Caring for Exogenous Cushing Syndrome’s Patient
VerifiedAdded on 2023/04/10
|12
|2186
|148
AI Summary
This article discusses the care for a patient with Exogenous Cushing Syndrome, including the causes, incidence, risk factors, and impact on the patient and their family. It also covers the signs and symptoms, pathophysiology, and pharmacodynamics & pharmacokinetics of corticosteroids. A nursing care plan is provided for managing the disease.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Caring for Exogenous Cushing Syndrome’s Patient
Student’s Name
Professor’s Name
Institution Affiliation
Date
Student’s Name
Professor’s Name
Institution Affiliation
Date
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Case study chosen; 2
Question one; Exogenous Cushing Syndrome
The major disease that Maureen is infected with is the Exogenous Cushing Syndrome.
The disease is a disorder in which the Cushing syndrome occurs due to the higher level of
cortisol hormone than normal.
Cause
Exogenous Cushing syndrome occurs to a person when he/she uses synthetic
glucocorticoid medicines to treat a disease. Exogenous means something from outside the body,
such that the exogenous Cushing syndrome will occur when a person uses human-made
glucocorticoid medicines to treat an illness. Some of the diseases that are mostly treated with
glucocorticoids medicines are inflammatory bowel disease, joints disease like rheumatoid
arthritis, type 2 diabetes and brain tumors (Sharma, Nieman &Feelders, 2015).
Incidence
According to the case study two, the patient, Maureen was diagnosed with two diseases;
rheumatoid arthritis (RA) and type two diabetes. Maureen was diagnosed with RA at an early
age when she was 15 years. After multiple exacerbations of rheumatoid arthritis, she was advised
by her general practitioner (GP) to start using a high dose of corticosteroids. For type two
diabetes, Maureen uses metformin for control. The two diseases that Maureen has been
diagnosed with are the major incidences that have led to the occurrence of the exogenous
Cushing syndrome due to the synthetic medicines she has been using to treat those diseases.
Risk factors
Question one; Exogenous Cushing Syndrome
The major disease that Maureen is infected with is the Exogenous Cushing Syndrome.
The disease is a disorder in which the Cushing syndrome occurs due to the higher level of
cortisol hormone than normal.
Cause
Exogenous Cushing syndrome occurs to a person when he/she uses synthetic
glucocorticoid medicines to treat a disease. Exogenous means something from outside the body,
such that the exogenous Cushing syndrome will occur when a person uses human-made
glucocorticoid medicines to treat an illness. Some of the diseases that are mostly treated with
glucocorticoids medicines are inflammatory bowel disease, joints disease like rheumatoid
arthritis, type 2 diabetes and brain tumors (Sharma, Nieman &Feelders, 2015).
Incidence
According to the case study two, the patient, Maureen was diagnosed with two diseases;
rheumatoid arthritis (RA) and type two diabetes. Maureen was diagnosed with RA at an early
age when she was 15 years. After multiple exacerbations of rheumatoid arthritis, she was advised
by her general practitioner (GP) to start using a high dose of corticosteroids. For type two
diabetes, Maureen uses metformin for control. The two diseases that Maureen has been
diagnosed with are the major incidences that have led to the occurrence of the exogenous
Cushing syndrome due to the synthetic medicines she has been using to treat those diseases.
Risk factors
A person with exogenous Cushing syndrome may develop some of the health
complications which are as follows; a person with a low immune system may have frequent
cases of infections. An exogenous Cushing syndrome patient is at risk of developing diabetes
complication as Maureen has developed type 2 diabetes. Risk of blood clots is high to a person
with exogenous Cushing syndrome. A person with this disease develops complications like
osteoporosis (weak bones) and increased risk of fractures.
Impact on the patient and the family
The clinical complications of the exogenous Cushing's syndrome negatively do impact
the quality of life of the patient due to the increased morbidity due to other infective diseases and
cardiovascular complications. The patient with Cushing’s syndrome is advised to visit a
neurocognitive specialist and psychiatrist due to patient’s mental disorders like mania,
depression and anxiety. This is because most patient suffering from Cushing syndrome
frequently do complain of changes in the physical appearance like where Maureen’s face started
to become round, her fats mainly concentrated at her abdominal area and a hump between her
shoulders. Other complain that Maureen’s husband noticed were fatigue and emotional
instability as it interferes with the family life and workplace performance.
The disease has a lot of impact on the family in terms of daily activities and medical cost.
Also, there are a lot of duties that are affected in the family that could be done by the patient.
After the patient is discharged from the hospital due some of the required exacerbations like in
Maureen’s case, her husband has a burden of duties and daily activities to perform while taking
care of her to ensure a quick recovery. The family member as in Maureen’s husbands also suffers
depression due to the observable changes that occur to her wife both physical and emotional
(Wagner-Bartaket al, 2017).
complications which are as follows; a person with a low immune system may have frequent
cases of infections. An exogenous Cushing syndrome patient is at risk of developing diabetes
complication as Maureen has developed type 2 diabetes. Risk of blood clots is high to a person
with exogenous Cushing syndrome. A person with this disease develops complications like
osteoporosis (weak bones) and increased risk of fractures.
Impact on the patient and the family
The clinical complications of the exogenous Cushing's syndrome negatively do impact
the quality of life of the patient due to the increased morbidity due to other infective diseases and
cardiovascular complications. The patient with Cushing’s syndrome is advised to visit a
neurocognitive specialist and psychiatrist due to patient’s mental disorders like mania,
depression and anxiety. This is because most patient suffering from Cushing syndrome
frequently do complain of changes in the physical appearance like where Maureen’s face started
to become round, her fats mainly concentrated at her abdominal area and a hump between her
shoulders. Other complain that Maureen’s husband noticed were fatigue and emotional
instability as it interferes with the family life and workplace performance.
The disease has a lot of impact on the family in terms of daily activities and medical cost.
Also, there are a lot of duties that are affected in the family that could be done by the patient.
After the patient is discharged from the hospital due some of the required exacerbations like in
Maureen’s case, her husband has a burden of duties and daily activities to perform while taking
care of her to ensure a quick recovery. The family member as in Maureen’s husbands also suffers
depression due to the observable changes that occur to her wife both physical and emotional
(Wagner-Bartaket al, 2017).
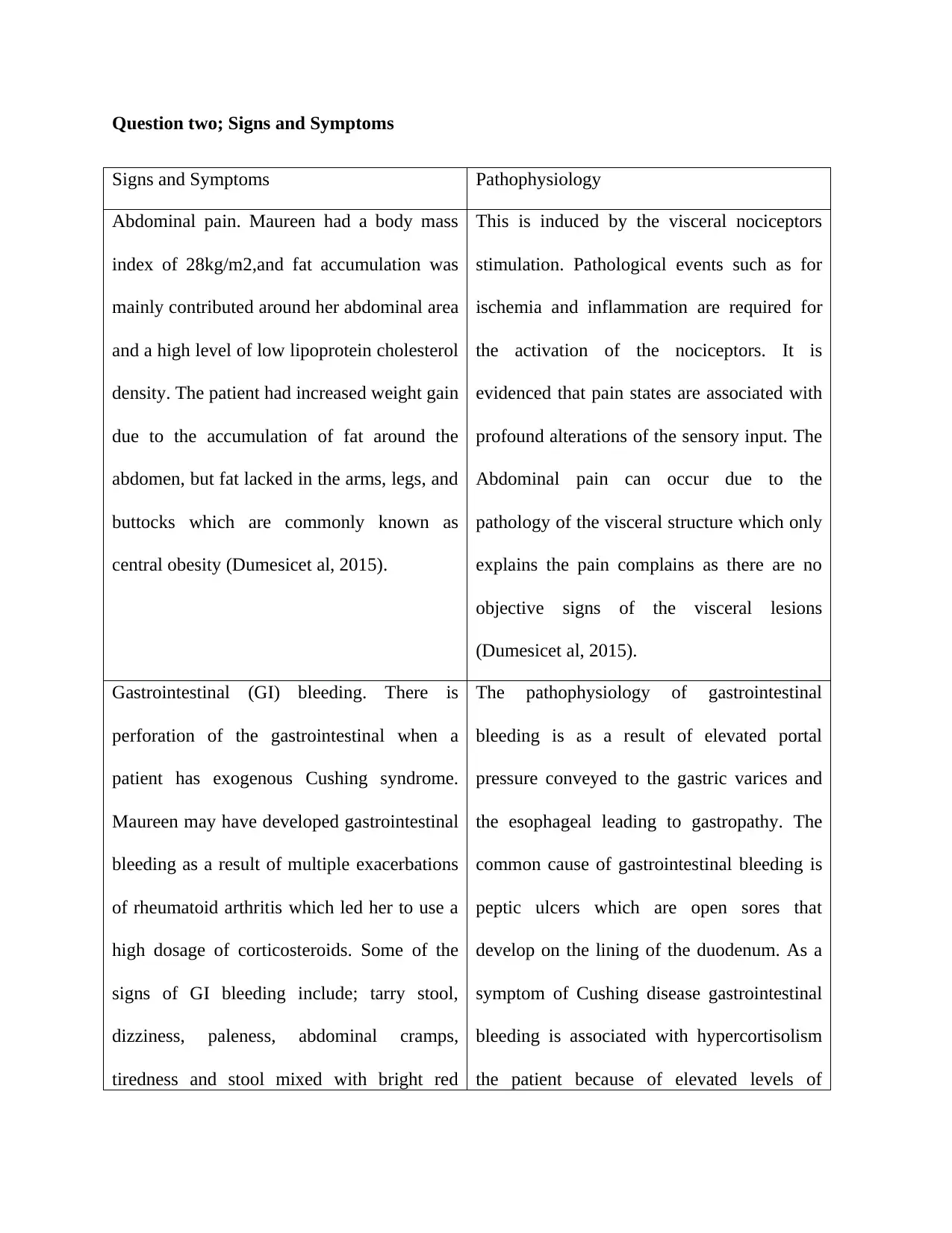
Question two; Signs and Symptoms
Signs and Symptoms Pathophysiology
Abdominal pain. Maureen had a body mass
index of 28kg/m2,and fat accumulation was
mainly contributed around her abdominal area
and a high level of low lipoprotein cholesterol
density. The patient had increased weight gain
due to the accumulation of fat around the
abdomen, but fat lacked in the arms, legs, and
buttocks which are commonly known as
central obesity (Dumesicet al, 2015).
This is induced by the visceral nociceptors
stimulation. Pathological events such as for
ischemia and inflammation are required for
the activation of the nociceptors. It is
evidenced that pain states are associated with
profound alterations of the sensory input. The
Abdominal pain can occur due to the
pathology of the visceral structure which only
explains the pain complains as there are no
objective signs of the visceral lesions
(Dumesicet al, 2015).
Gastrointestinal (GI) bleeding. There is
perforation of the gastrointestinal when a
patient has exogenous Cushing syndrome.
Maureen may have developed gastrointestinal
bleeding as a result of multiple exacerbations
of rheumatoid arthritis which led her to use a
high dosage of corticosteroids. Some of the
signs of GI bleeding include; tarry stool,
dizziness, paleness, abdominal cramps,
tiredness and stool mixed with bright red
The pathophysiology of gastrointestinal
bleeding is as a result of elevated portal
pressure conveyed to the gastric varices and
the esophageal leading to gastropathy. The
common cause of gastrointestinal bleeding is
peptic ulcers which are open sores that
develop on the lining of the duodenum. As a
symptom of Cushing disease gastrointestinal
bleeding is associated with hypercortisolism
the patient because of elevated levels of
Signs and Symptoms Pathophysiology
Abdominal pain. Maureen had a body mass
index of 28kg/m2,and fat accumulation was
mainly contributed around her abdominal area
and a high level of low lipoprotein cholesterol
density. The patient had increased weight gain
due to the accumulation of fat around the
abdomen, but fat lacked in the arms, legs, and
buttocks which are commonly known as
central obesity (Dumesicet al, 2015).
This is induced by the visceral nociceptors
stimulation. Pathological events such as for
ischemia and inflammation are required for
the activation of the nociceptors. It is
evidenced that pain states are associated with
profound alterations of the sensory input. The
Abdominal pain can occur due to the
pathology of the visceral structure which only
explains the pain complains as there are no
objective signs of the visceral lesions
(Dumesicet al, 2015).
Gastrointestinal (GI) bleeding. There is
perforation of the gastrointestinal when a
patient has exogenous Cushing syndrome.
Maureen may have developed gastrointestinal
bleeding as a result of multiple exacerbations
of rheumatoid arthritis which led her to use a
high dosage of corticosteroids. Some of the
signs of GI bleeding include; tarry stool,
dizziness, paleness, abdominal cramps,
tiredness and stool mixed with bright red
The pathophysiology of gastrointestinal
bleeding is as a result of elevated portal
pressure conveyed to the gastric varices and
the esophageal leading to gastropathy. The
common cause of gastrointestinal bleeding is
peptic ulcers which are open sores that
develop on the lining of the duodenum. As a
symptom of Cushing disease gastrointestinal
bleeding is associated with hypercortisolism
the patient because of elevated levels of
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
blood. cortisol serum due to clinical signs of
perforations (Nieman, 2015).
Fatigue. Maureen’s fatigue has been
worsening. Her blood pressure was 154/106
mmHg, PR of 88bpm and RR of 18bpm on
assessment. When a person has fatigue,
he/she experiences a vast range of physical
emotional and mental symptoms. These signs
include; dizziness, moodiness, chronic
tiredness, and aching muscles
It is caused by a poor supply of blood to the
body tissues. Poor supply of blood can be due
to some inflammation diseases as a result of
the accumulation of fat in a certain part of the
body. The pathophysiology of fatigue can be
described as a disorder of the immune
response to an antigenic challenge or a
precipitating infection (Lacroix, Feelders,
Stratakis &Nieman, 2015).
Question three; Pharmacodynamics & pharmacokinetics of corticosteroids
Taking oral corticosteroids drugs in high doses for a long period can to a patient
developing exogenous Cushing syndrome. The corticosteroids are also useful in minimizing
surgical risk and improve signs and symptoms before and after the surgery. They are useful also
in control of cortisol production. These medications include prednisone of which Maureen is
currently using which have a similar consequence in the body as cortisol produced in the body.
For example, the cobicistat and ritonavir are potent inhibitors of P450 3A4 (CYP3A4)
cytochrome activity (Wood, Lacy, Johnston,Weigle & Dhanireddy, 2015).
The corticosteroids are used as sub-therapeutic doses in combination with other drugs
like Cushing syndrome protease inhibitors and prednisolone so that to increase their
concentrations and lower their dosing. Maureen’s blood test shown low cortisol and ACTH
perforations (Nieman, 2015).
Fatigue. Maureen’s fatigue has been
worsening. Her blood pressure was 154/106
mmHg, PR of 88bpm and RR of 18bpm on
assessment. When a person has fatigue,
he/she experiences a vast range of physical
emotional and mental symptoms. These signs
include; dizziness, moodiness, chronic
tiredness, and aching muscles
It is caused by a poor supply of blood to the
body tissues. Poor supply of blood can be due
to some inflammation diseases as a result of
the accumulation of fat in a certain part of the
body. The pathophysiology of fatigue can be
described as a disorder of the immune
response to an antigenic challenge or a
precipitating infection (Lacroix, Feelders,
Stratakis &Nieman, 2015).
Question three; Pharmacodynamics & pharmacokinetics of corticosteroids
Taking oral corticosteroids drugs in high doses for a long period can to a patient
developing exogenous Cushing syndrome. The corticosteroids are also useful in minimizing
surgical risk and improve signs and symptoms before and after the surgery. They are useful also
in control of cortisol production. These medications include prednisone of which Maureen is
currently using which have a similar consequence in the body as cortisol produced in the body.
For example, the cobicistat and ritonavir are potent inhibitors of P450 3A4 (CYP3A4)
cytochrome activity (Wood, Lacy, Johnston,Weigle & Dhanireddy, 2015).
The corticosteroids are used as sub-therapeutic doses in combination with other drugs
like Cushing syndrome protease inhibitors and prednisolone so that to increase their
concentrations and lower their dosing. Maureen’s blood test shown low cortisol and ACTH
levels due to continuous usage of corticosteroids medicines. These drugs after combinations with
protease inhibitors, the pharmacokinetic manipulation as a result of interactions with CYP3A4
substrate leads to the observed body effects (Elliot et al, 2016). The increase of the exogenous
corticosteroids plasma concentrations and their half-life may lead to exogenous Cushing
syndrome and at supraphysiological levels to suppress adrenocorticotropic hormone (ACTH)and
secretion of the endogenous corticosteroids which result to the insufficiency of secondary
adrenal.
Maureen has been using metformin to manage type diabetes mellitus which have
contributed to the immune suppression due to the glucocorticoids leading to side effects like
fluid shift, brain changes and psychological changes. The pharmacokinetic mechanism of the
glucocorticoids affects the body as the initial steroids bind to the intracellular glucocorticoid
receptors then translocation to the nucleus and changes in the transcription of the gene. In the
unbound state the intracellular glucocorticoids receptors are bound to the stable proteins such as
immunophilin and shock protein 90 (Morgan, Hassan-Smith &Lavery, 2016).
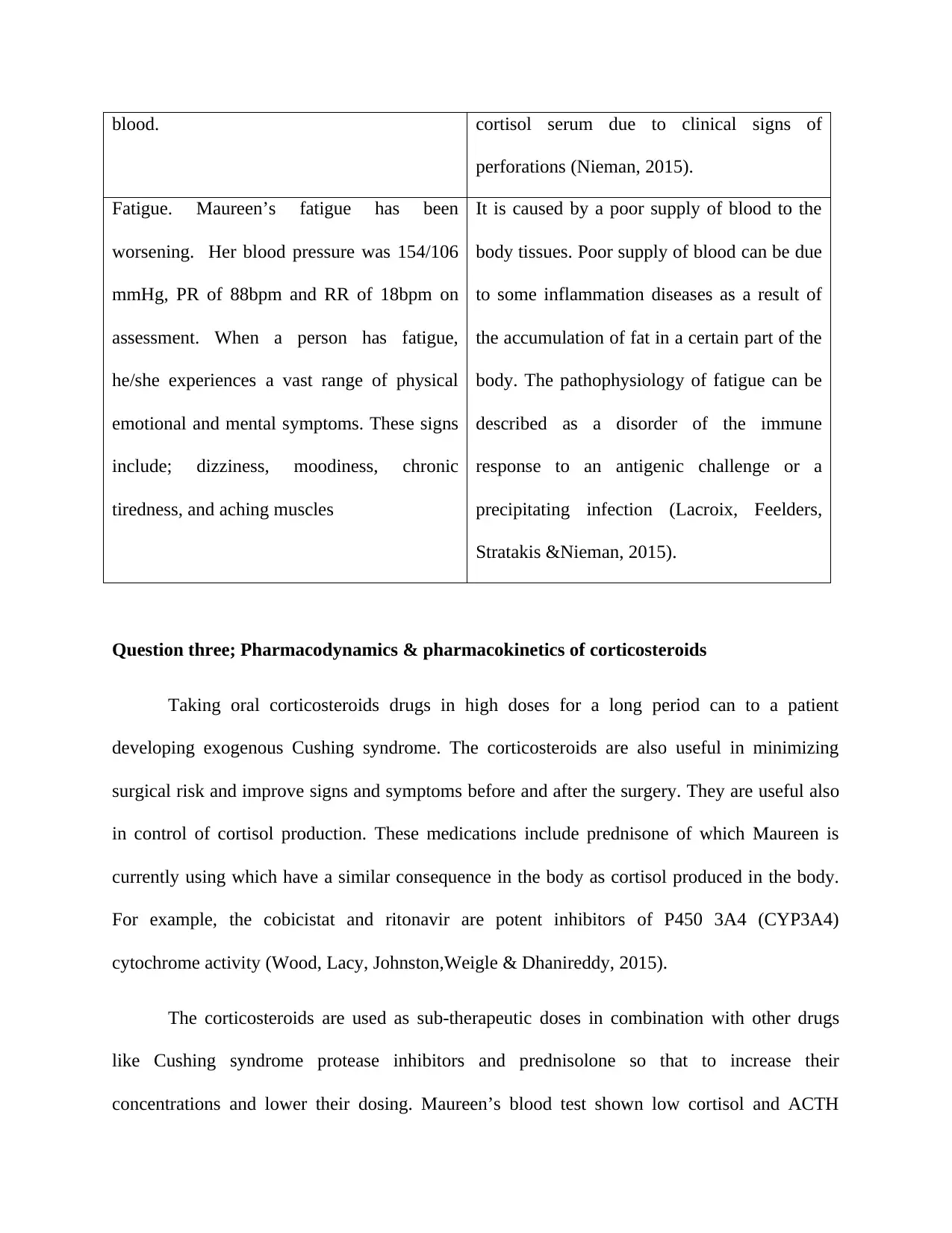
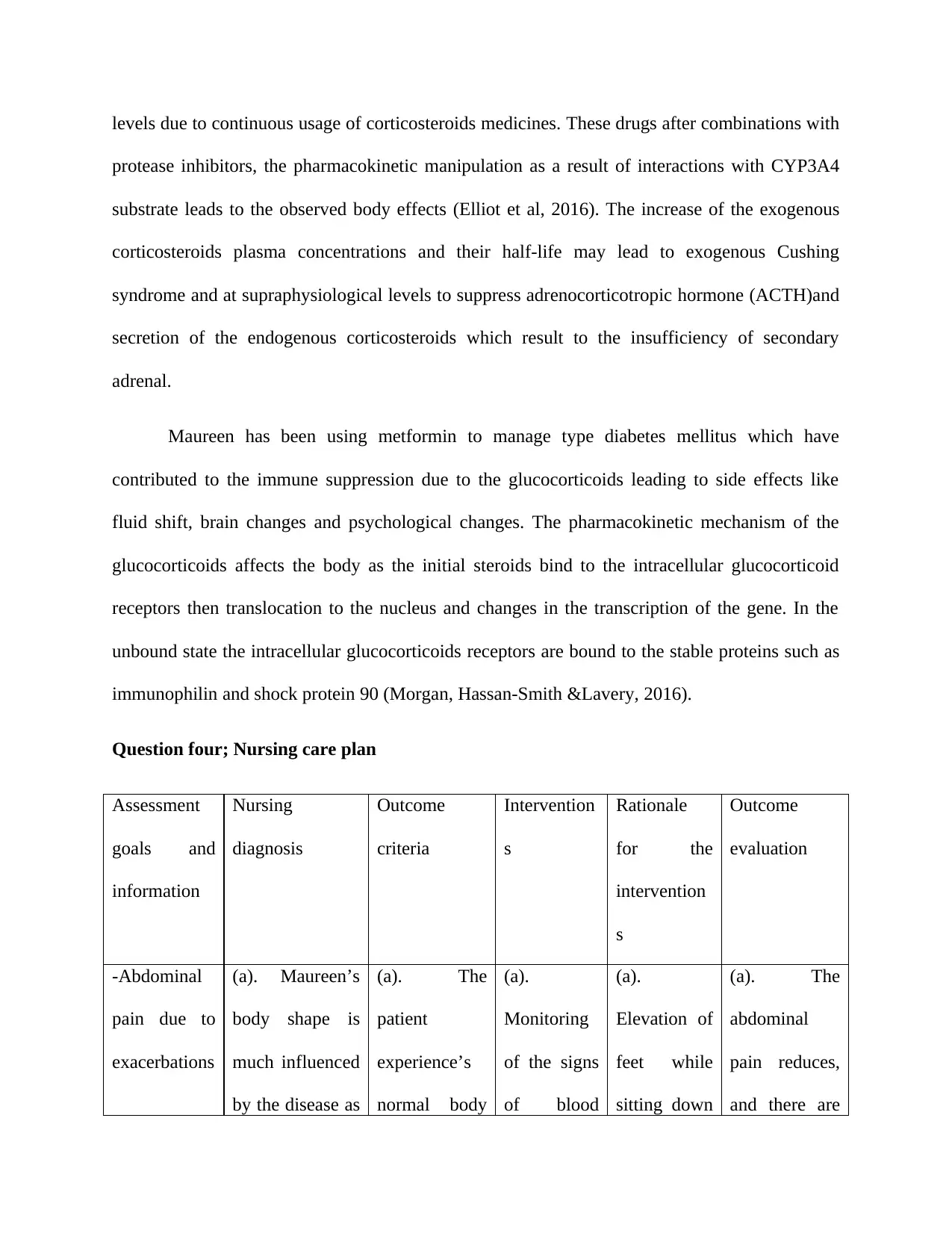
Question four; Nursing care plan
Assessment
goals and
information
Nursing
diagnosis
Outcome
criteria
Intervention
s
Rationale
for the
intervention
s
Outcome
evaluation
-Abdominal
pain due to
exacerbations
(a). Maureen’s
body shape is
much influenced
by the disease as
(a). The
patient
experience’s
normal body
(a).
Monitoring
of the signs
of blood
(a).
Elevation of
feet while
sitting down
(a). The
abdominal
pain reduces,
and there are
protease inhibitors, the pharmacokinetic manipulation as a result of interactions with CYP3A4
substrate leads to the observed body effects (Elliot et al, 2016). The increase of the exogenous
corticosteroids plasma concentrations and their half-life may lead to exogenous Cushing
syndrome and at supraphysiological levels to suppress adrenocorticotropic hormone (ACTH)and
secretion of the endogenous corticosteroids which result to the insufficiency of secondary
adrenal.
Maureen has been using metformin to manage type diabetes mellitus which have
contributed to the immune suppression due to the glucocorticoids leading to side effects like
fluid shift, brain changes and psychological changes. The pharmacokinetic mechanism of the
glucocorticoids affects the body as the initial steroids bind to the intracellular glucocorticoid
receptors then translocation to the nucleus and changes in the transcription of the gene. In the
unbound state the intracellular glucocorticoids receptors are bound to the stable proteins such as
immunophilin and shock protein 90 (Morgan, Hassan-Smith &Lavery, 2016).
Question four; Nursing care plan
Assessment
goals and
information
Nursing
diagnosis
Outcome
criteria
Intervention
s
Rationale
for the
intervention
s
Outcome
evaluation
-Abdominal
pain due to
exacerbations
(a). Maureen’s
body shape is
much influenced
by the disease as
(a). The
patient
experience’s
normal body
(a).
Monitoring
of the signs
of blood
(a).
Elevation of
feet while
sitting down
(a). The
abdominal
pain reduces,
and there are
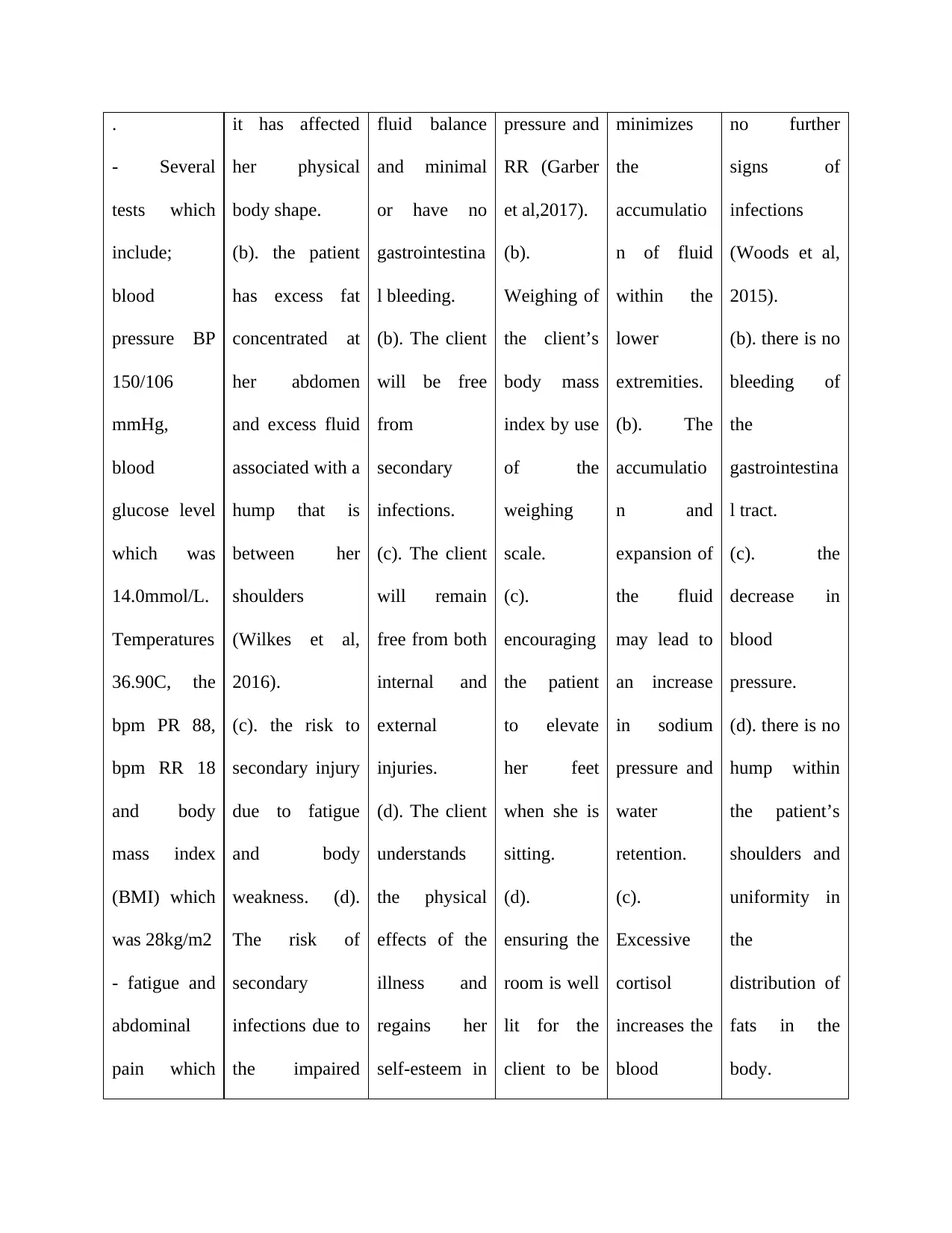
.
- Several
tests which
include;
blood
pressure BP
150/106
mmHg,
blood
glucose level
which was
14.0mmol/L.
Temperatures
36.90C, the
bpm PR 88,
bpm RR 18
and body
mass index
(BMI) which
was 28kg/m2
- fatigue and
abdominal
pain which
it has affected
her physical
body shape.
(b). the patient
has excess fat
concentrated at
her abdomen
and excess fluid
associated with a
hump that is
between her
shoulders
(Wilkes et al,
2016).
(c). the risk to
secondary injury
due to fatigue
and body
weakness. (d).
The risk of
secondary
infections due to
the impaired
fluid balance
and minimal
or have no
gastrointestina
l bleeding.
(b). The client
will be free
from
secondary
infections.
(c). The client
will remain
free from both
internal and
external
injuries.
(d). The client
understands
the physical
effects of the
illness and
regains her
self-esteem in
pressure and
RR (Garber
et al,2017).
(b).
Weighing of
the client’s
body mass
index by use
of the
weighing
scale.
(c).
encouraging
the patient
to elevate
her feet
when she is
sitting.
(d).
ensuring the
room is well
lit for the
client to be
minimizes
the
accumulatio
n of fluid
within the
lower
extremities.
(b). The
accumulatio
n and
expansion of
the fluid
may lead to
an increase
in sodium
pressure and
water
retention.
(c).
Excessive
cortisol
increases the
blood
no further
signs of
infections
(Woods et al,
2015).
(b). there is no
bleeding of
the
gastrointestina
l tract.
(c). the
decrease in
blood
pressure.
(d). there is no
hump within
the patient’s
shoulders and
uniformity in
the
distribution of
fats in the
body.
- Several
tests which
include;
blood
pressure BP
150/106
mmHg,
blood
glucose level
which was
14.0mmol/L.
Temperatures
36.90C, the
bpm PR 88,
bpm RR 18
and body
mass index
(BMI) which
was 28kg/m2
- fatigue and
abdominal
pain which
it has affected
her physical
body shape.
(b). the patient
has excess fat
concentrated at
her abdomen
and excess fluid
associated with a
hump that is
between her
shoulders
(Wilkes et al,
2016).
(c). the risk to
secondary injury
due to fatigue
and body
weakness. (d).
The risk of
secondary
infections due to
the impaired
fluid balance
and minimal
or have no
gastrointestina
l bleeding.
(b). The client
will be free
from
secondary
infections.
(c). The client
will remain
free from both
internal and
external
injuries.
(d). The client
understands
the physical
effects of the
illness and
regains her
self-esteem in
pressure and
RR (Garber
et al,2017).
(b).
Weighing of
the client’s
body mass
index by use
of the
weighing
scale.
(c).
encouraging
the patient
to elevate
her feet
when she is
sitting.
(d).
ensuring the
room is well
lit for the
client to be
minimizes
the
accumulatio
n of fluid
within the
lower
extremities.
(b). The
accumulatio
n and
expansion of
the fluid
may lead to
an increase
in sodium
pressure and
water
retention.
(c).
Excessive
cortisol
increases the
blood
no further
signs of
infections
(Woods et al,
2015).
(b). there is no
bleeding of
the
gastrointestina
l tract.
(c). the
decrease in
blood
pressure.
(d). there is no
hump within
the patient’s
shoulders and
uniformity in
the
distribution of
fats in the
body.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
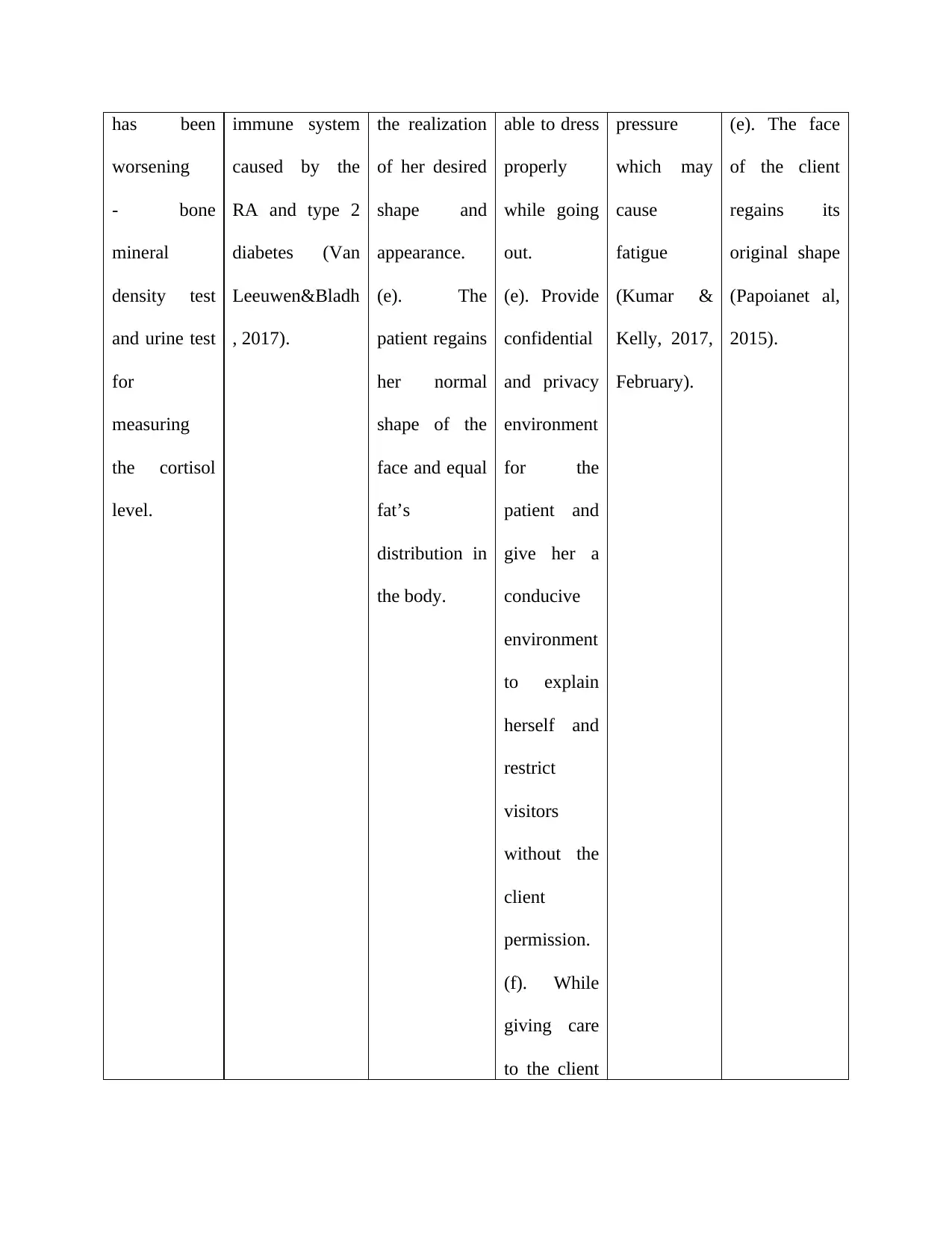
has been
worsening
- bone
mineral
density test
and urine test
for
measuring
the cortisol
level.
immune system
caused by the
RA and type 2
diabetes (Van
Leeuwen&Bladh
, 2017).
the realization
of her desired
shape and
appearance.
(e). The
patient regains
her normal
shape of the
face and equal
fat’s
distribution in
the body.
able to dress
properly
while going
out.
(e). Provide
confidential
and privacy
environment
for the
patient and
give her a
conducive
environment
to explain
herself and
restrict
visitors
without the
client
permission.
(f). While
giving care
to the client
pressure
which may
cause
fatigue
(Kumar &
Kelly, 2017,
February).
(e). The face
of the client
regains its
original shape
(Papoianet al,
2015).
worsening
- bone
mineral
density test
and urine test
for
measuring
the cortisol
level.
immune system
caused by the
RA and type 2
diabetes (Van
Leeuwen&Bladh
, 2017).
the realization
of her desired
shape and
appearance.
(e). The
patient regains
her normal
shape of the
face and equal
fat’s
distribution in
the body.
able to dress
properly
while going
out.
(e). Provide
confidential
and privacy
environment
for the
patient and
give her a
conducive
environment
to explain
herself and
restrict
visitors
without the
client
permission.
(f). While
giving care
to the client
pressure
which may
cause
fatigue
(Kumar &
Kelly, 2017,
February).
(e). The face
of the client
regains its
original shape
(Papoianet al,
2015).
ensure strict
surgical
sepsis
(Nieman et
al, 2015).
surgical
sepsis
(Nieman et
al, 2015).
References
Dumesic, D. A., Oberfield, S. E., Stener-Victorin, E., Marshall, J. C., Laven, J. S., &Legro, R. S.
(2015). Scientific statement on the diagnostic criteria, epidemiology, pathophysiology,
and molecular genetics of polycystic ovary syndrome. Endocrine reviews, 36(5), 487-
525.
Elliot, E. R., Theodoraki, A., Jain, L. R., Marshall, N. J., Boffito, M., Baldeweg, S. E., & Waters,
L. J. (2016). Iatrogenic Cushing’s syndrome due to drug interaction between
glucocorticoids and the ritonavir or cobicistat containing HIV therapies. Clinical
Medicine, 16(5), 412-418.
Garber, A. J., Abrahamson, M. J., Barzilay, J. I., Blonde, L., Bloomgarden, Z. T., Bush, M. A., ...
& Garber, J. R. (2017). Consensus statement by the American Association of Clinical
Endocrinologists and American College of Endocrinology on the comprehensive type 2
diabetes management algorithm–2017 executive summary. Endocrine Practice, 23(2),
207-238.
Kumar, S., & Kelly, A. S. (2017, February). Review of childhood obesity: from epidemiology,
etiology, and comorbidities to clinical assessment and treatment. In Mayo Clinic
Proceedings (Vol. 92, No. 2, pp. 251-265). Elsevier.
Lacroix, A., Feelders, R. A., Stratakis, C. A., &Nieman, L. K. (2015). Cushing's syndrome. The
lancet, 386(9996), 913-927.
Dumesic, D. A., Oberfield, S. E., Stener-Victorin, E., Marshall, J. C., Laven, J. S., &Legro, R. S.
(2015). Scientific statement on the diagnostic criteria, epidemiology, pathophysiology,
and molecular genetics of polycystic ovary syndrome. Endocrine reviews, 36(5), 487-
525.
Elliot, E. R., Theodoraki, A., Jain, L. R., Marshall, N. J., Boffito, M., Baldeweg, S. E., & Waters,
L. J. (2016). Iatrogenic Cushing’s syndrome due to drug interaction between
glucocorticoids and the ritonavir or cobicistat containing HIV therapies. Clinical
Medicine, 16(5), 412-418.
Garber, A. J., Abrahamson, M. J., Barzilay, J. I., Blonde, L., Bloomgarden, Z. T., Bush, M. A., ...
& Garber, J. R. (2017). Consensus statement by the American Association of Clinical
Endocrinologists and American College of Endocrinology on the comprehensive type 2
diabetes management algorithm–2017 executive summary. Endocrine Practice, 23(2),
207-238.
Kumar, S., & Kelly, A. S. (2017, February). Review of childhood obesity: from epidemiology,
etiology, and comorbidities to clinical assessment and treatment. In Mayo Clinic
Proceedings (Vol. 92, No. 2, pp. 251-265). Elsevier.
Lacroix, A., Feelders, R. A., Stratakis, C. A., &Nieman, L. K. (2015). Cushing's syndrome. The
lancet, 386(9996), 913-927.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Morgan, S. A., Hassan-Smith, Z. K., &Lavery, G. G. (2016). Mechanisms in endocrinology:
tissue-specific activation of cortisol in Cushing’s syndrome. European journal of
endocrinology, 175(2), R81-R87.
Nieman, L. K. (2015). Cushing's syndrome: update on signs, symptoms and biochemical
screening. European Journal of Endocrinology, 173(4), M33-M38.
Nieman, L. K., Biller, B. M., Findling, J. W., Murad, M. H., Newell-Price, J., Savage, M. O.,
&Tabarin, A. (2015). Treatment of Cushing's syndrome: an endocrine society clinical
practice guideline. The Journal of Clinical Endocrinology & Metabolism, 100(8), 2807-
2831.creening. European Journal of Endocrinology, 173(4), M33-M38.
Papoian, V., Biller, B. M., Webb, S. M., Campbell, K. K., Hodin, R. A., &Phitayakorn, R.
(2015). PATIENTS'PERCEPTION ON CLINICAL OUTCOME AND QUALITY OF
LIFE AFTER A DIAGNOSIS OF CUSHING SYNDROME. Endocrine Practice, 22(1),
51-67.
Sharma, S. T., Nieman, L. K., &Feelders, R. A. (2015). Cushing’s syndrome: epidemiology and
developments in disease management. Clinical epidemiology, 7, 281.
Van Leeuwen, A. M., &Bladh, M. L. (2017). Davis's comprehensive handbook of laboratory &
diagnostic tests with nursing implications. FA Davis.
Wagner-Bartak, N. A., Baiomy, A., Habra, M. A., Mukhi, S. V., Morani, A. C., Korivi, B. R., ...
&Elsayes, K. M. (2017). Cushing syndrome: diagnostic workup and imaging features,
tissue-specific activation of cortisol in Cushing’s syndrome. European journal of
endocrinology, 175(2), R81-R87.
Nieman, L. K. (2015). Cushing's syndrome: update on signs, symptoms and biochemical
screening. European Journal of Endocrinology, 173(4), M33-M38.
Nieman, L. K., Biller, B. M., Findling, J. W., Murad, M. H., Newell-Price, J., Savage, M. O.,
&Tabarin, A. (2015). Treatment of Cushing's syndrome: an endocrine society clinical
practice guideline. The Journal of Clinical Endocrinology & Metabolism, 100(8), 2807-
2831.creening. European Journal of Endocrinology, 173(4), M33-M38.
Papoian, V., Biller, B. M., Webb, S. M., Campbell, K. K., Hodin, R. A., &Phitayakorn, R.
(2015). PATIENTS'PERCEPTION ON CLINICAL OUTCOME AND QUALITY OF
LIFE AFTER A DIAGNOSIS OF CUSHING SYNDROME. Endocrine Practice, 22(1),
51-67.
Sharma, S. T., Nieman, L. K., &Feelders, R. A. (2015). Cushing’s syndrome: epidemiology and
developments in disease management. Clinical epidemiology, 7, 281.
Van Leeuwen, A. M., &Bladh, M. L. (2017). Davis's comprehensive handbook of laboratory &
diagnostic tests with nursing implications. FA Davis.
Wagner-Bartak, N. A., Baiomy, A., Habra, M. A., Mukhi, S. V., Morani, A. C., Korivi, B. R., ...
&Elsayes, K. M. (2017). Cushing syndrome: diagnostic workup and imaging features,
with clinical and pathologic correlation. American Journal of Roentgenology, 209(1), 19-
32.
Wilkes, G. M., & Barton-Burke, M. (2016). 2017 Oncology Nursing Drug Handbook. Jones &
Bartlett Learning.
Wood, B. R., Lacy, J. M., Johnston, C., Weigle, D. S., &Dhanireddy, S. (2015). Adrenal
insufficiency as a result of ritonavir and exogenous steroid exposure: report of 6 cases
and recommendation for management. Journal of the International Association of
Providers of AIDS Care (JIAPAC), 14(4), 300-305.
Woods, C. P., Argese, N., Chapman, M., Boot, C., Webster, R., Dabhi, V., ... & Crowley, R. K.
(2015). Adrenal suppression in patients taking inhaled glucocorticoids is highly prevalent
and management can be guided by morning cortisol. European journal of endocrinology,
173(5), 633-642.
32.
Wilkes, G. M., & Barton-Burke, M. (2016). 2017 Oncology Nursing Drug Handbook. Jones &
Bartlett Learning.
Wood, B. R., Lacy, J. M., Johnston, C., Weigle, D. S., &Dhanireddy, S. (2015). Adrenal
insufficiency as a result of ritonavir and exogenous steroid exposure: report of 6 cases
and recommendation for management. Journal of the International Association of
Providers of AIDS Care (JIAPAC), 14(4), 300-305.
Woods, C. P., Argese, N., Chapman, M., Boot, C., Webster, R., Dabhi, V., ... & Crowley, R. K.
(2015). Adrenal suppression in patients taking inhaled glucocorticoids is highly prevalent
and management can be guided by morning cortisol. European journal of endocrinology,
173(5), 633-642.
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





