Case Study on Congestive Cardiac Failure
VerifiedAdded on 2023/04/21
|12
|2528
|357
AI Summary
This case study explores the causes, symptoms, and nursing care plan for congestive cardiac failure. It discusses the impact of the disease on the patient and their family, as well as the pharmacology and pharmacokinetics of the medications used in treatment. The study also includes a nursing diagnosis and goals for patient care.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

CASE STUDY 1
CASE STUDY ON CONGESTIVE CARDIAC FAILURE
Name:
Institutional affiliation:
CASE STUDY ON CONGESTIVE CARDIAC FAILURE
Name:
Institutional affiliation:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

CASE STUDY 2
DISEASE
Congestive heart failure refers to a condition whereby the heart is unable to properly
pump blood to the body due to various factors which is generally referred to as cardiac output.
Preload is a term used to refer to the amount of pressure the ventricles exert so as to pump blood
into the blood vessels to the lungs and the body respectively. The preload is increased it
increases the chances of congestive heart failure. Systolic heart failure refers to the inability of
the ventricles to contract causing decreased pressure to pump blood out of the heart while
diastolic heart failure is the inability of the ventricle to relax hence become stiff and unable to fill
accordingly. Left sided heart failure refers to the inability of the left ventricle to contract and
therefore the backflow of blood to the pulmonary vessels which manifests in pulmonary edema,
cough and shortness of breath. Right sided heart failure is the inability of the right ventricle to
eject blood causing a back flow of blood to the tissues and the hepatic system.
The causes of congestive heart failure are coronary artery disease whereby the coronary
arteries supplying the myocardial tissues receive less oxygen causing ischemia due to
atherosclerosis and causing injury to the heart tissues which reduces contractility consequently
heart failure. Hypertension increases the heart workload to eject blood therefore the heart
mechanism is hypertrophy which then causes decreased contractility. Inefficient valves cause
backflow of blood causing heart failure and may be caused by viral infections and post
streptococcal immune reactions. Anemia is also a causative factor of heart failure as it causes
increased heart rate and consequently hypertrophy decreasing contractility of the
ventricles(Moe,et.al ,2015).
DISEASE
Congestive heart failure refers to a condition whereby the heart is unable to properly
pump blood to the body due to various factors which is generally referred to as cardiac output.
Preload is a term used to refer to the amount of pressure the ventricles exert so as to pump blood
into the blood vessels to the lungs and the body respectively. The preload is increased it
increases the chances of congestive heart failure. Systolic heart failure refers to the inability of
the ventricles to contract causing decreased pressure to pump blood out of the heart while
diastolic heart failure is the inability of the ventricle to relax hence become stiff and unable to fill
accordingly. Left sided heart failure refers to the inability of the left ventricle to contract and
therefore the backflow of blood to the pulmonary vessels which manifests in pulmonary edema,
cough and shortness of breath. Right sided heart failure is the inability of the right ventricle to
eject blood causing a back flow of blood to the tissues and the hepatic system.
The causes of congestive heart failure are coronary artery disease whereby the coronary
arteries supplying the myocardial tissues receive less oxygen causing ischemia due to
atherosclerosis and causing injury to the heart tissues which reduces contractility consequently
heart failure. Hypertension increases the heart workload to eject blood therefore the heart
mechanism is hypertrophy which then causes decreased contractility. Inefficient valves cause
backflow of blood causing heart failure and may be caused by viral infections and post
streptococcal immune reactions. Anemia is also a causative factor of heart failure as it causes
increased heart rate and consequently hypertrophy decreasing contractility of the
ventricles(Moe,et.al ,2015).

CASE STUDY 3
According to the Australian Institute of Health and Welfare(2017) around 4% of the
population aged 45 years and above are diagnosed with heart failure. The Aboriginal and Torres
Strait Islander people are twice likely to encounter increased morbidity and mortality rates than
other Australians. The risk factors of congestive heart failure include hypertension, previous
myocardial infarction, smoking, obesity, age, genetic predisposition and diabetes.
The disease impacts the patient emotionally, physically and mentally. The patient is
unable to perform activities of daily living due to fatigue and shortness of breath. This in the end
may affect their income as they will be unable to work and chronic hospitalizations therefore
losing their jobs. The patient loses may have poor mental health due to depression as the quality
of life decreases in a period of time(Liu, Chang, Wu & Tsai, 2015). Fear and anxiety of the
future such as impending death may worsen the situation. Continuous use of medication and
handling the side effects may be emotional for the patient.
The family of the patient has to deal with the financial implications of managing
congestive heart failure. It’s expensive to undergo medical procedures, buy drugs and accessories
that the patient needs. The family may lose the breadwinner who happens to be the patient
causing change in roles. This may also lead to the need of a care giver who is a family member
which leads to ceasing to go work.
According to the Australian Institute of Health and Welfare(2017) around 4% of the
population aged 45 years and above are diagnosed with heart failure. The Aboriginal and Torres
Strait Islander people are twice likely to encounter increased morbidity and mortality rates than
other Australians. The risk factors of congestive heart failure include hypertension, previous
myocardial infarction, smoking, obesity, age, genetic predisposition and diabetes.
The disease impacts the patient emotionally, physically and mentally. The patient is
unable to perform activities of daily living due to fatigue and shortness of breath. This in the end
may affect their income as they will be unable to work and chronic hospitalizations therefore
losing their jobs. The patient loses may have poor mental health due to depression as the quality
of life decreases in a period of time(Liu, Chang, Wu & Tsai, 2015). Fear and anxiety of the
future such as impending death may worsen the situation. Continuous use of medication and
handling the side effects may be emotional for the patient.
The family of the patient has to deal with the financial implications of managing
congestive heart failure. It’s expensive to undergo medical procedures, buy drugs and accessories
that the patient needs. The family may lose the breadwinner who happens to be the patient
causing change in roles. This may also lead to the need of a care giver who is a family member
which leads to ceasing to go work.

CASE STUDY 4
SIGNS AND SYMPTOMS PATHOPHYSIOLOGY
Increasing shortness of breath, inspiratory
crackles, swollen ankles
Left sided heart failure causes the left ventricle
unable to eject blood therefore blood causes
pulmonary edema in the lungs. This increases
pressure and therefore accumulation of fluid in
alveoli(Lala et.al,2015). There is decreased
gaseous exchange due to lowered surface area
occupied by the fluid causing breathlessness
and decreased oxygen saturation. Lung sounds
heard are inspiratory crackles which signify
presence of fluid in the lungs. In the peripheral
tissues there is accumulation of fluid as the
kidneys trigger the renin angiotensin
aldosterone cascade which leads to the retention
of salt and water. This causes accumulation of
fluid in the extremities and peripheral tissues.
Decreased ability to conduct gardening or go
for a walk. Cold fingers and toes and have to
wear bed socks
Fatigue results from two causes one being the
decreased oxygen saturation due to pulmonary
edema. This causes carbon (IV)oxide
accumulation when excess activities are
attempted. The high respiratory rate is a
compensation mechanism to increase oxygen
levels and decrease carbon (IV)oxide levels.
Secondly there is decreased blood levels being
circulated to the peripheral tissues hence unable
to conduct activities of daily living. The
kidneys release renin once there is a decrease in
glomerular perfusion which activates the
sympathetic nervous system(Mentz et.al,2015).
This causes vasoconstriction of blood vessels
hence cold fingers and toes.
SIGNS AND SYMPTOMS PATHOPHYSIOLOGY
Increasing shortness of breath, inspiratory
crackles, swollen ankles
Left sided heart failure causes the left ventricle
unable to eject blood therefore blood causes
pulmonary edema in the lungs. This increases
pressure and therefore accumulation of fluid in
alveoli(Lala et.al,2015). There is decreased
gaseous exchange due to lowered surface area
occupied by the fluid causing breathlessness
and decreased oxygen saturation. Lung sounds
heard are inspiratory crackles which signify
presence of fluid in the lungs. In the peripheral
tissues there is accumulation of fluid as the
kidneys trigger the renin angiotensin
aldosterone cascade which leads to the retention
of salt and water. This causes accumulation of
fluid in the extremities and peripheral tissues.
Decreased ability to conduct gardening or go
for a walk. Cold fingers and toes and have to
wear bed socks
Fatigue results from two causes one being the
decreased oxygen saturation due to pulmonary
edema. This causes carbon (IV)oxide
accumulation when excess activities are
attempted. The high respiratory rate is a
compensation mechanism to increase oxygen
levels and decrease carbon (IV)oxide levels.
Secondly there is decreased blood levels being
circulated to the peripheral tissues hence unable
to conduct activities of daily living. The
kidneys release renin once there is a decrease in
glomerular perfusion which activates the
sympathetic nervous system(Mentz et.al,2015).
This causes vasoconstriction of blood vessels
hence cold fingers and toes.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
CASE STUDY 5
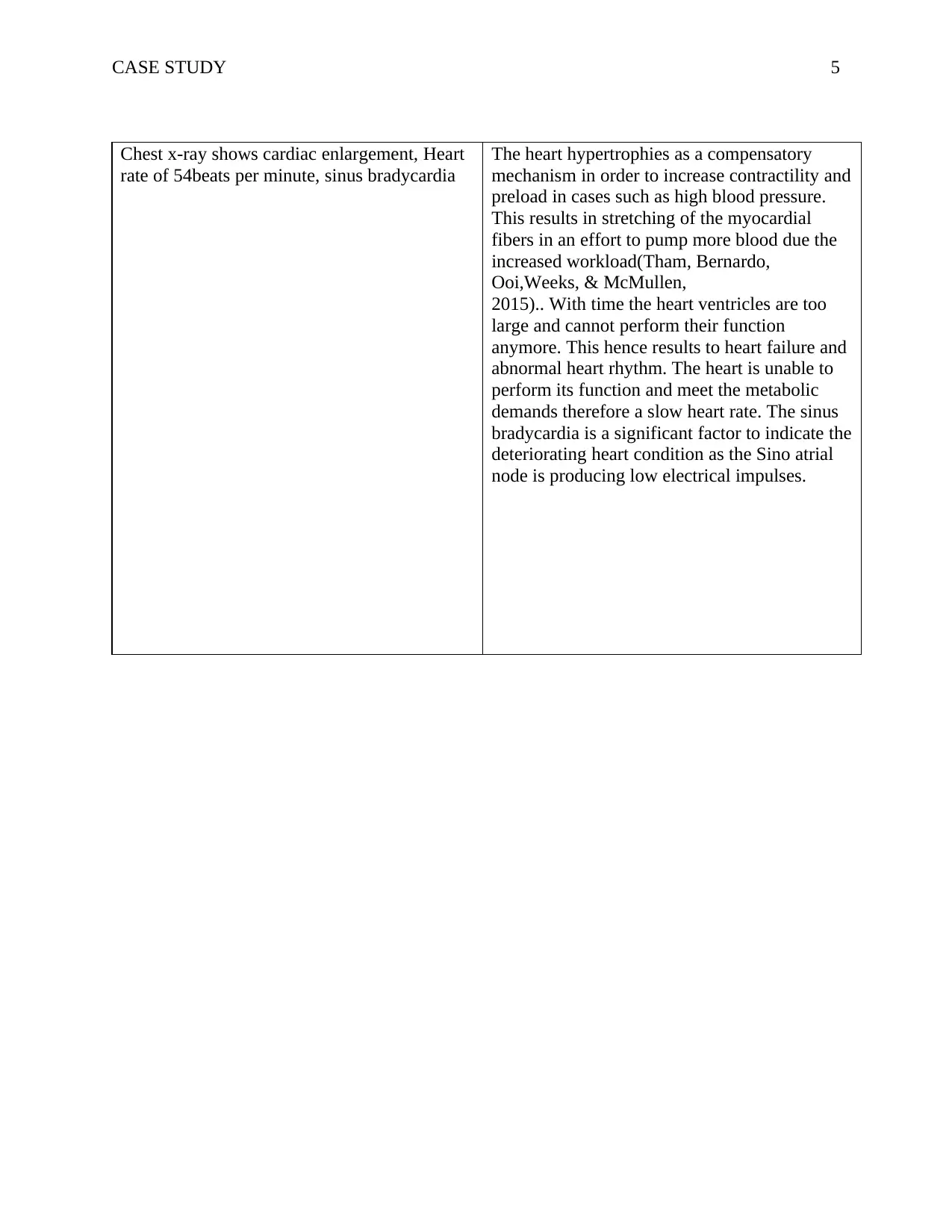
Chest x-ray shows cardiac enlargement, Heart
rate of 54beats per minute, sinus bradycardia
The heart hypertrophies as a compensatory
mechanism in order to increase contractility and
preload in cases such as high blood pressure.
This results in stretching of the myocardial
fibers in an effort to pump more blood due the
increased workload(Tham, Bernardo,
Ooi,Weeks, & McMullen,
2015).. With time the heart ventricles are too
large and cannot perform their function
anymore. This hence results to heart failure and
abnormal heart rhythm. The heart is unable to
perform its function and meet the metabolic
demands therefore a slow heart rate. The sinus
bradycardia is a significant factor to indicate the
deteriorating heart condition as the Sino atrial
node is producing low electrical impulses.
Chest x-ray shows cardiac enlargement, Heart
rate of 54beats per minute, sinus bradycardia
The heart hypertrophies as a compensatory
mechanism in order to increase contractility and
preload in cases such as high blood pressure.
This results in stretching of the myocardial
fibers in an effort to pump more blood due the
increased workload(Tham, Bernardo,
Ooi,Weeks, & McMullen,
2015).. With time the heart ventricles are too
large and cannot perform their function
anymore. This hence results to heart failure and
abnormal heart rhythm. The heart is unable to
perform its function and meet the metabolic
demands therefore a slow heart rate. The sinus
bradycardia is a significant factor to indicate the
deteriorating heart condition as the Sino atrial
node is producing low electrical impulses.

CASE STUDY 6
PHARMACOLOGY
PHARMACODYNAMICS
Enalapril belongs to the group of angiotensin converting enzyme inhibitor. These drugs
are available in oral and intravenous forms. The mechanism of action is inhibiting peptidyl
dipeptidase which converts angiotensin I to angiotensin II. Angiotensin II is responsible for
vasoconstriction and production of aldosterone which results in salt retention. Angiotensin
converting enzyme inhibitors therefore causes decreased workload to the heart by ensuring
diuresis and less fluid retention. This causes a decrease in pulmonary edema. Angiotensin II
causes vasoconstriction leading to increased preload therefore using ACE inhibitor causes
vasodilation. These drugs in conjunction with diuretics for maximum effects.
The side effects are potential hyperkalemia and therefore it is necessary to monitor
potassium levels(Chang, Sang, Leddy, Yahya, Kirchner,Inker & Grams, 2016).. Increased
diuresis also results in loss of sodium and fluid which may result in sudden hypotension. These
necessitates for documentation of input and output chart and monitoring sodium levels. Constant
cough and decreased renal function are among other side effects.
PHARMACOKINETICS
Angiotensin converting enzyme inhibitors in oral form are absorbed in the
gastrointestinal tract. The bioavailability of the drugs varies but the range is about 50-70% after
partial destruction by the digestive enzymes. The drug is available in the body bound in the
plasma to proteins. The drugs are available in active form while others have prodrugs such as
enalapril it is converted to enalaprilat which is the active form (McMurray,, Krum, Abraham,
Dickstein, Køber, Desai & Shao,2016).. The half-life of the drugs differs as that of captopril is 2
PHARMACOLOGY
PHARMACODYNAMICS
Enalapril belongs to the group of angiotensin converting enzyme inhibitor. These drugs
are available in oral and intravenous forms. The mechanism of action is inhibiting peptidyl
dipeptidase which converts angiotensin I to angiotensin II. Angiotensin II is responsible for
vasoconstriction and production of aldosterone which results in salt retention. Angiotensin
converting enzyme inhibitors therefore causes decreased workload to the heart by ensuring
diuresis and less fluid retention. This causes a decrease in pulmonary edema. Angiotensin II
causes vasoconstriction leading to increased preload therefore using ACE inhibitor causes
vasodilation. These drugs in conjunction with diuretics for maximum effects.
The side effects are potential hyperkalemia and therefore it is necessary to monitor
potassium levels(Chang, Sang, Leddy, Yahya, Kirchner,Inker & Grams, 2016).. Increased
diuresis also results in loss of sodium and fluid which may result in sudden hypotension. These
necessitates for documentation of input and output chart and monitoring sodium levels. Constant
cough and decreased renal function are among other side effects.
PHARMACOKINETICS
Angiotensin converting enzyme inhibitors in oral form are absorbed in the
gastrointestinal tract. The bioavailability of the drugs varies but the range is about 50-70% after
partial destruction by the digestive enzymes. The drug is available in the body bound in the
plasma to proteins. The drugs are available in active form while others have prodrugs such as
enalapril it is converted to enalaprilat which is the active form (McMurray,, Krum, Abraham,
Dickstein, Køber, Desai & Shao,2016).. The half-life of the drugs differs as that of captopril is 2

CASE STUDY 7
hours while that of enalapril is 11 hours, that of lisinopril is 12 hours. Angiotensin converting
enzyme inhibitors are eliminated by the renal system although a few are also eliminated by the
liver. This necessitates the need for monitoring the drug levels by urea and creatinine tests as the
risk of renal dysfunction in patients with congestive heart failure the contraindications in using
angiotensin converting enzyme inhibitors is in pregnant patients as it causes congenital
anomalies such as hydrocephalus and spina bifida(DeCara, Lang & Foley(2016).
hours while that of enalapril is 11 hours, that of lisinopril is 12 hours. Angiotensin converting
enzyme inhibitors are eliminated by the renal system although a few are also eliminated by the
liver. This necessitates the need for monitoring the drug levels by urea and creatinine tests as the
risk of renal dysfunction in patients with congestive heart failure the contraindications in using
angiotensin converting enzyme inhibitors is in pregnant patients as it causes congenital
anomalies such as hydrocephalus and spina bifida(DeCara, Lang & Foley(2016).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

CASE STUDY 8
NURSING CARE PLAN
ASSESSMENT NURSING
DIAGNOSE
S
GOALS INTERVEN
TION
RATIONA
LE
IMPLEMETAT
ION
EVALUATION
Swollen ankles
Inspiratory
crackles
Excess fluid
volume
related to
retention of
sodium as
evidenced by
swollen
ankles and
crackles on
auscultation
The patient
should
maintain a
normal
input and
output
The patient
have normal
lung sounds
on
auscultation
Administer
diuretics
while
limiting
water and
salt intake.
Auscultate
for lung
sounds to
assess
improvement
of the
condition
Diuretics
are used to
promote
water
excretion
which will
decrease
cardiac
output
(Damman,,
Kekshus,
Wikstrand,
Cleland,
Komajda,
Wedel, &
McMurray,
2016).
Clear lung
sounds are
evidence of
absence of
pulmonary
edema.
The nurse
administers
diuretics as
ordered while
monitoring the
input and output
chart via
catheterization.
The nurse
auscultates lung
sounds and
notes any
abnormality or
improvement.
The patient has a
normal input
output after
therapeutic
regimen.
The patient has
normal lung
sounds as there is
no pulmonary
edema.
Shortness of
breath
Cold feet
Dizziness
Decreased
cardiac
output
related to
impaired
myocardial
contraction
as evidenced
by cold feet
The patient
should have
improved
cardiac
output by
ability to
perform
activities
without
tachypnea
Patient
The nurse
administers
medication
enalapril
The nurse
administers
oxygen via a
Enalapril is
an
angiotensin
converting
enzyme
inhibitor
which
decreases
workload
and
increases
sodium
excretion
(Sharkey,
Ghafar,
O’Keeffe &
The nurse
monitors the
urinary output
of the patient
while assessing
risk of
complications
such as
hyperkalemia.
The nurse
administers
oxygen via the
The patient has
normal heart rate
and blood
pressure rate.
The patient has
normal oxygen
saturation levels
NURSING CARE PLAN
ASSESSMENT NURSING
DIAGNOSE
S
GOALS INTERVEN
TION
RATIONA
LE
IMPLEMETAT
ION
EVALUATION
Swollen ankles
Inspiratory
crackles
Excess fluid
volume
related to
retention of
sodium as
evidenced by
swollen
ankles and
crackles on
auscultation
The patient
should
maintain a
normal
input and
output
The patient
have normal
lung sounds
on
auscultation
Administer
diuretics
while
limiting
water and
salt intake.
Auscultate
for lung
sounds to
assess
improvement
of the
condition
Diuretics
are used to
promote
water
excretion
which will
decrease
cardiac
output
(Damman,,
Kekshus,
Wikstrand,
Cleland,
Komajda,
Wedel, &
McMurray,
2016).
Clear lung
sounds are
evidence of
absence of
pulmonary
edema.
The nurse
administers
diuretics as
ordered while
monitoring the
input and output
chart via
catheterization.
The nurse
auscultates lung
sounds and
notes any
abnormality or
improvement.
The patient has a
normal input
output after
therapeutic
regimen.
The patient has
normal lung
sounds as there is
no pulmonary
edema.
Shortness of
breath
Cold feet
Dizziness
Decreased
cardiac
output
related to
impaired
myocardial
contraction
as evidenced
by cold feet
The patient
should have
improved
cardiac
output by
ability to
perform
activities
without
tachypnea
Patient
The nurse
administers
medication
enalapril
The nurse
administers
oxygen via a
Enalapril is
an
angiotensin
converting
enzyme
inhibitor
which
decreases
workload
and
increases
sodium
excretion
(Sharkey,
Ghafar,
O’Keeffe &
The nurse
monitors the
urinary output
of the patient
while assessing
risk of
complications
such as
hyperkalemia.
The nurse
administers
oxygen via the
The patient has
normal heart rate
and blood
pressure rate.
The patient has
normal oxygen
saturation levels

CASE STUDY 9
should have
oxygen
saturation
levels of
97%
non-
breathable
mask while
monitoring
saturation
levels
Mulkerrin, ,
2019).
The
supplementa
l oxygen
ensures that
the oxygen
demand is
met
mask and
monitors
oxygen levels
at 95-97%.
Respiratory rate
of 30 breaths
per minute
Shortness of
breath
Dizziness
Ineffective
breathing
pattern
related to
pulmonary
edema
secondary to
heart failure
as evidenced
by tachypnea
The patient
maintains a
breathing
rate within
normal
range of 13
to 20
breaths per
minute
The patient
is able to
perform
breathing
exercises
which
assists in
oxygenation
The nurse
props the
patient in a
Semi-
Fowler’s
position
The nurse
teaches the
patient how
to take deep
breaths
during
inspiration.
Semi-
Fowler’s
position
improves
oxygenation
levels
especially
where it is
compromise
d
Deep
breathing
improves
lung
capacity and
improve
ventilation.
(Slater,
Abshire, &
Davidson20
18)
The nurse
elevates the
patient’s bed at
45 degrees and
explains to the
patient the
rationale.
The nurse
teaches the
patient how to
perform deep
inspiratory
breathes.
The patient has
normal breathing
pattern.
The patient can
perform deep
inspiratory
breaths on
instruction.
should have
oxygen
saturation
levels of
97%
non-
breathable
mask while
monitoring
saturation
levels
Mulkerrin, ,
2019).
The
supplementa
l oxygen
ensures that
the oxygen
demand is
met
mask and
monitors
oxygen levels
at 95-97%.
Respiratory rate
of 30 breaths
per minute
Shortness of
breath
Dizziness
Ineffective
breathing
pattern
related to
pulmonary
edema
secondary to
heart failure
as evidenced
by tachypnea
The patient
maintains a
breathing
rate within
normal
range of 13
to 20
breaths per
minute
The patient
is able to
perform
breathing
exercises
which
assists in
oxygenation
The nurse
props the
patient in a
Semi-
Fowler’s
position
The nurse
teaches the
patient how
to take deep
breaths
during
inspiration.
Semi-
Fowler’s
position
improves
oxygenation
levels
especially
where it is
compromise
d
Deep
breathing
improves
lung
capacity and
improve
ventilation.
(Slater,
Abshire, &
Davidson20
18)
The nurse
elevates the
patient’s bed at
45 degrees and
explains to the
patient the
rationale.
The nurse
teaches the
patient how to
perform deep
inspiratory
breathes.
The patient has
normal breathing
pattern.
The patient can
perform deep
inspiratory
breaths on
instruction.
CASE STUDY 10
REFERENCES
Australian Institute of Health and Welfare(2017).Statistics of prevalence among heart failure
Australians.Retrieved from: https://www.aihw.gov.au/reports/heart-stroke-vascular-
diseases/heart-failure-future/contents/summary
Chang, A. R., Sang, Y., Leddy, J., Yahya, T., Kirchner, H. L., Inker, L. A., ... & Grams, M. E.
(2016). Antihypertensive medications and the prevalence of hyperkalemia in a large
health system. Hypertension, 67(6), 1181-1188.
Damman, K., Kjekshus, J., Wikstrand, J., Cleland, J. G., Komajda, M., Wedel, H., ... &
McMurray, J. J. (2016). Loop diuretics, renal function and clinical outcome in patients
with heart failure and reduced ejection fraction. European journal of heart failure, 18(3),
328-336.
DeCara, J. M., Lang, R. M., & Foley, M. R. (2016). Management of heart failure during
pregnancy.
Lala, A., McNulty, S. E., Mentz, R. J., Dunlay, S. M., Vader, J. M., AbouEzzeddine, O. F., ... &
Bart, B. A. (2015). Relief and recurrence of congestion during and after hospitalization
for acute heart failure: insights from Diuretic Optimization Strategy Evaluation in Acute
Decompensated Heart Failure (DOSE-AHF) and Cardiorenal Rescue Study in Acute
Decompensated Heart Failure (CARESS-HF). Circulation: Heart Failure, 8(4), 741-748.
Liu, J. C., Chang, L. Y., Wu, S. Y., & Tsai, P. S. (2015). Resilience mediates the relationship
between depression and psychological health status in patients with heart failure: A cross-
sectional study. International Journal of Nursing Studies, 52(12), 1846-1853.
REFERENCES
Australian Institute of Health and Welfare(2017).Statistics of prevalence among heart failure
Australians.Retrieved from: https://www.aihw.gov.au/reports/heart-stroke-vascular-
diseases/heart-failure-future/contents/summary
Chang, A. R., Sang, Y., Leddy, J., Yahya, T., Kirchner, H. L., Inker, L. A., ... & Grams, M. E.
(2016). Antihypertensive medications and the prevalence of hyperkalemia in a large
health system. Hypertension, 67(6), 1181-1188.
Damman, K., Kjekshus, J., Wikstrand, J., Cleland, J. G., Komajda, M., Wedel, H., ... &
McMurray, J. J. (2016). Loop diuretics, renal function and clinical outcome in patients
with heart failure and reduced ejection fraction. European journal of heart failure, 18(3),
328-336.
DeCara, J. M., Lang, R. M., & Foley, M. R. (2016). Management of heart failure during
pregnancy.
Lala, A., McNulty, S. E., Mentz, R. J., Dunlay, S. M., Vader, J. M., AbouEzzeddine, O. F., ... &
Bart, B. A. (2015). Relief and recurrence of congestion during and after hospitalization
for acute heart failure: insights from Diuretic Optimization Strategy Evaluation in Acute
Decompensated Heart Failure (DOSE-AHF) and Cardiorenal Rescue Study in Acute
Decompensated Heart Failure (CARESS-HF). Circulation: Heart Failure, 8(4), 741-748.
Liu, J. C., Chang, L. Y., Wu, S. Y., & Tsai, P. S. (2015). Resilience mediates the relationship
between depression and psychological health status in patients with heart failure: A cross-
sectional study. International Journal of Nursing Studies, 52(12), 1846-1853.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
CASE STUDY 11
McMurray, J. J., Krum, H., Abraham, W. T., Dickstein, K., Køber, L. V., Desai, A. S., ... &
Shao, Q. (2016). Aliskiren, enalapril, or aliskiren and enalapril in heart failure. New
England Journal of Medicine, 374(16), 1521-1532.
Mentz, R. J., Stevens, S. R., DeVore, A. D., Lala, A., Vader, J. M., AbouEzzeddine, O. F., ... &
Goldsmith, S. R. (2015). Decongestion strategies and renin-angiotensin-aldosterone
system activation in acute heart failure. JACC: Heart Failure, 3(2), 97-107.
Moe, G. W., Ezekowitz, J. A., O'Meara, E., Lepage, S., Howlett, J. G., Fremes, S., ... & Estrella-
Holder, E. (2015). The 2014 Canadian Cardiovascular Society heart failure management
guidelines focus update: anemia, biomarkers, and recent therapeutic trial implications.
Canadian Journal of Cardiology, 31(1), 3-16.
Sharkey, A. T., Ghafar, M. Z., T O’Keeffe, S., & Mulkerrin, E. C. (2019). Angiotensin receptor
neprilysin inhibitors in older patients with heart failure. BMJ evidence-based medicine,
24(1), 5-7.
Slater, T., Abshire, M., & Davidson, P. (2018). Assessment of breathlessness: A critical
dimension of identifying cardiovascular disease. Australian Nursing and Midwifery
Journal, 25(9), 36.
Tham, Y. K., Bernardo, B. C., Ooi, J. Y., Weeks, K. L., & McMullen, J. R. (2015).
Pathophysiology of cardiac hypertrophy and heart failure: signaling pathways and novel
therapeutic targets. Archives of toxicology, 89(9), 1401-1438.
McMurray, J. J., Krum, H., Abraham, W. T., Dickstein, K., Køber, L. V., Desai, A. S., ... &
Shao, Q. (2016). Aliskiren, enalapril, or aliskiren and enalapril in heart failure. New
England Journal of Medicine, 374(16), 1521-1532.
Mentz, R. J., Stevens, S. R., DeVore, A. D., Lala, A., Vader, J. M., AbouEzzeddine, O. F., ... &
Goldsmith, S. R. (2015). Decongestion strategies and renin-angiotensin-aldosterone
system activation in acute heart failure. JACC: Heart Failure, 3(2), 97-107.
Moe, G. W., Ezekowitz, J. A., O'Meara, E., Lepage, S., Howlett, J. G., Fremes, S., ... & Estrella-
Holder, E. (2015). The 2014 Canadian Cardiovascular Society heart failure management
guidelines focus update: anemia, biomarkers, and recent therapeutic trial implications.
Canadian Journal of Cardiology, 31(1), 3-16.
Sharkey, A. T., Ghafar, M. Z., T O’Keeffe, S., & Mulkerrin, E. C. (2019). Angiotensin receptor
neprilysin inhibitors in older patients with heart failure. BMJ evidence-based medicine,
24(1), 5-7.
Slater, T., Abshire, M., & Davidson, P. (2018). Assessment of breathlessness: A critical
dimension of identifying cardiovascular disease. Australian Nursing and Midwifery
Journal, 25(9), 36.
Tham, Y. K., Bernardo, B. C., Ooi, J. Y., Weeks, K. L., & McMullen, J. R. (2015).
Pathophysiology of cardiac hypertrophy and heart failure: signaling pathways and novel
therapeutic targets. Archives of toxicology, 89(9), 1401-1438.

CASE STUDY 12
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





