PUBH6008 Research Proposal: Adherence, Readmission, & Cost Analysis
VerifiedAdded on 2022/10/17
|18
|3891
|26
Report
AI Summary
This research proposal aims to evaluate the relationship between adherence to drug prescriptions, readmission rates, and overall healthcare costs. It begins by highlighting the significance of medication adherence in reducing healthcare expenses and improving patient outcomes, noting the substantial financial burden of nonadherence. The proposal outlines the study's objectives, which include investigating the correlation between medication adherence and readmission rates, exploring the challenges posed by nonadherence, and identifying measures to improve adherence from both patient and healthcare provider perspectives. The literature review examines existing studies that demonstrate the impact of medication adherence on hospital admissions, healthcare costs, and patient outcomes, while also identifying gaps in the current research, such as the lack of qualitative analysis on patient behavior and perception. The proposal concludes by emphasizing the need for a psychological assessment of patient attitudes toward medication adherence to inform strategies for reducing nonadherence and improving healthcare efficiency. This document is available on Desklib, where students can find a wealth of resources including solved assignments and past papers.

RESEARCH PROPOSAL
EVALUATION THE INFLUENCE OF ADHERENCE TO DRUG PRESCRIPTION ON
READMISSION RATE AND OVERALL COST OF HEALTHCARE
BY
PROFESSORS/INSTRUCTOR
NAME OF THE UNIVERSITY
DATE OF SUBMISSION
EVALUATION THE INFLUENCE OF ADHERENCE TO DRUG PRESCRIPTION ON
READMISSION RATE AND OVERALL COST OF HEALTHCARE
BY
PROFESSORS/INSTRUCTOR
NAME OF THE UNIVERSITY
DATE OF SUBMISSION
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
INTRODUCTION.......................................................................................................................................3
Background.............................................................................................................................................3
Purpose of Study.....................................................................................................................................4
Rationale of the Study.............................................................................................................................5
Aim and Objectives.................................................................................................................................7
Research Question...................................................................................................................................7
LITERATURE REVIEW............................................................................................................................8
Review of Existing Studies......................................................................................................................8
Gaps in Literature..................................................................................................................................10
RESEARCH METHODOLOGY..............................................................................................................12
Methods.................................................................................................................................................12
Scope of the Review..............................................................................................................................12
Information Sources..............................................................................................................................12
Search strategy......................................................................................................................................13
Eligibility Criteria..................................................................................................................................13
Study inclusion criteria..........................................................................................................................13
Data Collection and Analysis................................................................................................................14
Risk of Bias...........................................................................................................................................14
Research Timeline.................................................................................................................................14
References.................................................................................................................................................16
INTRODUCTION.......................................................................................................................................3
Background.............................................................................................................................................3
Purpose of Study.....................................................................................................................................4
Rationale of the Study.............................................................................................................................5
Aim and Objectives.................................................................................................................................7
Research Question...................................................................................................................................7
LITERATURE REVIEW............................................................................................................................8
Review of Existing Studies......................................................................................................................8
Gaps in Literature..................................................................................................................................10
RESEARCH METHODOLOGY..............................................................................................................12
Methods.................................................................................................................................................12
Scope of the Review..............................................................................................................................12
Information Sources..............................................................................................................................12
Search strategy......................................................................................................................................13
Eligibility Criteria..................................................................................................................................13
Study inclusion criteria..........................................................................................................................13
Data Collection and Analysis................................................................................................................14
Risk of Bias...........................................................................................................................................14
Research Timeline.................................................................................................................................14
References.................................................................................................................................................16
INTRODUCTION
Background
Nonadherence to medication prescription is one of the leading public health issues that
affect the safety of patients and the overall cost of care to both healthcare facilities and patients.
According to a study conducted by Iuga and McGuire (2014), medication nonadherence
contributes significantly to the high cost of healthcare. As a result, having a practical framework
for adherence to medication prescription could improve patients' safety, lower the cost, and
reduce the length of admission for patients. Grantner, Romano, and Crosby (2019) note that the
proper use of prescription medication is an essential factor that lowers the cost of healthcare
services and promotes better health. Furthermore, several studies indicate that adhering to
medication regimens offer better prognosis in comparison to those who are not adherent (Burke
& Coleman, 2013; Omnicell, 2018; Miranda, Serag-Bolos, & Cooper, 2019).
Statistical data analyzed by Iuga and McGuire (2014) found that the healthcare system in
the United States exceeded 2.7 trillion representing 17.9% of the country's gross domestic
product. Further analysis revealed that 30% of the entire healthcare system is preventable since
its due to wasteful expenses. One of the areas of generating wastages is through medication
errors occurring due to ineffective administration of medication. Furthermore, Rosen et al.
(2017) note that for all medication-related causes of hospitalization in the United States,
nonadherence to medication prescription contributes to 33-69%. The nonadherence adds to over
$100 billion annually of the healthcare expenses. Another challenge in the healthcare system is
Background
Nonadherence to medication prescription is one of the leading public health issues that
affect the safety of patients and the overall cost of care to both healthcare facilities and patients.
According to a study conducted by Iuga and McGuire (2014), medication nonadherence
contributes significantly to the high cost of healthcare. As a result, having a practical framework
for adherence to medication prescription could improve patients' safety, lower the cost, and
reduce the length of admission for patients. Grantner, Romano, and Crosby (2019) note that the
proper use of prescription medication is an essential factor that lowers the cost of healthcare
services and promotes better health. Furthermore, several studies indicate that adhering to
medication regimens offer better prognosis in comparison to those who are not adherent (Burke
& Coleman, 2013; Omnicell, 2018; Miranda, Serag-Bolos, & Cooper, 2019).
Statistical data analyzed by Iuga and McGuire (2014) found that the healthcare system in
the United States exceeded 2.7 trillion representing 17.9% of the country's gross domestic
product. Further analysis revealed that 30% of the entire healthcare system is preventable since
its due to wasteful expenses. One of the areas of generating wastages is through medication
errors occurring due to ineffective administration of medication. Furthermore, Rosen et al.
(2017) note that for all medication-related causes of hospitalization in the United States,
nonadherence to medication prescription contributes to 33-69%. The nonadherence adds to over
$100 billion annually of the healthcare expenses. Another challenge in the healthcare system is
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
growing readmission penalties by the regulatory authorities, which leaves the hospitals with
struggling strategic plans to reduce the rate of readmission of patients (Hansen, Young, Hinami,
Leung, & Williams, 2011).
Despite the existence of a fundamental correlation between nonadherence to medication
and hospital readmission for patients, there lacks extensive assessment on the effects of
medication nonadherence. One study by Viswanathan et al. (2012) revealed that nonadherence is
a modifiable readmission predictor. Therefore, appropriate measures to reduce nonadherence
could positively impact patient experience and burden on hospitals by reducing treatment cost
and readmission rate. As such, identification of nonadherence patients in realtime could enhance
in attaining low cost of treatment and overall reduce the rate of readmission.
Purpose of the Study
The study aims at evaluating whether there exists a relationship between promoting
adherence to medication prescription on the rate of admission and cost of treatment. The
proposed research will explore nonadherence tools through consideration of the medication
behavior, adherence to medication barriers, and other associated behavior that promote
nonadherence. There is a need to examine whether nonadherence to drug prescription affects the
readmission rate and overall impact on the healthcare cost. Viswanathan et al. (2012) note that
though there exist efficacious medical treatments, there is a gap between the current practice
outcomes and desired state achievable. One of the critical elements identified by the study was
poor medication adherence. Viswanathan et al. (2012) argue that 20-30% of all medication
prescriptions are never administered as prescribed. Further findings from the study revealed that
50% of all medication prescription for chronic diseases are not taken as per the order. Therefore,
struggling strategic plans to reduce the rate of readmission of patients (Hansen, Young, Hinami,
Leung, & Williams, 2011).
Despite the existence of a fundamental correlation between nonadherence to medication
and hospital readmission for patients, there lacks extensive assessment on the effects of
medication nonadherence. One study by Viswanathan et al. (2012) revealed that nonadherence is
a modifiable readmission predictor. Therefore, appropriate measures to reduce nonadherence
could positively impact patient experience and burden on hospitals by reducing treatment cost
and readmission rate. As such, identification of nonadherence patients in realtime could enhance
in attaining low cost of treatment and overall reduce the rate of readmission.
Purpose of the Study
The study aims at evaluating whether there exists a relationship between promoting
adherence to medication prescription on the rate of admission and cost of treatment. The
proposed research will explore nonadherence tools through consideration of the medication
behavior, adherence to medication barriers, and other associated behavior that promote
nonadherence. There is a need to examine whether nonadherence to drug prescription affects the
readmission rate and overall impact on the healthcare cost. Viswanathan et al. (2012) note that
though there exist efficacious medical treatments, there is a gap between the current practice
outcomes and desired state achievable. One of the critical elements identified by the study was
poor medication adherence. Viswanathan et al. (2012) argue that 20-30% of all medication
prescriptions are never administered as prescribed. Further findings from the study revealed that
50% of all medication prescription for chronic diseases are not taken as per the order. Therefore,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
understanding the relationship between nonadherence on readmission rate and cost of medication
could help in determining strategic focus on prevention of nonadherence.
Rationale of the Study
Nonadherence is a critical topic for healthcare facilities and health professionals with
high commitment to reducing medication errors and avoidable causes for readmission that
escalate the overall cost of healthcare. Elliott (2013) explores the nonadherence in the United
Kingdom through consideration of how adherence to medication prescribed could enhance
improvement and reduction in cost by eliminating wastage in medicine. From the article, the
graph shown below indicates the significance of understanding the influence of adherence on the
cost of treatment and rate of readmission. From the chart below on worldwide estimates for
avoidable costs, nonadherence was considered to contribute to 57% of all preventable expenses.
This means that adherence to prescribed medication could significantly reduce the cost of
healthcare. The 57% nonadherence contribution to avoidable costs in the healthcare system
globally represent a US$269 billion of the total preventable expenses amounting to US$475
billion.
could help in determining strategic focus on prevention of nonadherence.
Rationale of the Study
Nonadherence is a critical topic for healthcare facilities and health professionals with
high commitment to reducing medication errors and avoidable causes for readmission that
escalate the overall cost of healthcare. Elliott (2013) explores the nonadherence in the United
Kingdom through consideration of how adherence to medication prescribed could enhance
improvement and reduction in cost by eliminating wastage in medicine. From the article, the
graph shown below indicates the significance of understanding the influence of adherence on the
cost of treatment and rate of readmission. From the chart below on worldwide estimates for
avoidable costs, nonadherence was considered to contribute to 57% of all preventable expenses.
This means that adherence to prescribed medication could significantly reduce the cost of
healthcare. The 57% nonadherence contribution to avoidable costs in the healthcare system
globally represent a US$269 billion of the total preventable expenses amounting to US$475
billion.
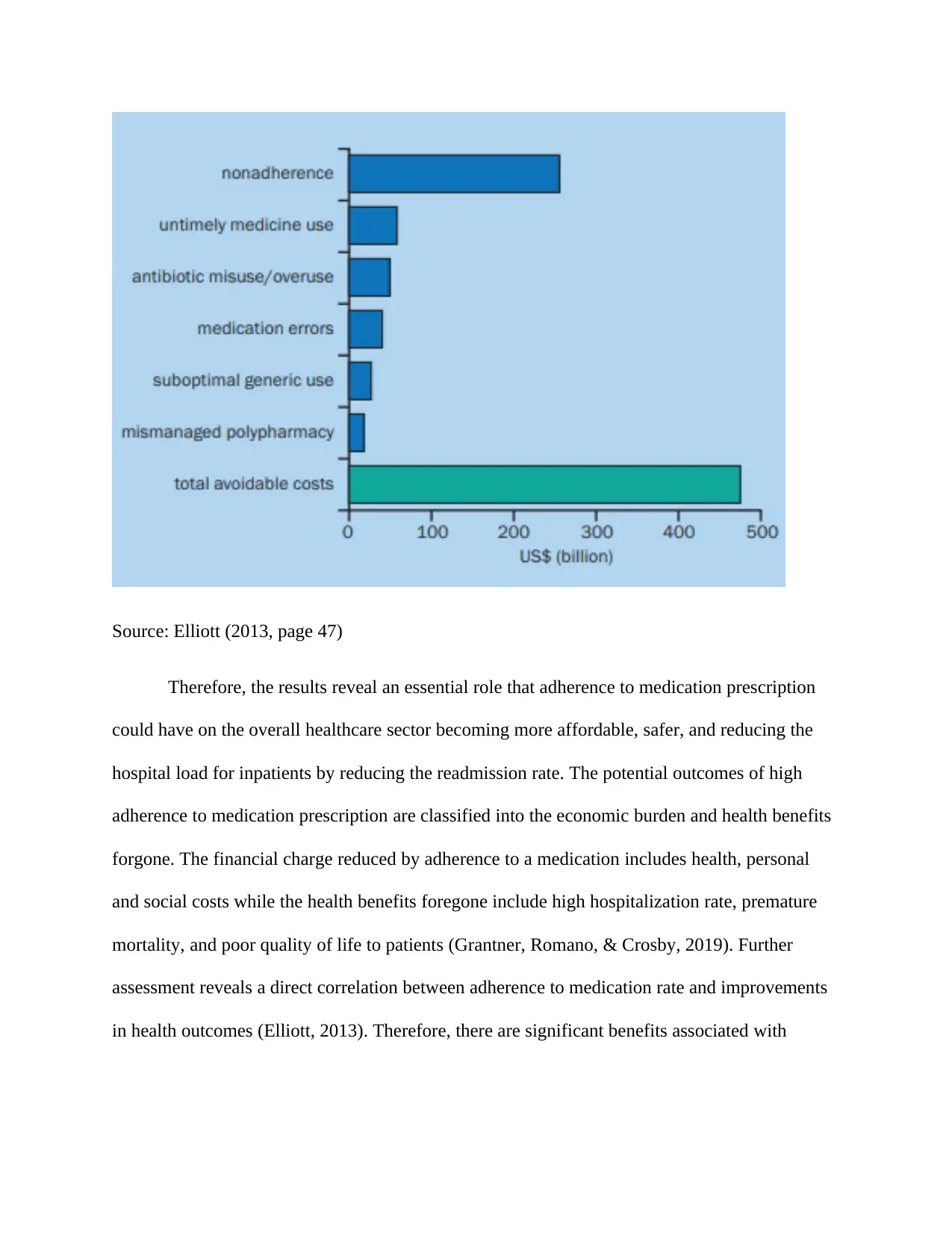
Source: Elliott (2013, page 47)
Therefore, the results reveal an essential role that adherence to medication prescription
could have on the overall healthcare sector becoming more affordable, safer, and reducing the
hospital load for inpatients by reducing the readmission rate. The potential outcomes of high
adherence to medication prescription are classified into the economic burden and health benefits
forgone. The financial charge reduced by adherence to a medication includes health, personal
and social costs while the health benefits foregone include high hospitalization rate, premature
mortality, and poor quality of life to patients (Grantner, Romano, & Crosby, 2019). Further
assessment reveals a direct correlation between adherence to medication rate and improvements
in health outcomes (Elliott, 2013). Therefore, there are significant benefits associated with
Therefore, the results reveal an essential role that adherence to medication prescription
could have on the overall healthcare sector becoming more affordable, safer, and reducing the
hospital load for inpatients by reducing the readmission rate. The potential outcomes of high
adherence to medication prescription are classified into the economic burden and health benefits
forgone. The financial charge reduced by adherence to a medication includes health, personal
and social costs while the health benefits foregone include high hospitalization rate, premature
mortality, and poor quality of life to patients (Grantner, Romano, & Crosby, 2019). Further
assessment reveals a direct correlation between adherence to medication rate and improvements
in health outcomes (Elliott, 2013). Therefore, there are significant benefits associated with
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
compliance through adherence to medication prescription on both health outcomes and economic
benefits.
Aim and Objectives
The aim of the study is evaluating the relationship between drug prescription adherence
on readmission rate and overall cost of healthcare. To meet the objective, the proposed research
will explore the following purposes:
1. Study the relationship between prescribed medication adherence with the rate of
readmission of patients and the overall cost of healthcare
2. Study whether nonadherence is a significant challenge for healthcare systems and
whether it is a severe cause for alarm by health professionals and policymakers
3. Explore how adherence affects readmission rate and how it impacts the overall healthcare
sector
4. Explore how adherence to prescribed medication affect the cost of the global healthcare
sector
5. Study appropriate measures that can reduce nonadherence in the healthcare setting from
both patient and healthcare service providers perspectives
Research Question
The research will use the research questions as the guide to better address the concept of
adherence to medication prescription on both costs of healthcare and readmission rate for
patients. The following research questions will guide the researcher in the collection, analysis,
and discussion of the research to effectively and holistically address all the segments of the
study.
benefits.
Aim and Objectives
The aim of the study is evaluating the relationship between drug prescription adherence
on readmission rate and overall cost of healthcare. To meet the objective, the proposed research
will explore the following purposes:
1. Study the relationship between prescribed medication adherence with the rate of
readmission of patients and the overall cost of healthcare
2. Study whether nonadherence is a significant challenge for healthcare systems and
whether it is a severe cause for alarm by health professionals and policymakers
3. Explore how adherence affects readmission rate and how it impacts the overall healthcare
sector
4. Explore how adherence to prescribed medication affect the cost of the global healthcare
sector
5. Study appropriate measures that can reduce nonadherence in the healthcare setting from
both patient and healthcare service providers perspectives
Research Question
The research will use the research questions as the guide to better address the concept of
adherence to medication prescription on both costs of healthcare and readmission rate for
patients. The following research questions will guide the researcher in the collection, analysis,
and discussion of the research to effectively and holistically address all the segments of the
study.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1. What is the relationship between prescribed medication adherence with the rate of
readmission of patients and the overall cost of healthcare?
2. Is nonadherence a significant challenge for healthcare systems does it have a serious
cause for alarm by health professionals and policymakers?
3. How does adherence to medication prescription affect readmission rate in the healthcare
sector?
4. How does adherence to prescribed medication affect the cost of the overall healthcare
sector?
5. What measures can reduce nonadherence in the healthcare setting from both patient and
healthcare service providers perspectives to reduce readmission rate and cost?
LITERATURE REVIEW
Review of Existing Studies
The researcher will review several studies to explore the influence of adherence to
medication on readmission rate and cost of treatment in the healthcare setting. Some of the
articles to review will be briefly explained in this section. The first study to consider will be by
Rosenet et al. (2017), which explore how patient medication adherence influences hospital
admission and readmissions. The study used a retrogressive cohort design in evaluating whether
patient adherence to medication had any influence on the readmission of patients with chronic
readmission of patients and the overall cost of healthcare?
2. Is nonadherence a significant challenge for healthcare systems does it have a serious
cause for alarm by health professionals and policymakers?
3. How does adherence to medication prescription affect readmission rate in the healthcare
sector?
4. How does adherence to prescribed medication affect the cost of the overall healthcare
sector?
5. What measures can reduce nonadherence in the healthcare setting from both patient and
healthcare service providers perspectives to reduce readmission rate and cost?
LITERATURE REVIEW
Review of Existing Studies
The researcher will review several studies to explore the influence of adherence to
medication on readmission rate and cost of treatment in the healthcare setting. Some of the
articles to review will be briefly explained in this section. The first study to consider will be by
Rosenet et al. (2017), which explore how patient medication adherence influences hospital
admission and readmissions. The study used a retrogressive cohort design in evaluating whether
patient adherence to medication had any influence on the readmission of patients with chronic
conditions and illnesses. The objective was attainable through a Morisky Medication Adherence
Scale (MMAS-4) administered during the hospital admission as a predictor of whether a patient
got readmission within 30 days. The results of this study indicated that patients who had low and
intermediate adherence rate had a readmission rate prediction of 20% in comparison to patients
with high adherence rate at 9.3% readmission rate. The further analysis with MMAS-4 revealed
that patients with low to moderate adherence rate to medication were 2.5 higher to have
readmission in comparison with those with high adherence rate. Therefore, high adherence to
medication resulted in low chances of getting hospital readmission.
The second study that the research will review is by Dilokthornsakul et al. (2016), which
evaluated the impact of medication adherence on direct healthcare cost and hospitalization to
patients diagnosed with schizophrenia in Thailand. The study applied a retrogressive quasi-
experimental design involving patients aged between 18–65 years. The outcomes of the study
indicated that the experimental group (optimal adherence) only three patients in a population of
224patients got readmission representing only 1.3%. However, the control group (under-
adherence) indicated seven readmissions out of a population of 218, which represented 3.2%.
The second element tested in the experimental study was direct healthcare cost. The
experimental group in the survey indicated a US$371 ± US$836 for optimal adherence against
US$386 ± US$734 for under adherence and US$508 ± US$2168 for the over adherence. The
results indicated that optimal adherence to medication could lower both the rate of readmission
as well as reduce the direct cost of healthcare.
The third study by Brown et al. (2016) evaluating the truths about medication adherence
and potential consequences. The research focused on the evaluation of how medication
adherence influences the healthcare system in terms of cost and outcome on the readmission rate
Scale (MMAS-4) administered during the hospital admission as a predictor of whether a patient
got readmission within 30 days. The results of this study indicated that patients who had low and
intermediate adherence rate had a readmission rate prediction of 20% in comparison to patients
with high adherence rate at 9.3% readmission rate. The further analysis with MMAS-4 revealed
that patients with low to moderate adherence rate to medication were 2.5 higher to have
readmission in comparison with those with high adherence rate. Therefore, high adherence to
medication resulted in low chances of getting hospital readmission.
The second study that the research will review is by Dilokthornsakul et al. (2016), which
evaluated the impact of medication adherence on direct healthcare cost and hospitalization to
patients diagnosed with schizophrenia in Thailand. The study applied a retrogressive quasi-
experimental design involving patients aged between 18–65 years. The outcomes of the study
indicated that the experimental group (optimal adherence) only three patients in a population of
224patients got readmission representing only 1.3%. However, the control group (under-
adherence) indicated seven readmissions out of a population of 218, which represented 3.2%.
The second element tested in the experimental study was direct healthcare cost. The
experimental group in the survey indicated a US$371 ± US$836 for optimal adherence against
US$386 ± US$734 for under adherence and US$508 ± US$2168 for the over adherence. The
results indicated that optimal adherence to medication could lower both the rate of readmission
as well as reduce the direct cost of healthcare.
The third study by Brown et al. (2016) evaluating the truths about medication adherence
and potential consequences. The research focused on the evaluation of how medication
adherence influences the healthcare system in terms of cost and outcome on the readmission rate
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
for patients. The first findings were that over 50% of patients taking prescription medication get
nonadherent at least once during the entire period of drugs. One of the reasons identified for
nonadherence were forgetfulness and lack of access. However, the researcher asserted that
intentional choices by a patient could also precipitate nonadherence. The review found that the
main predictors of adherence to medication included communication, trust, and empathy that can
not be directly measured through the administrative databases. From the study, a multifactorial
approach was vital in improving adherence by educating patients on medication benefits, having
trust on medication manufacturers and health practitioners, having confidence in healthcare
systems, and creating public awareness on the significance of proper adherence to medication.
Gaps in Literature
While there exist several studies conducted on adherence to medications involving
experimental and quantitative designs, there lack in-depth studies. These studies should have
evaluated the qualitative factors influencing adherence to medication by assessing the essential
perceptual and emotional elements of the patients towards optimal adherence to drugs. Sufficient
evidence from the literature reveals the use of optimal adherence to prescription medication in
reducing readmission rate and lowering cost of healthcare (Elliott, 2013; Iuga & McGuire, 2014;
Omnicell, 2018; Grantner, Romano, & Crosby, 2019). However, little research focused on
evaluating non-statistical or nonnumerical aspects like behavior and perception of health
practitioners and patients regarding the adherence to medication. Additionally, there are no
definitive research studies on the overall cost of healthcare due to adherence issues in a
healthcare setting. The current research focuses on a psychological assessment of behavior and
perception of patients towards the adherence to medication.
nonadherent at least once during the entire period of drugs. One of the reasons identified for
nonadherence were forgetfulness and lack of access. However, the researcher asserted that
intentional choices by a patient could also precipitate nonadherence. The review found that the
main predictors of adherence to medication included communication, trust, and empathy that can
not be directly measured through the administrative databases. From the study, a multifactorial
approach was vital in improving adherence by educating patients on medication benefits, having
trust on medication manufacturers and health practitioners, having confidence in healthcare
systems, and creating public awareness on the significance of proper adherence to medication.
Gaps in Literature
While there exist several studies conducted on adherence to medications involving
experimental and quantitative designs, there lack in-depth studies. These studies should have
evaluated the qualitative factors influencing adherence to medication by assessing the essential
perceptual and emotional elements of the patients towards optimal adherence to drugs. Sufficient
evidence from the literature reveals the use of optimal adherence to prescription medication in
reducing readmission rate and lowering cost of healthcare (Elliott, 2013; Iuga & McGuire, 2014;
Omnicell, 2018; Grantner, Romano, & Crosby, 2019). However, little research focused on
evaluating non-statistical or nonnumerical aspects like behavior and perception of health
practitioners and patients regarding the adherence to medication. Additionally, there are no
definitive research studies on the overall cost of healthcare due to adherence issues in a
healthcare setting. The current research focuses on a psychological assessment of behavior and
perception of patients towards the adherence to medication.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
A study conducted by Brown and Bussell (2011) revealed that many patients with
chronic illnesses experience difficulties in medication adherence. The study recommended a
multifactorial approach in promoting high adherence to medication. Additionally, research
evaluated the factors pertinent to promotion of medication adherence, which found the most
common cause of nonadherence were socio-economic factors (support from caregivers, family
and relatives, living conditions, and level of education), relationship between patients, health
professionals and healthcare systems, condition of patients, therapy-related, and patient-related
factors. While the majority of the study focused on the role of healthcare professionals and
healthcare systems, there is an inadequate investigation of patient-related factors. To understand
the implications of cognitive limitations and physical impairments on adherence rate, the
researcher requires an in-depth examination of the patient-centered challenges in reducing
nonadherence cases. The most instrumental patient-related factors are close to perceptual,
emotive, and psychological influences that are identifiable through an in-depth assessment. The
critical elements in this category comprise of lack of motivation, substance abuse, self-efficacy,
and lack of knowledge of the condition or disease under treatment.
chronic illnesses experience difficulties in medication adherence. The study recommended a
multifactorial approach in promoting high adherence to medication. Additionally, research
evaluated the factors pertinent to promotion of medication adherence, which found the most
common cause of nonadherence were socio-economic factors (support from caregivers, family
and relatives, living conditions, and level of education), relationship between patients, health
professionals and healthcare systems, condition of patients, therapy-related, and patient-related
factors. While the majority of the study focused on the role of healthcare professionals and
healthcare systems, there is an inadequate investigation of patient-related factors. To understand
the implications of cognitive limitations and physical impairments on adherence rate, the
researcher requires an in-depth examination of the patient-centered challenges in reducing
nonadherence cases. The most instrumental patient-related factors are close to perceptual,
emotive, and psychological influences that are identifiable through an in-depth assessment. The
critical elements in this category comprise of lack of motivation, substance abuse, self-efficacy,
and lack of knowledge of the condition or disease under treatment.
RESEARCH METHODOLOGY
Methods
The study will review the impact of improper adherence to medication on readmission
rate and cost of healthcare through a systematic review. The systematic review involves use of
existing studies through an adequately executed framework. The systematic review will retrieve
previous studies on the influence of nonadherence to medication on the cost of healthcare and
readmission rate considering high-quality sources of information.
Scope of the review
The studies to be included as sources of data will be from a wide range of peer-review
articles on the influence of nonadherence to medication on readmission rate of patients and the
overall cost of healthcare. The studies to be used will be peer-reviewed articles that evaluate
specific details of the impact that nonadherence has on cost and readmission rate. The wide range
of studies will include randomized controlled trials, sysrematic reviews of controlled trials,
quasi-experimental studies, quantitative studies as well as the qualitative studies. These sources
of data offer in-depth insight into the correlation between nonadherence to medication on the
cost of healthcare and the readmission rate of patients. Majority of the studies will be systematic
reviews of randomized controlled trials, randomized control trials (RCTs), cohort studies, and
pre-post intervention studies.
Information Sources
The data for the study will involve a collection of peer-reviewed articles retrieved from
difference scientific databases on healthcare and nursing such as Medline (Ovid), EBSCOhost,
EMBASE (Ovid), Cumulative Index to Nursing and Allied Health Literature (CINAHL), llied
and Complementary Medicine Database, Cochrane, Scopus, and Education Resources for the
Methods
The study will review the impact of improper adherence to medication on readmission
rate and cost of healthcare through a systematic review. The systematic review involves use of
existing studies through an adequately executed framework. The systematic review will retrieve
previous studies on the influence of nonadherence to medication on the cost of healthcare and
readmission rate considering high-quality sources of information.
Scope of the review
The studies to be included as sources of data will be from a wide range of peer-review
articles on the influence of nonadherence to medication on readmission rate of patients and the
overall cost of healthcare. The studies to be used will be peer-reviewed articles that evaluate
specific details of the impact that nonadherence has on cost and readmission rate. The wide range
of studies will include randomized controlled trials, sysrematic reviews of controlled trials,
quasi-experimental studies, quantitative studies as well as the qualitative studies. These sources
of data offer in-depth insight into the correlation between nonadherence to medication on the
cost of healthcare and the readmission rate of patients. Majority of the studies will be systematic
reviews of randomized controlled trials, randomized control trials (RCTs), cohort studies, and
pre-post intervention studies.
Information Sources
The data for the study will involve a collection of peer-reviewed articles retrieved from
difference scientific databases on healthcare and nursing such as Medline (Ovid), EBSCOhost,
EMBASE (Ovid), Cumulative Index to Nursing and Allied Health Literature (CINAHL), llied
and Complementary Medicine Database, Cochrane, Scopus, and Education Resources for the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 18
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





