Evidence-Based Practice for Alcohol Withdrawal: Assessment 3 Essay
VerifiedAdded on 2023/06/03
|7
|3014
|144
Essay
AI Summary
This essay critically evaluates three best practice evidence-based studies related to alcohol withdrawal syndrome, focusing on interventions and nursing implications. The essay begins with an introduction to alcoholism and its associated risks, including alcohol withdrawal syndrome and the challenges in addiction cessation treatment. The author, a registered nurse, aims to identify effective interventions for managing the complexities of alcohol withdrawal. The essay then presents an annotated bibliography of three studies: one on phenobarbital, one on dexmedetomidine, and another on nursing education protocols. The essay justifies the evidence by discussing the strengths and limitations of each study, including study design, sample size, and potential biases. It emphasizes the relevance of the findings to nursing practice, highlighting the importance of clinical expertise and patient values in implementing evidence-based interventions. The essay also discusses barriers to practice, such as the need for needs assessments and the importance of considering practical challenges faced by nurses. The conclusion emphasizes the importance of applying evidence-based practice to improve patient outcomes in the context of alcohol withdrawal.
Assessment 3
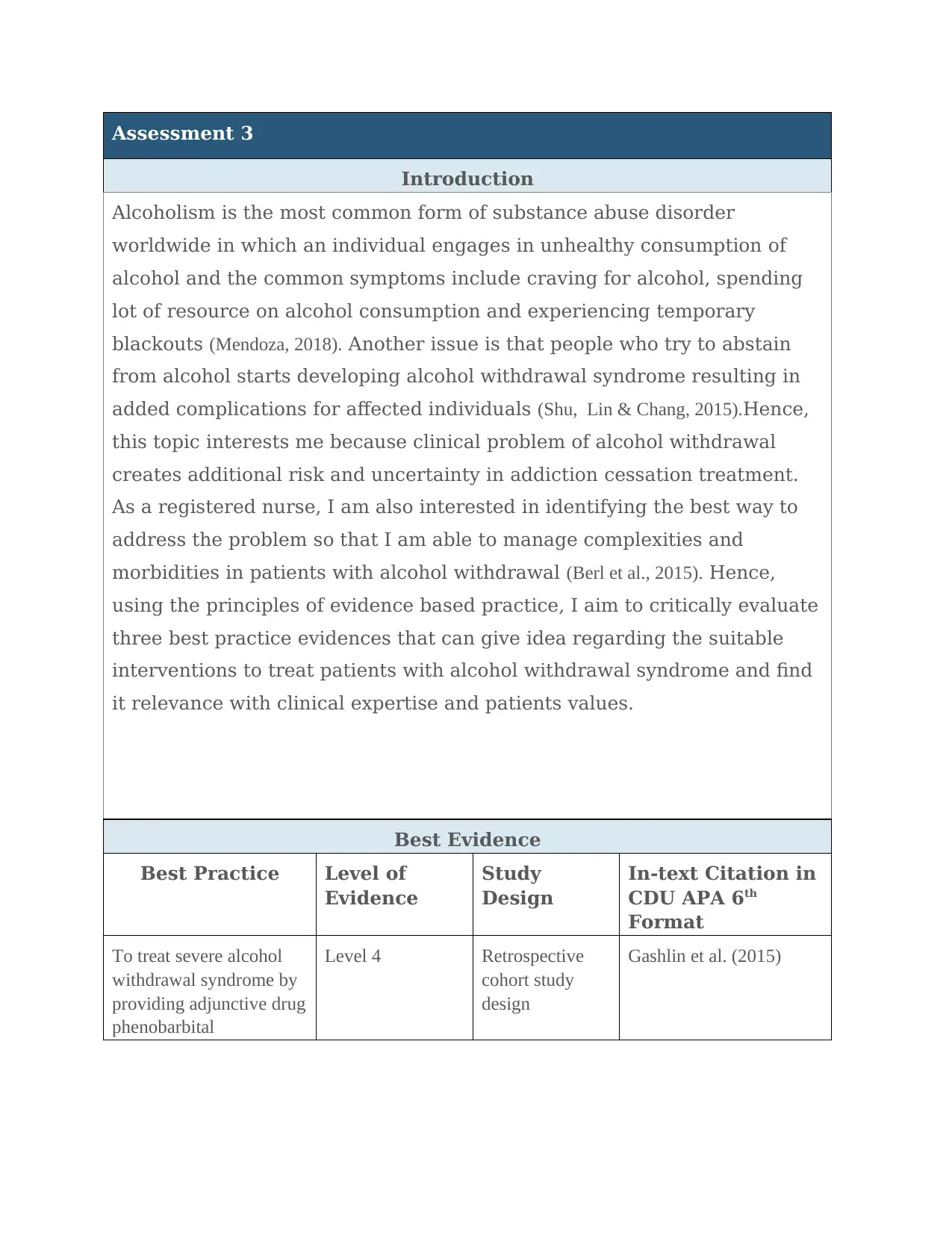
Introduction
Alcoholism is the most common form of substance abuse disorder
worldwide in which an individual engages in unhealthy consumption of
alcohol and the common symptoms include craving for alcohol, spending
lot of resource on alcohol consumption and experiencing temporary
blackouts (Mendoza, 2018). Another issue is that people who try to abstain
from alcohol starts developing alcohol withdrawal syndrome resulting in
added complications for affected individuals (Shu, Lin & Chang, 2015).Hence,
this topic interests me because clinical problem of alcohol withdrawal
creates additional risk and uncertainty in addiction cessation treatment.
As a registered nurse, I am also interested in identifying the best way to
address the problem so that I am able to manage complexities and
morbidities in patients with alcohol withdrawal (Berl et al., 2015). Hence,
using the principles of evidence based practice, I aim to critically evaluate
three best practice evidences that can give idea regarding the suitable
interventions to treat patients with alcohol withdrawal syndrome and find
it relevance with clinical expertise and patients values.
Best Evidence
Best Practice Level of
Evidence
Study
Design
In-text Citation in
CDU APA 6th
Format
To treat severe alcohol
withdrawal syndrome by
providing adjunctive drug
phenobarbital
Level 4 Retrospective
cohort study
design
Gashlin et al. (2015)
Introduction
Alcoholism is the most common form of substance abuse disorder
worldwide in which an individual engages in unhealthy consumption of
alcohol and the common symptoms include craving for alcohol, spending
lot of resource on alcohol consumption and experiencing temporary
blackouts (Mendoza, 2018). Another issue is that people who try to abstain
from alcohol starts developing alcohol withdrawal syndrome resulting in
added complications for affected individuals (Shu, Lin & Chang, 2015).Hence,
this topic interests me because clinical problem of alcohol withdrawal
creates additional risk and uncertainty in addiction cessation treatment.
As a registered nurse, I am also interested in identifying the best way to
address the problem so that I am able to manage complexities and
morbidities in patients with alcohol withdrawal (Berl et al., 2015). Hence,
using the principles of evidence based practice, I aim to critically evaluate
three best practice evidences that can give idea regarding the suitable
interventions to treat patients with alcohol withdrawal syndrome and find
it relevance with clinical expertise and patients values.
Best Evidence
Best Practice Level of
Evidence
Study
Design
In-text Citation in
CDU APA 6th
Format
To treat severe alcohol
withdrawal syndrome by
providing adjunctive drug
phenobarbital
Level 4 Retrospective
cohort study
design
Gashlin et al. (2015)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Use of dexmedetomidine
to treat alcohol
withdrawal
Level 4 Retrospective
study design
Frazee et al. (2014)
To provide nursing
education on community
hospital’s alcohol
withdrawal protocol.
Level 4 Retrospective
study design
Barrett et al. (2016)
Annotated Bibliography
Gashlin, L. Z., Groth, C. M., Wiegand, T. J., & Ashley, E. D. (2015). Comparison of
alcohol withdrawal outcomes in patients treated with benzodiazepines alone versus
adjunctive phenobarbital: a retrospective cohort study. Asia Pacific Journal of Medical
Toxicology, 4(1), 31-36. Retrieved from:
http://eprints.mums.ac.ir/7875/1/APJMT_Volume%204_Issue%201_Pages%2031-36.pdf
Level 4 (Retrospective cohort study)
Gashlin et al. (2015) revealed that the problem associated with high dose benzodiazepines
(BZDs) because of over-sedation effect on patient. In response to this problem, the author
suggested Phenobarbital (PBT) as an alternative option for the management of alcohol
withdrawal. The main purpose of research was to evaluate the effectiveness of PBT as an
adjunctive therapy for alcohol withdrawal treatment. The retrospective cohort study included
those patients who were treated either with BZD alone or BZDs with adjunctive PBT. In the
two groups, the CIWA score (Tool for alcohol withdrawal) was recorded 24 hours after first
dose and safety end points such as need for intubation, seizures, hemodynamic stability and
mortality was recorded in both groups of patients. The statistical analysis of research data gave
the indication that median duration of withdrawal symptoms of only 44 hours in the PBT-
adjunct group compared to 53 hours only in the BZD group. The conclusion from the results
was that PBT can be a safe alternative to BZDs for treatment of alcohol withdrawal patients.
Barrett, J., Jansen, M., Cooper, A., Felbinger, M., & Waters, F. (2016). Embracing a
nurse-driven alcohol withdrawal protocol through quality improvement. Journal of
addictions nursing, 27(4), 234-240. DOI: 10.1097/JAN.0000000000000142
Level 4(Retrospective cohort study)
The study by Barrett et al. (2016) gave an insight the importance of symptom triggered
protocols in decreasing alcohol withdrawal rate and problem of nurse’s non-compliance to
such protocols. The main aim of the study was to evaluate whether implementing educational
program can improve nursing compliance with alcohol withdrawal protocol or not. The
retrospective study was done in two stages. The first stage comprised conducting initial needs
assessment followed by nursing education and the second stage involved retrospective review
after education. Visual algorithm was used to simplify the alcohol withdrawal protocol and
guide nurses regarding the alcohol withdrawal pathway. The primary outcome of interest was
to treat alcohol
withdrawal
Level 4 Retrospective
study design
Frazee et al. (2014)
To provide nursing
education on community
hospital’s alcohol
withdrawal protocol.
Level 4 Retrospective
study design
Barrett et al. (2016)
Annotated Bibliography
Gashlin, L. Z., Groth, C. M., Wiegand, T. J., & Ashley, E. D. (2015). Comparison of
alcohol withdrawal outcomes in patients treated with benzodiazepines alone versus
adjunctive phenobarbital: a retrospective cohort study. Asia Pacific Journal of Medical
Toxicology, 4(1), 31-36. Retrieved from:
http://eprints.mums.ac.ir/7875/1/APJMT_Volume%204_Issue%201_Pages%2031-36.pdf
Level 4 (Retrospective cohort study)
Gashlin et al. (2015) revealed that the problem associated with high dose benzodiazepines
(BZDs) because of over-sedation effect on patient. In response to this problem, the author
suggested Phenobarbital (PBT) as an alternative option for the management of alcohol
withdrawal. The main purpose of research was to evaluate the effectiveness of PBT as an
adjunctive therapy for alcohol withdrawal treatment. The retrospective cohort study included
those patients who were treated either with BZD alone or BZDs with adjunctive PBT. In the
two groups, the CIWA score (Tool for alcohol withdrawal) was recorded 24 hours after first
dose and safety end points such as need for intubation, seizures, hemodynamic stability and
mortality was recorded in both groups of patients. The statistical analysis of research data gave
the indication that median duration of withdrawal symptoms of only 44 hours in the PBT-
adjunct group compared to 53 hours only in the BZD group. The conclusion from the results
was that PBT can be a safe alternative to BZDs for treatment of alcohol withdrawal patients.
Barrett, J., Jansen, M., Cooper, A., Felbinger, M., & Waters, F. (2016). Embracing a
nurse-driven alcohol withdrawal protocol through quality improvement. Journal of
addictions nursing, 27(4), 234-240. DOI: 10.1097/JAN.0000000000000142
Level 4(Retrospective cohort study)
The study by Barrett et al. (2016) gave an insight the importance of symptom triggered
protocols in decreasing alcohol withdrawal rate and problem of nurse’s non-compliance to
such protocols. The main aim of the study was to evaluate whether implementing educational
program can improve nursing compliance with alcohol withdrawal protocol or not. The
retrospective study was done in two stages. The first stage comprised conducting initial needs
assessment followed by nursing education and the second stage involved retrospective review
after education. Visual algorithm was used to simplify the alcohol withdrawal protocol and
guide nurses regarding the alcohol withdrawal pathway. The primary outcome of interest was
nurse’s compliance rate and secondary outcome included hospital stay and CIWA score for
assessment of alcohol withdrawal. The statistical analysis of research data revealed increase in
compliance of 1-hour assessment after the educational intervention. However, major difference
was not found for 6-hour assessment. The author concluded that nursing education has the
potential to improve compliance with alcohol withdrawal protocol, but future study must
evaluate the impact of assessment frequency intervals on patient outcomes.
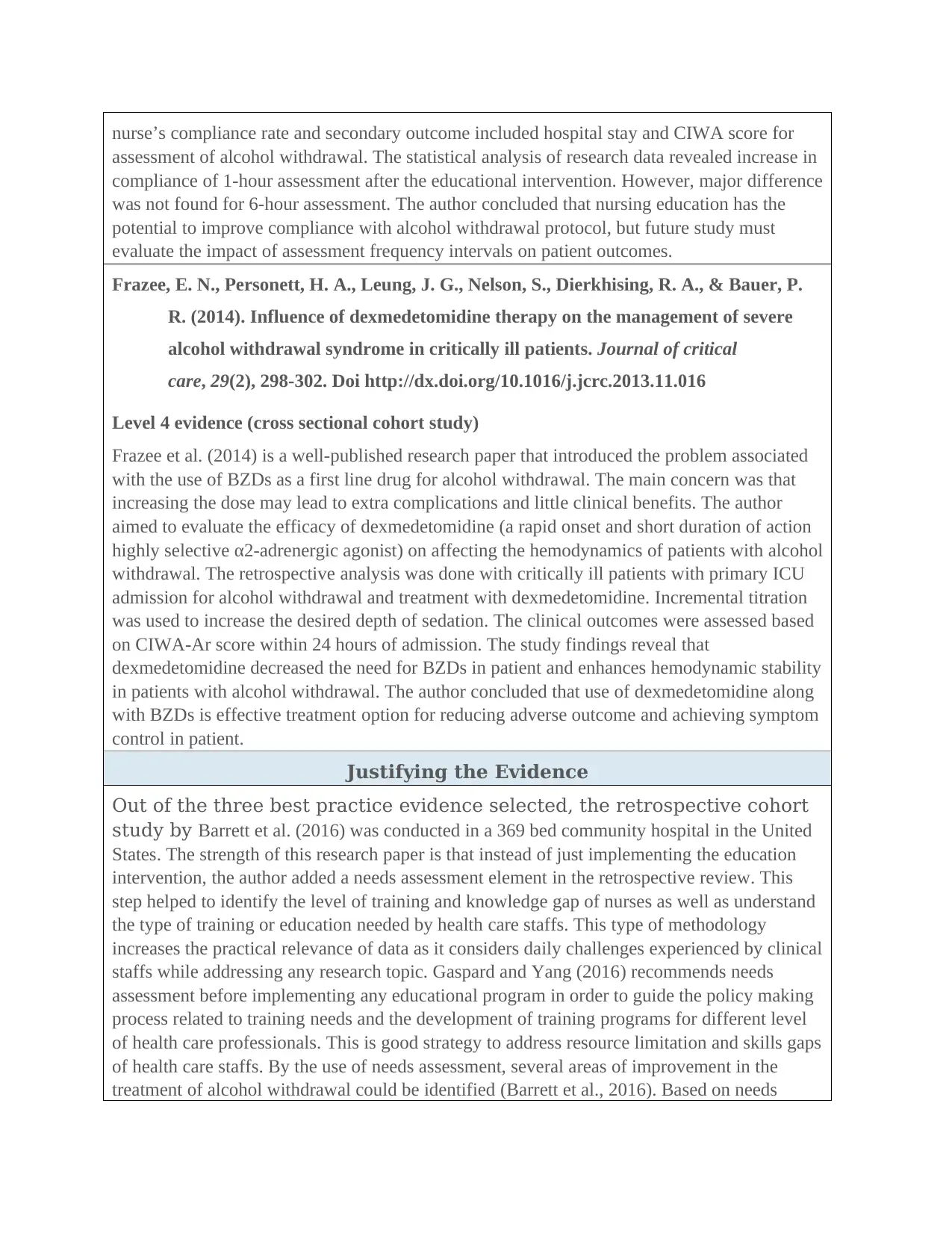
Frazee, E. N., Personett, H. A., Leung, J. G., Nelson, S., Dierkhising, R. A., & Bauer, P.
R. (2014). Influence of dexmedetomidine therapy on the management of severe
alcohol withdrawal syndrome in critically ill patients. Journal of critical
care, 29(2), 298-302. Doi http://dx.doi.org/10.1016/j.jcrc.2013.11.016
Level 4 evidence (cross sectional cohort study)
Frazee et al. (2014) is a well-published research paper that introduced the problem associated
with the use of BZDs as a first line drug for alcohol withdrawal. The main concern was that
increasing the dose may lead to extra complications and little clinical benefits. The author
aimed to evaluate the efficacy of dexmedetomidine (a rapid onset and short duration of action
highly selective α2-adrenergic agonist) on affecting the hemodynamics of patients with alcohol
withdrawal. The retrospective analysis was done with critically ill patients with primary ICU
admission for alcohol withdrawal and treatment with dexmedetomidine. Incremental titration
was used to increase the desired depth of sedation. The clinical outcomes were assessed based
on CIWA-Ar score within 24 hours of admission. The study findings reveal that
dexmedetomidine decreased the need for BZDs in patient and enhances hemodynamic stability
in patients with alcohol withdrawal. The author concluded that use of dexmedetomidine along
with BZDs is effective treatment option for reducing adverse outcome and achieving symptom
control in patient.
Justifying the Evidence
Out of the three best practice evidence selected, the retrospective cohort
study by Barrett et al. (2016) was conducted in a 369 bed community hospital in the United
States. The strength of this research paper is that instead of just implementing the education
intervention, the author added a needs assessment element in the retrospective review. This
step helped to identify the level of training and knowledge gap of nurses as well as understand
the type of training or education needed by health care staffs. This type of methodology
increases the practical relevance of data as it considers daily challenges experienced by clinical
staffs while addressing any research topic. Gaspard and Yang (2016) recommends needs
assessment before implementing any educational program in order to guide the policy making
process related to training needs and the development of training programs for different level
of health care professionals. This is good strategy to address resource limitation and skills gaps
of health care staffs. By the use of needs assessment, several areas of improvement in the
treatment of alcohol withdrawal could be identified (Barrett et al., 2016). Based on needs
assessment of alcohol withdrawal. The statistical analysis of research data revealed increase in
compliance of 1-hour assessment after the educational intervention. However, major difference
was not found for 6-hour assessment. The author concluded that nursing education has the
potential to improve compliance with alcohol withdrawal protocol, but future study must
evaluate the impact of assessment frequency intervals on patient outcomes.
Frazee, E. N., Personett, H. A., Leung, J. G., Nelson, S., Dierkhising, R. A., & Bauer, P.
R. (2014). Influence of dexmedetomidine therapy on the management of severe
alcohol withdrawal syndrome in critically ill patients. Journal of critical
care, 29(2), 298-302. Doi http://dx.doi.org/10.1016/j.jcrc.2013.11.016
Level 4 evidence (cross sectional cohort study)
Frazee et al. (2014) is a well-published research paper that introduced the problem associated
with the use of BZDs as a first line drug for alcohol withdrawal. The main concern was that
increasing the dose may lead to extra complications and little clinical benefits. The author
aimed to evaluate the efficacy of dexmedetomidine (a rapid onset and short duration of action
highly selective α2-adrenergic agonist) on affecting the hemodynamics of patients with alcohol
withdrawal. The retrospective analysis was done with critically ill patients with primary ICU
admission for alcohol withdrawal and treatment with dexmedetomidine. Incremental titration
was used to increase the desired depth of sedation. The clinical outcomes were assessed based
on CIWA-Ar score within 24 hours of admission. The study findings reveal that
dexmedetomidine decreased the need for BZDs in patient and enhances hemodynamic stability
in patients with alcohol withdrawal. The author concluded that use of dexmedetomidine along
with BZDs is effective treatment option for reducing adverse outcome and achieving symptom
control in patient.
Justifying the Evidence
Out of the three best practice evidence selected, the retrospective cohort
study by Barrett et al. (2016) was conducted in a 369 bed community hospital in the United
States. The strength of this research paper is that instead of just implementing the education
intervention, the author added a needs assessment element in the retrospective review. This
step helped to identify the level of training and knowledge gap of nurses as well as understand
the type of training or education needed by health care staffs. This type of methodology
increases the practical relevance of data as it considers daily challenges experienced by clinical
staffs while addressing any research topic. Gaspard and Yang (2016) recommends needs
assessment before implementing any educational program in order to guide the policy making
process related to training needs and the development of training programs for different level
of health care professionals. This is good strategy to address resource limitation and skills gaps
of health care staffs. By the use of needs assessment, several areas of improvement in the
treatment of alcohol withdrawal could be identified (Barrett et al., 2016). Based on needs
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
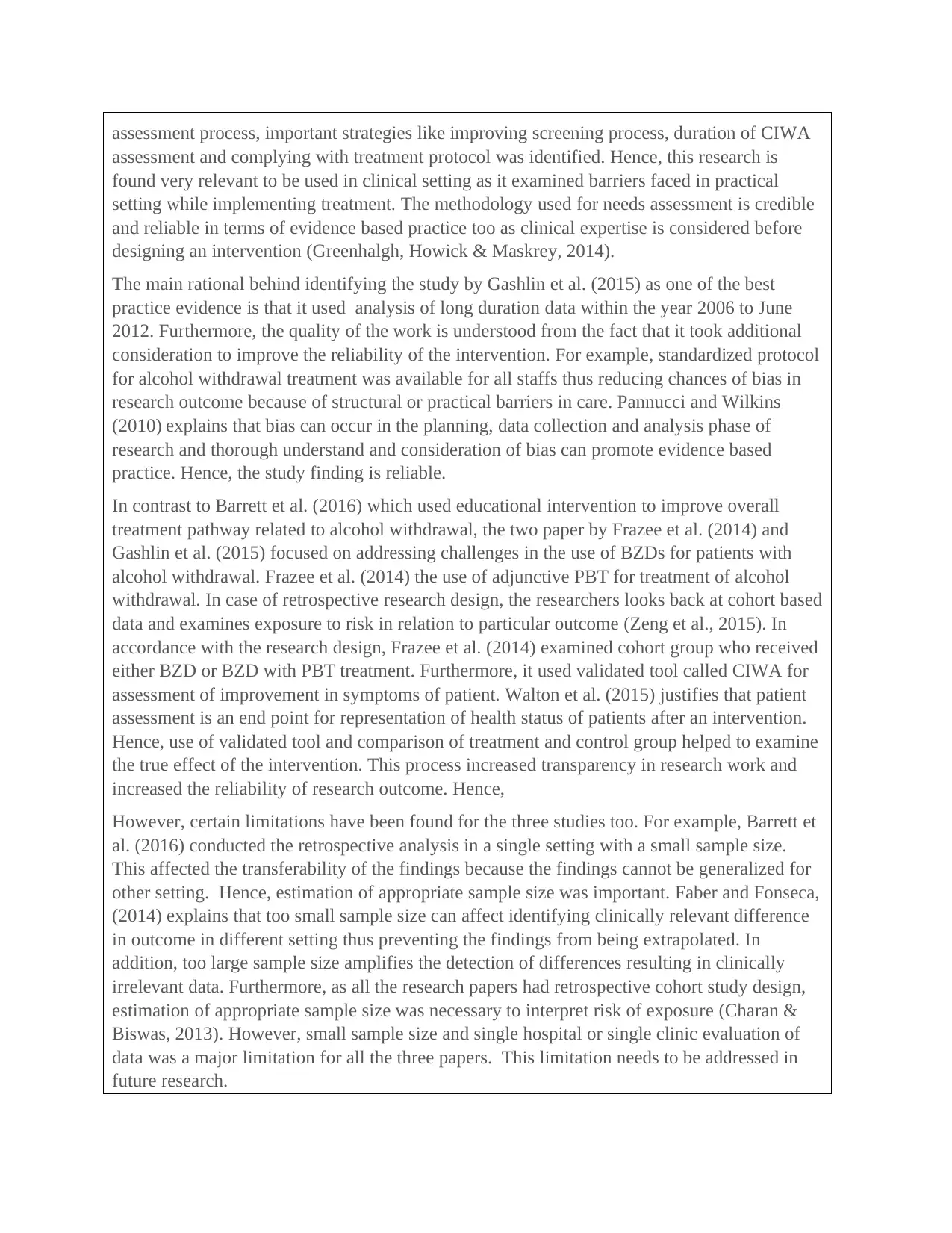
assessment process, important strategies like improving screening process, duration of CIWA
assessment and complying with treatment protocol was identified. Hence, this research is
found very relevant to be used in clinical setting as it examined barriers faced in practical
setting while implementing treatment. The methodology used for needs assessment is credible
and reliable in terms of evidence based practice too as clinical expertise is considered before
designing an intervention (Greenhalgh, Howick & Maskrey, 2014).
The main rational behind identifying the study by Gashlin et al. (2015) as one of the best
practice evidence is that it used analysis of long duration data within the year 2006 to June
2012. Furthermore, the quality of the work is understood from the fact that it took additional
consideration to improve the reliability of the intervention. For example, standardized protocol
for alcohol withdrawal treatment was available for all staffs thus reducing chances of bias in
research outcome because of structural or practical barriers in care. Pannucci and Wilkins
(2010) explains that bias can occur in the planning, data collection and analysis phase of
research and thorough understand and consideration of bias can promote evidence based
practice. Hence, the study finding is reliable.
In contrast to Barrett et al. (2016) which used educational intervention to improve overall
treatment pathway related to alcohol withdrawal, the two paper by Frazee et al. (2014) and
Gashlin et al. (2015) focused on addressing challenges in the use of BZDs for patients with
alcohol withdrawal. Frazee et al. (2014) the use of adjunctive PBT for treatment of alcohol
withdrawal. In case of retrospective research design, the researchers looks back at cohort based
data and examines exposure to risk in relation to particular outcome (Zeng et al., 2015). In
accordance with the research design, Frazee et al. (2014) examined cohort group who received
either BZD or BZD with PBT treatment. Furthermore, it used validated tool called CIWA for
assessment of improvement in symptoms of patient. Walton et al. (2015) justifies that patient
assessment is an end point for representation of health status of patients after an intervention.
Hence, use of validated tool and comparison of treatment and control group helped to examine
the true effect of the intervention. This process increased transparency in research work and
increased the reliability of research outcome. Hence,
However, certain limitations have been found for the three studies too. For example, Barrett et
al. (2016) conducted the retrospective analysis in a single setting with a small sample size.
This affected the transferability of the findings because the findings cannot be generalized for
other setting. Hence, estimation of appropriate sample size was important. Faber and Fonseca,
(2014) explains that too small sample size can affect identifying clinically relevant difference
in outcome in different setting thus preventing the findings from being extrapolated. In
addition, too large sample size amplifies the detection of differences resulting in clinically
irrelevant data. Furthermore, as all the research papers had retrospective cohort study design,
estimation of appropriate sample size was necessary to interpret risk of exposure (Charan &
Biswas, 2013). However, small sample size and single hospital or single clinic evaluation of
data was a major limitation for all the three papers. This limitation needs to be addressed in
future research.
assessment and complying with treatment protocol was identified. Hence, this research is
found very relevant to be used in clinical setting as it examined barriers faced in practical
setting while implementing treatment. The methodology used for needs assessment is credible
and reliable in terms of evidence based practice too as clinical expertise is considered before
designing an intervention (Greenhalgh, Howick & Maskrey, 2014).
The main rational behind identifying the study by Gashlin et al. (2015) as one of the best
practice evidence is that it used analysis of long duration data within the year 2006 to June
2012. Furthermore, the quality of the work is understood from the fact that it took additional
consideration to improve the reliability of the intervention. For example, standardized protocol
for alcohol withdrawal treatment was available for all staffs thus reducing chances of bias in
research outcome because of structural or practical barriers in care. Pannucci and Wilkins
(2010) explains that bias can occur in the planning, data collection and analysis phase of
research and thorough understand and consideration of bias can promote evidence based
practice. Hence, the study finding is reliable.
In contrast to Barrett et al. (2016) which used educational intervention to improve overall
treatment pathway related to alcohol withdrawal, the two paper by Frazee et al. (2014) and
Gashlin et al. (2015) focused on addressing challenges in the use of BZDs for patients with
alcohol withdrawal. Frazee et al. (2014) the use of adjunctive PBT for treatment of alcohol
withdrawal. In case of retrospective research design, the researchers looks back at cohort based
data and examines exposure to risk in relation to particular outcome (Zeng et al., 2015). In
accordance with the research design, Frazee et al. (2014) examined cohort group who received
either BZD or BZD with PBT treatment. Furthermore, it used validated tool called CIWA for
assessment of improvement in symptoms of patient. Walton et al. (2015) justifies that patient
assessment is an end point for representation of health status of patients after an intervention.
Hence, use of validated tool and comparison of treatment and control group helped to examine
the true effect of the intervention. This process increased transparency in research work and
increased the reliability of research outcome. Hence,
However, certain limitations have been found for the three studies too. For example, Barrett et
al. (2016) conducted the retrospective analysis in a single setting with a small sample size.
This affected the transferability of the findings because the findings cannot be generalized for
other setting. Hence, estimation of appropriate sample size was important. Faber and Fonseca,
(2014) explains that too small sample size can affect identifying clinically relevant difference
in outcome in different setting thus preventing the findings from being extrapolated. In
addition, too large sample size amplifies the detection of differences resulting in clinically
irrelevant data. Furthermore, as all the research papers had retrospective cohort study design,
estimation of appropriate sample size was necessary to interpret risk of exposure (Charan &
Biswas, 2013). However, small sample size and single hospital or single clinic evaluation of
data was a major limitation for all the three papers. This limitation needs to be addressed in
future research.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Relevance to Nursing and Barriers to Practice
To apply the evidence in nursing practice, it is necessary to critically evaluate the application
of research papers in terms of the principles of evidence based practice. According to evidence
based practice, it is necessary to critically evaluate the research evidence and its application in
clinical practice by consideration of patients value, clinical expertise and clinical context
(DiCenso, Guyatt & Ciliska, 2014).In this context, the research paper by Barret et al. (2016) is
considered the best evidence to be applied in nursing practice. This can be said because it
considered the clinical expertise of nurses before implementing the educational intervention. It
also took steps to simplify the protocol so that maximum adherence to protocol could be
achieved. By the inclusion of needs assessment step in the research methodology, the research
showed that practical concerns faced by nurses during alcohol withdrawal treatment was
addressed. For example, by the use of needs assessment, the researcher was able to identify
delays in CIWA assessment for patient and presence of variety of treatment plans for patient.
This finding gave the guidance to identify areas of improvement and find out the common
reason behind non-compliance with alcohol withdrawal treatment protocol among nurses.
Feeney et al. (2015) also gives the justification that certain restraining forces exist in health
care setting which restricts nurses from following the alcohol withdrawal protocol. Hence, as
Barrett et al. (2016) has considered clinical expertise before implementing the intervention, the
evidence can be applied in nursing practice. Nursing administrators can take similar steps to
embrace the intervention in real setting.
The study by Barrett et al. (2016) can also be applied in nursing practice because it has no risk
of challenging patient values. Instead, it encouraged regular monitoring and assessment of
patient from the time of admission. Hence, this would increase patient satisfaction with care
and increase patient-nurse engagement too.
References
Barrett, J., Jansen, M., Cooper, A., Felbinger, M., & Waters, F. (2016). Embracing a nurse-driven
alcohol withdrawal protocol through quality improvement. Journal of addictions
nursing, 27(4), 234-240. DOI: 10.1097/JAN.0000000000000142
Berl, K., Collins, M. L., Melson, J., Mooney, R., Muffley, C., & Wright-Glover, A. (2015). Improving
Nursing Knowledge of Alcohol Withdrawal: Second Generation Education Strategies. Journal
for Nurses in Professional Development, 31(6), 328–332.
http://doi.org/10.1097/NND.0000000000000176
Charan, J., & Biswas, T. (2013). How to Calculate Sample Size for Different Study Designs in Medical
Research? Indian Journal of Psychological Medicine, 35(2), 121–126.
http://doi.org/10.4103/0253-7176.116232
To apply the evidence in nursing practice, it is necessary to critically evaluate the application
of research papers in terms of the principles of evidence based practice. According to evidence
based practice, it is necessary to critically evaluate the research evidence and its application in
clinical practice by consideration of patients value, clinical expertise and clinical context
(DiCenso, Guyatt & Ciliska, 2014).In this context, the research paper by Barret et al. (2016) is
considered the best evidence to be applied in nursing practice. This can be said because it
considered the clinical expertise of nurses before implementing the educational intervention. It
also took steps to simplify the protocol so that maximum adherence to protocol could be
achieved. By the inclusion of needs assessment step in the research methodology, the research
showed that practical concerns faced by nurses during alcohol withdrawal treatment was
addressed. For example, by the use of needs assessment, the researcher was able to identify
delays in CIWA assessment for patient and presence of variety of treatment plans for patient.
This finding gave the guidance to identify areas of improvement and find out the common
reason behind non-compliance with alcohol withdrawal treatment protocol among nurses.
Feeney et al. (2015) also gives the justification that certain restraining forces exist in health
care setting which restricts nurses from following the alcohol withdrawal protocol. Hence, as
Barrett et al. (2016) has considered clinical expertise before implementing the intervention, the
evidence can be applied in nursing practice. Nursing administrators can take similar steps to
embrace the intervention in real setting.
The study by Barrett et al. (2016) can also be applied in nursing practice because it has no risk
of challenging patient values. Instead, it encouraged regular monitoring and assessment of
patient from the time of admission. Hence, this would increase patient satisfaction with care
and increase patient-nurse engagement too.
References
Barrett, J., Jansen, M., Cooper, A., Felbinger, M., & Waters, F. (2016). Embracing a nurse-driven
alcohol withdrawal protocol through quality improvement. Journal of addictions
nursing, 27(4), 234-240. DOI: 10.1097/JAN.0000000000000142
Berl, K., Collins, M. L., Melson, J., Mooney, R., Muffley, C., & Wright-Glover, A. (2015). Improving
Nursing Knowledge of Alcohol Withdrawal: Second Generation Education Strategies. Journal
for Nurses in Professional Development, 31(6), 328–332.
http://doi.org/10.1097/NND.0000000000000176
Charan, J., & Biswas, T. (2013). How to Calculate Sample Size for Different Study Designs in Medical
Research? Indian Journal of Psychological Medicine, 35(2), 121–126.
http://doi.org/10.4103/0253-7176.116232
DiCenso, A., Guyatt, G., & Ciliska, D. (2014). Evidence-Based Nursing-E-Book: A Guide to Clinical
Practice. Elsevier Health Sciences. Retrieved from: http://www.feliceapicella.it/nurs.pdf
Faber, J., & Fonseca, L. M. (2014). How sample size influences research outcomes. Dental Press
Journal of Orthodontics, 19(4), 27–29. http://doi.org/10.1590/2176-9451.19.4.027-029.ebo
Feeney, C., Alter, H. J., Jacobsen, E., Rehrer, M., Shao, S., Subramanian, I., & Clements, R. C. (2015).
A simplified protocol for the treatment of alcohol withdrawal. Journal of addiction
medicine, 9(6), 485-490. doi: 10.1097/ADM.0000000000000167
Frazee, E. N., Personett, H. A., Leung, J. G., Nelson, S., Dierkhising, R. A., & Bauer, P. R. (2014).
Influence of dexmedetomidine therapy on the management of severe alcohol withdrawal
syndrome in critically ill patients. Journal of critical care, 29(2), 298-302. Doi
http://dx.doi.org/10.1016/j.jcrc.2013.11.016
Gashlin, L. Z., Groth, C. M., Wiegand, T. J., & Ashley, E. D. (2015). Comparison of alcohol
withdrawal outcomes in patients treated with benzodiazepines alone versus adjunctive
phenobarbital: a retrospective cohort study. Asia Pacific Journal of Medical Toxicology, 4(1),
31-36. Retrieved from: http://eprints.mums.ac.ir/7875/1/APJMT_Volume%204_Issue
%201_Pages%2031-36.pdf
Gaspard, J., & Yang, C.-M. (2016). Training needs assessment of health care professionals in a
developing country: the example of Saint Lucia. BMC Medical Education, 16, 112.
http://doi.org/10.1186/s12909-016-0638-9
Greenhalgh, T., Howick, J., & Maskrey, N. (2014). Evidence based medicine: a movement in
crisis?. Bmj, 348, g3725.
Mendoza, R. L. (2018). Is medical treatment of Alcohol Withdrawal Syndrome a Stag Hunt?
Challenges and opportunities in managing risk and uncertainty in addiction cessation. Risk
Management and Healthcare Policy, 11, 1–14. http://doi.org/10.2147/RMHP.S144831
Pannucci, C. J., & Wilkins, E. G. (2010). Identifying and Avoiding Bias in Research. Plastic and
Reconstructive Surgery, 126(2), 619–625. http://doi.org/10.1097/PRS.0b013e3181de24bc
Shu, J. E., Lin, A., & Chang, G. (2015). Alcohol withdrawal treatment in the medically hospitalized
patient: a pilot study assessing predictors for medical or psychiatric
complications. Psychosomatics, 56(5), 547-555. https://doi.org/10.1016/j.psym.2014.12.002
Walton, M. K., Powers, J. H., Hobart, J., Patrick, D. L., Marquis, P., Vamvakas, S., … Burke, L.
Practice. Elsevier Health Sciences. Retrieved from: http://www.feliceapicella.it/nurs.pdf
Faber, J., & Fonseca, L. M. (2014). How sample size influences research outcomes. Dental Press
Journal of Orthodontics, 19(4), 27–29. http://doi.org/10.1590/2176-9451.19.4.027-029.ebo
Feeney, C., Alter, H. J., Jacobsen, E., Rehrer, M., Shao, S., Subramanian, I., & Clements, R. C. (2015).
A simplified protocol for the treatment of alcohol withdrawal. Journal of addiction
medicine, 9(6), 485-490. doi: 10.1097/ADM.0000000000000167
Frazee, E. N., Personett, H. A., Leung, J. G., Nelson, S., Dierkhising, R. A., & Bauer, P. R. (2014).
Influence of dexmedetomidine therapy on the management of severe alcohol withdrawal
syndrome in critically ill patients. Journal of critical care, 29(2), 298-302. Doi
http://dx.doi.org/10.1016/j.jcrc.2013.11.016
Gashlin, L. Z., Groth, C. M., Wiegand, T. J., & Ashley, E. D. (2015). Comparison of alcohol
withdrawal outcomes in patients treated with benzodiazepines alone versus adjunctive
phenobarbital: a retrospective cohort study. Asia Pacific Journal of Medical Toxicology, 4(1),
31-36. Retrieved from: http://eprints.mums.ac.ir/7875/1/APJMT_Volume%204_Issue
%201_Pages%2031-36.pdf
Gaspard, J., & Yang, C.-M. (2016). Training needs assessment of health care professionals in a
developing country: the example of Saint Lucia. BMC Medical Education, 16, 112.
http://doi.org/10.1186/s12909-016-0638-9
Greenhalgh, T., Howick, J., & Maskrey, N. (2014). Evidence based medicine: a movement in
crisis?. Bmj, 348, g3725.
Mendoza, R. L. (2018). Is medical treatment of Alcohol Withdrawal Syndrome a Stag Hunt?
Challenges and opportunities in managing risk and uncertainty in addiction cessation. Risk
Management and Healthcare Policy, 11, 1–14. http://doi.org/10.2147/RMHP.S144831
Pannucci, C. J., & Wilkins, E. G. (2010). Identifying and Avoiding Bias in Research. Plastic and
Reconstructive Surgery, 126(2), 619–625. http://doi.org/10.1097/PRS.0b013e3181de24bc
Shu, J. E., Lin, A., & Chang, G. (2015). Alcohol withdrawal treatment in the medically hospitalized
patient: a pilot study assessing predictors for medical or psychiatric
complications. Psychosomatics, 56(5), 547-555. https://doi.org/10.1016/j.psym.2014.12.002
Walton, M. K., Powers, J. H., Hobart, J., Patrick, D. L., Marquis, P., Vamvakas, S., … Burke, L.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
(2015). Clinical Outcome Assessments: Conceptual Foundation–Report of the ISPOR Clinical
Outcomes Assessment – Emerging Good Practices for Outcomes Research Task Force DOES
THIS HAVE TO BE LABLED AS PART 1. Value in Health : The Journal of the International
Society for Pharmacoeconomics and Outcomes Research, 18(6), 741–752.
http://doi.org/10.1016/j.jval.2015.08.006
Zeng, X., Zhang, Y., Kwong, J. S., Zhang, C., Li, S., Sun, F., ... & Du, L. (2015). The methodological
quality assessment tools for preclinical and clinical studies, systematic review and meta‐
analysis, and clinical practice guideline: a systematic review. Journal of evidence-based
medicine, 8(1), 2-10.
Outcomes Assessment – Emerging Good Practices for Outcomes Research Task Force DOES
THIS HAVE TO BE LABLED AS PART 1. Value in Health : The Journal of the International
Society for Pharmacoeconomics and Outcomes Research, 18(6), 741–752.
http://doi.org/10.1016/j.jval.2015.08.006
Zeng, X., Zhang, Y., Kwong, J. S., Zhang, C., Li, S., Sun, F., ... & Du, L. (2015). The methodological
quality assessment tools for preclinical and clinical studies, systematic review and meta‐
analysis, and clinical practice guideline: a systematic review. Journal of evidence-based
medicine, 8(1), 2-10.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





