Cervical Cancer Awareness: Prevention Strategies and Nursing Role
VerifiedAdded on 2023/06/11
|1
|1289
|97
Presentation
AI Summary
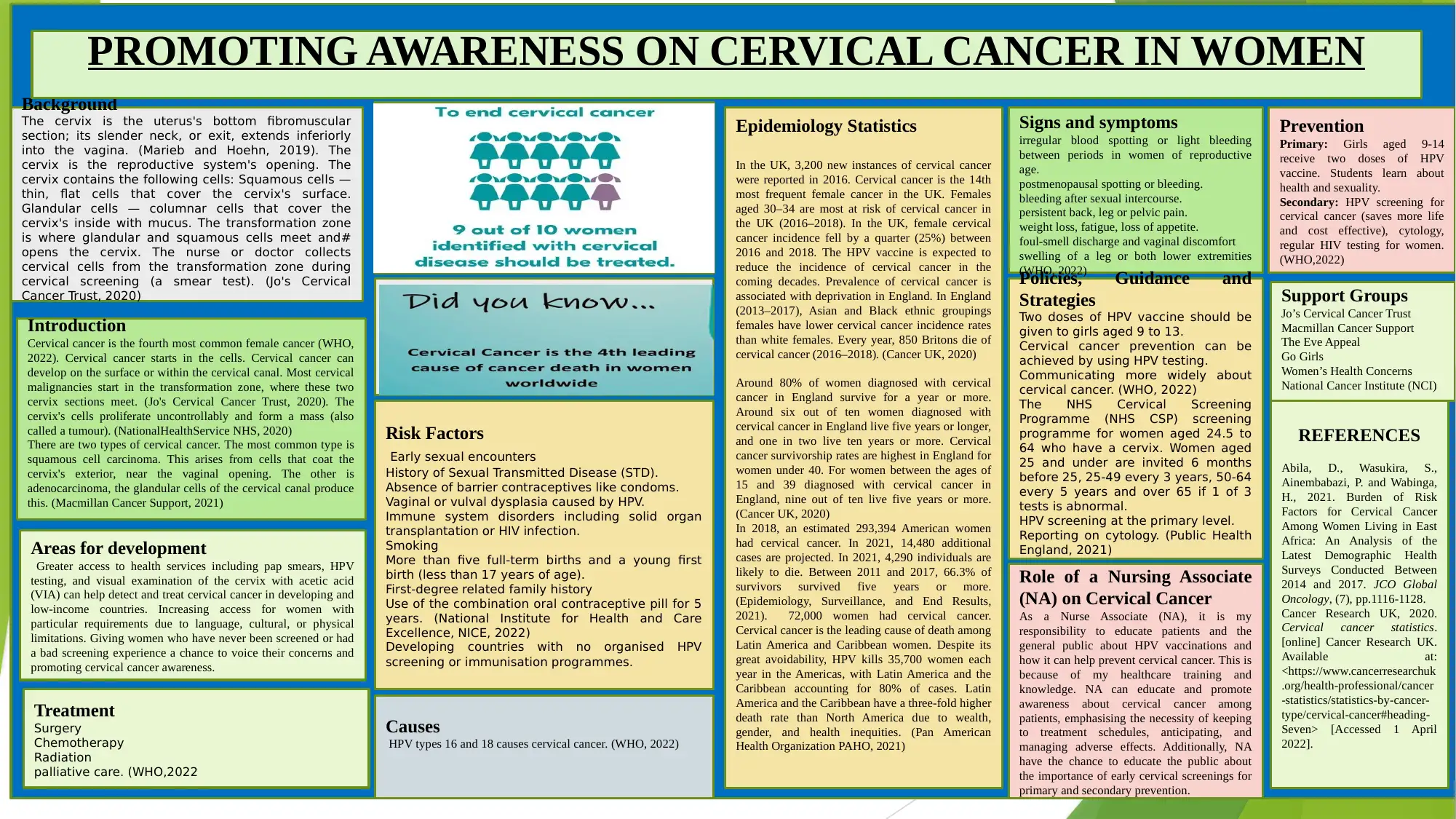
This presentation provides an overview of cervical cancer, including its background, epidemiology, risk factors, causes, signs and symptoms, and available treatments. It highlights the role of a Nursing Associate (NA) in promoting awareness about HPV vaccinations, the importance of cervical screenings, and adherence to treatment schedules. The presentation emphasizes primary prevention strategies such as HPV vaccination for girls aged 9-14 and secondary prevention methods like HPV screening and regular HIV testing for women. Additionally, it lists support groups available for individuals affected by cervical cancer. The presentation also includes relevant policies, guidance, and strategies from organizations like the WHO and NHS, along with a comprehensive reference list.
Background
The cervix is the uterus's bottom fibromuscular
section; its slender neck, or exit, extends inferiorly
into the vagina. (Marieb and Hoehn, 2019). The
cervix is the reproductive system's opening. The
cervix contains the following cells: Squamous cells —
thin, flat cells that cover the cervix's surface.
Glandular cells — columnar cells that cover the
cervix's inside with mucus. The transformation zone
is where glandular and squamous cells meet and#
opens the cervix. The nurse or doctor collects
cervical cells from the transformation zone during
cervical screening (a smear test). (Jo's Cervical
Cancer Trust, 2020)
PROMOTING AWARENESS ON CERVICAL CANCER IN WOMEN
Introduction
Cervical cancer is the fourth most common female cancer (WHO,
2022). Cervical cancer starts in the cells. Cervical cancer can
develop on the surface or within the cervical canal. Most cervical
malignancies start in the transformation zone, where these two
cervix sections meet. (Jo's Cervical Cancer Trust, 2020). The
cervix's cells proliferate uncontrollably and form a mass (also
called a tumour). (NationalHealthService NHS, 2020)
There are two types of cervical cancer. The most common type is
squamous cell carcinoma. This arises from cells that coat the
cervix's exterior, near the vaginal opening. The other is
adenocarcinoma, the glandular cells of the cervical canal produce
this. (Macmillan Cancer Support, 2021)
Epidemiology Statistics
In the UK, 3,200 new instances of cervical cancer
were reported in 2016. Cervical cancer is the 14th
most frequent female cancer in the UK. Females
aged 30–34 are most at risk of cervical cancer in
the UK (2016–2018). In the UK, female cervical
cancer incidence fell by a quarter (25%) between
2016 and 2018. The HPV vaccine is expected to
reduce the incidence of cervical cancer in the
coming decades. Prevalence of cervical cancer is
associated with deprivation in England. In England
(2013–2017), Asian and Black ethnic groupings
females have lower cervical cancer incidence rates
than white females. Every year, 850 Britons die of
cervical cancer (2016–2018). (Cancer UK, 2020)
Around 80% of women diagnosed with cervical
cancer in England survive for a year or more.
Around six out of ten women diagnosed with
cervical cancer in England live five years or longer,
and one in two live ten years or more. Cervical
cancer survivorship rates are highest in England for
women under 40. For women between the ages of
15 and 39 diagnosed with cervical cancer in
England, nine out of ten live five years or more.
(Cancer UK, 2020)
In 2018, an estimated 293,394 American women
had cervical cancer. In 2021, 14,480 additional
cases are projected. In 2021, 4,290 individuals are
likely to die. Between 2011 and 2017, 66.3% of
survivors survived five years or more.
(Epidemiology, Surveillance, and End Results,
2021). 72,000 women had cervical cancer.
Cervical cancer is the leading cause of death among
Latin America and Caribbean women. Despite its
great avoidability, HPV kills 35,700 women each
year in the Americas, with Latin America and the
Caribbean accounting for 80% of cases. Latin
America and the Caribbean have a three-fold higher
death rate than North America due to wealth,
gender, and health inequities. (Pan American
Health Organization PAHO, 2021)
Signs and symptoms
irregular blood spotting or light bleeding
between periods in women of reproductive
age.
postmenopausal spotting or bleeding.
bleeding after sexual intercourse.
persistent back, leg or pelvic pain.
weight loss, fatigue, loss of appetite.
foul-smell discharge and vaginal discomfort
swelling of a leg or both lower extremities
(WHO, 2022)
.Policies, Guidance and
Strategies
Two doses of HPV vaccine should be
given to girls aged 9 to 13.
Cervical cancer prevention can be
achieved by using HPV testing.
Communicating more widely about
cervical cancer. (WHO, 2022)
The NHS Cervical Screening
Programme (NHS CSP) screening
programme for women aged 24.5 to
64 who have a cervix. Women aged
25 and under are invited 6 months
before 25, 25-49 every 3 years, 50-64
every 5 years and over 65 if 1 of 3
tests is abnormal.
HPV screening at the primary level.
Reporting on cytology. (Public Health
England, 2021)
Risk Factors
Early sexual encounters
History of Sexual Transmitted Disease (STD).
Absence of barrier contraceptives like condoms.
Vaginal or vulval dysplasia caused by HPV.
Immune system disorders including solid organ
transplantation or HIV infection.
Smoking
More than five full-term births and a young first
birth (less than 17 years of age).
First-degree related family history
Use of the combination oral contraceptive pill for 5
years. (National Institute for Health and Care
Excellence, NICE, 2022)
Developing countries with no organised HPV
screening or immunisation programmes.
Causes
HPV types 16 and 18 causes cervical cancer. (WHO, 2022)
Prevention
Primary: Girls aged 9-14
receive two doses of HPV
vaccine. Students learn about
health and sexuality.
Secondary: HPV screening for
cervical cancer (saves more life
and cost effective), cytology,
regular HIV testing for women.
(WHO,2022)
Support Groups
Jo’s Cervical Cancer Trust
Macmillan Cancer Support
The Eve Appeal
Go Girls
Women’s Health Concerns
National Cancer Institute (NCI)
REFERENCES
Abila, D., Wasukira, S.,
Ainembabazi, P. and Wabinga,
H., 2021. Burden of Risk
Factors for Cervical Cancer
Among Women Living in East
Africa: An Analysis of the
Latest Demographic Health
Surveys Conducted Between
2014 and 2017. JCO Global
Oncology, (7), pp.1116-1128.
Cancer Research UK, 2020.
Cervical cancer statistics.
[online] Cancer Research UK.
Available at:
<https://www.cancerresearchuk
.org/health-professional/cancer
-statistics/statistics-by-cancer-
type/cervical-cancer#heading-
Seven> [Accessed 1 April
2022].
Areas for development
Greater access to health services including pap smears, HPV
testing, and visual examination of the cervix with acetic acid
(VIA) can help detect and treat cervical cancer in developing and
low-income countries. Increasing access for women with
particular requirements due to language, cultural, or physical
limitations. Giving women who have never been screened or had
a bad screening experience a chance to voice their concerns and
promoting cervical cancer awareness.
Treatment
Surgery
Chemotherapy
Radiation
palliative care. (WHO,2022
Role of a Nursing Associate
(NA) on Cervical Cancer
As a Nurse Associate (NA), it is my
responsibility to educate patients and the
general public about HPV vaccinations and
how it can help prevent cervical cancer. This is
because of my healthcare training and
knowledge. NA can educate and promote
awareness about cervical cancer among
patients, emphasising the necessity of keeping
to treatment schedules, anticipating, and
managing adverse effects. Additionally, NA
have the chance to educate the public about
the importance of early cervical screenings for
primary and secondary prevention.
The cervix is the uterus's bottom fibromuscular
section; its slender neck, or exit, extends inferiorly
into the vagina. (Marieb and Hoehn, 2019). The
cervix is the reproductive system's opening. The
cervix contains the following cells: Squamous cells —
thin, flat cells that cover the cervix's surface.
Glandular cells — columnar cells that cover the
cervix's inside with mucus. The transformation zone
is where glandular and squamous cells meet and#
opens the cervix. The nurse or doctor collects
cervical cells from the transformation zone during
cervical screening (a smear test). (Jo's Cervical
Cancer Trust, 2020)
PROMOTING AWARENESS ON CERVICAL CANCER IN WOMEN
Introduction
Cervical cancer is the fourth most common female cancer (WHO,
2022). Cervical cancer starts in the cells. Cervical cancer can
develop on the surface or within the cervical canal. Most cervical
malignancies start in the transformation zone, where these two
cervix sections meet. (Jo's Cervical Cancer Trust, 2020). The
cervix's cells proliferate uncontrollably and form a mass (also
called a tumour). (NationalHealthService NHS, 2020)
There are two types of cervical cancer. The most common type is
squamous cell carcinoma. This arises from cells that coat the
cervix's exterior, near the vaginal opening. The other is
adenocarcinoma, the glandular cells of the cervical canal produce
this. (Macmillan Cancer Support, 2021)
Epidemiology Statistics
In the UK, 3,200 new instances of cervical cancer
were reported in 2016. Cervical cancer is the 14th
most frequent female cancer in the UK. Females
aged 30–34 are most at risk of cervical cancer in
the UK (2016–2018). In the UK, female cervical
cancer incidence fell by a quarter (25%) between
2016 and 2018. The HPV vaccine is expected to
reduce the incidence of cervical cancer in the
coming decades. Prevalence of cervical cancer is
associated with deprivation in England. In England
(2013–2017), Asian and Black ethnic groupings
females have lower cervical cancer incidence rates
than white females. Every year, 850 Britons die of
cervical cancer (2016–2018). (Cancer UK, 2020)
Around 80% of women diagnosed with cervical
cancer in England survive for a year or more.
Around six out of ten women diagnosed with
cervical cancer in England live five years or longer,
and one in two live ten years or more. Cervical
cancer survivorship rates are highest in England for
women under 40. For women between the ages of
15 and 39 diagnosed with cervical cancer in
England, nine out of ten live five years or more.
(Cancer UK, 2020)
In 2018, an estimated 293,394 American women
had cervical cancer. In 2021, 14,480 additional
cases are projected. In 2021, 4,290 individuals are
likely to die. Between 2011 and 2017, 66.3% of
survivors survived five years or more.
(Epidemiology, Surveillance, and End Results,
2021). 72,000 women had cervical cancer.
Cervical cancer is the leading cause of death among
Latin America and Caribbean women. Despite its
great avoidability, HPV kills 35,700 women each
year in the Americas, with Latin America and the
Caribbean accounting for 80% of cases. Latin
America and the Caribbean have a three-fold higher
death rate than North America due to wealth,
gender, and health inequities. (Pan American
Health Organization PAHO, 2021)
Signs and symptoms
irregular blood spotting or light bleeding
between periods in women of reproductive
age.
postmenopausal spotting or bleeding.
bleeding after sexual intercourse.
persistent back, leg or pelvic pain.
weight loss, fatigue, loss of appetite.
foul-smell discharge and vaginal discomfort
swelling of a leg or both lower extremities
(WHO, 2022)
.Policies, Guidance and
Strategies
Two doses of HPV vaccine should be
given to girls aged 9 to 13.
Cervical cancer prevention can be
achieved by using HPV testing.
Communicating more widely about
cervical cancer. (WHO, 2022)
The NHS Cervical Screening
Programme (NHS CSP) screening
programme for women aged 24.5 to
64 who have a cervix. Women aged
25 and under are invited 6 months
before 25, 25-49 every 3 years, 50-64
every 5 years and over 65 if 1 of 3
tests is abnormal.
HPV screening at the primary level.
Reporting on cytology. (Public Health
England, 2021)
Risk Factors
Early sexual encounters
History of Sexual Transmitted Disease (STD).
Absence of barrier contraceptives like condoms.
Vaginal or vulval dysplasia caused by HPV.
Immune system disorders including solid organ
transplantation or HIV infection.
Smoking
More than five full-term births and a young first
birth (less than 17 years of age).
First-degree related family history
Use of the combination oral contraceptive pill for 5
years. (National Institute for Health and Care
Excellence, NICE, 2022)
Developing countries with no organised HPV
screening or immunisation programmes.
Causes
HPV types 16 and 18 causes cervical cancer. (WHO, 2022)
Prevention
Primary: Girls aged 9-14
receive two doses of HPV
vaccine. Students learn about
health and sexuality.
Secondary: HPV screening for
cervical cancer (saves more life
and cost effective), cytology,
regular HIV testing for women.
(WHO,2022)
Support Groups
Jo’s Cervical Cancer Trust
Macmillan Cancer Support
The Eve Appeal
Go Girls
Women’s Health Concerns
National Cancer Institute (NCI)
REFERENCES
Abila, D., Wasukira, S.,
Ainembabazi, P. and Wabinga,
H., 2021. Burden of Risk
Factors for Cervical Cancer
Among Women Living in East
Africa: An Analysis of the
Latest Demographic Health
Surveys Conducted Between
2014 and 2017. JCO Global
Oncology, (7), pp.1116-1128.
Cancer Research UK, 2020.
Cervical cancer statistics.
[online] Cancer Research UK.
Available at:
<https://www.cancerresearchuk
.org/health-professional/cancer
-statistics/statistics-by-cancer-
type/cervical-cancer#heading-
Seven> [Accessed 1 April
2022].
Areas for development
Greater access to health services including pap smears, HPV
testing, and visual examination of the cervix with acetic acid
(VIA) can help detect and treat cervical cancer in developing and
low-income countries. Increasing access for women with
particular requirements due to language, cultural, or physical
limitations. Giving women who have never been screened or had
a bad screening experience a chance to voice their concerns and
promoting cervical cancer awareness.
Treatment
Surgery
Chemotherapy
Radiation
palliative care. (WHO,2022
Role of a Nursing Associate
(NA) on Cervical Cancer
As a Nurse Associate (NA), it is my
responsibility to educate patients and the
general public about HPV vaccinations and
how it can help prevent cervical cancer. This is
because of my healthcare training and
knowledge. NA can educate and promote
awareness about cervical cancer among
patients, emphasising the necessity of keeping
to treatment schedules, anticipating, and
managing adverse effects. Additionally, NA
have the chance to educate the public about
the importance of early cervical screenings for
primary and secondary prevention.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



