Gold Coast University: 2804NRS Spinal Cord Compression Case Study
VerifiedAdded on 2022/09/15
|7
|1528
|18
Case Study
AI Summary
This case study examines a 65-year-old woman, Susan Kennedy, presenting with spinal cord compression due to osteoporotic vertebral fractures. The assignment details the patient's symptoms including back pain, numbness, and high blood pressure, along with hyperreflexia. It explores the aetiology, pathophysiology, diagnostic methods such as MRI and CT scans, and treatment options including medication, physical therapy, and epidural steroids. The analysis covers risk factors like osteoporosis and trauma, the step-by-step sequence of the links between the aetiology and the pathophysiology of the diagnosed disease, and the clinical manifestations. A concept map is included that visually represents the connections between risk factors, aetiology, pathophysiology, clinical manifestations, diagnostic tests, and treatment modalities. The assignment aims to demonstrate clinical reasoning skills and the ability to differentiate normal from abnormal presentations in a nursing context. The document also includes a concept map that visually represents the connections between risk factors, aetiology, pathophysiology, clinical manifestations, diagnostic tests, and treatment modalities, and a references list.

Running head: CASE STUDY
Case Study
Name of the Student
Name of the University
Author Note
Case Study
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
CASE STUDY
Spinal cord compression
Spinal cord compression develops when the spinal cord is compressed due to fracture
in the bone, a tumour swelling and cracked intervertebral disc (Troke & Andrewes 2019). It
is observed as an abrupt crisis condition liberated of the cause and also needs fast diagnosis
and management to stop long-standing incapacity due to irreparable spinal cord damage. It is
most frequently caused by extra medullary lesion than intramedullary lesion. It is generally of
three types such as acute, sub-acute and chronic.
Aetiology
The acute compression occurs due to trauma which is a vertebral fracture along with
displacement of fracture, chronic injury in the discs or metastatic tumour. The process
bandages or displaces venous, arterials, and cerebrospinal spaces or the cord itself. The root
dysfunction is common in this disease, which includes loss of sensations, movement
problems, and loss of motor functions. The common symptoms of this disease are pain
specially in the lower back side, numbness, high blood pressure and problem in movement.
The patient in this case study has symptoms such as lower back pain, numbness in legs, the
blood pressure was also high. Hyperreflexia is a condition of upper motor neuron
dysfunctioning. It also disrupts the lower neural functions. The risk factors are tumour due to
vertebral fracture, osteoporosis and trauma. It may also lead to spinal deformity. The patient
had osteoporosis which is commonly caused due to osteoarthritis. It also common among
aged women due to weak bones. The pressure in the nerve cells specially in the lumbar
region results in equine syndrome that results in loss of bowel movements, numbness in legs
and pain specially during movement.
Pathophysiology
CASE STUDY
Spinal cord compression
Spinal cord compression develops when the spinal cord is compressed due to fracture
in the bone, a tumour swelling and cracked intervertebral disc (Troke & Andrewes 2019). It
is observed as an abrupt crisis condition liberated of the cause and also needs fast diagnosis
and management to stop long-standing incapacity due to irreparable spinal cord damage. It is
most frequently caused by extra medullary lesion than intramedullary lesion. It is generally of
three types such as acute, sub-acute and chronic.
Aetiology
The acute compression occurs due to trauma which is a vertebral fracture along with
displacement of fracture, chronic injury in the discs or metastatic tumour. The process
bandages or displaces venous, arterials, and cerebrospinal spaces or the cord itself. The root
dysfunction is common in this disease, which includes loss of sensations, movement
problems, and loss of motor functions. The common symptoms of this disease are pain
specially in the lower back side, numbness, high blood pressure and problem in movement.
The patient in this case study has symptoms such as lower back pain, numbness in legs, the
blood pressure was also high. Hyperreflexia is a condition of upper motor neuron
dysfunctioning. It also disrupts the lower neural functions. The risk factors are tumour due to
vertebral fracture, osteoporosis and trauma. It may also lead to spinal deformity. The patient
had osteoporosis which is commonly caused due to osteoarthritis. It also common among
aged women due to weak bones. The pressure in the nerve cells specially in the lumbar
region results in equine syndrome that results in loss of bowel movements, numbness in legs
and pain specially during movement.
Pathophysiology
2
CASE STUDY
The pathophysiology of spinal cord damage can be considered as acute influence or
compression. The patient in the case study developed this condition of compression due to
osteoporosis. The reason for the numbness, hyperreflexia, loss of sensation are as follows-
Acute impact damage is basically a shock of the spinal cord. This sort of damage triggers a
cascade of proceedings engrossed in the grey matter, and effects in haemorrhagic necrosis.
The originating occurrence is a hypo perfusion of the grey matter. Upsurges in intracellular
calcium and reperfusion damage show key parts in cellular wound, and happen initially after
injury (Manson, Warnock & Crowther 2017). The degree of necrosis is dependent on the
quantity of early strength of trauma, but also contains associated compression, perfusion
stresses and blood movement (Kaplow & Iyere 2016). Spinal cord firmness happens when a
bulk imposes on the spinal cord producing amplified parenchymal pressure (Epstein 2018).
The tissue reaction is demyelination, gliosis and axonal loss. This happens in the white
matter, while grey matter structures are conserved. Rapid or a serious gradation of density
will effect in downfall of the venous lateral of the microvasculature, subsequent in vasogenic
oedema. Vasogenic oedema impairs parenchymal compression, and may clue to quick
development of dysfunction. Management of firmness should focus on elimination of the
offending mass. The blood pressure rises due to mainly of two factors such as elasticity and
defective body activity (McIlroy & Bell 2017). The spinal injury damages the transduction of
signals from the brain the other parts of the body. This condition implies that the blood
vessels and the heart fail to receive signals for adjusting the pressure or constricts more force
or transfers less amount of blood in brain. This changes can severely affects the blood
pressure as well as lowers the chance of recovery. In chronic condition, it may lead to
autonomic dysreflexia, which is a nervous response of the body due to painful stimulus. It is
also common in-patient with T6 injury.
Diagnostic Methods and Treatment
CASE STUDY
The pathophysiology of spinal cord damage can be considered as acute influence or
compression. The patient in the case study developed this condition of compression due to
osteoporosis. The reason for the numbness, hyperreflexia, loss of sensation are as follows-
Acute impact damage is basically a shock of the spinal cord. This sort of damage triggers a
cascade of proceedings engrossed in the grey matter, and effects in haemorrhagic necrosis.
The originating occurrence is a hypo perfusion of the grey matter. Upsurges in intracellular
calcium and reperfusion damage show key parts in cellular wound, and happen initially after
injury (Manson, Warnock & Crowther 2017). The degree of necrosis is dependent on the
quantity of early strength of trauma, but also contains associated compression, perfusion
stresses and blood movement (Kaplow & Iyere 2016). Spinal cord firmness happens when a
bulk imposes on the spinal cord producing amplified parenchymal pressure (Epstein 2018).
The tissue reaction is demyelination, gliosis and axonal loss. This happens in the white
matter, while grey matter structures are conserved. Rapid or a serious gradation of density
will effect in downfall of the venous lateral of the microvasculature, subsequent in vasogenic
oedema. Vasogenic oedema impairs parenchymal compression, and may clue to quick
development of dysfunction. Management of firmness should focus on elimination of the
offending mass. The blood pressure rises due to mainly of two factors such as elasticity and
defective body activity (McIlroy & Bell 2017). The spinal injury damages the transduction of
signals from the brain the other parts of the body. This condition implies that the blood
vessels and the heart fail to receive signals for adjusting the pressure or constricts more force
or transfers less amount of blood in brain. This changes can severely affects the blood
pressure as well as lowers the chance of recovery. In chronic condition, it may lead to
autonomic dysreflexia, which is a nervous response of the body due to painful stimulus. It is
also common in-patient with T6 injury.
Diagnostic Methods and Treatment
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
CASE STUDY
The disease can be diagnosed by gadolinium-enhanced magnetic resonance imaging,
magnetic resonance imaging and plain spine x-ray and computed tomography of spine. MRI
uses computer and field to form a clear and spine picture along with its surrounding
(Paniagua-Collado & Cauli 2018). The computed tomography uses x-rays and technologies to
identify the fractured or slide bones in different angles. These techniques detect the
abnormalities such as pinched nerves, soft tissues, and calcified tissues (Gutt et al. 2018).. A
CT scan technique helps in diagnosis of fractures and osteoarthritis. Other factors that are
considered in diagnosis are immunosuppression, loss of rectal reflex, malignancy (Tsagozis
& Bauer 2019). The condition can be treated by dexamethasone drug given intravenously or
radiation therapy, the drug inhibits the cells and suppresses the activity of inflammatory
chemical mediators (Kaplow & APRN-CCNS 2016). Anti-inflammatory drug can help in
reducing the state of the patient along with relaxation from pain. Epidural steroid injections
also used in the treatment of compression. A non-pharmacological intervention includes
physical therapy such as light or mild exercises, which is beneficial in strengthening the
abdominal muscles especially in the legs. Applying ice or heat pad can also reduce the
painful condition or acupuncture (Fenton et al. 2019).
CASE STUDY
The disease can be diagnosed by gadolinium-enhanced magnetic resonance imaging,
magnetic resonance imaging and plain spine x-ray and computed tomography of spine. MRI
uses computer and field to form a clear and spine picture along with its surrounding
(Paniagua-Collado & Cauli 2018). The computed tomography uses x-rays and technologies to
identify the fractured or slide bones in different angles. These techniques detect the
abnormalities such as pinched nerves, soft tissues, and calcified tissues (Gutt et al. 2018).. A
CT scan technique helps in diagnosis of fractures and osteoarthritis. Other factors that are
considered in diagnosis are immunosuppression, loss of rectal reflex, malignancy (Tsagozis
& Bauer 2019). The condition can be treated by dexamethasone drug given intravenously or
radiation therapy, the drug inhibits the cells and suppresses the activity of inflammatory
chemical mediators (Kaplow & APRN-CCNS 2016). Anti-inflammatory drug can help in
reducing the state of the patient along with relaxation from pain. Epidural steroid injections
also used in the treatment of compression. A non-pharmacological intervention includes
physical therapy such as light or mild exercises, which is beneficial in strengthening the
abdominal muscles especially in the legs. Applying ice or heat pad can also reduce the
painful condition or acupuncture (Fenton et al. 2019).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
CASE STUDY
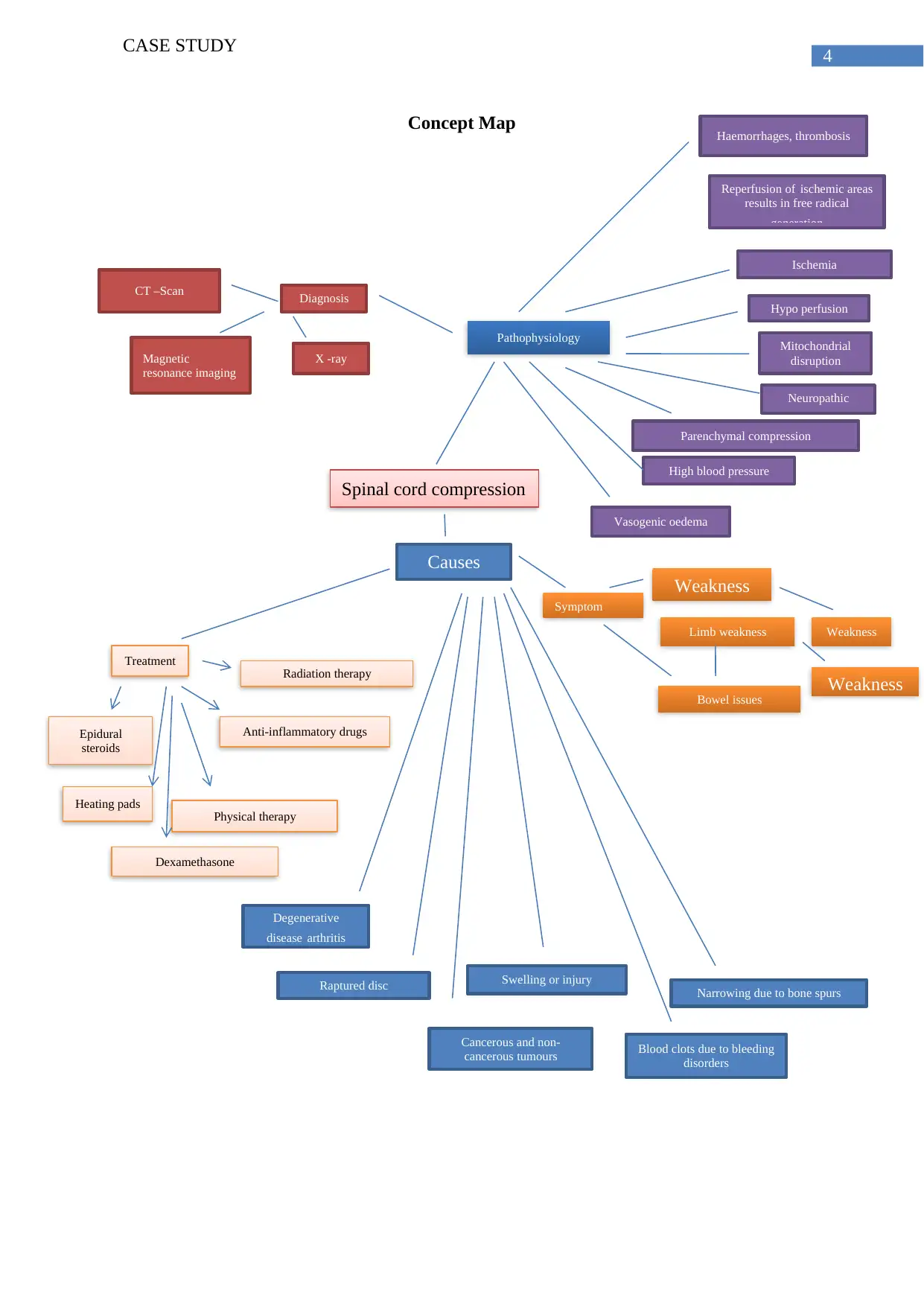
Concept Map
Spinal cord compression
Degenerative
disease arthritis
Causes
Blood clots due to bleeding
disorders
Raptured disc Swelling or injury
Cancerous and non-
cancerous tumours
Narrowing due to bone spurs
Treatment
Epidural
steroids
Anti-inflammatory drugs
Heating pads Physical therapy
Dexamethasone
Radiation therapy
Magnetic
resonance imaging
CT –Scan
X -ray
Diagnosis
Haemorrhages, thrombosis
Reperfusion of ischemic areas
results in free radical
generation
Ischemia
Hypo perfusion
Mitochondrial
disruption
Neuropathic
pain
Parenchymal compression
High blood pressure
Vasogenic oedema
Weakness
Limb weakness
Symptom
Bowel issues
Weakness
Weakness
Pathophysiology
CASE STUDY
Concept Map
Spinal cord compression
Degenerative
disease arthritis
Causes
Blood clots due to bleeding
disorders
Raptured disc Swelling or injury
Cancerous and non-
cancerous tumours
Narrowing due to bone spurs
Treatment
Epidural
steroids
Anti-inflammatory drugs
Heating pads Physical therapy
Dexamethasone
Radiation therapy
Magnetic
resonance imaging
CT –Scan
X -ray
Diagnosis
Haemorrhages, thrombosis
Reperfusion of ischemic areas
results in free radical
generation
Ischemia
Hypo perfusion
Mitochondrial
disruption
Neuropathic
pain
Parenchymal compression
High blood pressure
Vasogenic oedema
Weakness
Limb weakness
Symptom
Bowel issues
Weakness
Weakness
Pathophysiology
5
CASE STUDY
References
Epstein, N. E. (2018). Nursing review of spinal meningiomas. Surgical neurology
international, 9. doi: 10.4103/sni.sni_408_17
Fenton, M., Goyal, S., Gatfield, E. R., & Forner, S. (2019). An electronic proforma to
improve documentation for cases of metastatic spinal cord compression: A quality-
improvement project. Clinical Oncology, 31, e6. Retrieved from
https://www.clinicaloncologyonline.net/article/S0936-6555(19)30404-2/abstract
Gutt, R., Malhotra, S., Jolly, S., Moghanaki, D., Cheuk, A. V., Fosmire, H., ... & Dawson, G.
(2018). Management of metastatic spinal cord compression among Veterans Health
Administration radiation oncologists. Annals of palliative medicine, 7(2), 234-241.
Retrieved from https://europepmc.org/article/med/29764185
Kaplow, R., & APRN-CCNS, A. O. C. N. S. (2016). spinal cord compression. Retrieved from
https://alliedhealth.ceconnection.com/files/UnderstandingSpinalCordCompression-
1491248755836.pdf
Kaplow, R., & Iyere, K. (2016). Understanding spinal cord compression. Nursing2019, 46(9),
44-51. Retrieved from
https://journals.lww.com/nursing/Fulltext/2016/09000/Understanding_spinal_cord_co
mpression.10.aspx
Manson, J., Warnock, C., & Crowther, L. (2017). Patient’s experiences of being discharged
home from hospital following a diagnosis of malignant spinal cord
compression. Supportive Care in Cancer, 25(6), 1829-1836. Retrieved from
https://link.springer.com/article/10.1007/s00520-017-3577-z
CASE STUDY
References
Epstein, N. E. (2018). Nursing review of spinal meningiomas. Surgical neurology
international, 9. doi: 10.4103/sni.sni_408_17
Fenton, M., Goyal, S., Gatfield, E. R., & Forner, S. (2019). An electronic proforma to
improve documentation for cases of metastatic spinal cord compression: A quality-
improvement project. Clinical Oncology, 31, e6. Retrieved from
https://www.clinicaloncologyonline.net/article/S0936-6555(19)30404-2/abstract
Gutt, R., Malhotra, S., Jolly, S., Moghanaki, D., Cheuk, A. V., Fosmire, H., ... & Dawson, G.
(2018). Management of metastatic spinal cord compression among Veterans Health
Administration radiation oncologists. Annals of palliative medicine, 7(2), 234-241.
Retrieved from https://europepmc.org/article/med/29764185
Kaplow, R., & APRN-CCNS, A. O. C. N. S. (2016). spinal cord compression. Retrieved from
https://alliedhealth.ceconnection.com/files/UnderstandingSpinalCordCompression-
1491248755836.pdf
Kaplow, R., & Iyere, K. (2016). Understanding spinal cord compression. Nursing2019, 46(9),
44-51. Retrieved from
https://journals.lww.com/nursing/Fulltext/2016/09000/Understanding_spinal_cord_co
mpression.10.aspx
Manson, J., Warnock, C., & Crowther, L. (2017). Patient’s experiences of being discharged
home from hospital following a diagnosis of malignant spinal cord
compression. Supportive Care in Cancer, 25(6), 1829-1836. Retrieved from
https://link.springer.com/article/10.1007/s00520-017-3577-z
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
CASE STUDY
McIlroy, S., & Bell, D. (2017). Change in Mobility and Survival Three Months after
Treatment for Metastatic Spinal Cord Compression. Results of a Multi-Centre
Prospective Audit. The Spine Journal, 17(3), S30.
DOI: https://doi.org/10.1016/j.spinee.2016.12.094
Paniagua-Collado, M., & Cauli, O. (2018). Non-pharmacological interventions in patients
with spinal cord compression: a systematic review. Journal of neuro-
oncology, 136(3), 423-434. https://doi.org/10.1007/s11060-017-2684-5
Troke, R., & Andrewes, T. (2019). Nursing considerations for supporting cancer patients with
metastatic spinal cord compression: a literature review. British Journal of
Nursing, 28(17), S24-S29. doi/abs/10.12968/bjon.2019.28.17.S24
Tsagozis, P., & Bauer, H. C. (2019). Outcome of Surgical Treatment for Spinal Cord
Compression in Patients With Hematological Malignancy. International journal of
spine surgery, 13(2), 186-191. DOI: https://doi.org/10.14444/6025
CASE STUDY
McIlroy, S., & Bell, D. (2017). Change in Mobility and Survival Three Months after
Treatment for Metastatic Spinal Cord Compression. Results of a Multi-Centre
Prospective Audit. The Spine Journal, 17(3), S30.
DOI: https://doi.org/10.1016/j.spinee.2016.12.094
Paniagua-Collado, M., & Cauli, O. (2018). Non-pharmacological interventions in patients
with spinal cord compression: a systematic review. Journal of neuro-
oncology, 136(3), 423-434. https://doi.org/10.1007/s11060-017-2684-5
Troke, R., & Andrewes, T. (2019). Nursing considerations for supporting cancer patients with
metastatic spinal cord compression: a literature review. British Journal of
Nursing, 28(17), S24-S29. doi/abs/10.12968/bjon.2019.28.17.S24
Tsagozis, P., & Bauer, H. C. (2019). Outcome of Surgical Treatment for Spinal Cord
Compression in Patients With Hematological Malignancy. International journal of
spine surgery, 13(2), 186-191. DOI: https://doi.org/10.14444/6025
1 out of 7
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.

