Comprehensive Analysis of Blood: From Composition to Blood Groups
VerifiedAdded on 2023/04/20
|13
|3043
|375
Report
AI Summary
This report provides a comprehensive overview of blood, a crucial fluid in humans and animals responsible for transporting nutrients, respiratory gases, and waste. It details the composition of blood, including plasma, erythrocytes, leukocytes, and thrombocytes, and their respective functions in transport, protection, and regulation. The report explains hematopoiesis, the process of blood cell formation, and erythrocyte differentiation. It further discusses the different types of leukocytes and their roles in the immune system, including neutrophils, eosinophils, basophils, lymphocytes, and monocytes. The process of hemostasis, involving vasoconstriction, platelet plug formation, and blood coagulation, is also explained. Finally, the report touches on blood group classification based on the ABO system.

Blood 1
THE BLOOD
By (Student’s Name)
Professor’s Name
College
Course
Date
THE BLOOD
By (Student’s Name)
Professor’s Name
College
Course
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Blood 2
THE BLOOD
Introduction
Blood is a fluid within the bodies of human beings and animals which transports nutrients,
respiratory gases and other organic wastes from the cells of the body to the excretory organs of
the body. The fluid is pumped by the heart organ to all body parts after which the blood returns
to the heart for the repetition of the process (Artkins et al.2017). It flows through the specialized
blood vessels; arteries, veins and capillaries to the respective body cells and tissues.
Components of blood and Functions of blood
The blood constitutes majorly the blood plasma which is the blood fluid. The plasma is 92%
made of water in volume with the remaining portion containing proteins, ions, glucose, blood
cells, and carbon dioxide. The albumin as a major protein within the blood plasma controls the
blood hypotonic pressure (Burnstock 2015). Other components of blood include cells suspended
by the plasma. The blood cells are of different types mainly erythrocytes, leukocytes, and
thrombocytes. The erythrocytes are the most abundant as they are containing hemoglobin which
binds with oxygen hence facilitating respiration. Blood plays major roles including:
Transport
Blood is responsible for the transport and supply of the following in the body.
THE BLOOD
Introduction
Blood is a fluid within the bodies of human beings and animals which transports nutrients,
respiratory gases and other organic wastes from the cells of the body to the excretory organs of
the body. The fluid is pumped by the heart organ to all body parts after which the blood returns
to the heart for the repetition of the process (Artkins et al.2017). It flows through the specialized
blood vessels; arteries, veins and capillaries to the respective body cells and tissues.
Components of blood and Functions of blood
The blood constitutes majorly the blood plasma which is the blood fluid. The plasma is 92%
made of water in volume with the remaining portion containing proteins, ions, glucose, blood
cells, and carbon dioxide. The albumin as a major protein within the blood plasma controls the
blood hypotonic pressure (Burnstock 2015). Other components of blood include cells suspended
by the plasma. The blood cells are of different types mainly erythrocytes, leukocytes, and
thrombocytes. The erythrocytes are the most abundant as they are containing hemoglobin which
binds with oxygen hence facilitating respiration. Blood plays major roles including:
Transport
Blood is responsible for the transport and supply of the following in the body.
Blood 3
Transportation of oxygen gas from the gaseous exchange site, lungs to the body cells and
carbon dioxide to the excretion organ.
The supply of nutrients to the body parts from the digestive tracts where they are assimilated.
Transportation of waste products from the body cells to the detoxification organ like the liver
or the excretory organs like kidney.
Hormonal movement in the body from their secretory organs to the target cells.
Distribution of heat evenly across all parts of the body hence regulating body temperature.
Protection.
Leukocytes are responsible for the destruction of any pathogenic microorganisms which may
find its way into the body thus protecting the body from infections.
Antibodies which are found in the blood are also capable of destroying pathogens in the body
thus protecting the body from infection.
Thrombocytes play a vital role in blood coagulation hence minimizing blood loss through
any mechanical external injury.
Regulation
The blood regulates the body’s pH through interaction with the acids and bases in the body.
Water balance in the body hence ensuring balanced osmotic and ionic pressure.
Transportation of oxygen gas from the gaseous exchange site, lungs to the body cells and
carbon dioxide to the excretion organ.
The supply of nutrients to the body parts from the digestive tracts where they are assimilated.
Transportation of waste products from the body cells to the detoxification organ like the liver
or the excretory organs like kidney.
Hormonal movement in the body from their secretory organs to the target cells.
Distribution of heat evenly across all parts of the body hence regulating body temperature.
Protection.
Leukocytes are responsible for the destruction of any pathogenic microorganisms which may
find its way into the body thus protecting the body from infections.
Antibodies which are found in the blood are also capable of destroying pathogens in the body
thus protecting the body from infection.
Thrombocytes play a vital role in blood coagulation hence minimizing blood loss through
any mechanical external injury.
Regulation
The blood regulates the body’s pH through interaction with the acids and bases in the body.
Water balance in the body hence ensuring balanced osmotic and ionic pressure.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Blood 4
Blood is responsible for regulation of the body’s temperature by equal distribution of heat
throughout the body.
Blood cell formation
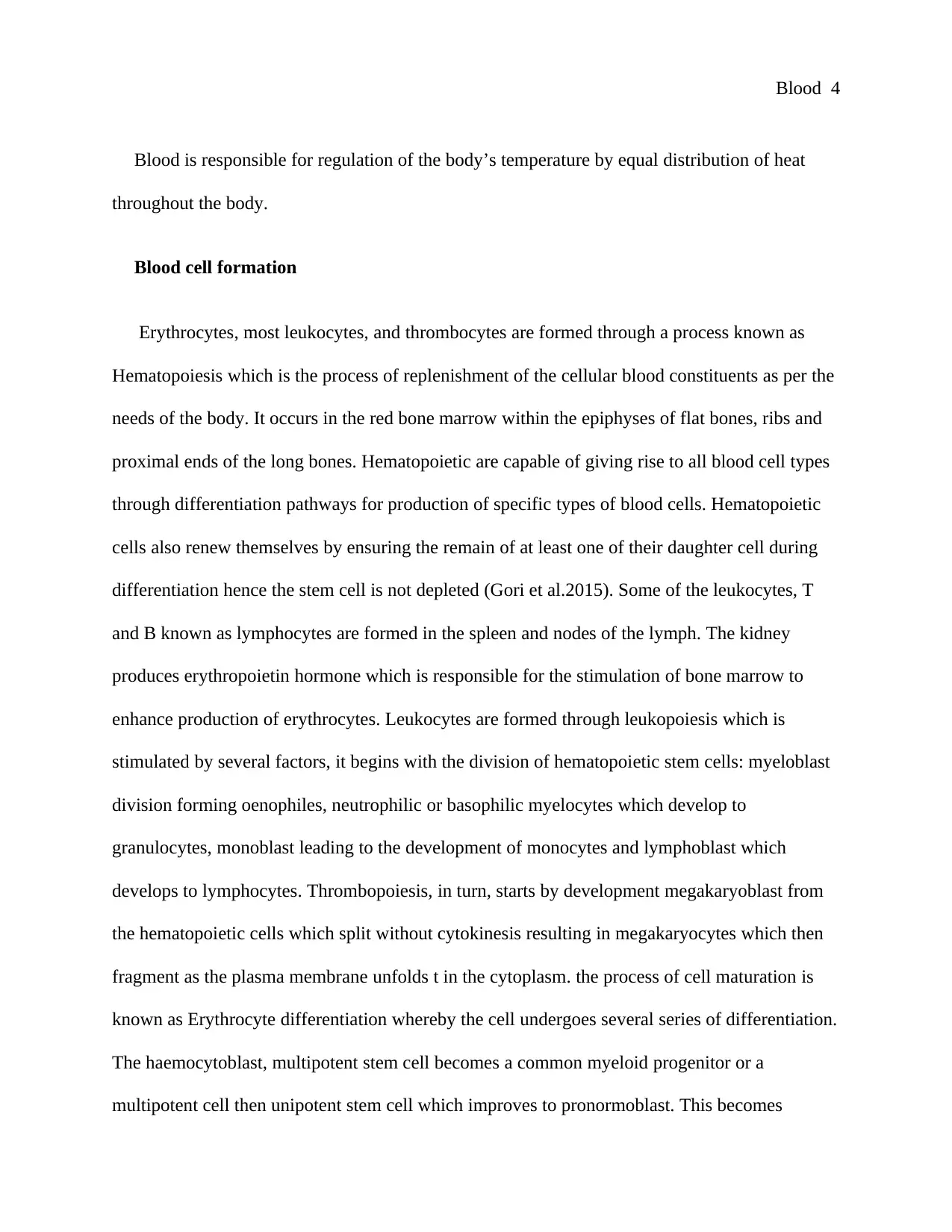
Erythrocytes, most leukocytes, and thrombocytes are formed through a process known as
Hematopoiesis which is the process of replenishment of the cellular blood constituents as per the
needs of the body. It occurs in the red bone marrow within the epiphyses of flat bones, ribs and
proximal ends of the long bones. Hematopoietic are capable of giving rise to all blood cell types
through differentiation pathways for production of specific types of blood cells. Hematopoietic
cells also renew themselves by ensuring the remain of at least one of their daughter cell during
differentiation hence the stem cell is not depleted (Gori et al.2015). Some of the leukocytes, T
and B known as lymphocytes are formed in the spleen and nodes of the lymph. The kidney
produces erythropoietin hormone which is responsible for the stimulation of bone marrow to
enhance production of erythrocytes. Leukocytes are formed through leukopoiesis which is
stimulated by several factors, it begins with the division of hematopoietic stem cells: myeloblast
division forming oenophiles, neutrophilic or basophilic myelocytes which develop to
granulocytes, monoblast leading to the development of monocytes and lymphoblast which
develops to lymphocytes. Thrombopoiesis, in turn, starts by development megakaryoblast from
the hematopoietic cells which split without cytokinesis resulting in megakaryocytes which then
fragment as the plasma membrane unfolds t in the cytoplasm. the process of cell maturation is
known as Erythrocyte differentiation whereby the cell undergoes several series of differentiation.
The haemocytoblast, multipotent stem cell becomes a common myeloid progenitor or a
multipotent cell then unipotent stem cell which improves to pronormoblast. This becomes
Blood is responsible for regulation of the body’s temperature by equal distribution of heat
throughout the body.
Blood cell formation
Erythrocytes, most leukocytes, and thrombocytes are formed through a process known as
Hematopoiesis which is the process of replenishment of the cellular blood constituents as per the
needs of the body. It occurs in the red bone marrow within the epiphyses of flat bones, ribs and
proximal ends of the long bones. Hematopoietic are capable of giving rise to all blood cell types
through differentiation pathways for production of specific types of blood cells. Hematopoietic
cells also renew themselves by ensuring the remain of at least one of their daughter cell during
differentiation hence the stem cell is not depleted (Gori et al.2015). Some of the leukocytes, T
and B known as lymphocytes are formed in the spleen and nodes of the lymph. The kidney
produces erythropoietin hormone which is responsible for the stimulation of bone marrow to
enhance production of erythrocytes. Leukocytes are formed through leukopoiesis which is
stimulated by several factors, it begins with the division of hematopoietic stem cells: myeloblast
division forming oenophiles, neutrophilic or basophilic myelocytes which develop to
granulocytes, monoblast leading to the development of monocytes and lymphoblast which
develops to lymphocytes. Thrombopoiesis, in turn, starts by development megakaryoblast from
the hematopoietic cells which split without cytokinesis resulting in megakaryocytes which then
fragment as the plasma membrane unfolds t in the cytoplasm. the process of cell maturation is
known as Erythrocyte differentiation whereby the cell undergoes several series of differentiation.
The haemocytoblast, multipotent stem cell becomes a common myeloid progenitor or a
multipotent cell then unipotent stem cell which improves to pronormoblast. This becomes
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Blood 5
basophilic before turning to polychromatophilic then orthochromatic. At this stage, there is the
expulsion of the nucleus before the cell becomes reticulocyte. The cell is then released from bone
marrow at the 7th stage.
Hemocytoblast
Common myeloid progenitor Common lymphoid progenitor
Erythrocyte Mast cell Myoblast Natural killer cell Small lymphocyte
T lymhocyte
Megakaryocyte Basophile Neutrophil Eosinophil Monocyte B lymphocyte
Plasma cell
Thrombocyte Macrophage
Red Blood Cells
A mature erythrocyte lacks a nucleus and other cell organelles creating additional space for
hemoglobin. They however have proteins which enable the cell to maintain its unique flexibility
nature hence they can squeeze through thin blood capillaries. Erythrocytes are biconcave in
shape, thin at the center and plump at the periphery of the cell (Tsvirkun et al.2017). The shape
basophilic before turning to polychromatophilic then orthochromatic. At this stage, there is the
expulsion of the nucleus before the cell becomes reticulocyte. The cell is then released from bone
marrow at the 7th stage.
Hemocytoblast
Common myeloid progenitor Common lymphoid progenitor
Erythrocyte Mast cell Myoblast Natural killer cell Small lymphocyte
T lymhocyte
Megakaryocyte Basophile Neutrophil Eosinophil Monocyte B lymphocyte
Plasma cell
Thrombocyte Macrophage
Red Blood Cells
A mature erythrocyte lacks a nucleus and other cell organelles creating additional space for
hemoglobin. They however have proteins which enable the cell to maintain its unique flexibility
nature hence they can squeeze through thin blood capillaries. Erythrocytes are biconcave in
shape, thin at the center and plump at the periphery of the cell (Tsvirkun et al.2017). The shape
Blood 6
increases surface area to volume ratio upon which the gases diffuse easily to the blood plasma
and through the capillary walls.
Hemoglobin which is a molecule within the red blood cells is made up of folded protein
chains known as globin. Each of the globins contains red pigmentation of heme which comprises
of the ion of iron (Fe2+). Every ion in the heme is capable of binding one oxygen molecule.
Hemoglobin binds with oxygen to form oxyhemoglobin after which it distributes the oxygen to
the body. Hemoglobin can also combine with carbon dioxide to form carbaminohemoglobin
whereby it carries the gases to lungs for excretion (Alayash 2017). However, a high amount of
carbon dioxide is carried in the blood plasma as ions of bicarbonate.
The body has a mechanism of dealing with the situations whereby red blood cells get
damaged or get worn out. Liver, spleen and the lymph nodes are the body organs which recycle
red blood cells in such incidences. About 90%are recycled by the macrophages which are found
in the organs the remaining ones are lysed directly into blood plasma as a result of pressure. A
macrophage engulfs the cells, places the cell into a vacuole and then fuses the lysosomes. The
digestive enzymes within the lysosomes are responsible which breakdown the erythrocytes.
Breakdown of the hemoglobin into globin and heme then there is a further breakdown of protein
globin into its constituents of amino acid, the heme group is broken to iron and bilirubin. The
cell can either reuse the byproducts of the breakdown or they get ferried to the bone marrow
whereby they can be reused information of new red blood cells, the bilibrium is excreted through
the kidney.
White Blood Cells
increases surface area to volume ratio upon which the gases diffuse easily to the blood plasma
and through the capillary walls.
Hemoglobin which is a molecule within the red blood cells is made up of folded protein
chains known as globin. Each of the globins contains red pigmentation of heme which comprises
of the ion of iron (Fe2+). Every ion in the heme is capable of binding one oxygen molecule.
Hemoglobin binds with oxygen to form oxyhemoglobin after which it distributes the oxygen to
the body. Hemoglobin can also combine with carbon dioxide to form carbaminohemoglobin
whereby it carries the gases to lungs for excretion (Alayash 2017). However, a high amount of
carbon dioxide is carried in the blood plasma as ions of bicarbonate.
The body has a mechanism of dealing with the situations whereby red blood cells get
damaged or get worn out. Liver, spleen and the lymph nodes are the body organs which recycle
red blood cells in such incidences. About 90%are recycled by the macrophages which are found
in the organs the remaining ones are lysed directly into blood plasma as a result of pressure. A
macrophage engulfs the cells, places the cell into a vacuole and then fuses the lysosomes. The
digestive enzymes within the lysosomes are responsible which breakdown the erythrocytes.
Breakdown of the hemoglobin into globin and heme then there is a further breakdown of protein
globin into its constituents of amino acid, the heme group is broken to iron and bilirubin. The
cell can either reuse the byproducts of the breakdown or they get ferried to the bone marrow
whereby they can be reused information of new red blood cells, the bilibrium is excreted through
the kidney.
White Blood Cells
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Blood 7
Leukocytes the blood cells which are responsible for the immunity system of the human
body. They are normally occurring in a buffy surface as a fine white layer of nucleated cells
deposits erythrocytes and blood serum. The cells have a nucleus, unlike erythrocytes and
thrombocytes. Leukocytes are classified into various categories by structure, size, and functions.
The two major classifications by formation, whether they are granulocytes or agranulocytes or by
the lineage of the cell. The categories are further split into other major types: eosinophils,
basophils, lymphocytes, monocyte, and neutrophils (Vestweber 2015). Granulocytes can be
distinguished from the granulocytes through observation of the shape of their nucleus which is
lobbed into segments and having large cytoplasmic granules. Lineage is another way of
contrasting the cells, myeloid cells can be distinguishable from the lymphoid cells by using
hematopoietic lineage whereby they are further classified as T and B cells.
Neutrophils
They are the most abundant leukocytes. They are in two functional subpopulations,
neutrophil-killers and neutrophil-cagers. They respond first to any infection hence defending the
body against bacterial and fungal infections. Their nucleus is malty lobbed connected by thin
strands, their cytoplasm looks transparent due to light granules which, when stained appear lilac
pale, they occur phagocytic active hence available in high quantity of pus from wounds
(Papayannopoulos 2018). They are incapable of renewing lysosomes within themselves, this
makes them die after phagocytosing pathogens. They have a lifespan of about 5days. Before they
die to form pus.
Eosinophil
Leukocytes the blood cells which are responsible for the immunity system of the human
body. They are normally occurring in a buffy surface as a fine white layer of nucleated cells
deposits erythrocytes and blood serum. The cells have a nucleus, unlike erythrocytes and
thrombocytes. Leukocytes are classified into various categories by structure, size, and functions.
The two major classifications by formation, whether they are granulocytes or agranulocytes or by
the lineage of the cell. The categories are further split into other major types: eosinophils,
basophils, lymphocytes, monocyte, and neutrophils (Vestweber 2015). Granulocytes can be
distinguished from the granulocytes through observation of the shape of their nucleus which is
lobbed into segments and having large cytoplasmic granules. Lineage is another way of
contrasting the cells, myeloid cells can be distinguishable from the lymphoid cells by using
hematopoietic lineage whereby they are further classified as T and B cells.
Neutrophils
They are the most abundant leukocytes. They are in two functional subpopulations,
neutrophil-killers and neutrophil-cagers. They respond first to any infection hence defending the
body against bacterial and fungal infections. Their nucleus is malty lobbed connected by thin
strands, their cytoplasm looks transparent due to light granules which, when stained appear lilac
pale, they occur phagocytic active hence available in high quantity of pus from wounds
(Papayannopoulos 2018). They are incapable of renewing lysosomes within themselves, this
makes them die after phagocytosing pathogens. They have a lifespan of about 5days. Before they
die to form pus.
Eosinophil
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Blood 8
They are about 2% to 4% of the leukocytes They are commonly found in digestive,
respiratory tracts, urinary tracts, and membranes with mucous. They are responsible in response
with the parasitic infections and are predominantly inflammatory cells in case of allergic
reactions they also secret chemical compounds which destroys large parasites like worms in the
body. They are bi-lobed, lobes connected with slender strands and have a cytoplasm full of
granules.
Basophil
They are rare in the body and can be recognized by dark violet granules and are bi-lobed or
trilobed. They are responsible for allergic and antigen whereby they release histamine to cause
dilation of blood vessels (Hoffmann et al. 2015) This makes blood vessels more permeable hence
easing other cells ways of reaching the injured body part.it is also responsible for signaling other
white blood cells to the infected area through secretion of the chemical compound.
Lymphocyte
They are majorly found in the lymphatic system. They are distinguishable by their nucleus
which is deeply stained and not centrally located, plus cytoplasm which is fairly small.
Antibodies made by B cells bind the pathogens blocking their inversion and activating
complement system for their annihilation. The grouping of T-cells are, CD4+ helper T-
lymphocyte have T-lymphocyte receptor and CD4 which in unison binds the antigenic peptide
with T-lymphocyte performing other roles together with the production of cytokines in the
coordination of the defense system.CD8+ h cytotoxic T-lymphocytes engulf antigens available
They are about 2% to 4% of the leukocytes They are commonly found in digestive,
respiratory tracts, urinary tracts, and membranes with mucous. They are responsible in response
with the parasitic infections and are predominantly inflammatory cells in case of allergic
reactions they also secret chemical compounds which destroys large parasites like worms in the
body. They are bi-lobed, lobes connected with slender strands and have a cytoplasm full of
granules.
Basophil
They are rare in the body and can be recognized by dark violet granules and are bi-lobed or
trilobed. They are responsible for allergic and antigen whereby they release histamine to cause
dilation of blood vessels (Hoffmann et al. 2015) This makes blood vessels more permeable hence
easing other cells ways of reaching the injured body part.it is also responsible for signaling other
white blood cells to the infected area through secretion of the chemical compound.
Lymphocyte
They are majorly found in the lymphatic system. They are distinguishable by their nucleus
which is deeply stained and not centrally located, plus cytoplasm which is fairly small.
Antibodies made by B cells bind the pathogens blocking their inversion and activating
complement system for their annihilation. The grouping of T-cells are, CD4+ helper T-
lymphocyte have T-lymphocyte receptor and CD4 which in unison binds the antigenic peptide
with T-lymphocyte performing other roles together with the production of cytokines in the
coordination of the defense system.CD8+ h cytotoxic T-lymphocytes engulf antigens available
Blood 9
on MHC 1 composite of virus infection and kill them (Koh et al.2015). Natural killers are also
capable of killing body cells which do not display MHC class I molecules
Monocyte
They are the largest type of leukocytes and normally share functions with the neutrophils but
have a longer lifespan. They work by presenting pieces of pathogens to T-cells for recognition
and destruction (Das et al.2015). Unlike other cells, they are able to replenish their lysosomes.
They are usually having a kidney-shaped nucleus, typical granulation, and abundance in the
cytoplasm.
Hemostasis
This is the process of slow down and clotting of the blood to minimize or prevent blood
during injury. The blood fluid turns to jelly state. It involves three steps, vasoconstriction, the
formation of the platelets plug and lastly the blood coagulation which enhances the platelets plug
with fibrin mesh which holds together the clot (Austin 2017. This reduces and ceases blood flow
and allows for the restoration of the injured tissue.
In the case of Mark, the medical team applied sterile dressing and pressure. The pressure was
necessary as it would reduce bleeding, during bleeding, the blood comes out at a given pressure
hence the need for application of counter pressure which should slightly higher than the blood
pressure, this will reduce blood flow and give time for clotting (Kairinos et al. 2018).
Furthermore, pressure pushes the blood vessels against the bones, this results in forced
vasocontraction which in turn reduces the amount of blood flowing through the vessels.
on MHC 1 composite of virus infection and kill them (Koh et al.2015). Natural killers are also
capable of killing body cells which do not display MHC class I molecules
Monocyte
They are the largest type of leukocytes and normally share functions with the neutrophils but
have a longer lifespan. They work by presenting pieces of pathogens to T-cells for recognition
and destruction (Das et al.2015). Unlike other cells, they are able to replenish their lysosomes.
They are usually having a kidney-shaped nucleus, typical granulation, and abundance in the
cytoplasm.
Hemostasis
This is the process of slow down and clotting of the blood to minimize or prevent blood
during injury. The blood fluid turns to jelly state. It involves three steps, vasoconstriction, the
formation of the platelets plug and lastly the blood coagulation which enhances the platelets plug
with fibrin mesh which holds together the clot (Austin 2017. This reduces and ceases blood flow
and allows for the restoration of the injured tissue.
In the case of Mark, the medical team applied sterile dressing and pressure. The pressure was
necessary as it would reduce bleeding, during bleeding, the blood comes out at a given pressure
hence the need for application of counter pressure which should slightly higher than the blood
pressure, this will reduce blood flow and give time for clotting (Kairinos et al. 2018).
Furthermore, pressure pushes the blood vessels against the bones, this results in forced
vasocontraction which in turn reduces the amount of blood flowing through the vessels.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Blood 10
Marks body would, in turn, adjust by vasocontraction hence making the blood vessels
narrower, this will slow down the blood flow to the affected area. Secondly, the body will form a
plug made of platelets which will prevent blood loss as the clot will be occurring slowly as the
healing process begins.
Blood Group
Blood is classified into various groups according to the presence or absence of the blood
antibodies and inherited antigenic substances within the red blood cells. The groups are normally
inherited and are a share of contribution from the parents ABO grouping system of blood
considers the antigens A and B and two antibodies (A and B) in individuals with antigens being
found in erythrocytes and antibodies in the plasma (Cooling 2015). The blood here if further
classified into group A with antigen A and antibody B, group B with antigen B and antibody B,
group AB with antigen AB and with no antibodies and group O with no antigen and with
antibody AB.
Rh system of blood grouping. D is the most important Rh antigen as it is most likely to
provoke immune system-negative can produce IgG Anti-D antibodies instead.
Blood compatibility highly considers the antigens, individuals of blood group AB have both
AB antigens and does not contain any antibody against AB antigen hence can be given blood by
the other blood groups and can only give blood to individuals with AB blood group. Group A has
antigen A and IgM antibodies against antigen B, because of this, it can be given blood from
groups A and O and can give blood to blood group A or B. Blood group B have got antigen B,
therefore, can only receive blood from blood group B or blood group O. And can donate blood to
Marks body would, in turn, adjust by vasocontraction hence making the blood vessels
narrower, this will slow down the blood flow to the affected area. Secondly, the body will form a
plug made of platelets which will prevent blood loss as the clot will be occurring slowly as the
healing process begins.
Blood Group
Blood is classified into various groups according to the presence or absence of the blood
antibodies and inherited antigenic substances within the red blood cells. The groups are normally
inherited and are a share of contribution from the parents ABO grouping system of blood
considers the antigens A and B and two antibodies (A and B) in individuals with antigens being
found in erythrocytes and antibodies in the plasma (Cooling 2015). The blood here if further
classified into group A with antigen A and antibody B, group B with antigen B and antibody B,
group AB with antigen AB and with no antibodies and group O with no antigen and with
antibody AB.
Rh system of blood grouping. D is the most important Rh antigen as it is most likely to
provoke immune system-negative can produce IgG Anti-D antibodies instead.
Blood compatibility highly considers the antigens, individuals of blood group AB have both
AB antigens and does not contain any antibody against AB antigen hence can be given blood by
the other blood groups and can only give blood to individuals with AB blood group. Group A has
antigen A and IgM antibodies against antigen B, because of this, it can be given blood from
groups A and O and can give blood to blood group A or B. Blood group B have got antigen B,
therefore, can only receive blood from blood group B or blood group O. And can donate blood to
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Blood 11
group B or AB. Blood group O do not have A, B antigens with their blood having antibodies
IgM anti-A anti-B hence they can only be given from blood group O but can donate blood to any
of the blood groups (Gabriel 2019).
Conclusion
Blood is an important component of the body, the work has highlighted blood components,
blood formation, roles of the blood and its components in the body, blood group, and blood
compatibility and lastly hemostasis with reference to the given scenario. The work portrays the
importance of blood component in human life.
group B or AB. Blood group O do not have A, B antigens with their blood having antibodies
IgM anti-A anti-B hence they can only be given from blood group O but can donate blood to any
of the blood groups (Gabriel 2019).
Conclusion
Blood is an important component of the body, the work has highlighted blood components,
blood formation, roles of the blood and its components in the body, blood group, and blood
compatibility and lastly hemostasis with reference to the given scenario. The work portrays the
importance of blood component in human life.
Blood 12
References
Alayash, A., 2017. Hemoglobin-based blood substitutes and the treatment of sickle cell disease:
more harm than help?. Biomolecules, 7(1), p.2.
Atkins, C.G., Buckley, K., Blades, M.W. and Turner, R.F., 2017. Raman spectroscopy of blood
and blood components. Applied spectroscopy, 71(5), pp.767-793.
Austin, S.K., 2017. Haemostasis. Medicine, 45(4), pp.204-208.
Burnstock, G., 2015. Blood cells: an historical account of the roles of purinergic
signalling. Purinergic signalling, 11(4), pp.411-434.
Cooling, L., 2015. Blood groups in infection and host susceptibility. Clinical microbiology
reviews, 28(3), pp.801-870.
Das, A., Sinha, M., Datta, S., Abas, M., Chaffee, S., Sen, C.K. and Roy, S., 2015. Monocyte and
macrophage plasticity in tissue repair and regeneration. The American journal of
pathology, 185(10), pp.2596-2606.
Gabriel, C., 2016. Choosing the right blood products for transplant patients. ISBT Science
Series, 11(S1), pp.105-110.
Gori, J.L., Butler, J.M., Chan, Y.Y., Chandrasekaran, D., Poulos, M.G., Ginsberg, M., Nolan,
D.J., Elemento, O., Wood, B.L., Adair, J.E. and Rafii, S., 2015. Vascular niche promotes
hematopoietic multipotent progenitor formation from pluripotent stem cells. The Journal of
clinical investigation, 125(3), pp.1243-1254.
References
Alayash, A., 2017. Hemoglobin-based blood substitutes and the treatment of sickle cell disease:
more harm than help?. Biomolecules, 7(1), p.2.
Atkins, C.G., Buckley, K., Blades, M.W. and Turner, R.F., 2017. Raman spectroscopy of blood
and blood components. Applied spectroscopy, 71(5), pp.767-793.
Austin, S.K., 2017. Haemostasis. Medicine, 45(4), pp.204-208.
Burnstock, G., 2015. Blood cells: an historical account of the roles of purinergic
signalling. Purinergic signalling, 11(4), pp.411-434.
Cooling, L., 2015. Blood groups in infection and host susceptibility. Clinical microbiology
reviews, 28(3), pp.801-870.
Das, A., Sinha, M., Datta, S., Abas, M., Chaffee, S., Sen, C.K. and Roy, S., 2015. Monocyte and
macrophage plasticity in tissue repair and regeneration. The American journal of
pathology, 185(10), pp.2596-2606.
Gabriel, C., 2016. Choosing the right blood products for transplant patients. ISBT Science
Series, 11(S1), pp.105-110.
Gori, J.L., Butler, J.M., Chan, Y.Y., Chandrasekaran, D., Poulos, M.G., Ginsberg, M., Nolan,
D.J., Elemento, O., Wood, B.L., Adair, J.E. and Rafii, S., 2015. Vascular niche promotes
hematopoietic multipotent progenitor formation from pluripotent stem cells. The Journal of
clinical investigation, 125(3), pp.1243-1254.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





