Aboriginal And Torres Strait Islanders
Added on 2022-09-12
1 Pages1896 Words11 Views
References
Childhood obesity in aboriginal and Torres strait community
in central Australia
Eat fit,
Stay fit!CHILDHOOD OBESITY
CHILDHOOD OBESITYName of the student: Name of the student:
.
Childhood obesity is a complicated and a major health concern in
Australia, particularly in the remote areas of Central Australia such as
Aboriginal and Torres Strait islanders. It is observed in children above
the average weight within their height and age and is found 1 in 4
children of Australia. The factors causing overweight and obesity in
children are similar to these observed in adults which include genetic
composition and lifestyle factors. Other factors include cultural
background and environmental factors (Sanders et al., 2015).
Childhood obesity contributes to 16% of the health gap between the
Aboriginal and non-Aboriginal populations.
Impact on individual
• Emotional- Obesity has a direct impact on the psychological state of the child due to the overweight.
• Social- The social stigma surrounding overweight people, particularly in the younger generation
affects the social inclusion of the child (Sahoo et al., 2015).
• Academic performance- An unhealthy social and emotional state of mind is directly associated with
poor academic performance (Black, Johnston & Peeters, 2015).
• Physical health- a number of problems are associated with being overweight such as physical activity
and sports (Laws et al., 2014).
• Self-esteem- A poor academic performance along with low physical, social and emotional conditions
lead to reduced self confidence of the children (Galván et al., 2014).
• Medical impact- Childhood obesity not only affects the psychology and mental health of the person
but also causes clinical conditions that can stay over the life span of the child. These include
vulnerability to metabolic complications, cardiovascular diseases and type 2 diabetes.
Impact on community and
population
Childhood obesity has a direct impact on the
individual directly which in turn affects the
community, as a whole. Obesity in childhood
develops adults with long-term disabilities which
impact the health quality of the entire community
(McHugh, 2016). The people of Aboriginal and Torres
Strait community in rural central Australia do not
have adequate access to health services. The
increased incidents of obesity among children of
central Australia Aboriginal populations also widen
the health gap between them and the non-
indegenous and affluent populations.
Key areas of changes
• Urbanisation- Colonisation has led to losing traditional living increasing westernization among Aboriginal and Torres Strait
islanders of central Australia, especially among the children. This has changed their lifestyle and affected the health of
children (Valeggia & Snodgrass, 2015).
• Sub-standard housing- Due to poor economic status of majority of this community’s population, their housings are also
below standard and depict high risk of developing chronic conditions such as childhood obesity as children are more
susceptible to diseases than the adults.
• Food insecurity- The forceful removal of the Aboriginal people from their traditional lands led to the inability of these
people to access and maintain traditional food habits and adopt western habits of packaged and junk food, which is
exceptionally high in the children (Dyer et al., 2017).
• Economic factors- The people of this community living in the remote areas of central Australia face increased financial
burden and are unable to maintain high and quality standards of living which affect the health of the people, including
their children and in accessing health services on time to reduce comorbidities.
• Inadequate access to healthcare services- This indegenous community resides in the remote central areas where proper
health care facilities are inadequate and often below standard.
• Activity levels- These children demonstrate reduced physical activity compared to other children and low levels of
involvement in sports. The shift of the traditional lifestyle of these people to the westernized culture has reduced their
physical activities, making them prone to obesity.
• Socio-cultural factors. The population of Aboriginal and Torres Strait islanders in central Australia encourage unhealthy
habits if food and risk factors developing the risk of obesity in children.
Plan of Action
Ash, T., Agaronov, A., Aftosmes-Tobio, A., & Davison, K. K. (2017). Family-based childhood obesity prevention interventions: a systematic review and quantitative content analysis. International Journal of Behavioral Nutrition and Physical Activity, 14(1), 113.
Black, N., Johnston, D. W., & Peeters, A. (2015). Childhood obesity and cognitive achievement.
Health economics,
24(9), 1082-1100.
Browne, J., Adams, K., Atkinson, P., Gleeson, D., & Hayes, R. (2018). Food and nutrition programs for Aboriginal and Torres Strait Islander Australians: an overview of systematic reviews.
Australian Health Review,
42(6), 689-697.
Burrows, T., Hutchesson, M., Chai, L. K., Rollo, M., Skinner, G., & Collins, C. (2015). Nutrition interventions for prevention and management of childhood obesity: what do parents want from an eHealth program?. Nutrients, 7(12), 10469-10479.
Dyer, S. M., Gomersall, J. S., Smithers, L. G., Davy, C., Coleman, D. T., & Street, J. M. (2017). Prevalence and characteristics of overweight and obesity in indigenous Australian children: a systematic review. Critical reviews in food science and nutrition, 57(7), 1365-1376.
Galván, M., Uauy, R., López-Rodríguez, G., & Kain, J. (2014). Association between childhood obesity, cognitive development, physical fitness and social-emotional wellbeing in a transitional economy. Annals of human biology, 41(2), 101-106.
Hardy, L. L., O'Hara, B. J., Hector, D., Engelen, L., & Eades, S. J. (2014). Temporal trends in weight and current weight‐related behaviour of Australian Aboriginal school‐aged children. Medical Journal of Australia, 200(11), 667-671.
Ho, M., Garnett, S. P., & Baur, L. A. (2014). Childhood obesity and insulin resistance: how should it be managed?. Current treatment options in cardiovascular medicine, 16(12), 351.
Lakshman, R., Elks, C. E., & Ong, K. K. (2012). Childhood obesity. Circulation, 126(14), 1770-1779.
Laws, R., Campbell, K. J., Van Der Pligt, P., Russell, G., Ball, K., Lynch, J., ... & Denney-Wilson, E. (2014). The impact of interventions to prevent obesity or improve obesity related behaviours in children (0–5 years) from socioeconomically disadvantaged and/or indigenous families: a systematic review. BMC public health, 14(1), 779.
McHugh, B. (2016). The childhood obesity epidemic. Journal of the Australian Traditional-Medicine Society, 22(2), 94-99.
Sahoo, K., Sahoo, B., Choudhury, A. K., Sofi, N. Y., Kumar, R., & Bhadoria, A. S. (2015). Childhood obesity: causes and consequences.
Journal of family medicine and primary care,
4(2), 187.
Sanders, R. H., Han, A., Baker, J. S., & Cobley, S. (2015). Childhood obesity and its physical and psychological co-morbidities: a systematic review of Australian children and adolescents.
European journal of pediatrics,
174(6), 715-746.
Sherriff, S. L., Baur, L., Lambert, M. G., Dickson, M., Eades, S. J., & Muthayya, S. (2019). Aboriginal childhood overweight and obesity: the need for Aboriginal designed and led initiatives.
Public Health Research & Practice,
29(4).
Several programs have been implemented by the Government to regulate the factors contributing to obesity
among the children. Some of these policies include Go4fun, and Munch and Move. However, these programs
have demonstrated low adherence in completion of the program by Aboriginal children.
• An intervention that addresses their cultural backgrounds and aspects can be more useful (Sherriff et al.,
2019)
• A plan in collaboration with the specific needs and opinions of the end-users, the parents and children to
improve obesity trends in children may result in better outcomes (Ash et al., 2017).
• A program targeting changes in the habits of families and home-based environments enhance in instilling
healthy habits of nutrition and physical exercises.
A suitable promotion program aiming towards adopting culture practices and working with the parents of the community to address
the key areas of change such as nutritional intake and physical exercises can decrease the prevalence of childhood obesity among
the Aboriginal children (Burrows et al., 2015; Ho, Garnett & Baur, 2014). The key interventions of the program include:
• Address the parents or guardians of the children to bring about the change in lifestyle through parent-session groups.
• Parent-session groups act as forums where the parents can discuss and exchange ideas to inculcate changes in the nutrition and
physical activities of their children through family-focused and culturally acceptable reforms.
• While parents serve as agents of modifications, the children can participate and get involved in activity sessions such as cycling,
skating, swimming and outdoor sports ((Browne et al., 2018).).
• These activities can be incorporated into the school curriculum to engage the children in physical exercise.it will also help them
develop interest in these fields and pursue it further (Hardy et al., 2014).
• The government can also play a role in reforming the policies such that the price of packaged and junk food can be raised to
lower their intake among children and youth who will not be able to afford them regularly.
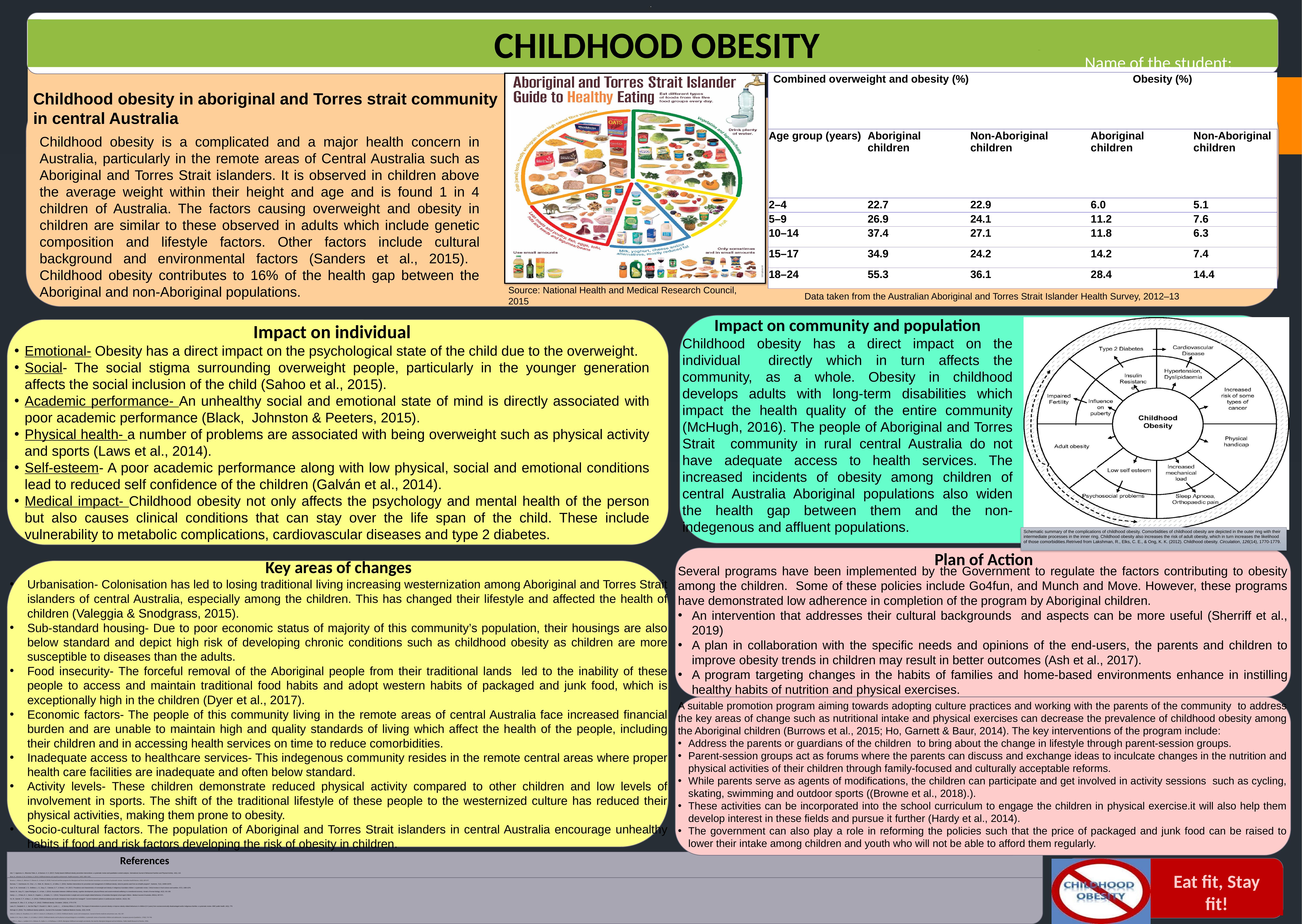
Combined overweight and obesity (%) Obesity (%)
Age group (years) Aboriginal
children
Non-Aboriginal
children
Aboriginal
children
Non-Aboriginal
children
2–4 22.7 22.9 6.0 5.1
5–9 26.9 24.1 11.2 7.6
10–14 37.4 27.1 11.8 6.3
15–17 34.9 24.2 14.2 7.4
18–24 55.3 36.1 28.4 14.4Schematic summary of the complications of childhood obesity. Comorbidities of childhood obesity are depicted in the outer ring with their
intermediate processes in the inner ring. Childhood obesity also increases the risk of adult obesity, which in turn increases the likelihood
of those comorbidities.Retrived from Lakshman, R., Elks, C. E., & Ong, K. K. (2012). Childhood obesity. Circulation, 126(14), 1770-1779.
Schematic summary of the complications of childhood obesity. Comorbidities of childhood obesity are depicted in the outer ring with their
intermediate processes in the inner ring. Childhood obesity also increases the risk of adult obesity, which in turn increases the likelihood
of those comorbidities.Retrived from Lakshman, R., Elks, C. E., & Ong, K. K. (2012). Childhood obesity. Circulation, 126(14), 1770-1779.
Source: National Health and Medical Research Council,
2015 Data taken from the Australian Aboriginal and Torres Strait Islander Health Survey, 2012–13
Childhood obesity in aboriginal and Torres strait community
in central Australia
Eat fit,
Stay fit!CHILDHOOD OBESITY
CHILDHOOD OBESITYName of the student: Name of the student:
.
Childhood obesity is a complicated and a major health concern in
Australia, particularly in the remote areas of Central Australia such as
Aboriginal and Torres Strait islanders. It is observed in children above
the average weight within their height and age and is found 1 in 4
children of Australia. The factors causing overweight and obesity in
children are similar to these observed in adults which include genetic
composition and lifestyle factors. Other factors include cultural
background and environmental factors (Sanders et al., 2015).
Childhood obesity contributes to 16% of the health gap between the
Aboriginal and non-Aboriginal populations.
Impact on individual
• Emotional- Obesity has a direct impact on the psychological state of the child due to the overweight.
• Social- The social stigma surrounding overweight people, particularly in the younger generation
affects the social inclusion of the child (Sahoo et al., 2015).
• Academic performance- An unhealthy social and emotional state of mind is directly associated with
poor academic performance (Black, Johnston & Peeters, 2015).
• Physical health- a number of problems are associated with being overweight such as physical activity
and sports (Laws et al., 2014).
• Self-esteem- A poor academic performance along with low physical, social and emotional conditions
lead to reduced self confidence of the children (Galván et al., 2014).
• Medical impact- Childhood obesity not only affects the psychology and mental health of the person
but also causes clinical conditions that can stay over the life span of the child. These include
vulnerability to metabolic complications, cardiovascular diseases and type 2 diabetes.
Impact on community and
population
Childhood obesity has a direct impact on the
individual directly which in turn affects the
community, as a whole. Obesity in childhood
develops adults with long-term disabilities which
impact the health quality of the entire community
(McHugh, 2016). The people of Aboriginal and Torres
Strait community in rural central Australia do not
have adequate access to health services. The
increased incidents of obesity among children of
central Australia Aboriginal populations also widen
the health gap between them and the non-
indegenous and affluent populations.
Key areas of changes
• Urbanisation- Colonisation has led to losing traditional living increasing westernization among Aboriginal and Torres Strait
islanders of central Australia, especially among the children. This has changed their lifestyle and affected the health of
children (Valeggia & Snodgrass, 2015).
• Sub-standard housing- Due to poor economic status of majority of this community’s population, their housings are also
below standard and depict high risk of developing chronic conditions such as childhood obesity as children are more
susceptible to diseases than the adults.
• Food insecurity- The forceful removal of the Aboriginal people from their traditional lands led to the inability of these
people to access and maintain traditional food habits and adopt western habits of packaged and junk food, which is
exceptionally high in the children (Dyer et al., 2017).
• Economic factors- The people of this community living in the remote areas of central Australia face increased financial
burden and are unable to maintain high and quality standards of living which affect the health of the people, including
their children and in accessing health services on time to reduce comorbidities.
• Inadequate access to healthcare services- This indegenous community resides in the remote central areas where proper
health care facilities are inadequate and often below standard.
• Activity levels- These children demonstrate reduced physical activity compared to other children and low levels of
involvement in sports. The shift of the traditional lifestyle of these people to the westernized culture has reduced their
physical activities, making them prone to obesity.
• Socio-cultural factors. The population of Aboriginal and Torres Strait islanders in central Australia encourage unhealthy
habits if food and risk factors developing the risk of obesity in children.
Plan of Action
Ash, T., Agaronov, A., Aftosmes-Tobio, A., & Davison, K. K. (2017). Family-based childhood obesity prevention interventions: a systematic review and quantitative content analysis. International Journal of Behavioral Nutrition and Physical Activity, 14(1), 113.
Black, N., Johnston, D. W., & Peeters, A. (2015). Childhood obesity and cognitive achievement.
Health economics,
24(9), 1082-1100.
Browne, J., Adams, K., Atkinson, P., Gleeson, D., & Hayes, R. (2018). Food and nutrition programs for Aboriginal and Torres Strait Islander Australians: an overview of systematic reviews.
Australian Health Review,
42(6), 689-697.
Burrows, T., Hutchesson, M., Chai, L. K., Rollo, M., Skinner, G., & Collins, C. (2015). Nutrition interventions for prevention and management of childhood obesity: what do parents want from an eHealth program?. Nutrients, 7(12), 10469-10479.
Dyer, S. M., Gomersall, J. S., Smithers, L. G., Davy, C., Coleman, D. T., & Street, J. M. (2017). Prevalence and characteristics of overweight and obesity in indigenous Australian children: a systematic review. Critical reviews in food science and nutrition, 57(7), 1365-1376.
Galván, M., Uauy, R., López-Rodríguez, G., & Kain, J. (2014). Association between childhood obesity, cognitive development, physical fitness and social-emotional wellbeing in a transitional economy. Annals of human biology, 41(2), 101-106.
Hardy, L. L., O'Hara, B. J., Hector, D., Engelen, L., & Eades, S. J. (2014). Temporal trends in weight and current weight‐related behaviour of Australian Aboriginal school‐aged children. Medical Journal of Australia, 200(11), 667-671.
Ho, M., Garnett, S. P., & Baur, L. A. (2014). Childhood obesity and insulin resistance: how should it be managed?. Current treatment options in cardiovascular medicine, 16(12), 351.
Lakshman, R., Elks, C. E., & Ong, K. K. (2012). Childhood obesity. Circulation, 126(14), 1770-1779.
Laws, R., Campbell, K. J., Van Der Pligt, P., Russell, G., Ball, K., Lynch, J., ... & Denney-Wilson, E. (2014). The impact of interventions to prevent obesity or improve obesity related behaviours in children (0–5 years) from socioeconomically disadvantaged and/or indigenous families: a systematic review. BMC public health, 14(1), 779.
McHugh, B. (2016). The childhood obesity epidemic. Journal of the Australian Traditional-Medicine Society, 22(2), 94-99.
Sahoo, K., Sahoo, B., Choudhury, A. K., Sofi, N. Y., Kumar, R., & Bhadoria, A. S. (2015). Childhood obesity: causes and consequences.
Journal of family medicine and primary care,
4(2), 187.
Sanders, R. H., Han, A., Baker, J. S., & Cobley, S. (2015). Childhood obesity and its physical and psychological co-morbidities: a systematic review of Australian children and adolescents.
European journal of pediatrics,
174(6), 715-746.
Sherriff, S. L., Baur, L., Lambert, M. G., Dickson, M., Eades, S. J., & Muthayya, S. (2019). Aboriginal childhood overweight and obesity: the need for Aboriginal designed and led initiatives.
Public Health Research & Practice,
29(4).
Several programs have been implemented by the Government to regulate the factors contributing to obesity
among the children. Some of these policies include Go4fun, and Munch and Move. However, these programs
have demonstrated low adherence in completion of the program by Aboriginal children.
• An intervention that addresses their cultural backgrounds and aspects can be more useful (Sherriff et al.,
2019)
• A plan in collaboration with the specific needs and opinions of the end-users, the parents and children to
improve obesity trends in children may result in better outcomes (Ash et al., 2017).
• A program targeting changes in the habits of families and home-based environments enhance in instilling
healthy habits of nutrition and physical exercises.
A suitable promotion program aiming towards adopting culture practices and working with the parents of the community to address
the key areas of change such as nutritional intake and physical exercises can decrease the prevalence of childhood obesity among
the Aboriginal children (Burrows et al., 2015; Ho, Garnett & Baur, 2014). The key interventions of the program include:
• Address the parents or guardians of the children to bring about the change in lifestyle through parent-session groups.
• Parent-session groups act as forums where the parents can discuss and exchange ideas to inculcate changes in the nutrition and
physical activities of their children through family-focused and culturally acceptable reforms.
• While parents serve as agents of modifications, the children can participate and get involved in activity sessions such as cycling,
skating, swimming and outdoor sports ((Browne et al., 2018).).
• These activities can be incorporated into the school curriculum to engage the children in physical exercise.it will also help them
develop interest in these fields and pursue it further (Hardy et al., 2014).
• The government can also play a role in reforming the policies such that the price of packaged and junk food can be raised to
lower their intake among children and youth who will not be able to afford them regularly.
Combined overweight and obesity (%) Obesity (%)
Age group (years) Aboriginal
children
Non-Aboriginal
children
Aboriginal
children
Non-Aboriginal
children
2–4 22.7 22.9 6.0 5.1
5–9 26.9 24.1 11.2 7.6
10–14 37.4 27.1 11.8 6.3
15–17 34.9 24.2 14.2 7.4
18–24 55.3 36.1 28.4 14.4Schematic summary of the complications of childhood obesity. Comorbidities of childhood obesity are depicted in the outer ring with their
intermediate processes in the inner ring. Childhood obesity also increases the risk of adult obesity, which in turn increases the likelihood
of those comorbidities.Retrived from Lakshman, R., Elks, C. E., & Ong, K. K. (2012). Childhood obesity. Circulation, 126(14), 1770-1779.
Schematic summary of the complications of childhood obesity. Comorbidities of childhood obesity are depicted in the outer ring with their
intermediate processes in the inner ring. Childhood obesity also increases the risk of adult obesity, which in turn increases the likelihood
of those comorbidities.Retrived from Lakshman, R., Elks, C. E., & Ong, K. K. (2012). Childhood obesity. Circulation, 126(14), 1770-1779.
Source: National Health and Medical Research Council,
2015 Data taken from the Australian Aboriginal and Torres Strait Islander Health Survey, 2012–13
End of preview
Want to access all the pages? Upload your documents or become a member.
Related Documents
Childhood obesity has become the most concerning issuelg...
|1
|2455
|16
Nutrition and Society of the Aboriginal Peoplelg...
|8
|1671
|312
Obesity and Community Childrenlg...
|1
|532
|42
Childhood Obesity: Inequity and Interventionslg...
|9
|2788
|48
Childhood Obesity: Impact, Key Areas of Change, and Action Planlg...
|1
|1428
|57
Childhood Obesity: Impact, Key Areas for Change, and Action Planlg...
|8
|1904
|92
