Assignment On Nursing Student Institution 2022
VerifiedAdded on 2022/09/16
|11
|3856
|19
Assignment
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Nursing
Student assignment
Institution
Student assignment
Institution
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Introduction
This report will discuss Alice McCallum's case study. The patient was admitted in the
hospital three days ago after being referred by her GP. She presented with confusion and an
increased risk of falls due to hyponatremia. On assessment during admission, she had a GCS of
14 and generalized weakness on both legs. She also presented with bilateral limb spasm. She was
managed on sodium chloride 0.9%, and the patient showed a marked improvement. However,
her condition worsened about an hour ago, and her GCS is 13, and the patient is confused and
feeling drowsy. The report will, therefore, discuss sepsis (infection) and fluid volume deficit as
the two actual problems presented by the patient. The pathophysiology of these conditions will
be discussed, and appropriate interventions needed to manage these conditions will be presented.
Goals and expected outcomes will also be presented together with how to evaluate.
1. Infection
Infection is caused by the entry of micro-organisms into the body of an individual mainly
due to break or altered body defence mechanisms such as the skin or insertion of foreign bodies
into the body. Most common micro-organisms are the bacteria. They include streptococcus,
staphylococcus, and pneumococcus. Others include viruses, protozoa and parasites such as
trachinalis spiralis (Gast &Porter 2020). These organisms enter the body and start multiplying.
The body recognizes micro-organism as foreign and initiates a response. The infection can be
either local or systemic or both. The body responds to a local infection through inflammation
(Kourtis et al. 2019).
Inflammation is the activation of the immune system due to stimulus usually micro-
organisms. This involves both the cellular and humoral components (Liu et al. 2017).
Inflammation has three phases which are the acute, sub-acute and chronic phases. The acute
phase, which usually lasts for about three days, is characterized by swelling, redness, pain, loss
of function and heat. This is caused by constriction of arterioles at the site of injury initially and
vasodilation and increased capillary permeability later. This is due to the release of chemical
mediators which relax the smooth muscles of arterioles. This leads to the exit of protein-rich
fluid into the interstitial space initiating an inflammatory response. This fluid contains plasma
components such as albumin, fibrinogen and kinins. This, therefore, leads to symptoms of
inflammation which include swelling, redness, pain, loss of function and heat (Ahmed et al.
2017)
This report will discuss Alice McCallum's case study. The patient was admitted in the
hospital three days ago after being referred by her GP. She presented with confusion and an
increased risk of falls due to hyponatremia. On assessment during admission, she had a GCS of
14 and generalized weakness on both legs. She also presented with bilateral limb spasm. She was
managed on sodium chloride 0.9%, and the patient showed a marked improvement. However,
her condition worsened about an hour ago, and her GCS is 13, and the patient is confused and
feeling drowsy. The report will, therefore, discuss sepsis (infection) and fluid volume deficit as
the two actual problems presented by the patient. The pathophysiology of these conditions will
be discussed, and appropriate interventions needed to manage these conditions will be presented.
Goals and expected outcomes will also be presented together with how to evaluate.
1. Infection
Infection is caused by the entry of micro-organisms into the body of an individual mainly
due to break or altered body defence mechanisms such as the skin or insertion of foreign bodies
into the body. Most common micro-organisms are the bacteria. They include streptococcus,
staphylococcus, and pneumococcus. Others include viruses, protozoa and parasites such as
trachinalis spiralis (Gast &Porter 2020). These organisms enter the body and start multiplying.
The body recognizes micro-organism as foreign and initiates a response. The infection can be
either local or systemic or both. The body responds to a local infection through inflammation
(Kourtis et al. 2019).
Inflammation is the activation of the immune system due to stimulus usually micro-
organisms. This involves both the cellular and humoral components (Liu et al. 2017).
Inflammation has three phases which are the acute, sub-acute and chronic phases. The acute
phase, which usually lasts for about three days, is characterized by swelling, redness, pain, loss
of function and heat. This is caused by constriction of arterioles at the site of injury initially and
vasodilation and increased capillary permeability later. This is due to the release of chemical
mediators which relax the smooth muscles of arterioles. This leads to the exit of protein-rich
fluid into the interstitial space initiating an inflammatory response. This fluid contains plasma
components such as albumin, fibrinogen and kinins. This, therefore, leads to symptoms of
inflammation which include swelling, redness, pain, loss of function and heat (Ahmed et al.
2017)
During the sub-acute phase, the phagocytic cells move to the site of injury. In response,
leukocytes, platelets and erythrocytes adhere to the endothelial cell surface. Neutrophils are the
first polymorphonuclear leucocytes to reach the site of the infection (Martinez et al. 2016). Then
followed by basophils and eosinophils and finally, the macrophages predominate. The
macrophages remove damaged tissues, and the repair face is followed if the cause of
inflammation is eliminated. If not, then the inflammation moves to chronic phase causing more
tissue destruction (Kikuchi et al. 2018).
Fever is the body’s response to an infection. An infection in the body activates cytokines
to induce an upward displacement of the temperature set point in the body to increase body
temperature. This is mediated with an increase in the synthesis of prostaglandins which act on
the hypothalamus to raise the temperature setpoint (Eldin et al. 2017). It is believed that an
increase in body temperature enhances immune function and inhibits pathogens growth.
Increased infiltration of polymorphonuclear leukocytes increases white blood cell count in the
body. This is because the cells are attempting to eliminate the infection-causing micro-
organisms. The patient shivers as a response to fever. This is because the body tries to generate
more heat.
The first nursing intervention is the administration of an antipyretic to reduce the fever
and also to expose the patient. Paracetamol can be used as an antipyretic agent. This is because
paracetamol inhibits the synthesis of prostaglandins; therefore, a decrease in temperature set
point. It also promotes heat loss through vasodilation of cutaneous blood vessels and sweating
helping to reset the hypothalamic set point. Very high temperatures can damage the brain. The
nurse should monitor for any side effects and toxicities that can arise due to administration of the
drug (Chiumello, Gotti & Vergani 2017).
Another intervention is the administration of antibiotics as prescribed. Broad-spectrum
antibiotics should be administered, but antibiotics sensitive to the organism should be
administered once specificity has been identified. Antibiotics such as Amoxicillin, ceftriaxone,
and ceftazidime. Can be administered to eliminate the organisms (Moon 2019). These drugs
target specific molecules that are present in infection-causing organisms but not in the body
cells. These include cell wall components, certain proteins such as the 30s and other components.
The drugs target these components causing the death of the organisms. Once destroyed, they are
eliminated by the body as waste products. Antibiotics are administered for a certain period of
leukocytes, platelets and erythrocytes adhere to the endothelial cell surface. Neutrophils are the
first polymorphonuclear leucocytes to reach the site of the infection (Martinez et al. 2016). Then
followed by basophils and eosinophils and finally, the macrophages predominate. The
macrophages remove damaged tissues, and the repair face is followed if the cause of
inflammation is eliminated. If not, then the inflammation moves to chronic phase causing more
tissue destruction (Kikuchi et al. 2018).
Fever is the body’s response to an infection. An infection in the body activates cytokines
to induce an upward displacement of the temperature set point in the body to increase body
temperature. This is mediated with an increase in the synthesis of prostaglandins which act on
the hypothalamus to raise the temperature setpoint (Eldin et al. 2017). It is believed that an
increase in body temperature enhances immune function and inhibits pathogens growth.
Increased infiltration of polymorphonuclear leukocytes increases white blood cell count in the
body. This is because the cells are attempting to eliminate the infection-causing micro-
organisms. The patient shivers as a response to fever. This is because the body tries to generate
more heat.
The first nursing intervention is the administration of an antipyretic to reduce the fever
and also to expose the patient. Paracetamol can be used as an antipyretic agent. This is because
paracetamol inhibits the synthesis of prostaglandins; therefore, a decrease in temperature set
point. It also promotes heat loss through vasodilation of cutaneous blood vessels and sweating
helping to reset the hypothalamic set point. Very high temperatures can damage the brain. The
nurse should monitor for any side effects and toxicities that can arise due to administration of the
drug (Chiumello, Gotti & Vergani 2017).
Another intervention is the administration of antibiotics as prescribed. Broad-spectrum
antibiotics should be administered, but antibiotics sensitive to the organism should be
administered once specificity has been identified. Antibiotics such as Amoxicillin, ceftriaxone,
and ceftazidime. Can be administered to eliminate the organisms (Moon 2019). These drugs
target specific molecules that are present in infection-causing organisms but not in the body
cells. These include cell wall components, certain proteins such as the 30s and other components.
The drugs target these components causing the death of the organisms. Once destroyed, they are
eliminated by the body as waste products. Antibiotics are administered for a certain period of
time, preferable 14 days in order to eliminate the organism fully. The nurse should, therefore,
ensure that the patient receives her medication in the right dosage, route and time as prescribed,
especially when the patient is confused. Drug adherence will help prevent resistance and quick
elimination of the disease-causing micro-organism (Gaal et al. 2016).
The third nursing intervention is practising aseptic technique to prevent further infection.
Sites of intravenous insertion should be dressed using aseptic technique and dressed with a sterile
dressing material. Any other procedure such as intravenous drug administration should also be
carried out using aseptic technique. This will prevent the introduction of micro-organisms to the
patient's body which is already weak (Team, 2019).
The first nursing goal is that the patient shall demonstrate a decrease in temperature to
37.2 at the end of one hour. This is after administration of paracetamol and exposing the patient.
This can be evaluated by taking the patients temperature after every 15 minutes to evaluate if the
temperature is decreasing. If there is no change in temperature or continued increase in
temperature, the intervention should be reviewed or changed to an appropriate one after
identifying the problem (Erickson, 2018).
Another goal is that the patient shall demonstrate a decrease in symptoms of
inflammation at the end of the shift and resolve of the symptoms at the end one week. Antibiotics
acts on the organisms responsible for the infection. Once the organisms are eliminated,
symptoms disappear. Daily evaluation should be taken obtaining both objective and subjective
data to identify any arising complications or improvement. This will enable the nurse to
implement the appropriate intervention as soon as possible to prevent complications and
facilitate quick recovery.
Any signs of new infection should always be observed at the site of intravenous insertion
or any other part.
2. Fluid volume deficit
The second actual problem is fluid volume deficit. The patent has a low blood pressure of
98/60 mmHg, tachycardia HR of 135 beats per minute, increased capillary refill time of 4
seconds and cool extremities (Tigabu et al. 2018). These signs are an indication of reduced fluid
volume in the body. Sodium plays an important role in increasing the amount of body fluid in the
body. Bendroflumethiazide is a diuretic agent and is used to reduce blood pressure by increasing
water loss through urination and inhibits sodium reabsorption.
ensure that the patient receives her medication in the right dosage, route and time as prescribed,
especially when the patient is confused. Drug adherence will help prevent resistance and quick
elimination of the disease-causing micro-organism (Gaal et al. 2016).
The third nursing intervention is practising aseptic technique to prevent further infection.
Sites of intravenous insertion should be dressed using aseptic technique and dressed with a sterile
dressing material. Any other procedure such as intravenous drug administration should also be
carried out using aseptic technique. This will prevent the introduction of micro-organisms to the
patient's body which is already weak (Team, 2019).
The first nursing goal is that the patient shall demonstrate a decrease in temperature to
37.2 at the end of one hour. This is after administration of paracetamol and exposing the patient.
This can be evaluated by taking the patients temperature after every 15 minutes to evaluate if the
temperature is decreasing. If there is no change in temperature or continued increase in
temperature, the intervention should be reviewed or changed to an appropriate one after
identifying the problem (Erickson, 2018).
Another goal is that the patient shall demonstrate a decrease in symptoms of
inflammation at the end of the shift and resolve of the symptoms at the end one week. Antibiotics
acts on the organisms responsible for the infection. Once the organisms are eliminated,
symptoms disappear. Daily evaluation should be taken obtaining both objective and subjective
data to identify any arising complications or improvement. This will enable the nurse to
implement the appropriate intervention as soon as possible to prevent complications and
facilitate quick recovery.
Any signs of new infection should always be observed at the site of intravenous insertion
or any other part.
2. Fluid volume deficit
The second actual problem is fluid volume deficit. The patent has a low blood pressure of
98/60 mmHg, tachycardia HR of 135 beats per minute, increased capillary refill time of 4
seconds and cool extremities (Tigabu et al. 2018). These signs are an indication of reduced fluid
volume in the body. Sodium plays an important role in increasing the amount of body fluid in the
body. Bendroflumethiazide is a diuretic agent and is used to reduce blood pressure by increasing
water loss through urination and inhibits sodium reabsorption.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Sodium is important in water reabsorption by the kidneys increasing amount of fluids and
blood pressure. This is achieved through the renin-angiotensin-aldosterone system. This is a
hormonal system which regulates blood pressure and fluid and electrolyte balance in the body.
When the blood supply to the kidney decreases, the kidney releases renin into the circulation.
Renin then converts the angiotensinogen to angiotensin I and to angiotensin II by angiotensin-
converting enzyme. Angiotensin II is a potent vasoconstrictor that narrows the blood vessels,
subsequently increasing blood pressure. It also stimulates aldosterone secretion from the adrenal
cortex. Aldosterone increases sodium reabsorption in the kidney tubules. Increased sodium
levels in the kidney tubules increase water reabsorption increasing blood pressure. Reduced
sodium level, therefore, does not produce this effect.
Bendroflumethiazide inhibits active chloride reabsorption via the Na-Cl cotransporter
leading to increased sodium excretion in the distal convoluted tubule. The drug also binds to the
sodium –chloride transporter leading to inhibition of transportation of sodium ion across the
renal tubular epithelium (Macfarlane et al. 2019). This increases sodium and potassium excretion
further. Increased sodium excretion and water excretion reduces body fluid amount. This causes
low blood pressure which, when prolonged, can progress to hypotensive shock. The patient is
presenting with a blood pressure of 98/60 mmHg, which is lower than normal (120/80-140/90
mmHg). The decrease in the amount of fluid or blood volume decreases ventricular filling and
subsequently, cardiac output. Decreased cardiac output leads to an increase in heart rate to
increase the amount of blood flow to the tissues. The patient has a heart rate of 135 beats per
minute (Normal 60-100 bpm) (Saleh, McGarry, Chaw, & Elkordy, 2018).
Decreased blood flow to the body tissues leads to a decrease in the amount of oxygen
supplied to the tissues SP02 93% (normal (95-100%). The body, therefore, responds by
increasing respiratory rate in order to increase oxygen levels in the tissues. The patient has a
respiratory rate of 25 breaths per minute (Normal 16-20 breaths per minute) (Kumar, 2018).
When the amount of blood in the body decreases, a greater percentage is delivered to the vital
organs such as the brain, the kidney and the heart. Therefore, the blood supply to the extremities
and the superficial organs is decreased. The patient has cool extremities due to decreased blood
flow to the extremities. Capillary refill time is also increased 4 seconds (normal <3 seconds) due
to reduced blood flow (Ait-Oufella &Bakker, 2016).
blood pressure. This is achieved through the renin-angiotensin-aldosterone system. This is a
hormonal system which regulates blood pressure and fluid and electrolyte balance in the body.
When the blood supply to the kidney decreases, the kidney releases renin into the circulation.
Renin then converts the angiotensinogen to angiotensin I and to angiotensin II by angiotensin-
converting enzyme. Angiotensin II is a potent vasoconstrictor that narrows the blood vessels,
subsequently increasing blood pressure. It also stimulates aldosterone secretion from the adrenal
cortex. Aldosterone increases sodium reabsorption in the kidney tubules. Increased sodium
levels in the kidney tubules increase water reabsorption increasing blood pressure. Reduced
sodium level, therefore, does not produce this effect.
Bendroflumethiazide inhibits active chloride reabsorption via the Na-Cl cotransporter
leading to increased sodium excretion in the distal convoluted tubule. The drug also binds to the
sodium –chloride transporter leading to inhibition of transportation of sodium ion across the
renal tubular epithelium (Macfarlane et al. 2019). This increases sodium and potassium excretion
further. Increased sodium excretion and water excretion reduces body fluid amount. This causes
low blood pressure which, when prolonged, can progress to hypotensive shock. The patient is
presenting with a blood pressure of 98/60 mmHg, which is lower than normal (120/80-140/90
mmHg). The decrease in the amount of fluid or blood volume decreases ventricular filling and
subsequently, cardiac output. Decreased cardiac output leads to an increase in heart rate to
increase the amount of blood flow to the tissues. The patient has a heart rate of 135 beats per
minute (Normal 60-100 bpm) (Saleh, McGarry, Chaw, & Elkordy, 2018).
Decreased blood flow to the body tissues leads to a decrease in the amount of oxygen
supplied to the tissues SP02 93% (normal (95-100%). The body, therefore, responds by
increasing respiratory rate in order to increase oxygen levels in the tissues. The patient has a
respiratory rate of 25 breaths per minute (Normal 16-20 breaths per minute) (Kumar, 2018).
When the amount of blood in the body decreases, a greater percentage is delivered to the vital
organs such as the brain, the kidney and the heart. Therefore, the blood supply to the extremities
and the superficial organs is decreased. The patient has cool extremities due to decreased blood
flow to the extremities. Capillary refill time is also increased 4 seconds (normal <3 seconds) due
to reduced blood flow (Ait-Oufella &Bakker, 2016).
The first nursing intervention is the administration of intravenous fluids to correct low
blood pressure (Perner 2018). Fluids commonly used include normal saline and ringers lactate.
The amount of fluids to be administered depends on the level of blood pressure and general
wellbeing of an individual. Administration of fluids increases the amount of body fluids which
promotes tissue perfusion and raises blood pressure to normal level (Montomoli, Donati &Ince,
2019). The nurse should calculate the number of drops to be delivered to the patient depending
on the time the fluid should run. The nurse should also monitor for any signs of fluid overload,
especially when the patient is not alert. Increase in the amount of body fluid increases cardiac
output and consequentially increase in the amount of oxygen delivered to the tissues. This will,
therefore, lead to a decrease in heart rate and respiratory rate to normal as a signal is sent to the
respiratory centre and heart rate regulatory centre (McClain & McManus, 2019).
The nurse can also administer oxygen to the patient. Oxygen supply helps in increasing
the amount of oxygen reaching the tissues, especially when blood levels are low. This promotes
tissue oxygenation and prevents tissue damage. This can also help in correcting acidosis (Parotto
et al. 2018).
The patient should also be encouraged to take fluids orally as soon as she tolerates. This
will help increase fluid volume further (Nohara et al. 2019).
The nursing goal is that the patient shall demonstrate a normotensive state within a period
of 2 hours. The patients’ blood pressure shall normalize to between 128/86 mmHg the heart rate
will decrease to 78 beats per minute and respiratory rate to 18 breaths per minute. The
extremities will be warm and pink in colour, and capillary refill time will reduce to 2 seconds.
The patient will also demonstrate an improvement in a mental state to being alert or a GCS of 15.
The interventions implemented can be evaluated by taking patients vital signs every 15
minutes to elicit any change. If there is an improvement, then the intervention should be
continued, but if not, a review should be done and an appropriate intervention initiated as soon as
possible.
Conclusion
Normal body fluid balance is important as an alteration in fluid volume alters the
electrolyte levels, which can lead to complications if immediate interventions are not
implemented. Decreased fluid volume causes a decrease in blood pressure, an increase in heart
blood pressure (Perner 2018). Fluids commonly used include normal saline and ringers lactate.
The amount of fluids to be administered depends on the level of blood pressure and general
wellbeing of an individual. Administration of fluids increases the amount of body fluids which
promotes tissue perfusion and raises blood pressure to normal level (Montomoli, Donati &Ince,
2019). The nurse should calculate the number of drops to be delivered to the patient depending
on the time the fluid should run. The nurse should also monitor for any signs of fluid overload,
especially when the patient is not alert. Increase in the amount of body fluid increases cardiac
output and consequentially increase in the amount of oxygen delivered to the tissues. This will,
therefore, lead to a decrease in heart rate and respiratory rate to normal as a signal is sent to the
respiratory centre and heart rate regulatory centre (McClain & McManus, 2019).
The nurse can also administer oxygen to the patient. Oxygen supply helps in increasing
the amount of oxygen reaching the tissues, especially when blood levels are low. This promotes
tissue oxygenation and prevents tissue damage. This can also help in correcting acidosis (Parotto
et al. 2018).
The patient should also be encouraged to take fluids orally as soon as she tolerates. This
will help increase fluid volume further (Nohara et al. 2019).
The nursing goal is that the patient shall demonstrate a normotensive state within a period
of 2 hours. The patients’ blood pressure shall normalize to between 128/86 mmHg the heart rate
will decrease to 78 beats per minute and respiratory rate to 18 breaths per minute. The
extremities will be warm and pink in colour, and capillary refill time will reduce to 2 seconds.
The patient will also demonstrate an improvement in a mental state to being alert or a GCS of 15.
The interventions implemented can be evaluated by taking patients vital signs every 15
minutes to elicit any change. If there is an improvement, then the intervention should be
continued, but if not, a review should be done and an appropriate intervention initiated as soon as
possible.
Conclusion
Normal body fluid balance is important as an alteration in fluid volume alters the
electrolyte levels, which can lead to complications if immediate interventions are not
implemented. Decreased fluid volume causes a decrease in blood pressure, an increase in heart
rate, increase in respiratory rate and decrease in oxygen saturation. This can be intervened by
fluid and oxygen administration. Infection is another condition that can alter normal body
functioning. It is caused by micro-organisms but most commonly bacteria. Administration of
antibiotics and practising aseptic techniques helps in the management of infections or sepsis.
fluid and oxygen administration. Infection is another condition that can alter normal body
functioning. It is caused by micro-organisms but most commonly bacteria. Administration of
antibiotics and practising aseptic techniques helps in the management of infections or sepsis.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
References
Ahmed, S.M.U., Luo, L., Namani, A., Wang, X.J. Tang, X., (2017). Nrf2 signalling pathway:
Pivotal roles in inflammation. Biochimica et Biophysica Acta (BBA)-Molecular Basis of
Disease, 1863(2), 585-597.
Ait-Oufella, H. & Bakker, J. (2016). Understanding the clinical signs of poor tissue perfusion
during septic shock. Intensive care medicine, 42(12), 2070-2072.
Chiumello, D., Gotti, M. & Vergani, G. (2017). Paracetamol in fever in critically ill patients—an
update. Journal of critical care, 38, 245-252.
Eldin, C., Melenotte, C., Mediannikov, O., Ghigo, E., Million, M., Edouard, S., Mege, J.L.,
Maurin, M. &Raoult, D., (2017). From Q fever to Coxiella burnetii infection: a paradigm
change. Clinical microbiology reviews, 30(1), 115-190.
Erickson, T. (2018). Veterans and Pain: Taking Control with SMART Goals.
Gaal, A., Bailey, B., Patel, Y., Smiley, N., Dodson, T., Kim, D. & Dillon, J., (2016). Limiting
antibiotics when managing mandible fractures may not increase infection risk—Journal
of Oral and Maxillofacial Surgery, 74(10), 2008-2018.
Gast, R.K. &Porter Jr, RE, (2020). Salmonella infections. Diseases of poultry, pp.717-753.
Kikuchi, K., Iida, M., Ikeda, N., Moriyama, S., Hamada, M., Takahashi, S., Kitamura, H.,
Watanabe, T., Hasegawa, Y., Hase, K. & Fukuhara, T., (2018). Macrophages switch their
phenotype by regulating Maf expression during different phases of inflammation. The
Journal of Immunology, 201(2), 635-651.
Kumar, P. (2018). Fluid Resuscitation. In ICU Manual (pp. 722-728). jaypee.
Liu, T., Zhang, L., Joo, D. and Sun, SC, (2017). NF-κB signalling in inflammation. Signal
transduction and targeted therapy, 2(1), 1-9.
Macfarlane, T.V., Pigazzani, F., Flynn, R.W. &MacDonald, TM, (2019). The effect of
indapamide vs. Bendroflumethiazide for primary hypertension: a systematic review.
British Journal of Clinical Pharmacology, 85(2), 285-303.
Martínez-Cengotitabengoa, M., MacDowell, K.S., Alberich, S., Diaz, F.J., García-Bueno, B.,
Rodriguez-Jimenez, R., Bioque, M., Berrocoso, E., Parellada, M., Lobo, A. & Saiz, P.A.,
(2016). BDNF and NGF signalling in early phases of psychosis: relationship with
inflammation and response to antipsychotics after 1 year. Schizophrenia bulletin,
42(1),142-151.
Ahmed, S.M.U., Luo, L., Namani, A., Wang, X.J. Tang, X., (2017). Nrf2 signalling pathway:
Pivotal roles in inflammation. Biochimica et Biophysica Acta (BBA)-Molecular Basis of
Disease, 1863(2), 585-597.
Ait-Oufella, H. & Bakker, J. (2016). Understanding the clinical signs of poor tissue perfusion
during septic shock. Intensive care medicine, 42(12), 2070-2072.
Chiumello, D., Gotti, M. & Vergani, G. (2017). Paracetamol in fever in critically ill patients—an
update. Journal of critical care, 38, 245-252.
Eldin, C., Melenotte, C., Mediannikov, O., Ghigo, E., Million, M., Edouard, S., Mege, J.L.,
Maurin, M. &Raoult, D., (2017). From Q fever to Coxiella burnetii infection: a paradigm
change. Clinical microbiology reviews, 30(1), 115-190.
Erickson, T. (2018). Veterans and Pain: Taking Control with SMART Goals.
Gaal, A., Bailey, B., Patel, Y., Smiley, N., Dodson, T., Kim, D. & Dillon, J., (2016). Limiting
antibiotics when managing mandible fractures may not increase infection risk—Journal
of Oral and Maxillofacial Surgery, 74(10), 2008-2018.
Gast, R.K. &Porter Jr, RE, (2020). Salmonella infections. Diseases of poultry, pp.717-753.
Kikuchi, K., Iida, M., Ikeda, N., Moriyama, S., Hamada, M., Takahashi, S., Kitamura, H.,
Watanabe, T., Hasegawa, Y., Hase, K. & Fukuhara, T., (2018). Macrophages switch their
phenotype by regulating Maf expression during different phases of inflammation. The
Journal of Immunology, 201(2), 635-651.
Kumar, P. (2018). Fluid Resuscitation. In ICU Manual (pp. 722-728). jaypee.
Liu, T., Zhang, L., Joo, D. and Sun, SC, (2017). NF-κB signalling in inflammation. Signal
transduction and targeted therapy, 2(1), 1-9.
Macfarlane, T.V., Pigazzani, F., Flynn, R.W. &MacDonald, TM, (2019). The effect of
indapamide vs. Bendroflumethiazide for primary hypertension: a systematic review.
British Journal of Clinical Pharmacology, 85(2), 285-303.
Martínez-Cengotitabengoa, M., MacDowell, K.S., Alberich, S., Diaz, F.J., García-Bueno, B.,
Rodriguez-Jimenez, R., Bioque, M., Berrocoso, E., Parellada, M., Lobo, A. & Saiz, P.A.,
(2016). BDNF and NGF signalling in early phases of psychosis: relationship with
inflammation and response to antipsychotics after 1 year. Schizophrenia bulletin,
42(1),142-151.
McClain, C.D. & McManus, M.L. (2019). Fluid management. In A practice of anesthesia for
infants and children (199-216). Content Repository Only!.
Montomoli, J., Donati, A. & Ince, C. (2019). Should Albumin be the Colloid of Choice for Fluid
Resuscitation in Hypovolemic Patients?. In the Annual Update in Intensive Care and
Emergency Medicine 2019 (277-292). Springer, Cham.
Moon, M.S. (2019). Essential Basic Bacteriology in Managing Musculoarticuloskeletal
Infection: Bacterial Anatomy, Their Behavior, Host Phagocytic Activity, Immune
System, Nutrition, And Antibiotics. Asian spine journal, 13(2),343.
Nohara, T., Kato, Y., Nakano, T., Nakagawa, T., Iwamoto, H., Yaegashi, H., Nakashima, K.,
Iijima, M., Kawaguchi, S., Shigehara, K. &Izumi, K., (2019). Intraoperative hypotension
caused by oral administration of 5‐aminolevulinic acid for photodynamic diagnosis in
patients with bladder cancer. International Journal of Urology, 26(11), 1064-1068.
Parotto, M., Ouzounian, M., Fedorko, L., Oreopoulos, G., Lindsay, T. &Katznelson, R., (2018).
Hyperbaric oxygen therapy for spinal cord ischaemia after complex aortic repair—a
retrospective review. Anaesthesiology intensive therapy, 50(2), 103-109.
Perner, A., Cecconi, M., Cronhjort, M., Darmon, M., Jakob, S.M., Pettilä, V. &van der Horst,
I.C., (2018). Expert statement for the management of hypovolemia in sepsis. Intensive
care medicine, 44(6), 791-798.
Saleh, A., McGarry, K., Chaw, CS &Elkordy, AA, (2018). Feasibility of using gluconolactone,
trehalose and hydroxy-propyl gamma-cyclodextrin to enhance bendroflumethiazide
dissolution using lyophilization and physical mixing techniques. Pharmaceutics, 10(1),
22.
Team, AFE (2019). Aseptic Technique (ANTT®) Tutorial. Acute Care.
Tigabu, B.M., Davari, M., Kebriaeezadeh, A. &Mojtahedzadeh, M. (2018). Fluid volume, fluid
balance and patient outcome in severe sepsis and septic shock: a systematic review.
Journal of critical care, 48, 153-159.
infants and children (199-216). Content Repository Only!.
Montomoli, J., Donati, A. & Ince, C. (2019). Should Albumin be the Colloid of Choice for Fluid
Resuscitation in Hypovolemic Patients?. In the Annual Update in Intensive Care and
Emergency Medicine 2019 (277-292). Springer, Cham.
Moon, M.S. (2019). Essential Basic Bacteriology in Managing Musculoarticuloskeletal
Infection: Bacterial Anatomy, Their Behavior, Host Phagocytic Activity, Immune
System, Nutrition, And Antibiotics. Asian spine journal, 13(2),343.
Nohara, T., Kato, Y., Nakano, T., Nakagawa, T., Iwamoto, H., Yaegashi, H., Nakashima, K.,
Iijima, M., Kawaguchi, S., Shigehara, K. &Izumi, K., (2019). Intraoperative hypotension
caused by oral administration of 5‐aminolevulinic acid for photodynamic diagnosis in
patients with bladder cancer. International Journal of Urology, 26(11), 1064-1068.
Parotto, M., Ouzounian, M., Fedorko, L., Oreopoulos, G., Lindsay, T. &Katznelson, R., (2018).
Hyperbaric oxygen therapy for spinal cord ischaemia after complex aortic repair—a
retrospective review. Anaesthesiology intensive therapy, 50(2), 103-109.
Perner, A., Cecconi, M., Cronhjort, M., Darmon, M., Jakob, S.M., Pettilä, V. &van der Horst,
I.C., (2018). Expert statement for the management of hypovolemia in sepsis. Intensive
care medicine, 44(6), 791-798.
Saleh, A., McGarry, K., Chaw, CS &Elkordy, AA, (2018). Feasibility of using gluconolactone,
trehalose and hydroxy-propyl gamma-cyclodextrin to enhance bendroflumethiazide
dissolution using lyophilization and physical mixing techniques. Pharmaceutics, 10(1),
22.
Team, AFE (2019). Aseptic Technique (ANTT®) Tutorial. Acute Care.
Tigabu, B.M., Davari, M., Kebriaeezadeh, A. &Mojtahedzadeh, M. (2018). Fluid volume, fluid
balance and patient outcome in severe sepsis and septic shock: a systematic review.
Journal of critical care, 48, 153-159.
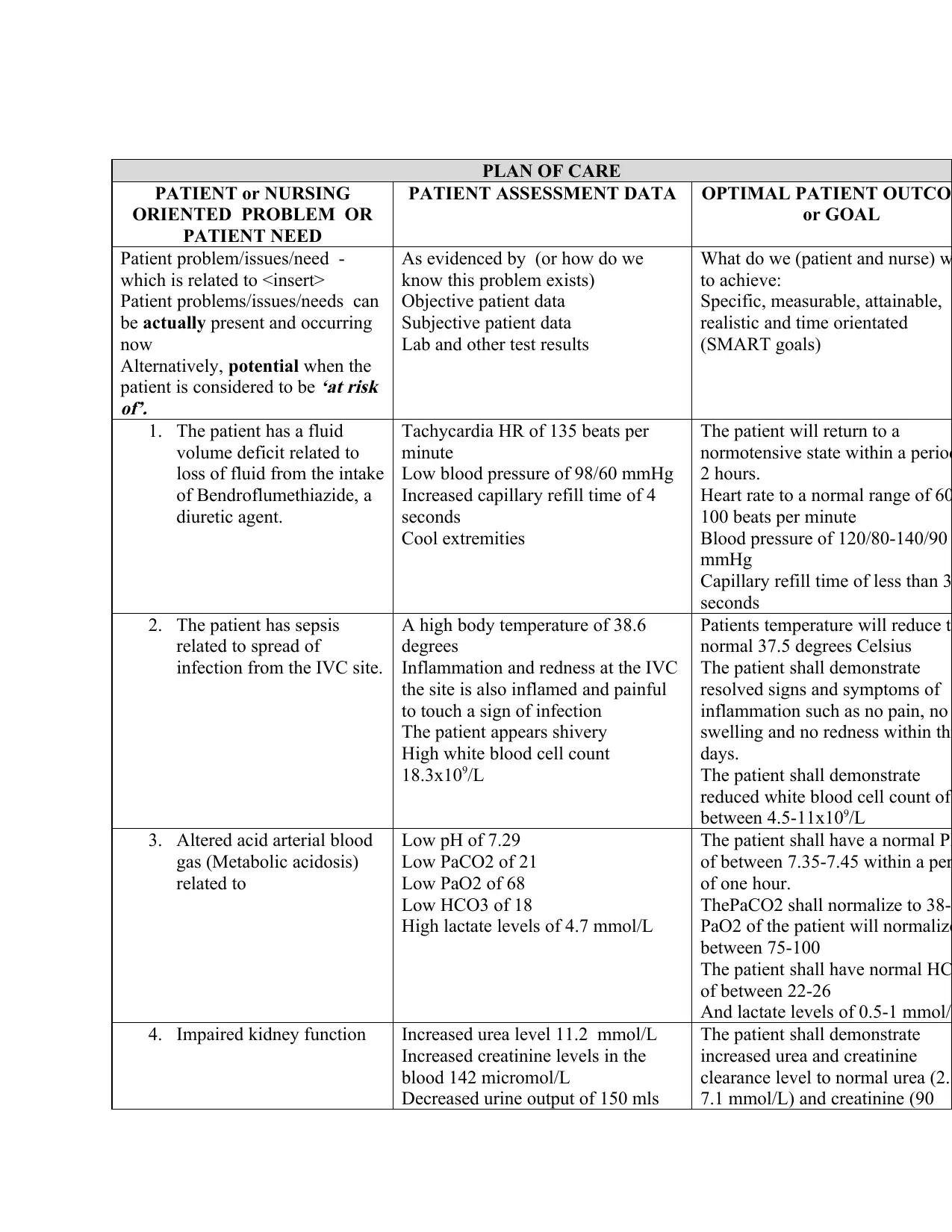
PLAN OF CARE
PATIENT or NURSING
ORIENTED PROBLEM OR
PATIENT NEED
PATIENT ASSESSMENT DATA OPTIMAL PATIENT OUTCOM
or GOAL
Patient problem/issues/need -
which is related to <insert>
Patient problems/issues/needs can
be actually present and occurring
now
Alternatively, potential when the
patient is considered to be
‘at risk
of’.
As evidenced by (or how do we
know this problem exists)
Objective patient data
Subjective patient data
Lab and other test results
What do we (patient and nurse) w
to achieve:
Specific, measurable, attainable,
realistic and time orientated
(SMART goals)
1. The patient has a fluid
volume deficit related to
loss of fluid from the intake
of Bendroflumethiazide, a
diuretic agent.
Tachycardia HR of 135 beats per
minute
Low blood pressure of 98/60 mmHg
Increased capillary refill time of 4
seconds
Cool extremities
The patient will return to a
normotensive state within a period
2 hours.
Heart rate to a normal range of 60
100 beats per minute
Blood pressure of 120/80-140/90
mmHg
Capillary refill time of less than 3
seconds
2. The patient has sepsis
related to spread of
infection from the IVC site.
A high body temperature of 38.6
degrees
Inflammation and redness at the IVC
the site is also inflamed and painful
to touch a sign of infection
The patient appears shivery
High white blood cell count
18.3x109/L
Patients temperature will reduce to
normal 37.5 degrees Celsius
The patient shall demonstrate
resolved signs and symptoms of
inflammation such as no pain, no
swelling and no redness within thr
days.
The patient shall demonstrate
reduced white blood cell count of
between 4.5-11x109/L
3. Altered acid arterial blood
gas (Metabolic acidosis)
related to
Low pH of 7.29
Low PaCO2 of 21
Low PaO2 of 68
Low HCO3 of 18
High lactate levels of 4.7 mmol/L
The patient shall have a normal PH
of between 7.35-7.45 within a per
of one hour.
ThePaCO2 shall normalize to 38-4
PaO2 of the patient will normalize
between 75-100
The patient shall have normal HC
of between 22-26
And lactate levels of 0.5-1 mmol/L
4. Impaired kidney function Increased urea level 11.2 mmol/L
Increased creatinine levels in the
blood 142 micromol/L
Decreased urine output of 150 mls
The patient shall demonstrate
increased urea and creatinine
clearance level to normal urea (2.5
7.1 mmol/L) and creatinine (90
PATIENT or NURSING
ORIENTED PROBLEM OR
PATIENT NEED
PATIENT ASSESSMENT DATA OPTIMAL PATIENT OUTCOM
or GOAL
Patient problem/issues/need -
which is related to <insert>
Patient problems/issues/needs can
be actually present and occurring
now
Alternatively, potential when the
patient is considered to be
‘at risk
of’.
As evidenced by (or how do we
know this problem exists)
Objective patient data
Subjective patient data
Lab and other test results
What do we (patient and nurse) w
to achieve:
Specific, measurable, attainable,
realistic and time orientated
(SMART goals)
1. The patient has a fluid
volume deficit related to
loss of fluid from the intake
of Bendroflumethiazide, a
diuretic agent.
Tachycardia HR of 135 beats per
minute
Low blood pressure of 98/60 mmHg
Increased capillary refill time of 4
seconds
Cool extremities
The patient will return to a
normotensive state within a period
2 hours.
Heart rate to a normal range of 60
100 beats per minute
Blood pressure of 120/80-140/90
mmHg
Capillary refill time of less than 3
seconds
2. The patient has sepsis
related to spread of
infection from the IVC site.
A high body temperature of 38.6
degrees
Inflammation and redness at the IVC
the site is also inflamed and painful
to touch a sign of infection
The patient appears shivery
High white blood cell count
18.3x109/L
Patients temperature will reduce to
normal 37.5 degrees Celsius
The patient shall demonstrate
resolved signs and symptoms of
inflammation such as no pain, no
swelling and no redness within thr
days.
The patient shall demonstrate
reduced white blood cell count of
between 4.5-11x109/L
3. Altered acid arterial blood
gas (Metabolic acidosis)
related to
Low pH of 7.29
Low PaCO2 of 21
Low PaO2 of 68
Low HCO3 of 18
High lactate levels of 4.7 mmol/L
The patient shall have a normal PH
of between 7.35-7.45 within a per
of one hour.
ThePaCO2 shall normalize to 38-4
PaO2 of the patient will normalize
between 75-100
The patient shall have normal HC
of between 22-26
And lactate levels of 0.5-1 mmol/L
4. Impaired kidney function Increased urea level 11.2 mmol/L
Increased creatinine levels in the
blood 142 micromol/L
Decreased urine output of 150 mls
The patient shall demonstrate
increased urea and creatinine
clearance level to normal urea (2.5
7.1 mmol/L) and creatinine (90
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
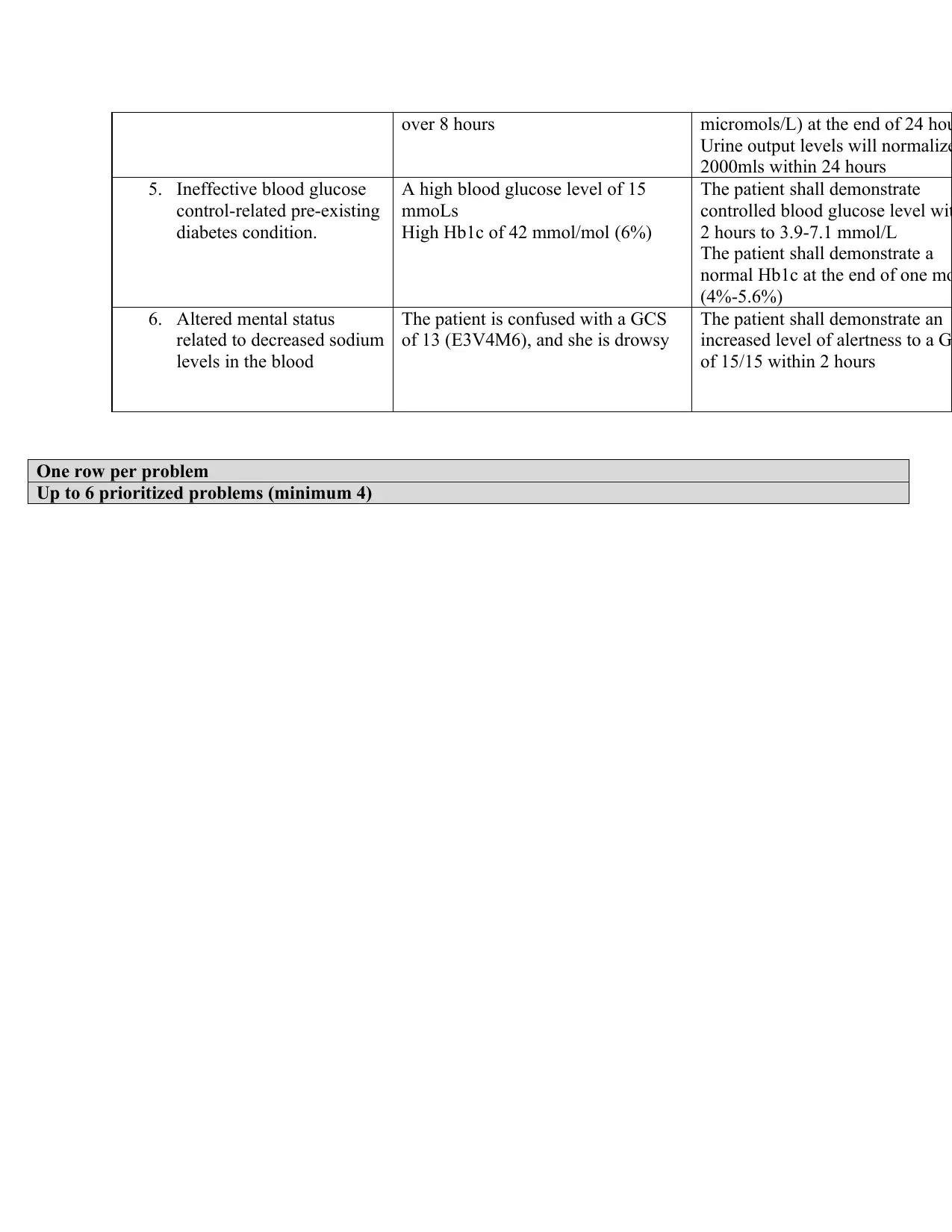
over 8 hours micromols/L) at the end of 24 hou
Urine output levels will normalize
2000mls within 24 hours
5. Ineffective blood glucose
control-related pre-existing
diabetes condition.
A high blood glucose level of 15
mmoLs
High Hb1c of 42 mmol/mol (6%)
The patient shall demonstrate
controlled blood glucose level wit
2 hours to 3.9-7.1 mmol/L
The patient shall demonstrate a
normal Hb1c at the end of one mo
(4%-5.6%)
6. Altered mental status
related to decreased sodium
levels in the blood
The patient is confused with a GCS
of 13 (E3V4M6), and she is drowsy
The patient shall demonstrate an
increased level of alertness to a G
of 15/15 within 2 hours
One row per problem
Up to 6 prioritized problems (minimum 4)
Urine output levels will normalize
2000mls within 24 hours
5. Ineffective blood glucose
control-related pre-existing
diabetes condition.
A high blood glucose level of 15
mmoLs
High Hb1c of 42 mmol/mol (6%)
The patient shall demonstrate
controlled blood glucose level wit
2 hours to 3.9-7.1 mmol/L
The patient shall demonstrate a
normal Hb1c at the end of one mo
(4%-5.6%)
6. Altered mental status
related to decreased sodium
levels in the blood
The patient is confused with a GCS
of 13 (E3V4M6), and she is drowsy
The patient shall demonstrate an
increased level of alertness to a G
of 15/15 within 2 hours
One row per problem
Up to 6 prioritized problems (minimum 4)
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





