Care Plan for Mr. Ron Fraser: Addressing Gaseous Exchange & Overload
VerifiedAdded on 2023/06/13
|7
|1810
|475
Case Study
AI Summary
This assignment presents two comprehensive care plans for Mr. Ron Fraser, a patient experiencing deteriorating kidney function. The first care plan addresses ineffective gaseous exchange related to pulmonary edema secondary to heart failure, outlining interventions such as oxygen administration, semi-Fowler's positioning, diuretic administration, and promoting rest. The second care plan focuses on fluid volume overload related to decreased kidney function, detailing interventions like diuretic administration, sodium and fluid restriction, monitoring input and output, and patient education. Both care plans include nursing diagnoses, SMART goals, priority nursing actions, and rationales for each action, aiming to improve the patient's condition and overall health outcome. Desklib offers a wealth of similar solved assignments and study resources for students.
CARE PLAN TEMPLATE
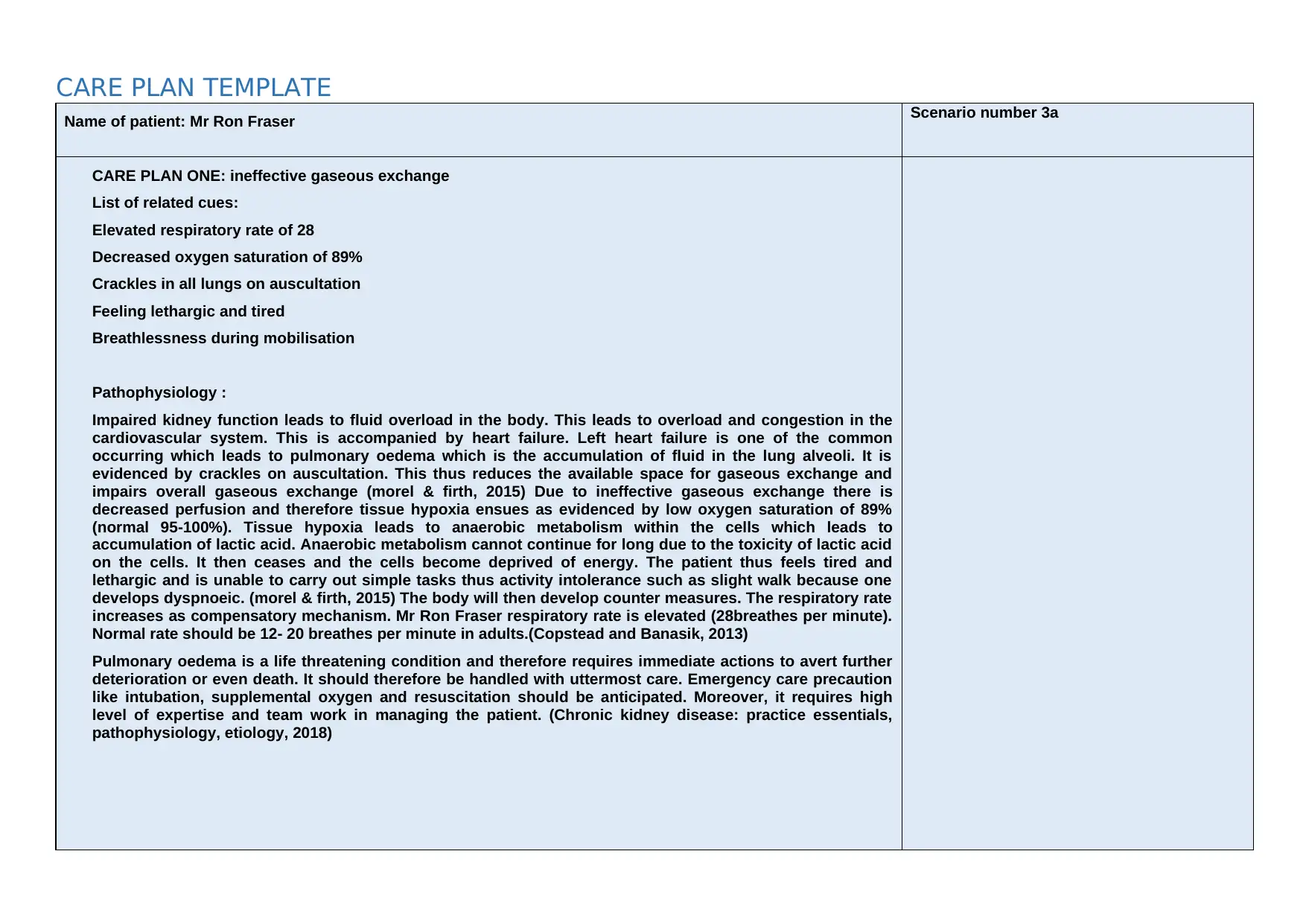
Name of patient: Mr Ron Fraser Scenario number 3a
CARE PLAN ONE: ineffective gaseous exchange
List of related cues:
Elevated respiratory rate of 28
Decreased oxygen saturation of 89%
Crackles in all lungs on auscultation
Feeling lethargic and tired
Breathlessness during mobilisation
Pathophysiology :
Impaired kidney function leads to fluid overload in the body. This leads to overload and congestion in the
cardiovascular system. This is accompanied by heart failure. Left heart failure is one of the common
occurring which leads to pulmonary oedema which is the accumulation of fluid in the lung alveoli. It is
evidenced by crackles on auscultation. This thus reduces the available space for gaseous exchange and
impairs overall gaseous exchange (morel & firth, 2015) Due to ineffective gaseous exchange there is
decreased perfusion and therefore tissue hypoxia ensues as evidenced by low oxygen saturation of 89%
(normal 95-100%). Tissue hypoxia leads to anaerobic metabolism within the cells which leads to
accumulation of lactic acid. Anaerobic metabolism cannot continue for long due to the toxicity of lactic acid
on the cells. It then ceases and the cells become deprived of energy. The patient thus feels tired and
lethargic and is unable to carry out simple tasks thus activity intolerance such as slight walk because one
develops dyspnoeic. (morel & firth, 2015) The body will then develop counter measures. The respiratory rate
increases as compensatory mechanism. Mr Ron Fraser respiratory rate is elevated (28breathes per minute).
Normal rate should be 12- 20 breathes per minute in adults.(Copstead and Banasik, 2013)
Pulmonary oedema is a life threatening condition and therefore requires immediate actions to avert further
deterioration or even death. It should therefore be handled with uttermost care. Emergency care precaution
like intubation, supplemental oxygen and resuscitation should be anticipated. Moreover, it requires high
level of expertise and team work in managing the patient. (Chronic kidney disease: practice essentials,
pathophysiology, etiology, 2018)
Name of patient: Mr Ron Fraser Scenario number 3a
CARE PLAN ONE: ineffective gaseous exchange
List of related cues:
Elevated respiratory rate of 28
Decreased oxygen saturation of 89%
Crackles in all lungs on auscultation
Feeling lethargic and tired
Breathlessness during mobilisation
Pathophysiology :
Impaired kidney function leads to fluid overload in the body. This leads to overload and congestion in the
cardiovascular system. This is accompanied by heart failure. Left heart failure is one of the common
occurring which leads to pulmonary oedema which is the accumulation of fluid in the lung alveoli. It is
evidenced by crackles on auscultation. This thus reduces the available space for gaseous exchange and
impairs overall gaseous exchange (morel & firth, 2015) Due to ineffective gaseous exchange there is
decreased perfusion and therefore tissue hypoxia ensues as evidenced by low oxygen saturation of 89%
(normal 95-100%). Tissue hypoxia leads to anaerobic metabolism within the cells which leads to
accumulation of lactic acid. Anaerobic metabolism cannot continue for long due to the toxicity of lactic acid
on the cells. It then ceases and the cells become deprived of energy. The patient thus feels tired and
lethargic and is unable to carry out simple tasks thus activity intolerance such as slight walk because one
develops dyspnoeic. (morel & firth, 2015) The body will then develop counter measures. The respiratory rate
increases as compensatory mechanism. Mr Ron Fraser respiratory rate is elevated (28breathes per minute).
Normal rate should be 12- 20 breathes per minute in adults.(Copstead and Banasik, 2013)
Pulmonary oedema is a life threatening condition and therefore requires immediate actions to avert further
deterioration or even death. It should therefore be handled with uttermost care. Emergency care precaution
like intubation, supplemental oxygen and resuscitation should be anticipated. Moreover, it requires high
level of expertise and team work in managing the patient. (Chronic kidney disease: practice essentials,
pathophysiology, etiology, 2018)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CARE PLAN TEMPLATE
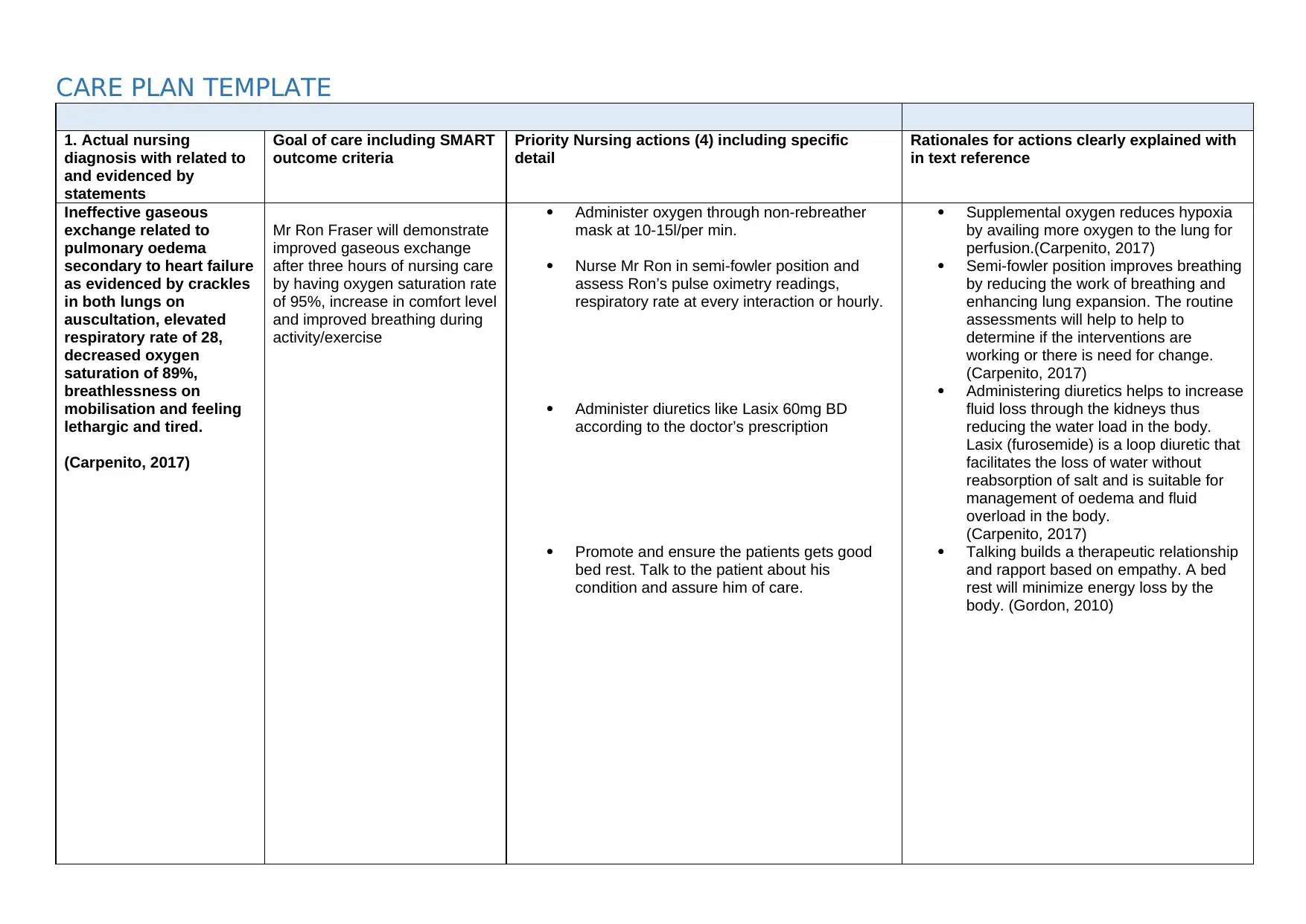
1. Actual nursing
diagnosis with related to
and evidenced by
statements
Goal of care including SMART
outcome criteria
Priority Nursing actions (4) including specific
detail
Rationales for actions clearly explained with
in text reference
Ineffective gaseous
exchange related to
pulmonary oedema
secondary to heart failure
as evidenced by crackles
in both lungs on
auscultation, elevated
respiratory rate of 28,
decreased oxygen
saturation of 89%,
breathlessness on
mobilisation and feeling
lethargic and tired.
(Carpenito, 2017)
Mr Ron Fraser will demonstrate
improved gaseous exchange
after three hours of nursing care
by having oxygen saturation rate
of 95%, increase in comfort level
and improved breathing during
activity/exercise
Administer oxygen through non-rebreather
mask at 10-15l/per min.
Nurse Mr Ron in semi-fowler position and
assess Ron’s pulse oximetry readings,
respiratory rate at every interaction or hourly.
Administer diuretics like Lasix 60mg BD
according to the doctor’s prescription
Promote and ensure the patients gets good
bed rest. Talk to the patient about his
condition and assure him of care.
Supplemental oxygen reduces hypoxia
by availing more oxygen to the lung for
perfusion.(Carpenito, 2017)
Semi-fowler position improves breathing
by reducing the work of breathing and
enhancing lung expansion. The routine
assessments will help to help to
determine if the interventions are
working or there is need for change.
(Carpenito, 2017)
Administering diuretics helps to increase
fluid loss through the kidneys thus
reducing the water load in the body.
Lasix (furosemide) is a loop diuretic that
facilitates the loss of water without
reabsorption of salt and is suitable for
management of oedema and fluid
overload in the body.
(Carpenito, 2017)
Talking builds a therapeutic relationship
and rapport based on empathy. A bed
rest will minimize energy loss by the
body. (Gordon, 2010)
1. Actual nursing
diagnosis with related to
and evidenced by
statements
Goal of care including SMART
outcome criteria
Priority Nursing actions (4) including specific
detail
Rationales for actions clearly explained with
in text reference
Ineffective gaseous
exchange related to
pulmonary oedema
secondary to heart failure
as evidenced by crackles
in both lungs on
auscultation, elevated
respiratory rate of 28,
decreased oxygen
saturation of 89%,
breathlessness on
mobilisation and feeling
lethargic and tired.
(Carpenito, 2017)
Mr Ron Fraser will demonstrate
improved gaseous exchange
after three hours of nursing care
by having oxygen saturation rate
of 95%, increase in comfort level
and improved breathing during
activity/exercise
Administer oxygen through non-rebreather
mask at 10-15l/per min.
Nurse Mr Ron in semi-fowler position and
assess Ron’s pulse oximetry readings,
respiratory rate at every interaction or hourly.
Administer diuretics like Lasix 60mg BD
according to the doctor’s prescription
Promote and ensure the patients gets good
bed rest. Talk to the patient about his
condition and assure him of care.
Supplemental oxygen reduces hypoxia
by availing more oxygen to the lung for
perfusion.(Carpenito, 2017)
Semi-fowler position improves breathing
by reducing the work of breathing and
enhancing lung expansion. The routine
assessments will help to help to
determine if the interventions are
working or there is need for change.
(Carpenito, 2017)
Administering diuretics helps to increase
fluid loss through the kidneys thus
reducing the water load in the body.
Lasix (furosemide) is a loop diuretic that
facilitates the loss of water without
reabsorption of salt and is suitable for
management of oedema and fluid
overload in the body.
(Carpenito, 2017)
Talking builds a therapeutic relationship
and rapport based on empathy. A bed
rest will minimize energy loss by the
body. (Gordon, 2010)
CARE PLAN TEMPLATE
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CARE PLAN TEMPLATE
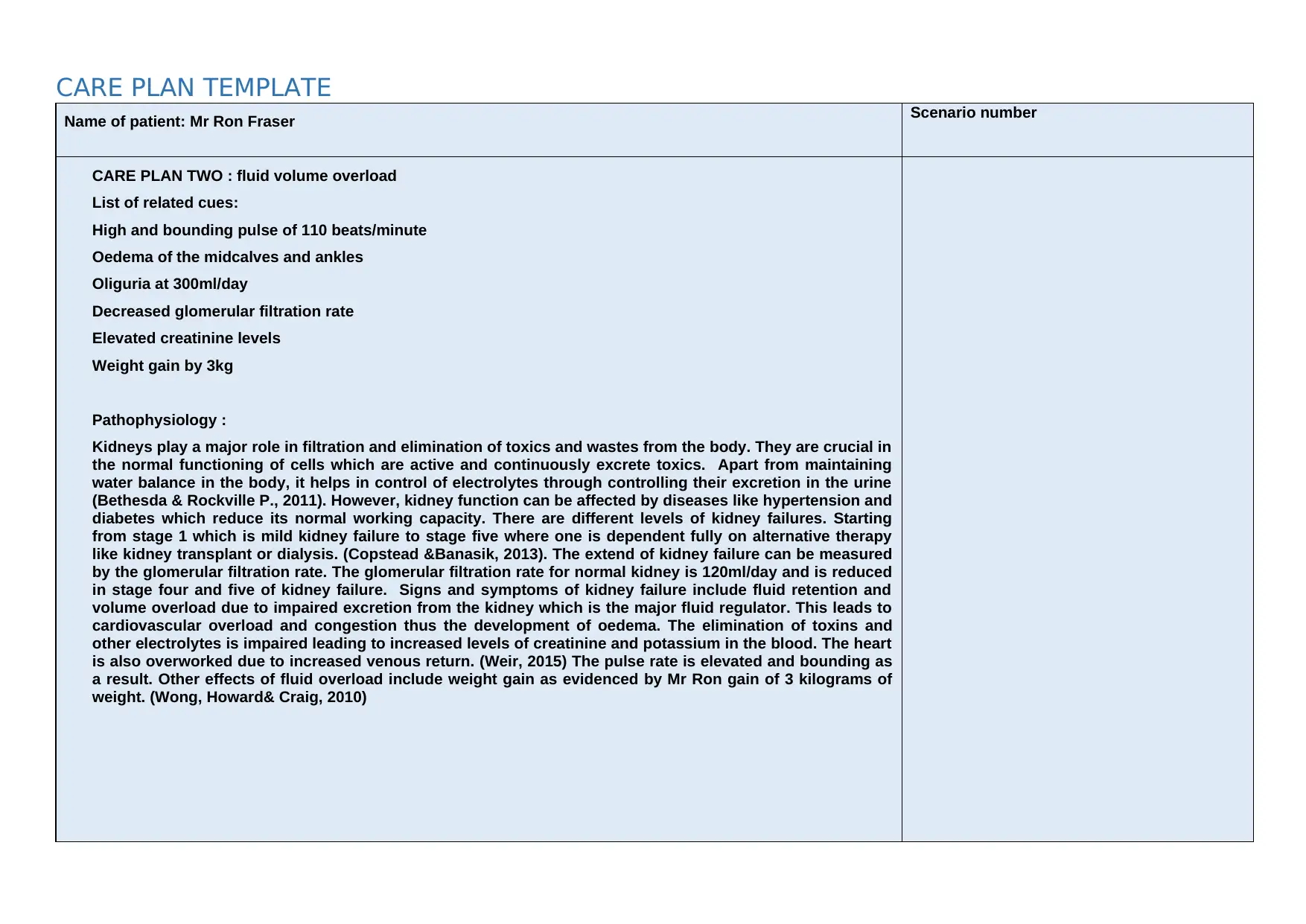
Name of patient: Mr Ron Fraser Scenario number
CARE PLAN TWO : fluid volume overload
List of related cues:
High and bounding pulse of 110 beats/minute
Oedema of the midcalves and ankles
Oliguria at 300ml/day
Decreased glomerular filtration rate
Elevated creatinine levels
Weight gain by 3kg
Pathophysiology :
Kidneys play a major role in filtration and elimination of toxics and wastes from the body. They are crucial in
the normal functioning of cells which are active and continuously excrete toxics. Apart from maintaining
water balance in the body, it helps in control of electrolytes through controlling their excretion in the urine
(Bethesda & Rockville P., 2011). However, kidney function can be affected by diseases like hypertension and
diabetes which reduce its normal working capacity. There are different levels of kidney failures. Starting
from stage 1 which is mild kidney failure to stage five where one is dependent fully on alternative therapy
like kidney transplant or dialysis. (Copstead &Banasik, 2013). The extend of kidney failure can be measured
by the glomerular filtration rate. The glomerular filtration rate for normal kidney is 120ml/day and is reduced
in stage four and five of kidney failure. Signs and symptoms of kidney failure include fluid retention and
volume overload due to impaired excretion from the kidney which is the major fluid regulator. This leads to
cardiovascular overload and congestion thus the development of oedema. The elimination of toxins and
other electrolytes is impaired leading to increased levels of creatinine and potassium in the blood. The heart
is also overworked due to increased venous return. (Weir, 2015) The pulse rate is elevated and bounding as
a result. Other effects of fluid overload include weight gain as evidenced by Mr Ron gain of 3 kilograms of
weight. (Wong, Howard& Craig, 2010)
Name of patient: Mr Ron Fraser Scenario number
CARE PLAN TWO : fluid volume overload
List of related cues:
High and bounding pulse of 110 beats/minute
Oedema of the midcalves and ankles
Oliguria at 300ml/day
Decreased glomerular filtration rate
Elevated creatinine levels
Weight gain by 3kg
Pathophysiology :
Kidneys play a major role in filtration and elimination of toxics and wastes from the body. They are crucial in
the normal functioning of cells which are active and continuously excrete toxics. Apart from maintaining
water balance in the body, it helps in control of electrolytes through controlling their excretion in the urine
(Bethesda & Rockville P., 2011). However, kidney function can be affected by diseases like hypertension and
diabetes which reduce its normal working capacity. There are different levels of kidney failures. Starting
from stage 1 which is mild kidney failure to stage five where one is dependent fully on alternative therapy
like kidney transplant or dialysis. (Copstead &Banasik, 2013). The extend of kidney failure can be measured
by the glomerular filtration rate. The glomerular filtration rate for normal kidney is 120ml/day and is reduced
in stage four and five of kidney failure. Signs and symptoms of kidney failure include fluid retention and
volume overload due to impaired excretion from the kidney which is the major fluid regulator. This leads to
cardiovascular overload and congestion thus the development of oedema. The elimination of toxins and
other electrolytes is impaired leading to increased levels of creatinine and potassium in the blood. The heart
is also overworked due to increased venous return. (Weir, 2015) The pulse rate is elevated and bounding as
a result. Other effects of fluid overload include weight gain as evidenced by Mr Ron gain of 3 kilograms of
weight. (Wong, Howard& Craig, 2010)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CARE PLAN TEMPLATE
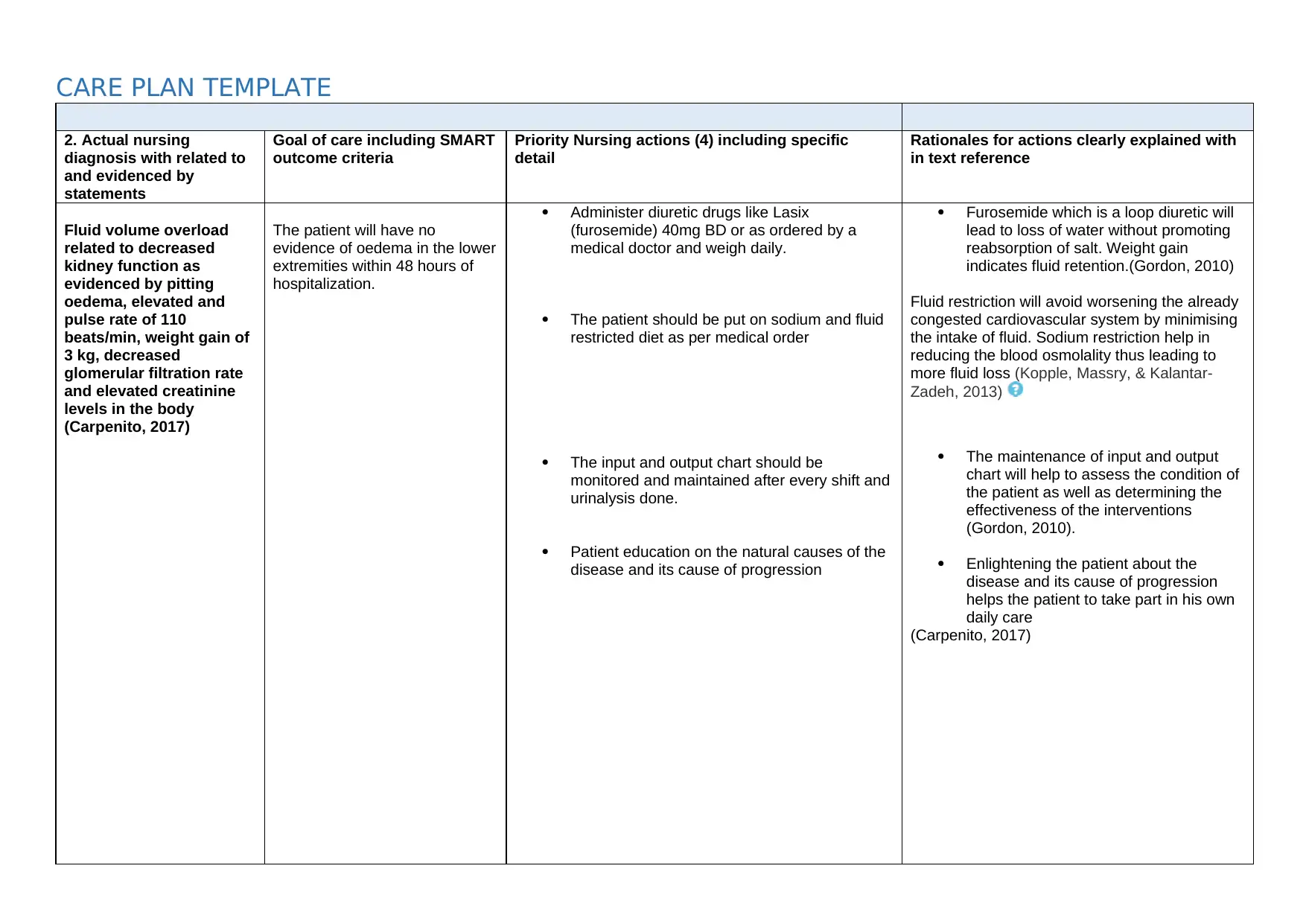
2. Actual nursing
diagnosis with related to
and evidenced by
statements
Goal of care including SMART
outcome criteria
Priority Nursing actions (4) including specific
detail
Rationales for actions clearly explained with
in text reference
Fluid volume overload
related to decreased
kidney function as
evidenced by pitting
oedema, elevated and
pulse rate of 110
beats/min, weight gain of
3 kg, decreased
glomerular filtration rate
and elevated creatinine
levels in the body
(Carpenito, 2017)
The patient will have no
evidence of oedema in the lower
extremities within 48 hours of
hospitalization.
Administer diuretic drugs like Lasix
(furosemide) 40mg BD or as ordered by a
medical doctor and weigh daily.
The patient should be put on sodium and fluid
restricted diet as per medical order
The input and output chart should be
monitored and maintained after every shift and
urinalysis done.
Patient education on the natural causes of the
disease and its cause of progression
Furosemide which is a loop diuretic will
lead to loss of water without promoting
reabsorption of salt. Weight gain
indicates fluid retention.(Gordon, 2010)
Fluid restriction will avoid worsening the already
congested cardiovascular system by minimising
the intake of fluid. Sodium restriction help in
reducing the blood osmolality thus leading to
more fluid loss (Kopple, Massry, & Kalantar-
Zadeh, 2013)
The maintenance of input and output
chart will help to assess the condition of
the patient as well as determining the
effectiveness of the interventions
(Gordon, 2010).
Enlightening the patient about the
disease and its cause of progression
helps the patient to take part in his own
daily care
(Carpenito, 2017)
2. Actual nursing
diagnosis with related to
and evidenced by
statements
Goal of care including SMART
outcome criteria
Priority Nursing actions (4) including specific
detail
Rationales for actions clearly explained with
in text reference
Fluid volume overload
related to decreased
kidney function as
evidenced by pitting
oedema, elevated and
pulse rate of 110
beats/min, weight gain of
3 kg, decreased
glomerular filtration rate
and elevated creatinine
levels in the body
(Carpenito, 2017)
The patient will have no
evidence of oedema in the lower
extremities within 48 hours of
hospitalization.
Administer diuretic drugs like Lasix
(furosemide) 40mg BD or as ordered by a
medical doctor and weigh daily.
The patient should be put on sodium and fluid
restricted diet as per medical order
The input and output chart should be
monitored and maintained after every shift and
urinalysis done.
Patient education on the natural causes of the
disease and its cause of progression
Furosemide which is a loop diuretic will
lead to loss of water without promoting
reabsorption of salt. Weight gain
indicates fluid retention.(Gordon, 2010)
Fluid restriction will avoid worsening the already
congested cardiovascular system by minimising
the intake of fluid. Sodium restriction help in
reducing the blood osmolality thus leading to
more fluid loss (Kopple, Massry, & Kalantar-
Zadeh, 2013)
The maintenance of input and output
chart will help to assess the condition of
the patient as well as determining the
effectiveness of the interventions
(Gordon, 2010).
Enlightening the patient about the
disease and its cause of progression
helps the patient to take part in his own
daily care
(Carpenito, 2017)
CARE PLAN TEMPLATE
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CARE PLAN TEMPLATE
References
Bethesda & Rockville P. (2011) National Institute of Diabetes and Digestive and Kidney Diseases (U.S.) National Kidney and Urologic Diseases Information Clearinghouse
(U.S.). Kidney failure: What to expect. 89(3) pg. 564-572
Brown T. (2018) Medscape medical news; potential unsafe prescribing common in patients with chronic kidney disease. Retrieved from
https://www.medscape.com/viewarticle/893606
Carpenito, L. J. (2017). Ineffective gaseous exchange. In Handbook of nursing diagnosis (6th ed., pp. 89- 100). Washington DC, DC: Carpenito L J.
Chronic Kidney Disease: Practice Essentials, Pathophysiology, Aetiology. (2018, March 9). Retrieved from https://emedicine.medscape.com/article/238798
Copstead, L. E., & Banasik, J. L. (2013). Kidney failure. In Pathophysiology (7th ed., pp. 562- 570).
Gordon, M. (2010). Manual of nursing diagnosis: Including all diagnostic categories approved by the North American Nursing Diagnosis Association. Sudbury, MA: Jones and
Bartlett.
Herrero, R., Lorente, J. A., Herrero, R., Lorente, J. A., Sanchez, G., & Lorente, J. A. (2018). New insights into the mechanisms of pulmonary edema in acute lung
injury. Annals of Translational Medicine, 6, 2.)
Kopple, J. D., Massry, S. G., & Kalantar-Zadeh, K. (2013). Dietary management of fluid overload. In Nutritional management of renal disease (3rd ed., pp. 1089- 1090).
Amsterdam, am: Academic Press.
Morrell, N. W., & Firth, J. D. (2015). Pulmonary oedema. Oxford Medicine Online, 97(8), 1093-1095. doi:10.1093/med/9780199204854.003.161503_update_00
Levin A. (2008). Canadian society of nephrology. Guidelines for the management of chronic kidney disease: 179(11); pg. 1154-1162
Schnaper HW. (2014) .Clinical nephrology journal: remnant nephron physiology and the physiology of chronic kidney disease; 29(2) pg. 1119 – 1124
Weir, M. R. (2015). Kidney transplant. In Medical Management of Kidney Transplantation (7th ed., p. 456). Philadelphia: Wolters Kluwer.
WONG, G., HOWARD, K., & CRAIG, J. C. (2010). Clinical Research for Nephrologists: Economic evaluation in clinical nephrology: Part 2. Applying economic evaluations in
clinical nephrology. Nephrology, 15(5), pg.533-539.
References
Bethesda & Rockville P. (2011) National Institute of Diabetes and Digestive and Kidney Diseases (U.S.) National Kidney and Urologic Diseases Information Clearinghouse
(U.S.). Kidney failure: What to expect. 89(3) pg. 564-572
Brown T. (2018) Medscape medical news; potential unsafe prescribing common in patients with chronic kidney disease. Retrieved from
https://www.medscape.com/viewarticle/893606
Carpenito, L. J. (2017). Ineffective gaseous exchange. In Handbook of nursing diagnosis (6th ed., pp. 89- 100). Washington DC, DC: Carpenito L J.
Chronic Kidney Disease: Practice Essentials, Pathophysiology, Aetiology. (2018, March 9). Retrieved from https://emedicine.medscape.com/article/238798
Copstead, L. E., & Banasik, J. L. (2013). Kidney failure. In Pathophysiology (7th ed., pp. 562- 570).
Gordon, M. (2010). Manual of nursing diagnosis: Including all diagnostic categories approved by the North American Nursing Diagnosis Association. Sudbury, MA: Jones and
Bartlett.
Herrero, R., Lorente, J. A., Herrero, R., Lorente, J. A., Sanchez, G., & Lorente, J. A. (2018). New insights into the mechanisms of pulmonary edema in acute lung
injury. Annals of Translational Medicine, 6, 2.)
Kopple, J. D., Massry, S. G., & Kalantar-Zadeh, K. (2013). Dietary management of fluid overload. In Nutritional management of renal disease (3rd ed., pp. 1089- 1090).
Amsterdam, am: Academic Press.
Morrell, N. W., & Firth, J. D. (2015). Pulmonary oedema. Oxford Medicine Online, 97(8), 1093-1095. doi:10.1093/med/9780199204854.003.161503_update_00
Levin A. (2008). Canadian society of nephrology. Guidelines for the management of chronic kidney disease: 179(11); pg. 1154-1162
Schnaper HW. (2014) .Clinical nephrology journal: remnant nephron physiology and the physiology of chronic kidney disease; 29(2) pg. 1119 – 1124
Weir, M. R. (2015). Kidney transplant. In Medical Management of Kidney Transplantation (7th ed., p. 456). Philadelphia: Wolters Kluwer.
WONG, G., HOWARD, K., & CRAIG, J. C. (2010). Clinical Research for Nephrologists: Economic evaluation in clinical nephrology: Part 2. Applying economic evaluations in
clinical nephrology. Nephrology, 15(5), pg.533-539.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





