Care of Older Person with Cognitive Impairment: Delirium Management
VerifiedAdded on 2021/06/15
|13
|3173
|31
Report
AI Summary
This report focuses on the critical issue of delirium management in older adults, a common form of cognitive impairment. It explores various aspects of delirium, including the challenges in diagnosis due to its similarity with dementia, the importance of cognitive assessments, and the high mortality rate associated with the condition. The report provides five best practice recommendations: proper diagnosis through patient history and cognitive testing, prevention strategies targeting risk factors, fall prevention interventions, medication use (specifically antipsychotics for severe cases), and patient/family education. It also addresses nursing management of post-operative delirium, emphasizing fluid management, infection prevention, mobility, and medication minimization. The report highlights the impact of these recommendations on nursing practices, emphasizing the importance of early diagnosis, non-pharmacological interventions, and patient education to improve care and outcomes for older adults experiencing delirium.

Running head: CARE OF OLDER PERSON WITH COGNITIVE IMPAIRMENT
CARE OF OLDER PERSON WITH COGNITIVE IMPAIRMENT
Name of the student:
Name of the University:
Author note:
CARE OF OLDER PERSON WITH COGNITIVE IMPAIRMENT
Name of the student:
Name of the University:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1CARE OF OLDER PERSON WITH COGNITIVE IMPAIRMENT
Table of Contents
1. Introduction:........................................................................................................................2
2. Discussion:..........................................................................................................................2
2.1 Issue Related to Delirium:...........................................................................................2
2.2 Best Practice Recommendations:................................................................................3
2.3 Nursing Management of Post-operative Delirium in Older People:...........................8
2.4 Impact of the Recommendations on Nursing Management:.......................................9
3. Summary:............................................................................................................................9
Reference:................................................................................................................................11
Table of Contents
1. Introduction:........................................................................................................................2
2. Discussion:..........................................................................................................................2
2.1 Issue Related to Delirium:...........................................................................................2
2.2 Best Practice Recommendations:................................................................................3
2.3 Nursing Management of Post-operative Delirium in Older People:...........................8
2.4 Impact of the Recommendations on Nursing Management:.......................................9
3. Summary:............................................................................................................................9
Reference:................................................................................................................................11
2CARE OF OLDER PERSON WITH COGNITIVE IMPAIRMENT
1. Introduction:
Cognitive impairment is a condition of illness in which a person faces difficulties in
remembering, concentrating and learning things and lacks ability of taking decisions in their
regular life (Rock et al., 2014). The symptoms affect the daily life of the patient in an
effective way. Older people are more prone to the symptoms of cognitive impairment
(Mitchell et al., 2014). There are different forms of cognitive impairment such as dementia,
delirium and depression (Freitas et al., 2013). The chosen form of cognitive impairment for
the essay is delirium. The following paper will provide a brief idea about the relevant issue
regarding delirium, evidence supporting the issue, recommendations related practice and
clinical situation, evaluation of such recommendation regarding quality, clinical relevance
and applicability, nursing recommendations and a summary of the findings for face-to-face
tutorials.
2. Discussion:
2.1 Issue Related to Delirium:
There are many issues related to delirium in adults and older people. One of the main
issues regarding the older person is delirium management of older people in hospital.
Delirium is common in the hospitalized patients, mostly in the older person (Kalish, Gillham
& Unwin, 2014). The main problem is to recognize the illness, as the symptoms are alike
dementia. The fluctuating nature of the person makes it difficult to recognize the proper
symptoms (Gélinas et al.,2013). Thus, clinicians face some complexity to understand that
whether the person is suffering from delirium or dementia. The main reason of such
difficulties is the use of inadequate cognitive assessment and poor management in the
hospital (Freitas, S., Simões, Alves & Santana, 2013). It is important to diagnose the disease
1. Introduction:
Cognitive impairment is a condition of illness in which a person faces difficulties in
remembering, concentrating and learning things and lacks ability of taking decisions in their
regular life (Rock et al., 2014). The symptoms affect the daily life of the patient in an
effective way. Older people are more prone to the symptoms of cognitive impairment
(Mitchell et al., 2014). There are different forms of cognitive impairment such as dementia,
delirium and depression (Freitas et al., 2013). The chosen form of cognitive impairment for
the essay is delirium. The following paper will provide a brief idea about the relevant issue
regarding delirium, evidence supporting the issue, recommendations related practice and
clinical situation, evaluation of such recommendation regarding quality, clinical relevance
and applicability, nursing recommendations and a summary of the findings for face-to-face
tutorials.
2. Discussion:
2.1 Issue Related to Delirium:
There are many issues related to delirium in adults and older people. One of the main
issues regarding the older person is delirium management of older people in hospital.
Delirium is common in the hospitalized patients, mostly in the older person (Kalish, Gillham
& Unwin, 2014). The main problem is to recognize the illness, as the symptoms are alike
dementia. The fluctuating nature of the person makes it difficult to recognize the proper
symptoms (Gélinas et al.,2013). Thus, clinicians face some complexity to understand that
whether the person is suffering from delirium or dementia. The main reason of such
difficulties is the use of inadequate cognitive assessment and poor management in the
hospital (Freitas, S., Simões, Alves & Santana, 2013). It is important to diagnose the disease
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3CARE OF OLDER PERSON WITH COGNITIVE IMPAIRMENT
properly as a patient with delirium has high mortality rate. Hence, the poor delirium
recognizing process and the hospital management become a headache in order to manage
older person with delirium.
2.2 Best Practice Recommendations:
Best Practice Recommendation 1:
Proper diagnosis of delirium is important as the condition may lead to end of life issue
in the older people. Diagnosis need to be done in the basis of history of the patient,
because in many cases the symptoms arise due to effect of some past head injury, stroke
or other accidents. Hence, mental status assessment and some physical and neurological
tests are required to determine the nature of the illness. Cognitive testing need to be
provided to the patient to understand the different risk factors and to differentiate between
dementia and delirium (Hosie et al., 2013)
Quality and Level of the Evidence:
The recommendation is not based on high quality evidence. Many questions can be
raised regarding the clinical guideline. For example, whether the screening process is cost
effective or not, if it is acceptable to the patient and the role of such screening in
decreasing the mortality rate. However, researchers have stated that such screening test is
important to understand the severity of delirium and provide effective treatment to the
patient.
Clinical Relevance of the Evidence:
The recommendation regarding proper diagnosis of delirium is highly recommended
in the clinical practice. Cognitive test of every old age patient in the hospital before
admission is important to identify delirium within him or her. It will help to understand
properly as a patient with delirium has high mortality rate. Hence, the poor delirium
recognizing process and the hospital management become a headache in order to manage
older person with delirium.
2.2 Best Practice Recommendations:
Best Practice Recommendation 1:
Proper diagnosis of delirium is important as the condition may lead to end of life issue
in the older people. Diagnosis need to be done in the basis of history of the patient,
because in many cases the symptoms arise due to effect of some past head injury, stroke
or other accidents. Hence, mental status assessment and some physical and neurological
tests are required to determine the nature of the illness. Cognitive testing need to be
provided to the patient to understand the different risk factors and to differentiate between
dementia and delirium (Hosie et al., 2013)
Quality and Level of the Evidence:
The recommendation is not based on high quality evidence. Many questions can be
raised regarding the clinical guideline. For example, whether the screening process is cost
effective or not, if it is acceptable to the patient and the role of such screening in
decreasing the mortality rate. However, researchers have stated that such screening test is
important to understand the severity of delirium and provide effective treatment to the
patient.
Clinical Relevance of the Evidence:
The recommendation regarding proper diagnosis of delirium is highly recommended
in the clinical practice. Cognitive test of every old age patient in the hospital before
admission is important to identify delirium within him or her. It will help to understand
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4CARE OF OLDER PERSON WITH COGNITIVE IMPAIRMENT
the severity of the illness. The process can be proved efficient in reducing the severe
outcomes of delirium in older person.
Applicability of the Evidence:
The quality of the evidence not high, still it can be applied as clinical process
regarding the cure of delirium. It is important to recognize the nature of the disease in
order to cure it. Thus, without appropriate evidence, it is applicable to address the issue
of delirium management in older person in the hospital.
Best Practice Recommendation 2:
Prevention of delirium can decrease the rate of delirium in the older persons.
Prevention process needs to be done from the admission of the patient to throughout the
stay. The target area of the prevention process should be the risk factors of delirium
(Abraha, 2016). Some non-pharmacological process can be used as prevention of
delirium, such as inspire the patient for normal sleep-wake practice, allowing visit of the
family members, less changes in the nursing staff, mobilization and providing patient
friendly environment in the hospital (Devlin & Pohlman, 2014).
Quality and Level of the Evidence:
The quality of the recommendation is moderate. It is not ensured that such method
can prevent the risk factors of delirium, but according to the experts, such process of
prevention can reduce the incidence of delirium to an extent. Thus, the recommendation
can be proved helpful in managing delirium.
Clinical Relevance of the Evidence:
the severity of the illness. The process can be proved efficient in reducing the severe
outcomes of delirium in older person.
Applicability of the Evidence:
The quality of the evidence not high, still it can be applied as clinical process
regarding the cure of delirium. It is important to recognize the nature of the disease in
order to cure it. Thus, without appropriate evidence, it is applicable to address the issue
of delirium management in older person in the hospital.
Best Practice Recommendation 2:
Prevention of delirium can decrease the rate of delirium in the older persons.
Prevention process needs to be done from the admission of the patient to throughout the
stay. The target area of the prevention process should be the risk factors of delirium
(Abraha, 2016). Some non-pharmacological process can be used as prevention of
delirium, such as inspire the patient for normal sleep-wake practice, allowing visit of the
family members, less changes in the nursing staff, mobilization and providing patient
friendly environment in the hospital (Devlin & Pohlman, 2014).
Quality and Level of the Evidence:
The quality of the recommendation is moderate. It is not ensured that such method
can prevent the risk factors of delirium, but according to the experts, such process of
prevention can reduce the incidence of delirium to an extent. Thus, the recommendation
can be proved helpful in managing delirium.
Clinical Relevance of the Evidence:
5CARE OF OLDER PERSON WITH COGNITIVE IMPAIRMENT
The recommendation regarding prevention of delirium is mostly acceptable in the
clinical practice. If prevention process is done to every older person in the hospital, the
risk of suffering from delirium may be reduced. Thus, providing better environment and
care in order to prevent delirium in older person in the hospital from beginning is one of
the best recommendations in clinical practice.
Applicability of the Evidence:
The recommendation is highly acceptable in clinical practice as the process is low
cost effective. Such prevention process can decrease the number of incidents of delirium
in the older person. If the process cannot prevent the illness from being occurred, it can
still reduce the functional decline in the patient. Hence, the recommendation is acceptable
to the clinicians and the patients as well in order to solve the issue of delirium
management.
Best Practice Recommendation 3:
There is a risk factor of falls in the older persons with delirium. People with delirium
are more prone to falls; approximately, twice than a person who is cognitively intact
(Zaal et al., 2015). The falls may result in fatal or non-fatal injury. Functional recovery of
the injury is difficult for the person suffering from delirium (Winter, Watt & Peel, 2013).
It is important to take care of such person in an effective manner .Thus, fall prevention
interventions are required to reduce the risk factor. Knowledgeable caregiver is needed to
manage such older persons.
Quality and Level of the Evidence:
High quality evidences are not available for the recommendation. The numbers of
interventions that can be used in order to prevent the risk of fall in the older person with
The recommendation regarding prevention of delirium is mostly acceptable in the
clinical practice. If prevention process is done to every older person in the hospital, the
risk of suffering from delirium may be reduced. Thus, providing better environment and
care in order to prevent delirium in older person in the hospital from beginning is one of
the best recommendations in clinical practice.
Applicability of the Evidence:
The recommendation is highly acceptable in clinical practice as the process is low
cost effective. Such prevention process can decrease the number of incidents of delirium
in the older person. If the process cannot prevent the illness from being occurred, it can
still reduce the functional decline in the patient. Hence, the recommendation is acceptable
to the clinicians and the patients as well in order to solve the issue of delirium
management.
Best Practice Recommendation 3:
There is a risk factor of falls in the older persons with delirium. People with delirium
are more prone to falls; approximately, twice than a person who is cognitively intact
(Zaal et al., 2015). The falls may result in fatal or non-fatal injury. Functional recovery of
the injury is difficult for the person suffering from delirium (Winter, Watt & Peel, 2013).
It is important to take care of such person in an effective manner .Thus, fall prevention
interventions are required to reduce the risk factor. Knowledgeable caregiver is needed to
manage such older persons.
Quality and Level of the Evidence:
High quality evidences are not available for the recommendation. The numbers of
interventions that can be used in order to prevent the risk of fall in the older person with
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6CARE OF OLDER PERSON WITH COGNITIVE IMPAIRMENT
delirium are limited. However, study has proved that, interventions for prevent the risk of
fall is important as it can cause mild to severe injury. Use of reliable and valuable process
to prevent falls is important. The recommendation is useful with the support of experts.
Clinical Relevance of the Evidence:
The recommendation of falls prevention interventions is relevant to clinical practice.
Older person with delirium, especially over 75 years age, are more prone to falls. Proper
caregiver is required to pay attention to such person. Implementation of the
recommendation can be proved beneficial for managing older people with delirium in the
hospital.
Applicability of the Evidence:
However, there are very few evidences regarding falls prevention interventions, but it
is important to apply this recommendation in the clinical practice. Such interventions
could reduce the risk of falls in the older persons. Thus, best practice recommendation 3
is applicable in order to counter the issue of managing older person with delirium in
hospital.
Best Practice Recommendation 4:
Medication for delirium is not always applicable, but in case of severe delirium in
older person, medication is provided in order to reduce the severity of the illness. To
control the aggressiveness of the patients, antipsychotic medication such as Haloperidol
can be provided (Meagher et al., 2013).
Quality and Level of the Evidence:
delirium are limited. However, study has proved that, interventions for prevent the risk of
fall is important as it can cause mild to severe injury. Use of reliable and valuable process
to prevent falls is important. The recommendation is useful with the support of experts.
Clinical Relevance of the Evidence:
The recommendation of falls prevention interventions is relevant to clinical practice.
Older person with delirium, especially over 75 years age, are more prone to falls. Proper
caregiver is required to pay attention to such person. Implementation of the
recommendation can be proved beneficial for managing older people with delirium in the
hospital.
Applicability of the Evidence:
However, there are very few evidences regarding falls prevention interventions, but it
is important to apply this recommendation in the clinical practice. Such interventions
could reduce the risk of falls in the older persons. Thus, best practice recommendation 3
is applicable in order to counter the issue of managing older person with delirium in
hospital.
Best Practice Recommendation 4:
Medication for delirium is not always applicable, but in case of severe delirium in
older person, medication is provided in order to reduce the severity of the illness. To
control the aggressiveness of the patients, antipsychotic medication such as Haloperidol
can be provided (Meagher et al., 2013).
Quality and Level of the Evidence:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7CARE OF OLDER PERSON WITH COGNITIVE IMPAIRMENT
The quality of the evidence not high, as there is limited information in the evidence.
Side effects of the medication are not mentioned properly. Still the recommendation is
useful, as many knowledgeable experts have supported the evidence with their concern.
Clinical Relevance of the Evidence:
The recommendation is relevant to the clinical practice. Antipsychotic medication is
useful in controlling the aggressiveness of the patient. It is important for the clinicians to
know the limitations of the medication.
Applicability of the Evidence:
The best recommendation 4 is applicable in clinical practice in order to control the
aggressive patients. Though medication is not always needed for every person with
delirium, but in case of older people with severe illness, the medication is helpful.
Best Practice Recommendation 5:
People are not informed properly about delirium and its effects. It is important to
provide proper information regarding delirium to every people, so that they can
understand the importance of the treatment. The information that will be provided should
be collect considering culture and ethics. It will help individual to accept the treatment
procedure (Yanamadal, Wieland & Heflin, 2013).
Quality and Level of the Evidence:
The evidence for best recommendation 4 is appropriate. The evidence has provided
importance of intervention of education in order to make it understandable to all.
However, the information needs to be acceptable to all.
Clinical Relevance of the Evidence:
The quality of the evidence not high, as there is limited information in the evidence.
Side effects of the medication are not mentioned properly. Still the recommendation is
useful, as many knowledgeable experts have supported the evidence with their concern.
Clinical Relevance of the Evidence:
The recommendation is relevant to the clinical practice. Antipsychotic medication is
useful in controlling the aggressiveness of the patient. It is important for the clinicians to
know the limitations of the medication.
Applicability of the Evidence:
The best recommendation 4 is applicable in clinical practice in order to control the
aggressive patients. Though medication is not always needed for every person with
delirium, but in case of older people with severe illness, the medication is helpful.
Best Practice Recommendation 5:
People are not informed properly about delirium and its effects. It is important to
provide proper information regarding delirium to every people, so that they can
understand the importance of the treatment. The information that will be provided should
be collect considering culture and ethics. It will help individual to accept the treatment
procedure (Yanamadal, Wieland & Heflin, 2013).
Quality and Level of the Evidence:
The evidence for best recommendation 4 is appropriate. The evidence has provided
importance of intervention of education in order to make it understandable to all.
However, the information needs to be acceptable to all.
Clinical Relevance of the Evidence:
8CARE OF OLDER PERSON WITH COGNITIVE IMPAIRMENT
The recommendation is relevant to clinical practice as information provided by the
clinicians to the patients and their families will help them to understand the condition of
the patient in a better way.
Applicability of the Evidence:
Providing knowledge is something that is applicable in any field. Application of such
recommendation is useful to expand the information about delirium prevention or
treatment. It will help to create awareness about the illness and clear confusion regarding
this.
2.3 Nursing Management of Post-operative Delirium in Older People:
Post-operative delirium occurs in older people after major surgery. Study has shown
that older person with gastrointestinal surgery are more prone to post-operative delirium
(Scholz et al., 2016). There are many ways of managing such patients. It is important to
provide enough fluid to an older person in order to avoid dehydration. Proper dressing is
required after surgery to prevent infection. The nurses should make sure that patients are
walking multiple times per day. Orientation of the patient to their known location is
important. The nurses should remain aware of minimizing the use of medicine for sleep. Non-
opioid medication can be provided to the patients in order to minimize the pain. There is no
proper evidence regarding the treatment of post-operative delirium. However, treatment of
post-operative delirium is important as it can affect both physical and mental health of the
patient and even can cause death (Bilotta et al., 2013).
2.4 Impact of the Recommendations on Nursing Management:
The recommendations could play an important role in improving the process of
nursing management. Proper diagnosis is an important factor to resolve the issue of delirium
management and it will help the nurses to understand the nature of the illness (Grassi et al.,
The recommendation is relevant to clinical practice as information provided by the
clinicians to the patients and their families will help them to understand the condition of
the patient in a better way.
Applicability of the Evidence:
Providing knowledge is something that is applicable in any field. Application of such
recommendation is useful to expand the information about delirium prevention or
treatment. It will help to create awareness about the illness and clear confusion regarding
this.
2.3 Nursing Management of Post-operative Delirium in Older People:
Post-operative delirium occurs in older people after major surgery. Study has shown
that older person with gastrointestinal surgery are more prone to post-operative delirium
(Scholz et al., 2016). There are many ways of managing such patients. It is important to
provide enough fluid to an older person in order to avoid dehydration. Proper dressing is
required after surgery to prevent infection. The nurses should make sure that patients are
walking multiple times per day. Orientation of the patient to their known location is
important. The nurses should remain aware of minimizing the use of medicine for sleep. Non-
opioid medication can be provided to the patients in order to minimize the pain. There is no
proper evidence regarding the treatment of post-operative delirium. However, treatment of
post-operative delirium is important as it can affect both physical and mental health of the
patient and even can cause death (Bilotta et al., 2013).
2.4 Impact of the Recommendations on Nursing Management:
The recommendations could play an important role in improving the process of
nursing management. Proper diagnosis is an important factor to resolve the issue of delirium
management and it will help the nurses to understand the nature of the illness (Grassi et al.,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9CARE OF OLDER PERSON WITH COGNITIVE IMPAIRMENT
2015). Non-pharmacological treatment is important to prevent or reduce the risk factors of
delirium and it could help to reduce the headache of the management by reducing the
number of incidence of delirium. Proper information provided by the clinicians will help the
patient to understand treatment process and it will decrease the difficulties of the nurses in
providing care.
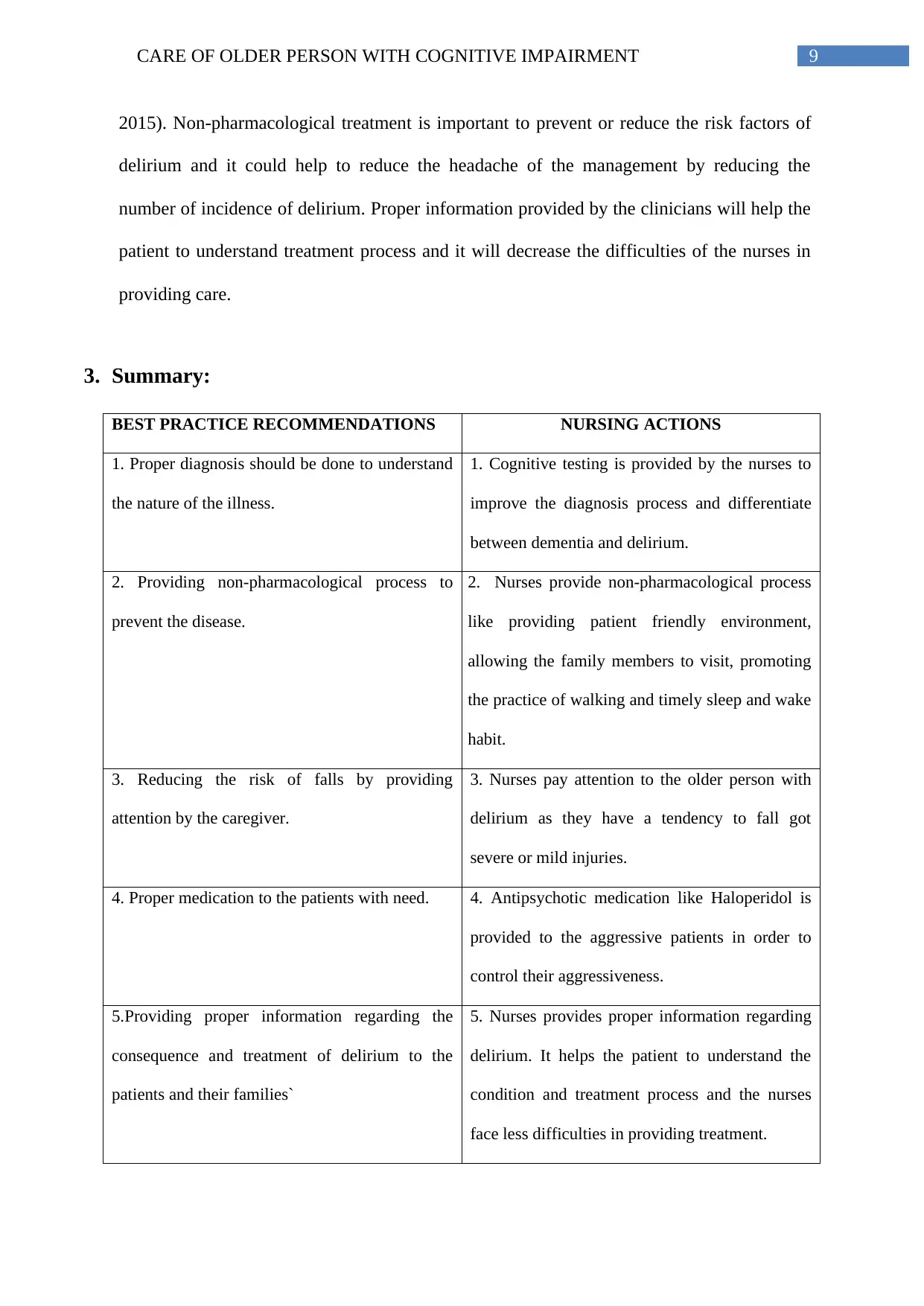
3. Summary:
BEST PRACTICE RECOMMENDATIONS NURSING ACTIONS
1. Proper diagnosis should be done to understand
the nature of the illness.
1. Cognitive testing is provided by the nurses to
improve the diagnosis process and differentiate
between dementia and delirium.
2. Providing non-pharmacological process to
prevent the disease.
2. Nurses provide non-pharmacological process
like providing patient friendly environment,
allowing the family members to visit, promoting
the practice of walking and timely sleep and wake
habit.
3. Reducing the risk of falls by providing
attention by the caregiver.
3. Nurses pay attention to the older person with
delirium as they have a tendency to fall got
severe or mild injuries.
4. Proper medication to the patients with need. 4. Antipsychotic medication like Haloperidol is
provided to the aggressive patients in order to
control their aggressiveness.
5.Providing proper information regarding the
consequence and treatment of delirium to the
patients and their families`
5. Nurses provides proper information regarding
delirium. It helps the patient to understand the
condition and treatment process and the nurses
face less difficulties in providing treatment.
2015). Non-pharmacological treatment is important to prevent or reduce the risk factors of
delirium and it could help to reduce the headache of the management by reducing the
number of incidence of delirium. Proper information provided by the clinicians will help the
patient to understand treatment process and it will decrease the difficulties of the nurses in
providing care.
3. Summary:
BEST PRACTICE RECOMMENDATIONS NURSING ACTIONS
1. Proper diagnosis should be done to understand
the nature of the illness.
1. Cognitive testing is provided by the nurses to
improve the diagnosis process and differentiate
between dementia and delirium.
2. Providing non-pharmacological process to
prevent the disease.
2. Nurses provide non-pharmacological process
like providing patient friendly environment,
allowing the family members to visit, promoting
the practice of walking and timely sleep and wake
habit.
3. Reducing the risk of falls by providing
attention by the caregiver.
3. Nurses pay attention to the older person with
delirium as they have a tendency to fall got
severe or mild injuries.
4. Proper medication to the patients with need. 4. Antipsychotic medication like Haloperidol is
provided to the aggressive patients in order to
control their aggressiveness.
5.Providing proper information regarding the
consequence and treatment of delirium to the
patients and their families`
5. Nurses provides proper information regarding
delirium. It helps the patient to understand the
condition and treatment process and the nurses
face less difficulties in providing treatment.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

10CARE OF OLDER PERSON WITH COGNITIVE IMPAIRMENT
.
.
11CARE OF OLDER PERSON WITH COGNITIVE IMPAIRMENT
Reference:
Abraha, I., Rimland, J. M., Trotta, F., Pierini, V., Cruz-Jentoft, A., Soiza, R., ... & Cherubini,
A. (2016). Non-pharmacological interventions to prevent or treat delirium in older
patients: clinical practice recommendations the SENATOR-ONTOP series. The
journal of nutrition, health & aging, 20(9), 927-936.
Bilotta, F., Lauretta, M. P., Borozdina, A., Mizikov, V. M., & Rosa, G. (2013). Postoperative
delirium: risk factors, diagnosis and perioperative care. Minerva Anestesiol, 79(9),
1066-1076.
Devlin, J. W., & Pohlman, A. S. (2014). Everybody, every day: an “awakening and breathing
coordination, delirium monitoring/management, and early exercise/mobility” culture
is feasible in your ICU. Critical care medicine, 42(5), 1280-1281.
Freitas, S., Simões, M. R., Alves, L., & Santana, I. (2013). Montreal cognitive assessment:
validation study for mild cognitive impairment and Alzheimer disease. Alzheimer
Disease & Associated Disorders, 27(1), 37-43.
Freitas, S., Simões, M. R., Alves, L., & Santana, I. (2013). Montreal cognitive assessment:
validation study for mild cognitive impairment and Alzheimer disease. Alzheimer
Disease & Associated Disorders, 27(1), 37-43.
Gélinas, C., Klein, K., Naidech, A. M., & Skrobik, Y. (2013). Pain, sedation, and delirium
management in the neurocritically ill: lessons learned from recent research.
In Seminars in respiratory and critical care medicine (Vol. 34, No. 02, pp. 236-243).
Thieme Medical Publishers.
Reference:
Abraha, I., Rimland, J. M., Trotta, F., Pierini, V., Cruz-Jentoft, A., Soiza, R., ... & Cherubini,
A. (2016). Non-pharmacological interventions to prevent or treat delirium in older
patients: clinical practice recommendations the SENATOR-ONTOP series. The
journal of nutrition, health & aging, 20(9), 927-936.
Bilotta, F., Lauretta, M. P., Borozdina, A., Mizikov, V. M., & Rosa, G. (2013). Postoperative
delirium: risk factors, diagnosis and perioperative care. Minerva Anestesiol, 79(9),
1066-1076.
Devlin, J. W., & Pohlman, A. S. (2014). Everybody, every day: an “awakening and breathing
coordination, delirium monitoring/management, and early exercise/mobility” culture
is feasible in your ICU. Critical care medicine, 42(5), 1280-1281.
Freitas, S., Simões, M. R., Alves, L., & Santana, I. (2013). Montreal cognitive assessment:
validation study for mild cognitive impairment and Alzheimer disease. Alzheimer
Disease & Associated Disorders, 27(1), 37-43.
Freitas, S., Simões, M. R., Alves, L., & Santana, I. (2013). Montreal cognitive assessment:
validation study for mild cognitive impairment and Alzheimer disease. Alzheimer
Disease & Associated Disorders, 27(1), 37-43.
Gélinas, C., Klein, K., Naidech, A. M., & Skrobik, Y. (2013). Pain, sedation, and delirium
management in the neurocritically ill: lessons learned from recent research.
In Seminars in respiratory and critical care medicine (Vol. 34, No. 02, pp. 236-243).
Thieme Medical Publishers.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





