Comprehensive Report: Bipolar Disorder, Care Pathways, and Treatments
VerifiedAdded on 2022/12/23
|9
|2529
|34
Report
AI Summary
This report provides a comprehensive overview of bipolar disorder, also known as manic depression. It begins with an introduction defining the disorder and its impact on mood, energy, and behavior. The main body delves into the examination of bipolar disorder, including the different types, symptoms, and associated risks. It highlights the importance of planning safe and effective care for individuals experiencing the disorder, discussing carer responsibilities, and emergency planning. The report explores the signs and symptoms, including mood episodes and psychotic symptoms, as well as the factors contributing to the risk of developing bipolar disorder. The report also outlines effective pathways of care, emphasizing the combination of medications and mental therapy, including biopsychosocial, recovery-oriented, and trauma-informed care approaches. The report concludes by summarizing the key findings and emphasizing the importance of early intervention and comprehensive care for individuals affected by bipolar disorder.
Bipolar Disorder
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
INTRODUCTION...........................................................................................................................2
MAIN BODY...................................................................................................................................2
Examine Bipolar Disorder and plan for safe and effective care of a person experiencing this
disorder...................................................................................................................................2
Signs and symptoms and any risks that are associated with the disorder..............................4
Most effective pathway of care for this person and treatment could be provided.................5
CONCLUSION................................................................................................................................7
REFERENCES................................................................................................................................8
INTRODUCTION...........................................................................................................................2
MAIN BODY...................................................................................................................................2
Examine Bipolar Disorder and plan for safe and effective care of a person experiencing this
disorder...................................................................................................................................2
Signs and symptoms and any risks that are associated with the disorder..............................4
Most effective pathway of care for this person and treatment could be provided.................5
CONCLUSION................................................................................................................................7
REFERENCES................................................................................................................................8
INTRODUCTION
Bipolar disorder can be defined as manic depression which depicts mental sickness that
tends to bring changes in mood at the high and low level and also fluctuate the timing factor of
power, thoughts ,sleep and behaviour. Individuals who suffers from bipolar disorder tends to
include time duration in which they feel extremely happy, energised, very sad, hopeless and
sluggish. This disorder includes the feeling of impulsive and reckless decision making and
people also suffers from delusions and hallucinations (Dols & Beekman, (2018)).
Bipolar disorder also carries a term which is “hypomania” that leads to mild indication of
mania where people does not have hallucinations and increased symptoms does not interfere in
usual routine. This disorder includes few episodes of depression which is also known as manic
depression. Apart from this, people with bipolar disorder tends to have trouble in order to
manage their life tasks at the work or maintaining relationships. It does not include any sort for
cure but there are various treatment options that are available which are useful in order to
manage the symptoms. In regard of this, the report leads to cover details regarding the bipolar
disorder and effective care to the specific individual. It also depicts the suitable signs and
symptoms of this disorder and effective pathway to provide treatment to an individual.
MAIN BODY
Examine Bipolar Disorder and plan for safe and effective care of a person experiencing bipolar
disorder
Bipolar disorder which is also known as manic depression is a psychological illness which
leads to extreme changes in the level of activity. These changes leads to impact the overall
ability of an individual in order to carry their business task. This disorder tends to develop in
older teenagers and young adults which are of average age of around 25 years (Dome, Rihmer &
Gonda, (2019)). According to the, National Alliance on Mental illness which is nearly 3% of
adults in United States have bipolar disorder. In regard of this, there are six types of bipolar
disorder that range from most severe to least severe:
Bipolar I disorder
Bipolar II disorder
Cyclothymic disorder (cyclothymia)
Substance/medication induced bipolar and related disorder
Bipolar disorder can be defined as manic depression which depicts mental sickness that
tends to bring changes in mood at the high and low level and also fluctuate the timing factor of
power, thoughts ,sleep and behaviour. Individuals who suffers from bipolar disorder tends to
include time duration in which they feel extremely happy, energised, very sad, hopeless and
sluggish. This disorder includes the feeling of impulsive and reckless decision making and
people also suffers from delusions and hallucinations (Dols & Beekman, (2018)).
Bipolar disorder also carries a term which is “hypomania” that leads to mild indication of
mania where people does not have hallucinations and increased symptoms does not interfere in
usual routine. This disorder includes few episodes of depression which is also known as manic
depression. Apart from this, people with bipolar disorder tends to have trouble in order to
manage their life tasks at the work or maintaining relationships. It does not include any sort for
cure but there are various treatment options that are available which are useful in order to
manage the symptoms. In regard of this, the report leads to cover details regarding the bipolar
disorder and effective care to the specific individual. It also depicts the suitable signs and
symptoms of this disorder and effective pathway to provide treatment to an individual.
MAIN BODY
Examine Bipolar Disorder and plan for safe and effective care of a person experiencing bipolar
disorder
Bipolar disorder which is also known as manic depression is a psychological illness which
leads to extreme changes in the level of activity. These changes leads to impact the overall
ability of an individual in order to carry their business task. This disorder tends to develop in
older teenagers and young adults which are of average age of around 25 years (Dome, Rihmer &
Gonda, (2019)). According to the, National Alliance on Mental illness which is nearly 3% of
adults in United States have bipolar disorder. In regard of this, there are six types of bipolar
disorder that range from most severe to least severe:
Bipolar I disorder
Bipolar II disorder
Cyclothymic disorder (cyclothymia)
Substance/medication induced bipolar and related disorder
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Bipolar and related disorder because of other medical condition
Unspecified bipolar and related disorder
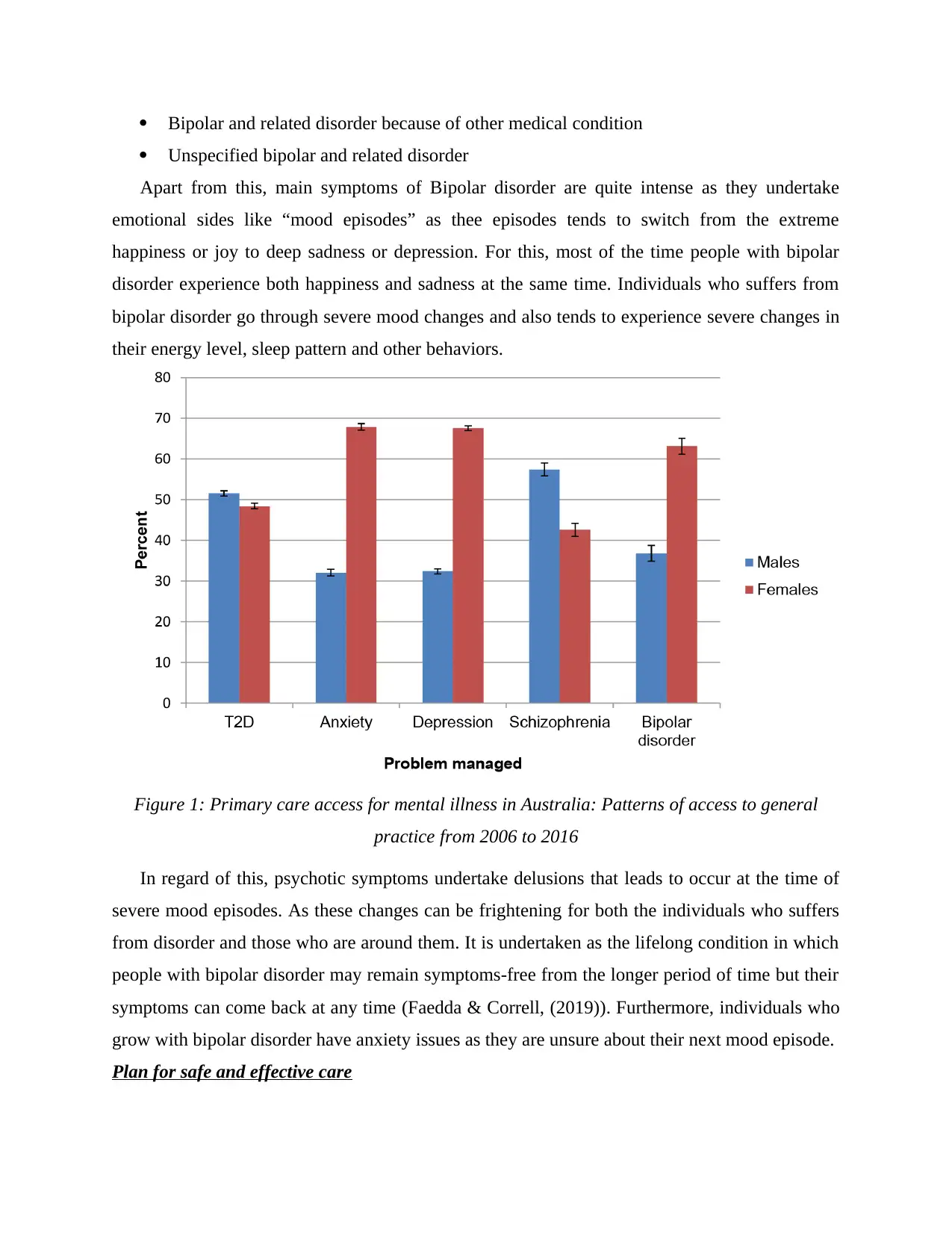
Apart from this, main symptoms of Bipolar disorder are quite intense as they undertake
emotional sides like “mood episodes” as thee episodes tends to switch from the extreme
happiness or joy to deep sadness or depression. For this, most of the time people with bipolar
disorder experience both happiness and sadness at the same time. Individuals who suffers from
bipolar disorder go through severe mood changes and also tends to experience severe changes in
their energy level, sleep pattern and other behaviors.
Figure 1: Primary care access for mental illness in Australia: Patterns of access to general
practice from 2006 to 2016
In regard of this, psychotic symptoms undertake delusions that leads to occur at the time of
severe mood episodes. As these changes can be frightening for both the individuals who suffers
from disorder and those who are around them. It is undertaken as the lifelong condition in which
people with bipolar disorder may remain symptoms-free from the longer period of time but their
symptoms can come back at any time (Faedda & Correll, (2019)). Furthermore, individuals who
grow with bipolar disorder have anxiety issues as they are unsure about their next mood episode.
Plan for safe and effective care
Unspecified bipolar and related disorder
Apart from this, main symptoms of Bipolar disorder are quite intense as they undertake
emotional sides like “mood episodes” as thee episodes tends to switch from the extreme
happiness or joy to deep sadness or depression. For this, most of the time people with bipolar
disorder experience both happiness and sadness at the same time. Individuals who suffers from
bipolar disorder go through severe mood changes and also tends to experience severe changes in
their energy level, sleep pattern and other behaviors.
Figure 1: Primary care access for mental illness in Australia: Patterns of access to general
practice from 2006 to 2016
In regard of this, psychotic symptoms undertake delusions that leads to occur at the time of
severe mood episodes. As these changes can be frightening for both the individuals who suffers
from disorder and those who are around them. It is undertaken as the lifelong condition in which
people with bipolar disorder may remain symptoms-free from the longer period of time but their
symptoms can come back at any time (Faedda & Correll, (2019)). Furthermore, individuals who
grow with bipolar disorder have anxiety issues as they are unsure about their next mood episode.
Plan for safe and effective care
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Living with this disorder is not an easy task as these individuals need proper support in order
to make proper difference in their life conditions prominently their mood episodes. In regard of
this, some of the major steps are discussed as:
Individual who provide care and treatment need to know about bipolar disorder like they
need to understand the symptoms of depressive episodes which is helpful in order to react
effectively during the mood changes.
Carer need to listen by offering answers and advice which is useful for them to deal with
someone who is suffering from bipolar disorder (Hansson & Landén, (2018)). They listen
effectively by paying attention over the words of patient, staying calm while having
conversations, avoid arguments and avoid any sort of topic that seems to frustrate them.
Carer need to be active while offering suitable sessions and therapy and also visit
continuously to doctor by taking regular appointments.
Carer need to make plan as it is important to have an emergency plan which they need to
use it at the time of severe mood episodes. This plan need to include individuals who
have special feelings suicidal at the depressive episode.
Carer need to be understanding for the mental disorders to understand regarding their
experiencing. They also try to understand regarding the offerings and support that can
make big difference.
Signs and symptoms and any risks that are associated with the disorder
National institute of mental health depicts the main symptoms of bipolar disorder which
leads to alternate suitable episodes of low and high mood. In relation to this, change in energy
level, sleep patterns, focus ability and other features leads to change in behaviour of individual,
work relationship and other aspects of life (Wolfers & Marquand, (2018)). For this, most of the
people are experiencing change in mood and other factors which are related with bipolar disorder
that are quite acute in comparisn with mood change and other symptoms . For this, specific
attention is useful in order to make person feel healthier which is helpful in avoiding
medications. Despite from this, major prospects of bipolar disorder can make individual feel
good and also at the elevated mood as they lead to find more creative, talkative and sociable.
Symptoms
to make proper difference in their life conditions prominently their mood episodes. In regard of
this, some of the major steps are discussed as:
Individual who provide care and treatment need to know about bipolar disorder like they
need to understand the symptoms of depressive episodes which is helpful in order to react
effectively during the mood changes.
Carer need to listen by offering answers and advice which is useful for them to deal with
someone who is suffering from bipolar disorder (Hansson & Landén, (2018)). They listen
effectively by paying attention over the words of patient, staying calm while having
conversations, avoid arguments and avoid any sort of topic that seems to frustrate them.
Carer need to be active while offering suitable sessions and therapy and also visit
continuously to doctor by taking regular appointments.
Carer need to make plan as it is important to have an emergency plan which they need to
use it at the time of severe mood episodes. This plan need to include individuals who
have special feelings suicidal at the depressive episode.
Carer need to be understanding for the mental disorders to understand regarding their
experiencing. They also try to understand regarding the offerings and support that can
make big difference.
Signs and symptoms and any risks that are associated with the disorder
National institute of mental health depicts the main symptoms of bipolar disorder which
leads to alternate suitable episodes of low and high mood. In relation to this, change in energy
level, sleep patterns, focus ability and other features leads to change in behaviour of individual,
work relationship and other aspects of life (Wolfers & Marquand, (2018)). For this, most of the
people are experiencing change in mood and other factors which are related with bipolar disorder
that are quite acute in comparisn with mood change and other symptoms . For this, specific
attention is useful in order to make person feel healthier which is helpful in avoiding
medications. Despite from this, major prospects of bipolar disorder can make individual feel
good and also at the elevated mood as they lead to find more creative, talkative and sociable.
Symptoms
As per, International Bipolar Association,indications may vary among individuals as most
of the people tends to last for several months or years. Hence, the hypomania and mania include
fluctuation in moods and is more intense than hypomania as the symptoms include:
Damaged judgement
Feeling wired
Sleeping little but not feeling tired
Sense of distraction
Missing work
Underperforming
Engaging in risky behaviour
Talk a lot and rapidly
Jumping from one topic to another in conversation Denying or not realising that anything is wrong
Depressive symptoms
A feeling of despair, gloom and hopelessness
Extreme sadness
Insomnia and sleeping problems
Anxiety about minor issues
Pain or physical issues that do not respond to treatment
Sense of guilt
Eating more or eating less
Extreme tiredness and fatigue Difficulty in focusing and remembering
Risk factor associated with bipolar disorder
There are many factors which leads to increase in developing risk of bipolar disorder as the
act of triggers guides the first degree relative including parent or sibling, periods of high stress
like loved ones’ decease or other disturbing event, drug or alcohol abuse etc. .This disorder is
caused by various factors which includes: Biological differences- People with bipolar disorder tends to have physical changes in
their brains. The importance of these changes is uncertain but such changes helps in
pinpointing causes (Pinna & Baldessarini, (2019)).
of the people tends to last for several months or years. Hence, the hypomania and mania include
fluctuation in moods and is more intense than hypomania as the symptoms include:
Damaged judgement
Feeling wired
Sleeping little but not feeling tired
Sense of distraction
Missing work
Underperforming
Engaging in risky behaviour
Talk a lot and rapidly
Jumping from one topic to another in conversation Denying or not realising that anything is wrong
Depressive symptoms
A feeling of despair, gloom and hopelessness
Extreme sadness
Insomnia and sleeping problems
Anxiety about minor issues
Pain or physical issues that do not respond to treatment
Sense of guilt
Eating more or eating less
Extreme tiredness and fatigue Difficulty in focusing and remembering
Risk factor associated with bipolar disorder
There are many factors which leads to increase in developing risk of bipolar disorder as the
act of triggers guides the first degree relative including parent or sibling, periods of high stress
like loved ones’ decease or other disturbing event, drug or alcohol abuse etc. .This disorder is
caused by various factors which includes: Biological differences- People with bipolar disorder tends to have physical changes in
their brains. The importance of these changes is uncertain but such changes helps in
pinpointing causes (Pinna & Baldessarini, (2019)).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Genetics is the most common thing in individuals who have first degree relatives like
parents and siblings. Researchers are also trying to find genes that are involved in order
to cause bipolar disorder.
Furthermore, it also includes few complications and serious problems that leads to impact
every area of the life of individual like, problems related to alcohol use, suicide attempts, legal or
financial issues, damaged relationships and poor working performance (Bora, (2018)). Hence, if
an individual has another health conditions that has to be treated with bipolar disorder because
conditions can become worse which will lead to make treatment less successful.
Most effective pathway of care for this person and treatment could be provided
Most effective treatment for bipolar disorder is the combination of medications and mental
therapy because people take more than one drug such as mood stabilising drugs, benzodiazepine,
antipsychotic and antidepressant. Along with this, research has shown that the antidepressants
are quite reliable and safe in order to have effectiveness among individuals with bipolar disorder
which in the form of depression and also leads to make effective use of more controversial things
(Teixeira & Selvaraj, (2019)). Along with this, other types of medicines undertake some mood
stabilizers and suitable atypical antipsychotics which are usually for the line treatment for bipolar
depression. In regard of this, there are various ways to provide care to the individual who is
suffering from bipolar disorder which are as follows:
Biopsychosocial approach
1. This approach is effective as it leads to reduce and take away the pain of patients
undertaking the productivity range for having effective understanding the painful
sensation and searching the best treatment options that have arised due to the staggering
costs. Moreover, this approach also focuses on the sensational modals and the
neurological transmissions identified entirely on the biological level (Takaesu, (2018)).
This approach is useful to treat the patients who are suffering from bipolar disorder as
with the help of this approach people tends to analyse and recognise the relationship
among the central to offer effective health care, they can use self-awareness as the
therapeutic tool, elicit the history of patient in terms of life circumstance, provide
multidimensional treatment and so on.
Recovery-orientated care
parents and siblings. Researchers are also trying to find genes that are involved in order
to cause bipolar disorder.
Furthermore, it also includes few complications and serious problems that leads to impact
every area of the life of individual like, problems related to alcohol use, suicide attempts, legal or
financial issues, damaged relationships and poor working performance (Bora, (2018)). Hence, if
an individual has another health conditions that has to be treated with bipolar disorder because
conditions can become worse which will lead to make treatment less successful.
Most effective pathway of care for this person and treatment could be provided
Most effective treatment for bipolar disorder is the combination of medications and mental
therapy because people take more than one drug such as mood stabilising drugs, benzodiazepine,
antipsychotic and antidepressant. Along with this, research has shown that the antidepressants
are quite reliable and safe in order to have effectiveness among individuals with bipolar disorder
which in the form of depression and also leads to make effective use of more controversial things
(Teixeira & Selvaraj, (2019)). Along with this, other types of medicines undertake some mood
stabilizers and suitable atypical antipsychotics which are usually for the line treatment for bipolar
depression. In regard of this, there are various ways to provide care to the individual who is
suffering from bipolar disorder which are as follows:
Biopsychosocial approach
1. This approach is effective as it leads to reduce and take away the pain of patients
undertaking the productivity range for having effective understanding the painful
sensation and searching the best treatment options that have arised due to the staggering
costs. Moreover, this approach also focuses on the sensational modals and the
neurological transmissions identified entirely on the biological level (Takaesu, (2018)).
This approach is useful to treat the patients who are suffering from bipolar disorder as
with the help of this approach people tends to analyse and recognise the relationship
among the central to offer effective health care, they can use self-awareness as the
therapeutic tool, elicit the history of patient in terms of life circumstance, provide
multidimensional treatment and so on.
Recovery-orientated care
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
This type of care is helpful in relation to psychological health services by offering
informed treatment, rehabilitation and psychosocial support whose objective is to achieve best
outcome for mental health of people and their wellness .In regard to this, people need to
understand the suitable aspirations in order to adapt with suitable needs and precedence of
services. Recovery-oriented services invites all people and for affording them regarding safety
and respect (Tremain, Fletcher & Murray, (2020)). For this, the recovery-oriented mental health
services undertake suitable legislations and budgets to develop and draw for the own skillfulness
and resources to gain better experience to not live with mental health issues, help individuals to
take obligations and reclaim an active role in their life.
Trauma-informed care principles
It represents the trauma care that helps to interpret and consider the distributive nature of
trauma and will lead to development of environment for alleviating and improvement rather than
training and services. In this context, the intention of trauma care is not related with sexual,
physical and affectional abuse of trauma and helps in providing proper assistance services in
effective manner which is accessed and is suitable to those who have proper experience of
psychic trauma(Dome, Rihmer & Gonda, (2019)). Their are various challenges to execute
trauma informed approach that includes shortage of clear segmented definitions,converting
trauma informed care to particular training, services setting, care coordination, shortage of
counselling for providing complex system change and deficiency of evaluating models of trauma
informed care.
CONCLUSION
From the analysis of above presented meta-analysis it can be analysed that, bipolar disorder
is a common disorder, an individual going through this disorder faces various mood swings. This
not only affects its performances in personal life standard but also lead to difficulties in
performing various professional tasks assigned to that individual. Abnormalities within ALN and
related brain region, reduces individual's capacity to think and react to various situations and also
sometimes impact in decision making power of an individual. Several bipolar treatments are
available; it is suggested to every individual that as soon as symptoms of such disorder is seen
should take proper medications.
informed treatment, rehabilitation and psychosocial support whose objective is to achieve best
outcome for mental health of people and their wellness .In regard to this, people need to
understand the suitable aspirations in order to adapt with suitable needs and precedence of
services. Recovery-oriented services invites all people and for affording them regarding safety
and respect (Tremain, Fletcher & Murray, (2020)). For this, the recovery-oriented mental health
services undertake suitable legislations and budgets to develop and draw for the own skillfulness
and resources to gain better experience to not live with mental health issues, help individuals to
take obligations and reclaim an active role in their life.
Trauma-informed care principles
It represents the trauma care that helps to interpret and consider the distributive nature of
trauma and will lead to development of environment for alleviating and improvement rather than
training and services. In this context, the intention of trauma care is not related with sexual,
physical and affectional abuse of trauma and helps in providing proper assistance services in
effective manner which is accessed and is suitable to those who have proper experience of
psychic trauma(Dome, Rihmer & Gonda, (2019)). Their are various challenges to execute
trauma informed approach that includes shortage of clear segmented definitions,converting
trauma informed care to particular training, services setting, care coordination, shortage of
counselling for providing complex system change and deficiency of evaluating models of trauma
informed care.
CONCLUSION
From the analysis of above presented meta-analysis it can be analysed that, bipolar disorder
is a common disorder, an individual going through this disorder faces various mood swings. This
not only affects its performances in personal life standard but also lead to difficulties in
performing various professional tasks assigned to that individual. Abnormalities within ALN and
related brain region, reduces individual's capacity to think and react to various situations and also
sometimes impact in decision making power of an individual. Several bipolar treatments are
available; it is suggested to every individual that as soon as symptoms of such disorder is seen
should take proper medications.
REFERENCES
Books and Journals
Bora, E. (2018). Neurocognitive features in clinical subgroups of bipolar disorder: a meta-
analysis. Journal of affective disorders, 229, 125-134.
Dols, A., & Beekman, A. (2018). Older age bipolar disorder. Psychiatric Clinics, 41(1), 95-110.
Dome, P., Rihmer, Z., & Gonda, X. (2019). Suicide risk in bipolar disorder: a brief
review. Medicina, 55(8), 403.
Faedda, G. L & Correll, C. U. (2019). An International Society of Bipolar Disorders task force
report: Precursors and prodromes of bipolar disorder. Bipolar disorders, 21(8), 720-740.
Hansson, C & Landén, M. (2018). Risk factors for suicide in bipolar disorder: a cohort study of
12 850 patients. Acta Psychiatrica Scandinavica, 138(5), 456-463.
Pinna, M & Baldessarini, R. J. (2019). Attention deficit-hyperactivity disorder in adult bipolar
disorder patients. Journal of affective disorders, 243, 391-396.
Takaesu, Y. (2018). Circadian rhythm in bipolar disorder: a review of the literature. Psychiatry
and clinical neurosciences, 72(9), 673-682.
Teixeira, A. L & Selvaraj, S. (2019). Biomarkers for bipolar disorder: current status and
challenges ahead. Expert review of neurotherapeutics, 19(1), 67-81.
Tremain, H., Fletcher, K., & Murray, G. (2020). Number of episodes in bipolar disorder: The
case for more thoughtful conceptualization and measurement. Bipolar disorders, 22(3),
231-244.
Wolfers, T & Marquand, A. F. (2018). Mapping the heterogeneous phenotype of schizophrenia
and bipolar disorder using normative models. JAMA psychiatry, 75(11), 1146-1155.
Books and Journals
Bora, E. (2018). Neurocognitive features in clinical subgroups of bipolar disorder: a meta-
analysis. Journal of affective disorders, 229, 125-134.
Dols, A., & Beekman, A. (2018). Older age bipolar disorder. Psychiatric Clinics, 41(1), 95-110.
Dome, P., Rihmer, Z., & Gonda, X. (2019). Suicide risk in bipolar disorder: a brief
review. Medicina, 55(8), 403.
Faedda, G. L & Correll, C. U. (2019). An International Society of Bipolar Disorders task force
report: Precursors and prodromes of bipolar disorder. Bipolar disorders, 21(8), 720-740.
Hansson, C & Landén, M. (2018). Risk factors for suicide in bipolar disorder: a cohort study of
12 850 patients. Acta Psychiatrica Scandinavica, 138(5), 456-463.
Pinna, M & Baldessarini, R. J. (2019). Attention deficit-hyperactivity disorder in adult bipolar
disorder patients. Journal of affective disorders, 243, 391-396.
Takaesu, Y. (2018). Circadian rhythm in bipolar disorder: a review of the literature. Psychiatry
and clinical neurosciences, 72(9), 673-682.
Teixeira, A. L & Selvaraj, S. (2019). Biomarkers for bipolar disorder: current status and
challenges ahead. Expert review of neurotherapeutics, 19(1), 67-81.
Tremain, H., Fletcher, K., & Murray, G. (2020). Number of episodes in bipolar disorder: The
case for more thoughtful conceptualization and measurement. Bipolar disorders, 22(3),
231-244.
Wolfers, T & Marquand, A. F. (2018). Mapping the heterogeneous phenotype of schizophrenia
and bipolar disorder using normative models. JAMA psychiatry, 75(11), 1146-1155.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





