caused by long term
progressive and permanent loss of nephrons. In Steve’s case too, the risk of chronic kidney
disease increased because of long standing history of type 2 diabetes and hypertension. As
diabetes cause damage to the nerves and small blood vessels, it damages the small blood
vessels of the kidney resulting in water retention and swelling. Diabetic nephropathy or
diagnosis of kidney disease in patients with diabetes occurs because of interaction between
the metabolic and the hemodynamic pathways. The alteration of metabolic and hemodynamic
abnormalities and hemodynamic pathways result in inhibition of the various pathways and
various functional and structural changes contributing to albuminuria and renal function
decline. In addition, chronic kidney disease is often linked to presence of hypertension in an
individual because uncontrolled hypertension is associated with rapid progression of chronic
kidney disease and exacerbation of renal function because of volume expanasion and increase
in systemic vascular resistance. High blood pressure lead to intraglomerular pressure and
increase in protein filtration contributing to albuminaria. In many patient, proteinuria
develops due to progression of CKD and it contributes to poor prognosis of kidney disease
(Leticia & Charlotte, 2015). For this reason, blood pressure is prioritized in treatment of
patients with CKD (Judd & Calhoun, 2015). Hyperlipidemia is one of the risk factor of CKD
and patients with hypelipidemia are highly likely to suffer from CKD because of decrease in
HDL level. Therefore, history of diabetes, hyperlipidemia and hypertension has been
identified as a major risk factor of CKD in Steve’s case.
3NURSING
Link between disease pathophysiology and clinical manifestation:
Steve has been diagnosed with CKD. Changes in pathophysiology of kidney functions
manifest to produce different clinical manifestations in the patient. CKD is associated with
diminished renal reserve which ultimately progress to renal failure. The decrease in renal
function has an impact on kidney’s ability to maintain fluid and electrolyte homeostasis. The
disease progression starts with decrease in nephron numbers and hyperfiltration. Elevated
arterial pressure result in activation of RAAS (renin-angiotensin-aldosterone system) causing
proteinuria. Proteinuria is a condition associated with excessive protein excretion in the urine
and increase in protein uptake at the tubules results in inflammation of the glomerulus and
tubulus. These pathophysiological changes contribute result in reduction in functional renal
mass. The remaining nephrons begins a process of irreversible scelerosis leading to
progressive decline in GFR level (Glomerular Filration rate) and initiation of other systemic
complications (Webster et al., 2017). Hence, reduction in GFR is one of the major
pathophysiological changes following CKD.
With the decrease in GFR, a hyperbolic rise in plasma concentration of creatinine and
urea is seen. Kidney damage also results in accumulation of toxins and abnormal metabolism
of calcium and phosphorus (Combs, Teixeira & Germain, 2015, July). All these changes
contribute to manifestations of itching skin which was observed by Steve too. Secondary
sodium and water retention is also seen because of decrease in atrial natriuretic peptide
(ANP). Sodium and water retention manifests in the form of clinical symptoms of edema or
accumulation of water in the legs or foot of patient. The clinical symptom of edema was
found for Steve too as his leg was swollen at the end of the day. Kidney plays a major role in
maintaining acid-base balance too. However, during the course of CKD, decrease in renal
ammonium excretion occurs after decrease in GFR to less than 20 to 25 mL/min/1.73 m2 and
this results in decrease in serum bicarbonate concentration too (Kraut & Madias, 2016). This
Link between disease pathophysiology and clinical manifestation:
Steve has been diagnosed with CKD. Changes in pathophysiology of kidney functions
manifest to produce different clinical manifestations in the patient. CKD is associated with
diminished renal reserve which ultimately progress to renal failure. The decrease in renal
function has an impact on kidney’s ability to maintain fluid and electrolyte homeostasis. The
disease progression starts with decrease in nephron numbers and hyperfiltration. Elevated
arterial pressure result in activation of RAAS (renin-angiotensin-aldosterone system) causing
proteinuria. Proteinuria is a condition associated with excessive protein excretion in the urine
and increase in protein uptake at the tubules results in inflammation of the glomerulus and
tubulus. These pathophysiological changes contribute result in reduction in functional renal
mass. The remaining nephrons begins a process of irreversible scelerosis leading to
progressive decline in GFR level (Glomerular Filration rate) and initiation of other systemic
complications (Webster et al., 2017). Hence, reduction in GFR is one of the major
pathophysiological changes following CKD.
With the decrease in GFR, a hyperbolic rise in plasma concentration of creatinine and
urea is seen. Kidney damage also results in accumulation of toxins and abnormal metabolism
of calcium and phosphorus (Combs, Teixeira & Germain, 2015, July). All these changes
contribute to manifestations of itching skin which was observed by Steve too. Secondary
sodium and water retention is also seen because of decrease in atrial natriuretic peptide
(ANP). Sodium and water retention manifests in the form of clinical symptoms of edema or
accumulation of water in the legs or foot of patient. The clinical symptom of edema was
found for Steve too as his leg was swollen at the end of the day. Kidney plays a major role in
maintaining acid-base balance too. However, during the course of CKD, decrease in renal
ammonium excretion occurs after decrease in GFR to less than 20 to 25 mL/min/1.73 m2 and
this results in decrease in serum bicarbonate concentration too (Kraut & Madias, 2016). This
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4NURSING
results in metabolic acidosis for patients and this was observed during physical examination
of Steve too. In addition, the symptom of fatigue manifests because of anemia that occurs due
to lesser production of erythropoietin hormone by the damage kidneys and reduction in
functional renal mass.
Diagnostic test and treatment modalities for the diagnosed disorder:
In response to the issue of chronic kidney disease and presence of symptoms of edema
and worsening fatigue, it is suggested to conduct diagnostic investigations related to urine
test, blood test and imaging test. The main rationale behind the use of urine test is to evaluate
abnormalities in kidney function by detecting increase in urine protein levels because of
progression of the disease (Webster et al., 2011). According to Iseki (2011), urinalysis and
serum creatinine test is recommended to identify symptoms of proteinuria, decrease in GFR
(<50 ml/min/1.73 m2) and positive results for proteinuria. In addition, blood test is
recommended to patients with CKD to identify accumulation of waste products such as
creatinine and urea in the blood because of renal damage. Apart from the above two test,
ultrasound scan is also done to assess the structure of kidney and estimate level of damage to
the kidneys. Assessment of symptoms of edema, fatigue, weight loss and frequent urination
further confirms the diagnosis of CKD (Webster et al., 2011).
The treatment modalities that follow following the diagnosis include initiating
pharmacological treatment to control blood pressure, treat anemia, retain fluids and reduce
cholesterol level. Use of diuretics can reduce symptom of swelling for Steve. In addition, use
of angiotensin converting enzymes can maintain blood pressure and balance change in
electrolyte levels (Wu et al., 2016). Erthropoietin supplements can be recommended to Steve
in case of severe anemia (Bonomini et al., 2016).
results in metabolic acidosis for patients and this was observed during physical examination
of Steve too. In addition, the symptom of fatigue manifests because of anemia that occurs due
to lesser production of erythropoietin hormone by the damage kidneys and reduction in
functional renal mass.
Diagnostic test and treatment modalities for the diagnosed disorder:
In response to the issue of chronic kidney disease and presence of symptoms of edema
and worsening fatigue, it is suggested to conduct diagnostic investigations related to urine
test, blood test and imaging test. The main rationale behind the use of urine test is to evaluate
abnormalities in kidney function by detecting increase in urine protein levels because of
progression of the disease (Webster et al., 2011). According to Iseki (2011), urinalysis and
serum creatinine test is recommended to identify symptoms of proteinuria, decrease in GFR
(<50 ml/min/1.73 m2) and positive results for proteinuria. In addition, blood test is
recommended to patients with CKD to identify accumulation of waste products such as
creatinine and urea in the blood because of renal damage. Apart from the above two test,
ultrasound scan is also done to assess the structure of kidney and estimate level of damage to
the kidneys. Assessment of symptoms of edema, fatigue, weight loss and frequent urination
further confirms the diagnosis of CKD (Webster et al., 2011).
The treatment modalities that follow following the diagnosis include initiating
pharmacological treatment to control blood pressure, treat anemia, retain fluids and reduce
cholesterol level. Use of diuretics can reduce symptom of swelling for Steve. In addition, use
of angiotensin converting enzymes can maintain blood pressure and balance change in
electrolyte levels (Wu et al., 2016). Erthropoietin supplements can be recommended to Steve
in case of severe anemia (Bonomini et al., 2016).
5NURSING
References:
Better Health Channel (2018). Diabetes and kidney failure. Retrieved from:
https://www.betterhealth.vic.gov.au/health/ConditionsAndTreatments/diabetes-and-
kidney-failure
Bonomini, M., Del Vecchio, L., Sirolli, V., & Locatelli, F. (2016). New treatment approaches
for the anemia of CKD. American Journal of Kidney Diseases, 67(1), 133-142.
Combs, S. A., Teixeira, J. P., & Germain, M. J. (2015, July). Pruritus in kidney disease.
In Seminars in nephrology (Vol. 35, No. 4, pp. 383-391). WB Saunders.
Iseki, K. (2011). Role of urinalysis in the diagnosis of chronic kidney disease
(CKD). JMAJ, 54(1), 27-30.
Judd, E., & Calhoun, D. A. (2015). Management of hypertension in CKD: beyond the
guidelines. Advances in chronic kidney disease, 22(2), 116-122.
Kraut, J. A., & Madias, N. E. (2016). Metabolic acidosis of CKD: an update. American
Journal of Kidney Diseases, 67(2), 307-317.
Leticia, B., & Charlotte, R. Chronic Kidney Disease and Hypertension: A Destructive
Combination.[cited 2015 January 5]. Avaiable from: http://www. medscape.
com/viewarticle/766696_2.
Pecoits-Filho, R., Abensur, H., Betônico, C. C., Machado, A. D., Parente, E. B., Queiroz,
M., ... & Vencio, S. (2016). Interactions between kidney disease and diabetes:
dangerous liaisons. Diabetology & metabolic syndrome, 8(1), 50.
Webster, A. C., Nagler, E. V., Morton, R. L., & Masson, P. (2017). Chronic kidney
disease. The lancet, 389(10075), 1238-1252.
References:
Better Health Channel (2018). Diabetes and kidney failure. Retrieved from:
https://www.betterhealth.vic.gov.au/health/ConditionsAndTreatments/diabetes-and-
kidney-failure
Bonomini, M., Del Vecchio, L., Sirolli, V., & Locatelli, F. (2016). New treatment approaches
for the anemia of CKD. American Journal of Kidney Diseases, 67(1), 133-142.
Combs, S. A., Teixeira, J. P., & Germain, M. J. (2015, July). Pruritus in kidney disease.
In Seminars in nephrology (Vol. 35, No. 4, pp. 383-391). WB Saunders.
Iseki, K. (2011). Role of urinalysis in the diagnosis of chronic kidney disease
(CKD). JMAJ, 54(1), 27-30.
Judd, E., & Calhoun, D. A. (2015). Management of hypertension in CKD: beyond the
guidelines. Advances in chronic kidney disease, 22(2), 116-122.
Kraut, J. A., & Madias, N. E. (2016). Metabolic acidosis of CKD: an update. American
Journal of Kidney Diseases, 67(2), 307-317.
Leticia, B., & Charlotte, R. Chronic Kidney Disease and Hypertension: A Destructive
Combination.[cited 2015 January 5]. Avaiable from: http://www. medscape.
com/viewarticle/766696_2.
Pecoits-Filho, R., Abensur, H., Betônico, C. C., Machado, A. D., Parente, E. B., Queiroz,
M., ... & Vencio, S. (2016). Interactions between kidney disease and diabetes:
dangerous liaisons. Diabetology & metabolic syndrome, 8(1), 50.
Webster, A. C., Nagler, E. V., Morton, R. L., & Masson, P. (2017). Chronic kidney
disease. The lancet, 389(10075), 1238-1252.
6NURSING
Wu, L. S., Chang, S. H., Chang, G. J., Liu, J. R., Chan, Y. H., Lee, H. F., ... & See, L. C.
(2016). A comparison between angiotensin converting enzyme inhibitors and
angiotensin receptor blockers on end stage renal disease and major adverse
cardiovascular events in diabetic patients: a population-based dynamic cohort study in
Taiwan. Cardiovascular diabetology, 15(1), 56.
Wu, L. S., Chang, S. H., Chang, G. J., Liu, J. R., Chan, Y. H., Lee, H. F., ... & See, L. C.
(2016). A comparison between angiotensin converting enzyme inhibitors and
angiotensin receptor blockers on end stage renal disease and major adverse
cardiovascular events in diabetic patients: a population-based dynamic cohort study in
Taiwan. Cardiovascular diabetology, 15(1), 56.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





