Cardiometabolic Risk Factors and Obesity Severity in Young Individuals
VerifiedAdded on 2023/06/11
|11
|8718
|436
Essay
AI Summary
This study investigates the correlation between the severity of obesity and cardiometabolic risk factors in children and young adults using data from the National Health and Nutrition Examination Survey (NHANES) from 1999 to 2012. The research categorizes weight status based on BMI percentiles and analyzes the prevalence of abnormal values for total cholesterol, HDL cholesterol, LDL cholesterol, triglycerides, blood pressure, glycated hemoglobin, and fasting glucose. The findings indicate that increased obesity severity is associated with higher risks of low HDL cholesterol, elevated blood pressure, and increased triglyceride and glycated hemoglobin levels, particularly in boys and young men, emphasizing the need for targeted interventions to address cardiometabolic health in severely obese youth. Desklib offers a range of study tools and resources for students.
T h en e w e ngl a nd j o u r na lo f m e dic i n e
n engl j med 373;14nejm.org October 1, 2015 1307
From the Department of Pediatrics, Divi-
sion of General Pediatrics and Adolescent
Medicine, School of Medicine (A.C.S.,
E.M.P.), Department of Health Policy and
Management, Gillings School of Global
Public Health (A.C.S.), and Injury Preven-
tion Research Center (L.A.M.), University
of North Carolina at Chapel Hill, Chapel
Hill, and the Department of Pediatrics,
Wake Forest School of Medicine, and
Brenner FIT (Families in Training), Brenner
Children’s Hospital, Winston-Salem (J.A.S.)
— all in North Carolina. Address reprint
requests to Dr. Skinner at the Depart-
ment of Pediatrics, University of North
Carolina at Chapel Hill School of Medi-
cine, 231 MacNider, 229B, CB 7225, Chape
Hill, NC 27599, or at asheley@ unc . edu.
N Engl J Med 2015;373:1307-17.
DOI: 10.1056/NEJMoa1502821
Copyright © 2015 Massachusetts Medical Society.
BACKGROUND
The prevalence of severe obesity among children and young adults has increased
over the past decade. Although the prevalence of cardiometabolic risk factors is
relatively low among children and young adults who are overweight or obese, those
with more severe forms of obesity may be at greater risk.
METHODS
We performed a cross-sectional analysis of data from overweight or obese children
and young adults 3 to 19 years of age who were included in the National Health
and Nutrition Examination Survey from 1999 through 2012 to assess the preva-
lence of multiple cardiometabolic risk factors according to the severity of obesity.
Weight status was classified on the basis of measured height and weight. We used
standard definitions of abnormal values for total cholesterol, high-density lipopro-
tein (HDL) cholesterol, low-density lipoprotein cholesterol, triglycerides, blood
pressure, glycated hemoglobin, and fasting glucose and report the prevalence of
abnormal values in children and young adults according to weight status.
RESULTS
Among 8579 children and young adults with a body-mass index at the 85th per-
centile or higher (according to the Centers for Disease Control and Prevention
growth charts), 46.9% were overweight, 36.4% had class I obesity, 11.9% had class II
obesity, and 4.8% had class III obesity. Mean values for some, but not all, cardio-
metabolic variables were higher with greater severity of obesity in both male and
female participants, and the values were higher in male participants than in female
participants; for HDL cholesterol, the mean values were lower with greater sever-
ity of obesity. Multivariable models that controlled for age, race or ethnic group,
and sex showed that the greater the severity of obesity, the higher the risks of a
low HDL cholesterol level, high systolic and diastolic blood pressures, and high
triglyceride and glycated hemoglobin levels.
CONCLUSIONS
Severe obesity in children and young adults was associated with an increased
prevalence of cardiometabolic risk factors, particularly among boys and young men.
A BS TR AC T
Cardiometabolic Risks and Severity
of Obesity in Children and Young Adults
Asheley C. Skinner, Ph.D., Eliana M. Perrin, M.D., M.P.H.,
Leslie A. Moss, M.H.A., C.H.E.S., and Joseph A. Skelton, M.D.
Original Article
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
n engl j med 373;14nejm.org October 1, 2015 1307
From the Department of Pediatrics, Divi-
sion of General Pediatrics and Adolescent
Medicine, School of Medicine (A.C.S.,
E.M.P.), Department of Health Policy and
Management, Gillings School of Global
Public Health (A.C.S.), and Injury Preven-
tion Research Center (L.A.M.), University
of North Carolina at Chapel Hill, Chapel
Hill, and the Department of Pediatrics,
Wake Forest School of Medicine, and
Brenner FIT (Families in Training), Brenner
Children’s Hospital, Winston-Salem (J.A.S.)
— all in North Carolina. Address reprint
requests to Dr. Skinner at the Depart-
ment of Pediatrics, University of North
Carolina at Chapel Hill School of Medi-
cine, 231 MacNider, 229B, CB 7225, Chape
Hill, NC 27599, or at asheley@ unc . edu.
N Engl J Med 2015;373:1307-17.
DOI: 10.1056/NEJMoa1502821
Copyright © 2015 Massachusetts Medical Society.
BACKGROUND
The prevalence of severe obesity among children and young adults has increased
over the past decade. Although the prevalence of cardiometabolic risk factors is
relatively low among children and young adults who are overweight or obese, those
with more severe forms of obesity may be at greater risk.
METHODS
We performed a cross-sectional analysis of data from overweight or obese children
and young adults 3 to 19 years of age who were included in the National Health
and Nutrition Examination Survey from 1999 through 2012 to assess the preva-
lence of multiple cardiometabolic risk factors according to the severity of obesity.
Weight status was classified on the basis of measured height and weight. We used
standard definitions of abnormal values for total cholesterol, high-density lipopro-
tein (HDL) cholesterol, low-density lipoprotein cholesterol, triglycerides, blood
pressure, glycated hemoglobin, and fasting glucose and report the prevalence of
abnormal values in children and young adults according to weight status.
RESULTS
Among 8579 children and young adults with a body-mass index at the 85th per-
centile or higher (according to the Centers for Disease Control and Prevention
growth charts), 46.9% were overweight, 36.4% had class I obesity, 11.9% had class II
obesity, and 4.8% had class III obesity. Mean values for some, but not all, cardio-
metabolic variables were higher with greater severity of obesity in both male and
female participants, and the values were higher in male participants than in female
participants; for HDL cholesterol, the mean values were lower with greater sever-
ity of obesity. Multivariable models that controlled for age, race or ethnic group,
and sex showed that the greater the severity of obesity, the higher the risks of a
low HDL cholesterol level, high systolic and diastolic blood pressures, and high
triglyceride and glycated hemoglobin levels.
CONCLUSIONS
Severe obesity in children and young adults was associated with an increased
prevalence of cardiometabolic risk factors, particularly among boys and young men.
A BS TR AC T
Cardiometabolic Risks and Severity
of Obesity in Children and Young Adults
Asheley C. Skinner, Ph.D., Eliana M. Perrin, M.D., M.P.H.,
Leslie A. Moss, M.H.A., C.H.E.S., and Joseph A. Skelton, M.D.
Original Article
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
n engl j med 373;14nejm.org October 1, 20151308
T h en e w e ngl a nd j o u r na lo f m e dic i n e
The prevalence of severe obesity
among children and young adults has in-
creased in recent years1 and has led to a
heightened awareness and concern about the
cardiovascular and metabolic health of persons
in this age group. In 1999–2004, almost 4% of
children and young adults in the United States
2 to 19 years of age were classified as having
severe obesity,2 and as recently as 2011–2012, the
prevalence of severe obesity increased to approxi-
mately 6% in this age group1; however, the preva-
lence of cardiometabolic risk factors accompa-
nying severe obesity in these children and young
adults is unclear.
Cardiometabolic risk factors are more preva-
lent among overweight or obese children and
young adults than among those of healthy
weight.3 However, the use of only a single cate-
gory for obesity does not take into account the
varying severity of obesity. The American Heart
Association identified several relatively small
studies that showed that more severe forms of
obesity were associated with a greater immedi-
ate risk of complications related to weight, includ-
ing abnormal lipid and blood glucose levels and
increased blood-pressure levels4; however, various
definitions of severe obesity were used in these
studies. Clearer guidelines now exist to define
severe obesity as 120% of the 95th percentile for
body-mass index (BMI, the weight in kilograms
divided by the square of the height in meters)
and to define markedly severe obesity as 140%
of the 95th percentile.1,4 As children approach
adulthood, these high percentile curves approxi-
mate a BMI of at least 35 for severe obesity (class
II obesity) and a BMI of at least 40 for markedly
severe obesity (class III obesity).1 To improve the
understanding of the distribution of cardiometa-
bolic risk factors, we examined the prevalence of
multiple cardiometabolic risk factors according
to the severity of obesity using nationally repre-
sentative data.
Methods
Data Source and Study Design
We obtained data from the National Health and
Nutrition Examination Survey (NHANES, 1999–
2012). The NHANES includes a stratified, multi-
stage probability sample of the civilian, non-
institutionalizedU.S. population.The data
obtained included responses to an in-home in-
terview on a variety of demographic variables and
health topics, findings from a physical examina-
tion performed at a mobile examination center
that included measured height and weight, and
laboratory measurements.5 The National Cen-
ter for Health Statistics (NCHS) designed the
NHANES and collected the data after obtaining
written informed consent from the participants
or their parents or guardians and assent from
minors; most components of the NHANES, in-
cluding those used in the current study, are pub-
licly available. The first author designed and
performed the analyses, with no input from the
NCHS, and assumes responsibility for the analy-
ses. The institutional review board at the Univer-
sity of North Carolina at Chapel Hill, in accor-
dance with the Code of Federal Regulations,
deemed this study to be exempt from further re-
view and from the requirement to obtain written
informed consent because it used only deidentified
secondary data.
Study Sample
Our study sample included NHANES participants
who were 3 to 19 years of age at the time of
examination. We excluded 513 children and young
adults with missing BMI values. Given our focus
on obesity, we excluded 807 participants who were
underweight and 15,469 participants who had a
healthy weight (i.e., all participants who were
below the 85th percentile for age-specific and
sex-specific BMI, as defined below). Thus, the fi-
nal sample comprised 8579 children and young
adults. Because certain NHANES measures have
a more targeted sampling frame (e.g., limited to
specific ages), specific reported measures had
different sample sizes (Table 1).5
Weight Status
We classified weight status using height and
weight measurements obtained at the time of
the physicalexaminationcomponentof the
NHANES to calculate BMI and to determine the
BMI percentile, which we derived from the Cen-
ters for Disease Control and Prevention (CDC)
growth charts using the SAS code that was
developed for this purpose.6 In 2011–2012, the
NHANES reported age in years for children and
young adults 2 to 19 years of age, rather than
age in months as in previous releases; age in
months was reported only for children from
birth to 2 years of age. To estimate the preva-
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
T h en e w e ngl a nd j o u r na lo f m e dic i n e
The prevalence of severe obesity
among children and young adults has in-
creased in recent years1 and has led to a
heightened awareness and concern about the
cardiovascular and metabolic health of persons
in this age group. In 1999–2004, almost 4% of
children and young adults in the United States
2 to 19 years of age were classified as having
severe obesity,2 and as recently as 2011–2012, the
prevalence of severe obesity increased to approxi-
mately 6% in this age group1; however, the preva-
lence of cardiometabolic risk factors accompa-
nying severe obesity in these children and young
adults is unclear.
Cardiometabolic risk factors are more preva-
lent among overweight or obese children and
young adults than among those of healthy
weight.3 However, the use of only a single cate-
gory for obesity does not take into account the
varying severity of obesity. The American Heart
Association identified several relatively small
studies that showed that more severe forms of
obesity were associated with a greater immedi-
ate risk of complications related to weight, includ-
ing abnormal lipid and blood glucose levels and
increased blood-pressure levels4; however, various
definitions of severe obesity were used in these
studies. Clearer guidelines now exist to define
severe obesity as 120% of the 95th percentile for
body-mass index (BMI, the weight in kilograms
divided by the square of the height in meters)
and to define markedly severe obesity as 140%
of the 95th percentile.1,4 As children approach
adulthood, these high percentile curves approxi-
mate a BMI of at least 35 for severe obesity (class
II obesity) and a BMI of at least 40 for markedly
severe obesity (class III obesity).1 To improve the
understanding of the distribution of cardiometa-
bolic risk factors, we examined the prevalence of
multiple cardiometabolic risk factors according
to the severity of obesity using nationally repre-
sentative data.
Methods
Data Source and Study Design
We obtained data from the National Health and
Nutrition Examination Survey (NHANES, 1999–
2012). The NHANES includes a stratified, multi-
stage probability sample of the civilian, non-
institutionalizedU.S. population.The data
obtained included responses to an in-home in-
terview on a variety of demographic variables and
health topics, findings from a physical examina-
tion performed at a mobile examination center
that included measured height and weight, and
laboratory measurements.5 The National Cen-
ter for Health Statistics (NCHS) designed the
NHANES and collected the data after obtaining
written informed consent from the participants
or their parents or guardians and assent from
minors; most components of the NHANES, in-
cluding those used in the current study, are pub-
licly available. The first author designed and
performed the analyses, with no input from the
NCHS, and assumes responsibility for the analy-
ses. The institutional review board at the Univer-
sity of North Carolina at Chapel Hill, in accor-
dance with the Code of Federal Regulations,
deemed this study to be exempt from further re-
view and from the requirement to obtain written
informed consent because it used only deidentified
secondary data.
Study Sample
Our study sample included NHANES participants
who were 3 to 19 years of age at the time of
examination. We excluded 513 children and young
adults with missing BMI values. Given our focus
on obesity, we excluded 807 participants who were
underweight and 15,469 participants who had a
healthy weight (i.e., all participants who were
below the 85th percentile for age-specific and
sex-specific BMI, as defined below). Thus, the fi-
nal sample comprised 8579 children and young
adults. Because certain NHANES measures have
a more targeted sampling frame (e.g., limited to
specific ages), specific reported measures had
different sample sizes (Table 1).5
Weight Status
We classified weight status using height and
weight measurements obtained at the time of
the physicalexaminationcomponentof the
NHANES to calculate BMI and to determine the
BMI percentile, which we derived from the Cen-
ters for Disease Control and Prevention (CDC)
growth charts using the SAS code that was
developed for this purpose.6 In 2011–2012, the
NHANES reported age in years for children and
young adults 2 to 19 years of age, rather than
age in months as in previous releases; age in
months was reported only for children from
birth to 2 years of age. To estimate the preva-
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
n engl j med 373;14nejm.org October 1, 2015 1309
Cardiometabolic Risks and Obesity Severity in Children
lence of obesity consistently across our study
period, we used the midpoints of the whole-year
ages of the children in all calculations (e.g., an
11-year-old child was considered to be 11.5 years
of age). This method of calculation yielded
prevalence rates that were similar to calculations
based on age in months, with differences of 0.1
to 0.2 percentage points,1 and was used for all
2-year cycles of the NHANES to ensure consis-
tency in the determinations of weight status.
The weight categories according to age-spe-
cific and sex-specific BMI percentiles that we
used in the current study were as follows: over-
weight (≥85th to <95th percentile), class I obe-
sity (≥95th percentile to <120% of the 95th per-
centile), class II obesity (≥120% to <140% of the
95th percentile, or BMI ≥35, whichever was
lower), and class III obesity (≥140% of the 95th
percentile, or BMI ≥40, whichever was lower).
The definitions of healthy weight, overweight,
and obesity were based on the recommendations
of the CDC,7 and the definition of class II obe-
sity was based on the recommendation of the
American Heart Association.4 We used the range
of 120% to less than 140% of the 95th percentile
to define class II obesity instead of the 99th
percentile or higher because the former defini-
tion has been shown to have more stability in
estimation procedures.8 We used 140% of the
95th percentile to define class III obesity be-
cause it approximated a BMI of 40 in late adoles-
cence, the same age at which 120% of the 95th
percentile approximated a BMI of 35.1 Among
adults, persons with these ranges of BMI are
considered to be at a higher risk for earlier
death.9 The BMI percentiles in our study were
not derived from the study sample we evaluated
but were defined by the CDC growth charts that
used a historical sample; this allowed for a con-
sistent categorization of weight status through-
out the entire study sample.
Cardiometabolic Risk Factors
Because we evaluated children and young adults,
we examined variables that are associated with
known cardiometabolic risk rather than hard end
points of cardiovascular events. Total cholesterol
and high-density lipoprotein (HDL) cholesterol
levels were measured in the full study sample in
the targeted age ranges, whereas measurements
of low-density lipoprotein (LDL) cholesterol and
triglyceride levels were limited to a subgroup of
participants who underwent an examination in
the morning as part of the NHANES study pro-
cedures. Fasting times varied among partici-
pants in whom fasting laboratory studies were
performed. We used standard cutoff values for
levels of total cholesterol (≥200 mg per deciliter
[>5.18 mmol per liter]), HDL cholesterol (<35 mg
per deciliter [<0.9 mmol per liter]), LDL choles-
terol (≥130 mg per deciliter [≥3.4 mmol per
liter]), and triglycerides (≥150 mg per deciliter
[>1.7 mmol per liter]) to define abnormal values;
when the recommendations for cutoff values
were inconsistent, we chose the more conserva-
tive definition.10-12
Blood pressure was recorded as the mean
value of up to three measurements or as a single
measurement (86% of the children and young
adults had three measurements, 8% had two, and
6% had one). For children younger than 18 years
of age, we used standardized blood pressure
tables in which abnormal values were deter-
mined according to age, sex, and height; abnor-
mal values were defined as any value that was in
at least the 95th percentile in those tables.13 For
young adults 18 and 19 years of age, we used
cutoffs of 140 mm Hg for systolic blood pressure
and 90 mm Hg for diastolic blood pressure.14
Glycated hemoglobin levels were measured in
all participants 12 years of age or older as part
of the standard NHANES laboratory measure-
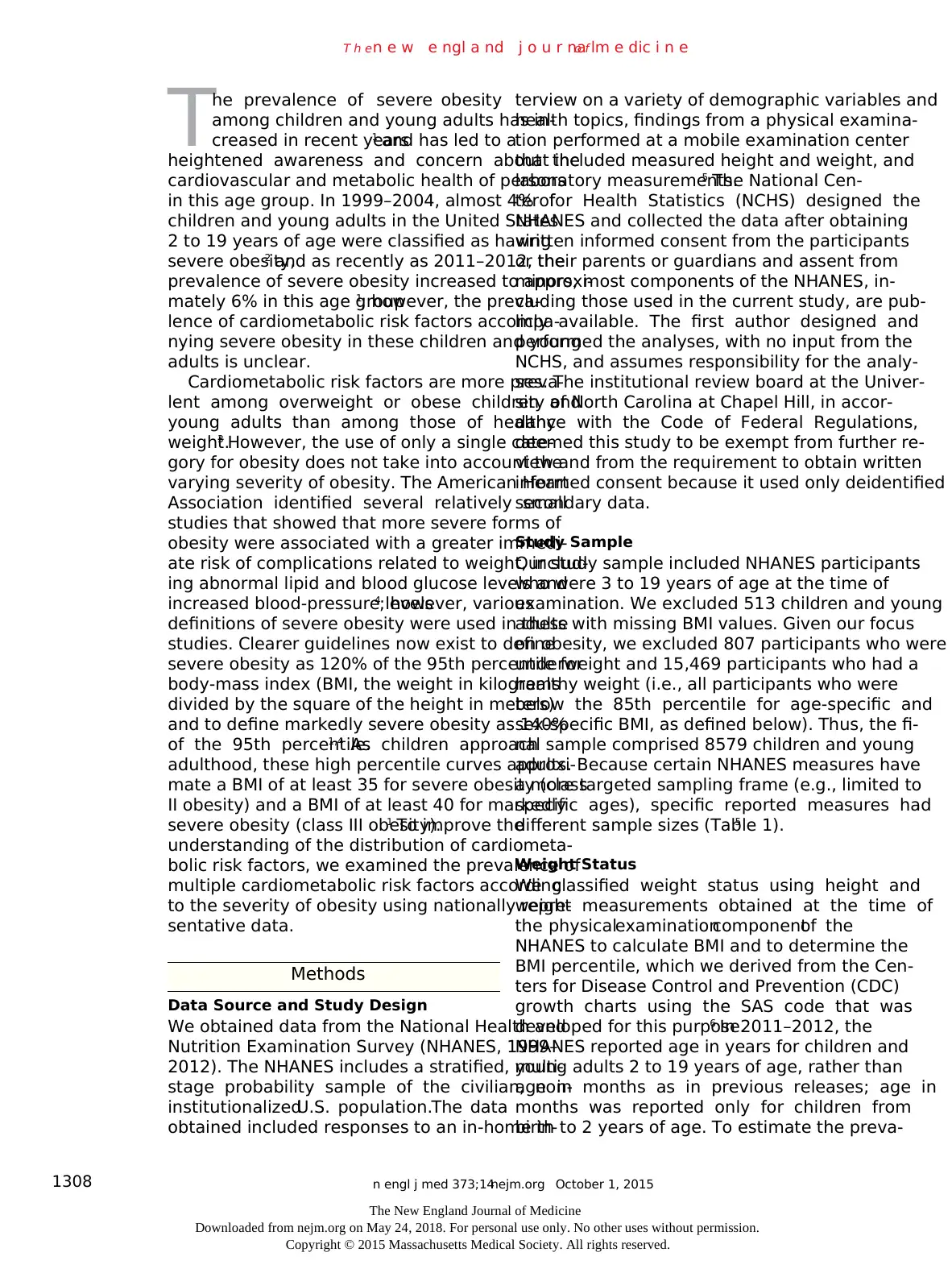
Variable Age Range
No. of
Participants
Evaluated
Definition of
Abnormal Value
yr
Total cholesterol 3–19 6876 ≥200 mg/dl
HDL cholesterol 3–19 6873 <35 mg/dl
Systolic BP 8–19 6412 ≥95th percentile
Diastolic BP 8–19 6412 ≥95th percentile
LDL cholesterol 3–19 2464 ≥130 mg/dl
Triglycerides 3–19 2537 ≥150 mg/dl
Glycated hemoglobin 12–19 4237 >5.7%
Glucose 12–19 1991 ≥100 mg/dl
* A total of 8579 children and young adults 3 to 19 years of age were eva
To convert the values for cholesterol to millimoles per liter, multiply by 0
To convert the values for triglycerides to millimoles per liter, multiply by
0.0113. To convert the values for glucose to millimoles per liter, multiply
0.0555. BP denotes blood pressure, HDL high-density lipoprotein, and LD
low-density lipoprotein.
Table 1. Definitions of Abnormal Values for Risk-Factor Variables
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
Cardiometabolic Risks and Obesity Severity in Children
lence of obesity consistently across our study
period, we used the midpoints of the whole-year
ages of the children in all calculations (e.g., an
11-year-old child was considered to be 11.5 years
of age). This method of calculation yielded
prevalence rates that were similar to calculations
based on age in months, with differences of 0.1
to 0.2 percentage points,1 and was used for all
2-year cycles of the NHANES to ensure consis-
tency in the determinations of weight status.
The weight categories according to age-spe-
cific and sex-specific BMI percentiles that we
used in the current study were as follows: over-
weight (≥85th to <95th percentile), class I obe-
sity (≥95th percentile to <120% of the 95th per-
centile), class II obesity (≥120% to <140% of the
95th percentile, or BMI ≥35, whichever was
lower), and class III obesity (≥140% of the 95th
percentile, or BMI ≥40, whichever was lower).
The definitions of healthy weight, overweight,
and obesity were based on the recommendations
of the CDC,7 and the definition of class II obe-
sity was based on the recommendation of the
American Heart Association.4 We used the range
of 120% to less than 140% of the 95th percentile
to define class II obesity instead of the 99th
percentile or higher because the former defini-
tion has been shown to have more stability in
estimation procedures.8 We used 140% of the
95th percentile to define class III obesity be-
cause it approximated a BMI of 40 in late adoles-
cence, the same age at which 120% of the 95th
percentile approximated a BMI of 35.1 Among
adults, persons with these ranges of BMI are
considered to be at a higher risk for earlier
death.9 The BMI percentiles in our study were
not derived from the study sample we evaluated
but were defined by the CDC growth charts that
used a historical sample; this allowed for a con-
sistent categorization of weight status through-
out the entire study sample.
Cardiometabolic Risk Factors
Because we evaluated children and young adults,
we examined variables that are associated with
known cardiometabolic risk rather than hard end
points of cardiovascular events. Total cholesterol
and high-density lipoprotein (HDL) cholesterol
levels were measured in the full study sample in
the targeted age ranges, whereas measurements
of low-density lipoprotein (LDL) cholesterol and
triglyceride levels were limited to a subgroup of
participants who underwent an examination in
the morning as part of the NHANES study pro-
cedures. Fasting times varied among partici-
pants in whom fasting laboratory studies were
performed. We used standard cutoff values for
levels of total cholesterol (≥200 mg per deciliter
[>5.18 mmol per liter]), HDL cholesterol (<35 mg
per deciliter [<0.9 mmol per liter]), LDL choles-
terol (≥130 mg per deciliter [≥3.4 mmol per
liter]), and triglycerides (≥150 mg per deciliter
[>1.7 mmol per liter]) to define abnormal values;
when the recommendations for cutoff values
were inconsistent, we chose the more conserva-
tive definition.10-12
Blood pressure was recorded as the mean
value of up to three measurements or as a single
measurement (86% of the children and young
adults had three measurements, 8% had two, and
6% had one). For children younger than 18 years
of age, we used standardized blood pressure
tables in which abnormal values were deter-
mined according to age, sex, and height; abnor-
mal values were defined as any value that was in
at least the 95th percentile in those tables.13 For
young adults 18 and 19 years of age, we used
cutoffs of 140 mm Hg for systolic blood pressure
and 90 mm Hg for diastolic blood pressure.14
Glycated hemoglobin levels were measured in
all participants 12 years of age or older as part
of the standard NHANES laboratory measure-
Variable Age Range
No. of
Participants
Evaluated
Definition of
Abnormal Value
yr
Total cholesterol 3–19 6876 ≥200 mg/dl
HDL cholesterol 3–19 6873 <35 mg/dl
Systolic BP 8–19 6412 ≥95th percentile
Diastolic BP 8–19 6412 ≥95th percentile
LDL cholesterol 3–19 2464 ≥130 mg/dl
Triglycerides 3–19 2537 ≥150 mg/dl
Glycated hemoglobin 12–19 4237 >5.7%
Glucose 12–19 1991 ≥100 mg/dl
* A total of 8579 children and young adults 3 to 19 years of age were eva
To convert the values for cholesterol to millimoles per liter, multiply by 0
To convert the values for triglycerides to millimoles per liter, multiply by
0.0113. To convert the values for glucose to millimoles per liter, multiply
0.0555. BP denotes blood pressure, HDL high-density lipoprotein, and LD
low-density lipoprotein.
Table 1. Definitions of Abnormal Values for Risk-Factor Variables
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
n engl j med 373;14nejm.org October 1, 20151310
T h en e w e ngl a nd j o u r na lo f m e dic i n e
ments; a value greater than 5.7% was defined as
abnormal. Fasting glucose was measured in the
subgroup of NHANES participants who attended
the morning session; a value of 100 mg per deci-
liter or higher (≥5.6 mmol per liter) was defined
as abnormal. The definitions of abnormal values
for glycated hemoglobin and fasting glucose
were based on recommendations by the Ameri-
can Diabetes Association for identifying persons
at high risk for diabetes.15
Detailed information about the collection and
measurement procedures of the NHANES can be
found in the NHANES Laboratory Procedures
Manual.16 The specific measures obtained and
the age group for which they were obtained varied
by NHANES cycle. The sampling frame for each
laboratory measure is detailed in the NHANES
content brochure.5 The ages for the sampling
frame, the total sample size, and the definitions
used for abnormal values are shown in Table 1.
We did not limit lipid values to those measured
when the participants were fasting because previ-
ous research has shown that the differences in
values according to fasting status are minimal.17
Statistical Analysis
The primary results of the bivariate analysis are
presented as mean values for cardiometabolic
variables and for prevalence of cardiometabolic
risk factors, according to weight status. All dif-
ferences were examined with the use of adjusted
Wald tests. We report only the results of joint
Wald tests of differences across all four weight
categories and include 95% confidence intervals
to allow for further interpretation of the differ-
ences between specific groups (e.g., class II obe-
sity as compared with class III obesity). We report
mean values for all children and young adults, as
well as for male and female participants sepa-
rately. Because the quantification of risk is criti-
cal to policy development, we report the results
of a further examination of the prevalence of
cardiometabolic risk factors by weight category
according to subgroups defined by age, sex, and
race or ethnic group. Age, sex, and race or ethnic
group categories were specified before analysis,
and we report all cardiometabolic risk factors
for each. We provide sample sizes throughout
our results for reference, but all reported mean
values, percentages, prevalence values, and results
of statistical tests are weighted to represent the
U.S. population.
Multivariable analyses were performed with
the use of generalized linear models with a loga-
rithmic link. Exponentiation of the coefficients
was used to report risk ratios for the effect of
obesity severity on cardiometabolic risks. All
analyses were adjusted for the strata, primary
sampling units, and probability weights used in
the complex survey design of the NHANES18,19
and were performed with the use of the survey
estimation routines in Stata software, version
13.1 (StataCorp). We pooled all years and ad-
justed the probability weight accordingly, as di-
rected by the NCHS.19 Because our primary inter-
est was the relationship between severe obesity
and cardiometabolic risks and because the prev-
alence of obesity changed minimally during the
time frame of our study,1 we did not perform any
time-trend analysis in this study. P values of less
than 0.05 were considered to indicate statistical
significance, although the differences between
the groups are better represented by the confi-
dence intervals, and we believe that the focus
should be on the clinical importance of the esti-
mates rather than on statistical significance.
Finally, missing data were due primarily to the
design of the NHANES, and therefore no addi-
tional imputation of data was performed.
R esult s
Among the 8579 children and young adults with
a BMI at the 85th percentile or higher, 46.9%
were overweight, 36.4% had class I obesity, 11.9%
had class II obesity, and 4.8% had class III obe-
sity (Table 2). Table S1 in the Supplementary
Appendix (available with the full text of this arti-
cle at NEJM.org) shows the mean values for each
cardiometabolic variable in all participants and
separately in male and female participants. With
few exceptions, in both male and female partici-
pants, the mean values for the cardiometabolic
variables were higher with greater severity of
obesity; for HDL cholesterol, the mean values
were lower with greater severity of obesity.
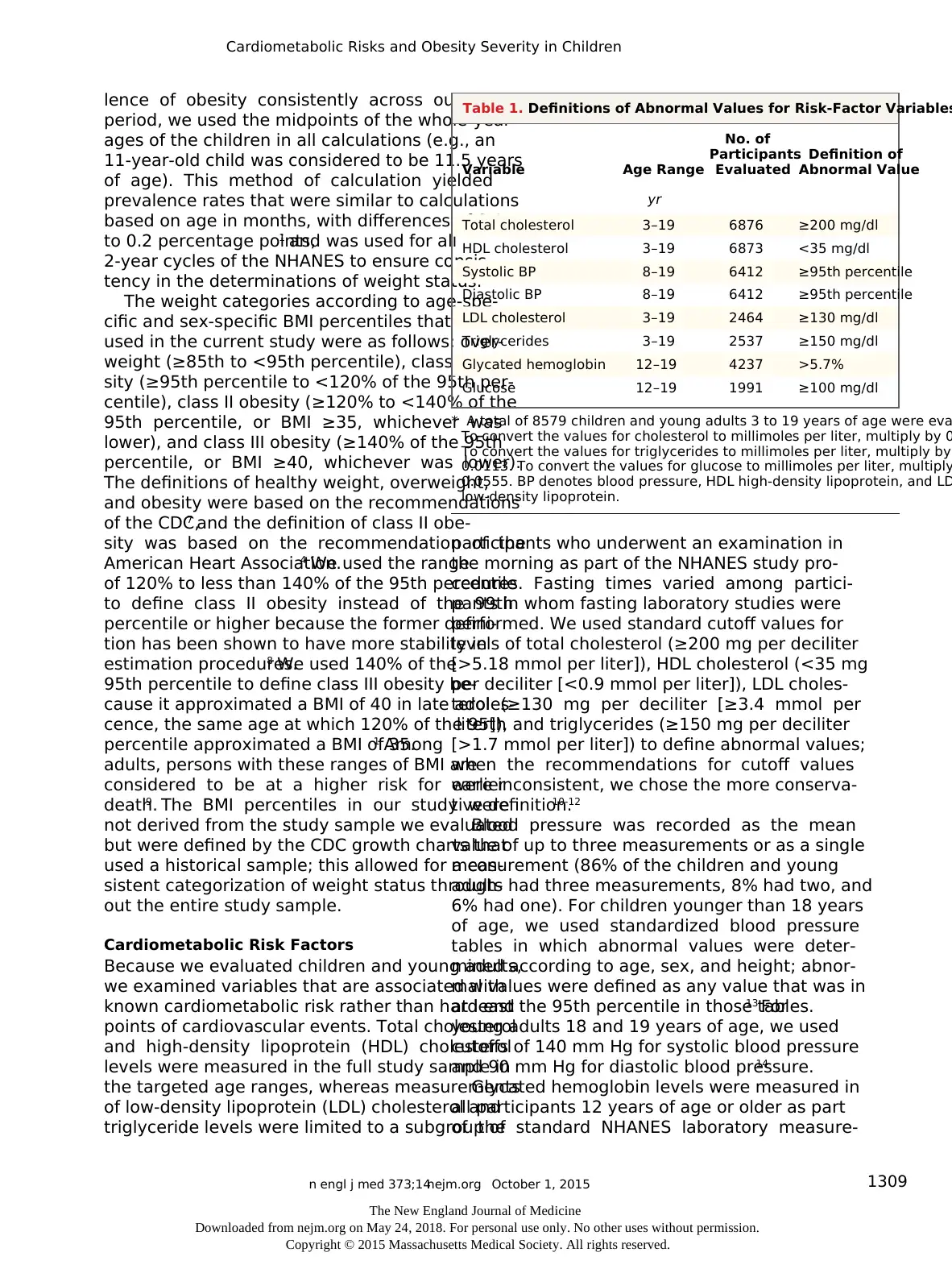
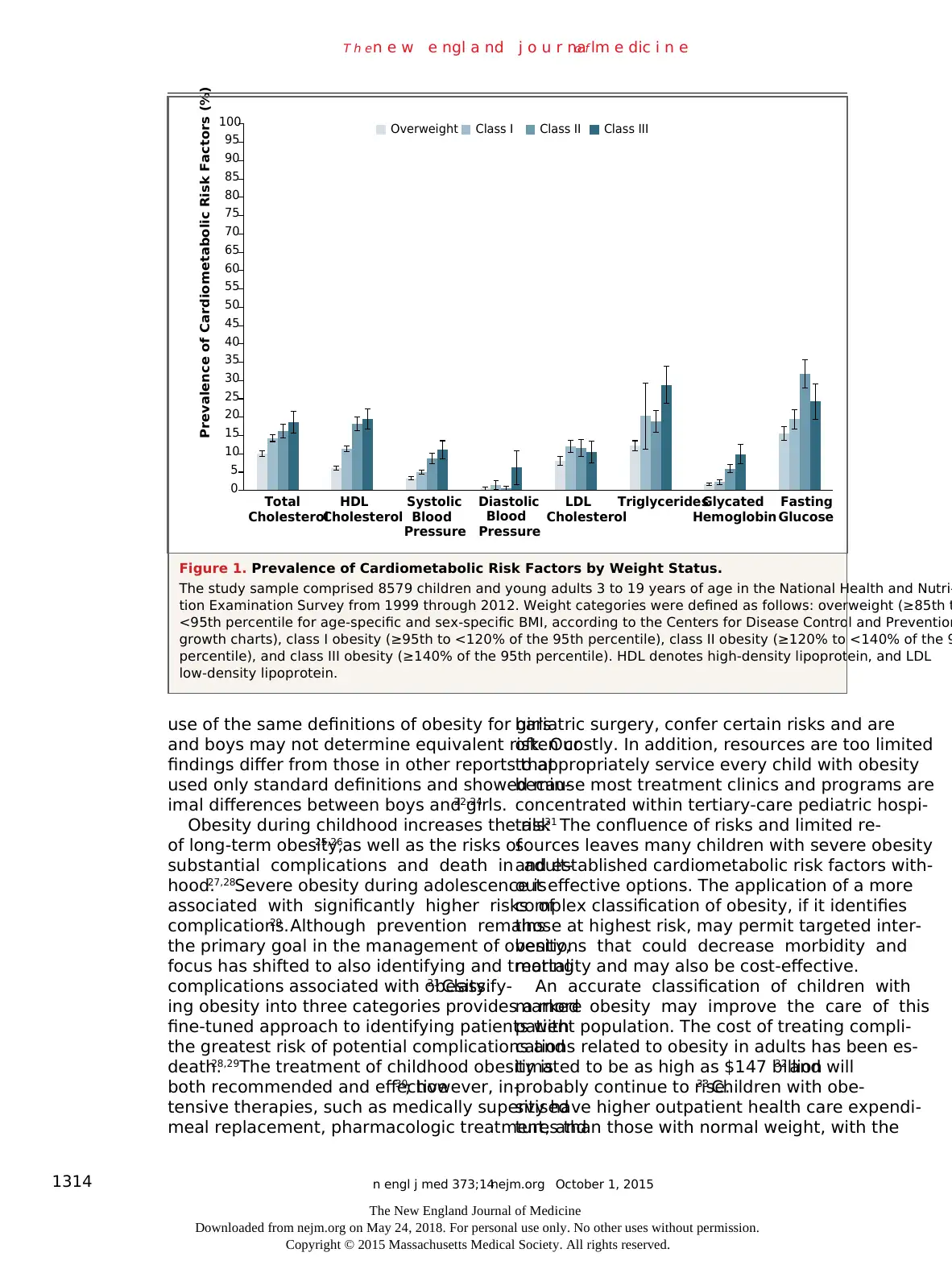
Table 3 and Figure 1 show the prevalence of
abnormal values for each cardiometabolic vari-
able. As was the case with mean values for car-
diometabolic variables, the prevalence of abnor-
mal values was higher with greater severity of
obesity. Table 3 also shows the statistical sig-
nificance of differences across all weight catego-
ries, although the multivariable analyses described
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
T h en e w e ngl a nd j o u r na lo f m e dic i n e
ments; a value greater than 5.7% was defined as
abnormal. Fasting glucose was measured in the
subgroup of NHANES participants who attended
the morning session; a value of 100 mg per deci-
liter or higher (≥5.6 mmol per liter) was defined
as abnormal. The definitions of abnormal values
for glycated hemoglobin and fasting glucose
were based on recommendations by the Ameri-
can Diabetes Association for identifying persons
at high risk for diabetes.15
Detailed information about the collection and
measurement procedures of the NHANES can be
found in the NHANES Laboratory Procedures
Manual.16 The specific measures obtained and
the age group for which they were obtained varied
by NHANES cycle. The sampling frame for each
laboratory measure is detailed in the NHANES
content brochure.5 The ages for the sampling
frame, the total sample size, and the definitions
used for abnormal values are shown in Table 1.
We did not limit lipid values to those measured
when the participants were fasting because previ-
ous research has shown that the differences in
values according to fasting status are minimal.17
Statistical Analysis
The primary results of the bivariate analysis are
presented as mean values for cardiometabolic
variables and for prevalence of cardiometabolic
risk factors, according to weight status. All dif-
ferences were examined with the use of adjusted
Wald tests. We report only the results of joint
Wald tests of differences across all four weight
categories and include 95% confidence intervals
to allow for further interpretation of the differ-
ences between specific groups (e.g., class II obe-
sity as compared with class III obesity). We report
mean values for all children and young adults, as
well as for male and female participants sepa-
rately. Because the quantification of risk is criti-
cal to policy development, we report the results
of a further examination of the prevalence of
cardiometabolic risk factors by weight category
according to subgroups defined by age, sex, and
race or ethnic group. Age, sex, and race or ethnic
group categories were specified before analysis,
and we report all cardiometabolic risk factors
for each. We provide sample sizes throughout
our results for reference, but all reported mean
values, percentages, prevalence values, and results
of statistical tests are weighted to represent the
U.S. population.
Multivariable analyses were performed with
the use of generalized linear models with a loga-
rithmic link. Exponentiation of the coefficients
was used to report risk ratios for the effect of
obesity severity on cardiometabolic risks. All
analyses were adjusted for the strata, primary
sampling units, and probability weights used in
the complex survey design of the NHANES18,19
and were performed with the use of the survey
estimation routines in Stata software, version
13.1 (StataCorp). We pooled all years and ad-
justed the probability weight accordingly, as di-
rected by the NCHS.19 Because our primary inter-
est was the relationship between severe obesity
and cardiometabolic risks and because the prev-
alence of obesity changed minimally during the
time frame of our study,1 we did not perform any
time-trend analysis in this study. P values of less
than 0.05 were considered to indicate statistical
significance, although the differences between
the groups are better represented by the confi-
dence intervals, and we believe that the focus
should be on the clinical importance of the esti-
mates rather than on statistical significance.
Finally, missing data were due primarily to the
design of the NHANES, and therefore no addi-
tional imputation of data was performed.
R esult s
Among the 8579 children and young adults with
a BMI at the 85th percentile or higher, 46.9%
were overweight, 36.4% had class I obesity, 11.9%
had class II obesity, and 4.8% had class III obe-
sity (Table 2). Table S1 in the Supplementary
Appendix (available with the full text of this arti-
cle at NEJM.org) shows the mean values for each
cardiometabolic variable in all participants and
separately in male and female participants. With
few exceptions, in both male and female partici-
pants, the mean values for the cardiometabolic
variables were higher with greater severity of
obesity; for HDL cholesterol, the mean values
were lower with greater severity of obesity.
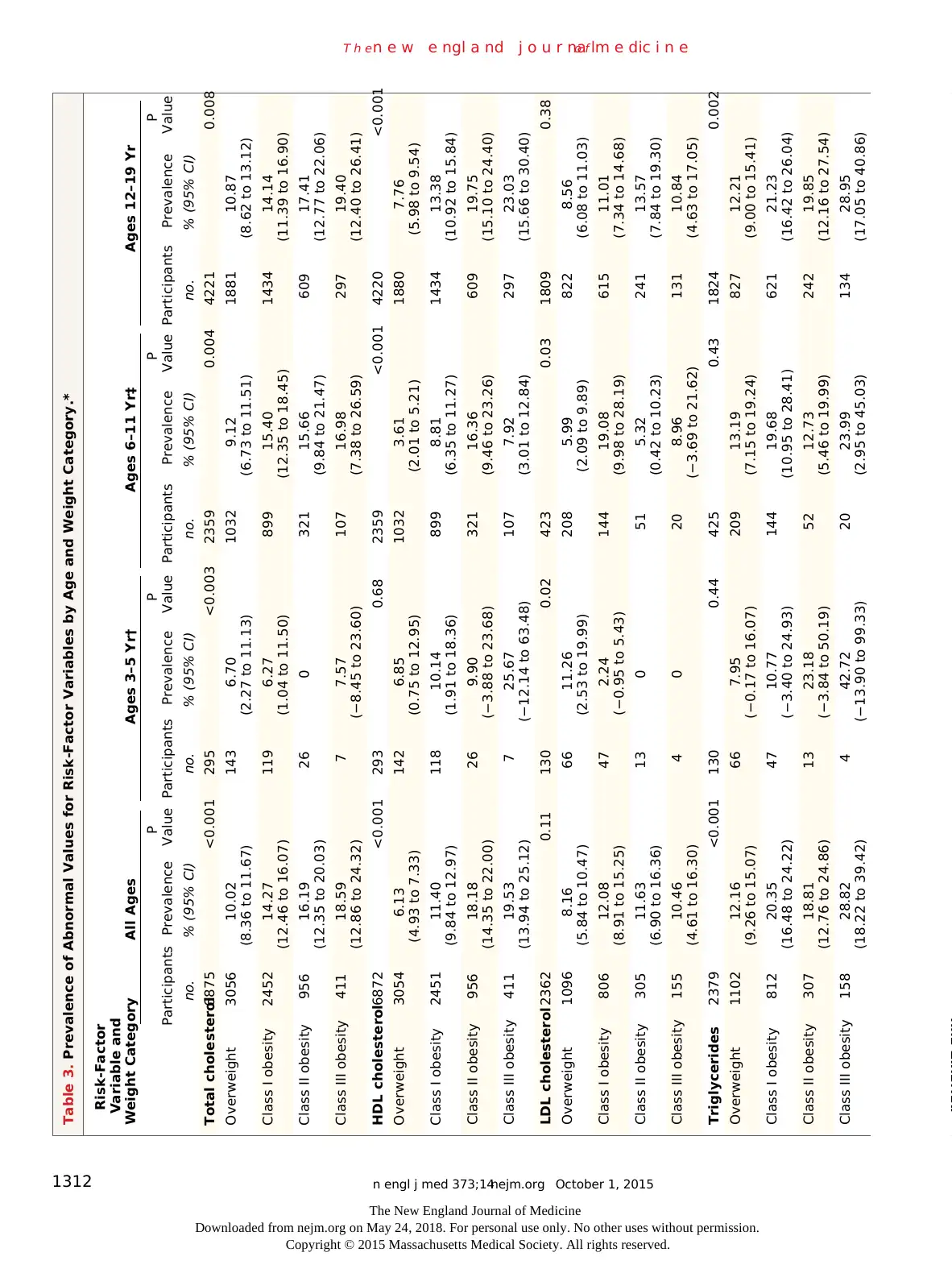
Table 3 and Figure 1 show the prevalence of
abnormal values for each cardiometabolic vari-
able. As was the case with mean values for car-
diometabolic variables, the prevalence of abnor-
mal values was higher with greater severity of
obesity. Table 3 also shows the statistical sig-
nificance of differences across all weight catego-
ries, although the multivariable analyses described
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
n engl j med 373;14nejm.org October 1, 2015 1311
Cardiometabolic Risks and Obesity Severity in Children
below better represent the differences between
individual categories. We report our findings for
all age groups; however, the sample sizes for
children 3 to 5 years of age were very small, and
the associated point estimates for those partici-
pants must be interpreted with caution. Among
participants 12 to 19 years of age, the prevalence
of all risk factors, with the exception of LDL
cholesterol, increased by weight category, and
most risk factors increased by weight category
among children 6 to 11 years of age. Prevalence
according to sex and race or ethnic group are
shown in Tables S2 and S3 in the Supplementary
Appendix, respectively.
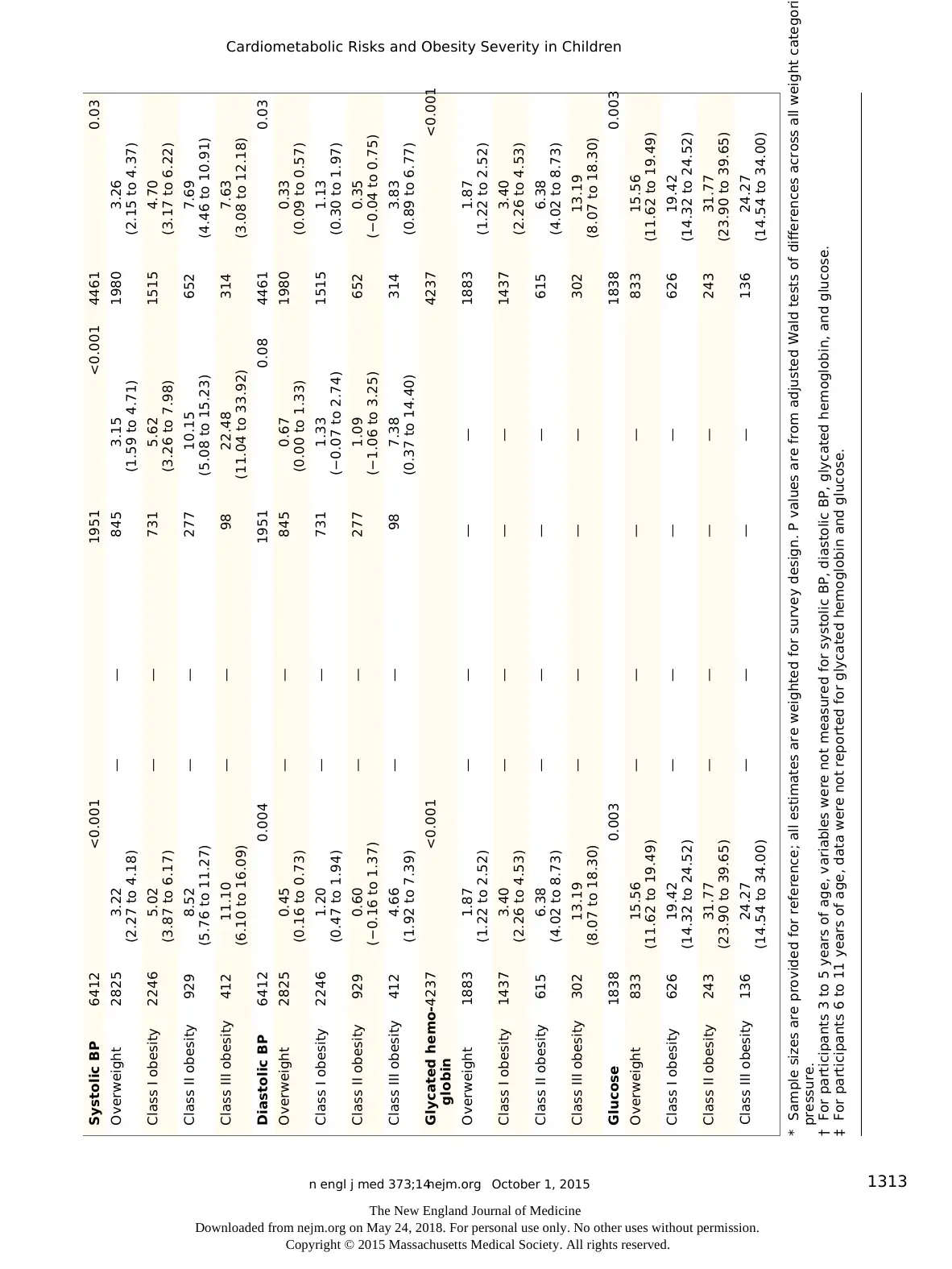
Table 4 shows the results from multivariable
general linear models (see Table S4 in the Supple-
mentary Appendix for data on all variables). In
models that controlled for age, race or ethnic
group, and sex, the risks of low HDL cholesterol
level, high systolic blood pressure, high diastolic
blood pressure, high triglyceride level, and high
glycated hemoglobin level were greater among
children and young adults with class III obesity
than among those with class I obesity. There were
few significant differences in these variables ac-
cording to weight category among female partici-
pants, but all the differences remained significant
among male participants. As expected, overweight
children and young adults had a lower risk of most
risk factors than did those with class I obesity.
Discussion
Severe obesity in children and young adults is
associated with a high prevalence of abnormal
levels of cardiometabolic variables. A high prev-
alence of abnormal values for certain variables
among children and young adults with class II
or class III obesity may provide important infor-
mation beyond that identified with the use of
standard obesity classifications, especially for boys
and young men. The greater prevalence among
participants 12 to 19 years of age is consistent
with a previous report of the overall U.S. popula-
tion of children and adolescents.20
Determination of the severity of obesity can
help identify children and young adults who are
at the greatest risk for the negative health effects
associated with obesity. Current guidelines for
screening do not differentiate among levels of
obesity.7,21Although the prevalence of abnormal
values does not increase with obesity severity in
the case of all risk-factor variables, our findings
of greater risks of abnormal HDL cholesterol
level, systolic blood pressure, and glucose metab-
olism support the stratification of risk on the
basis of the American Heart Association recom-
mendations for classification of a higher level of
obesity at 120% of the 95th percentile.4 Our
findings of the additional risk of abnormal tri-
glyceride and glycated hemoglobin levels provide
initial support for further risk strati fication ac-
cording to 140% of the 95th per centile.
The differences between male and female
participants in our study are notable; severe
obesity is associated with a higher prevalence of
abnormal systolic blood pressure, triglyceride
level, and glycated hemoglobin level among male
participants than among female participants. It
is possible that cardiometabolic risk factors de-
velop earlier in boys than in girls. Alternatively,
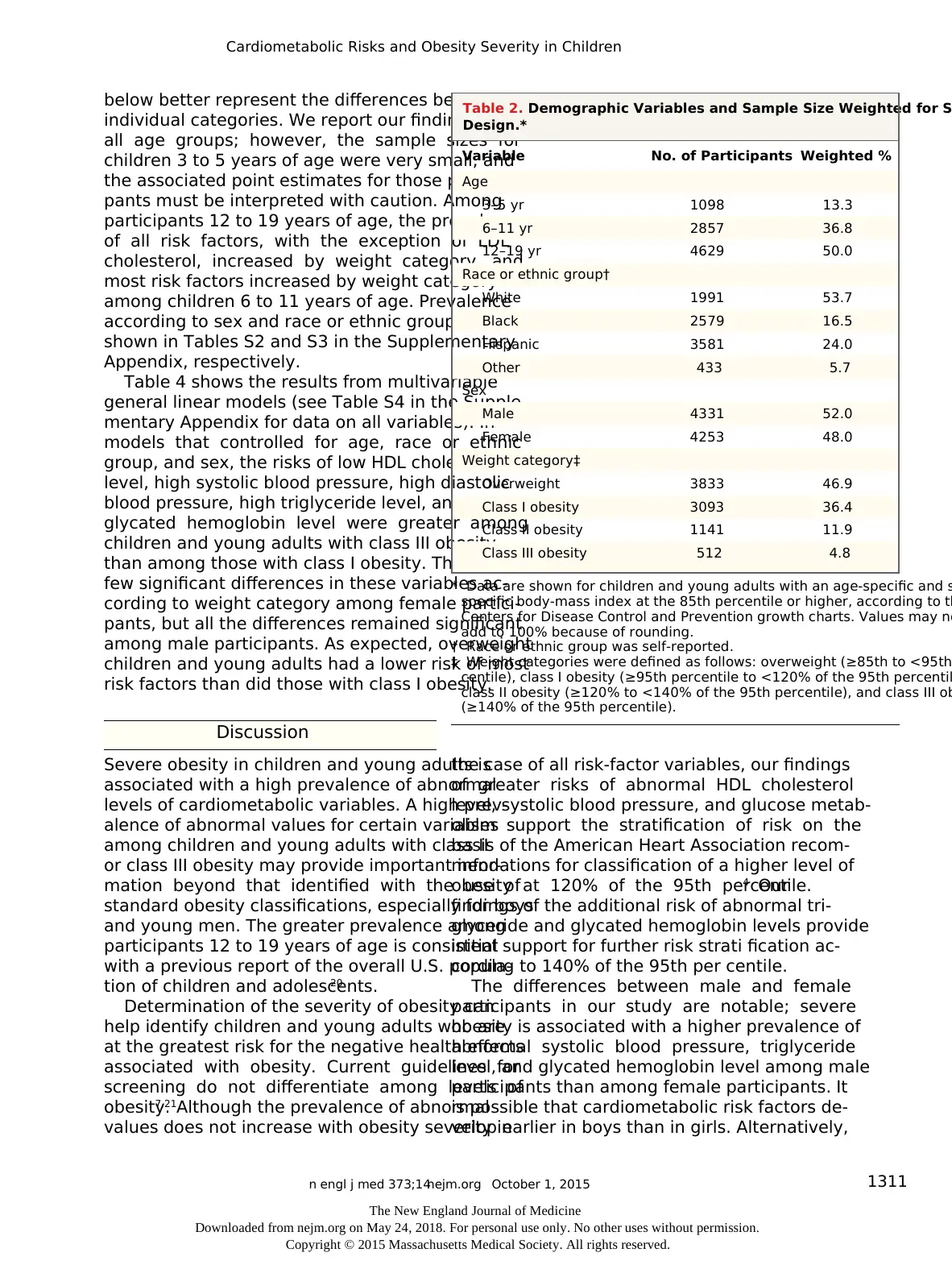
Variable No. of Participants Weighted %
Age
3–5 yr 1098 13.3
6–11 yr 2857 36.8
12–19 yr 4629 50.0
Race or ethnic group†
White 1991 53.7
Black 2579 16.5
Hispanic 3581 24.0
Other 433 5.7
Sex
Male 4331 52.0
Female 4253 48.0
Weight category‡
Overweight 3833 46.9
Class I obesity 3093 36.4
Class II obesity 1141 11.9
Class III obesity 512 4.8
* Data are shown for children and young adults with an age-specific and s
specific body-mass index at the 85th percentile or higher, according to th
Centers for Disease Control and Prevention growth charts. Values may no
add to 100% because of rounding.
† Race or ethnic group was self-reported.
‡ Weight categories were defined as follows: overweight (≥85th to <95th
centile), class I obesity (≥95th percentile to <120% of the 95th percentil
class II obesity (≥120% to <140% of the 95th percentile), and class III ob
(≥140% of the 95th percentile).
Table 2. Demographic Variables and Sample Size Weighted for S
Design.*
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
Cardiometabolic Risks and Obesity Severity in Children
below better represent the differences between
individual categories. We report our findings for
all age groups; however, the sample sizes for
children 3 to 5 years of age were very small, and
the associated point estimates for those partici-
pants must be interpreted with caution. Among
participants 12 to 19 years of age, the prevalence
of all risk factors, with the exception of LDL
cholesterol, increased by weight category, and
most risk factors increased by weight category
among children 6 to 11 years of age. Prevalence
according to sex and race or ethnic group are
shown in Tables S2 and S3 in the Supplementary
Appendix, respectively.
Table 4 shows the results from multivariable
general linear models (see Table S4 in the Supple-
mentary Appendix for data on all variables). In
models that controlled for age, race or ethnic
group, and sex, the risks of low HDL cholesterol
level, high systolic blood pressure, high diastolic
blood pressure, high triglyceride level, and high
glycated hemoglobin level were greater among
children and young adults with class III obesity
than among those with class I obesity. There were
few significant differences in these variables ac-
cording to weight category among female partici-
pants, but all the differences remained significant
among male participants. As expected, overweight
children and young adults had a lower risk of most
risk factors than did those with class I obesity.
Discussion
Severe obesity in children and young adults is
associated with a high prevalence of abnormal
levels of cardiometabolic variables. A high prev-
alence of abnormal values for certain variables
among children and young adults with class II
or class III obesity may provide important infor-
mation beyond that identified with the use of
standard obesity classifications, especially for boys
and young men. The greater prevalence among
participants 12 to 19 years of age is consistent
with a previous report of the overall U.S. popula-
tion of children and adolescents.20
Determination of the severity of obesity can
help identify children and young adults who are
at the greatest risk for the negative health effects
associated with obesity. Current guidelines for
screening do not differentiate among levels of
obesity.7,21Although the prevalence of abnormal
values does not increase with obesity severity in
the case of all risk-factor variables, our findings
of greater risks of abnormal HDL cholesterol
level, systolic blood pressure, and glucose metab-
olism support the stratification of risk on the
basis of the American Heart Association recom-
mendations for classification of a higher level of
obesity at 120% of the 95th percentile.4 Our
findings of the additional risk of abnormal tri-
glyceride and glycated hemoglobin levels provide
initial support for further risk strati fication ac-
cording to 140% of the 95th per centile.
The differences between male and female
participants in our study are notable; severe
obesity is associated with a higher prevalence of
abnormal systolic blood pressure, triglyceride
level, and glycated hemoglobin level among male
participants than among female participants. It
is possible that cardiometabolic risk factors de-
velop earlier in boys than in girls. Alternatively,
Variable No. of Participants Weighted %
Age
3–5 yr 1098 13.3
6–11 yr 2857 36.8
12–19 yr 4629 50.0
Race or ethnic group†
White 1991 53.7
Black 2579 16.5
Hispanic 3581 24.0
Other 433 5.7
Sex
Male 4331 52.0
Female 4253 48.0
Weight category‡
Overweight 3833 46.9
Class I obesity 3093 36.4
Class II obesity 1141 11.9
Class III obesity 512 4.8
* Data are shown for children and young adults with an age-specific and s
specific body-mass index at the 85th percentile or higher, according to th
Centers for Disease Control and Prevention growth charts. Values may no
add to 100% because of rounding.
† Race or ethnic group was self-reported.
‡ Weight categories were defined as follows: overweight (≥85th to <95th
centile), class I obesity (≥95th percentile to <120% of the 95th percentil
class II obesity (≥120% to <140% of the 95th percentile), and class III ob
(≥140% of the 95th percentile).
Table 2. Demographic Variables and Sample Size Weighted for S
Design.*
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
n engl j med 373;14nejm.org October 1, 20151312
T h en e w e ngl a nd j o u r na lo f m e dic i n e
Table 3. Prevalence of Abnormal Values for Risk-Factor Variables by Age and Weight Category.*
Risk-Factor
Variable and
Weight Category All Ages Ages 3–5 Yr† Ages 6–11 Yr‡ Ages 12–19 Yr
Participants Prevalence
P
Value Participants Prevalence
P
Value Participants Prevalence
P
Value Participants Prevalence
P
Value
no. % (95% CI) no. % (95% CI) no. % (95% CI) no. % (95% CI)
Total cholesterol6875 <0.001 295 <0.003 2359 0.004 4221 0.008
Overweight 3056 10.02
(8.36 to 11.67)
143 6.70
(2.27 to 11.13)
1032 9.12
(6.73 to 11.51)
1881 10.87
(8.62 to 13.12)
Class I obesity 2452 14.27
(12.46 to 16.07)
119 6.27
(1.04 to 11.50)
899 15.40
(12.35 to 18.45)
1434 14.14
(11.39 to 16.90)
Class II obesity 956 16.19
(12.35 to 20.03)
26 0 321 15.66
(9.84 to 21.47)
609 17.41
(12.77 to 22.06)
Class III obesity 411 18.59
(12.86 to 24.32)
7 7.57
(−8.45 to 23.60)
107 16.98
(7.38 to 26.59)
297 19.40
(12.40 to 26.41)
HDL cholesterol6872 <0.001 293 0.68 2359 <0.001 4220 <0.001
Overweight 3054 6.13
(4.93 to 7.33)
142 6.85
(0.75 to 12.95)
1032 3.61
(2.01 to 5.21)
1880 7.76
(5.98 to 9.54)
Class I obesity 2451 11.40
(9.84 to 12.97)
118 10.14
(1.91 to 18.36)
899 8.81
(6.35 to 11.27)
1434 13.38
(10.92 to 15.84)
Class II obesity 956 18.18
(14.35 to 22.00)
26 9.90
(−3.88 to 23.68)
321 16.36
(9.46 to 23.26)
609 19.75
(15.10 to 24.40)
Class III obesity 411 19.53
(13.94 to 25.12)
7 25.67
(−12.14 to 63.48)
107 7.92
(3.01 to 12.84)
297 23.03
(15.66 to 30.40)
LDL cholesterol2362 0.11 130 0.02 423 0.03 1809 0.38
Overweight 1096 8.16
(5.84 to 10.47)
66 11.26
(2.53 to 19.99)
208 5.99
(2.09 to 9.89)
822 8.56
(6.08 to 11.03)
Class I obesity 806 12.08
(8.91 to 15.25)
47 2.24
(−0.95 to 5.43)
144 19.08
(9.98 to 28.19)
615 11.01
(7.34 to 14.68)
Class II obesity 305 11.63
(6.90 to 16.36)
13 0 51 5.32
(0.42 to 10.23)
241 13.57
(7.84 to 19.30)
Class III obesity 155 10.46
(4.61 to 16.30)
4 0 20 8.96
(−3.69 to 21.62)
131 10.84
(4.63 to 17.05)
Triglycerides 2379 <0.001 130 0.44 425 0.43 1824 0.002
Overweight 1102 12.16
(9.26 to 15.07)
66 7.95
(−0.17 to 16.07)
209 13.19
(7.15 to 19.24)
827 12.21
(9.00 to 15.41)
Class I obesity 812 20.35
(16.48 to 24.22)
47 10.77
(−3.40 to 24.93)
144 19.68
(10.95 to 28.41)
621 21.23
(16.42 to 26.04)
Class II obesity 307 18.81
(12.76 to 24.86)
13 23.18
(−3.84 to 50.19)
52 12.73
(5.46 to 19.99)
242 19.85
(12.16 to 27.54)
Class III obesity 158 28.82
(18.22 to 39.42)
4 42.72
(−13.90 to 99.33)
20 23.99
(2.95 to 45.03)
134 28.95
(17.05 to 40.86)
Risk-Factor
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
T h en e w e ngl a nd j o u r na lo f m e dic i n e
Table 3. Prevalence of Abnormal Values for Risk-Factor Variables by Age and Weight Category.*
Risk-Factor
Variable and
Weight Category All Ages Ages 3–5 Yr† Ages 6–11 Yr‡ Ages 12–19 Yr
Participants Prevalence
P
Value Participants Prevalence
P
Value Participants Prevalence
P
Value Participants Prevalence
P
Value
no. % (95% CI) no. % (95% CI) no. % (95% CI) no. % (95% CI)
Total cholesterol6875 <0.001 295 <0.003 2359 0.004 4221 0.008
Overweight 3056 10.02
(8.36 to 11.67)
143 6.70
(2.27 to 11.13)
1032 9.12
(6.73 to 11.51)
1881 10.87
(8.62 to 13.12)
Class I obesity 2452 14.27
(12.46 to 16.07)
119 6.27
(1.04 to 11.50)
899 15.40
(12.35 to 18.45)
1434 14.14
(11.39 to 16.90)
Class II obesity 956 16.19
(12.35 to 20.03)
26 0 321 15.66
(9.84 to 21.47)
609 17.41
(12.77 to 22.06)
Class III obesity 411 18.59
(12.86 to 24.32)
7 7.57
(−8.45 to 23.60)
107 16.98
(7.38 to 26.59)
297 19.40
(12.40 to 26.41)
HDL cholesterol6872 <0.001 293 0.68 2359 <0.001 4220 <0.001
Overweight 3054 6.13
(4.93 to 7.33)
142 6.85
(0.75 to 12.95)
1032 3.61
(2.01 to 5.21)
1880 7.76
(5.98 to 9.54)
Class I obesity 2451 11.40
(9.84 to 12.97)
118 10.14
(1.91 to 18.36)
899 8.81
(6.35 to 11.27)
1434 13.38
(10.92 to 15.84)
Class II obesity 956 18.18
(14.35 to 22.00)
26 9.90
(−3.88 to 23.68)
321 16.36
(9.46 to 23.26)
609 19.75
(15.10 to 24.40)
Class III obesity 411 19.53
(13.94 to 25.12)
7 25.67
(−12.14 to 63.48)
107 7.92
(3.01 to 12.84)
297 23.03
(15.66 to 30.40)
LDL cholesterol2362 0.11 130 0.02 423 0.03 1809 0.38
Overweight 1096 8.16
(5.84 to 10.47)
66 11.26
(2.53 to 19.99)
208 5.99
(2.09 to 9.89)
822 8.56
(6.08 to 11.03)
Class I obesity 806 12.08
(8.91 to 15.25)
47 2.24
(−0.95 to 5.43)
144 19.08
(9.98 to 28.19)
615 11.01
(7.34 to 14.68)
Class II obesity 305 11.63
(6.90 to 16.36)
13 0 51 5.32
(0.42 to 10.23)
241 13.57
(7.84 to 19.30)
Class III obesity 155 10.46
(4.61 to 16.30)
4 0 20 8.96
(−3.69 to 21.62)
131 10.84
(4.63 to 17.05)
Triglycerides 2379 <0.001 130 0.44 425 0.43 1824 0.002
Overweight 1102 12.16
(9.26 to 15.07)
66 7.95
(−0.17 to 16.07)
209 13.19
(7.15 to 19.24)
827 12.21
(9.00 to 15.41)
Class I obesity 812 20.35
(16.48 to 24.22)
47 10.77
(−3.40 to 24.93)
144 19.68
(10.95 to 28.41)
621 21.23
(16.42 to 26.04)
Class II obesity 307 18.81
(12.76 to 24.86)
13 23.18
(−3.84 to 50.19)
52 12.73
(5.46 to 19.99)
242 19.85
(12.16 to 27.54)
Class III obesity 158 28.82
(18.22 to 39.42)
4 42.72
(−13.90 to 99.33)
20 23.99
(2.95 to 45.03)
134 28.95
(17.05 to 40.86)
Risk-Factor
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
n engl j med 373;14nejm.org October 1, 2015 1313
Cardiometabolic Risks and Obesity Severity in Children
Variable and
Weight Category All Ages Ages 3–5 Yr† Ages 6–11 Yr‡ Ages 12–19 Yr
Participants Prevalence
P
Value Participants Prevalence
P
Value Participants Prevalence
P
Value Participants Prevalence
P
Value
no. % (95% CI) no. % (95% CI) no. % (95% CI) no. % (95% CI)
Systolic BP 6412 <0.001 1951 <0.001 4461 0.03
Overweight 2825 3.22
(2.27 to 4.18)
— — 845 3.15
(1.59 to 4.71)
1980 3.26
(2.15 to 4.37)
Class I obesity 2246 5.02
(3.87 to 6.17)
— — 731 5.62
(3.26 to 7.98)
1515 4.70
(3.17 to 6.22)
Class II obesity 929 8.52
(5.76 to 11.27)
— — 277 10.15
(5.08 to 15.23)
652 7.69
(4.46 to 10.91)
Class III obesity 412 11.10
(6.10 to 16.09)
— — 98 22.48
(11.04 to 33.92)
314 7.63
(3.08 to 12.18)
Diastolic BP 6412 0.004 1951 0.08 4461 0.03
Overweight 2825 0.45
(0.16 to 0.73)
— — 845 0.67
(0.00 to 1.33)
1980 0.33
(0.09 to 0.57)
Class I obesity 2246 1.20
(0.47 to 1.94)
— — 731 1.33
(−0.07 to 2.74)
1515 1.13
(0.30 to 1.97)
Class II obesity 929 0.60
(−0.16 to 1.37)
— — 277 1.09
(−1.06 to 3.25)
652 0.35
(−0.04 to 0.75)
Class III obesity 412 4.66
(1.92 to 7.39)
— — 98 7.38
(0.37 to 14.40)
314 3.83
(0.89 to 6.77)
Glycated hemo-
globin
4237 <0.001 4237 <0.001
Overweight 1883 1.87
(1.22 to 2.52)
— — — — 1883 1.87
(1.22 to 2.52)
Class I obesity 1437 3.40
(2.26 to 4.53)
— — — — 1437 3.40
(2.26 to 4.53)
Class II obesity 615 6.38
(4.02 to 8.73)
— — — — 615 6.38
(4.02 to 8.73)
Class III obesity 302 13.19
(8.07 to 18.30)
— — — — 302 13.19
(8.07 to 18.30)
Glucose 1838 0.003 1838 0.003
Overweight 833 15.56
(11.62 to 19.49)
— — — — 833 15.56
(11.62 to 19.49)
Class I obesity 626 19.42
(14.32 to 24.52)
— — — — 626 19.42
(14.32 to 24.52)
Class II obesity 243 31.77
(23.90 to 39.65)
— — — — 243 31.77
(23.90 to 39.65)
Class III obesity 136 24.27
(14.54 to 34.00)
— — — — 136 24.27
(14.54 to 34.00)
* Sample sizes are provided for reference; all estimates are weighted for survey design. P values are from adjusted Wald tests of differences across all weight categorie
pressure.
† For participants 3 to 5 years of age, variables were not measured for systolic BP, diastolic BP, glycated hemoglobin, and glucose.
‡ For participants 6 to 11 years of age, data were not reported for glycated hemoglobin and glucose.
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
Cardiometabolic Risks and Obesity Severity in Children
Variable and
Weight Category All Ages Ages 3–5 Yr† Ages 6–11 Yr‡ Ages 12–19 Yr
Participants Prevalence
P
Value Participants Prevalence
P
Value Participants Prevalence
P
Value Participants Prevalence
P
Value
no. % (95% CI) no. % (95% CI) no. % (95% CI) no. % (95% CI)
Systolic BP 6412 <0.001 1951 <0.001 4461 0.03
Overweight 2825 3.22
(2.27 to 4.18)
— — 845 3.15
(1.59 to 4.71)
1980 3.26
(2.15 to 4.37)
Class I obesity 2246 5.02
(3.87 to 6.17)
— — 731 5.62
(3.26 to 7.98)
1515 4.70
(3.17 to 6.22)
Class II obesity 929 8.52
(5.76 to 11.27)
— — 277 10.15
(5.08 to 15.23)
652 7.69
(4.46 to 10.91)
Class III obesity 412 11.10
(6.10 to 16.09)
— — 98 22.48
(11.04 to 33.92)
314 7.63
(3.08 to 12.18)
Diastolic BP 6412 0.004 1951 0.08 4461 0.03
Overweight 2825 0.45
(0.16 to 0.73)
— — 845 0.67
(0.00 to 1.33)
1980 0.33
(0.09 to 0.57)
Class I obesity 2246 1.20
(0.47 to 1.94)
— — 731 1.33
(−0.07 to 2.74)
1515 1.13
(0.30 to 1.97)
Class II obesity 929 0.60
(−0.16 to 1.37)
— — 277 1.09
(−1.06 to 3.25)
652 0.35
(−0.04 to 0.75)
Class III obesity 412 4.66
(1.92 to 7.39)
— — 98 7.38
(0.37 to 14.40)
314 3.83
(0.89 to 6.77)
Glycated hemo-
globin
4237 <0.001 4237 <0.001
Overweight 1883 1.87
(1.22 to 2.52)
— — — — 1883 1.87
(1.22 to 2.52)
Class I obesity 1437 3.40
(2.26 to 4.53)
— — — — 1437 3.40
(2.26 to 4.53)
Class II obesity 615 6.38
(4.02 to 8.73)
— — — — 615 6.38
(4.02 to 8.73)
Class III obesity 302 13.19
(8.07 to 18.30)
— — — — 302 13.19
(8.07 to 18.30)
Glucose 1838 0.003 1838 0.003
Overweight 833 15.56
(11.62 to 19.49)
— — — — 833 15.56
(11.62 to 19.49)
Class I obesity 626 19.42
(14.32 to 24.52)
— — — — 626 19.42
(14.32 to 24.52)
Class II obesity 243 31.77
(23.90 to 39.65)
— — — — 243 31.77
(23.90 to 39.65)
Class III obesity 136 24.27
(14.54 to 34.00)
— — — — 136 24.27
(14.54 to 34.00)
* Sample sizes are provided for reference; all estimates are weighted for survey design. P values are from adjusted Wald tests of differences across all weight categorie
pressure.
† For participants 3 to 5 years of age, variables were not measured for systolic BP, diastolic BP, glycated hemoglobin, and glucose.
‡ For participants 6 to 11 years of age, data were not reported for glycated hemoglobin and glucose.
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
n engl j med 373;14nejm.org October 1, 20151314
T h en e w e ngl a nd j o u r na lo f m e dic i n e
use of the same definitions of obesity for girls
and boys may not determine equivalent risk. Our
findings differ from those in other reports that
used only standard definitions and showed min-
imal differences between boys and girls.22-24
Obesity during childhood increases the risk
of long-term obesity,25,26as well as the risks of
substantial complications and death in adult-
hood.27,28Severe obesity during adolescence is
associated with significantly higher risks of
complications.29 Although prevention remains
the primary goal in the management of obesity,
focus has shifted to also identifying and treating
complications associated with obesity.21 Classify-
ing obesity into three categories provides a more
fine-tuned approach to identifying patients with
the greatest risk of potential complications and
death.28,29The treatment of childhood obesity is
both recommended and effective30
; however, in-
tensive therapies, such as medically supervised
meal replacement, pharmacologic treatment, and
bariatric surgery, confer certain risks and are
often costly. In addition, resources are too limited
to appropriately service every child with obesity
because most treatment clinics and programs are
concentrated within tertiary-care pediatric hospi-
tals.31 The confluence of risks and limited re-
sources leaves many children with severe obesity
and established cardiometabolic risk factors with-
out effective options. The application of a more
complex classification of obesity, if it identifies
those at highest risk, may permit targeted inter-
ventions that could decrease morbidity and
mortality and may also be cost-effective.
An accurate classification of children with
marked obesity may improve the care of this
patient population. The cost of treating compli-
cations related to obesity in adults has been es-
timated to be as high as $147 billion32 and will
probably continue to rise.33 Children with obe-
sity have higher outpatient health care expendi-
tures than those with normal weight, with the
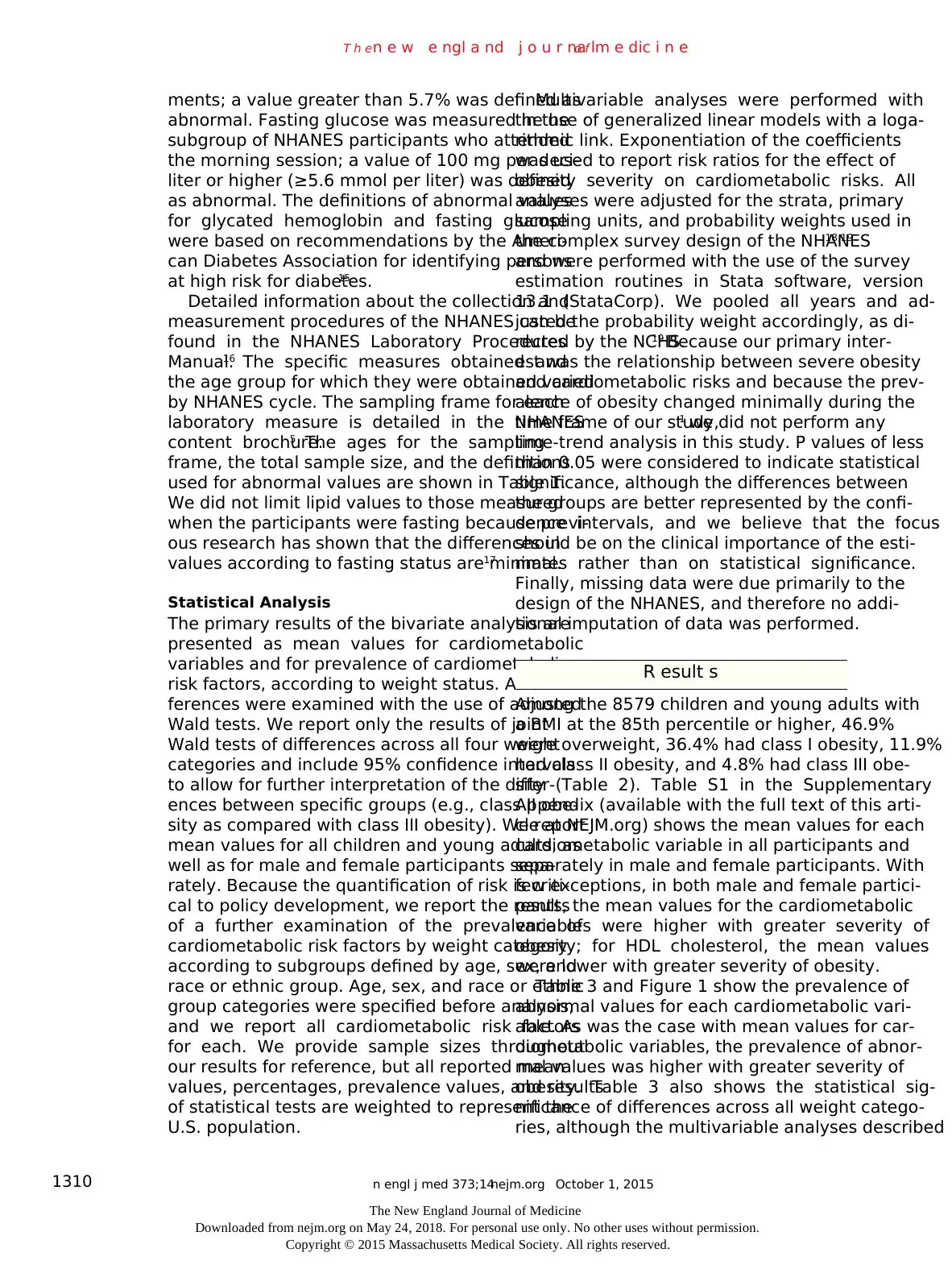
Figure 1. Prevalence of Cardiometabolic Risk Factors by Weight Status.
The study sample comprised 8579 children and young adults 3 to 19 years of age in the National Health and Nutri-
tion Examination Survey from 1999 through 2012. Weight categories were defined as follows: overweight (≥85th t
<95th percentile for age-specific and sex-specific BMI, according to the Centers for Disease Control and Prevention
growth charts), class I obesity (≥95th to <120% of the 95th percentile), class II obesity (≥120% to <140% of the 9
percentile), and class III obesity (≥140% of the 95th percentile). HDL denotes high-density lipoprotein, and LDL
low-density lipoprotein.
Prevalence of Cardiometabolic Risk Factors (%)
40
30
35
25
20
10
5
15
0
80
70
75
65
95
85
90
100
60
50
45
55
Total
Cholesterol
HDL
Cholesterol
LDL
Cholesterol
TriglyceridesGlycated
Hemoglobin
Fasting
Glucose
Systolic
Blood
Pressure
Diastolic
Blood
Pressure
Overweight Class II Class IIIClass I
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
T h en e w e ngl a nd j o u r na lo f m e dic i n e
use of the same definitions of obesity for girls
and boys may not determine equivalent risk. Our
findings differ from those in other reports that
used only standard definitions and showed min-
imal differences between boys and girls.22-24
Obesity during childhood increases the risk
of long-term obesity,25,26as well as the risks of
substantial complications and death in adult-
hood.27,28Severe obesity during adolescence is
associated with significantly higher risks of
complications.29 Although prevention remains
the primary goal in the management of obesity,
focus has shifted to also identifying and treating
complications associated with obesity.21 Classify-
ing obesity into three categories provides a more
fine-tuned approach to identifying patients with
the greatest risk of potential complications and
death.28,29The treatment of childhood obesity is
both recommended and effective30
; however, in-
tensive therapies, such as medically supervised
meal replacement, pharmacologic treatment, and
bariatric surgery, confer certain risks and are
often costly. In addition, resources are too limited
to appropriately service every child with obesity
because most treatment clinics and programs are
concentrated within tertiary-care pediatric hospi-
tals.31 The confluence of risks and limited re-
sources leaves many children with severe obesity
and established cardiometabolic risk factors with-
out effective options. The application of a more
complex classification of obesity, if it identifies
those at highest risk, may permit targeted inter-
ventions that could decrease morbidity and
mortality and may also be cost-effective.
An accurate classification of children with
marked obesity may improve the care of this
patient population. The cost of treating compli-
cations related to obesity in adults has been es-
timated to be as high as $147 billion32 and will
probably continue to rise.33 Children with obe-
sity have higher outpatient health care expendi-
tures than those with normal weight, with the
Figure 1. Prevalence of Cardiometabolic Risk Factors by Weight Status.
The study sample comprised 8579 children and young adults 3 to 19 years of age in the National Health and Nutri-
tion Examination Survey from 1999 through 2012. Weight categories were defined as follows: overweight (≥85th t
<95th percentile for age-specific and sex-specific BMI, according to the Centers for Disease Control and Prevention
growth charts), class I obesity (≥95th to <120% of the 95th percentile), class II obesity (≥120% to <140% of the 9
percentile), and class III obesity (≥140% of the 95th percentile). HDL denotes high-density lipoprotein, and LDL
low-density lipoprotein.
Prevalence of Cardiometabolic Risk Factors (%)
40
30
35
25
20
10
5
15
0
80
70
75
65
95
85
90
100
60
50
45
55
Total
Cholesterol
HDL
Cholesterol
LDL
Cholesterol
TriglyceridesGlycated
Hemoglobin
Fasting
Glucose
Systolic
Blood
Pressure
Diastolic
Blood
Pressure
Overweight Class II Class IIIClass I
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
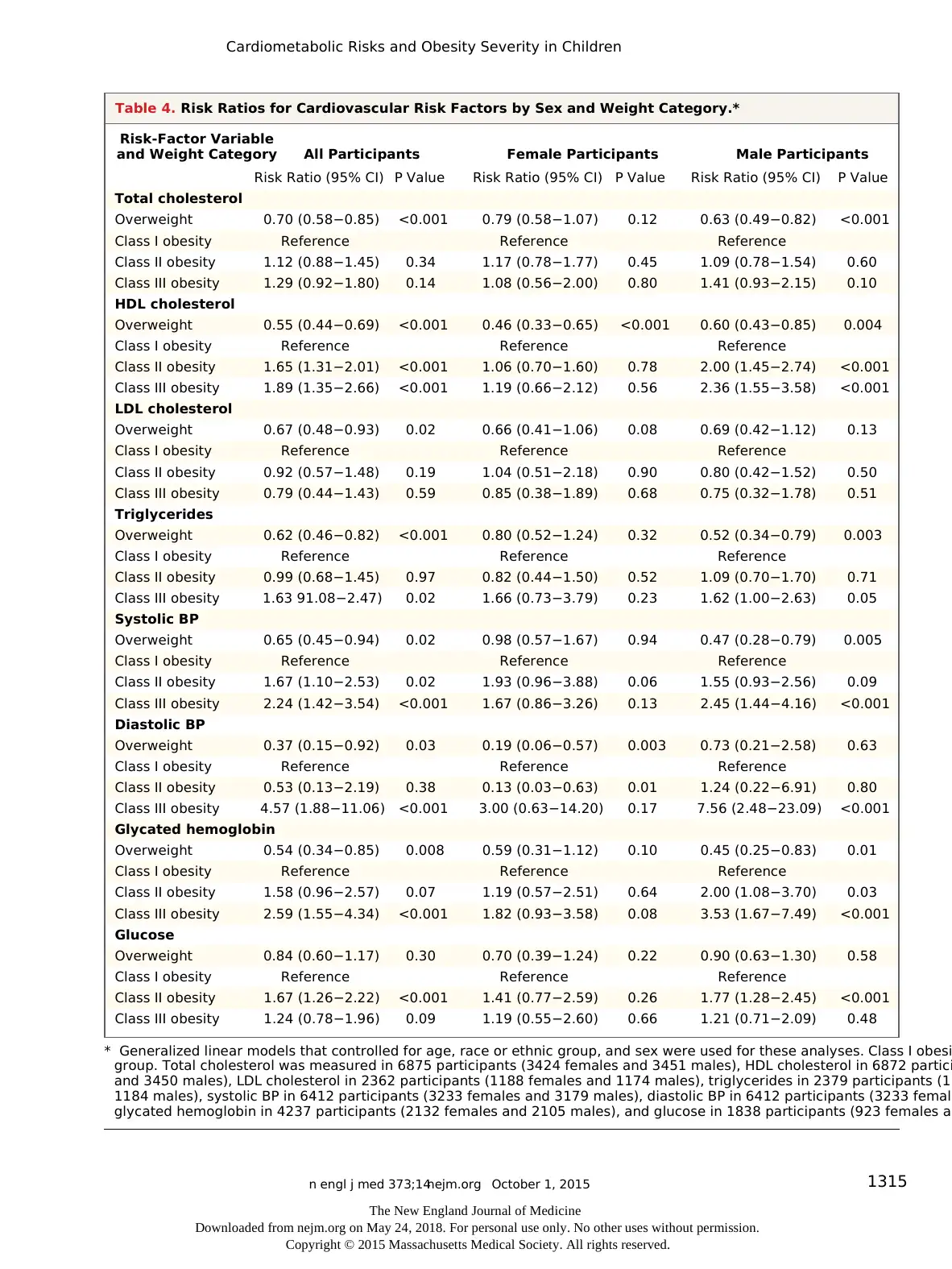
n engl j med 373;14nejm.org October 1, 2015 1315
Cardiometabolic Risks and Obesity Severity in Children
Risk-Factor Variable
and Weight Category All Participants Female Participants Male Participants
Risk Ratio (95% CI) P Value Risk Ratio (95% CI) P Value Risk Ratio (95% CI) P Value
Total cholesterol
Overweight 0.70 (0.58−0.85) <0.001 0.79 (0.58−1.07) 0.12 0.63 (0.49−0.82) <0.001
Class I obesity Reference Reference Reference
Class II obesity 1.12 (0.88−1.45) 0.34 1.17 (0.78−1.77) 0.45 1.09 (0.78−1.54) 0.60
Class III obesity 1.29 (0.92−1.80) 0.14 1.08 (0.56−2.00) 0.80 1.41 (0.93−2.15) 0.10
HDL cholesterol
Overweight 0.55 (0.44−0.69) <0.001 0.46 (0.33−0.65) <0.001 0.60 (0.43−0.85) 0.004
Class I obesity Reference Reference Reference
Class II obesity 1.65 (1.31−2.01) <0.001 1.06 (0.70−1.60) 0.78 2.00 (1.45−2.74) <0.001
Class III obesity 1.89 (1.35−2.66) <0.001 1.19 (0.66−2.12) 0.56 2.36 (1.55−3.58) <0.001
LDL cholesterol
Overweight 0.67 (0.48−0.93) 0.02 0.66 (0.41−1.06) 0.08 0.69 (0.42−1.12) 0.13
Class I obesity Reference Reference Reference
Class II obesity 0.92 (0.57−1.48) 0.19 1.04 (0.51−2.18) 0.90 0.80 (0.42−1.52) 0.50
Class III obesity 0.79 (0.44−1.43) 0.59 0.85 (0.38−1.89) 0.68 0.75 (0.32−1.78) 0.51
Triglycerides
Overweight 0.62 (0.46−0.82) <0.001 0.80 (0.52−1.24) 0.32 0.52 (0.34−0.79) 0.003
Class I obesity Reference Reference Reference
Class II obesity 0.99 (0.68−1.45) 0.97 0.82 (0.44−1.50) 0.52 1.09 (0.70−1.70) 0.71
Class III obesity 1.63 91.08−2.47) 0.02 1.66 (0.73−3.79) 0.23 1.62 (1.00−2.63) 0.05
Systolic BP
Overweight 0.65 (0.45−0.94) 0.02 0.98 (0.57−1.67) 0.94 0.47 (0.28−0.79) 0.005
Class I obesity Reference Reference Reference
Class II obesity 1.67 (1.10−2.53) 0.02 1.93 (0.96−3.88) 0.06 1.55 (0.93−2.56) 0.09
Class III obesity 2.24 (1.42−3.54) <0.001 1.67 (0.86−3.26) 0.13 2.45 (1.44−4.16) <0.001
Diastolic BP
Overweight 0.37 (0.15−0.92) 0.03 0.19 (0.06−0.57) 0.003 0.73 (0.21−2.58) 0.63
Class I obesity Reference Reference Reference
Class II obesity 0.53 (0.13−2.19) 0.38 0.13 (0.03−0.63) 0.01 1.24 (0.22−6.91) 0.80
Class III obesity 4.57 (1.88−11.06) <0.001 3.00 (0.63−14.20) 0.17 7.56 (2.48−23.09) <0.001
Glycated hemoglobin
Overweight 0.54 (0.34−0.85) 0.008 0.59 (0.31−1.12) 0.10 0.45 (0.25−0.83) 0.01
Class I obesity Reference Reference Reference
Class II obesity 1.58 (0.96−2.57) 0.07 1.19 (0.57−2.51) 0.64 2.00 (1.08−3.70) 0.03
Class III obesity 2.59 (1.55−4.34) <0.001 1.82 (0.93−3.58) 0.08 3.53 (1.67−7.49) <0.001
Glucose
Overweight 0.84 (0.60−1.17) 0.30 0.70 (0.39−1.24) 0.22 0.90 (0.63−1.30) 0.58
Class I obesity Reference Reference Reference
Class II obesity 1.67 (1.26−2.22) <0.001 1.41 (0.77−2.59) 0.26 1.77 (1.28−2.45) <0.001
Class III obesity 1.24 (0.78−1.96) 0.09 1.19 (0.55−2.60) 0.66 1.21 (0.71−2.09) 0.48
* Generalized linear models that controlled for age, race or ethnic group, and sex were used for these analyses. Class I obesi
group. Total cholesterol was measured in 6875 participants (3424 females and 3451 males), HDL cholesterol in 6872 partici
and 3450 males), LDL cholesterol in 2362 participants (1188 females and 1174 males), triglycerides in 2379 participants (11
1184 males), systolic BP in 6412 participants (3233 females and 3179 males), diastolic BP in 6412 participants (3233 female
glycated hemoglobin in 4237 participants (2132 females and 2105 males), and glucose in 1838 participants (923 females an
Table 4. Risk Ratios for Cardiovascular Risk Factors by Sex and Weight Category.*
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
Cardiometabolic Risks and Obesity Severity in Children
Risk-Factor Variable
and Weight Category All Participants Female Participants Male Participants
Risk Ratio (95% CI) P Value Risk Ratio (95% CI) P Value Risk Ratio (95% CI) P Value
Total cholesterol
Overweight 0.70 (0.58−0.85) <0.001 0.79 (0.58−1.07) 0.12 0.63 (0.49−0.82) <0.001
Class I obesity Reference Reference Reference
Class II obesity 1.12 (0.88−1.45) 0.34 1.17 (0.78−1.77) 0.45 1.09 (0.78−1.54) 0.60
Class III obesity 1.29 (0.92−1.80) 0.14 1.08 (0.56−2.00) 0.80 1.41 (0.93−2.15) 0.10
HDL cholesterol
Overweight 0.55 (0.44−0.69) <0.001 0.46 (0.33−0.65) <0.001 0.60 (0.43−0.85) 0.004
Class I obesity Reference Reference Reference
Class II obesity 1.65 (1.31−2.01) <0.001 1.06 (0.70−1.60) 0.78 2.00 (1.45−2.74) <0.001
Class III obesity 1.89 (1.35−2.66) <0.001 1.19 (0.66−2.12) 0.56 2.36 (1.55−3.58) <0.001
LDL cholesterol
Overweight 0.67 (0.48−0.93) 0.02 0.66 (0.41−1.06) 0.08 0.69 (0.42−1.12) 0.13
Class I obesity Reference Reference Reference
Class II obesity 0.92 (0.57−1.48) 0.19 1.04 (0.51−2.18) 0.90 0.80 (0.42−1.52) 0.50
Class III obesity 0.79 (0.44−1.43) 0.59 0.85 (0.38−1.89) 0.68 0.75 (0.32−1.78) 0.51
Triglycerides
Overweight 0.62 (0.46−0.82) <0.001 0.80 (0.52−1.24) 0.32 0.52 (0.34−0.79) 0.003
Class I obesity Reference Reference Reference
Class II obesity 0.99 (0.68−1.45) 0.97 0.82 (0.44−1.50) 0.52 1.09 (0.70−1.70) 0.71
Class III obesity 1.63 91.08−2.47) 0.02 1.66 (0.73−3.79) 0.23 1.62 (1.00−2.63) 0.05
Systolic BP
Overweight 0.65 (0.45−0.94) 0.02 0.98 (0.57−1.67) 0.94 0.47 (0.28−0.79) 0.005
Class I obesity Reference Reference Reference
Class II obesity 1.67 (1.10−2.53) 0.02 1.93 (0.96−3.88) 0.06 1.55 (0.93−2.56) 0.09
Class III obesity 2.24 (1.42−3.54) <0.001 1.67 (0.86−3.26) 0.13 2.45 (1.44−4.16) <0.001
Diastolic BP
Overweight 0.37 (0.15−0.92) 0.03 0.19 (0.06−0.57) 0.003 0.73 (0.21−2.58) 0.63
Class I obesity Reference Reference Reference
Class II obesity 0.53 (0.13−2.19) 0.38 0.13 (0.03−0.63) 0.01 1.24 (0.22−6.91) 0.80
Class III obesity 4.57 (1.88−11.06) <0.001 3.00 (0.63−14.20) 0.17 7.56 (2.48−23.09) <0.001
Glycated hemoglobin
Overweight 0.54 (0.34−0.85) 0.008 0.59 (0.31−1.12) 0.10 0.45 (0.25−0.83) 0.01
Class I obesity Reference Reference Reference
Class II obesity 1.58 (0.96−2.57) 0.07 1.19 (0.57−2.51) 0.64 2.00 (1.08−3.70) 0.03
Class III obesity 2.59 (1.55−4.34) <0.001 1.82 (0.93−3.58) 0.08 3.53 (1.67−7.49) <0.001
Glucose
Overweight 0.84 (0.60−1.17) 0.30 0.70 (0.39−1.24) 0.22 0.90 (0.63−1.30) 0.58
Class I obesity Reference Reference Reference
Class II obesity 1.67 (1.26−2.22) <0.001 1.41 (0.77−2.59) 0.26 1.77 (1.28−2.45) <0.001
Class III obesity 1.24 (0.78−1.96) 0.09 1.19 (0.55−2.60) 0.66 1.21 (0.71−2.09) 0.48
* Generalized linear models that controlled for age, race or ethnic group, and sex were used for these analyses. Class I obesi
group. Total cholesterol was measured in 6875 participants (3424 females and 3451 males), HDL cholesterol in 6872 partici
and 3450 males), LDL cholesterol in 2362 participants (1188 females and 1174 males), triglycerides in 2379 participants (11
1184 males), systolic BP in 6412 participants (3233 females and 3179 males), diastolic BP in 6412 participants (3233 female
glycated hemoglobin in 4237 participants (2132 females and 2105 males), and glucose in 1838 participants (923 females an
Table 4. Risk Ratios for Cardiovascular Risk Factors by Sex and Weight Category.*
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
n engl j med 373;14nejm.org October 1, 20151316
T h en e w e ngl a nd j o u r na lo f m e dic i n e
increased costs believed to stem from the evalu-
ation and treatment of coexisting conditions34
;
an improved estimation of risk that is based on
obesity severity could lower the costs of evalua-
tion without resulting in missed diagnoses of co-
existing conditions. Children with severe obesity
already have increased cardiometabolic risk, which
may predict the early onset of serious diseases
such as hypertension and diabetes.
As older adolescents transition to young
adulthood, the recognition that teens with obe-
sity have increased cardiometabolic risk will be
important. Current treatment approaches are
not as effective at higher levels of obesity than
they are at lower levels of obesity.35-37The find-
ings in our study, when considered in the con-
text of the negative effect that these risk factors
have on subsequent quality of life,38 imply a
need for the early identification of abnormal
weight gain, primary and secondary prevention
of obesity, and systemwide policy changes in
the evaluation and management of obesity in
health care.39
We examined a range of cardiometabolic risk-
factor variables in a large and nationally repre-
sentative population; however, our study has cer-
tain methodologic limitations. First, because this
is a cross-sectional study, we could not show
causality between obesity and risk factors. Sec-
ond, although we used standard definitions of
abnormal values for risk-factor variables, the cross-
sectional design did not allow us to examine the
effects of these abnormal values on future mor-
bidity or mortality. Finally, the sample size was
small in certain subgroups, particularly in the
subgroup of young children, which resulted in
wide confidence intervals and point estimates
that should be interpreted with caution.
In conclusion, severe obesity in children and
young adults is associated with a high prevalence
of abnormal levels of cardiometabolic risk-factor
variables. The prevalence of these abnormal val-
ues among children and young adults appears to
be dependent on both age and severity of obe-
sity. The inclusion of class II obesity in the stan-
dard obesity classification may assist in the iden-
tification of children who could be at the greatest
risk for abnormal levels of HDL cholesterol, sys-
tolic blood pressure, and glucose, and the inclu-
sion of class III obesity in the standard obesity
classification may assist in the identification of
those at the greatest risk for abnormal levels of
triglycerides, diastolic blood pressure, and glycat-
ed hemoglobin.
Disclosure forms provided by the authors are available with
the full text of this article at NEJM.org.
References
1. Skinner AC, Skelton JA. Prevalence
and trends in obesity and severe obesity
among children in the United States,
1999-2012. JAMA Pediatr 2014; 168: 561-6.
2. Skelton JA, Cook SR, Auinger P, Klein
JD, Barlow SE. Prevalence and trends of
severe obesity among US children and
adolescents. Acad Pediatr 2009; 9: 322-9.
3. Skinner AC, Mayer ML, Flower K,
Weinberger M. Health status and health
care expenditures in a nationally repre-
sentative sample: how do overweight and
healthy-weight children compare? Pediat-
rics 2008; 121(2): e269-e277.
4. Kelly AS, Barlow SE, Rao G, et al. Se-
vere obesity in children and adolescents:
identification, associated health risks,
and treatment approaches: a scientific
statement from the American Heart As-
sociation. Circulation 2013; 128: 1689-712.
5. National Center for Health Statistics.
National Health and Nutrition Examination
Survey 1999–2014 survey content brochure
(http://www .cdc .gov/ nchs/ data/ nhanes/
survey_content_99_14 .pdf).
6. Centers for Disease Control and Pre-
vention. A SAS program for the 2000
CDC growth charts: (ages 0 to <20 years).
2011 (http://www .cdc .gov/ nccdphp/ dnpao/
growthcharts/ resources/ sas .htm).
7. Barlow SE. Expert committee recom-
mendations regarding the prevention, as-
sessment, and treatment of child and ado-
lescent overweight and obesity: summary
report. Pediatrics 2007; 120: Suppl 4: S164-
S192.
8. Flegal KM, Wei R, Ogden CL, Freed-
man DS, Johnson CL, Curtin LR. Charac-
terizing extreme values of body mass
index-for-age by using the 2000 Centers
for Disease Control and Prevention growth
charts. Am J Clin Nutr 2009; 90: 1314-20.
9. Berrington de Gonzalez A, Hartge P,
Cerhan JR, et al. Body-mass index and
mortality among 1.46 million white
adults. N Engl J Med 2010; 363: 2211-9.
10. Expert Panel on Integrated Guidelines
for Cardiovascular Health and Risk Re-
duction in Children and Adolescents, Na-
tional Heart, Lung, and Blood Institute.
Expert panel on integrated guidelines for
cardiovascular health and risk reduction in
children and adolescents: summary report.
Pediatrics 2011; 128: Suppl 5: S213-S256.
11. Daniels SR, Greer FR. Lipid screening
and cardiovascular health in childhood.
Pediatrics 2008; 122: 198-208.
12.Kavey RE, Daniels SR, Lauer RM,
Atkins DL, Hayman LL, Taubert K.
American Heart Association guidelines
for primary prevention of atherosclerotic
cardiovascular disease beginning in child-
hood. Circulation 2003; 107: 1562-6.
13. National High Blood Pressure Educa-
tion Program Working Group on High
Blood Pressure in Children and Adoles-
cents. The fourth report on the diagnosis,
evaluation, and treatment of high blood
pressure in children and adolescents. Pe-
diatrics 2004; 114: Suppl 2: 555-76.
14. Chobanian AV, Bakris GL, Black HR,
et al. The seventh report of the Joint Na-
tional Committee on Prevention, Detec-
tion, Evaluation, and Treatment of High
Blood Pressure: the JNC 7 report. JAMA
2003; 289: 2560-72.
15. American Diabetes Association. Diag-
nosis and classification of diabetes melli-
tus. Diabetes Care 2014; 37: Suppl 1: S81-S90.
16. Centers for Disease Control and Preven-
tion. National Health and Nutrition Exami-
nation Survey (NHANES) laboratory proce-
dures manual 2011 (http://www .cdc .gov/
nchs/ data/ nhanes/ nhanes_11_12/ 2011-12_
Laboratory_Procedures_Manual .pdf).
17.Steiner MJ, Skinner AC, Perrin EM.
Fasting might not be necessary before
lipid screening: a nationally representative
cross-sectional study. Pediatrics 2011; 128:
463-70.
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
T h en e w e ngl a nd j o u r na lo f m e dic i n e
increased costs believed to stem from the evalu-
ation and treatment of coexisting conditions34
;
an improved estimation of risk that is based on
obesity severity could lower the costs of evalua-
tion without resulting in missed diagnoses of co-
existing conditions. Children with severe obesity
already have increased cardiometabolic risk, which
may predict the early onset of serious diseases
such as hypertension and diabetes.
As older adolescents transition to young
adulthood, the recognition that teens with obe-
sity have increased cardiometabolic risk will be
important. Current treatment approaches are
not as effective at higher levels of obesity than
they are at lower levels of obesity.35-37The find-
ings in our study, when considered in the con-
text of the negative effect that these risk factors
have on subsequent quality of life,38 imply a
need for the early identification of abnormal
weight gain, primary and secondary prevention
of obesity, and systemwide policy changes in
the evaluation and management of obesity in
health care.39
We examined a range of cardiometabolic risk-
factor variables in a large and nationally repre-
sentative population; however, our study has cer-
tain methodologic limitations. First, because this
is a cross-sectional study, we could not show
causality between obesity and risk factors. Sec-
ond, although we used standard definitions of
abnormal values for risk-factor variables, the cross-
sectional design did not allow us to examine the
effects of these abnormal values on future mor-
bidity or mortality. Finally, the sample size was
small in certain subgroups, particularly in the
subgroup of young children, which resulted in
wide confidence intervals and point estimates
that should be interpreted with caution.
In conclusion, severe obesity in children and
young adults is associated with a high prevalence
of abnormal levels of cardiometabolic risk-factor
variables. The prevalence of these abnormal val-
ues among children and young adults appears to
be dependent on both age and severity of obe-
sity. The inclusion of class II obesity in the stan-
dard obesity classification may assist in the iden-
tification of children who could be at the greatest
risk for abnormal levels of HDL cholesterol, sys-
tolic blood pressure, and glucose, and the inclu-
sion of class III obesity in the standard obesity
classification may assist in the identification of
those at the greatest risk for abnormal levels of
triglycerides, diastolic blood pressure, and glycat-
ed hemoglobin.
Disclosure forms provided by the authors are available with
the full text of this article at NEJM.org.
References
1. Skinner AC, Skelton JA. Prevalence
and trends in obesity and severe obesity
among children in the United States,
1999-2012. JAMA Pediatr 2014; 168: 561-6.
2. Skelton JA, Cook SR, Auinger P, Klein
JD, Barlow SE. Prevalence and trends of
severe obesity among US children and
adolescents. Acad Pediatr 2009; 9: 322-9.
3. Skinner AC, Mayer ML, Flower K,
Weinberger M. Health status and health
care expenditures in a nationally repre-
sentative sample: how do overweight and
healthy-weight children compare? Pediat-
rics 2008; 121(2): e269-e277.
4. Kelly AS, Barlow SE, Rao G, et al. Se-
vere obesity in children and adolescents:
identification, associated health risks,
and treatment approaches: a scientific
statement from the American Heart As-
sociation. Circulation 2013; 128: 1689-712.
5. National Center for Health Statistics.
National Health and Nutrition Examination
Survey 1999–2014 survey content brochure
(http://www .cdc .gov/ nchs/ data/ nhanes/
survey_content_99_14 .pdf).
6. Centers for Disease Control and Pre-
vention. A SAS program for the 2000
CDC growth charts: (ages 0 to <20 years).
2011 (http://www .cdc .gov/ nccdphp/ dnpao/
growthcharts/ resources/ sas .htm).
7. Barlow SE. Expert committee recom-
mendations regarding the prevention, as-
sessment, and treatment of child and ado-
lescent overweight and obesity: summary
report. Pediatrics 2007; 120: Suppl 4: S164-
S192.
8. Flegal KM, Wei R, Ogden CL, Freed-
man DS, Johnson CL, Curtin LR. Charac-
terizing extreme values of body mass
index-for-age by using the 2000 Centers
for Disease Control and Prevention growth
charts. Am J Clin Nutr 2009; 90: 1314-20.
9. Berrington de Gonzalez A, Hartge P,
Cerhan JR, et al. Body-mass index and
mortality among 1.46 million white
adults. N Engl J Med 2010; 363: 2211-9.
10. Expert Panel on Integrated Guidelines
for Cardiovascular Health and Risk Re-
duction in Children and Adolescents, Na-
tional Heart, Lung, and Blood Institute.
Expert panel on integrated guidelines for
cardiovascular health and risk reduction in
children and adolescents: summary report.
Pediatrics 2011; 128: Suppl 5: S213-S256.
11. Daniels SR, Greer FR. Lipid screening
and cardiovascular health in childhood.
Pediatrics 2008; 122: 198-208.
12.Kavey RE, Daniels SR, Lauer RM,
Atkins DL, Hayman LL, Taubert K.
American Heart Association guidelines
for primary prevention of atherosclerotic
cardiovascular disease beginning in child-
hood. Circulation 2003; 107: 1562-6.
13. National High Blood Pressure Educa-
tion Program Working Group on High
Blood Pressure in Children and Adoles-
cents. The fourth report on the diagnosis,
evaluation, and treatment of high blood
pressure in children and adolescents. Pe-
diatrics 2004; 114: Suppl 2: 555-76.
14. Chobanian AV, Bakris GL, Black HR,
et al. The seventh report of the Joint Na-
tional Committee on Prevention, Detec-
tion, Evaluation, and Treatment of High
Blood Pressure: the JNC 7 report. JAMA
2003; 289: 2560-72.
15. American Diabetes Association. Diag-
nosis and classification of diabetes melli-
tus. Diabetes Care 2014; 37: Suppl 1: S81-S90.
16. Centers for Disease Control and Preven-
tion. National Health and Nutrition Exami-
nation Survey (NHANES) laboratory proce-
dures manual 2011 (http://www .cdc .gov/
nchs/ data/ nhanes/ nhanes_11_12/ 2011-12_
Laboratory_Procedures_Manual .pdf).
17.Steiner MJ, Skinner AC, Perrin EM.
Fasting might not be necessary before
lipid screening: a nationally representative
cross-sectional study. Pediatrics 2011; 128:
463-70.
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
n engl j med 373;14nejm.org October 1, 2015 1317
Cardiometabolic Risks and Obesity Severity in Children
18.Johnson CL, Paulose-Ram R, Ogden
CL, et al. National Health and Nutrition
Examination Survey: analytic guidelines,
1999-2010. Vital Health Stat 2 2013; 161:
1-24.
19. Centers for Disease Control and Pre-
vention. National Health and Nutrition
Examination Survey: analytic guidelines,
2011-2012.2013 (http://www .cdc .gov/
nchs/ data/ nhanes/ analytic_guidelines_11
_12 .pdf).
20.Kit BK, Kuklina E, Carroll MD,
Ostchega Y, Freedman DS, Ogden CL.
Prevalence of and trends in dyslipidemia
and blood pressure among US children
and adolescents, 1999-2012. JAMA Pedi-
atr 2015; 169: 272-9.
21.Krebs NF, Himes JH, Jacobson D,
Nicklas TA, Guilday P, Styne D. Assess-
ment of child and adolescent overweight
and obesity. Pediatrics 2007; 120: Suppl 4:
S193-S228.
22.Freedman DS, Mei Z, Srinivasan SR,
Berenson GS, Dietz WH. Cardiovascular
risk factors and excess adiposity among
overweight children and adolescents: the
Bogalusa Heart Study. J Pediatr 2007;
150(1): 12.e2-17.e2.
23.Freedman DS, Dietz WH, Srinivasan
SR, Berenson GS. The relation of over-
weight to cardiovascularrisk factors
among children and adolescents: the Bo-
galusa Heart Study. Pediatrics 1999; 103:
1175-82.
24.Lambert M, Delvin EE, Levy E, et al.
Prevalence of cardiometabolic risk fac-
tors by weight status in a population-
based sample of Quebec children and
adolescents. Can J Cardiol 2008; 24: 575-
83.
25.Field AE, Cook NR, Gillman MW.
Weight status in childhood as a predictor
of becoming overweight or hypertensive in
early adulthood. Obes Res 2005; 13: 163-9.
26.Guo SS, Wu W, Chumlea WC, Roche
AF. Predicting overweight and obesity in
adulthood from body mass index values
in childhood and adolescence. Am J Clin
Nutr 2002; 76: 653-8.
27.EngelandA, Bjørge T, TverdalA,
Søgaard AJ. Obesity in adolescence and
adulthood and the risk of adult mortality.
Epidemiology 2004; 15: 79-85.
28.Franks PW, Hanson RL, Knowler WC,
SieversML, BennettPH, Looker HC.
Childhood obesity, other cardiovascular
risk factors, and premature death. N Engl
J Med 2010; 362: 485-93.
29.Inge TH, King WC, Jenkins TM, et al.
The effect of obesity in adolescence on
adult health status. Pediatrics 2013; 132:
1098-104.
30.Whitlock EP, O’Connor EA, Williams
SB, Beil TL, Lutz KW. Effectiveness of
weight management interventions in chil-
dren: a targeted systematic review for the
USPSTF. Pediatrics 2010; 125(2): e396-e418.
31. Children’s Hospital Association.
Obesity services: 2013 survey findings
of children’s hospitals (https:/ / www
.childrenshospitals .org/ ~/ media/ Files/
CHA/ Main/ Issues_and_Advocacy/ Key
_Issues/ Child_Health/ Obesity/ 2013_survey
_findings_obesity_services_report
_050114 .pdf).
32.Finkelstein EA, Trogdon JG, Brown
DS, Allaire BT, Dellea PS, Kamal-Bahl SJ.
The lifetime medical cost burden of over-
weight and obesity: implications for obe-
sity prevention. Obesity (Silver Spring)
2008; 16: 1843-8.
33. Wang YC, McPherson K, Marsh T,
Gortmaker SL, Brown M. Health and eco-
nomic burden of the projected obesity
trends in the USA and the UK. Lancet
2011; 378: 815-25.
34.Trasande L, Chatterjee S. The impact
of obesity on health service utilization
and costs in childhood. Obesity (Silver
Spring) 2009; 17: 1749-54.
35. Johnston CA, Tyler C, Palcic JL, Stans-
berry SA, Gallagher MR, Foreyt JP. Small-
er weight changes in standardized body
mass index in response to treatment as
weight classification increases. J Pediatr
2011; 158: 624-7.
36.Kalarchian MA, Levine MD, Arslanian
SA, et al. Family-based treatment of se-
vere pediatric obesity: randomized, con-
trolled trial. Pediatrics 2009; 124: 1060-8.
37.Danielsson P, Kowalski J, Ekblom Ö,
Marcus C. Response of severely obese
children and adolescents to behavioral
treatment. Arch Pediatr Adolesc Med
2012; 166: 1103-8.
38.Schwimmer JB, Burwinkle TM, Varni
JW. Health-related quality of life of se-
verely obese children and adolescents.
JAMA 2003; 289: 1813-9.
39. Dietz WH, Baur LA, Hall K, et al. Man-
agementof obesity:improvementof
health-care training and systems for pre-
vention and care. Lancet 2015; 385: 2521-33.
Copyright © 2015 Massachusetts Medical Society.
posting presentations from medical meetings online
Online posting of an audio or video recording of an oral presentation at
a medical meeting, with selected slides from the presentation, is not considered
prior publication. Authors should feel free to call or send e-mail to the
Journal’s Editorial Offices if there are any questions about this policy.
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
Cardiometabolic Risks and Obesity Severity in Children
18.Johnson CL, Paulose-Ram R, Ogden
CL, et al. National Health and Nutrition
Examination Survey: analytic guidelines,
1999-2010. Vital Health Stat 2 2013; 161:
1-24.
19. Centers for Disease Control and Pre-
vention. National Health and Nutrition
Examination Survey: analytic guidelines,
2011-2012.2013 (http://www .cdc .gov/
nchs/ data/ nhanes/ analytic_guidelines_11
_12 .pdf).
20.Kit BK, Kuklina E, Carroll MD,
Ostchega Y, Freedman DS, Ogden CL.
Prevalence of and trends in dyslipidemia
and blood pressure among US children
and adolescents, 1999-2012. JAMA Pedi-
atr 2015; 169: 272-9.
21.Krebs NF, Himes JH, Jacobson D,
Nicklas TA, Guilday P, Styne D. Assess-
ment of child and adolescent overweight
and obesity. Pediatrics 2007; 120: Suppl 4:
S193-S228.
22.Freedman DS, Mei Z, Srinivasan SR,
Berenson GS, Dietz WH. Cardiovascular
risk factors and excess adiposity among
overweight children and adolescents: the
Bogalusa Heart Study. J Pediatr 2007;
150(1): 12.e2-17.e2.
23.Freedman DS, Dietz WH, Srinivasan
SR, Berenson GS. The relation of over-
weight to cardiovascularrisk factors
among children and adolescents: the Bo-
galusa Heart Study. Pediatrics 1999; 103:
1175-82.
24.Lambert M, Delvin EE, Levy E, et al.
Prevalence of cardiometabolic risk fac-
tors by weight status in a population-
based sample of Quebec children and
adolescents. Can J Cardiol 2008; 24: 575-
83.
25.Field AE, Cook NR, Gillman MW.
Weight status in childhood as a predictor
of becoming overweight or hypertensive in
early adulthood. Obes Res 2005; 13: 163-9.
26.Guo SS, Wu W, Chumlea WC, Roche
AF. Predicting overweight and obesity in
adulthood from body mass index values
in childhood and adolescence. Am J Clin
Nutr 2002; 76: 653-8.
27.EngelandA, Bjørge T, TverdalA,
Søgaard AJ. Obesity in adolescence and
adulthood and the risk of adult mortality.
Epidemiology 2004; 15: 79-85.
28.Franks PW, Hanson RL, Knowler WC,
SieversML, BennettPH, Looker HC.
Childhood obesity, other cardiovascular
risk factors, and premature death. N Engl
J Med 2010; 362: 485-93.
29.Inge TH, King WC, Jenkins TM, et al.
The effect of obesity in adolescence on
adult health status. Pediatrics 2013; 132:
1098-104.
30.Whitlock EP, O’Connor EA, Williams
SB, Beil TL, Lutz KW. Effectiveness of
weight management interventions in chil-
dren: a targeted systematic review for the
USPSTF. Pediatrics 2010; 125(2): e396-e418.
31. Children’s Hospital Association.
Obesity services: 2013 survey findings
of children’s hospitals (https:/ / www
.childrenshospitals .org/ ~/ media/ Files/
CHA/ Main/ Issues_and_Advocacy/ Key
_Issues/ Child_Health/ Obesity/ 2013_survey
_findings_obesity_services_report
_050114 .pdf).
32.Finkelstein EA, Trogdon JG, Brown
DS, Allaire BT, Dellea PS, Kamal-Bahl SJ.
The lifetime medical cost burden of over-
weight and obesity: implications for obe-
sity prevention. Obesity (Silver Spring)
2008; 16: 1843-8.
33. Wang YC, McPherson K, Marsh T,
Gortmaker SL, Brown M. Health and eco-
nomic burden of the projected obesity
trends in the USA and the UK. Lancet
2011; 378: 815-25.
34.Trasande L, Chatterjee S. The impact
of obesity on health service utilization
and costs in childhood. Obesity (Silver
Spring) 2009; 17: 1749-54.
35. Johnston CA, Tyler C, Palcic JL, Stans-
berry SA, Gallagher MR, Foreyt JP. Small-
er weight changes in standardized body
mass index in response to treatment as
weight classification increases. J Pediatr
2011; 158: 624-7.
36.Kalarchian MA, Levine MD, Arslanian
SA, et al. Family-based treatment of se-
vere pediatric obesity: randomized, con-
trolled trial. Pediatrics 2009; 124: 1060-8.
37.Danielsson P, Kowalski J, Ekblom Ö,
Marcus C. Response of severely obese
children and adolescents to behavioral
treatment. Arch Pediatr Adolesc Med
2012; 166: 1103-8.
38.Schwimmer JB, Burwinkle TM, Varni
JW. Health-related quality of life of se-
verely obese children and adolescents.
JAMA 2003; 289: 1813-9.
39. Dietz WH, Baur LA, Hall K, et al. Man-
agementof obesity:improvementof
health-care training and systems for pre-
vention and care. Lancet 2015; 385: 2521-33.
Copyright © 2015 Massachusetts Medical Society.
posting presentations from medical meetings online
Online posting of an audio or video recording of an oral presentation at
a medical meeting, with selected slides from the presentation, is not considered
prior publication. Authors should feel free to call or send e-mail to the
Journal’s Editorial Offices if there are any questions about this policy.
The New England Journal of Medicine
Downloaded from nejm.org on May 24, 2018. For personal use only. No other uses without permission.
Copyright © 2015 Massachusetts Medical Society. All rights reserved.
1 out of 11
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.