PUBH6005: Critical Appraisal of Epidemiological Studies Assignment
VerifiedAdded on 2023/03/17
|18
|2917
|56
Report
AI Summary
This report presents a critical appraisal of three epidemiological studies, each employing a different research design, as required by the PUBH6005 Epidemiology course. The studies, focusing on public health interventions and risk factors, are evaluated using the CASP (Critical Appraisal Skills Programme) checklists. The first study, a randomized controlled trial, examines a school-based behavioral intervention to reduce smokeless tobacco and betel quid use among adolescents in Karachi. The second study employs a cross-sectional design to investigate the determinants of smokeless tobacco and betel quid use. The third study utilizes a multicenter case-control design to assess the association between tobacco, alcohol, betel quid, and the risk of head and neck cancer in East Asia. Each study is assessed based on its methodology, including the clarity of the research question, study design, participant selection, measurement of exposure and outcomes, handling of confounding factors, and statistical analysis. The report provides detailed comments and justifications for each checklist question, evaluating the strengths and limitations of each study and assessing the applicability of their findings. The report concludes with an overall assessment of the validity and reliability of each study and its contribution to the field of public health.

Running head: CASP 1
CASP
Name
Institutional Affiliation
CASP
Name
Institutional Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CASP 2
Hussain, A., Zaheer, S., & Shafique, K. (2018). School-based behavioral intervention to reduce
the habit of smokeless tobacco and betel quid use in high-risk youth in Karachi: A randomized
controlled trial. PloS one, 13(11), e0206919. https://journals.plos.org/plosone/article?
id=10.1371/journal.pone.0206919
No. Question ANS
.
Justification
1. Did the trial address a clearly-focused
issue?
Yes The study focused on the reducing
the increased use of smokeless
tobacco (SLT) alongside betel liquid
(BQ) chewing amongst South East
Asian adolescents which shot from
7% to 15% between the years 2004
and 2013. The study appreciated the
need for present intervention to alter
the perception of this group
regarding the SLT and BQ’s harmful
effects by urging them to quit
(Hussain, Zaheer & Shafique, 2018).
2. Was the assignment of patients to
treatments randomized?
Yes. The RCT involved 2140 adolescents
from twenty-six public and private-
sector schools in Karachi. Following
randomization, 1185 adolescents
were put in intervention group and
Hussain, A., Zaheer, S., & Shafique, K. (2018). School-based behavioral intervention to reduce
the habit of smokeless tobacco and betel quid use in high-risk youth in Karachi: A randomized
controlled trial. PloS one, 13(11), e0206919. https://journals.plos.org/plosone/article?
id=10.1371/journal.pone.0206919
No. Question ANS
.
Justification
1. Did the trial address a clearly-focused
issue?
Yes The study focused on the reducing
the increased use of smokeless
tobacco (SLT) alongside betel liquid
(BQ) chewing amongst South East
Asian adolescents which shot from
7% to 15% between the years 2004
and 2013. The study appreciated the
need for present intervention to alter
the perception of this group
regarding the SLT and BQ’s harmful
effects by urging them to quit
(Hussain, Zaheer & Shafique, 2018).
2. Was the assignment of patients to
treatments randomized?
Yes. The RCT involved 2140 adolescents
from twenty-six public and private-
sector schools in Karachi. Following
randomization, 1185 adolescents
were put in intervention group and
CASP 3
subsequently administered behavior-
charging intervention (BCI). 955
adolescents were assigned to control
group.
3. Were all the patients who entered the
trial properly accounted for at its
conclusion?
Yes A total of 2200 adolescents from 26
schools took part in this
intervention. The missing
information from sixty students
dropped the sample to 2140. This
was what the ultimate analyses were
done on. The intervention group
constituted 1185 people while the
control group had 955 people.
Following intervention, 169 subjects
(both groups) got lost to follow-up
because of their absence on school
visit day hence rate of retention
stood at 92 percent. The chewers of
BQ and SLT in the control group
stood at 40 percent which got
decreased to 25% during follow-up,
with eight percent quit rate. In the
intervention group, starting rate
subsequently administered behavior-
charging intervention (BCI). 955
adolescents were assigned to control
group.
3. Were all the patients who entered the
trial properly accounted for at its
conclusion?
Yes A total of 2200 adolescents from 26
schools took part in this
intervention. The missing
information from sixty students
dropped the sample to 2140. This
was what the ultimate analyses were
done on. The intervention group
constituted 1185 people while the
control group had 955 people.
Following intervention, 169 subjects
(both groups) got lost to follow-up
because of their absence on school
visit day hence rate of retention
stood at 92 percent. The chewers of
BQ and SLT in the control group
stood at 40 percent which got
decreased to 25% during follow-up,
with eight percent quit rate. In the
intervention group, starting rate
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CASP 4
stood at 44.7% and got lowered to
11.6 percent. Intervention group had
29% participants ceasing their use
following intervention.
4. Were patients, health workers, and
study personnel “blind” to treatment?
Yes The intervention materials were only
given to the control clusters
following the end of the study as this
catered for ethical parameters.
5. Were the groups similar at the start of
the trial?
Yes All the students were similar at the
beginning of the study as they were
randomly selected and randomized
to avoid any selection bias. They
were students from private and
public schools in Karachi.
6. Aside from experimental intervention,
were the groups treated equally?
Yes. Both groups were equally treated.
They were randomly selected and
randomized to avoid any bias. Also,
they were all given a gift hamper
with branded tooth-paste (identity
concealed) to evade conflict of
interest, a tooth brush (identity
concealed to evade conflict of
interest) as well as a pencil with
stood at 44.7% and got lowered to
11.6 percent. Intervention group had
29% participants ceasing their use
following intervention.
4. Were patients, health workers, and
study personnel “blind” to treatment?
Yes The intervention materials were only
given to the control clusters
following the end of the study as this
catered for ethical parameters.
5. Were the groups similar at the start of
the trial?
Yes All the students were similar at the
beginning of the study as they were
randomly selected and randomized
to avoid any selection bias. They
were students from private and
public schools in Karachi.
6. Aside from experimental intervention,
were the groups treated equally?
Yes. Both groups were equally treated.
They were randomly selected and
randomized to avoid any bias. Also,
they were all given a gift hamper
with branded tooth-paste (identity
concealed) to evade conflict of
interest, a tooth brush (identity
concealed to evade conflict of
interest) as well as a pencil with
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CASP 5
imprints, “SAY NO TO
CHALIA/betel nut ad GHUTKA
(SLT). Informed consent was
obtained from all of them.
7. How large was the treatment effects? The treatment effects was large
enough. The researchers expected
variations in the effect sizes of the
BCI in private and government
schools because of variations in
socioeconomic conditions of
learners in every school type,
product availability in different
school types, and varying cultural
background of every school type.
The effect sizes in the study in terms
of alterations in perceptions and
knowledge stood significantly quite
promising among users of than
nonusers. The BCI was also
effective in both nonusers and users
in the intervention groups and
helpful in altering participants’
perceptions that using SLT remains
imprints, “SAY NO TO
CHALIA/betel nut ad GHUTKA
(SLT). Informed consent was
obtained from all of them.
7. How large was the treatment effects? The treatment effects was large
enough. The researchers expected
variations in the effect sizes of the
BCI in private and government
schools because of variations in
socioeconomic conditions of
learners in every school type,
product availability in different
school types, and varying cultural
background of every school type.
The effect sizes in the study in terms
of alterations in perceptions and
knowledge stood significantly quite
promising among users of than
nonusers. The BCI was also
effective in both nonusers and users
in the intervention groups and
helpful in altering participants’
perceptions that using SLT remains
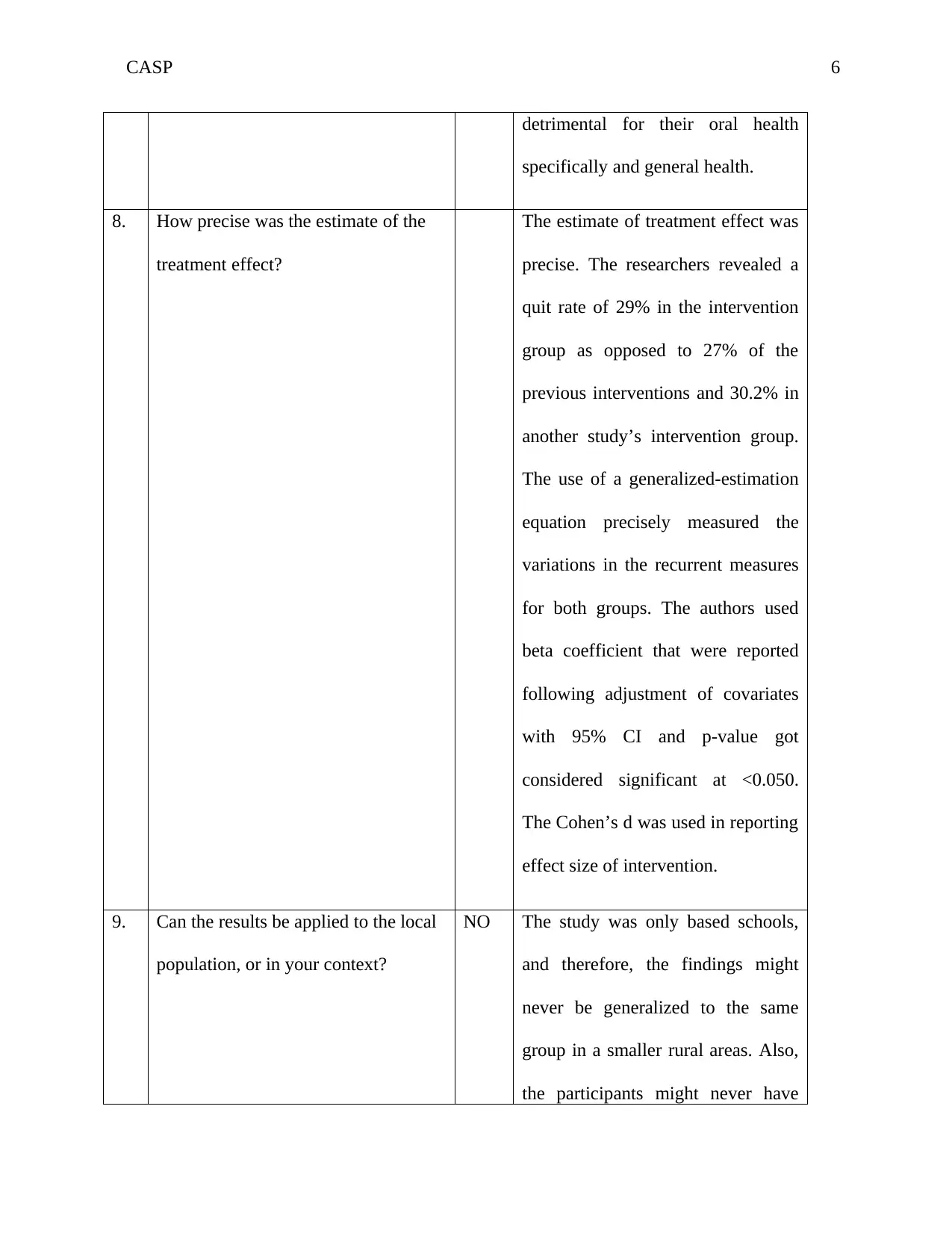
CASP 6
detrimental for their oral health
specifically and general health.
8. How precise was the estimate of the
treatment effect?
The estimate of treatment effect was
precise. The researchers revealed a
quit rate of 29% in the intervention
group as opposed to 27% of the
previous interventions and 30.2% in
another study’s intervention group.
The use of a generalized-estimation
equation precisely measured the
variations in the recurrent measures
for both groups. The authors used
beta coefficient that were reported
following adjustment of covariates
with 95% CI and p-value got
considered significant at <0.050.
The Cohen’s d was used in reporting
effect size of intervention.
9. Can the results be applied to the local
population, or in your context?
NO The study was only based schools,
and therefore, the findings might
never be generalized to the same
group in a smaller rural areas. Also,
the participants might never have
detrimental for their oral health
specifically and general health.
8. How precise was the estimate of the
treatment effect?
The estimate of treatment effect was
precise. The researchers revealed a
quit rate of 29% in the intervention
group as opposed to 27% of the
previous interventions and 30.2% in
another study’s intervention group.
The use of a generalized-estimation
equation precisely measured the
variations in the recurrent measures
for both groups. The authors used
beta coefficient that were reported
following adjustment of covariates
with 95% CI and p-value got
considered significant at <0.050.
The Cohen’s d was used in reporting
effect size of intervention.
9. Can the results be applied to the local
population, or in your context?
NO The study was only based schools,
and therefore, the findings might
never be generalized to the same
group in a smaller rural areas. Also,
the participants might never have
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
CASP 7
accurately reported their perception
and knowledge alterations because
such questions might get
misinterpreted.
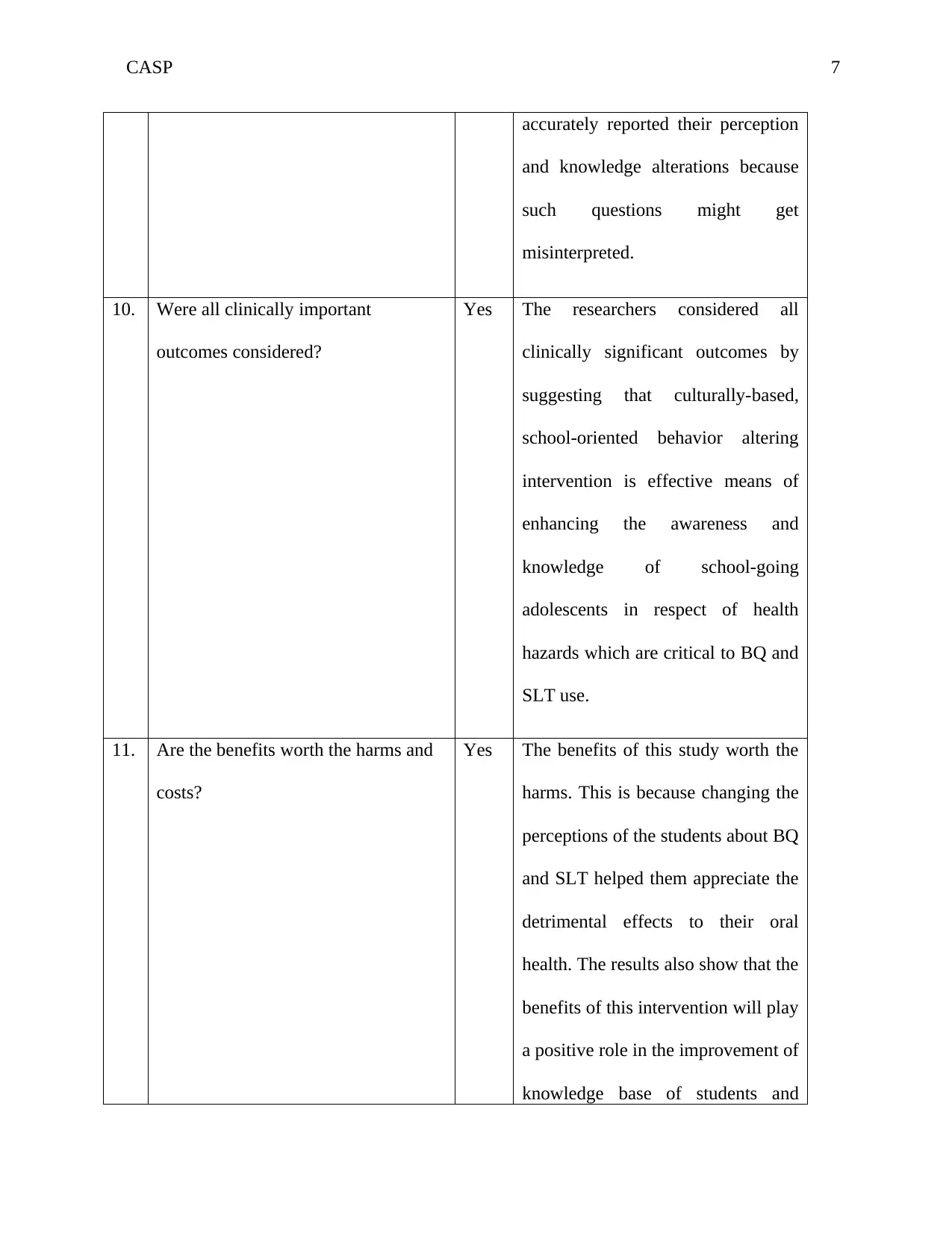
10. Were all clinically important
outcomes considered?
Yes The researchers considered all
clinically significant outcomes by
suggesting that culturally-based,
school-oriented behavior altering
intervention is effective means of
enhancing the awareness and
knowledge of school-going
adolescents in respect of health
hazards which are critical to BQ and
SLT use.
11. Are the benefits worth the harms and
costs?
Yes The benefits of this study worth the
harms. This is because changing the
perceptions of the students about BQ
and SLT helped them appreciate the
detrimental effects to their oral
health. The results also show that the
benefits of this intervention will play
a positive role in the improvement of
knowledge base of students and
accurately reported their perception
and knowledge alterations because
such questions might get
misinterpreted.
10. Were all clinically important
outcomes considered?
Yes The researchers considered all
clinically significant outcomes by
suggesting that culturally-based,
school-oriented behavior altering
intervention is effective means of
enhancing the awareness and
knowledge of school-going
adolescents in respect of health
hazards which are critical to BQ and
SLT use.
11. Are the benefits worth the harms and
costs?
Yes The benefits of this study worth the
harms. This is because changing the
perceptions of the students about BQ
and SLT helped them appreciate the
detrimental effects to their oral
health. The results also show that the
benefits of this intervention will play
a positive role in the improvement of
knowledge base of students and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CASP 8
showcase positive healthy
perceptions about BQ and SLT use,
hence promoting abstinence from
such risky substances.
Hussain, A., Zaheer, S., & Shafique, K. (2017). Individual, social and environmental
determinants of smokeless tobacco and betel quid use amongst adolescents of Karachi: a school-
based cross-sectional survey. BMC public health, 17(1), 913.
https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-017-4916-1
Table 1. CASP checklist for cross sectional study
No. Questions ANS
.
Comments/justification
1. Were the criteria for inclusion in the
sample clearly defined?
Yes They were to be from either of the six
districts, or the 26 clusters (secondary
schools). They were to fall between 11
and 16 years and also study in grade VI-
Grade X. The students of younger or
older than eleven to sixteen years, as
well as those students who already were
going through oral cancer treatment
were never included. Also, where the
showcase positive healthy
perceptions about BQ and SLT use,
hence promoting abstinence from
such risky substances.
Hussain, A., Zaheer, S., & Shafique, K. (2017). Individual, social and environmental
determinants of smokeless tobacco and betel quid use amongst adolescents of Karachi: a school-
based cross-sectional survey. BMC public health, 17(1), 913.
https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-017-4916-1
Table 1. CASP checklist for cross sectional study
No. Questions ANS
.
Comments/justification
1. Were the criteria for inclusion in the
sample clearly defined?
Yes They were to be from either of the six
districts, or the 26 clusters (secondary
schools). They were to fall between 11
and 16 years and also study in grade VI-
Grade X. The students of younger or
older than eleven to sixteen years, as
well as those students who already were
going through oral cancer treatment
were never included. Also, where the
CASP 9
invited school refused to participate,
they would be replaced by sending a
new invitation to another school
(Hussain, Zaheer & Shafique, 2017).
2. Were the study subjects and the setting
described in detail?
Yes The study subjects were of eleven to
sixteen years of age, studying in grade
VI-Grade X. The setting was the
secondary schools.
3. Was the exposure measured in a valid
and reliable way?
Yes The exposure was measured validly and
reliability based on the
4. Were the objectives, standard and criteria
used for the measurement of the
condition?
Can’t
tell
It is not clear from the study whether
these parameters were highlighted
apparently.
5. Were confounding factors identified? Yes Ongoing treatment for oral cancer led to
exclusion.
6. Were strategies to deal with confounding
factors stated?
Yes. The strategies included doing
multivariate adjustments.
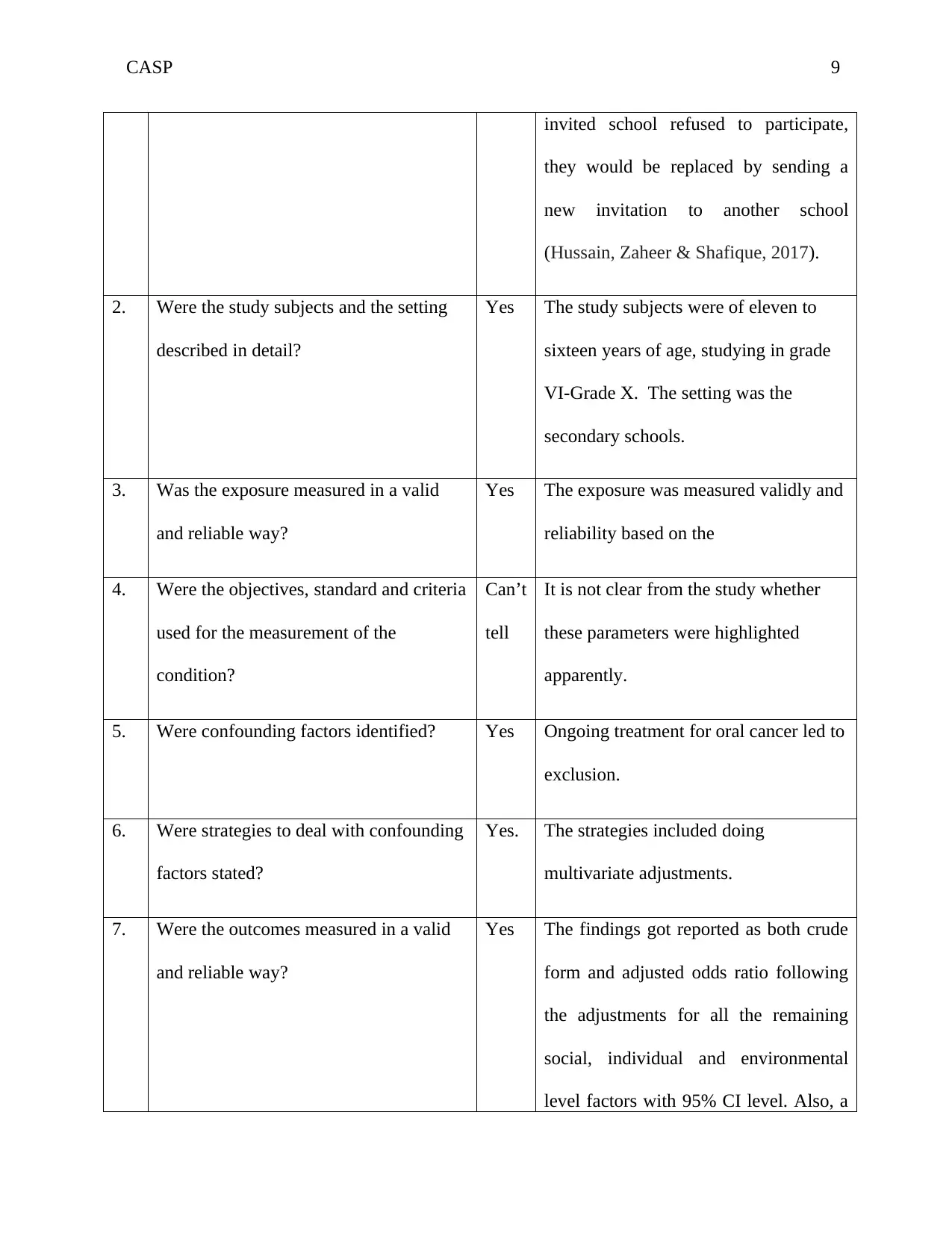
7. Were the outcomes measured in a valid
and reliable way?
Yes The findings got reported as both crude
form and adjusted odds ratio following
the adjustments for all the remaining
social, individual and environmental
level factors with 95% CI level. Also, a
invited school refused to participate,
they would be replaced by sending a
new invitation to another school
(Hussain, Zaheer & Shafique, 2017).
2. Were the study subjects and the setting
described in detail?
Yes The study subjects were of eleven to
sixteen years of age, studying in grade
VI-Grade X. The setting was the
secondary schools.
3. Was the exposure measured in a valid
and reliable way?
Yes The exposure was measured validly and
reliability based on the
4. Were the objectives, standard and criteria
used for the measurement of the
condition?
Can’t
tell
It is not clear from the study whether
these parameters were highlighted
apparently.
5. Were confounding factors identified? Yes Ongoing treatment for oral cancer led to
exclusion.
6. Were strategies to deal with confounding
factors stated?
Yes. The strategies included doing
multivariate adjustments.
7. Were the outcomes measured in a valid
and reliable way?
Yes The findings got reported as both crude
form and adjusted odds ratio following
the adjustments for all the remaining
social, individual and environmental
level factors with 95% CI level. Also, a
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
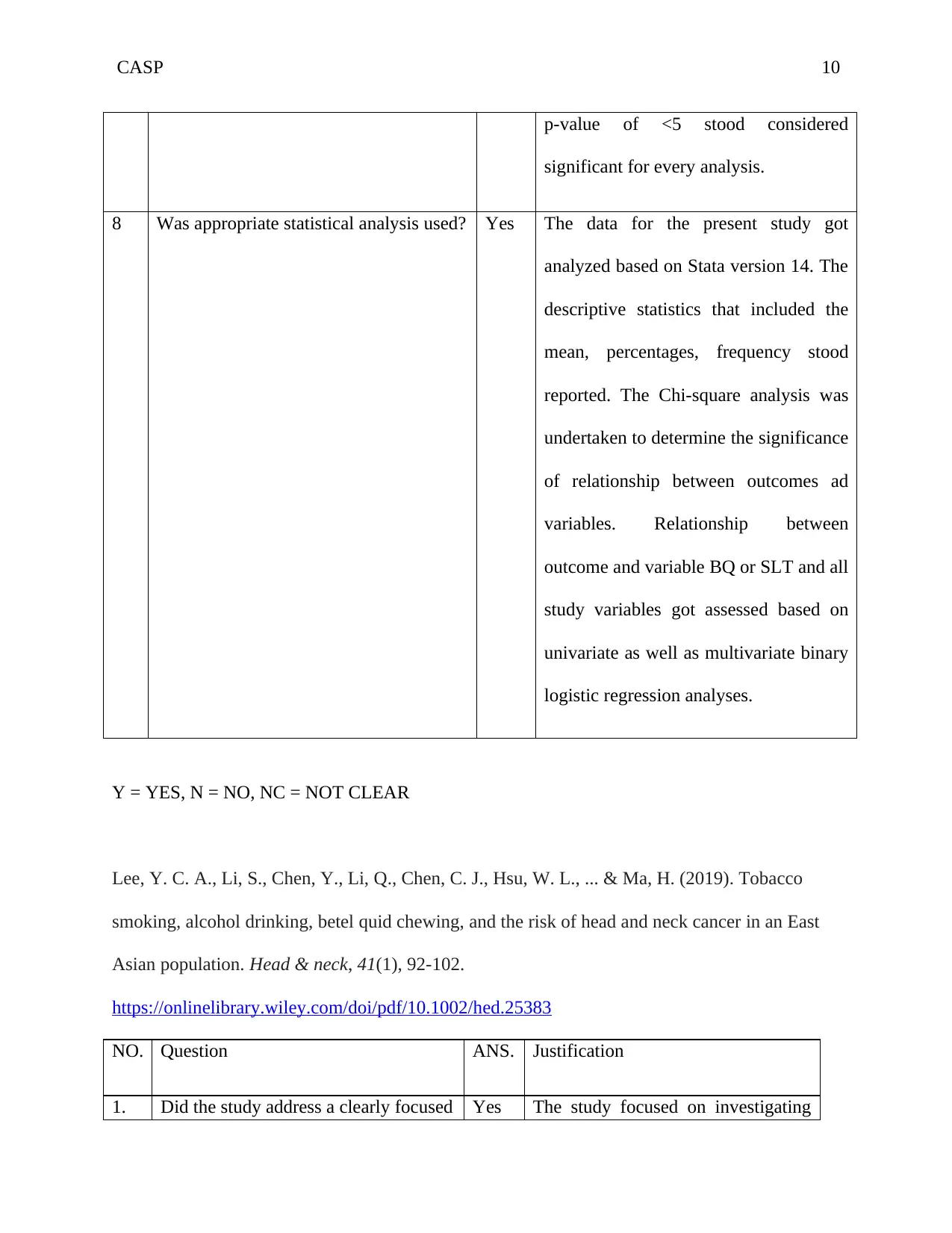
CASP 10
p-value of <5 stood considered
significant for every analysis.
8 Was appropriate statistical analysis used? Yes The data for the present study got
analyzed based on Stata version 14. The
descriptive statistics that included the
mean, percentages, frequency stood
reported. The Chi-square analysis was
undertaken to determine the significance
of relationship between outcomes ad
variables. Relationship between
outcome and variable BQ or SLT and all
study variables got assessed based on
univariate as well as multivariate binary
logistic regression analyses.
Y = YES, N = NO, NC = NOT CLEAR
Lee, Y. C. A., Li, S., Chen, Y., Li, Q., Chen, C. J., Hsu, W. L., ... & Ma, H. (2019). Tobacco
smoking, alcohol drinking, betel quid chewing, and the risk of head and neck cancer in an East
Asian population. Head & neck, 41(1), 92-102.
https://onlinelibrary.wiley.com/doi/pdf/10.1002/hed.25383
NO. Question ANS. Justification
1. Did the study address a clearly focused Yes The study focused on investigating
p-value of <5 stood considered
significant for every analysis.
8 Was appropriate statistical analysis used? Yes The data for the present study got
analyzed based on Stata version 14. The
descriptive statistics that included the
mean, percentages, frequency stood
reported. The Chi-square analysis was
undertaken to determine the significance
of relationship between outcomes ad
variables. Relationship between
outcome and variable BQ or SLT and all
study variables got assessed based on
univariate as well as multivariate binary
logistic regression analyses.
Y = YES, N = NO, NC = NOT CLEAR
Lee, Y. C. A., Li, S., Chen, Y., Li, Q., Chen, C. J., Hsu, W. L., ... & Ma, H. (2019). Tobacco
smoking, alcohol drinking, betel quid chewing, and the risk of head and neck cancer in an East
Asian population. Head & neck, 41(1), 92-102.
https://onlinelibrary.wiley.com/doi/pdf/10.1002/hed.25383
NO. Question ANS. Justification
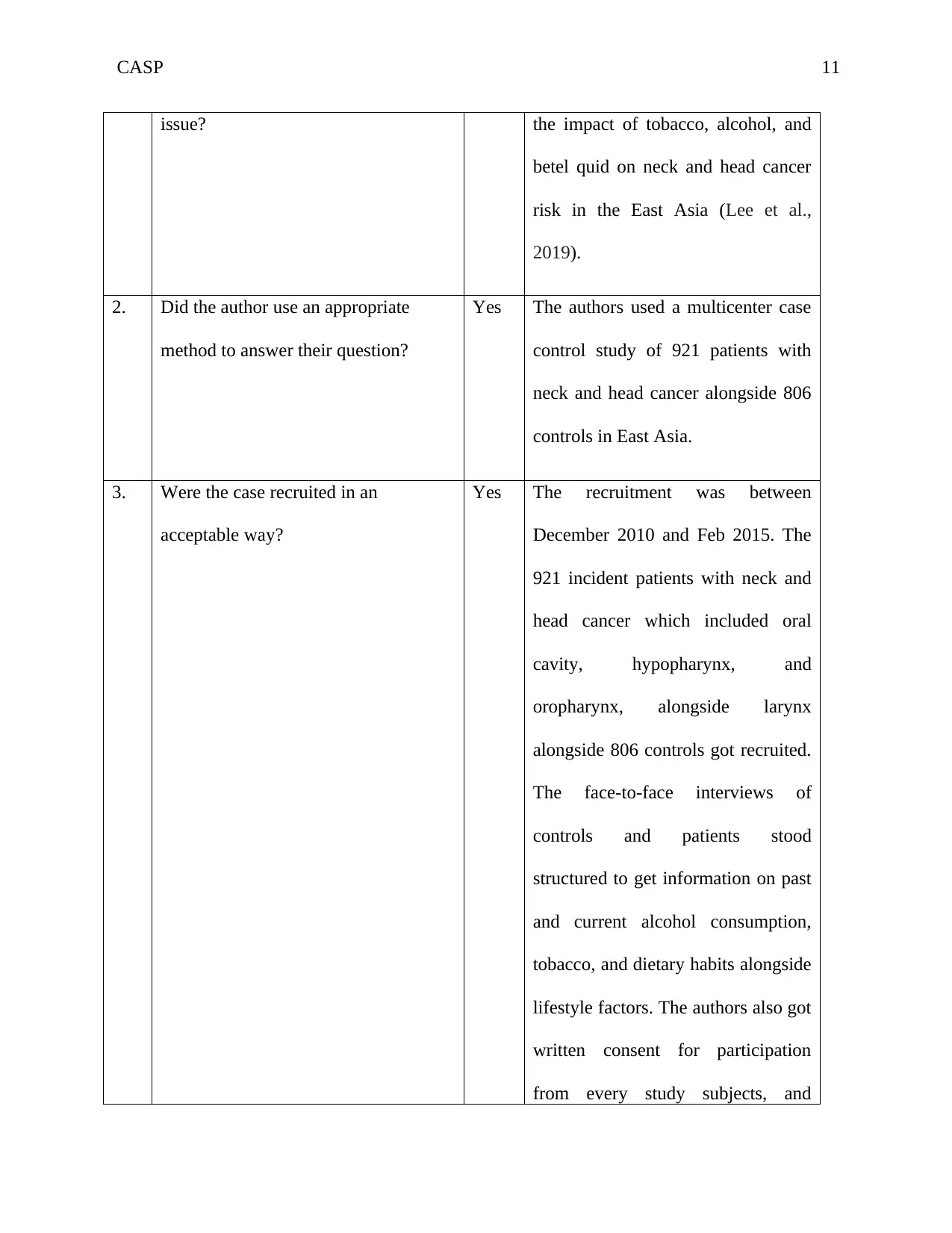
1. Did the study address a clearly focused Yes The study focused on investigating
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CASP 11
issue? the impact of tobacco, alcohol, and
betel quid on neck and head cancer
risk in the East Asia (Lee et al.,
2019).
2. Did the author use an appropriate
method to answer their question?
Yes The authors used a multicenter case
control study of 921 patients with
neck and head cancer alongside 806
controls in East Asia.
3. Were the case recruited in an
acceptable way?
Yes The recruitment was between
December 2010 and Feb 2015. The
921 incident patients with neck and
head cancer which included oral
cavity, hypopharynx, and
oropharynx, alongside larynx
alongside 806 controls got recruited.
The face-to-face interviews of
controls and patients stood
structured to get information on past
and current alcohol consumption,
tobacco, and dietary habits alongside
lifestyle factors. The authors also got
written consent for participation
from every study subjects, and
issue? the impact of tobacco, alcohol, and
betel quid on neck and head cancer
risk in the East Asia (Lee et al.,
2019).
2. Did the author use an appropriate
method to answer their question?
Yes The authors used a multicenter case
control study of 921 patients with
neck and head cancer alongside 806
controls in East Asia.
3. Were the case recruited in an
acceptable way?
Yes The recruitment was between
December 2010 and Feb 2015. The
921 incident patients with neck and
head cancer which included oral
cavity, hypopharynx, and
oropharynx, alongside larynx
alongside 806 controls got recruited.
The face-to-face interviews of
controls and patients stood
structured to get information on past
and current alcohol consumption,
tobacco, and dietary habits alongside
lifestyle factors. The authors also got
written consent for participation
from every study subjects, and
CASP 12
institutional ethical approval for the
human subjects study being obtained
at the University of Utah besides the
Universities in Fujian, Beijing,
Taiwan, Shanghai, Henan, and
Sichuan. The criteria for inclusion
for patient included age between 18
and 80-years-old and incident
patients with neck and head cancer
(tumors being assigned 1 of the five
categories.
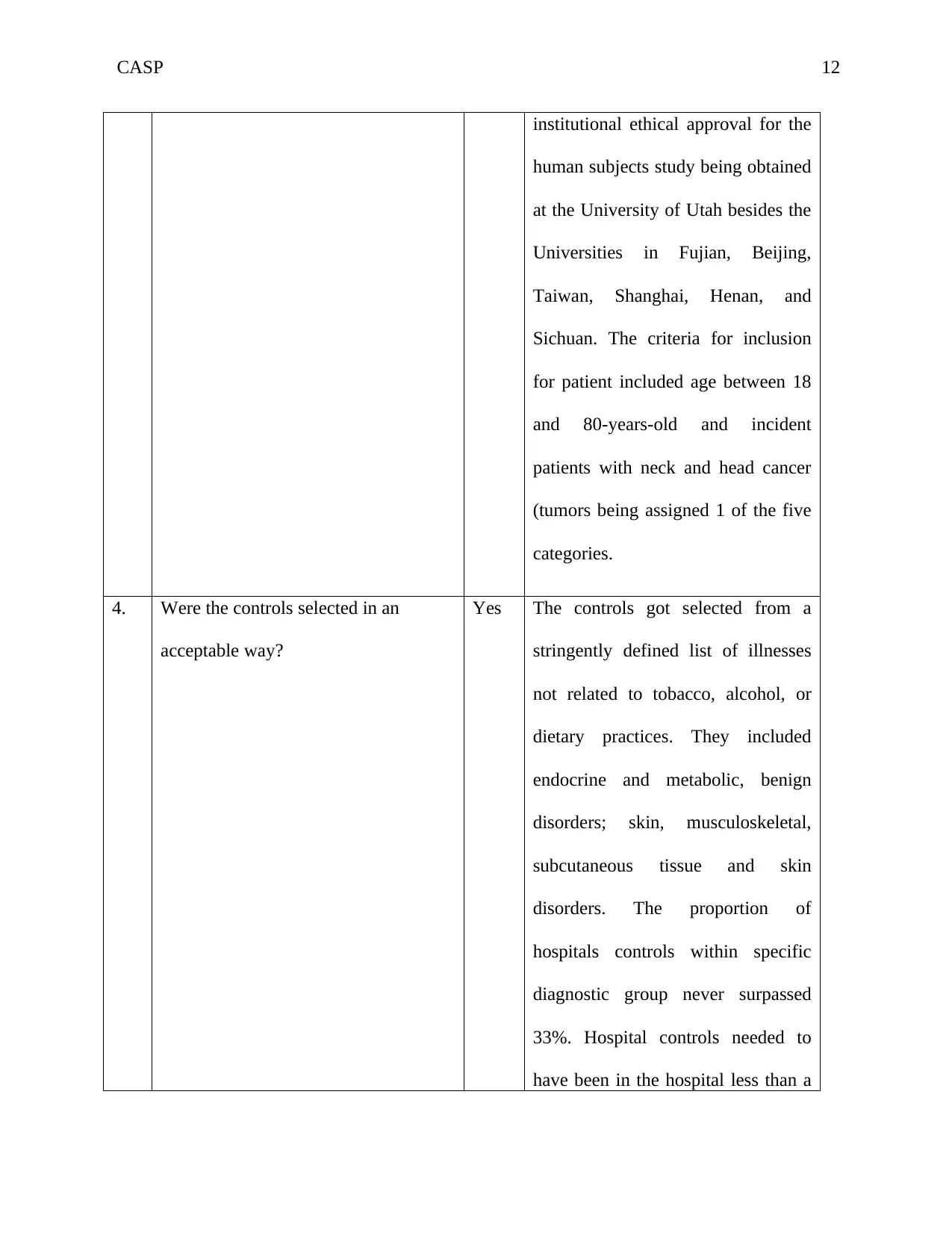
4. Were the controls selected in an
acceptable way?
Yes The controls got selected from a
stringently defined list of illnesses
not related to tobacco, alcohol, or
dietary practices. They included
endocrine and metabolic, benign
disorders; skin, musculoskeletal,
subcutaneous tissue and skin
disorders. The proportion of
hospitals controls within specific
diagnostic group never surpassed
33%. Hospital controls needed to
have been in the hospital less than a
institutional ethical approval for the
human subjects study being obtained
at the University of Utah besides the
Universities in Fujian, Beijing,
Taiwan, Shanghai, Henan, and
Sichuan. The criteria for inclusion
for patient included age between 18
and 80-years-old and incident
patients with neck and head cancer
(tumors being assigned 1 of the five
categories.
4. Were the controls selected in an
acceptable way?
Yes The controls got selected from a
stringently defined list of illnesses
not related to tobacco, alcohol, or
dietary practices. They included
endocrine and metabolic, benign
disorders; skin, musculoskeletal,
subcutaneous tissue and skin
disorders. The proportion of
hospitals controls within specific
diagnostic group never surpassed
33%. Hospital controls needed to
have been in the hospital less than a
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 18
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.