Breathlessness | Nursing | Case Study
VerifiedAdded on 2022/09/01
|11
|2842
|16
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: NURSING
Nursing
Name of the Student
Name of the University
Author Note
Nursing
Name of the Student
Name of the University
Author Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1
NURSING
Introduction
The following assignment is based on the case study of Russell who is a truck driver.
Russell is 68 years old. He was admitted to the Monash Health with symptoms of
breathlessness. Doctor’s investigation revealed that Russell has developed heart failure.
Russell has previous reported cases of heart attack and COPD and he was an active smoker.
This assignment is questions and answers based assignment. The initiation of the assignment
will be done based on the reasons underlying Russell’s heart failure. This will be followed by
detailed description of the exacerbations of COPD followed by the mode of actions of certain
medications and nursing interventions (non-pharmacological) in order to manage the nursing
priority.
Risk factors contributed to disease development
Russell had encountered heart failure 15-years ago and the same was treated with
stent. Fatima, Naqvi and Hanook (2019) older adults who are above 60 years of age and have
previous reported cases of cardiovascular stroke are more vulnerable to develop heart failure.
The presence of reported cases of Chronic Obstructive Pulmonary Disease (COPD) further
increases the overall risk factors of heart failure. Russell had COPD for the past 30 years and
had smoking habits. Bayrak and Tosun (2018) stated that presence of COPD, for a prolong
tenure of time decrease the overall oxygen carrying capacity of the lungs and thereby
decreasing the overall oxygen content of blood. In the absence of adequate oxygen in the
heart, the cardiac muscles are being forced to pump at higher rated and thus increasing the
heart rate and blood pressure and thereby increasing the risk factors of heart failure. Russell
also had previous pre-disposition of hyper-tension as indicated by the medication history if
anti-hypertensive drug (Atenolol). Fatima, Naqvi and Hanook (2019) further argued that
presence of COPD increase the tendency of heart failure due to the formation of pulmonary
NURSING
Introduction
The following assignment is based on the case study of Russell who is a truck driver.
Russell is 68 years old. He was admitted to the Monash Health with symptoms of
breathlessness. Doctor’s investigation revealed that Russell has developed heart failure.
Russell has previous reported cases of heart attack and COPD and he was an active smoker.
This assignment is questions and answers based assignment. The initiation of the assignment
will be done based on the reasons underlying Russell’s heart failure. This will be followed by
detailed description of the exacerbations of COPD followed by the mode of actions of certain
medications and nursing interventions (non-pharmacological) in order to manage the nursing
priority.
Risk factors contributed to disease development
Russell had encountered heart failure 15-years ago and the same was treated with
stent. Fatima, Naqvi and Hanook (2019) older adults who are above 60 years of age and have
previous reported cases of cardiovascular stroke are more vulnerable to develop heart failure.
The presence of reported cases of Chronic Obstructive Pulmonary Disease (COPD) further
increases the overall risk factors of heart failure. Russell had COPD for the past 30 years and
had smoking habits. Bayrak and Tosun (2018) stated that presence of COPD, for a prolong
tenure of time decrease the overall oxygen carrying capacity of the lungs and thereby
decreasing the overall oxygen content of blood. In the absence of adequate oxygen in the
heart, the cardiac muscles are being forced to pump at higher rated and thus increasing the
heart rate and blood pressure and thereby increasing the risk factors of heart failure. Russell
also had previous pre-disposition of hyper-tension as indicated by the medication history if
anti-hypertensive drug (Atenolol). Fatima, Naqvi and Hanook (2019) further argued that
presence of COPD increase the tendency of heart failure due to the formation of pulmonary
2
NURSING
oedema. In this case, the chest X-ray of Russell revealed that cardiophrenic and costophrenic
angles indicating suggestive of pulmonary oedema. This again increases the risk factors of
heart failure. The Echocardio-gram indicated dilated left ventricle along with dysfunction in
the systolic side of the heart with left ventricular ejection fraction (LVEF) is 25%., indicating
the chances of left-sided heart failure.
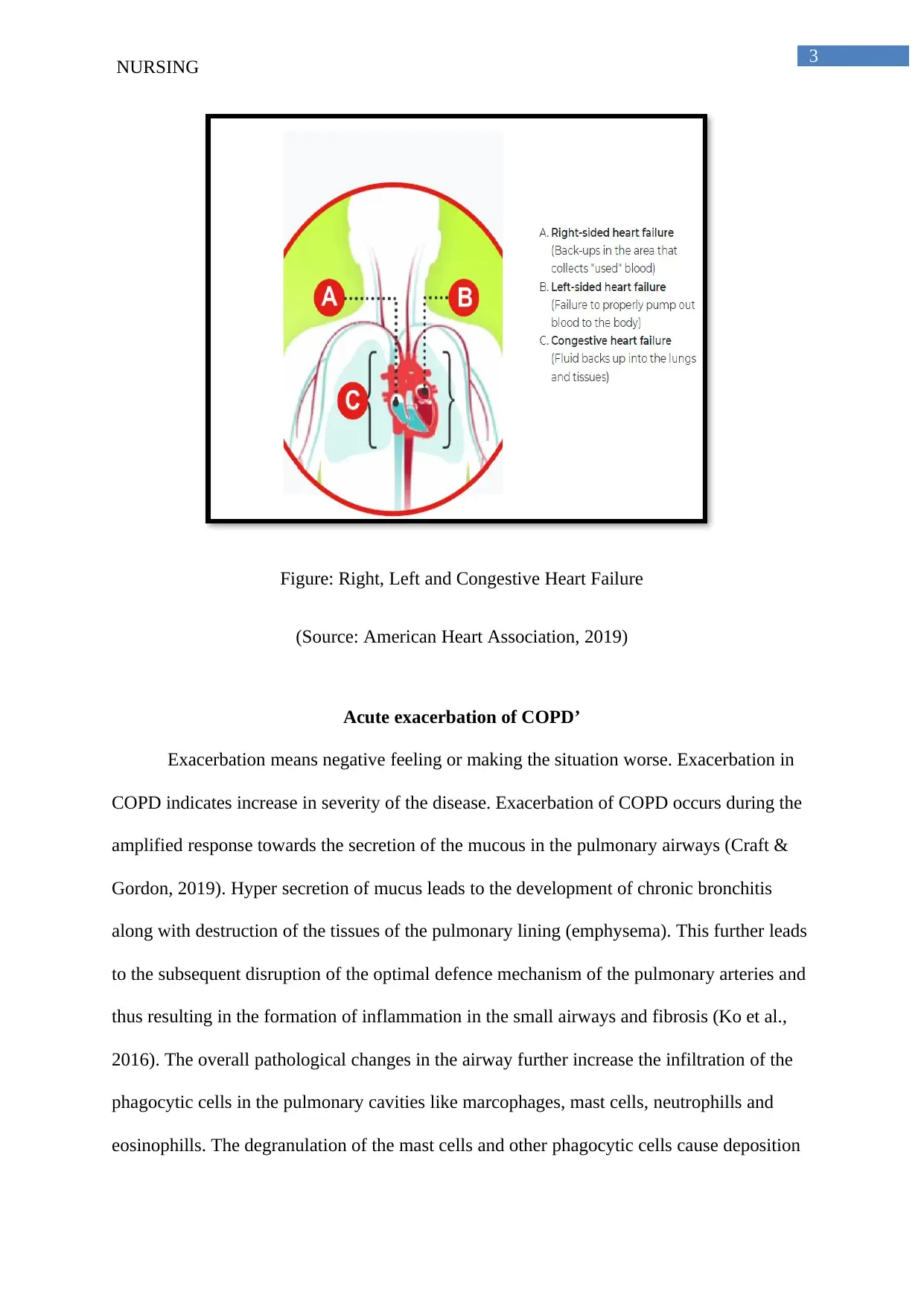
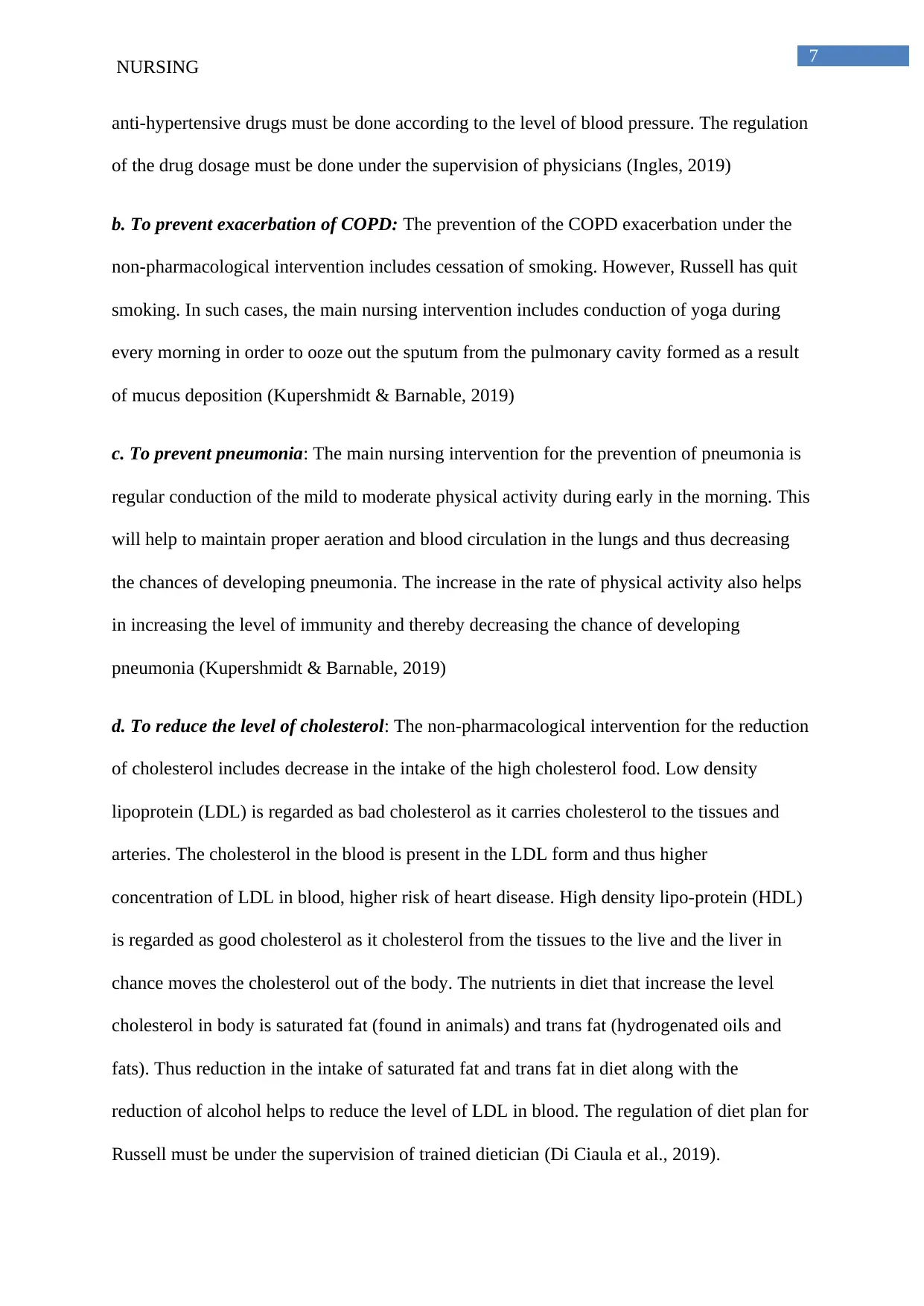
Pathophysiology of left and right sided heart’s failure
There are two types of heart failure, left and right sided heart failure. The left sided
heart failure is again divided into two categories. First one is diastolic heart failure occurring
due to preserved ejection fraction and the second one is systolic heart failure occurring due to
reduced ejection fraction. Russell is suffering from left sided systolic heart failure because his
echo-cardiogram indicated reduced left ventricular ejection fraction. The right sided-heart
failure occurs as a result of occurrence of the left sided heart failure (Bosch et al., 2017).
After the failure of the left sided heart, the overall fluid pressure is transferred to the lungs.
This leads to the damage of the arteries and veins present at the right side of the heart. The
damage of the right sided ventricle and arteries ultimately leads to the back flow of the blood
into the veins and ultimately resulting in the development of the right sided heart failure. In
case of the right sided heart failure, the main symptoms that are pronounced included
swelling of the peripheral regions of the body like the foot ankle along with swelling of the
gastro-intestinal tract of liver (Bosch et al., 2017).
The detection of the left sided heart failure can be done with the help of echo-cardio-
gram as in case of Russell. In case of right-sided heart failure, the detection can be done with
the both echo-cardiogram and by conducting the chest X-ray. The result of the chest X-ray
will indicate the presence of pulmonary congestion (Bosch et al., 2017).
NURSING
oedema. In this case, the chest X-ray of Russell revealed that cardiophrenic and costophrenic
angles indicating suggestive of pulmonary oedema. This again increases the risk factors of
heart failure. The Echocardio-gram indicated dilated left ventricle along with dysfunction in
the systolic side of the heart with left ventricular ejection fraction (LVEF) is 25%., indicating
the chances of left-sided heart failure.
Pathophysiology of left and right sided heart’s failure
There are two types of heart failure, left and right sided heart failure. The left sided
heart failure is again divided into two categories. First one is diastolic heart failure occurring
due to preserved ejection fraction and the second one is systolic heart failure occurring due to
reduced ejection fraction. Russell is suffering from left sided systolic heart failure because his
echo-cardiogram indicated reduced left ventricular ejection fraction. The right sided-heart
failure occurs as a result of occurrence of the left sided heart failure (Bosch et al., 2017).
After the failure of the left sided heart, the overall fluid pressure is transferred to the lungs.
This leads to the damage of the arteries and veins present at the right side of the heart. The
damage of the right sided ventricle and arteries ultimately leads to the back flow of the blood
into the veins and ultimately resulting in the development of the right sided heart failure. In
case of the right sided heart failure, the main symptoms that are pronounced included
swelling of the peripheral regions of the body like the foot ankle along with swelling of the
gastro-intestinal tract of liver (Bosch et al., 2017).
The detection of the left sided heart failure can be done with the help of echo-cardio-
gram as in case of Russell. In case of right-sided heart failure, the detection can be done with
the both echo-cardiogram and by conducting the chest X-ray. The result of the chest X-ray
will indicate the presence of pulmonary congestion (Bosch et al., 2017).
3
NURSING
Figure: Right, Left and Congestive Heart Failure
(Source: American Heart Association, 2019)
Acute exacerbation of COPD’
Exacerbation means negative feeling or making the situation worse. Exacerbation in
COPD indicates increase in severity of the disease. Exacerbation of COPD occurs during the
amplified response towards the secretion of the mucous in the pulmonary airways (Craft &
Gordon, 2019). Hyper secretion of mucus leads to the development of chronic bronchitis
along with destruction of the tissues of the pulmonary lining (emphysema). This further leads
to the subsequent disruption of the optimal defence mechanism of the pulmonary arteries and
thus resulting in the formation of inflammation in the small airways and fibrosis (Ko et al.,
2016). The overall pathological changes in the airway further increase the infiltration of the
phagocytic cells in the pulmonary cavities like marcophages, mast cells, neutrophills and
eosinophills. The degranulation of the mast cells and other phagocytic cells cause deposition
NURSING
Figure: Right, Left and Congestive Heart Failure
(Source: American Heart Association, 2019)
Acute exacerbation of COPD’
Exacerbation means negative feeling or making the situation worse. Exacerbation in
COPD indicates increase in severity of the disease. Exacerbation of COPD occurs during the
amplified response towards the secretion of the mucous in the pulmonary airways (Craft &
Gordon, 2019). Hyper secretion of mucus leads to the development of chronic bronchitis
along with destruction of the tissues of the pulmonary lining (emphysema). This further leads
to the subsequent disruption of the optimal defence mechanism of the pulmonary arteries and
thus resulting in the formation of inflammation in the small airways and fibrosis (Ko et al.,
2016). The overall pathological changes in the airway further increase the infiltration of the
phagocytic cells in the pulmonary cavities like marcophages, mast cells, neutrophills and
eosinophills. The degranulation of the mast cells and other phagocytic cells cause deposition
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4
NURSING
of the anti-inflammatory inhibitors in the pulmonary cavities and thus hampering the oxygen
carrying capacity of the lungs and increasing exacerbation. Acute exacerbations are regarded
as one of the leading cause of hospitalization among the older adults leading to increased rate
of mortality and morbidity (Flattet et al., 2017). In the domain of exacerbation of the COPD,
Crisafulli, Barbeta, Ielpo and Torres (2018) have stated that smoking for a prolong period of
time, leads to the loss of elasticity of the pulmonary tissues along with damage of cilia of the
lungs and thus increasing the exacerbations further and increased need for hospitalization.
In case of Russell, the increase in the cellular infiltrate inside the pulmonary cavities
and resulting in the acute exacerbation of COPD is due to the previous habit of smoking.
Russell used to smoke 20 cigarettes per day when he was 18 years and he ceased cigarette
smoking after encountering the heart attack (15 years back). This prolong tendency of
cigarette smoking resulting in thick mucus deposition in the pulmonary cavities and the
generation of the inflammatory response increase the severity of the COPD. Exacerbations of
COPD is common among the male, and cigarette smoking in Russell have increased his
severity further (Ko et al., 2016).
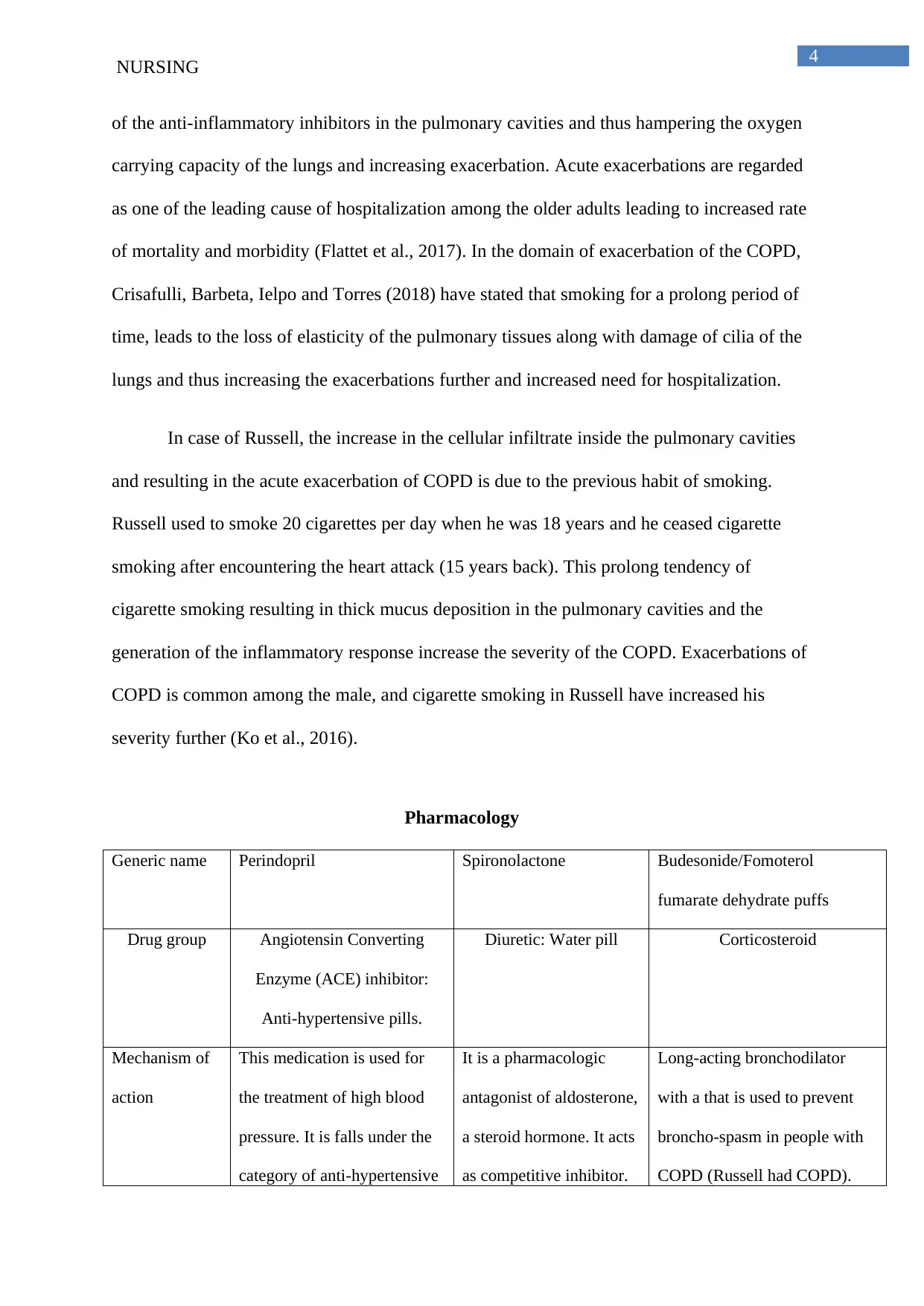
Pharmacology
Generic name Perindopril Spironolactone Budesonide/Fomoterol
fumarate dehydrate puffs
Drug group Angiotensin Converting
Enzyme (ACE) inhibitor:
Anti-hypertensive pills.
Diuretic: Water pill Corticosteroid
Mechanism of
action
This medication is used for
the treatment of high blood
pressure. It is falls under the
category of anti-hypertensive
It is a pharmacologic
antagonist of aldosterone,
a steroid hormone. It acts
as competitive inhibitor.
Long-acting bronchodilator
with a that is used to prevent
broncho-spasm in people with
COPD (Russell had COPD).
NURSING
of the anti-inflammatory inhibitors in the pulmonary cavities and thus hampering the oxygen
carrying capacity of the lungs and increasing exacerbation. Acute exacerbations are regarded
as one of the leading cause of hospitalization among the older adults leading to increased rate
of mortality and morbidity (Flattet et al., 2017). In the domain of exacerbation of the COPD,
Crisafulli, Barbeta, Ielpo and Torres (2018) have stated that smoking for a prolong period of
time, leads to the loss of elasticity of the pulmonary tissues along with damage of cilia of the
lungs and thus increasing the exacerbations further and increased need for hospitalization.
In case of Russell, the increase in the cellular infiltrate inside the pulmonary cavities
and resulting in the acute exacerbation of COPD is due to the previous habit of smoking.
Russell used to smoke 20 cigarettes per day when he was 18 years and he ceased cigarette
smoking after encountering the heart attack (15 years back). This prolong tendency of
cigarette smoking resulting in thick mucus deposition in the pulmonary cavities and the
generation of the inflammatory response increase the severity of the COPD. Exacerbations of
COPD is common among the male, and cigarette smoking in Russell have increased his
severity further (Ko et al., 2016).
Pharmacology
Generic name Perindopril Spironolactone Budesonide/Fomoterol
fumarate dehydrate puffs
Drug group Angiotensin Converting
Enzyme (ACE) inhibitor:
Anti-hypertensive pills.
Diuretic: Water pill Corticosteroid
Mechanism of
action
This medication is used for
the treatment of high blood
pressure. It is falls under the
category of anti-hypertensive
It is a pharmacologic
antagonist of aldosterone,
a steroid hormone. It acts
as competitive inhibitor.
Long-acting bronchodilator
with a that is used to prevent
broncho-spasm in people with
COPD (Russell had COPD).
5
NURSING
pills. It is also used for the
prevention of heart attack.
ACE inhibitors inhibits the
formation fo angiotensin II
from angiotensin I under the
action of renin, a proteolytic
enzyme. Angiotensin acts as a
vaso-constrictor that promote
contraction of the smooth
muscles. Under the absence
of angiotensin II, there occurs
relaxation of the cardiac
muscles thus helping to
reduce the heart rate and
blood pressure.
It promotes competitive
binding of receptors
located at the
aldosterone-dependent
sodium potassium
exchange sites of the
distal convoluted renal
tubule of the pair of
kidneys. The medication
helps release additional
fluid through urine and
helping to reduce the
unwanted water retention
of the body. This
medication is given to
Russell in order to reduce
the peripheral water
retention at the
extremities of the leg like
feet and ankles
Dilatation of the bronchial
muscles helps in the relaxation
of the pulmonary arteries. This
help in the reduction of
shortness of breath and easy
relaxation of the pulmonary
vesicles and thus helping to
reduce the difficulty of
breathing and dyspenea. Russell
has lately suffering from
shortness of breath (for the past
three months) and this was
relieved only upon using three
pillows
Complications 1. ACE inhibitor causes
retention of potassium by
increase the re-uptake of
potassium from the distal
collecting tubule. This
hampers the sodim-potassium
balance of the body and
increase in the overall
1. The medication is
potentially fatal when
taken in association with
ACE inhibitor (anti-
hypertensive drug). This
combination of thee two
contradictory drug causes
1. Problem in sleeping due to
sudden feeling of anxiety and
the condition is more prevalent
in supine position that is why
Russell was feeling comfortable
over three pillows.
2. Increase in the rate of heart
beat arising out of dilation of
NURSING
pills. It is also used for the
prevention of heart attack.
ACE inhibitors inhibits the
formation fo angiotensin II
from angiotensin I under the
action of renin, a proteolytic
enzyme. Angiotensin acts as a
vaso-constrictor that promote
contraction of the smooth
muscles. Under the absence
of angiotensin II, there occurs
relaxation of the cardiac
muscles thus helping to
reduce the heart rate and
blood pressure.
It promotes competitive
binding of receptors
located at the
aldosterone-dependent
sodium potassium
exchange sites of the
distal convoluted renal
tubule of the pair of
kidneys. The medication
helps release additional
fluid through urine and
helping to reduce the
unwanted water retention
of the body. This
medication is given to
Russell in order to reduce
the peripheral water
retention at the
extremities of the leg like
feet and ankles
Dilatation of the bronchial
muscles helps in the relaxation
of the pulmonary arteries. This
help in the reduction of
shortness of breath and easy
relaxation of the pulmonary
vesicles and thus helping to
reduce the difficulty of
breathing and dyspenea. Russell
has lately suffering from
shortness of breath (for the past
three months) and this was
relieved only upon using three
pillows
Complications 1. ACE inhibitor causes
retention of potassium by
increase the re-uptake of
potassium from the distal
collecting tubule. This
hampers the sodim-potassium
balance of the body and
increase in the overall
1. The medication is
potentially fatal when
taken in association with
ACE inhibitor (anti-
hypertensive drug). This
combination of thee two
contradictory drug causes
1. Problem in sleeping due to
sudden feeling of anxiety and
the condition is more prevalent
in supine position that is why
Russell was feeling comfortable
over three pillows.
2. Increase in the rate of heart
beat arising out of dilation of
6
NURSING
potassium concentration of
the body (hyperkalemia).
However, the potassium level
of Russell is within the
normal range
2. Swelling of hand and feet
is second major
complications of this
medication causing oedema.
The signs of oedema is
evident in Russell in both legs
renal impairment.
2. Vomiting, diarrhea and
stomach pain are second
major complication of
this medication leading to
the degeneration of
dehydration
the smooth bronchial muscles
and thus increasing the rate of
blood pressure further
Nursing
consideration
1. Proper regulation of salt
content in the diet
2. Checking the blood
pressure periodically to avoid
the chances of hypotension
1. Development of
fatigue and nausea
2. Monitoring of urine
output to prevent
dehydration
1. Frequent checking of the
respiratory rate
2. Frequent checking of the
oxygen saturation of the body
in order to avoid the chances of
hypoxia with the help of the
pulse oxymetry
(Source: Rosenjack & Burcham, 2016; Tiziani, 2017)
Non-pharmacological interventions
q. Heart failure: The non-pharmacological intervention for the management of heart failure
includes frequent checking of the blood pressure, pulse rate and respiratory rate. The
estimation of this vital statistics will help in ascertaining the condition of the heart and
indicating any chances of alarming situation. The checking of the vital signs must be done
once per week with the help of the pulse oxymetry and the regulation of the dosage of the
NURSING
potassium concentration of
the body (hyperkalemia).
However, the potassium level
of Russell is within the
normal range
2. Swelling of hand and feet
is second major
complications of this
medication causing oedema.
The signs of oedema is
evident in Russell in both legs
renal impairment.
2. Vomiting, diarrhea and
stomach pain are second
major complication of
this medication leading to
the degeneration of
dehydration
the smooth bronchial muscles
and thus increasing the rate of
blood pressure further
Nursing
consideration
1. Proper regulation of salt
content in the diet
2. Checking the blood
pressure periodically to avoid
the chances of hypotension
1. Development of
fatigue and nausea
2. Monitoring of urine
output to prevent
dehydration
1. Frequent checking of the
respiratory rate
2. Frequent checking of the
oxygen saturation of the body
in order to avoid the chances of
hypoxia with the help of the
pulse oxymetry
(Source: Rosenjack & Burcham, 2016; Tiziani, 2017)
Non-pharmacological interventions
q. Heart failure: The non-pharmacological intervention for the management of heart failure
includes frequent checking of the blood pressure, pulse rate and respiratory rate. The
estimation of this vital statistics will help in ascertaining the condition of the heart and
indicating any chances of alarming situation. The checking of the vital signs must be done
once per week with the help of the pulse oxymetry and the regulation of the dosage of the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
NURSING
anti-hypertensive drugs must be done according to the level of blood pressure. The regulation
of the drug dosage must be done under the supervision of physicians (Ingles, 2019)
b. To prevent exacerbation of COPD: The prevention of the COPD exacerbation under the
non-pharmacological intervention includes cessation of smoking. However, Russell has quit
smoking. In such cases, the main nursing intervention includes conduction of yoga during
every morning in order to ooze out the sputum from the pulmonary cavity formed as a result
of mucus deposition (Kupershmidt & Barnable, 2019)
c. To prevent pneumonia: The main nursing intervention for the prevention of pneumonia is
regular conduction of the mild to moderate physical activity during early in the morning. This
will help to maintain proper aeration and blood circulation in the lungs and thus decreasing
the chances of developing pneumonia. The increase in the rate of physical activity also helps
in increasing the level of immunity and thereby decreasing the chance of developing
pneumonia (Kupershmidt & Barnable, 2019)
d. To reduce the level of cholesterol: The non-pharmacological intervention for the reduction
of cholesterol includes decrease in the intake of the high cholesterol food. Low density
lipoprotein (LDL) is regarded as bad cholesterol as it carries cholesterol to the tissues and
arteries. The cholesterol in the blood is present in the LDL form and thus higher
concentration of LDL in blood, higher risk of heart disease. High density lipo-protein (HDL)
is regarded as good cholesterol as it cholesterol from the tissues to the live and the liver in
chance moves the cholesterol out of the body. The nutrients in diet that increase the level
cholesterol in body is saturated fat (found in animals) and trans fat (hydrogenated oils and
fats). Thus reduction in the intake of saturated fat and trans fat in diet along with the
reduction of alcohol helps to reduce the level of LDL in blood. The regulation of diet plan for
Russell must be under the supervision of trained dietician (Di Ciaula et al., 2019).
NURSING
anti-hypertensive drugs must be done according to the level of blood pressure. The regulation
of the drug dosage must be done under the supervision of physicians (Ingles, 2019)
b. To prevent exacerbation of COPD: The prevention of the COPD exacerbation under the
non-pharmacological intervention includes cessation of smoking. However, Russell has quit
smoking. In such cases, the main nursing intervention includes conduction of yoga during
every morning in order to ooze out the sputum from the pulmonary cavity formed as a result
of mucus deposition (Kupershmidt & Barnable, 2019)
c. To prevent pneumonia: The main nursing intervention for the prevention of pneumonia is
regular conduction of the mild to moderate physical activity during early in the morning. This
will help to maintain proper aeration and blood circulation in the lungs and thus decreasing
the chances of developing pneumonia. The increase in the rate of physical activity also helps
in increasing the level of immunity and thereby decreasing the chance of developing
pneumonia (Kupershmidt & Barnable, 2019)
d. To reduce the level of cholesterol: The non-pharmacological intervention for the reduction
of cholesterol includes decrease in the intake of the high cholesterol food. Low density
lipoprotein (LDL) is regarded as bad cholesterol as it carries cholesterol to the tissues and
arteries. The cholesterol in the blood is present in the LDL form and thus higher
concentration of LDL in blood, higher risk of heart disease. High density lipo-protein (HDL)
is regarded as good cholesterol as it cholesterol from the tissues to the live and the liver in
chance moves the cholesterol out of the body. The nutrients in diet that increase the level
cholesterol in body is saturated fat (found in animals) and trans fat (hydrogenated oils and
fats). Thus reduction in the intake of saturated fat and trans fat in diet along with the
reduction of alcohol helps to reduce the level of LDL in blood. The regulation of diet plan for
Russell must be under the supervision of trained dietician (Di Ciaula et al., 2019).
8
NURSING
Conclusion
Thus from the above discussion, it can be concluded that, in case of Russell, the main
reason behind the development of the heart attack is prolong pre-disposition of COPD along
with long-term unhealthy lifestyle habit of smoking. Russell had encountered left sided heart
failure as indicated by the echocardiogram and the x-ray report. The X-ray report also
indicated the presence of pulmonary oedema. Pulmonary oedema is a indication of acute
exacerbation of the COPD leading to lung congestion from the mucous deposition. The
medication management of COPD mainly directed towards reducing hypertension, renal
management and management of shortness of breath. The main nursing interventions (non-
pharmacological interventions) will be directed towards the management of heart failure,
prevent exacerbation of COPD, pneumonia, and management of high level of cholesterol.
NURSING
Conclusion
Thus from the above discussion, it can be concluded that, in case of Russell, the main
reason behind the development of the heart attack is prolong pre-disposition of COPD along
with long-term unhealthy lifestyle habit of smoking. Russell had encountered left sided heart
failure as indicated by the echocardiogram and the x-ray report. The X-ray report also
indicated the presence of pulmonary oedema. Pulmonary oedema is a indication of acute
exacerbation of the COPD leading to lung congestion from the mucous deposition. The
medication management of COPD mainly directed towards reducing hypertension, renal
management and management of shortness of breath. The main nursing interventions (non-
pharmacological interventions) will be directed towards the management of heart failure,
prevent exacerbation of COPD, pneumonia, and management of high level of cholesterol.
9
NURSING
References
American Heart Association. (2019). Types of Heart Failure. Access date: 27th March 2020.
Retrieved from: https://www.heart.org/en/health-topics/heart-failure/what-is-heart-
failure/types-of-heart-failure
Bayrak, D., & Tosun, N. (2018). Determination of nursing activities for prevention of heart
attack and stroke in hypertension patients. International Journal of Caring
Sciences, 11(2), 1073.
https://www.researchgate.net/profile/Damla_Bayrak/publication/328957303_Determi
nation_of_Nursing_Activities_For_Prevention_of_Heart_Attack_and_Stroke_in_Hyp
ertension_Patients/links/5bed561992851c6b27c041ae/Determination-of-Nursing-
Activities-For-Prevention-of-Heart-Attack-and-Stroke-in-Hypertension-Patients.pdf
Bosch, L., Lam, C. S., Gong, L., Chan, S. P., Sim, D., Yeo, D., ... & Richards, A. M. (2017).
Right ventricular dysfunction in left‐sided heart failure with preserved versus reduced
ejection fraction. European journal of heart failure, 19(12), 1664-1671.
https://doi.org/10.1002/ejhf.873
Craft, J.A. & Gordon, C.J. (2019). Understanding Pathophysiology 3rd Edition (Australia
and New Zealand).Elsevier . ISBN: 1978-0-323-35409-7
Crisafulli, E., Barbeta, E., Ielpo, A., & Torres, A. (2018). Management of severe acute
exacerbations of COPD: an updated narrative review. Multidisciplinary respiratory
medicine, 13(1), 36. https://doi.org/10.1186/s40248-018-0149-0
Di Ciaula, A., Garruti, G., Frühbeck, G., De Angelis, M., De Bari, O., Wang, D. Q. H., ... &
Portincasa, P. (2019). The role of diet in the pathogenesis of cholesterol
NURSING
References
American Heart Association. (2019). Types of Heart Failure. Access date: 27th March 2020.
Retrieved from: https://www.heart.org/en/health-topics/heart-failure/what-is-heart-
failure/types-of-heart-failure
Bayrak, D., & Tosun, N. (2018). Determination of nursing activities for prevention of heart
attack and stroke in hypertension patients. International Journal of Caring
Sciences, 11(2), 1073.
https://www.researchgate.net/profile/Damla_Bayrak/publication/328957303_Determi
nation_of_Nursing_Activities_For_Prevention_of_Heart_Attack_and_Stroke_in_Hyp
ertension_Patients/links/5bed561992851c6b27c041ae/Determination-of-Nursing-
Activities-For-Prevention-of-Heart-Attack-and-Stroke-in-Hypertension-Patients.pdf
Bosch, L., Lam, C. S., Gong, L., Chan, S. P., Sim, D., Yeo, D., ... & Richards, A. M. (2017).
Right ventricular dysfunction in left‐sided heart failure with preserved versus reduced
ejection fraction. European journal of heart failure, 19(12), 1664-1671.
https://doi.org/10.1002/ejhf.873
Craft, J.A. & Gordon, C.J. (2019). Understanding Pathophysiology 3rd Edition (Australia
and New Zealand).Elsevier . ISBN: 1978-0-323-35409-7
Crisafulli, E., Barbeta, E., Ielpo, A., & Torres, A. (2018). Management of severe acute
exacerbations of COPD: an updated narrative review. Multidisciplinary respiratory
medicine, 13(1), 36. https://doi.org/10.1186/s40248-018-0149-0
Di Ciaula, A., Garruti, G., Frühbeck, G., De Angelis, M., De Bari, O., Wang, D. Q. H., ... &
Portincasa, P. (2019). The role of diet in the pathogenesis of cholesterol
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10
NURSING
gallstones. Current medicinal chemistry, 26(19), 3620-3638.
DOI: https://doi.org/10.2174/0929867324666170530080636
Fatima, Z., Naqvi, I. B., & Hanook, S. (2019). A Statistical Study to Identify the Risk Factors
of Heart Attack. J Biom Biostat, 10(430), 2. https://www.hilarispublisher.com/open-
access/a-statistical-study-to-identify-the-risk-factors-of-heart-attack.pdf
Flattet, Y., Garin, N., Serratrice, J., Perrier, A., Stirnemann, J., & Carballo, S. (2017).
Determining prognosis in acute exacerbation of COPD. International journal of
chronic obstructive pulmonary disease, 12, 467. doi: 10.2147/COPD.S122382
Ingles, A. (2019). Heart Failure (HF) Nurse Navigator Program Interventions Decrease HF
Readmission Rates. https://digitalcommons.psjhealth.org/cgi/viewcontent.cgi?
article=1012&context=sjo-ebp
Ko, F. W., Chan, K. P., Hui, D. S., Goddard, J. R., Shaw, J. G., Reid, D. W., & Yang, I. A.
(2016). Acute exacerbation of COPD. Respirology, 21(7), 1152-1165.
https://doi.org/10.1111/resp.12780
Kupershmidt, S., & Barnable, T. (2019). Definition of a Yoga Breathing (Pranayama)
Protocol That Improves Lung Function. Holistic nursing practice, 33(4), 197-203.
doi: 10.1097/HNP.0000000000000331
Rosenjack, R. & Burcham, L.D. (2016). Lehne`s Pharmacology for Nursing Care (10th Ed).
Elsevier Saunders.ISBN: 978-0-323-32190-7
Tiziani, A. (2017). Harvard`s Nursing Guide to Drugs (10th edition). Elsevier Australia.
ISBN: 9780729542548
NURSING
gallstones. Current medicinal chemistry, 26(19), 3620-3638.
DOI: https://doi.org/10.2174/0929867324666170530080636
Fatima, Z., Naqvi, I. B., & Hanook, S. (2019). A Statistical Study to Identify the Risk Factors
of Heart Attack. J Biom Biostat, 10(430), 2. https://www.hilarispublisher.com/open-
access/a-statistical-study-to-identify-the-risk-factors-of-heart-attack.pdf
Flattet, Y., Garin, N., Serratrice, J., Perrier, A., Stirnemann, J., & Carballo, S. (2017).
Determining prognosis in acute exacerbation of COPD. International journal of
chronic obstructive pulmonary disease, 12, 467. doi: 10.2147/COPD.S122382
Ingles, A. (2019). Heart Failure (HF) Nurse Navigator Program Interventions Decrease HF
Readmission Rates. https://digitalcommons.psjhealth.org/cgi/viewcontent.cgi?
article=1012&context=sjo-ebp
Ko, F. W., Chan, K. P., Hui, D. S., Goddard, J. R., Shaw, J. G., Reid, D. W., & Yang, I. A.
(2016). Acute exacerbation of COPD. Respirology, 21(7), 1152-1165.
https://doi.org/10.1111/resp.12780
Kupershmidt, S., & Barnable, T. (2019). Definition of a Yoga Breathing (Pranayama)
Protocol That Improves Lung Function. Holistic nursing practice, 33(4), 197-203.
doi: 10.1097/HNP.0000000000000331
Rosenjack, R. & Burcham, L.D. (2016). Lehne`s Pharmacology for Nursing Care (10th Ed).
Elsevier Saunders.ISBN: 978-0-323-32190-7
Tiziani, A. (2017). Harvard`s Nursing Guide to Drugs (10th edition). Elsevier Australia.
ISBN: 9780729542548
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





