CVD Risk Factors: Income & Education
VerifiedAdded on 2020/04/13
|23
|4540
|370
AI Summary
This assignment analyzes the relationship between cardiovascular disease (CVD) and two key social determinants of health: income and education. It utilizes data from Statistics Canada's Canadian Community Health Survey to illustrate how these factors influence CVD prevalence among older adults. The analysis involves comparing rates of CVD across different income levels and educational qualifications, highlighting potential disparities. The assignment also references the World Health Organization's Social Determinants of Health model to provide a broader context for understanding the complex interplay between social factors and health outcomes.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 1
Cardiovascular Disease and Social Determinants
Name
Institution
Cardiovascular Disease and Social Determinants
Name
Institution
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 2
The Impacts of the Social Determinants of Health on Cardiovascular Disease in Older
Adults
Nearly six percent of Canadians were living with cardiovascular disease (CVD) in 2015;
a disease which has a mortality rate of 194.7 deaths per 100,000 (Public Health Agency of
Canada, 2017b). Older adults are one of many vulnerable populations in Canada and there are a
variety of factors that make them more vulnerable. This paper will explore how social
determinants of health (SDOH), specifically socioeconomic status, affects Canadian and
international multicultural older adult populations with (CVD), include a SDOH model, followed
by public health implications that arise as a result of this issue. We will examine why these
socioeconomic status may affect this vulnerable population and explore information about CVD.
For the purposes of this research, older adults are defined as individuals between the ages
of 55 and 79. According to Raphael (2016), there are many factors that make senior populations
more vulnerable or susceptible to higher mortality rates; those including, but are not limited to
SDOH such as personal health practices/coping, education, socioeconomic status (SES), gender,
and social support systems. When examining the rates of CVD in older adults a comparison will
be made between those of low and high SES. SES will be measured using household income and
The Impacts of the Social Determinants of Health on Cardiovascular Disease in Older
Adults
Nearly six percent of Canadians were living with cardiovascular disease (CVD) in 2015;
a disease which has a mortality rate of 194.7 deaths per 100,000 (Public Health Agency of
Canada, 2017b). Older adults are one of many vulnerable populations in Canada and there are a
variety of factors that make them more vulnerable. This paper will explore how social
determinants of health (SDOH), specifically socioeconomic status, affects Canadian and
international multicultural older adult populations with (CVD), include a SDOH model, followed
by public health implications that arise as a result of this issue. We will examine why these
socioeconomic status may affect this vulnerable population and explore information about CVD.
For the purposes of this research, older adults are defined as individuals between the ages
of 55 and 79. According to Raphael (2016), there are many factors that make senior populations
more vulnerable or susceptible to higher mortality rates; those including, but are not limited to
SDOH such as personal health practices/coping, education, socioeconomic status (SES), gender,
and social support systems. When examining the rates of CVD in older adults a comparison will
be made between those of low and high SES. SES will be measured using household income and
CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 3
level of education. The writers of this paper believe that older adults that have a lower level of
education will have a higher rate of CVD disease due to diminished access or knowledge to
support and foundations to live or obtain a better quality of lifestyle. The writers also believe that
along with a lower level of education would contribute to a lower level of income, thus putting
older adults in a position to not obtain a healthier lifestyle and higher quality of living.
Cardiovascular diseases affect the heart and blood vessels and includes coronary heart
disease, cerebrovascular disease, peripheral arterial disease, rheumatic heart disease, congenital
heart disease, deep vein thrombosis and pulmonary embolism (World Health Organization,
2017). CVD is a rampant problem for developing nations and is the number one cause of death
worldwide (World Health Organization, 2017). According to the Canadian Chronic Disease
Surveillance System (CCDSS) incident rates of heart attacks in the Canadian population for age
groups, 50 - 64 and 65-79 are 2.38% and 5.55%, respectively (Public Health Agency of Canada,
2017c). This is much higher than age groups 35 - 49, who were 0.61% of the population that
experience heart attacks (Public Health Agency of Canada, 2017c). In the United States, 69.1%
of men and 67.9% of women aged 60 - 79 suffer from some form of CVD (American Heart
Association, 2016). Diseases of the heart are the lead cause of death for American women over
65 years old (American Heart Association, 2016).
CVD is commonly diagnosed by a physician in regular or emergency room visits. Data is
then collected through a variety of sampling methods. Specifically, the CCDSS collects data
based on health insurance registry databases that are linked to physician billing and hospital
level of education. The writers of this paper believe that older adults that have a lower level of
education will have a higher rate of CVD disease due to diminished access or knowledge to
support and foundations to live or obtain a better quality of lifestyle. The writers also believe that
along with a lower level of education would contribute to a lower level of income, thus putting
older adults in a position to not obtain a healthier lifestyle and higher quality of living.
Cardiovascular diseases affect the heart and blood vessels and includes coronary heart
disease, cerebrovascular disease, peripheral arterial disease, rheumatic heart disease, congenital
heart disease, deep vein thrombosis and pulmonary embolism (World Health Organization,
2017). CVD is a rampant problem for developing nations and is the number one cause of death
worldwide (World Health Organization, 2017). According to the Canadian Chronic Disease
Surveillance System (CCDSS) incident rates of heart attacks in the Canadian population for age
groups, 50 - 64 and 65-79 are 2.38% and 5.55%, respectively (Public Health Agency of Canada,
2017c). This is much higher than age groups 35 - 49, who were 0.61% of the population that
experience heart attacks (Public Health Agency of Canada, 2017c). In the United States, 69.1%
of men and 67.9% of women aged 60 - 79 suffer from some form of CVD (American Heart
Association, 2016). Diseases of the heart are the lead cause of death for American women over
65 years old (American Heart Association, 2016).
CVD is commonly diagnosed by a physician in regular or emergency room visits. Data is
then collected through a variety of sampling methods. Specifically, the CCDSS collects data
based on health insurance registry databases that are linked to physician billing and hospital
CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 4
databases (Public Health Agency of Canada, 2017a). Through this collection technique, errors
from self-reporting are avoided. Another common information data base is the Canadian
Community Health Survey (CCHS). A survey is provided to a cross-section of the country who
then are responsible for self-reporting (Statistics Canada, 2016). When self-reporting is used for
collecting information there is always a chance that respondents will be intentionally dishonest
or misunderstand a question and provide the wrong answer.
SES and education are SDOH that are the strongest predictors to affect CVD (Joffres et
al., 2013; Winkleby et al., 1992). SES reflects spending ability, housing, diet, and medical care
based on income, whereas education reflects skills for social, psychological, and economic
resources (Winkleby et al., 1992).
A healthy diet is essential for the prevention of CVD yet income can be a stumbling block as
much of heart disease medication costs are not covered under Medicare (Gucciardi et al., 2009).
Those with low income tend to lack insurance coverage that covers expensive medications such
as those for CVD, which are among the most expensive within Canada (Booth et al., 2012;
Campbell et al., 2012). Booth et al. (2012) found an increase in diabetes related mortality rates
between those of high and low SES especially in those over the age of 65. Woodward et al.
(2015) revealed that CVD is associated with lower SES. A community-based study from Turkey
revealed that unhealthy diet was associated with lower SES (OR = 3.31) and lower education
(OR=4.48) (Simsek et al., 2013).
databases (Public Health Agency of Canada, 2017a). Through this collection technique, errors
from self-reporting are avoided. Another common information data base is the Canadian
Community Health Survey (CCHS). A survey is provided to a cross-section of the country who
then are responsible for self-reporting (Statistics Canada, 2016). When self-reporting is used for
collecting information there is always a chance that respondents will be intentionally dishonest
or misunderstand a question and provide the wrong answer.
SES and education are SDOH that are the strongest predictors to affect CVD (Joffres et
al., 2013; Winkleby et al., 1992). SES reflects spending ability, housing, diet, and medical care
based on income, whereas education reflects skills for social, psychological, and economic
resources (Winkleby et al., 1992).
A healthy diet is essential for the prevention of CVD yet income can be a stumbling block as
much of heart disease medication costs are not covered under Medicare (Gucciardi et al., 2009).
Those with low income tend to lack insurance coverage that covers expensive medications such
as those for CVD, which are among the most expensive within Canada (Booth et al., 2012;
Campbell et al., 2012). Booth et al. (2012) found an increase in diabetes related mortality rates
between those of high and low SES especially in those over the age of 65. Woodward et al.
(2015) revealed that CVD is associated with lower SES. A community-based study from Turkey
revealed that unhealthy diet was associated with lower SES (OR = 3.31) and lower education
(OR=4.48) (Simsek et al., 2013).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 5
A lack of education can have profound effects in those with CVD. In developing countries, there
is often a gap in hypertension treatment for seniors due to lack of knowledge of what
hypertension is and preventative signs (Maurer & Ramos, 2015). Maurer & Ramos (2015) reveal
that low-cost treatment options for hypertension exist and could increase awareness in seniors.
Seniors of higher SES are associated with higher physical activity, greater nutritional habits and
lower risk of smoking compared to those of lower SES (Campbell et al., 2012). This means that
those of low SES are associated with increased use of healthcare services that have little impact
on poorer health outcomes and mortality (Campbell et al., 2012).
It's important to assess how determinants are measured. The studies referenced in this paper
directly evaluated income, education and CVD data utilizing census reports, self-reporting data
and medical records.
SES was measured using household income and level of education, any additional information
on education, income, and occupation was ascertained through questionnaires. For example, one
study measured income using the "median household income level of an individual’s
neighborhood of residence on 1, April, 2002 from the 2001 Canadian Census. Neighborhoods
were defined using small geographic units (dissemination areas) from Statistics Canada" (Booth
et al., 2012).
Woodward et al. (2015) measured education by using self-reported data, falling into one of three
groups. Group one had no completed education or completed only primary school. Group two
A lack of education can have profound effects in those with CVD. In developing countries, there
is often a gap in hypertension treatment for seniors due to lack of knowledge of what
hypertension is and preventative signs (Maurer & Ramos, 2015). Maurer & Ramos (2015) reveal
that low-cost treatment options for hypertension exist and could increase awareness in seniors.
Seniors of higher SES are associated with higher physical activity, greater nutritional habits and
lower risk of smoking compared to those of lower SES (Campbell et al., 2012). This means that
those of low SES are associated with increased use of healthcare services that have little impact
on poorer health outcomes and mortality (Campbell et al., 2012).
It's important to assess how determinants are measured. The studies referenced in this paper
directly evaluated income, education and CVD data utilizing census reports, self-reporting data
and medical records.
SES was measured using household income and level of education, any additional information
on education, income, and occupation was ascertained through questionnaires. For example, one
study measured income using the "median household income level of an individual’s
neighborhood of residence on 1, April, 2002 from the 2001 Canadian Census. Neighborhoods
were defined using small geographic units (dissemination areas) from Statistics Canada" (Booth
et al., 2012).
Woodward et al. (2015) measured education by using self-reported data, falling into one of three
groups. Group one had no completed education or completed only primary school. Group two
CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 6
composed of people who completed secondary school; and lastly group three completed tertiary
education (university or college).
Booth et al. (2012) recorded "baseline CVD, acute myocardial infarction, and stroke, based on
relevant diagnostic codes from hospital discharge records. Co-morbidity was captured using
diagnostic codes listed in hospital records and physicians’ service claims from the year prior to
baseline to create distinct case-mix categories based on the Johns Hopkins Adjusted Clinical
Groups case-mix system."
If blood pressure and cholesterol levels were used to determine CVD risk, they were obtained
using standard protocols as in Woodward et al. (2015) and Winkleby et al., (1992).
Specific Canadian Data
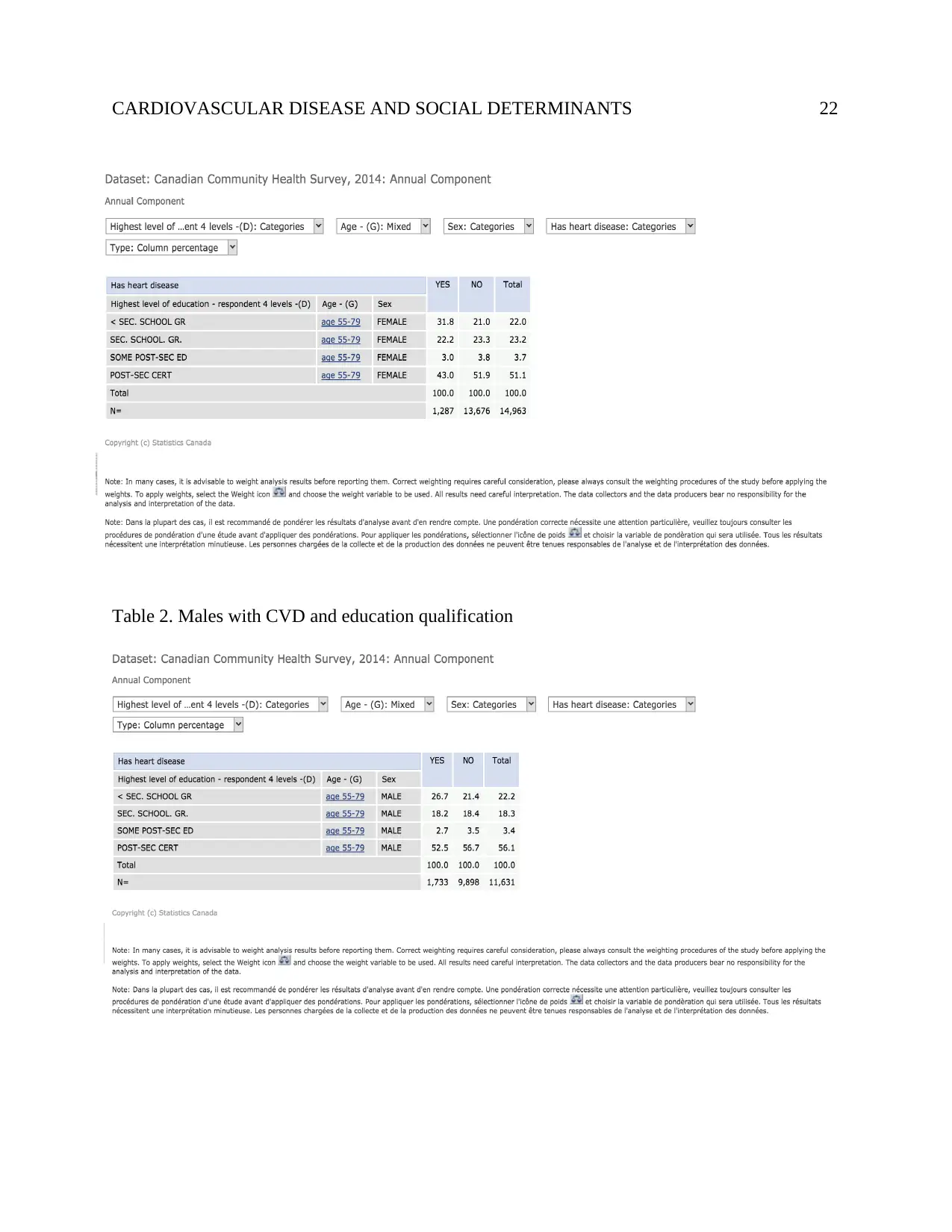
The CCHS is a cross-sectional study in Canada that measures rates of different health
outcomes in the country. The most recent complete survey data is from 2014. Based on the
survey design, the most efficient way to access the rates of CVD was by studying those who self-
reported having heart disease. Data was collected for those with heart disease and was then
compared to level of education and to person income. Only the data for those aged 55 to 79 was
analyzed.
When studying the rates of heart disease in both older adult males and females it was
noted that the highest rates were in those that had completed post-secondary education followed
secondly by those who had not completed secondary education (Statistics Canada, 2016). It is
likely that there are confounding factors that create the high rates of heart disease in those with
composed of people who completed secondary school; and lastly group three completed tertiary
education (university or college).
Booth et al. (2012) recorded "baseline CVD, acute myocardial infarction, and stroke, based on
relevant diagnostic codes from hospital discharge records. Co-morbidity was captured using
diagnostic codes listed in hospital records and physicians’ service claims from the year prior to
baseline to create distinct case-mix categories based on the Johns Hopkins Adjusted Clinical
Groups case-mix system."
If blood pressure and cholesterol levels were used to determine CVD risk, they were obtained
using standard protocols as in Woodward et al. (2015) and Winkleby et al., (1992).
Specific Canadian Data
The CCHS is a cross-sectional study in Canada that measures rates of different health
outcomes in the country. The most recent complete survey data is from 2014. Based on the
survey design, the most efficient way to access the rates of CVD was by studying those who self-
reported having heart disease. Data was collected for those with heart disease and was then
compared to level of education and to person income. Only the data for those aged 55 to 79 was
analyzed.
When studying the rates of heart disease in both older adult males and females it was
noted that the highest rates were in those that had completed post-secondary education followed
secondly by those who had not completed secondary education (Statistics Canada, 2016). It is
likely that there are confounding factors that create the high rates of heart disease in those with
CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 7
the highest education level. In males, 26.7% of heart disease occurs in those with less than
secondary education, 18.2% in those who had completed secondary education, and only 2.7% of
those who had completed some post-secondary education (Statistics Canada, 2016). Similarly for
females, 31.8% of heart disease occurs in those with less than secondary education, 22.2% in
those who had completed secondary education, and only 3.0% of those who had completed some
post-secondary education (Statistics Canada, 2016). This data shows that to a certain extent, an
increase in education is correlated with a decrease in heart disease.
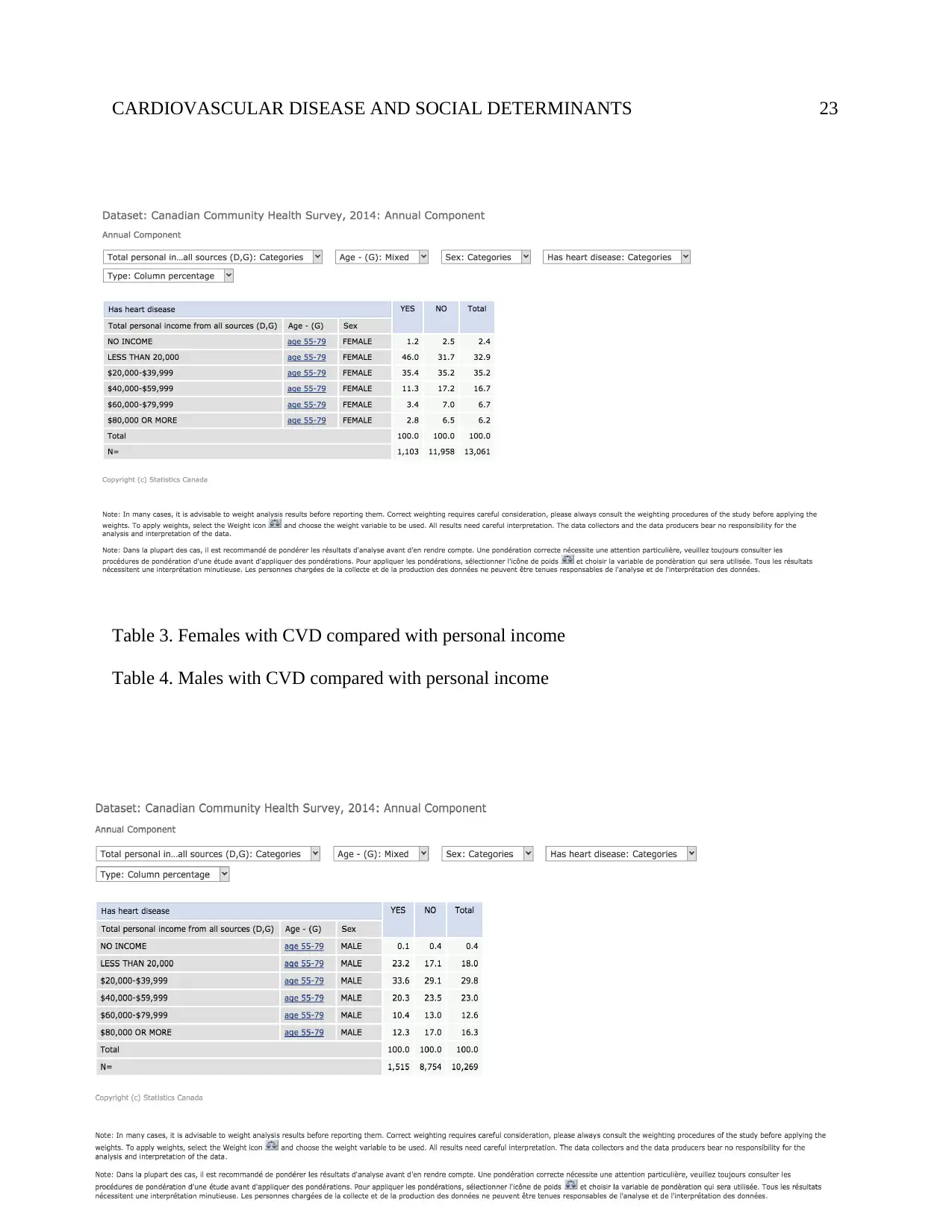
When comparing rates of heart disease to income levels it is found that those with
income rates less than $20,000 to $39,999 had significantly greater rates of heart disease
(Statistics Canada, 2016). For males, 23.2% of all heart disease occurs in those with less than
$20,000 income and 33.6% occurs among those with $20,000 to $39,000 income (Statistics
Canada, 2016). In females, 46% of all heart disease occurs in those with less than $20,000
income and 35.4% occurs among those with $20,000 to $39,000 income (Statistics Canada,
2016). In both male and female populations the rates continue to drop as income rises with rates
in the final category, income greater than $80,000, at 12.3% for males and 2.8% for females
(Statistics Canada, 2016). A very clear correlation can be noted between that of low income and
heart disease.
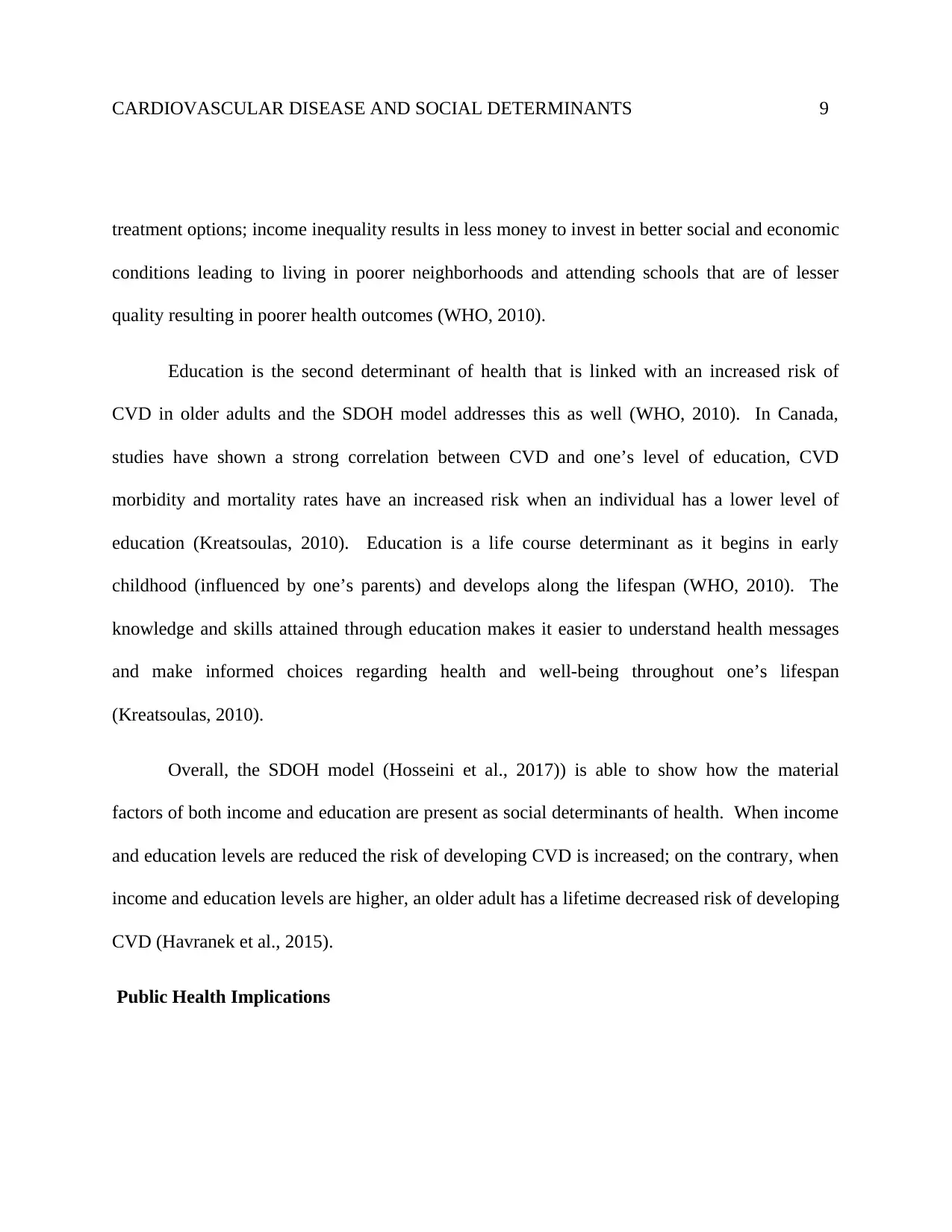
The Social Determinants of Health Model
The social determinants of health (SDOH) model (WHO, 2010) is the conceptual model
(refer to Appendix A) used to show how political, social and economic mechanisms strongly
the highest education level. In males, 26.7% of heart disease occurs in those with less than
secondary education, 18.2% in those who had completed secondary education, and only 2.7% of
those who had completed some post-secondary education (Statistics Canada, 2016). Similarly for
females, 31.8% of heart disease occurs in those with less than secondary education, 22.2% in
those who had completed secondary education, and only 3.0% of those who had completed some
post-secondary education (Statistics Canada, 2016). This data shows that to a certain extent, an
increase in education is correlated with a decrease in heart disease.
When comparing rates of heart disease to income levels it is found that those with
income rates less than $20,000 to $39,999 had significantly greater rates of heart disease
(Statistics Canada, 2016). For males, 23.2% of all heart disease occurs in those with less than
$20,000 income and 33.6% occurs among those with $20,000 to $39,000 income (Statistics
Canada, 2016). In females, 46% of all heart disease occurs in those with less than $20,000
income and 35.4% occurs among those with $20,000 to $39,000 income (Statistics Canada,
2016). In both male and female populations the rates continue to drop as income rises with rates
in the final category, income greater than $80,000, at 12.3% for males and 2.8% for females
(Statistics Canada, 2016). A very clear correlation can be noted between that of low income and
heart disease.
The Social Determinants of Health Model
The social determinants of health (SDOH) model (WHO, 2010) is the conceptual model
(refer to Appendix A) used to show how political, social and economic mechanisms strongly
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 8
influence an individual's’ socioeconomic position. In addition, there are three major factors
which influence an individual’s health, which are: material, psychosocial and biological and
behavioral factors (WHO, 2010). Material factors are things like housing, community
environment, and place of employment (WHO. 2010). Psychosocial factors are one’s family,
friends and social networks (WHO, 2010). Lastly, biological and behavioral factors are things
like lifestyle choices, genetics, nutrition, and personal health habits (WHO, 2010). All of these
factors affect an older adult’s ability to access health care and as a result influence their risk of
developing cardiovascular disease (CVD).
The SDOH model (WHO, 2010) specifically addresses the two determinants of health:
income and education which are related to an increase in CVD in older adults. Both income and
education fall under the category “material factors” because they are specifically related to
financial gain and the attainment of skill/s (WHO, 2010). Income is a major determinant of
health because it most directly measures material resources and also has a cumulative effect over
an individual’s life course as it’s the one socioeconomic indicator that can change the most
quickly, as income varies often (Havranek et al., 2015). Studies have shown that after
controlling other sociodemographic factors, there was a 40-50% decrease in mortality from CVD
with increasing family income (Havranek et al., 2015). The SDOH model discusses how several
factors result in low income increasing one’s risk of CVD and other illnesses, for example:
income inequality causes stress for those who make less money, resulting in poorer health;
income inequality results in fewer economic resources for poorer individuals resulting in less
influence an individual's’ socioeconomic position. In addition, there are three major factors
which influence an individual’s health, which are: material, psychosocial and biological and
behavioral factors (WHO, 2010). Material factors are things like housing, community
environment, and place of employment (WHO. 2010). Psychosocial factors are one’s family,
friends and social networks (WHO, 2010). Lastly, biological and behavioral factors are things
like lifestyle choices, genetics, nutrition, and personal health habits (WHO, 2010). All of these
factors affect an older adult’s ability to access health care and as a result influence their risk of
developing cardiovascular disease (CVD).
The SDOH model (WHO, 2010) specifically addresses the two determinants of health:
income and education which are related to an increase in CVD in older adults. Both income and
education fall under the category “material factors” because they are specifically related to
financial gain and the attainment of skill/s (WHO, 2010). Income is a major determinant of
health because it most directly measures material resources and also has a cumulative effect over
an individual’s life course as it’s the one socioeconomic indicator that can change the most
quickly, as income varies often (Havranek et al., 2015). Studies have shown that after
controlling other sociodemographic factors, there was a 40-50% decrease in mortality from CVD
with increasing family income (Havranek et al., 2015). The SDOH model discusses how several
factors result in low income increasing one’s risk of CVD and other illnesses, for example:
income inequality causes stress for those who make less money, resulting in poorer health;
income inequality results in fewer economic resources for poorer individuals resulting in less
CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 9
treatment options; income inequality results in less money to invest in better social and economic
conditions leading to living in poorer neighborhoods and attending schools that are of lesser
quality resulting in poorer health outcomes (WHO, 2010).
Education is the second determinant of health that is linked with an increased risk of
CVD in older adults and the SDOH model addresses this as well (WHO, 2010). In Canada,
studies have shown a strong correlation between CVD and one’s level of education, CVD
morbidity and mortality rates have an increased risk when an individual has a lower level of
education (Kreatsoulas, 2010). Education is a life course determinant as it begins in early
childhood (influenced by one’s parents) and develops along the lifespan (WHO, 2010). The
knowledge and skills attained through education makes it easier to understand health messages
and make informed choices regarding health and well-being throughout one’s lifespan
(Kreatsoulas, 2010).
Overall, the SDOH model (Hosseini et al., 2017)) is able to show how the material
factors of both income and education are present as social determinants of health. When income
and education levels are reduced the risk of developing CVD is increased; on the contrary, when
income and education levels are higher, an older adult has a lifetime decreased risk of developing
CVD (Havranek et al., 2015).
Public Health Implications
treatment options; income inequality results in less money to invest in better social and economic
conditions leading to living in poorer neighborhoods and attending schools that are of lesser
quality resulting in poorer health outcomes (WHO, 2010).
Education is the second determinant of health that is linked with an increased risk of
CVD in older adults and the SDOH model addresses this as well (WHO, 2010). In Canada,
studies have shown a strong correlation between CVD and one’s level of education, CVD
morbidity and mortality rates have an increased risk when an individual has a lower level of
education (Kreatsoulas, 2010). Education is a life course determinant as it begins in early
childhood (influenced by one’s parents) and develops along the lifespan (WHO, 2010). The
knowledge and skills attained through education makes it easier to understand health messages
and make informed choices regarding health and well-being throughout one’s lifespan
(Kreatsoulas, 2010).
Overall, the SDOH model (Hosseini et al., 2017)) is able to show how the material
factors of both income and education are present as social determinants of health. When income
and education levels are reduced the risk of developing CVD is increased; on the contrary, when
income and education levels are higher, an older adult has a lifetime decreased risk of developing
CVD (Havranek et al., 2015).
Public Health Implications
CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 10
Public Health interventions that target material factors (socioeconomic status and
education) from the Social Determinant of Health Model will help to decrease CVD in older
adults. Interventions that address socioeconomic status (SES) will uncover greater reasoning for
gaps in policies which will help to address physical activity, nutritional habits and smoking
habits (Campbell et al., 2012; Booth et al., 2012). Booth et al. (2012) suggests that interventions
that address SES will uncover that older adults with lower income are unable to pay for
expensive medications, especially due to lack of an insurance plans, thus policies need to address
this. Canadians with lower SES tend to use more healthcare services that have little impact on
CVD due to lack of income to obtain healthier lifestyle changes (Campbell et al., 2012).
Research suggests that there are gaps in awareness of pre-CVD symptoms and treatment (Joffres,
2013), especially within third world countries and low- middle income households (Maurer &
Ramos, 2015). Low-cost treatments exist for CVD management, but many older adults are
unaware of them (Maurer & Ramos, 2015). Many older adults are also unaware that they are
manifesting symptoms for CVD and interventions need to increase educational efforts especially
within small rural communities (Maurer & Ramos, 2015). Interventions that address the lack of
education to include incentives for healthcare professionals to screen older adults for
hypertension yearly will not only increase awareness but will also help to change unhealthy
behaviour (Maurer & Ramos, 2015; Campbell, 2012; Bloetzer et al., 2015). Research indicates
that plans for interventions have been made to increase CVD awareness in numerous countries,
Public Health interventions that target material factors (socioeconomic status and
education) from the Social Determinant of Health Model will help to decrease CVD in older
adults. Interventions that address socioeconomic status (SES) will uncover greater reasoning for
gaps in policies which will help to address physical activity, nutritional habits and smoking
habits (Campbell et al., 2012; Booth et al., 2012). Booth et al. (2012) suggests that interventions
that address SES will uncover that older adults with lower income are unable to pay for
expensive medications, especially due to lack of an insurance plans, thus policies need to address
this. Canadians with lower SES tend to use more healthcare services that have little impact on
CVD due to lack of income to obtain healthier lifestyle changes (Campbell et al., 2012).
Research suggests that there are gaps in awareness of pre-CVD symptoms and treatment (Joffres,
2013), especially within third world countries and low- middle income households (Maurer &
Ramos, 2015). Low-cost treatments exist for CVD management, but many older adults are
unaware of them (Maurer & Ramos, 2015). Many older adults are also unaware that they are
manifesting symptoms for CVD and interventions need to increase educational efforts especially
within small rural communities (Maurer & Ramos, 2015). Interventions that address the lack of
education to include incentives for healthcare professionals to screen older adults for
hypertension yearly will not only increase awareness but will also help to change unhealthy
behaviour (Maurer & Ramos, 2015; Campbell, 2012; Bloetzer et al., 2015). Research indicates
that plans for interventions have been made to increase CVD awareness in numerous countries,
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 11
but there seems to lack implementation and evaluation of programs (Maurer & Ramos, 2015;
Joffres et al., 2013).
England is leading in public health interventions by using government organizations to promote
and educate the public on the risk of salt and implementing a bonus payment initiative to general
practitioners to achieve targets for hypertension care (Joffres et al., 2013). The Public Health
Agency of Canada (PHAC) suggests that education efforts need to extend to hard to reach
populations such as Indigenous communities and healthcare professionals need to be conscience
of individuals who may not seem to be at risk (Campbell et al., 2012). The PHAC aso suggests
that policies need to be transparent and take an upstream approach through cabinet level
committees to include incentives for collaboration (Campbell et al., 2012).
Finland has implemented a sodium reduction strategy in 2010 that was very effective in treating
and controlling hypertension, reducing medical costs and preventing CVD disease earlier in
patients (Campbell et al., 2012). Policies that create supportive environments make healthy
choices easier by include reducing sodium in processed foods like Finland, restricting processed
trans fats, allowing low income households to afford healthy food and creating pricing policies to
restrict energy-dense foods (Campbell et al., 2012). Healthy interventions need to reflect
community needs (Campbell et al., 2012). Canada has implemented healthy food procurement
policies in public schools to remove soft drinks and junk food, but this could be taken a step
but there seems to lack implementation and evaluation of programs (Maurer & Ramos, 2015;
Joffres et al., 2013).
England is leading in public health interventions by using government organizations to promote
and educate the public on the risk of salt and implementing a bonus payment initiative to general
practitioners to achieve targets for hypertension care (Joffres et al., 2013). The Public Health
Agency of Canada (PHAC) suggests that education efforts need to extend to hard to reach
populations such as Indigenous communities and healthcare professionals need to be conscience
of individuals who may not seem to be at risk (Campbell et al., 2012). The PHAC aso suggests
that policies need to be transparent and take an upstream approach through cabinet level
committees to include incentives for collaboration (Campbell et al., 2012).
Finland has implemented a sodium reduction strategy in 2010 that was very effective in treating
and controlling hypertension, reducing medical costs and preventing CVD disease earlier in
patients (Campbell et al., 2012). Policies that create supportive environments make healthy
choices easier by include reducing sodium in processed foods like Finland, restricting processed
trans fats, allowing low income households to afford healthy food and creating pricing policies to
restrict energy-dense foods (Campbell et al., 2012). Healthy interventions need to reflect
community needs (Campbell et al., 2012). Canada has implemented healthy food procurement
policies in public schools to remove soft drinks and junk food, but this could be taken a step
CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 12
further to implement this policy in health care facilities, workplaces, correctional institutions and
military bases (Campbell et al., 2012). The United Kingdom has implemented a total ban on junk
food ads during children’s programs and adult programs at peak watching times, which could
also be implemented in Canada to help prevent CVD earlier than in senior age (Campbell et al.,
2012).
Alternative programs not already discussed include community-linkage systems and
environmental approaches to prevent CVD. (Greenlund et al., 2012)
Greenlund et al., 2012, describe successful community programs such as the, Sickness
Prevention Achieved Through Regional Collaboration (SPARC) which coordinate with
community partners to deliver screening and preventative healthcare such as a set of
recommended immunization, cancer, and CVD screening services to older adults in places where
they can be easily accessed.
Environmental approaches include promoting healthy choices, availability, accessibility to
information, and resources for the entire population, not just high risk groups. For example the
Center for Disease Control (CDC) is working with restaurants and food manufactures to reduce
the amount of sodium in processed and restaurant foods. (Greenlund et al., 2012).
Historically these initiatives have been successful. In the past, government agencies and
the food industry have worked together to “address nutritional problems by fortifying foods with
minerals and vitamins (e.g., vitamin D fortification of milk to prevent rickets, niacin fortification
further to implement this policy in health care facilities, workplaces, correctional institutions and
military bases (Campbell et al., 2012). The United Kingdom has implemented a total ban on junk
food ads during children’s programs and adult programs at peak watching times, which could
also be implemented in Canada to help prevent CVD earlier than in senior age (Campbell et al.,
2012).
Alternative programs not already discussed include community-linkage systems and
environmental approaches to prevent CVD. (Greenlund et al., 2012)
Greenlund et al., 2012, describe successful community programs such as the, Sickness
Prevention Achieved Through Regional Collaboration (SPARC) which coordinate with
community partners to deliver screening and preventative healthcare such as a set of
recommended immunization, cancer, and CVD screening services to older adults in places where
they can be easily accessed.
Environmental approaches include promoting healthy choices, availability, accessibility to
information, and resources for the entire population, not just high risk groups. For example the
Center for Disease Control (CDC) is working with restaurants and food manufactures to reduce
the amount of sodium in processed and restaurant foods. (Greenlund et al., 2012).
Historically these initiatives have been successful. In the past, government agencies and
the food industry have worked together to “address nutritional problems by fortifying foods with
minerals and vitamins (e.g., vitamin D fortification of milk to prevent rickets, niacin fortification
CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 13
of flour to prevent pellagra, and folic acid fortification of flour to prevent neural tube defects).”
(Greenlund et al., 2012).
Unfortunately these type of changes take time, lifestyle changes, and significant
resources and may require government subsidies to bring about change. The 2010 Healthy
Hunger-Free Kids Act costing approximately $10 billion annually (Healthy, Hunger-Free Kids
Act of 2010, n.d) is an example of a government initiative to reduce childhood obesity, a
preventative strategy against obesity, CVD, diabetes and various health related problems. The act
has both pros and cons and has been all but eliminated by the Trump administration. Successes
of the program include, “increased nutritional value, iron, calcium, vitamin A, vitamin C, and
protein nutrition” and decreased caloric intake, which benefited children with obesity (Cornish et
al., 2016). However the program also had its critics. Students complained about poor portion
sizes, bland food and a study published by the Harvard School of Public Health “discovered that
about 60 percent of vegetables and roughly 40 percent of fresh fruit are thrown away due to no
interest.” (Healthy, Hunger-Free Kids Act of 2010, n.d)
Public health interventions are clearly beneficial for the reduced risk of CVD. It is imperative
that investments are made towards health education with a focus towards individuals from lower
income and socioeconomic households.
Conclusion and Summary
of flour to prevent pellagra, and folic acid fortification of flour to prevent neural tube defects).”
(Greenlund et al., 2012).
Unfortunately these type of changes take time, lifestyle changes, and significant
resources and may require government subsidies to bring about change. The 2010 Healthy
Hunger-Free Kids Act costing approximately $10 billion annually (Healthy, Hunger-Free Kids
Act of 2010, n.d) is an example of a government initiative to reduce childhood obesity, a
preventative strategy against obesity, CVD, diabetes and various health related problems. The act
has both pros and cons and has been all but eliminated by the Trump administration. Successes
of the program include, “increased nutritional value, iron, calcium, vitamin A, vitamin C, and
protein nutrition” and decreased caloric intake, which benefited children with obesity (Cornish et
al., 2016). However the program also had its critics. Students complained about poor portion
sizes, bland food and a study published by the Harvard School of Public Health “discovered that
about 60 percent of vegetables and roughly 40 percent of fresh fruit are thrown away due to no
interest.” (Healthy, Hunger-Free Kids Act of 2010, n.d)
Public health interventions are clearly beneficial for the reduced risk of CVD. It is imperative
that investments are made towards health education with a focus towards individuals from lower
income and socioeconomic households.
Conclusion and Summary
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 14
Income and social determinants have generally determined the CVD prevalence in
Canada. It has been shown the CVD’s prevalence in high -income economies. Also, Canadians
with lower SES tend to use more healthcare services that have little impact on CVD due to lack
of income to obtain healthier lifestyle change. In Canada, it is expected that CVD will still be the
leading cause of death even by 2030. The CVD is a major issue in Canada since it accounts for
higher number of deaths than any other illness in the country. Because of the higher magnitude
of CVD in Canada, the studies are being directed towards the social determinants of health
(SDH). These are the risk factors “causes of causes”). Thus Canada wants to control the impacts
of social environment on people sharing a community as mechanism to reduce CVD prevalence.
The implications of this study is that Public Health interventions that target material factors
(socioeconomic status and education) from the Social Determinant of Health Model will help
decrease CVD in older adults. The future study should focus on interventions that address
socioeconomic status (SES) to uncover greater reasoning for gaps in policies. This will help
address physical activity, nutritional habits and smoking habits.
Income and social determinants have generally determined the CVD prevalence in
Canada. It has been shown the CVD’s prevalence in high -income economies. Also, Canadians
with lower SES tend to use more healthcare services that have little impact on CVD due to lack
of income to obtain healthier lifestyle change. In Canada, it is expected that CVD will still be the
leading cause of death even by 2030. The CVD is a major issue in Canada since it accounts for
higher number of deaths than any other illness in the country. Because of the higher magnitude
of CVD in Canada, the studies are being directed towards the social determinants of health
(SDH). These are the risk factors “causes of causes”). Thus Canada wants to control the impacts
of social environment on people sharing a community as mechanism to reduce CVD prevalence.
The implications of this study is that Public Health interventions that target material factors
(socioeconomic status and education) from the Social Determinant of Health Model will help
decrease CVD in older adults. The future study should focus on interventions that address
socioeconomic status (SES) to uncover greater reasoning for gaps in policies. This will help
address physical activity, nutritional habits and smoking habits.

CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 15
References
American Heart Association. (2016). Statistical Fact Sheet 2016 Update: Older Americans &
Cardiovascular Diseases. Retrieved from https://www.heart.org/idc/groups/heart-
public/@wcm/@sop/@smd/documents/downloadable/ucm_483970.pdf
Havranek, E. P., Mujahid, M. S., Barr, D. A., Blair, I. V., Cohen, M. S., Cruz-Flores, S., & ...
Yancy, C. W. (2015). Social Determinants of Risk and Outcomes for
Cardiovascular Disease. Circulation, 132(9), 873-898.
doi:10.1161/CIR.0000000000000228
Hosseini, S., Arab, M., Emamgholipour, S., Rashidian, A., Monterzari A., & Zaboli, R. (2017).
Conceptual Models of Social Determinants of Health: A Narrative Review. Iranian
Journal of Public Health, 46(4), 435–446.
Kreatsoulas, C., & Anand, S. S. (2010). The impact of social determinants on cardiovascular
disease. The Canadian Journal of Cardiology, 26(Suppl C), 8C–13C.
References
American Heart Association. (2016). Statistical Fact Sheet 2016 Update: Older Americans &
Cardiovascular Diseases. Retrieved from https://www.heart.org/idc/groups/heart-
public/@wcm/@sop/@smd/documents/downloadable/ucm_483970.pdf
Havranek, E. P., Mujahid, M. S., Barr, D. A., Blair, I. V., Cohen, M. S., Cruz-Flores, S., & ...
Yancy, C. W. (2015). Social Determinants of Risk and Outcomes for
Cardiovascular Disease. Circulation, 132(9), 873-898.
doi:10.1161/CIR.0000000000000228
Hosseini, S., Arab, M., Emamgholipour, S., Rashidian, A., Monterzari A., & Zaboli, R. (2017).
Conceptual Models of Social Determinants of Health: A Narrative Review. Iranian
Journal of Public Health, 46(4), 435–446.
Kreatsoulas, C., & Anand, S. S. (2010). The impact of social determinants on cardiovascular
disease. The Canadian Journal of Cardiology, 26(Suppl C), 8C–13C.
CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 16
Public Health Agency of Canada. (2017a). Canadian chronic disease surveillance system
methods report abridged version for v2015 and v2016 (Dementia, Including Alzheimer’s
Disease). Retrieved from
https://infobase.phac-aspc.gc.ca/ccdss-scsmc/data-tool/Methods
Public Health Agency of Canada. (2017b). The 2017 Canadian chronic disease indicators.
Health Promotion and Chronic Disease Prevention in Canada Research, Policy and
Practice, 37(8), 248-251. Retrieved from https://www.canada.ca/content/dam/phac-
aspc/documents/services/publications/health-promotion-chronic-disease-prevention-
canada-research-policy-practice/vol-37-no-8-2017/ar-03-eng.pdf
Public Health Agency of Canada. (2017c). Public health infobase: Canadian Chronic Disease
Surveillance System (CCDSS). Retrieved from https://infobase.phac-aspc.gc.ca/CCDSS-
SCSMC/data-tool/?
l=eng&HRs=00&DDLV=CDSAMI&DDLM=ASIR&1=M&2=F&DDLFrm=1999&DD
LTo=2012&=10&VIEW=2
Raphael, D. (2016). Social determinants of health: Canadian perspectives. Toronto: Canadian
Scholars Press Inc.
Statistics Canada. (2016). Canadian Community Health Survey – Annual Component (CCHS).
Retrieved from http://www23.statcan.gc.ca/imdb/p2SV.pl?
Function=getSurvey&SDDS=3226
World Health Organization (WHO) 2010. A conceptual model framework for action on the
Public Health Agency of Canada. (2017a). Canadian chronic disease surveillance system
methods report abridged version for v2015 and v2016 (Dementia, Including Alzheimer’s
Disease). Retrieved from
https://infobase.phac-aspc.gc.ca/ccdss-scsmc/data-tool/Methods
Public Health Agency of Canada. (2017b). The 2017 Canadian chronic disease indicators.
Health Promotion and Chronic Disease Prevention in Canada Research, Policy and
Practice, 37(8), 248-251. Retrieved from https://www.canada.ca/content/dam/phac-
aspc/documents/services/publications/health-promotion-chronic-disease-prevention-
canada-research-policy-practice/vol-37-no-8-2017/ar-03-eng.pdf
Public Health Agency of Canada. (2017c). Public health infobase: Canadian Chronic Disease
Surveillance System (CCDSS). Retrieved from https://infobase.phac-aspc.gc.ca/CCDSS-
SCSMC/data-tool/?
l=eng&HRs=00&DDLV=CDSAMI&DDLM=ASIR&1=M&2=F&DDLFrm=1999&DD
LTo=2012&=10&VIEW=2
Raphael, D. (2016). Social determinants of health: Canadian perspectives. Toronto: Canadian
Scholars Press Inc.
Statistics Canada. (2016). Canadian Community Health Survey – Annual Component (CCHS).
Retrieved from http://www23.statcan.gc.ca/imdb/p2SV.pl?
Function=getSurvey&SDDS=3226
World Health Organization (WHO) 2010. A conceptual model framework for action on the
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 17
Social determinants of health. Retrieved
from:http://www.who.int/social_determinants/corner/SDHDP2.pdf page 9
World Health Organization. (2017). Cardiovascular diseases (CVDs). Retrieved from
http://www.who.int/mediacentre/factsheets/fs317/en/
Table 1, 2 Statistics Canada. (2016). Canadian Community Health Survey, 2014: Annual
component [public-use microdata file]. Ottawa, Ontario: Statistics Canada. Health Statistics
Division, Data Liberation Initiative [producer and distributor]. Retrieved From
http://odesi1.scholarsportal.info.ezproxy.lakeheadu.ca/webview/index.jsp?object=http%3A%2F
%2F142.150.190.11%3A80%2Fobj%2FfStudy%2Fcchs-82M0013-E-2014-Annual-
component&headers=http%3A%2F%2F142.150.190.11%3A80%2Fobj%2FfVariable%2Fcchs-
82M0013-E-2014-Annual-component_V100
Table 3, 4 Statistics Canada. (2016). Canadian Community Health Survey, 2014: Annual
component [public-use microdata file]. Ottawa, Ontario: Statistics Canada. Health Statistics
Division, Data Liberation Initiative [producer and distributor]. Retrieved From
http://odesi1.scholarsportal.info.ezproxy.lakeheadu.ca/webview/index.jsp?object=http%3A%2F
Social determinants of health. Retrieved
from:http://www.who.int/social_determinants/corner/SDHDP2.pdf page 9
World Health Organization. (2017). Cardiovascular diseases (CVDs). Retrieved from
http://www.who.int/mediacentre/factsheets/fs317/en/
Table 1, 2 Statistics Canada. (2016). Canadian Community Health Survey, 2014: Annual
component [public-use microdata file]. Ottawa, Ontario: Statistics Canada. Health Statistics
Division, Data Liberation Initiative [producer and distributor]. Retrieved From
http://odesi1.scholarsportal.info.ezproxy.lakeheadu.ca/webview/index.jsp?object=http%3A%2F
%2F142.150.190.11%3A80%2Fobj%2FfStudy%2Fcchs-82M0013-E-2014-Annual-
component&headers=http%3A%2F%2F142.150.190.11%3A80%2Fobj%2FfVariable%2Fcchs-
82M0013-E-2014-Annual-component_V100
Table 3, 4 Statistics Canada. (2016). Canadian Community Health Survey, 2014: Annual
component [public-use microdata file]. Ottawa, Ontario: Statistics Canada. Health Statistics
Division, Data Liberation Initiative [producer and distributor]. Retrieved From
http://odesi1.scholarsportal.info.ezproxy.lakeheadu.ca/webview/index.jsp?object=http%3A%2F
CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 18
%2F142.150.190.11%3A80%2Fobj%2FfStudy%2Fcchs-82M0013-E-2014-Annual-
component&headers=http%3A%2F%2F142.150.190.11%3A80%2Fobj%2FfVariable%2Fcchs-
82M0013-E-2014-Annual-component_V100
%2F142.150.190.11%3A80%2Fobj%2FfStudy%2Fcchs-82M0013-E-2014-Annual-
component&headers=http%3A%2F%2F142.150.190.11%3A80%2Fobj%2FfVariable%2Fcchs-
82M0013-E-2014-Annual-component_V100
CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 19
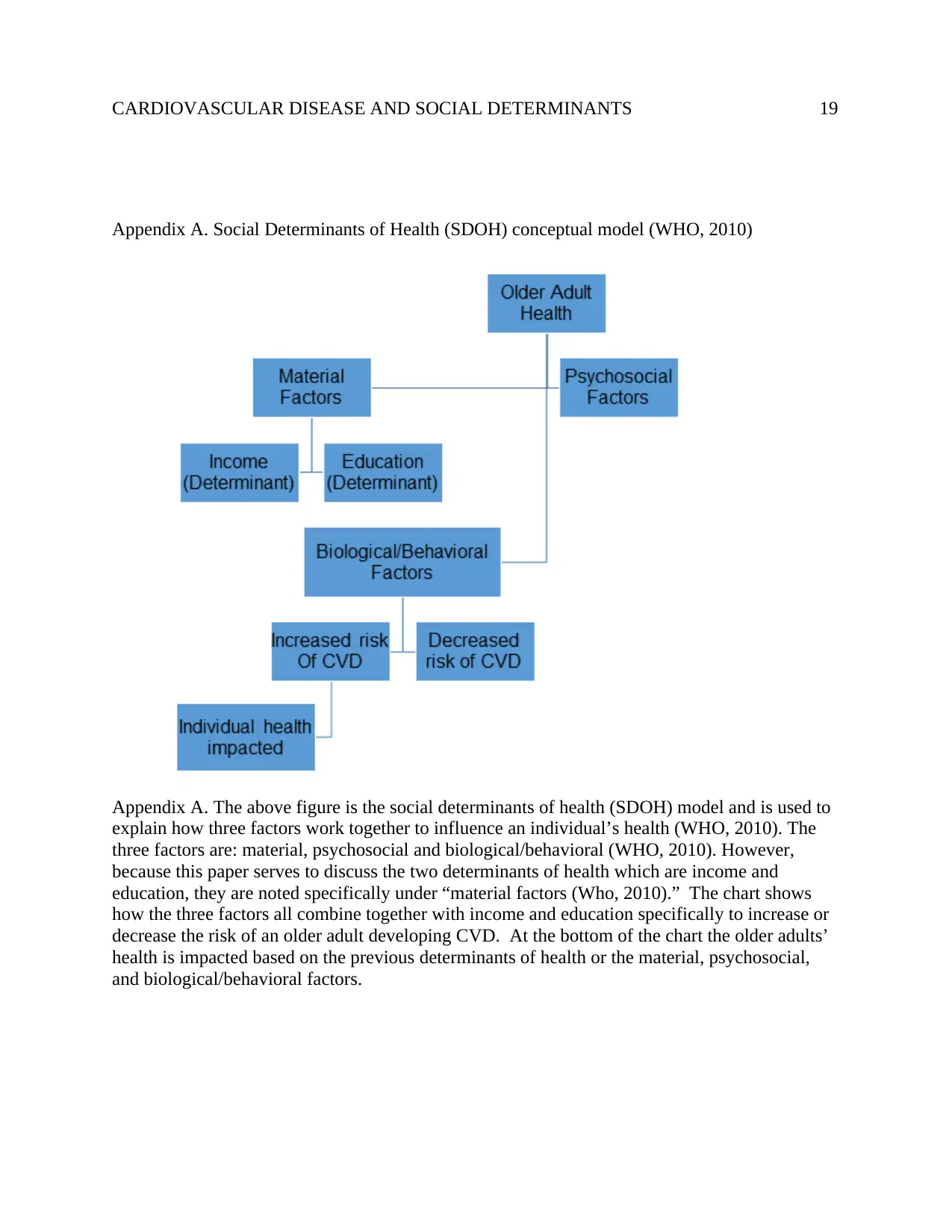
Appendix A. Social Determinants of Health (SDOH) conceptual model (WHO, 2010)
Appendix A. The above figure is the social determinants of health (SDOH) model and is used to
explain how three factors work together to influence an individual’s health (WHO, 2010). The
three factors are: material, psychosocial and biological/behavioral (WHO, 2010). However,
because this paper serves to discuss the two determinants of health which are income and
education, they are noted specifically under “material factors (Who, 2010).” The chart shows
how the three factors all combine together with income and education specifically to increase or
decrease the risk of an older adult developing CVD. At the bottom of the chart the older adults’
health is impacted based on the previous determinants of health or the material, psychosocial,
and biological/behavioral factors.
Appendix A. Social Determinants of Health (SDOH) conceptual model (WHO, 2010)
Appendix A. The above figure is the social determinants of health (SDOH) model and is used to
explain how three factors work together to influence an individual’s health (WHO, 2010). The
three factors are: material, psychosocial and biological/behavioral (WHO, 2010). However,
because this paper serves to discuss the two determinants of health which are income and
education, they are noted specifically under “material factors (Who, 2010).” The chart shows
how the three factors all combine together with income and education specifically to increase or
decrease the risk of an older adult developing CVD. At the bottom of the chart the older adults’
health is impacted based on the previous determinants of health or the material, psychosocial,
and biological/behavioral factors.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 20

CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 21
Tables
Table 1. Females with CVD and education qualification
Tables
Table 1. Females with CVD and education qualification
CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 22
Table 2. Males with CVD and education qualification
Table 2. Males with CVD and education qualification
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
CARDIOVASCULAR DISEASE AND SOCIAL DETERMINANTS 23
Table 3. Females with CVD compared with personal income
Table 4. Males with CVD compared with personal income
Table 3. Females with CVD compared with personal income
Table 4. Males with CVD compared with personal income
1 out of 23
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





