HLTENN011 Case Study: Implementing and Monitoring Patient Care
VerifiedAdded on 2022/11/18
|23
|6126
|279
Case Study
AI Summary
This case study analyzes a patient's acute health problems, detailing nursing interventions from preoperative procedures to emergency responses. It covers topics such as the importance of medical history, NGT care, small bowel obstruction management, and the rationale for being nil by mouth. The study outlines nursing procedures for various scenarios, including pain relief, lung function support, and mobilization post-surgery. It also addresses emergency situations like cardiac arrest, detailing nursing roles, medication administration, and documentation. Furthermore, the case study examines parenteral nutrition, PICC line care, and the importance of patient education and support, offering a comprehensive overview of nursing care in acute settings. The student provides the nursing interventions for the patient in various situations.

Running head: CASE STUDY ANALYSIS
CASE STUDY ANALYSIS
Name of Student:
Name of University:
Author’s Note:
CASE STUDY ANALYSIS
Name of Student:
Name of University:
Author’s Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1CASE STUDY ANALYSIS
Answer no 1.
It is of prime importance to recognize the medical history of the Mr Jones prior going to
Operation Theater to know about the previous medication and allergies to avoid any health risk
to the patients.
Answer no 2.
The use of NGT for the purpose of drainage, the three major complication of abdominal are as
follows:
1. Esophageal perforation
2. Abdominal gastric
3. Peritonitis (Wan Fu &Yin, 2015).
Answer no 3.
Nursing intervention for caring of the patient with NGT are as follow:
1. Nurse monitor the output of the drainage and take X-ray to place the NG tube in correct
position.
2. Nurse perform suctioning of the drainage every 4 hours of the intervals.
3. Nurse check the placement of tube for the indication of its migration.
4. Nurse make note of the about its mark in the patient and measure the exterior length of
the tube and check it with the preferred length documented in the chart.
5. Nurse assess the patient for any sign of skin infections (Chang et al., 2015).
6. Nurse need to clean the area surrounding the tube at an interval of every 4 hours.
Answer no 1.
It is of prime importance to recognize the medical history of the Mr Jones prior going to
Operation Theater to know about the previous medication and allergies to avoid any health risk
to the patients.
Answer no 2.
The use of NGT for the purpose of drainage, the three major complication of abdominal are as
follows:
1. Esophageal perforation
2. Abdominal gastric
3. Peritonitis (Wan Fu &Yin, 2015).
Answer no 3.
Nursing intervention for caring of the patient with NGT are as follow:
1. Nurse monitor the output of the drainage and take X-ray to place the NG tube in correct
position.
2. Nurse perform suctioning of the drainage every 4 hours of the intervals.
3. Nurse check the placement of tube for the indication of its migration.
4. Nurse make note of the about its mark in the patient and measure the exterior length of
the tube and check it with the preferred length documented in the chart.
5. Nurse assess the patient for any sign of skin infections (Chang et al., 2015).
6. Nurse need to clean the area surrounding the tube at an interval of every 4 hours.
2CASE STUDY ANALYSIS
Answer no 4.
Mr. Jones was instructed to be nil my mouth because he was suffering from non-
functional bowel and it may require immediate operation. Nil by mouth is important to be
maintained before surgery for the reason to administer anesthesia as it reduces the risk of
pulmonary aspiration if content of gastric are vomited (Stimac et al., 2016). However, it was also
important to for Mr Jones to be nil by mouth as he was vomiting and experiencing abdominal
pain. Nil by mouth helps to control vomiting and reduce abdominal complication.
It was significant to preserve chart of strict fluid balance of the patient because of his
dehydration issue. The chart will give necessary information to the surgeon about his intake of
fluid as it will make easier for him to administer relevant medication as per the condition of the
patient (Watson & Austin, 2018).
Answer no 5.
Three preoperative nursing procedures for small bowel obstruction are as follows:
1. Nurse follows the bowel preparation procedure in order to clean the bowel by the use of
oral or parenteral antibiotics.
2. Nurse inserts the nasogastric tube in the patient to empty the stomach to reduce the
peritoneal contamination (Cima et al., 2017).
3. Nurse perform common blood test which include standard count of blood, aPPt,
concentration of creatinine, glucose and sodium.
Answer no 6.
a) When the intestine is proximally dilated because of increase of swallowed air and
gastrointestinal secretion reasons for Small - bowel obstruction. The dilation causes
Answer no 4.
Mr. Jones was instructed to be nil my mouth because he was suffering from non-
functional bowel and it may require immediate operation. Nil by mouth is important to be
maintained before surgery for the reason to administer anesthesia as it reduces the risk of
pulmonary aspiration if content of gastric are vomited (Stimac et al., 2016). However, it was also
important to for Mr Jones to be nil by mouth as he was vomiting and experiencing abdominal
pain. Nil by mouth helps to control vomiting and reduce abdominal complication.
It was significant to preserve chart of strict fluid balance of the patient because of his
dehydration issue. The chart will give necessary information to the surgeon about his intake of
fluid as it will make easier for him to administer relevant medication as per the condition of the
patient (Watson & Austin, 2018).
Answer no 5.
Three preoperative nursing procedures for small bowel obstruction are as follows:
1. Nurse follows the bowel preparation procedure in order to clean the bowel by the use of
oral or parenteral antibiotics.
2. Nurse inserts the nasogastric tube in the patient to empty the stomach to reduce the
peritoneal contamination (Cima et al., 2017).
3. Nurse perform common blood test which include standard count of blood, aPPt,
concentration of creatinine, glucose and sodium.
Answer no 6.
a) When the intestine is proximally dilated because of increase of swallowed air and
gastrointestinal secretion reasons for Small - bowel obstruction. The dilation causes
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3CASE STUDY ANALYSIS
stimulation of activity of cell secretory system which outcome in intensive fluid
accumulation. It increase the peristalsis in the stomach which cause recurrent of loose
stools and flatus (DiBaise & Motil, 2016).
b) In order to explain this to patient, it is important to know his cultural background to
acknowledge about his preferred language. If language of the patient is different
translator is used to explain the pathophysiology or nurse can use pictorial representation
to describe him the process of bowel obstruction (Ashing, Chávez & George, 2017).
Answer no 7.
Pain relief- Nurse will explain that after operation he may experience stomach pain which can
remain for 4-6 hours. Nurse will educated about the type of medication he would be given and its
possible side effect (Glowacki, 2015).
Lung function- Nurse educate patient that he might feel difficulty in breathing after operation
and he will be given oxygen if such scenario exist (Zhao et al., 2016). Nurse will educate about
breathing exercise to improve the gaseous exchange by the lungs.
Mobilization post theater- Nurse will give knowledge to the patient that he would not be able to
mobilize for 1-2 days after operations and he was given advised about the measures that need to
be taken after such period of time (Yeung, 2016). Nurse will assign physiotherapy for the patient
to make him mobile which will eventually be helpful in reducing the risk of DVT.
Answer no 8.
The seven important information that need to be received from the theatre nurse during
handover:
stimulation of activity of cell secretory system which outcome in intensive fluid
accumulation. It increase the peristalsis in the stomach which cause recurrent of loose
stools and flatus (DiBaise & Motil, 2016).
b) In order to explain this to patient, it is important to know his cultural background to
acknowledge about his preferred language. If language of the patient is different
translator is used to explain the pathophysiology or nurse can use pictorial representation
to describe him the process of bowel obstruction (Ashing, Chávez & George, 2017).
Answer no 7.
Pain relief- Nurse will explain that after operation he may experience stomach pain which can
remain for 4-6 hours. Nurse will educated about the type of medication he would be given and its
possible side effect (Glowacki, 2015).
Lung function- Nurse educate patient that he might feel difficulty in breathing after operation
and he will be given oxygen if such scenario exist (Zhao et al., 2016). Nurse will educate about
breathing exercise to improve the gaseous exchange by the lungs.
Mobilization post theater- Nurse will give knowledge to the patient that he would not be able to
mobilize for 1-2 days after operations and he was given advised about the measures that need to
be taken after such period of time (Yeung, 2016). Nurse will assign physiotherapy for the patient
to make him mobile which will eventually be helpful in reducing the risk of DVT.
Answer no 8.
The seven important information that need to be received from the theatre nurse during
handover:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4CASE STUDY ANALYSIS
1. The medical history of patient.
2. Lab test record of the patient before operation.
3. Medication administered before and during the operation of the patient.
4. Status of patient and vital sign of patient during operation.
5. Measure taken to prepare the patient for the operations (Vikberg, Lindqvist & Nylander,
2017).
6. Any allergic response was noticed in the patient due to medication.
7. Diet plan of the patient that he was following.
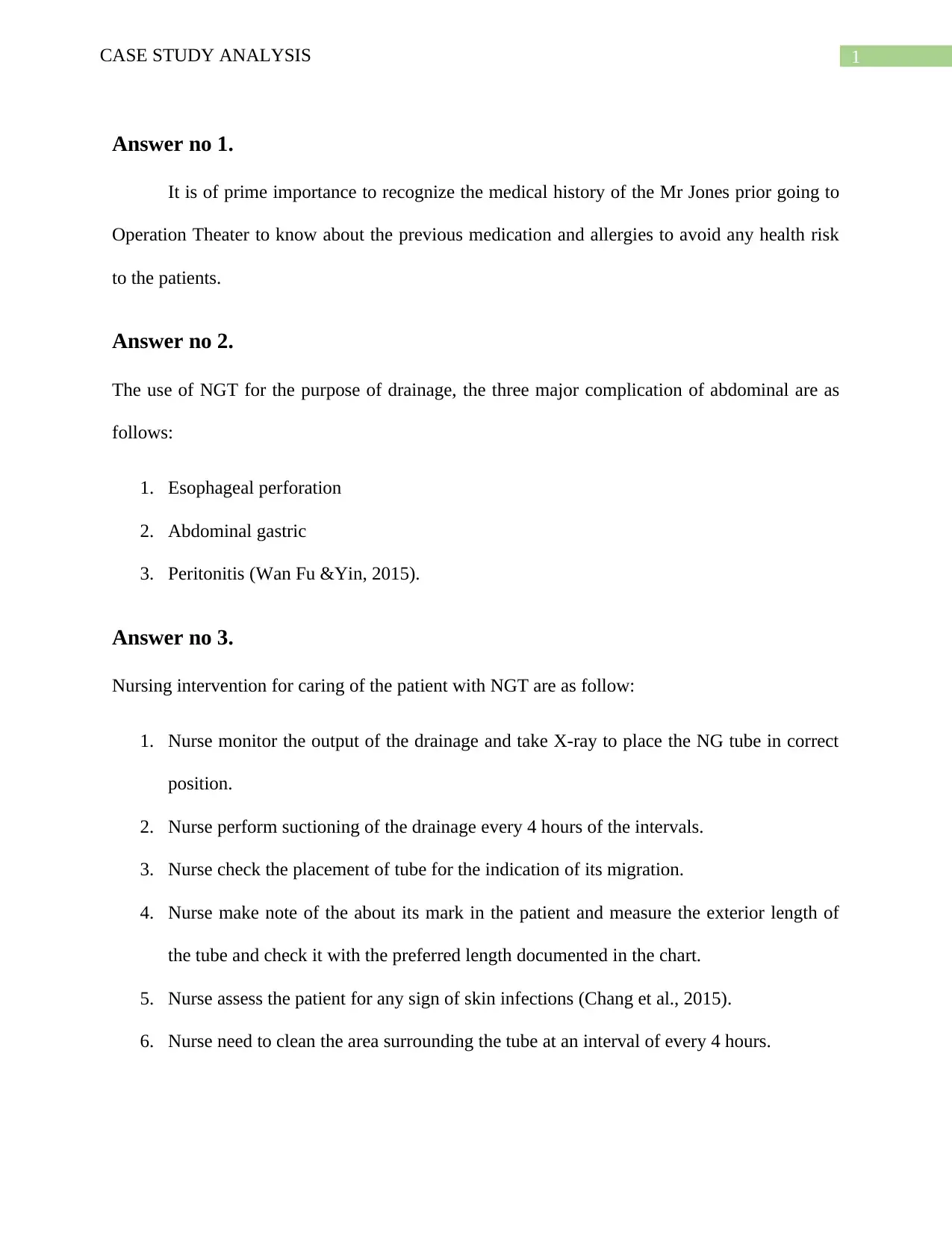
Answer no 9.
Category Nursing interventions
Pressure area care Nurse will try to keep the skin of the
pressure area clean and dry.
Nurse will make sure that area is not
vigorously rubbed or massaged to
avoid any risk (Osborne et al., 2015).
Lung function Nurse will check the breathing rate of
the patient every 6 hours of intervals.
Nurse will assess the function of lung
by measuring the oxygen saturation
level of the patient at equal interval
(Flohr et al., 2018).
Range of motion Nurse will encourage the patient to
perform physical activities.
Nurse will plan physiotherapy for the
patient, which will help in making the
patient mobile.
Psychological support Nurse will encourage and motivate the
patient to cope with the pain and
health issue.
Nurse will educate and inspire the
patient he will be alright after the
operation to make him mentally stable
(Woodhead, Northrop & Edelstein,
2016).
1. The medical history of patient.
2. Lab test record of the patient before operation.
3. Medication administered before and during the operation of the patient.
4. Status of patient and vital sign of patient during operation.
5. Measure taken to prepare the patient for the operations (Vikberg, Lindqvist & Nylander,
2017).
6. Any allergic response was noticed in the patient due to medication.
7. Diet plan of the patient that he was following.
Answer no 9.
Category Nursing interventions
Pressure area care Nurse will try to keep the skin of the
pressure area clean and dry.
Nurse will make sure that area is not
vigorously rubbed or massaged to
avoid any risk (Osborne et al., 2015).
Lung function Nurse will check the breathing rate of
the patient every 6 hours of intervals.
Nurse will assess the function of lung
by measuring the oxygen saturation
level of the patient at equal interval
(Flohr et al., 2018).
Range of motion Nurse will encourage the patient to
perform physical activities.
Nurse will plan physiotherapy for the
patient, which will help in making the
patient mobile.
Psychological support Nurse will encourage and motivate the
patient to cope with the pain and
health issue.
Nurse will educate and inspire the
patient he will be alright after the
operation to make him mentally stable
(Woodhead, Northrop & Edelstein,
2016).
5CASE STUDY ANALYSIS
Answer no 10.
Four non-verbal signs that Mr Jones displayed when suffering chronic pain are:
1. Face expression such as frowning and distorted expression.
2. Body movement like fidgeting
3. Change in mobility such as inactivity and restlessness (Ayasrah, 2019).
4. Crying and distress
Answer no 11.
Two nursing intervention that needs to be performed when patient seems unconscious
and drowsy are as follows:
1. Nurse will immediately monitor the blood pressure and heart rate of the patient.
2. Nurse will provide neurological examination to access the level of unconscious of the
patient (Noome et al., 2016).
Answer no 12.
Two nursing intervention that will be performed when condition of Mr Jones started to
deteriorate:
1. Nurse will provide external oxygen to the patient immediately to bring back the level of
oxygen to normal. As per the Australian standard, 4083, nurse need to call blue code for
medical emergency.
2. Nurse will administer medication in consultation with the doctor for his decreasing heart
rate to normalize the blood circulation (Stewart et al., 2016).
Answer no 10.
Four non-verbal signs that Mr Jones displayed when suffering chronic pain are:
1. Face expression such as frowning and distorted expression.
2. Body movement like fidgeting
3. Change in mobility such as inactivity and restlessness (Ayasrah, 2019).
4. Crying and distress
Answer no 11.
Two nursing intervention that needs to be performed when patient seems unconscious
and drowsy are as follows:
1. Nurse will immediately monitor the blood pressure and heart rate of the patient.
2. Nurse will provide neurological examination to access the level of unconscious of the
patient (Noome et al., 2016).
Answer no 12.
Two nursing intervention that will be performed when condition of Mr Jones started to
deteriorate:
1. Nurse will provide external oxygen to the patient immediately to bring back the level of
oxygen to normal. As per the Australian standard, 4083, nurse need to call blue code for
medical emergency.
2. Nurse will administer medication in consultation with the doctor for his decreasing heart
rate to normalize the blood circulation (Stewart et al., 2016).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6CASE STUDY ANALYSIS
Answer no 13.
a) The role of nurse in emergency situation to assess the Mr Jones who is undergoing
situation of cardiac arrests and full respiratory is of great importance. It is the
responsibility of the nurse to give effective care to the patient to improve the health
disorder of the patients. Nurse is responsible to monitor the health status of the patient
and in case of any deterioration must communicate the issue to the responsible health
care professional. Nurse will make assessment for the respiratory system (Hogan et al.,
2016). Nurse will document the symptoms that will be shown by the patient by recording
all the vital signs at regular interval. Nurse will also make neurological assessment in
order to record the changes. Additionally, it can be said nurse will keep record of his
heart rate and blood pressure to monitor the working and function of heart. All the
records are documented by the enrolled nurse and communicated to the undersigned
health care professional to keep the health status normal.
b) The routine members of the emergency response team are as follow s
Trained medical practitioner
Specialist nurse
Trained staffs (Topple et al., 2016).
Answer no 14.
The first line drugs that need to be given and prepared in the urgent situation of patient is
adrenaline given intravenously to control the cardiac arrest of the patient, accompanied with
administration of oxygen (Ventura et al., 2015).
Answer no 13.
a) The role of nurse in emergency situation to assess the Mr Jones who is undergoing
situation of cardiac arrests and full respiratory is of great importance. It is the
responsibility of the nurse to give effective care to the patient to improve the health
disorder of the patients. Nurse is responsible to monitor the health status of the patient
and in case of any deterioration must communicate the issue to the responsible health
care professional. Nurse will make assessment for the respiratory system (Hogan et al.,
2016). Nurse will document the symptoms that will be shown by the patient by recording
all the vital signs at regular interval. Nurse will also make neurological assessment in
order to record the changes. Additionally, it can be said nurse will keep record of his
heart rate and blood pressure to monitor the working and function of heart. All the
records are documented by the enrolled nurse and communicated to the undersigned
health care professional to keep the health status normal.
b) The routine members of the emergency response team are as follow s
Trained medical practitioner
Specialist nurse
Trained staffs (Topple et al., 2016).
Answer no 14.
The first line drugs that need to be given and prepared in the urgent situation of patient is
adrenaline given intravenously to control the cardiac arrest of the patient, accompanied with
administration of oxygen (Ventura et al., 2015).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7CASE STUDY ANALYSIS
Answer no 15.
Nurse are the responsible body who keeps record of the all the vital signs and
improvement in the condition of the patient. Progress note is the health record of the patient that
reflects the assessment made by the nurse while handling the patient. For this, nurse need to
document the date and time of the observation in addition to their designation and name. The
progress for the Mr Jones will include the subjective data, which he has communicated to the
nurse irrespective of verbal and non-verbal signs. All the changes and vital records of the patient
from the initials that were noticed was documented in the progress notes. The progress notes also
include the deterioration and any sign of improvement of the patients (Douglas et al., 2016).
Therefore, objective data is the important part of the progress notes. The assessment that will be
made by the nurse will be documented in the notes which will include all the important
procedure conducted to provide effective care to the patient, the details of the medication that has
been given and which currently being given are listed in the progress notes. It will also constitute
the plan of action made by the nurse that need to be taken for the patient.
Answer no 16.
a) Following are the steps which need to be maintained for commencing the parenteral
nutrition are as follows:
For the initial stage, nurse have to gain written permission from the health
registrar regarding IV fluid order form for the formulation.
Baseline weight of the patient will be recorded of the patients.
The total parenteral nutrition received from the pharmacy must be kept in the
refrigerator until it is administered.
Answer no 15.
Nurse are the responsible body who keeps record of the all the vital signs and
improvement in the condition of the patient. Progress note is the health record of the patient that
reflects the assessment made by the nurse while handling the patient. For this, nurse need to
document the date and time of the observation in addition to their designation and name. The
progress for the Mr Jones will include the subjective data, which he has communicated to the
nurse irrespective of verbal and non-verbal signs. All the changes and vital records of the patient
from the initials that were noticed was documented in the progress notes. The progress notes also
include the deterioration and any sign of improvement of the patients (Douglas et al., 2016).
Therefore, objective data is the important part of the progress notes. The assessment that will be
made by the nurse will be documented in the notes which will include all the important
procedure conducted to provide effective care to the patient, the details of the medication that has
been given and which currently being given are listed in the progress notes. It will also constitute
the plan of action made by the nurse that need to be taken for the patient.
Answer no 16.
a) Following are the steps which need to be maintained for commencing the parenteral
nutrition are as follows:
For the initial stage, nurse have to gain written permission from the health
registrar regarding IV fluid order form for the formulation.
Baseline weight of the patient will be recorded of the patients.
The total parenteral nutrition received from the pharmacy must be kept in the
refrigerator until it is administered.
8CASE STUDY ANALYSIS
Nurse would assess the baseline record of the blood like LFT, BGLs, UEC
triglyceride, iron, and Sodium and calcium level.
Nurse need to maintain hygiene before giving parenteral nutrition.
Nurse will then clean the dressing trolley with detergent (McClave et al., 2016).
Nurse will recheck the prescription of TPN against the one which is prepared in
consultation with the other nurse.
Nurse will then explain the whole procedure to the patient with aim to obtain
informed consent from the patient.
Before commencing the TPN, nurse will attend identification of the patient by
evaluating it with other staffs and checking band of patient.
Maintain hand hygiene before giving TPN to the patient (Cederholm et al., 2017).
b) Four features of the nursing care which is obligatory when giving care to Patient with a
PICC line are as follows:
Nurse need to assess the flow of blood and easy flushing in the patient to ensure
the patency of the PICC. If the nurse notice any sluggish flow or problem in
flushing, they have to inform the issue to the PICC line specialist.
Nurse should not take Blood pressure on the arm of the patient that has PICC line
inserted (Zhou et al., 2018).
According to the CINS guideline nurse need to maintain the hygiene of the patient
by changing the dressing of the patient and cleaning and protecting the site with
sterile dressing.
Nurse will inspect the patient for minimum of 8 hours for the sign of
inflammation after giving PICC line to the patient (Webster et al., 2017).
Nurse would assess the baseline record of the blood like LFT, BGLs, UEC
triglyceride, iron, and Sodium and calcium level.
Nurse need to maintain hygiene before giving parenteral nutrition.
Nurse will then clean the dressing trolley with detergent (McClave et al., 2016).
Nurse will recheck the prescription of TPN against the one which is prepared in
consultation with the other nurse.
Nurse will then explain the whole procedure to the patient with aim to obtain
informed consent from the patient.
Before commencing the TPN, nurse will attend identification of the patient by
evaluating it with other staffs and checking band of patient.
Maintain hand hygiene before giving TPN to the patient (Cederholm et al., 2017).
b) Four features of the nursing care which is obligatory when giving care to Patient with a
PICC line are as follows:
Nurse need to assess the flow of blood and easy flushing in the patient to ensure
the patency of the PICC. If the nurse notice any sluggish flow or problem in
flushing, they have to inform the issue to the PICC line specialist.
Nurse should not take Blood pressure on the arm of the patient that has PICC line
inserted (Zhou et al., 2018).
According to the CINS guideline nurse need to maintain the hygiene of the patient
by changing the dressing of the patient and cleaning and protecting the site with
sterile dressing.
Nurse will inspect the patient for minimum of 8 hours for the sign of
inflammation after giving PICC line to the patient (Webster et al., 2017).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9CASE STUDY ANALYSIS
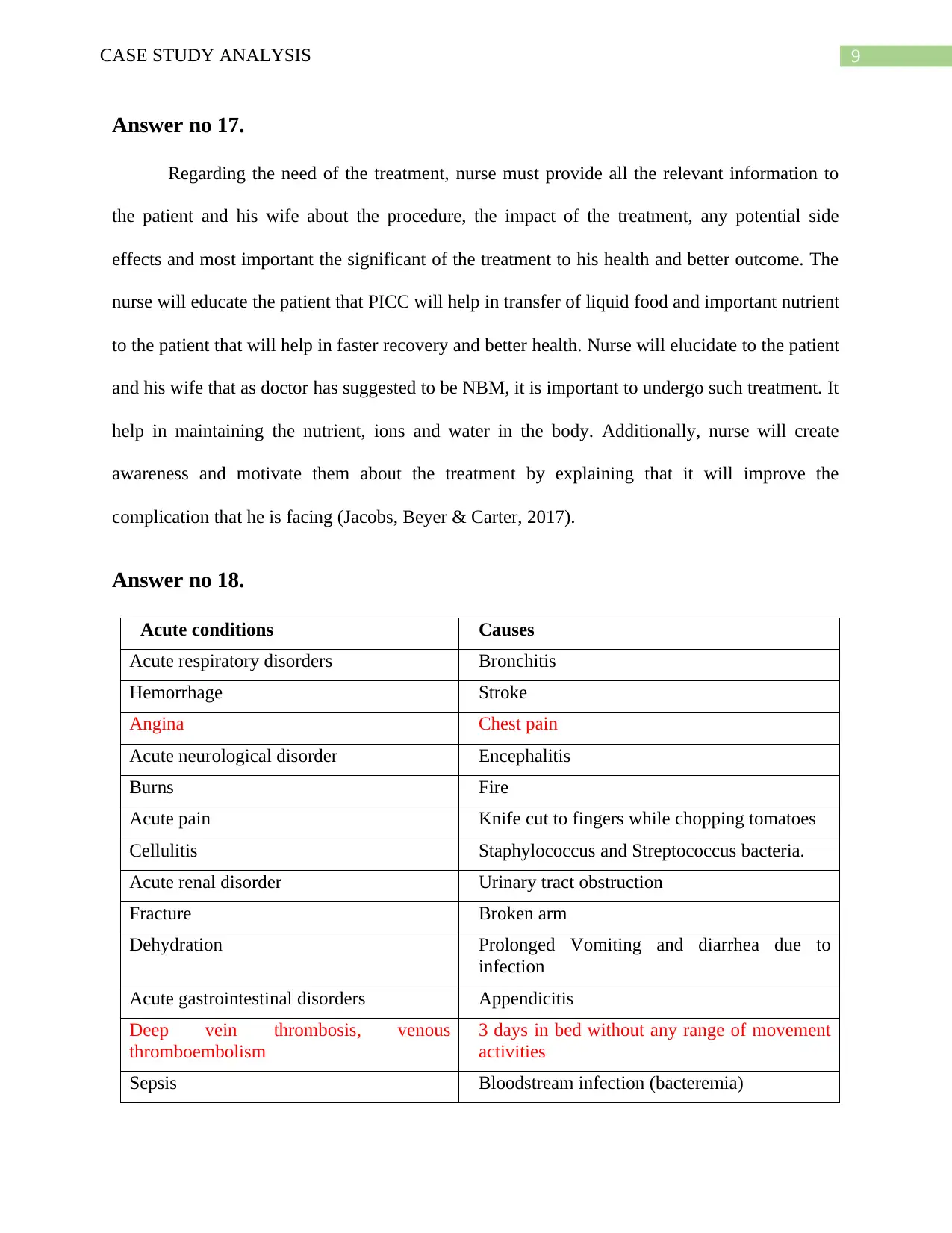
Answer no 17.
Regarding the need of the treatment, nurse must provide all the relevant information to
the patient and his wife about the procedure, the impact of the treatment, any potential side
effects and most important the significant of the treatment to his health and better outcome. The
nurse will educate the patient that PICC will help in transfer of liquid food and important nutrient
to the patient that will help in faster recovery and better health. Nurse will elucidate to the patient
and his wife that as doctor has suggested to be NBM, it is important to undergo such treatment. It
help in maintaining the nutrient, ions and water in the body. Additionally, nurse will create
awareness and motivate them about the treatment by explaining that it will improve the
complication that he is facing (Jacobs, Beyer & Carter, 2017).
Answer no 18.
Acute conditions Causes
Acute respiratory disorders Bronchitis
Hemorrhage Stroke
Angina Chest pain
Acute neurological disorder Encephalitis
Burns Fire
Acute pain Knife cut to fingers while chopping tomatoes
Cellulitis Staphylococcus and Streptococcus bacteria.
Acute renal disorder Urinary tract obstruction
Fracture Broken arm
Dehydration Prolonged Vomiting and diarrhea due to
infection
Acute gastrointestinal disorders Appendicitis
Deep vein thrombosis, venous
thromboembolism
3 days in bed without any range of movement
activities
Sepsis Bloodstream infection (bacteremia)
Answer no 17.
Regarding the need of the treatment, nurse must provide all the relevant information to
the patient and his wife about the procedure, the impact of the treatment, any potential side
effects and most important the significant of the treatment to his health and better outcome. The
nurse will educate the patient that PICC will help in transfer of liquid food and important nutrient
to the patient that will help in faster recovery and better health. Nurse will elucidate to the patient
and his wife that as doctor has suggested to be NBM, it is important to undergo such treatment. It
help in maintaining the nutrient, ions and water in the body. Additionally, nurse will create
awareness and motivate them about the treatment by explaining that it will improve the
complication that he is facing (Jacobs, Beyer & Carter, 2017).
Answer no 18.
Acute conditions Causes
Acute respiratory disorders Bronchitis
Hemorrhage Stroke
Angina Chest pain
Acute neurological disorder Encephalitis
Burns Fire
Acute pain Knife cut to fingers while chopping tomatoes
Cellulitis Staphylococcus and Streptococcus bacteria.
Acute renal disorder Urinary tract obstruction
Fracture Broken arm
Dehydration Prolonged Vomiting and diarrhea due to
infection
Acute gastrointestinal disorders Appendicitis
Deep vein thrombosis, venous
thromboembolism
3 days in bed without any range of movement
activities
Sepsis Bloodstream infection (bacteremia)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10CASE STUDY ANALYSIS
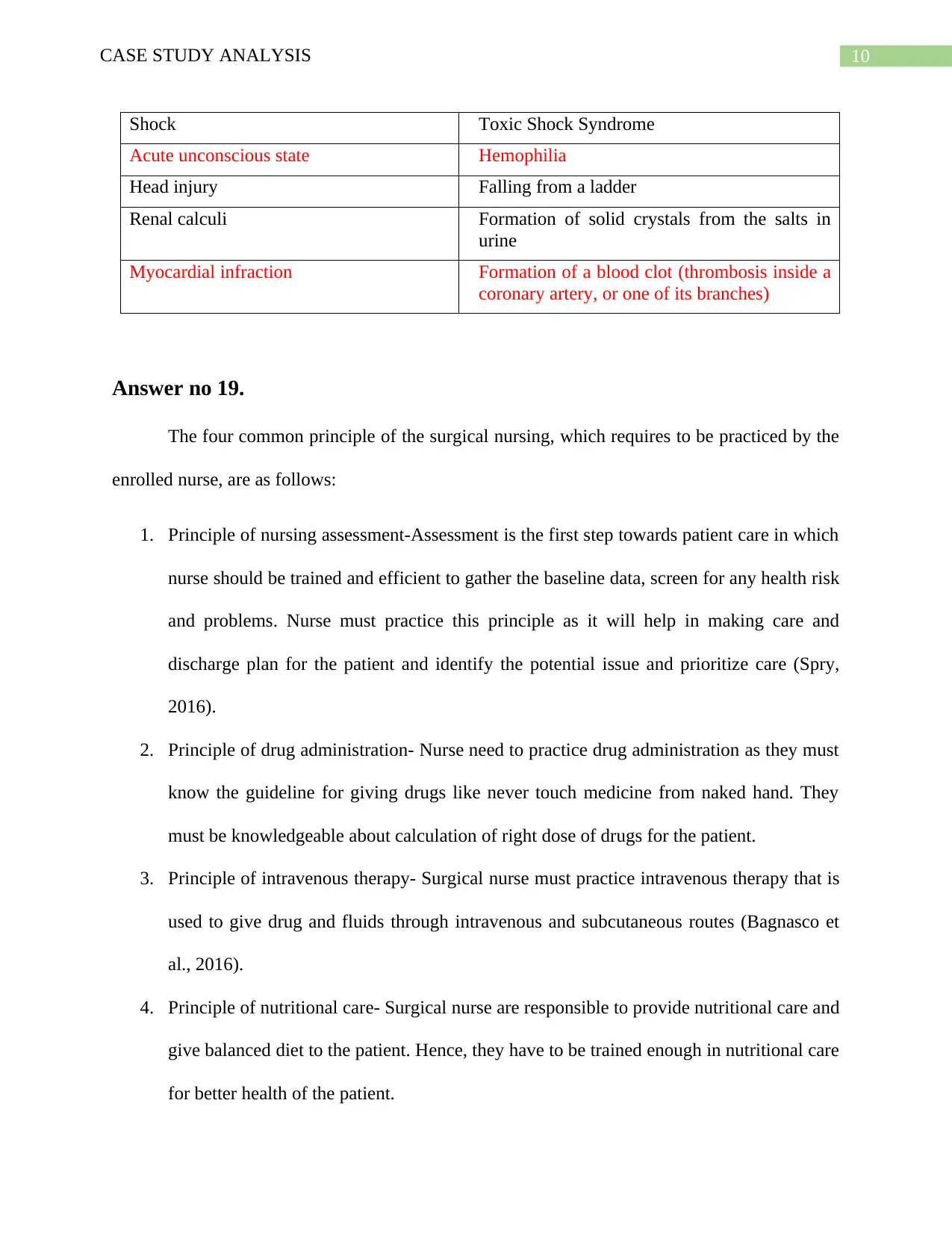
Shock Toxic Shock Syndrome
Acute unconscious state Hemophilia
Head injury Falling from a ladder
Renal calculi Formation of solid crystals from the salts in
urine
Myocardial infraction Formation of a blood clot (thrombosis inside a
coronary artery, or one of its branches)
Answer no 19.
The four common principle of the surgical nursing, which requires to be practiced by the
enrolled nurse, are as follows:
1. Principle of nursing assessment-Assessment is the first step towards patient care in which
nurse should be trained and efficient to gather the baseline data, screen for any health risk
and problems. Nurse must practice this principle as it will help in making care and
discharge plan for the patient and identify the potential issue and prioritize care (Spry,
2016).
2. Principle of drug administration- Nurse need to practice drug administration as they must
know the guideline for giving drugs like never touch medicine from naked hand. They
must be knowledgeable about calculation of right dose of drugs for the patient.
3. Principle of intravenous therapy- Surgical nurse must practice intravenous therapy that is
used to give drug and fluids through intravenous and subcutaneous routes (Bagnasco et
al., 2016).
4. Principle of nutritional care- Surgical nurse are responsible to provide nutritional care and
give balanced diet to the patient. Hence, they have to be trained enough in nutritional care
for better health of the patient.
Shock Toxic Shock Syndrome
Acute unconscious state Hemophilia
Head injury Falling from a ladder
Renal calculi Formation of solid crystals from the salts in
urine
Myocardial infraction Formation of a blood clot (thrombosis inside a
coronary artery, or one of its branches)
Answer no 19.
The four common principle of the surgical nursing, which requires to be practiced by the
enrolled nurse, are as follows:
1. Principle of nursing assessment-Assessment is the first step towards patient care in which
nurse should be trained and efficient to gather the baseline data, screen for any health risk
and problems. Nurse must practice this principle as it will help in making care and
discharge plan for the patient and identify the potential issue and prioritize care (Spry,
2016).
2. Principle of drug administration- Nurse need to practice drug administration as they must
know the guideline for giving drugs like never touch medicine from naked hand. They
must be knowledgeable about calculation of right dose of drugs for the patient.
3. Principle of intravenous therapy- Surgical nurse must practice intravenous therapy that is
used to give drug and fluids through intravenous and subcutaneous routes (Bagnasco et
al., 2016).
4. Principle of nutritional care- Surgical nurse are responsible to provide nutritional care and
give balanced diet to the patient. Hence, they have to be trained enough in nutritional care
for better health of the patient.
11CASE STUDY ANALYSIS
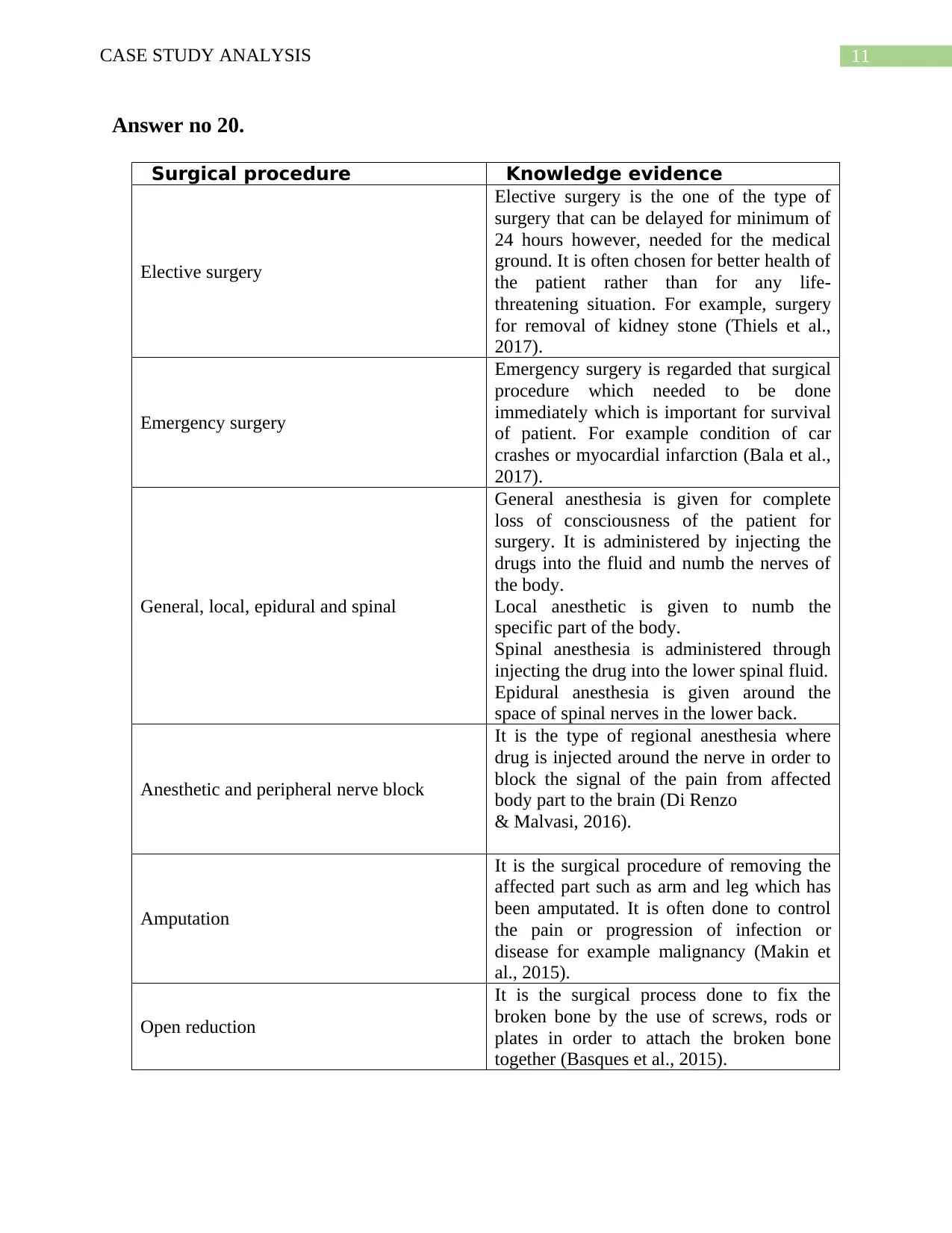
Answer no 20.
Surgical procedure Knowledge evidence
Elective surgery
Elective surgery is the one of the type of
surgery that can be delayed for minimum of
24 hours however, needed for the medical
ground. It is often chosen for better health of
the patient rather than for any life-
threatening situation. For example, surgery
for removal of kidney stone (Thiels et al.,
2017).
Emergency surgery
Emergency surgery is regarded that surgical
procedure which needed to be done
immediately which is important for survival
of patient. For example condition of car
crashes or myocardial infarction (Bala et al.,
2017).
General, local, epidural and spinal
General anesthesia is given for complete
loss of consciousness of the patient for
surgery. It is administered by injecting the
drugs into the fluid and numb the nerves of
the body.
Local anesthetic is given to numb the
specific part of the body.
Spinal anesthesia is administered through
injecting the drug into the lower spinal fluid.
Epidural anesthesia is given around the
space of spinal nerves in the lower back.
Anesthetic and peripheral nerve block
It is the type of regional anesthesia where
drug is injected around the nerve in order to
block the signal of the pain from affected
body part to the brain (Di Renzo
& Malvasi, 2016).
Amputation
It is the surgical procedure of removing the
affected part such as arm and leg which has
been amputated. It is often done to control
the pain or progression of infection or
disease for example malignancy (Makin et
al., 2015).
Open reduction
It is the surgical process done to fix the
broken bone by the use of screws, rods or
plates in order to attach the broken bone
together (Basques et al., 2015).
Answer no 20.
Surgical procedure Knowledge evidence
Elective surgery
Elective surgery is the one of the type of
surgery that can be delayed for minimum of
24 hours however, needed for the medical
ground. It is often chosen for better health of
the patient rather than for any life-
threatening situation. For example, surgery
for removal of kidney stone (Thiels et al.,
2017).
Emergency surgery
Emergency surgery is regarded that surgical
procedure which needed to be done
immediately which is important for survival
of patient. For example condition of car
crashes or myocardial infarction (Bala et al.,
2017).
General, local, epidural and spinal
General anesthesia is given for complete
loss of consciousness of the patient for
surgery. It is administered by injecting the
drugs into the fluid and numb the nerves of
the body.
Local anesthetic is given to numb the
specific part of the body.
Spinal anesthesia is administered through
injecting the drug into the lower spinal fluid.
Epidural anesthesia is given around the
space of spinal nerves in the lower back.
Anesthetic and peripheral nerve block
It is the type of regional anesthesia where
drug is injected around the nerve in order to
block the signal of the pain from affected
body part to the brain (Di Renzo
& Malvasi, 2016).
Amputation
It is the surgical procedure of removing the
affected part such as arm and leg which has
been amputated. It is often done to control
the pain or progression of infection or
disease for example malignancy (Makin et
al., 2015).
Open reduction
It is the surgical process done to fix the
broken bone by the use of screws, rods or
plates in order to attach the broken bone
together (Basques et al., 2015).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 23
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
