Analysis of a Dementia Patient: Care, Risks, and Management Report
VerifiedAdded on 2020/01/28
|13
|4650
|158
Report
AI Summary
This report provides a comprehensive care analysis of a dementia patient, examining the biological, psychological, social, and cultural determinants affecting their health. The analysis is based on a case study of a dementia patient, and it includes a detailed risk assessment and management plan, addressing potential issues such as falls, aggressive behavior, and other health complications. Furthermore, the report explores recovery principles, engagement processes, and the legal and ethical dimensions of dementia care, including the roles and responsibilities of mental health nurses. The report emphasizes the importance of early diagnosis, effective medication, and a supportive environment to improve the patient's quality of life and manage the progression of the illness. The report also highlights the significance of interdisciplinary care teams and the use of various assessment tools in providing comprehensive care for dementia patients.
Care analysis of a service user
experiencing acute and challenging
mental health problems
experiencing acute and challenging
mental health problems
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
Introduction..........................................................................................................................................4
Scenario.......................................................................................................................................4
Service users presenting problems, from the biopsychosocial perspective................................4
Risk assessment and management..............................................................................................5
Recovery principles and engagement processes.........................................................................7
Legal and Ethical dimensions for dementia patient....................................................................8
Legal Dimensions: Different Acts, policies and schedules for mental patients have been
implemented by the government of UK. All the Acts and policies are discussed below............8
Roles and responsibilities of mental health nurse.......................................................................9
Conclusion..........................................................................................................................................10
References..........................................................................................................................................12
Introduction..........................................................................................................................................4
Scenario.......................................................................................................................................4
Service users presenting problems, from the biopsychosocial perspective................................4
Risk assessment and management..............................................................................................5
Recovery principles and engagement processes.........................................................................7
Legal and Ethical dimensions for dementia patient....................................................................8
Legal Dimensions: Different Acts, policies and schedules for mental patients have been
implemented by the government of UK. All the Acts and policies are discussed below............8
Roles and responsibilities of mental health nurse.......................................................................9
Conclusion..........................................................................................................................................10
References..........................................................................................................................................12

Index of Tables
Table 1: Risk Assessment for Dementia Patients.................................................................................5
Table 1: Risk Assessment for Dementia Patients.................................................................................5
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
INTRODUCTION
Care analysis is an integral part of mental health care in health and social setting in UK. It
includes analysis and diagnosis of individuals mental conditions. The analysis provides basis for the
treatment and care plan to combat mental illness of affected service users. The present report
explores the biological, psychological, social and cultural determinants that greatly impact the
health of the mental patient given in the scenario (Cuthbert and Insel, 2013). In addition to this the
report also presents the risk assessment and management of the patient suffering from Dementia.
Besides this the report also talks about recovery principles and engagement processes in the care
analysis. Apart from this, the report also features the legal and ethical framework which play
important role in the care analysis of the metal patients. In addition to this, the roles and
responsibilities of mental health nurse is discussed in length.
Scenario
Jacob Edward, is a blogger and founder of Senior Planning which aims to provide free long
term care services for elderly patients. In one of his blog he narrates the story of establishing his
company after getting inspired from his personal experience about his grandfather who was in his
70s's and used to live alone at his residence. Jacob narrates that with progressive age his grandfather
started hallucinating for having raccoon in the attic of his house and in this attempt to find the
creature he fell down (The Genius of Caring, 2016). He was then taken to emergency room where
the health practitioner suggested the old man was suffering from Dementia. None of the family
members were unable to grasp the early warning signs of the mental disorder. Dementia is a mental
ailment which include agitation, anxiety, hallucinations and restlessness. He was then admitted to
memory care facility to treat his condition.
Service users presenting problems, from the biopsychosocial perspective
There are various factors that affect the mental health of the old man with Dementia in the
given scenario. These include biological, psychological, social and cultural determinants that
significantly give rise to cognitive and non cognitive symptoms of Dementia in individuals. These
factors are briefly discussed in the following points:
Biological Factors
Dementia is a mental disorder that is characterized by the loss of cognitive ability in
multiple domains in individuals. These domains include memory, learning, reading, writing, ability
to interpret immediate environment and information. Scientific research indicates that symptoms of
memory impairment is directly linked to neurological abnormalities. There are various neurological
systems which explains the abnormalities that are responsible of causing dementia in the elderly
person in the given scenario. These include Cholinergic, Dopaminergic, Serotonergic and
noradrenergic systems. The cholinergic system is the widely studied neurotransmitter system which
Care analysis is an integral part of mental health care in health and social setting in UK. It
includes analysis and diagnosis of individuals mental conditions. The analysis provides basis for the
treatment and care plan to combat mental illness of affected service users. The present report
explores the biological, psychological, social and cultural determinants that greatly impact the
health of the mental patient given in the scenario (Cuthbert and Insel, 2013). In addition to this the
report also presents the risk assessment and management of the patient suffering from Dementia.
Besides this the report also talks about recovery principles and engagement processes in the care
analysis. Apart from this, the report also features the legal and ethical framework which play
important role in the care analysis of the metal patients. In addition to this, the roles and
responsibilities of mental health nurse is discussed in length.
Scenario
Jacob Edward, is a blogger and founder of Senior Planning which aims to provide free long
term care services for elderly patients. In one of his blog he narrates the story of establishing his
company after getting inspired from his personal experience about his grandfather who was in his
70s's and used to live alone at his residence. Jacob narrates that with progressive age his grandfather
started hallucinating for having raccoon in the attic of his house and in this attempt to find the
creature he fell down (The Genius of Caring, 2016). He was then taken to emergency room where
the health practitioner suggested the old man was suffering from Dementia. None of the family
members were unable to grasp the early warning signs of the mental disorder. Dementia is a mental
ailment which include agitation, anxiety, hallucinations and restlessness. He was then admitted to
memory care facility to treat his condition.
Service users presenting problems, from the biopsychosocial perspective
There are various factors that affect the mental health of the old man with Dementia in the
given scenario. These include biological, psychological, social and cultural determinants that
significantly give rise to cognitive and non cognitive symptoms of Dementia in individuals. These
factors are briefly discussed in the following points:
Biological Factors
Dementia is a mental disorder that is characterized by the loss of cognitive ability in
multiple domains in individuals. These domains include memory, learning, reading, writing, ability
to interpret immediate environment and information. Scientific research indicates that symptoms of
memory impairment is directly linked to neurological abnormalities. There are various neurological
systems which explains the abnormalities that are responsible of causing dementia in the elderly
person in the given scenario. These include Cholinergic, Dopaminergic, Serotonergic and
noradrenergic systems. The cholinergic system is the widely studied neurotransmitter system which
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
elaborates that loss of neurons leads to deterioration in cognitive functions of brain increasing the
risks of mental disorders such as Dementia and Alzheimer's (Linda, 2010). In addition to this,
dopamerginic system is responsible for causing cognitive dysfunction among dementia patients. It
has been observed that genetic factors also triggers dementia symptoms. Several research studies
indicate that there are certain genes which are inherited by individuals induce onset of sporadic ad
familial forms of Alzheimer's which is the prognosis of Alzheimer's.
Psychological Factors
Apart from biological factors, several studies indicate that there are psychological risk
factors which significantly impact the health of patients suffering from Dementia and other mental
disorders. Neuroticism, social isolation and depression are such factors. The existence of depression
and anxiety increases the risk factor of dementia among individuals (Catriona and et.al., 2001).It
can be analyzed that the old man in the given scenario was living alone and was occasionally visited
by his family members. Thus, this can be a potential factor to trigger the symptoms of Dementia in
the elderly person.
Social Factors
In addition to this, social factors also impact the health of individuals suffering from mental
disorders. It has been observed that social determinants such as poor education, misuse of alcohol,
stressful living and working conditions elevate the risk of dementia among individuals. It has been
found in several studies that prevalence of dementia is more in poorly educated people. It has been
cited that highly educated people have better cognitive abilities which affects the rate of onset of the
mental disorder (Kullberg, Larsen and Sharp, 2013). However, it is unclear that education obtained
in childhood or lifelong acquisition of knowledge provides protection against dementia. Apart from
this, alcohol misuse is said to have negative impact on brain functions and thus elevates the risk of
dementia.
Risk assessment and management
In health and social care settings it is very important to carry out risk assessment effectively
to treat the patients who are at greater risk of developing dementia. Since it can be analyzed that no
family member detected the early signs of dementia in the old person however he was then
diagnosed with the condition after being admitted to emergency room. After being diagnosed with
dementia he was then referred to memory care facility. Health care professionals of the memory
care facility organization who play important role in risk assessment for the old dementia patient are
neurologists, neuropsychologist, geriatrician and mental health nurse. Risk assessment helps in the
early diagnosis of the existence of dementia which when remain untreated can progress into
Alzheimer's in the given scenario.
risks of mental disorders such as Dementia and Alzheimer's (Linda, 2010). In addition to this,
dopamerginic system is responsible for causing cognitive dysfunction among dementia patients. It
has been observed that genetic factors also triggers dementia symptoms. Several research studies
indicate that there are certain genes which are inherited by individuals induce onset of sporadic ad
familial forms of Alzheimer's which is the prognosis of Alzheimer's.
Psychological Factors
Apart from biological factors, several studies indicate that there are psychological risk
factors which significantly impact the health of patients suffering from Dementia and other mental
disorders. Neuroticism, social isolation and depression are such factors. The existence of depression
and anxiety increases the risk factor of dementia among individuals (Catriona and et.al., 2001).It
can be analyzed that the old man in the given scenario was living alone and was occasionally visited
by his family members. Thus, this can be a potential factor to trigger the symptoms of Dementia in
the elderly person.
Social Factors
In addition to this, social factors also impact the health of individuals suffering from mental
disorders. It has been observed that social determinants such as poor education, misuse of alcohol,
stressful living and working conditions elevate the risk of dementia among individuals. It has been
found in several studies that prevalence of dementia is more in poorly educated people. It has been
cited that highly educated people have better cognitive abilities which affects the rate of onset of the
mental disorder (Kullberg, Larsen and Sharp, 2013). However, it is unclear that education obtained
in childhood or lifelong acquisition of knowledge provides protection against dementia. Apart from
this, alcohol misuse is said to have negative impact on brain functions and thus elevates the risk of
dementia.
Risk assessment and management
In health and social care settings it is very important to carry out risk assessment effectively
to treat the patients who are at greater risk of developing dementia. Since it can be analyzed that no
family member detected the early signs of dementia in the old person however he was then
diagnosed with the condition after being admitted to emergency room. After being diagnosed with
dementia he was then referred to memory care facility. Health care professionals of the memory
care facility organization who play important role in risk assessment for the old dementia patient are
neurologists, neuropsychologist, geriatrician and mental health nurse. Risk assessment helps in the
early diagnosis of the existence of dementia which when remain untreated can progress into
Alzheimer's in the given scenario.
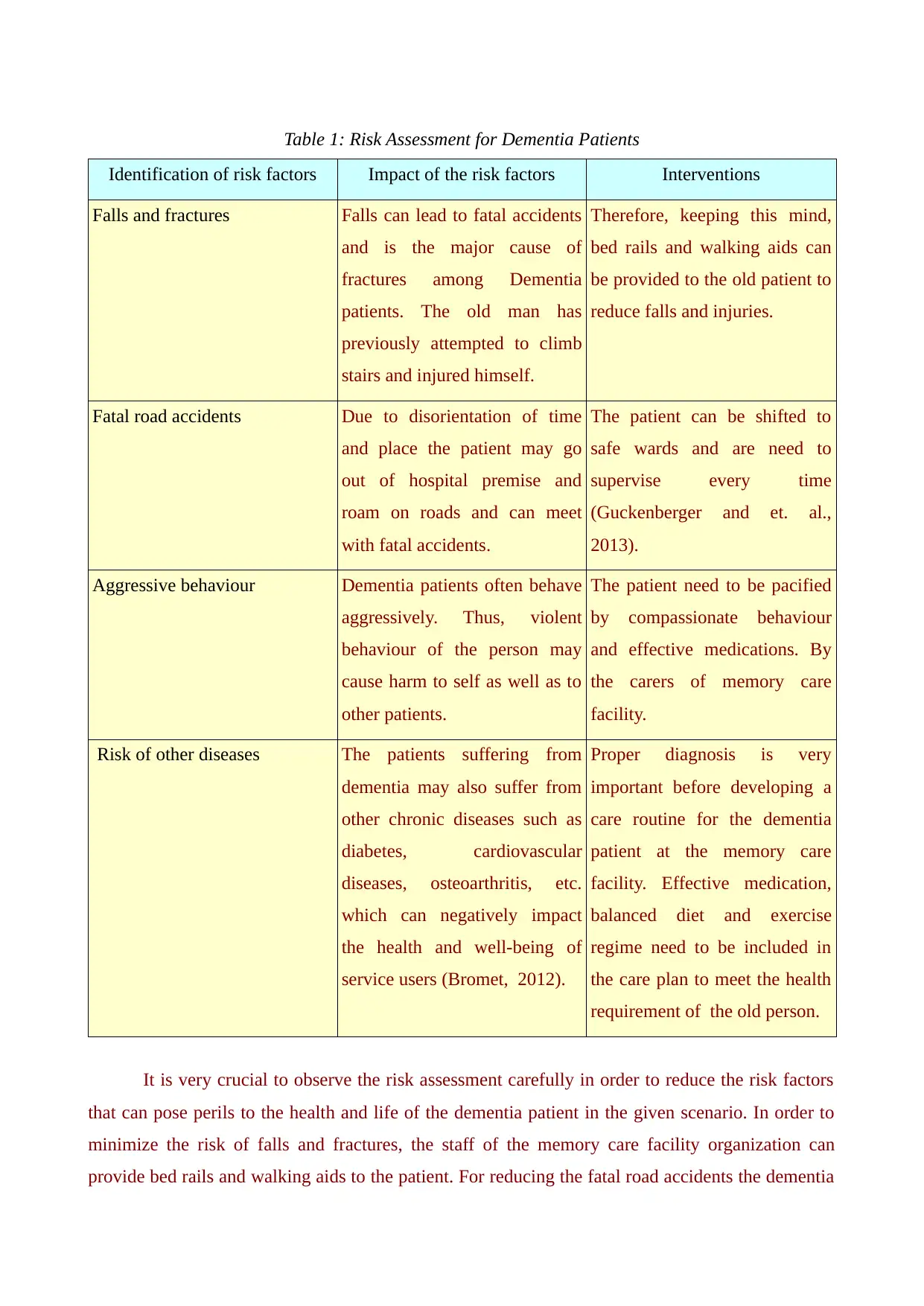
Table 1: Risk Assessment for Dementia Patients
Identification of risk factors Impact of the risk factors Interventions
Falls and fractures Falls can lead to fatal accidents
and is the major cause of
fractures among Dementia
patients. The old man has
previously attempted to climb
stairs and injured himself.
Therefore, keeping this mind,
bed rails and walking aids can
be provided to the old patient to
reduce falls and injuries.
Fatal road accidents Due to disorientation of time
and place the patient may go
out of hospital premise and
roam on roads and can meet
with fatal accidents.
The patient can be shifted to
safe wards and are need to
supervise every time
(Guckenberger and et. al.,
2013).
Aggressive behaviour Dementia patients often behave
aggressively. Thus, violent
behaviour of the person may
cause harm to self as well as to
other patients.
The patient need to be pacified
by compassionate behaviour
and effective medications. By
the carers of memory care
facility.
Risk of other diseases The patients suffering from
dementia may also suffer from
other chronic diseases such as
diabetes, cardiovascular
diseases, osteoarthritis, etc.
which can negatively impact
the health and well-being of
service users (Bromet, 2012).
Proper diagnosis is very
important before developing a
care routine for the dementia
patient at the memory care
facility. Effective medication,
balanced diet and exercise
regime need to be included in
the care plan to meet the health
requirement of the old person.
It is very crucial to observe the risk assessment carefully in order to reduce the risk factors
that can pose perils to the health and life of the dementia patient in the given scenario. In order to
minimize the risk of falls and fractures, the staff of the memory care facility organization can
provide bed rails and walking aids to the patient. For reducing the fatal road accidents the dementia
Identification of risk factors Impact of the risk factors Interventions
Falls and fractures Falls can lead to fatal accidents
and is the major cause of
fractures among Dementia
patients. The old man has
previously attempted to climb
stairs and injured himself.
Therefore, keeping this mind,
bed rails and walking aids can
be provided to the old patient to
reduce falls and injuries.
Fatal road accidents Due to disorientation of time
and place the patient may go
out of hospital premise and
roam on roads and can meet
with fatal accidents.
The patient can be shifted to
safe wards and are need to
supervise every time
(Guckenberger and et. al.,
2013).
Aggressive behaviour Dementia patients often behave
aggressively. Thus, violent
behaviour of the person may
cause harm to self as well as to
other patients.
The patient need to be pacified
by compassionate behaviour
and effective medications. By
the carers of memory care
facility.
Risk of other diseases The patients suffering from
dementia may also suffer from
other chronic diseases such as
diabetes, cardiovascular
diseases, osteoarthritis, etc.
which can negatively impact
the health and well-being of
service users (Bromet, 2012).
Proper diagnosis is very
important before developing a
care routine for the dementia
patient at the memory care
facility. Effective medication,
balanced diet and exercise
regime need to be included in
the care plan to meet the health
requirement of the old person.
It is very crucial to observe the risk assessment carefully in order to reduce the risk factors
that can pose perils to the health and life of the dementia patient in the given scenario. In order to
minimize the risk of falls and fractures, the staff of the memory care facility organization can
provide bed rails and walking aids to the patient. For reducing the fatal road accidents the dementia
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
patients can be shifted to safe wards and need to be supervised day in and day out (Fanning,
2013).There are various risk assessment tools that are used by care professionals of the memory
care facility to assess the risk factors for the old patient that are more prone to risk of Alzheimer's
which is a prognosis of dementia. These include Initial Dementia Assessment (IDA) which is an
effective tool that supports health practitioners in diagnosis and development of a care plan and
management of the elderly individual with dementia.
Risk Management
On the basis of risk assessment of the dementia patient in the given scenario, it is very
important to manage risk factors to ensure his health and safety. The risk management of the
dementia patient can be done in the following manner: Ensuring safety from falls: Falls are the serious risk factor that have detrimental effect on
the health and life of the older patient. In order to avoid falls care staff at memory care
facility needs to take care of objects that loosely lie on floors. Bed rails and walking aids can
be provided to the old patient for safe movement (World Health Organization, 2012). In
addition to this, the patient can be shifted to safe wards that are well guarded to supervise
him effectively. This will help in reducing the fatal accidents. Besides this, the things that
are required by the old dementia patient on a day to day basis such as water, eatables need to
be kept in his reach. Helping out in exercising: For facilitating the easy movement and maintaining the general
health of the elderly patient, care workers of the memory care facility are required to assist
him while exercising and physiotherapy. This not only improves locomotion of the service
user but also help in reducing the risk of falls and fractures. Effective medication: Proper assessment followed by effective medication can help in
improving the condition of the dementia patient in the given scenario. Medications do not
cure the mental condition completely but are useful in improving the brain functionality of
the affected individual. This helps in reducing the risk of Alzheimer's that is progressive
condition of Dementia. Improving lighting: In order to reduce falls, the premises of the memory care facility
organization in the given scenario needs to be well lit. As due to weak vision issues of the
older patient, improved lighting can be beneficial in reducing falls and fractures. Taking care of nutritional requirements: From the risk assessment the care professionals of
the memory care facility are required to develop sound care planning of the dementia patient
in the given case. The care routine of the service user include medication, physiotherapy and
balanced diet. A proper diet plan helps in meeting the nutritional demands of the old care
taker (Munn-Giddings and Winter, 2013).Healthy food not only improves stamina but also
2013).There are various risk assessment tools that are used by care professionals of the memory
care facility to assess the risk factors for the old patient that are more prone to risk of Alzheimer's
which is a prognosis of dementia. These include Initial Dementia Assessment (IDA) which is an
effective tool that supports health practitioners in diagnosis and development of a care plan and
management of the elderly individual with dementia.
Risk Management
On the basis of risk assessment of the dementia patient in the given scenario, it is very
important to manage risk factors to ensure his health and safety. The risk management of the
dementia patient can be done in the following manner: Ensuring safety from falls: Falls are the serious risk factor that have detrimental effect on
the health and life of the older patient. In order to avoid falls care staff at memory care
facility needs to take care of objects that loosely lie on floors. Bed rails and walking aids can
be provided to the old patient for safe movement (World Health Organization, 2012). In
addition to this, the patient can be shifted to safe wards that are well guarded to supervise
him effectively. This will help in reducing the fatal accidents. Besides this, the things that
are required by the old dementia patient on a day to day basis such as water, eatables need to
be kept in his reach. Helping out in exercising: For facilitating the easy movement and maintaining the general
health of the elderly patient, care workers of the memory care facility are required to assist
him while exercising and physiotherapy. This not only improves locomotion of the service
user but also help in reducing the risk of falls and fractures. Effective medication: Proper assessment followed by effective medication can help in
improving the condition of the dementia patient in the given scenario. Medications do not
cure the mental condition completely but are useful in improving the brain functionality of
the affected individual. This helps in reducing the risk of Alzheimer's that is progressive
condition of Dementia. Improving lighting: In order to reduce falls, the premises of the memory care facility
organization in the given scenario needs to be well lit. As due to weak vision issues of the
older patient, improved lighting can be beneficial in reducing falls and fractures. Taking care of nutritional requirements: From the risk assessment the care professionals of
the memory care facility are required to develop sound care planning of the dementia patient
in the given case. The care routine of the service user include medication, physiotherapy and
balanced diet. A proper diet plan helps in meeting the nutritional demands of the old care
taker (Munn-Giddings and Winter, 2013).Healthy food not only improves stamina but also
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
helps in resolving other health issues such as diabetes, obesity, hypertension, etc. Labeling stuff of daily use : In order to help the patient in remembering things, the stuff
which are used by the old patient on a regular basis can be labeled. This will help him in
carrying out his routine tasks independently.
Providing Occupational Therapy: Occupational therapy can be provided to the elderly
patient to provide him practical support in performing his day to day tasks at the memory
care facility. The therapy also helps in selecting assistive technology and equipment to
provide support to the service user such as providing hand rails in bathrooms to prevent
falls.
Recovery principles and engagement processes
Trained interdisciplinary care team of the memory care facility from various healthcare
centres such as neurologist, nurse practitioner, social worker and health educator are
appointed to deliver care training and exercise programs to patients suffering from
dementia. Caregivers are also given proper training to deal with the patients in a better way.
Comprehensive assessment tools are incorporated in the memory care facility to measure
and monitor patient and caregiver biological, physical and social requirements according to
requirements of both patients and healthcare professionals (Aveyard, 2014).
Local health bodies also provide help and support to the people who are suffering from
dementia by giving them emotional, mental and physical support.
Patient-centred, individualized care protocols that incorporate input from the patient and
caregiver can be launched and implemented by memory care facility organization to
improve the strategies and plans to treat patients with dementia and other mental disabilities.
Family-focused protocols and programs are also conducted by collaborative health
management team to improve family care needs. It also provides enhanced social assistance
with ready availability of communication through telephone or in-person consultation with
NP or SW. They also help in limiting inappropriate and inadequate use of sub acute medical
services such as emergency department, hospitalizations, surgical departments and various
other departments in a hospital (Bongar and Sullivan, 2013).
Care consultation models designed by various healthcare professionals from different health
authorities and hospitals helps in incorporating patient and caregiver needs and
requirements. It aids in improving knowledge, care confidence, command and header skills
(Cuthbert and Insel, 2013). It further also reduces individual health professional load and
stress, which also results in decreasing depression of dementia patients at personal level.
Legal and Ethical dimensions for dementia patient
Legal and ethical dimensions play very important role in care analysis of patients suffering
which are used by the old patient on a regular basis can be labeled. This will help him in
carrying out his routine tasks independently.
Providing Occupational Therapy: Occupational therapy can be provided to the elderly
patient to provide him practical support in performing his day to day tasks at the memory
care facility. The therapy also helps in selecting assistive technology and equipment to
provide support to the service user such as providing hand rails in bathrooms to prevent
falls.
Recovery principles and engagement processes
Trained interdisciplinary care team of the memory care facility from various healthcare
centres such as neurologist, nurse practitioner, social worker and health educator are
appointed to deliver care training and exercise programs to patients suffering from
dementia. Caregivers are also given proper training to deal with the patients in a better way.
Comprehensive assessment tools are incorporated in the memory care facility to measure
and monitor patient and caregiver biological, physical and social requirements according to
requirements of both patients and healthcare professionals (Aveyard, 2014).
Local health bodies also provide help and support to the people who are suffering from
dementia by giving them emotional, mental and physical support.
Patient-centred, individualized care protocols that incorporate input from the patient and
caregiver can be launched and implemented by memory care facility organization to
improve the strategies and plans to treat patients with dementia and other mental disabilities.
Family-focused protocols and programs are also conducted by collaborative health
management team to improve family care needs. It also provides enhanced social assistance
with ready availability of communication through telephone or in-person consultation with
NP or SW. They also help in limiting inappropriate and inadequate use of sub acute medical
services such as emergency department, hospitalizations, surgical departments and various
other departments in a hospital (Bongar and Sullivan, 2013).
Care consultation models designed by various healthcare professionals from different health
authorities and hospitals helps in incorporating patient and caregiver needs and
requirements. It aids in improving knowledge, care confidence, command and header skills
(Cuthbert and Insel, 2013). It further also reduces individual health professional load and
stress, which also results in decreasing depression of dementia patients at personal level.
Legal and Ethical dimensions for dementia patient
Legal and ethical dimensions play very important role in care analysis of patients suffering
from mental diseases. These are explained in the following points:
Legal Dimensions: Different Acts, policies and schedules for mental patients have been
implemented by the government of UK. All the Acts and policies are discussed below.
Mental Capacity Act 2007: The Mental Capacity Act was formulated to protect mental
patients who lack the mental capability to make decisions for themselves. The memory care
facility organization in the given scenario is required to follow the act while treating the
dementia patient (Newton, West and Schofield, 2014).
Discrimination and mental illness: Equality Act 2010: The Equality Act 2010 forbids
discrimination on caste, creed, age, sex and colour against patients with mental illness and
governs the authority to protect them accordingly. Data Protection Act 1998: The act is formulated by UK government to protect the data of
patients with severe mental ailments in health and social care setting (Data Protection Act
1988, 2016). It can be analysed that the memory care facility organization needs to abide by
the guidelines of the act to safeguard the personal information of the old dementia patient
from unauthorized access.
Ethical dimensions: The ethical framework in patients with mental illness is based on five
principles. These are as follows:
Liberty: Right to information and self determination should be given to the old patient with
dementia. No decisions related to the patient should be taken without his consent as it is
necessary to maintain confidentiality throughout the treatment (Zeilig, Fox and Killick,
2015). Beneficence: Comfort and benefits should be the prior consideration for the dementia
patient in the given scenario. It is the duty of caregivers at memory care facility to perform
only those tasks which benefits the old patient for his speedy recovery and care (Brody,
2016). Capacity and Competence: Only hospital authorities and officials are allowed to decide
whether a patient is capable of making decisions on his/her own basis (Newton, West and
Schofield, 2014). If a patient refuses to be treated for his\her mental illness, they should not
be forced to undertake the treatment. Quality of Life: Health care providers must observe the affected sufferer carefully and give
whatever means of joy and comfort are possible and on contrary, should try to resist
involvement that decreases the comfort level. The contact of a hand will give greater
comfort than a feeding tube. Further it is very necessary to realize the significance of
emotional and rational well being of the patient suffering from dementia. It is also necessary
Legal Dimensions: Different Acts, policies and schedules for mental patients have been
implemented by the government of UK. All the Acts and policies are discussed below.
Mental Capacity Act 2007: The Mental Capacity Act was formulated to protect mental
patients who lack the mental capability to make decisions for themselves. The memory care
facility organization in the given scenario is required to follow the act while treating the
dementia patient (Newton, West and Schofield, 2014).
Discrimination and mental illness: Equality Act 2010: The Equality Act 2010 forbids
discrimination on caste, creed, age, sex and colour against patients with mental illness and
governs the authority to protect them accordingly. Data Protection Act 1998: The act is formulated by UK government to protect the data of
patients with severe mental ailments in health and social care setting (Data Protection Act
1988, 2016). It can be analysed that the memory care facility organization needs to abide by
the guidelines of the act to safeguard the personal information of the old dementia patient
from unauthorized access.
Ethical dimensions: The ethical framework in patients with mental illness is based on five
principles. These are as follows:
Liberty: Right to information and self determination should be given to the old patient with
dementia. No decisions related to the patient should be taken without his consent as it is
necessary to maintain confidentiality throughout the treatment (Zeilig, Fox and Killick,
2015). Beneficence: Comfort and benefits should be the prior consideration for the dementia
patient in the given scenario. It is the duty of caregivers at memory care facility to perform
only those tasks which benefits the old patient for his speedy recovery and care (Brody,
2016). Capacity and Competence: Only hospital authorities and officials are allowed to decide
whether a patient is capable of making decisions on his/her own basis (Newton, West and
Schofield, 2014). If a patient refuses to be treated for his\her mental illness, they should not
be forced to undertake the treatment. Quality of Life: Health care providers must observe the affected sufferer carefully and give
whatever means of joy and comfort are possible and on contrary, should try to resist
involvement that decreases the comfort level. The contact of a hand will give greater
comfort than a feeding tube. Further it is very necessary to realize the significance of
emotional and rational well being of the patient suffering from dementia. It is also necessary
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
to respect him so that his negativity towards life decreases and he became capable of living
quality life (Gaudine LeFort Lamb and Thorne, 2014). Substituted Legal opinion: Physicians are required to carry out treatment in an effective
way so that the old patient can recover speedily. Without any legal guidance and law the
physicians should follow the hierarchy of informing any complications initially to close
family members of the patient.
Social Duty: All the actions should be agreeable, accountable and transparent. No
discrimination based on age, gender, religion, race, position or rank should be made and all
individuals with mental disability should be treated equally (Brody, 2016).
Roles and responsibilities of mental health nurse.
In order to understand the role and responsibilities of metal health nurse related to care
analysis of the dementia patient in the given scenario following points can be discussed:
Mental health care nurses are usually appointed to understand patients and provide direct
care for better recovery.
It should include enhancing ethnic and emotional needs, managing medication timings and
evaluating the process of improvement in the patient(Newton, West and Schofield, 2014).
These nurses should also cooperate with several interdisciplinary professionals to find out
and provide the best possible care to their patients.
Educating and informing the patients' family about his conditions and severity and how to
create a healthy environment for the patient to recover speedily (Zeilig, Fox and Killick,
2015).
Nurses at memory care facility take care of the old patient by making use of several
monitoring devices to keep a check on the dementia patient in the given scenario.
It is the responsibility of mental health nurse to provide emotional support to the old patient
suffering from dementia as recovery is faster in case of proper mental and emotional
support.
A better sense of communication between the old dementia patient and nurses should be
established so that the elderly patient feels comfortable to discuss his mental state with the
nurse effectively.
A plan of action should be designed according to the habits of the patient with dementia for
better comprehension of likes and dislikes.
It is the responsibility of mental health nurse to ensure that the old patient with dementia is
treated in a very respected and dignified manner so that he does not develop any negative
impact about the suffering he is going through (Zeilig, Fox and Killick, 2015).
Timely and weekly health programs on dementia and memory loss should be provided to the
quality life (Gaudine LeFort Lamb and Thorne, 2014). Substituted Legal opinion: Physicians are required to carry out treatment in an effective
way so that the old patient can recover speedily. Without any legal guidance and law the
physicians should follow the hierarchy of informing any complications initially to close
family members of the patient.
Social Duty: All the actions should be agreeable, accountable and transparent. No
discrimination based on age, gender, religion, race, position or rank should be made and all
individuals with mental disability should be treated equally (Brody, 2016).
Roles and responsibilities of mental health nurse.
In order to understand the role and responsibilities of metal health nurse related to care
analysis of the dementia patient in the given scenario following points can be discussed:
Mental health care nurses are usually appointed to understand patients and provide direct
care for better recovery.
It should include enhancing ethnic and emotional needs, managing medication timings and
evaluating the process of improvement in the patient(Newton, West and Schofield, 2014).
These nurses should also cooperate with several interdisciplinary professionals to find out
and provide the best possible care to their patients.
Educating and informing the patients' family about his conditions and severity and how to
create a healthy environment for the patient to recover speedily (Zeilig, Fox and Killick,
2015).
Nurses at memory care facility take care of the old patient by making use of several
monitoring devices to keep a check on the dementia patient in the given scenario.
It is the responsibility of mental health nurse to provide emotional support to the old patient
suffering from dementia as recovery is faster in case of proper mental and emotional
support.
A better sense of communication between the old dementia patient and nurses should be
established so that the elderly patient feels comfortable to discuss his mental state with the
nurse effectively.
A plan of action should be designed according to the habits of the patient with dementia for
better comprehension of likes and dislikes.
It is the responsibility of mental health nurse to ensure that the old patient with dementia is
treated in a very respected and dignified manner so that he does not develop any negative
impact about the suffering he is going through (Zeilig, Fox and Killick, 2015).
Timely and weekly health programs on dementia and memory loss should be provided to the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
patient and their family members so that they become aware of negative and positive aspects
of the disease.
It is necessary to guarantee safety and sense of self reliance to the old patient in the given
scenario as dementia patients are capable of harming and causing physical pain to
themselves (Newton, West and Schofield, 2014).
It the role of mental health nurse to look after the patient throughout the day. It should be
ensured no kind of physical, social and mental abuse is experienced by the patient.
Different therapies for recovery should be given as per suggested by physician so that the
patient starts living life normally with positivity (Brody, 2016).
It is the responsibility of mental health nurses to treat all patients equally irrespective of
their disease, age, religion and colour.
CONCLUSION
From the above report it can be concluded that in health and social care setting it is very
important to carry out care analysis effectively to promote the health and well being of patients
suffering from acute mental health disorders. It has been observed in the study that there are various
factors that impact the mental health of dementia patients. The factors included are biological,
psychological and social. In addition to this, risk assessment is carried out to identify the risk factors
that can negatively affect the well being of patients suffering from acute metal disorders. Apart from
this risk management is also important part of care analysis to treat service users affected with
different mental disorders. Besides this, legal and ethical dimensions are discussed in the study
which provides essential learning on these two aspects. The final part of the study features the roles
and responsibilities of mental health nurses who play very cardinal role in care analysis of mental
patients.
of the disease.
It is necessary to guarantee safety and sense of self reliance to the old patient in the given
scenario as dementia patients are capable of harming and causing physical pain to
themselves (Newton, West and Schofield, 2014).
It the role of mental health nurse to look after the patient throughout the day. It should be
ensured no kind of physical, social and mental abuse is experienced by the patient.
Different therapies for recovery should be given as per suggested by physician so that the
patient starts living life normally with positivity (Brody, 2016).
It is the responsibility of mental health nurses to treat all patients equally irrespective of
their disease, age, religion and colour.
CONCLUSION
From the above report it can be concluded that in health and social care setting it is very
important to carry out care analysis effectively to promote the health and well being of patients
suffering from acute mental health disorders. It has been observed in the study that there are various
factors that impact the mental health of dementia patients. The factors included are biological,
psychological and social. In addition to this, risk assessment is carried out to identify the risk factors
that can negatively affect the well being of patients suffering from acute metal disorders. Apart from
this risk management is also important part of care analysis to treat service users affected with
different mental disorders. Besides this, legal and ethical dimensions are discussed in the study
which provides essential learning on these two aspects. The final part of the study features the roles
and responsibilities of mental health nurses who play very cardinal role in care analysis of mental
patients.
REFERENCES
Books and Journals
Aveyard, H., 2014. Doing a literature review in health and social care: A practical guide. McGraw-
Hill Education (UK).
Barkley, R. A., 2014. Sluggish cognitive tempo (concentration deficit disorder?): current status,
future directions, and a plea to change the name. Journal of abnormal child psychology. 42(1).
pp.117-125.
Bongar, B. and Sullivan, G., 2013. The suicidal patient: Clinical and legal standards of care .
American Psychological Association.
Bromet, E. J., 2012. Mental health consequences of the Chernobyl disaster. Journal of radiological
protection. 32(1). p.N71.
Cuthbert, B. N. and Insel, T. R., 2013. Toward the future of psychiatric diagnosis: the seven pillars
of RDoC. BMC medicine. 11(1). p.126.
Ellefsen, K. L., 2015. Content Analysis of Archetypal Portrayal of Females in Picture Books Read
in Preschool Classrooms (Doctoral dissertation, Walden University).
Grajales III,and et. al., 2014. Social media: a review and tutorial of applications in medicine and
health care. Journal of medical Internet research. 16(2). p.e13.
Guckenberger, M. and et. al., 2013. Safety and efficacy of stereotactic body radiotherapy for stage I
non–small-cell lung cancer in routine clinical practice: a patterns-of-care and outcome analysis.
Journal of Thoracic Oncology. 8(8). pp.1050-1058.
Kullberg, A., Larsen, J. and Sharp, L., 2013. ‘Why is there another person's name on my infusion
bag?’Patient safety in chemotherapy care–A review of the literature. European Journal of
Oncology Nursing. 17(2). pp.228-235.
McGurk, S. R. and et. al., 2013. Mental health system funding of cognitive enhancement
interventions for schizophrenia: Summary and update of the New York Office of Mental Health
expert panel and stakeholder meeting. Psychiatric rehabilitation journal. 36(3).p.133.
Millar, R. and Hall, K., 2013. Social return on investment (SROI) and performance measurement:
The opportunities and barriers for social enterprises in health and social care. Public
Management Review. 15(6). pp.923-941.
Munn-Giddings, C. and Winter, R., 2013. A handbook for action research in health and social care.
Routledge.
Gaudine, A., LeFort, S., Lamb, M. & Thorne, L. 2014. Ethical conflicts with hospitals: The
perspective of nurses and physicians Nursing Ethics.18(6). pp.756–766.
Weimand, B., Sällström, C., Hall-Lord, M. & Hedelin, B. 2013 Nurses’ dilemmas concerning
support of relatives in mental health care. Nursing Ethics. 20(3). pp.285–299.
Brody, A.A., 2016. Dementia Palliative Care. In Dementia Care. Springer International Publishing.
Zimmerman, S., Sloane, P.D. and Reed, D., 2014. Dementia prevalence and care in assisted living.
Health Affairs. 33(4). pp.658-666.
Brown Wilson, C., Swarbrick, C., Pilling, M. and Keady, J., 2013. The senses in practice: enhancing
the quality of care for residents with dementia in care homes. Journal of advanced nursing.
69(1). pp.77-90.
World Health Organization, 2012. Dementia: a public health priority. World Health Organization.
Newton, P., Reeves, R., West, E. and Schofield, P., 2014. Patient-centred assessment and
management of pain for older adults with dementia in care home and acute settings. Reviews
in Clinical Gerontology. 24(02). pp.139-144.
Zeilig, H., Poland, F., Fox, C. and Killick, J., 2015. The arts in dementia care education: a
developmental study. Journal of Public Mental Health. 14(1). pp.18-23.
Orrell, M., 2012. The new generation of psychosocial interventions for dementia care. The British
Journal of Psychiatry. 201(5). pp.342-343.
Fanning, J., 2013. Risk and the Mental Health Act 2007.Springer International Publishing.
Wood, J., Wood, R., Falkowski, J. and Butler, J., 2015. Community Treatment Orders: Implications
Books and Journals
Aveyard, H., 2014. Doing a literature review in health and social care: A practical guide. McGraw-
Hill Education (UK).
Barkley, R. A., 2014. Sluggish cognitive tempo (concentration deficit disorder?): current status,
future directions, and a plea to change the name. Journal of abnormal child psychology. 42(1).
pp.117-125.
Bongar, B. and Sullivan, G., 2013. The suicidal patient: Clinical and legal standards of care .
American Psychological Association.
Bromet, E. J., 2012. Mental health consequences of the Chernobyl disaster. Journal of radiological
protection. 32(1). p.N71.
Cuthbert, B. N. and Insel, T. R., 2013. Toward the future of psychiatric diagnosis: the seven pillars
of RDoC. BMC medicine. 11(1). p.126.
Ellefsen, K. L., 2015. Content Analysis of Archetypal Portrayal of Females in Picture Books Read
in Preschool Classrooms (Doctoral dissertation, Walden University).
Grajales III,and et. al., 2014. Social media: a review and tutorial of applications in medicine and
health care. Journal of medical Internet research. 16(2). p.e13.
Guckenberger, M. and et. al., 2013. Safety and efficacy of stereotactic body radiotherapy for stage I
non–small-cell lung cancer in routine clinical practice: a patterns-of-care and outcome analysis.
Journal of Thoracic Oncology. 8(8). pp.1050-1058.
Kullberg, A., Larsen, J. and Sharp, L., 2013. ‘Why is there another person's name on my infusion
bag?’Patient safety in chemotherapy care–A review of the literature. European Journal of
Oncology Nursing. 17(2). pp.228-235.
McGurk, S. R. and et. al., 2013. Mental health system funding of cognitive enhancement
interventions for schizophrenia: Summary and update of the New York Office of Mental Health
expert panel and stakeholder meeting. Psychiatric rehabilitation journal. 36(3).p.133.
Millar, R. and Hall, K., 2013. Social return on investment (SROI) and performance measurement:
The opportunities and barriers for social enterprises in health and social care. Public
Management Review. 15(6). pp.923-941.
Munn-Giddings, C. and Winter, R., 2013. A handbook for action research in health and social care.
Routledge.
Gaudine, A., LeFort, S., Lamb, M. & Thorne, L. 2014. Ethical conflicts with hospitals: The
perspective of nurses and physicians Nursing Ethics.18(6). pp.756–766.
Weimand, B., Sällström, C., Hall-Lord, M. & Hedelin, B. 2013 Nurses’ dilemmas concerning
support of relatives in mental health care. Nursing Ethics. 20(3). pp.285–299.
Brody, A.A., 2016. Dementia Palliative Care. In Dementia Care. Springer International Publishing.
Zimmerman, S., Sloane, P.D. and Reed, D., 2014. Dementia prevalence and care in assisted living.
Health Affairs. 33(4). pp.658-666.
Brown Wilson, C., Swarbrick, C., Pilling, M. and Keady, J., 2013. The senses in practice: enhancing
the quality of care for residents with dementia in care homes. Journal of advanced nursing.
69(1). pp.77-90.
World Health Organization, 2012. Dementia: a public health priority. World Health Organization.
Newton, P., Reeves, R., West, E. and Schofield, P., 2014. Patient-centred assessment and
management of pain for older adults with dementia in care home and acute settings. Reviews
in Clinical Gerontology. 24(02). pp.139-144.
Zeilig, H., Poland, F., Fox, C. and Killick, J., 2015. The arts in dementia care education: a
developmental study. Journal of Public Mental Health. 14(1). pp.18-23.
Orrell, M., 2012. The new generation of psychosocial interventions for dementia care. The British
Journal of Psychiatry. 201(5). pp.342-343.
Fanning, J., 2013. Risk and the Mental Health Act 2007.Springer International Publishing.
Wood, J., Wood, R., Falkowski, J. and Butler, J., 2015. Community Treatment Orders: Implications
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




