Borderline Personality Disorder: Characteristics, Assessment, and Nursing Interventions
VerifiedAdded on 2023/01/10
|11
|2562
|90
AI Summary
This document provides an overview of Borderline Personality Disorder, including its characteristics, assessment methods, and nursing interventions. It discusses the importance of therapeutic communication and psychotherapy in managing the disorder. The document also highlights the prevalence of self-mutilation and suicide in individuals with Borderline Personality Disorder and suggests interventions to address these issues.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: BORDERLINE PERSONALITY DISORDER
Name of the student:
Name of the university:
Author note:
Name of the student:
Name of the university:
Author note:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
2
BORDERLINE PERSONALITY DISORDER
QUESTION 1:
The borderline disorder is also known as emotionally unstable personality disorder which
is characteristics by a long term pattern of abnormal behavior because of an unstable relationship
with others and an unstable sense of self as well as unstable emotions (Cristea et al., 2017). As
discussed by Schulze, Schmahl and Niedtfeld (2016), the patients who often exhibit the behavior
of borderline disorder have a tendency of self-harm. The simulation study represents the
borderline personality disorder of Mary who is 25 years old women diagnosed with the disease.
According to the diagnosis criteria for 301.83 Borderline Personality Disorder, the patient shows
the following pattern
• The frantic effort of avoiding real or imagined abandonment which further contributes to
mutilating behavior which was observed for Mary (Chu, Victor, & Klonsky, 2016).
• A pattern of the unstable and intense interpersonal relationship which can be characterized
by extremes of idealization and devaluation.
• The patient often shows identity disturbance characterized by persistent self-image (Fossati
et al., 2016).
• Impulsivity showed by the patients in two areas which are self-damaging. In the simulation,
the study patient showed the reckless attitude of consuming alcohol and cocaine on weekends
and going out with different guys (Chu, Victor, & Klonsky, (2016).
BORDERLINE PERSONALITY DISORDER
QUESTION 1:
The borderline disorder is also known as emotionally unstable personality disorder which
is characteristics by a long term pattern of abnormal behavior because of an unstable relationship
with others and an unstable sense of self as well as unstable emotions (Cristea et al., 2017). As
discussed by Schulze, Schmahl and Niedtfeld (2016), the patients who often exhibit the behavior
of borderline disorder have a tendency of self-harm. The simulation study represents the
borderline personality disorder of Mary who is 25 years old women diagnosed with the disease.
According to the diagnosis criteria for 301.83 Borderline Personality Disorder, the patient shows
the following pattern
• The frantic effort of avoiding real or imagined abandonment which further contributes to
mutilating behavior which was observed for Mary (Chu, Victor, & Klonsky, 2016).
• A pattern of the unstable and intense interpersonal relationship which can be characterized
by extremes of idealization and devaluation.
• The patient often shows identity disturbance characterized by persistent self-image (Fossati
et al., 2016).
• Impulsivity showed by the patients in two areas which are self-damaging. In the simulation,
the study patient showed the reckless attitude of consuming alcohol and cocaine on weekends
and going out with different guys (Chu, Victor, & Klonsky, (2016).
3
BORDERLINE PERSONALITY DISORDER
• Recurrent suicidal behavior or self-mutilation which was observed, inpatient. She developed
a tendency of self-harm such as cutting her wrist in 4 places, in last places she stitched in order to
avoid the feeling of emptiness (Morey, Benson, & Skodol, 2016).
• An intense feeling of emptiness which she was experiencing
• Intense anger issues and inability to control it.
• Transient as well as stress associated with paranoid ideations or severe dissociative
symptoms.
Question 2:
A borderline personality disorder is the most well-known and dramatic personality
disorder which is characterized by unstable emotions, impulsivity and identifies distortion and
unstable mood and unstable interpersonal relationship (Morey, Benson, & Skodol, 2016).
Patient with a personality disorder often acts impulse which is characterized by the potential for
self-mutilation such injury and stretches, social functioning and impaired coping mechanism.
• In this simulation, creating a therapeutic relationship who has personality disorder is crucial
nursing interventions. The patient often requires a sense of control and giving those choices such
as setting up for appointment may increase adherence (Linehan et al., 2015). In order to provide
the best support to the patient, nurses can involve patients in Impulse Control Training, anger
control and reduction training by providing emotional support, food management, and risk
identification (Morey, Benson, & Skodol, 2016). The nurses are required to involve family
members and other support members to reduce the feeling of abundance.
BORDERLINE PERSONALITY DISORDER
• Recurrent suicidal behavior or self-mutilation which was observed, inpatient. She developed
a tendency of self-harm such as cutting her wrist in 4 places, in last places she stitched in order to
avoid the feeling of emptiness (Morey, Benson, & Skodol, 2016).
• An intense feeling of emptiness which she was experiencing
• Intense anger issues and inability to control it.
• Transient as well as stress associated with paranoid ideations or severe dissociative
symptoms.
Question 2:
A borderline personality disorder is the most well-known and dramatic personality
disorder which is characterized by unstable emotions, impulsivity and identifies distortion and
unstable mood and unstable interpersonal relationship (Morey, Benson, & Skodol, 2016).
Patient with a personality disorder often acts impulse which is characterized by the potential for
self-mutilation such injury and stretches, social functioning and impaired coping mechanism.
• In this simulation, creating a therapeutic relationship who has personality disorder is crucial
nursing interventions. The patient often requires a sense of control and giving those choices such
as setting up for appointment may increase adherence (Linehan et al., 2015). In order to provide
the best support to the patient, nurses can involve patients in Impulse Control Training, anger
control and reduction training by providing emotional support, food management, and risk
identification (Morey, Benson, & Skodol, 2016). The nurses are required to involve family
members and other support members to reduce the feeling of abundance.
4
BORDERLINE PERSONALITY DISORDER
• Considering the therapeutic communication, nurse are require to be clear as the purpose of
communication , use open statement , maintain nonjudgmental attitude towards patients , redirect
the problem of patients , explore the situation to identify critical factors, encourage description of
patients, validate patient’s situation , supporting patients in making association with patients ,
identify the feelings of anxiety and threat, set limits and expectation if patient’s behavior,
focusing on the patient’s responsibility and suggest an alternative method of coping with the
disorder (Gunderson et al., 2015).
• In order to confront patients, nurses are required to set an amount of time for interactions and
incorporate family members in the interventions in order to provide a feeling of security. Setting
a limit is essential for working with the patient with borderline disorder (Costa et al., 2016). It is
important for a nurse to take time in order to set clear boundaries such as defining the
responsibility of patient and nurses during the session and repeating the limit frequently when
working with a personality disorder.
Question 3:
Splitting is considered as a defense mechanism by which people with borderline
personality disorder portrait people, events or themselves. As discussed by Fertuck, Fischer and
Beeney, (2018), splitting can interfere with relationship and contribute to intense and self-
destructive behavior. Patients with a borderline personality disorder often shows the splitting
which is manifested as following behavior:
BORDERLINE PERSONALITY DISORDER
• Considering the therapeutic communication, nurse are require to be clear as the purpose of
communication , use open statement , maintain nonjudgmental attitude towards patients , redirect
the problem of patients , explore the situation to identify critical factors, encourage description of
patients, validate patient’s situation , supporting patients in making association with patients ,
identify the feelings of anxiety and threat, set limits and expectation if patient’s behavior,
focusing on the patient’s responsibility and suggest an alternative method of coping with the
disorder (Gunderson et al., 2015).
• In order to confront patients, nurses are required to set an amount of time for interactions and
incorporate family members in the interventions in order to provide a feeling of security. Setting
a limit is essential for working with the patient with borderline disorder (Costa et al., 2016). It is
important for a nurse to take time in order to set clear boundaries such as defining the
responsibility of patient and nurses during the session and repeating the limit frequently when
working with a personality disorder.
Question 3:
Splitting is considered as a defense mechanism by which people with borderline
personality disorder portrait people, events or themselves. As discussed by Fertuck, Fischer and
Beeney, (2018), splitting can interfere with relationship and contribute to intense and self-
destructive behavior. Patients with a borderline personality disorder often shows the splitting
which is manifested as following behavior:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
5
BORDERLINE PERSONALITY DISORDER
• Acting out such as acting without thinking or considering the consequences of an action
(Vater et al., 2015). In the simulation study, the patient started picking on her wound stitches in
order to deal with the abandonment which experienced during the treatment in the hospital.
• Uncontrolled anger possibly followed by shame and guilt.
• The reactivity, irritability, and anxiety which was experienced by patients (Costa et al.,
2016). In the simulation study, the patient experienced anxiety and empty after being alone or
being abundant. She tried to call her best friend in order to avoid the feeling of anxiety.
• Patients often show unstable self-image or sense of self which includes seeing oneself as
non-existing. In the simulation study, the patient called her best friend and said she was about to
evaporate because nobody in the whole world cares about her.
• Impulsive behavior such as self-mutilation and consuming alcohol which was observed in the
simulation study (Vater et al., 2015).
• The tendency of self-harm which was also exhibited by the patient. She developed a
tendency of self-harm such as cutting her wrist in 4 places; in last places she stitched in order to
avoid the feeling of emptiness.
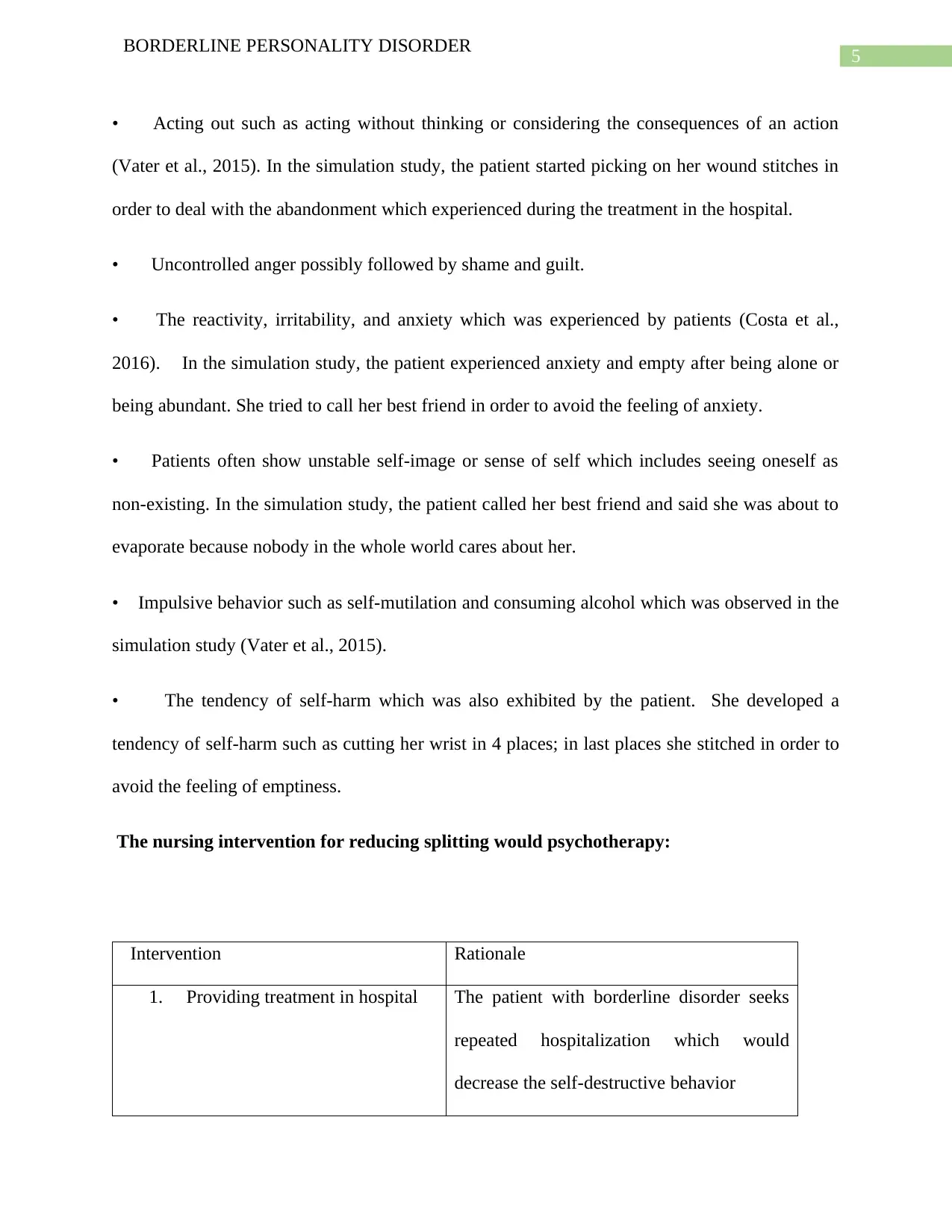
The nursing intervention for reducing splitting would psychotherapy:
Intervention Rationale
1. Providing treatment in hospital The patient with borderline disorder seeks
repeated hospitalization which would
decrease the self-destructive behavior
BORDERLINE PERSONALITY DISORDER
• Acting out such as acting without thinking or considering the consequences of an action
(Vater et al., 2015). In the simulation study, the patient started picking on her wound stitches in
order to deal with the abandonment which experienced during the treatment in the hospital.
• Uncontrolled anger possibly followed by shame and guilt.
• The reactivity, irritability, and anxiety which was experienced by patients (Costa et al.,
2016). In the simulation study, the patient experienced anxiety and empty after being alone or
being abundant. She tried to call her best friend in order to avoid the feeling of anxiety.
• Patients often show unstable self-image or sense of self which includes seeing oneself as
non-existing. In the simulation study, the patient called her best friend and said she was about to
evaporate because nobody in the whole world cares about her.
• Impulsive behavior such as self-mutilation and consuming alcohol which was observed in the
simulation study (Vater et al., 2015).
• The tendency of self-harm which was also exhibited by the patient. She developed a
tendency of self-harm such as cutting her wrist in 4 places; in last places she stitched in order to
avoid the feeling of emptiness.
The nursing intervention for reducing splitting would psychotherapy:
Intervention Rationale
1. Providing treatment in hospital The patient with borderline disorder seeks
repeated hospitalization which would
decrease the self-destructive behavior
6
BORDERLINE PERSONALITY DISORDER
2. Encouragement for the
verbalization of feelings,
perception and insecurities
The nurses are required to understand and
encourage the reason behind frustration
which will help to reduce the feeling of
frustration (Vater et al., 2015).
3. support the use of appropriate
defensive mechanism by patients
Discussing and understanding the feeling of
defenses would reduce the possibility of
acting out.
4. Scheme focused It is combined part of cognitive behavioral
therapy with other therapies which focus on
how patients see themselves. It is helps a
person to recognize negative thought and
adapt new strategies to cope up with disease
(Cristea et al., 2017).
Question 4:
Discuss nursing assessment and related interventions for self – mutilation.
The self-mutilation or self-harm is identified as one of the signs of borderline personality
disorder which observed in patients when patients want to avoid the feeling of abundance and
emptiness. The nurse assessment would:
BORDERLINE PERSONALITY DISORDER
2. Encouragement for the
verbalization of feelings,
perception and insecurities
The nurses are required to understand and
encourage the reason behind frustration
which will help to reduce the feeling of
frustration (Vater et al., 2015).
3. support the use of appropriate
defensive mechanism by patients
Discussing and understanding the feeling of
defenses would reduce the possibility of
acting out.
4. Scheme focused It is combined part of cognitive behavioral
therapy with other therapies which focus on
how patients see themselves. It is helps a
person to recognize negative thought and
adapt new strategies to cope up with disease
(Cristea et al., 2017).
Question 4:
Discuss nursing assessment and related interventions for self – mutilation.
The self-mutilation or self-harm is identified as one of the signs of borderline personality
disorder which observed in patients when patients want to avoid the feeling of abundance and
emptiness. The nurse assessment would:
7
BORDERLINE PERSONALITY DISORDER
1. Assessing the patient’s history of self-mutilation such as type of mutilation, frequency of the
behavior and stress presiding behavior which include the patterns and circumstances, which
induces the behavior (Terzi et al., 2016).
2. Identification of the feelings experienced by patients such as rage, anxiety, and emptiness
3. Exploration of feeling such as self-mutilation might be a way of relieving anxiety,
expression of self-hate and feeling alive (Terzi et al., 2016)
4. Identification of steps taken by patients when patients are experiencing an urge of self-
mutilation such as a person to call upon as observed in this simulation study.
The nursing intervention of the self-mutilation would be:
• Nurses are required to a matter of fact approach during the situation and avoiding criticisms
behavior
• Develop alternative behavior to self- mutilating behavior such as identification of actions
which might reduce the act of self-mutilation and identify the individuals whom patients can
contact when they experience the urge (Vega et al., 2017).
• Patients are required to provide with medications such as antidepressants to reduce anxiety
and behavior. It will reduce the behavior of self-injury.
• Patients are required to provide cognitive behavioral therapy which can help people to
identify and change inaccurate perception. It also helps to reduce the anxiety symptoms and
frequency self-harms (Vega et al., 2017).
Question 5:
BORDERLINE PERSONALITY DISORDER
1. Assessing the patient’s history of self-mutilation such as type of mutilation, frequency of the
behavior and stress presiding behavior which include the patterns and circumstances, which
induces the behavior (Terzi et al., 2016).
2. Identification of the feelings experienced by patients such as rage, anxiety, and emptiness
3. Exploration of feeling such as self-mutilation might be a way of relieving anxiety,
expression of self-hate and feeling alive (Terzi et al., 2016)
4. Identification of steps taken by patients when patients are experiencing an urge of self-
mutilation such as a person to call upon as observed in this simulation study.
The nursing intervention of the self-mutilation would be:
• Nurses are required to a matter of fact approach during the situation and avoiding criticisms
behavior
• Develop alternative behavior to self- mutilating behavior such as identification of actions
which might reduce the act of self-mutilation and identify the individuals whom patients can
contact when they experience the urge (Vega et al., 2017).
• Patients are required to provide with medications such as antidepressants to reduce anxiety
and behavior. It will reduce the behavior of self-injury.
• Patients are required to provide cognitive behavioral therapy which can help people to
identify and change inaccurate perception. It also helps to reduce the anxiety symptoms and
frequency self-harms (Vega et al., 2017).
Question 5:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
BORDERLINE PERSONALITY DISORDER
Suicide is one of the common symptoms of Borderline personality disorder identifies by DSM V
diagnostic criteria. As discussed by Andrewes et al. (2017), 80% of the patients who are
experiencing borderline disorder develop the tendency of suicide. Out of 80% who are
experiencing borderline personality disorder, 10% to 12% commit suicide as a symptom of the
disorder. Hence, nursing intervention is required to design for preventing suicide (Homan et al.,
2017). The crucial non-pharmacological intervention for reducing suicide is dialectical behavior
therapy. It is an evidence-based therapy developed by linen in order to treat chronically suicidal
individuals having borderline disorders (Homan et al., 2017). This therapy combines with
cognitive as well as behavioral techniques such as mindfulness behavior that emphasizes on
reframing the thoughts of the patients (Vega et al., 2017). Other interventions for precaution of
suicide include providing education to the patients and family members, Suicide assessment,
monitoring the behavior of the patients and self-harm and providing medication such as
antidepressants, antipsychotics and opioid antagonist for reducing the behavior of self-injury.
Question 5:
Reflective journal:
Considering the self-evaluation of the process, I have identified that previously I was
unaware of the borderline disorder and often confuse it with bipolar disorder or obsessive-
compulsive behavior. After completing the assessment I gained the understanding of the
borderline disorder and how to assess the patients as well as how to effectively manage the
patients. This will further help me to enhance my future practice since I would be incorporating
the knowledge in future practice. However, the weakness that was observed is that I felt lost
while I was gaining an understanding of the situation and I am biased towards the interventions
BORDERLINE PERSONALITY DISORDER
Suicide is one of the common symptoms of Borderline personality disorder identifies by DSM V
diagnostic criteria. As discussed by Andrewes et al. (2017), 80% of the patients who are
experiencing borderline disorder develop the tendency of suicide. Out of 80% who are
experiencing borderline personality disorder, 10% to 12% commit suicide as a symptom of the
disorder. Hence, nursing intervention is required to design for preventing suicide (Homan et al.,
2017). The crucial non-pharmacological intervention for reducing suicide is dialectical behavior
therapy. It is an evidence-based therapy developed by linen in order to treat chronically suicidal
individuals having borderline disorders (Homan et al., 2017). This therapy combines with
cognitive as well as behavioral techniques such as mindfulness behavior that emphasizes on
reframing the thoughts of the patients (Vega et al., 2017). Other interventions for precaution of
suicide include providing education to the patients and family members, Suicide assessment,
monitoring the behavior of the patients and self-harm and providing medication such as
antidepressants, antipsychotics and opioid antagonist for reducing the behavior of self-injury.
Question 5:
Reflective journal:
Considering the self-evaluation of the process, I have identified that previously I was
unaware of the borderline disorder and often confuse it with bipolar disorder or obsessive-
compulsive behavior. After completing the assessment I gained the understanding of the
borderline disorder and how to assess the patients as well as how to effectively manage the
patients. This will further help me to enhance my future practice since I would be incorporating
the knowledge in future practice. However, the weakness that was observed is that I felt lost
while I was gaining an understanding of the situation and I am biased towards the interventions
9
BORDERLINE PERSONALITY DISORDER
which can be provided to the patients. I would require to explore other interventions in order to
remove biases.
References:
Andrewes, H. E., Hulbert, C., Cotton, S. M., Betts, J., & Chanen, A. M. (2019). Relationships
between the frequency and severity of non‐suicidal self‐injury and suicide attempts in
youth with borderline personality disorder. Early intervention in psychiatry, 13(2), 194-
201.
Chu, C., Victor, S. E., & Klonsky, E. D. (2016). Characterizing positive and negative emotional
experiences in young adults with Borderline Personality Disorder symptoms. Journal of
clinical psychology, 72(9), 956-965.
Costa, J., Marôco, J., Pinto‐Gouveia, J., Ferreira, C., & Castilho, P. (2016). Validation of the
psychometric properties of the Self‐Compassion Scale. Testing the factorial validity and
factorial invariance of the measure among borderline personality disorder, anxiety
disorder, eating disorder and general populations. Clinical Psychology &
Psychotherapy, 23(5), 460-468.
Cristea, I. A., Gentili, C., Cotet, C. D., Palomba, D., Barbui, C., & Cuijpers, P. (2017). Efficacy
of psychotherapies for borderline personality disorder: a systematic review and meta-
analysis. Jama psychiatry, 74(4), 319-328.
Fertuck, E. A., Fischer, S., & Beeney, J. (2018). Social Cognition and Borderline Personality
Disorder: Splitting and Trust Impairment Findings. Psychiatric Clinics, 41(4), 613-632.
BORDERLINE PERSONALITY DISORDER
which can be provided to the patients. I would require to explore other interventions in order to
remove biases.
References:
Andrewes, H. E., Hulbert, C., Cotton, S. M., Betts, J., & Chanen, A. M. (2019). Relationships
between the frequency and severity of non‐suicidal self‐injury and suicide attempts in
youth with borderline personality disorder. Early intervention in psychiatry, 13(2), 194-
201.
Chu, C., Victor, S. E., & Klonsky, E. D. (2016). Characterizing positive and negative emotional
experiences in young adults with Borderline Personality Disorder symptoms. Journal of
clinical psychology, 72(9), 956-965.
Costa, J., Marôco, J., Pinto‐Gouveia, J., Ferreira, C., & Castilho, P. (2016). Validation of the
psychometric properties of the Self‐Compassion Scale. Testing the factorial validity and
factorial invariance of the measure among borderline personality disorder, anxiety
disorder, eating disorder and general populations. Clinical Psychology &
Psychotherapy, 23(5), 460-468.
Cristea, I. A., Gentili, C., Cotet, C. D., Palomba, D., Barbui, C., & Cuijpers, P. (2017). Efficacy
of psychotherapies for borderline personality disorder: a systematic review and meta-
analysis. Jama psychiatry, 74(4), 319-328.
Fertuck, E. A., Fischer, S., & Beeney, J. (2018). Social Cognition and Borderline Personality
Disorder: Splitting and Trust Impairment Findings. Psychiatric Clinics, 41(4), 613-632.
10
BORDERLINE PERSONALITY DISORDER
Fossati, A., Somma, A., Borroni, S., Maffei, C., Markon, K. E., & Krueger, R. F. (2016).
Borderline personality disorder and narcissistic personality disorder diagnoses from the
perspective of the DSM-5 personality traits: A study on Italian clinical participants. The
Journal of nervous and mental disease, 204(12), 939-949.
Gunderson, J. G., Herpertz, S. C., Skodol, A. E., Torgersen, S., & Zanarini, M. C. (2018).
Borderline personality disorder. Nature Reviews Disease Primers, 4, 18029.
Homan, K. J., Sim, L. A., Fargo, J. D., & Twohig, M. P. (2017). Five-year prospective
investigation of self-harm/suicide-related behaviors in the development of borderline
personality disorder. Personality Disorders: Theory, Research, and Treatment, 8(2), 183.
Linehan, M. M., Korslund, K. E., Harned, M. S., Gallop, R. J., Lungu, A., Neacsiu, A. D., ... &
Murray-Gregory, A. M. (2015). Dialectical behavior therapy for high suicide risk in
individuals with borderline personality disorder: a randomized clinical trial and
component analysis. JAMA psychiatry, 72(5), 475-482.
Morey, L. C., Benson, K. T., & Skodol, A. E. (2016). Relating DSM-5 section III personality
traits to section II personality disorder diagnoses. Psychological Medicine, 46(3), 647-
655.
Schulze, L., Schmahl, C., & Niedtfeld, I. (2016). Neural correlates of disturbed emotion
processing in borderline personality disorder: a multimodal meta-analysis. Biological
psychiatry, 79(2), 97-106.
Terzi, L., Martino, F., Berardi, D., Bortolotti, B., Sasdelli, A., & Menchetti, M. (2017).
Aggressive behavior and self-harm in Borderline Personality Disorder: The role of
BORDERLINE PERSONALITY DISORDER
Fossati, A., Somma, A., Borroni, S., Maffei, C., Markon, K. E., & Krueger, R. F. (2016).
Borderline personality disorder and narcissistic personality disorder diagnoses from the
perspective of the DSM-5 personality traits: A study on Italian clinical participants. The
Journal of nervous and mental disease, 204(12), 939-949.
Gunderson, J. G., Herpertz, S. C., Skodol, A. E., Torgersen, S., & Zanarini, M. C. (2018).
Borderline personality disorder. Nature Reviews Disease Primers, 4, 18029.
Homan, K. J., Sim, L. A., Fargo, J. D., & Twohig, M. P. (2017). Five-year prospective
investigation of self-harm/suicide-related behaviors in the development of borderline
personality disorder. Personality Disorders: Theory, Research, and Treatment, 8(2), 183.
Linehan, M. M., Korslund, K. E., Harned, M. S., Gallop, R. J., Lungu, A., Neacsiu, A. D., ... &
Murray-Gregory, A. M. (2015). Dialectical behavior therapy for high suicide risk in
individuals with borderline personality disorder: a randomized clinical trial and
component analysis. JAMA psychiatry, 72(5), 475-482.
Morey, L. C., Benson, K. T., & Skodol, A. E. (2016). Relating DSM-5 section III personality
traits to section II personality disorder diagnoses. Psychological Medicine, 46(3), 647-
655.
Schulze, L., Schmahl, C., & Niedtfeld, I. (2016). Neural correlates of disturbed emotion
processing in borderline personality disorder: a multimodal meta-analysis. Biological
psychiatry, 79(2), 97-106.
Terzi, L., Martino, F., Berardi, D., Bortolotti, B., Sasdelli, A., & Menchetti, M. (2017).
Aggressive behavior and self-harm in Borderline Personality Disorder: The role of
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
11
BORDERLINE PERSONALITY DISORDER
impulsivity and emotion dysregulation in a sample of outpatients. Psychiatry
research, 249, 321-326.
Vater, A., Schröder-Abé, M., Weißgerber, S., Roepke, S., & Schütz, A. (2015). Self-concept
structure and borderline personality disorder: evidence for negative
compartmentalization. Journal of behavior therapy and experimental psychiatry, 46, 50-
58.
Vega, D., Torrubia, R., Soto, À., Ribas, J., Soler, J., Pascual, J. C., ... & Marco-Pallarés, J.
(2017). Exploring the relationship between non suicidal self-injury and borderline
personality traits in young adults. Psychiatry research, 256, 403-411.
BORDERLINE PERSONALITY DISORDER
impulsivity and emotion dysregulation in a sample of outpatients. Psychiatry
research, 249, 321-326.
Vater, A., Schröder-Abé, M., Weißgerber, S., Roepke, S., & Schütz, A. (2015). Self-concept
structure and borderline personality disorder: evidence for negative
compartmentalization. Journal of behavior therapy and experimental psychiatry, 46, 50-
58.
Vega, D., Torrubia, R., Soto, À., Ribas, J., Soler, J., Pascual, J. C., ... & Marco-Pallarés, J.
(2017). Exploring the relationship between non suicidal self-injury and borderline
personality traits in young adults. Psychiatry research, 256, 403-411.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





