Barriers and Facilitators to Chronic Non-cancer Pain Management in Primary Care: A Qualitative Analysis of Primary Care Providers’ Experiences and Attitudes
Added on 2023-06-09
7 Pages9189 Words406 Views
Lincoln et al., J Palliative Care Med 2013, S3
DOI: 10.4172/2165-7386.S3-001
Research Article Open Access
J Palliative Care Med ISSN: 2165-7386 JPCM, an open access journal
Impact of Palliative
Care on Cancer Patients
Barriers and Facilitators to Chronic Non-cancer Pain Management
in Primary Care: A Qualitative Analysis of Primary Care Providers’
Experiences and Attitudes
L Elizabeth Lincoln1,2 *, Linda Pellico3 , Robert Kerns 2,4,5 and Daren Anderson6
1 Department of Medicine, Yale University School of Medicine, USA
2 VA Connecticut Health Care System, USA
3 Yale University School of Nursing, USA
4 Department of Psychiatry and Neurology, Yale University School of Medicine, USA
5 Department of Psychology, Yale University, USA
6 Community Health Center Inc., USA
Abstract
Objectives: Most patients with chronic non-cancer pain (CNCP) are cared for, by primary care providers (PCPs).
While some of the barriers faced by PCPs have been described, there is little information about PCPs’ experience with
factors that facilitate CNCP care.
Design: The study design was descriptive and qualitative. Data were analyzed using qualitative content analysis.
Krippendorff’s thematic clustering technique was used to identify the repetitive themes regarding PCPs’ experiences
related to CNCP management.
Subjects: Respondents were PCPs (n=45) in the VA Connecticut Healthcare System in two academically affiliated
institutions and six community based sites.
Results: Eleven themes were identified across systems, personal/professional, and interpersonal domains.
Barriers included inadequate training, organizational impediments, clinical quandaries and the frustrations that
accompany them, issues related to share care among PCPs and specialists, antagonistic aspects of provider-patient
interactions, skepticism, and time factors. Facilitators included the intellectual satisfaction of solving difficult diagnostic
and management problems, the ability to develop keener communication skills, the rewards of healing and building
therapeutic alliances with patients, universal protocols, and the availability of complementary and alternative medicine
resources and multidisciplinary care.
Conclusion: PCPs experience substantial difficulties in caring for patients with pain while acknowledging certain
positive aspects. There is a need for strategies that mitigate the barriers to pain management while bolstering the
positive aspects to improve care and provider satisfaction.
*Corresponding author: L Elizabeth Lincoln, Instructor, Department of
Medicine, Harvard Medical School, Massachusetts General Hospital 55 Fruit
St, Yawkey 4B, Suite 4700 Boston, MA 02114, USA, Tel: 203-752-6168; E-mail:
llincoln2@partners.org
Received February 25, 2013; Accepted March 08, 2013; Published March 11,
2013
Citation: Lincoln LE, Pellico L, Kerns R, Anderson D (2013) Barriers and Facilitators
to Chronic Non-cancer Pain Management in Primary Care: A Qualitative Analysis
of Primary Care Providers’ Experiences and Attitudes. J Palliative Care Med S3:
001. doi:10.4172/2165-7386.S3-001
Copyright: © 2013 Lincoln LE, et al. This is an open-access article distributed
under the terms of the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided the
original author and source are credited.
Keywords: Primary care; Chronic pain; Pain management; Primary
care providers; Ambulatory care
Introduction
Pain and effective pain care are among the most critical health
issues facing Americans. In 2011, the Institute of Medicine reported
that about one-third of all Americans experience persistent pain at an
annual cost of as much as $635 billion in medical treatment and lost
productivity. The report noted that military veterans are an especially
vulnerable group, with data documenting a particularly high prevalence
of pain and extraordinary rates of complexity associated with multiple
medical and mental health comorbidities [1].
Pain is the most common symptom reported by patients receiving
care in primary care, accounting for up to 40% of all visits to primary
care providers (PCPs) [2]. More than half of all patients who have
Chronic Non-Cancer Pain (CNCP) receive their care primarily from
PCPs [3]. Estimates suggest that as many as 50% of male veterans and
up to 75% of female veterans seen in Veteran’s Health Administration
(VHA) primary care settings report the presence of pain [4-6]. More
recent data suggest that the prevalence of CNCP, particularly painful
musculoskeletal disorders including chronic low back pain, is increasing
annually [7]. Cost effective strategies that improve the management of
CNCP in the primary care setting are needed to address the challenges
posed by this public health crisis.
The VHA has implemented a Stepped Care Model for Pain
Management (SCM-PM) as a national pain care strategy to meet the
needs of veterans [8]. The SCM-PM provides for effective assessment
and treatment of pain within primary care whenever possible, with
the capacity to escalate treatment options to include specialized care
and interdisciplinary approaches, if needed. Critical to the success of
the SCM-PM is the ability of PCPs and multidisciplinary primary care
teams to effectively access and manage most common pain conditions.
The SCM-PM is similar to that advocated by the American Academy
of Pain Medicine [9], and it was cited by the Institute of Medicine as a
potentially important model of care for persons with CNCP [1].
Unfortunately, the literature suggests that PCPs do not feel
adequately prepared to take on the role of frontline providers for
patients with CNCP. Although several studies have described PCPs’
attitudes and barriers to prescribing opioids for CNCP [10-14],
Journal of Palliative Care & Medicine
J
o
u
r
n
a
l
o
f
P
a
I
I
i
a
t
i
v
e
C
a
r
e
&
M
e
d
i
c
i
n
e
ISSN: 2165-7386
DOI: 10.4172/2165-7386.S3-001
Research Article Open Access
J Palliative Care Med ISSN: 2165-7386 JPCM, an open access journal
Impact of Palliative
Care on Cancer Patients
Barriers and Facilitators to Chronic Non-cancer Pain Management
in Primary Care: A Qualitative Analysis of Primary Care Providers’
Experiences and Attitudes
L Elizabeth Lincoln1,2 *, Linda Pellico3 , Robert Kerns 2,4,5 and Daren Anderson6
1 Department of Medicine, Yale University School of Medicine, USA
2 VA Connecticut Health Care System, USA
3 Yale University School of Nursing, USA
4 Department of Psychiatry and Neurology, Yale University School of Medicine, USA
5 Department of Psychology, Yale University, USA
6 Community Health Center Inc., USA
Abstract
Objectives: Most patients with chronic non-cancer pain (CNCP) are cared for, by primary care providers (PCPs).
While some of the barriers faced by PCPs have been described, there is little information about PCPs’ experience with
factors that facilitate CNCP care.
Design: The study design was descriptive and qualitative. Data were analyzed using qualitative content analysis.
Krippendorff’s thematic clustering technique was used to identify the repetitive themes regarding PCPs’ experiences
related to CNCP management.
Subjects: Respondents were PCPs (n=45) in the VA Connecticut Healthcare System in two academically affiliated
institutions and six community based sites.
Results: Eleven themes were identified across systems, personal/professional, and interpersonal domains.
Barriers included inadequate training, organizational impediments, clinical quandaries and the frustrations that
accompany them, issues related to share care among PCPs and specialists, antagonistic aspects of provider-patient
interactions, skepticism, and time factors. Facilitators included the intellectual satisfaction of solving difficult diagnostic
and management problems, the ability to develop keener communication skills, the rewards of healing and building
therapeutic alliances with patients, universal protocols, and the availability of complementary and alternative medicine
resources and multidisciplinary care.
Conclusion: PCPs experience substantial difficulties in caring for patients with pain while acknowledging certain
positive aspects. There is a need for strategies that mitigate the barriers to pain management while bolstering the
positive aspects to improve care and provider satisfaction.
*Corresponding author: L Elizabeth Lincoln, Instructor, Department of
Medicine, Harvard Medical School, Massachusetts General Hospital 55 Fruit
St, Yawkey 4B, Suite 4700 Boston, MA 02114, USA, Tel: 203-752-6168; E-mail:
llincoln2@partners.org
Received February 25, 2013; Accepted March 08, 2013; Published March 11,
2013
Citation: Lincoln LE, Pellico L, Kerns R, Anderson D (2013) Barriers and Facilitators
to Chronic Non-cancer Pain Management in Primary Care: A Qualitative Analysis
of Primary Care Providers’ Experiences and Attitudes. J Palliative Care Med S3:
001. doi:10.4172/2165-7386.S3-001
Copyright: © 2013 Lincoln LE, et al. This is an open-access article distributed
under the terms of the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided the
original author and source are credited.
Keywords: Primary care; Chronic pain; Pain management; Primary
care providers; Ambulatory care
Introduction
Pain and effective pain care are among the most critical health
issues facing Americans. In 2011, the Institute of Medicine reported
that about one-third of all Americans experience persistent pain at an
annual cost of as much as $635 billion in medical treatment and lost
productivity. The report noted that military veterans are an especially
vulnerable group, with data documenting a particularly high prevalence
of pain and extraordinary rates of complexity associated with multiple
medical and mental health comorbidities [1].
Pain is the most common symptom reported by patients receiving
care in primary care, accounting for up to 40% of all visits to primary
care providers (PCPs) [2]. More than half of all patients who have
Chronic Non-Cancer Pain (CNCP) receive their care primarily from
PCPs [3]. Estimates suggest that as many as 50% of male veterans and
up to 75% of female veterans seen in Veteran’s Health Administration
(VHA) primary care settings report the presence of pain [4-6]. More
recent data suggest that the prevalence of CNCP, particularly painful
musculoskeletal disorders including chronic low back pain, is increasing
annually [7]. Cost effective strategies that improve the management of
CNCP in the primary care setting are needed to address the challenges
posed by this public health crisis.
The VHA has implemented a Stepped Care Model for Pain
Management (SCM-PM) as a national pain care strategy to meet the
needs of veterans [8]. The SCM-PM provides for effective assessment
and treatment of pain within primary care whenever possible, with
the capacity to escalate treatment options to include specialized care
and interdisciplinary approaches, if needed. Critical to the success of
the SCM-PM is the ability of PCPs and multidisciplinary primary care
teams to effectively access and manage most common pain conditions.
The SCM-PM is similar to that advocated by the American Academy
of Pain Medicine [9], and it was cited by the Institute of Medicine as a
potentially important model of care for persons with CNCP [1].
Unfortunately, the literature suggests that PCPs do not feel
adequately prepared to take on the role of frontline providers for
patients with CNCP. Although several studies have described PCPs’
attitudes and barriers to prescribing opioids for CNCP [10-14],
Journal of Palliative Care & Medicine
J
o
u
r
n
a
l
o
f
P
a
I
I
i
a
t
i
v
e
C
a
r
e
&
M
e
d
i
c
i
n
e
ISSN: 2165-7386

Citation: Lincoln LE, Pellico L, Kerns R, Anderson D (2013) Barriers and Facilitators to Chronic Non-cancer Pain Management in Primary Care: A
Qualitative Analysis of Primary Care Providers’ Experiences and Attitudes. J Palliative Care Med S3: 001. doi:10.4172/2165-7386.S3-001
Page 2 of 7
J Palliative Care Med ISSN: 2165-7386 JPCM, an open access journal
Impact of Palliative
Care on Cancer Patients
provided with a study information sheet and a paper copy of the three
survey questions. Open-ended questions were selected for this survey
because this tactic offers a less biased approach rather than forced
participant responses and it facilitates spontaneity from respondents
[21]. Participants were recruited at practice meetings, via mailings, and
e-mail. Non-respondents were contacted again through e-mail by one
of the study staff. Study questions were:
1. Describe some barriers that you feel limit your ability to
manage chronic pain.
2. Can you describe some of the positive aspects related to caring
for patients with chronic pain?
3. What are some of the negative aspects about caring for patients
with chronic pain?
The PCPs’ written comments were typed verbatim into an excel
spread sheet and verified as accurate by comparing them to the
original survey data. Respondents’ comments totaled nearly 3000
words; individual comments ranged from one word (“time”) to 55
words (average, 11 words). Rather than code responses by each survey
question, all data were merged in order to comprehend meaning in its
entirety without losing connections between the three survey probes.
Three of the four authors read the aggregated comments in entirety
and inductively coded the comments. An inductive approach was
used to analyze the data since there is fragmented knowledge related
to the phenomenon of PCPs’ experience with CNCP using qualitative
methodology [22]. In inductive coding, the text progresses from
specific to general, so that individual instances are discerned and then
related into a larger whole that describes the phenomenon of interest.
Content analysis using Krippendorff’s method [23] was used to identify
repetitive themes. Coding consisted of the authors separately selecting
exact words, passages, or sentences, noting unique comments as well
as recurrent passages related to the research questions. Data were
grouped according to Krippendorff’s analytical technique of clustering
to identify phrases and sentences that shared some characteristics. As
an example, statements such as “suspicion,” “lack of trust in the experts’
expertise,” and “many comfortable patients state their pain score is 10”
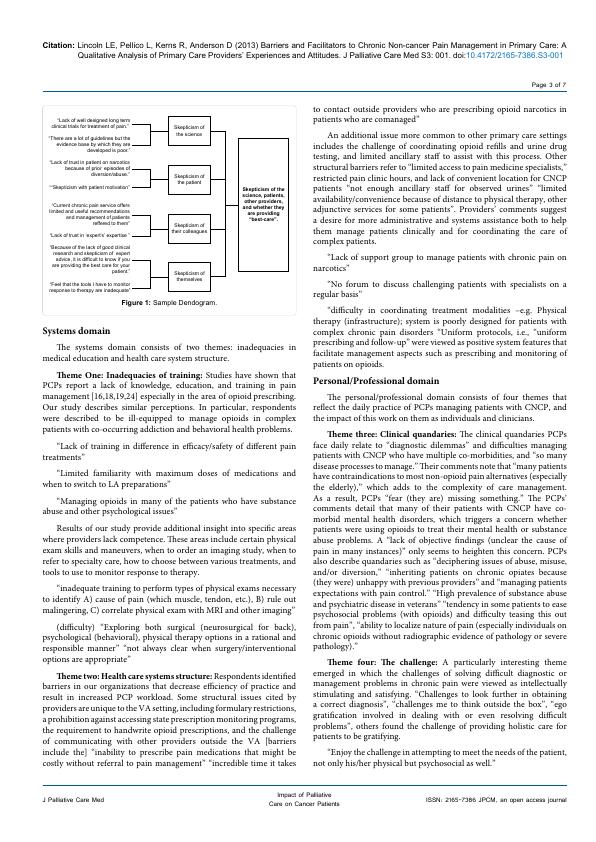
were categorized as skepticism. Dendrograms, or tree-like diagrams,
were then created to illustrate how data collapsed into clusters. An
example of a dendogram is presented in figure 1.
Authors consisted of a multidisciplinary team including a qualitative
nurse researcher, two primary care providers, and a pain psychologist.
The authors met frequently to discuss selection of passages, text
characteristics, and the transcripts were discussed line by line. Coding
among the researchers was reconciled to represent consensus about
the meaning of participant comments, and the construction of themes
was established by group consensus. An audit trail was created to
record personal reflections and to provide plausible interpretation and
evidence of consistency with the original data set. The audit trail was
shared with all authors. In addition, numerous participant quotes were
included in the results to enhance the credibility of our findings.
Results
Eleven themes were identified. The themes are artificially organized
into three domains as a taxonomy in which the reader can consider
the inter-relationships of the themes. They are: System, Personal/
Professional, and Interpersonal domains. Two of the eleven themes
interrelate across the three domains and therefore are described
separately.
few studies provide a broad overview of CNCP management from
a provider’s perspective. Previous surveys have shown that PCPs
have concerns about the prescribing of opioids and are fearful of
contributing to addiction. In addition, PCPs note the deficiency in
primary care education and training in pain management, and question
their capacity to provide optimal pain care [15-19]. Limitations of this
research include the fact that some of these studies targeted subsets of
the broader population of primary care patients with CNCP such as
patients having high rates of opioid utilization or addiction, or included
providers other than PCPs. More information is particularly needed
about the experiences and attitudes of PCPs serving the population
of veterans. There are even fewer studies using qualitative analysis
[17,19,20]. Qualitative research offers a method of inquiry that values
the identification of the human experience related to a phenomenon
of interest and may provide a more complete understanding of PCPs’
attitudes and experiences about pain management. Interestingly, to our
knowledge, no study has specifically inquired about the positive aspects
of pain management. While we know about some of the barriers to pain
care, there is relatively little information about factors that providers
feel facilitate the care of patients with chronic pain other than opioid
agreements and a strong therapeutic doctor-patient alliance [17,20].
Our objective in conducting this study was to further describe the
context of CNCP management in primary care by exploring PCPs’
experiences and viewpoints of barriers and facilitators using qualitative
analysis. We expected that the findings would highlight important
opportunities for improving the quality of chronic pain management
in primary care not previously identified. This study was part of a larger
research project to improve the care of veterans with chronic pain at
the VA Connecticut Healthcare System (VACHS) and its findings
will be used to promote knowledge uptake and inform system-wide
improvements in pain management across the VHA.
Methods
Setting
The primary care section of the VACHS provides medical care to
46,000 veterans. Primary care is provided by PCPs in two large academic
medical centers and six community based practices. Comprehensive
specialty care is available to all VACHS patients. Patients have access to
pain specialists who perform consultations and procedures, as well as
to an interdisciplinary pain center.
Sample
All PCPs (N=60) were invited to participate in the study by
completing a three item open response survey and a fifty item
knowledge questionnaire. Only results of the open response survey
are reported here. Forty-five PCPs participated, for a return rate of
75%. Respondents were 60% female and 40% male, with 40 Attending
Physicians, four Advanced Practice Registered Nurses (APRNs), and
one Physician Assistant (PA). Academic faculty numbered 26. Average
time in practice since graduation from training was 17 years. On
average, approximately five percent of each provider’s panel of patients
was being treated with prescription opioid medication.
Design
Survey questions were formed based upon current research
findings, overall aims of the study, and researchers’ experience treating
patients with chronic pain. This study was reviewed and approved by
the VACHS Human Studies Subcommittee, and the Yale University
School of Medicine Institutional Review Board. A waiver of written
informed consent was approved. All PCPs in the VACHS were
Qualitative Analysis of Primary Care Providers’ Experiences and Attitudes. J Palliative Care Med S3: 001. doi:10.4172/2165-7386.S3-001
Page 2 of 7
J Palliative Care Med ISSN: 2165-7386 JPCM, an open access journal
Impact of Palliative
Care on Cancer Patients
provided with a study information sheet and a paper copy of the three
survey questions. Open-ended questions were selected for this survey
because this tactic offers a less biased approach rather than forced
participant responses and it facilitates spontaneity from respondents
[21]. Participants were recruited at practice meetings, via mailings, and
e-mail. Non-respondents were contacted again through e-mail by one
of the study staff. Study questions were:
1. Describe some barriers that you feel limit your ability to
manage chronic pain.
2. Can you describe some of the positive aspects related to caring
for patients with chronic pain?
3. What are some of the negative aspects about caring for patients
with chronic pain?
The PCPs’ written comments were typed verbatim into an excel
spread sheet and verified as accurate by comparing them to the
original survey data. Respondents’ comments totaled nearly 3000
words; individual comments ranged from one word (“time”) to 55
words (average, 11 words). Rather than code responses by each survey
question, all data were merged in order to comprehend meaning in its
entirety without losing connections between the three survey probes.
Three of the four authors read the aggregated comments in entirety
and inductively coded the comments. An inductive approach was
used to analyze the data since there is fragmented knowledge related
to the phenomenon of PCPs’ experience with CNCP using qualitative
methodology [22]. In inductive coding, the text progresses from
specific to general, so that individual instances are discerned and then
related into a larger whole that describes the phenomenon of interest.
Content analysis using Krippendorff’s method [23] was used to identify
repetitive themes. Coding consisted of the authors separately selecting
exact words, passages, or sentences, noting unique comments as well
as recurrent passages related to the research questions. Data were
grouped according to Krippendorff’s analytical technique of clustering
to identify phrases and sentences that shared some characteristics. As
an example, statements such as “suspicion,” “lack of trust in the experts’
expertise,” and “many comfortable patients state their pain score is 10”
were categorized as skepticism. Dendrograms, or tree-like diagrams,
were then created to illustrate how data collapsed into clusters. An
example of a dendogram is presented in figure 1.
Authors consisted of a multidisciplinary team including a qualitative
nurse researcher, two primary care providers, and a pain psychologist.
The authors met frequently to discuss selection of passages, text
characteristics, and the transcripts were discussed line by line. Coding
among the researchers was reconciled to represent consensus about
the meaning of participant comments, and the construction of themes
was established by group consensus. An audit trail was created to
record personal reflections and to provide plausible interpretation and
evidence of consistency with the original data set. The audit trail was
shared with all authors. In addition, numerous participant quotes were
included in the results to enhance the credibility of our findings.
Results
Eleven themes were identified. The themes are artificially organized
into three domains as a taxonomy in which the reader can consider
the inter-relationships of the themes. They are: System, Personal/
Professional, and Interpersonal domains. Two of the eleven themes
interrelate across the three domains and therefore are described
separately.
few studies provide a broad overview of CNCP management from
a provider’s perspective. Previous surveys have shown that PCPs
have concerns about the prescribing of opioids and are fearful of
contributing to addiction. In addition, PCPs note the deficiency in
primary care education and training in pain management, and question
their capacity to provide optimal pain care [15-19]. Limitations of this
research include the fact that some of these studies targeted subsets of
the broader population of primary care patients with CNCP such as
patients having high rates of opioid utilization or addiction, or included
providers other than PCPs. More information is particularly needed
about the experiences and attitudes of PCPs serving the population
of veterans. There are even fewer studies using qualitative analysis
[17,19,20]. Qualitative research offers a method of inquiry that values
the identification of the human experience related to a phenomenon
of interest and may provide a more complete understanding of PCPs’
attitudes and experiences about pain management. Interestingly, to our
knowledge, no study has specifically inquired about the positive aspects
of pain management. While we know about some of the barriers to pain
care, there is relatively little information about factors that providers
feel facilitate the care of patients with chronic pain other than opioid
agreements and a strong therapeutic doctor-patient alliance [17,20].
Our objective in conducting this study was to further describe the
context of CNCP management in primary care by exploring PCPs’
experiences and viewpoints of barriers and facilitators using qualitative
analysis. We expected that the findings would highlight important
opportunities for improving the quality of chronic pain management
in primary care not previously identified. This study was part of a larger
research project to improve the care of veterans with chronic pain at
the VA Connecticut Healthcare System (VACHS) and its findings
will be used to promote knowledge uptake and inform system-wide
improvements in pain management across the VHA.
Methods
Setting
The primary care section of the VACHS provides medical care to
46,000 veterans. Primary care is provided by PCPs in two large academic
medical centers and six community based practices. Comprehensive
specialty care is available to all VACHS patients. Patients have access to
pain specialists who perform consultations and procedures, as well as
to an interdisciplinary pain center.
Sample
All PCPs (N=60) were invited to participate in the study by
completing a three item open response survey and a fifty item
knowledge questionnaire. Only results of the open response survey
are reported here. Forty-five PCPs participated, for a return rate of
75%. Respondents were 60% female and 40% male, with 40 Attending
Physicians, four Advanced Practice Registered Nurses (APRNs), and
one Physician Assistant (PA). Academic faculty numbered 26. Average
time in practice since graduation from training was 17 years. On
average, approximately five percent of each provider’s panel of patients
was being treated with prescription opioid medication.
Design
Survey questions were formed based upon current research
findings, overall aims of the study, and researchers’ experience treating
patients with chronic pain. This study was reviewed and approved by
the VACHS Human Studies Subcommittee, and the Yale University
School of Medicine Institutional Review Board. A waiver of written
informed consent was approved. All PCPs in the VACHS were

Citation: Lincoln LE, Pellico L, Kerns R, Anderson D (2013) Barriers and Facilitators to Chronic Non-cancer Pain Management in Primary Care: A
Qualitative Analysis of Primary Care Providers’ Experiences and Attitudes. J Palliative Care Med S3: 001. doi:10.4172/2165-7386.S3-001
Page 3 of 7
J Palliative Care Med ISSN: 2165-7386 JPCM, an open access journal
Impact of Palliative
Care on Cancer Patients
Systems domain
The systems domain consists of two themes: inadequacies in
medical education and health care system structure.
Theme One: Inadequacies of training: Studies have shown that
PCPs report a lack of knowledge, education, and training in pain
management [16,18,19,24] especially in the area of opioid prescribing.
Our study describes similar perceptions. In particular, respondents
were described to be ill-equipped to manage opioids in complex
patients with co-occurring addiction and behavioral health problems.
“Lack of training in difference in efficacy/safety of different pain
treatments”
“Limited familiarity with maximum doses of medications and
when to switch to LA preparations”
“Managing opioids in many of the patients who have substance
abuse and other psychological issues”
Results of our study provide additional insight into specific areas
where providers lack competence. These areas include certain physical
exam skills and maneuvers, when to order an imaging study, when to
refer to specialty care, how to choose between various treatments, and
tools to use to monitor response to therapy.
“inadequate training to perform types of physical exams necessary
to identify A) cause of pain (which muscle, tendon, etc.), B) rule out
malingering, C) correlate physical exam with MRI and other imaging”
(difficulty) “Exploring both surgical (neurosurgical for back),
psychological (behavioral), physical therapy options in a rational and
responsible manner” “not always clear when surgery/interventional
options are appropriate”
Theme two: Health care systems structure: Respondents identified
barriers in our organizations that decrease efficiency of practice and
result in increased PCP workload. Some structural issues cited by
providers are unique to the VA setting, including formulary restrictions,
a prohibition against accessing state prescription monitoring programs,
the requirement to handwrite opioid prescriptions, and the challenge
of communicating with other providers outside the VA [barriers
include the] “inability to prescribe pain medications that might be
costly without referral to pain management” “incredible time it takes
to contact outside providers who are prescribing opioid narcotics in
patients who are comanaged”
An additional issue more common to other primary care settings
includes the challenge of coordinating opioid refills and urine drug
testing, and limited ancillary staff to assist with this process. Other
structural barriers refer to “limited access to pain medicine specialists,”
restricted pain clinic hours, and lack of convenient location for CNCP
patients “not enough ancillary staff for observed urines” “limited
availability/convenience because of distance to physical therapy, other
adjunctive services for some patients”. Providers’ comments suggest
a desire for more administrative and systems assistance both to help
them manage patients clinically and for coordinating the care of
complex patients.
“Lack of support group to manage patients with chronic pain on
narcotics”
“No forum to discuss challenging patients with specialists on a
regular basis”
“difficulty in coordinating treatment modalities –e.g. Physical
therapy (infrastructure); system is poorly designed for patients with
complex chronic pain disorders “Uniform protocols, i.e., “uniform
prescribing and follow-up” were viewed as positive system features that
facilitate management aspects such as prescribing and monitoring of
patients on opioids.
Personal/Professional domain
The personal/professional domain consists of four themes that
reflect the daily practice of PCPs managing patients with CNCP, and
the impact of this work on them as individuals and clinicians.
Theme three: Clinical quandaries: The clinical quandaries PCPs
face daily relate to “diagnostic dilemmas” and difficulties managing
patients with CNCP who have multiple co-morbidities, and “so many
disease processes to manage.” Their comments note that “many patients
have contraindications to most non-opioid pain alternatives (especially
the elderly),” which adds to the complexity of care management.
As a result, PCPs “fear (they are) missing something.” The PCPs’
comments detail that many of their patients with CNCP have co-
morbid mental health disorders, which triggers a concern whether
patients were using opioids to treat their mental health or substance
abuse problems. A “lack of objective findings (unclear the cause of
pain in many instances)” only seems to heighten this concern. PCPs
also describe quandaries such as “deciphering issues of abuse, misuse,
and/or diversion,” “inheriting patients on chronic opiates because
(they were) unhappy with previous providers” and “managing patients
expectations with pain control.” “High prevalence of substance abuse
and psychiatric disease in veterans” “tendency in some patients to ease
psychosocial problems (with opioids) and difficulty teasing this out
from pain”, “ability to localize nature of pain (especially individuals on
chronic opioids without radiographic evidence of pathology or severe
pathology).”
Theme four: The challenge: A particularly interesting theme
emerged in which the challenges of solving difficult diagnostic or
management problems in chronic pain were viewed as intellectually
stimulating and satisfying. “Challenges to look further in obtaining
a correct diagnosis”, “challenges me to think outside the box”, “ego
gratification involved in dealing with or even resolving difficult
problems”, others found the challenge of providing holistic care for
patients to be gratifying.
“Enjoy the challenge in attempting to meet the needs of the patient,
not only his/her physical but psychosocial as well.”
Skepticism of the
science, patients,
other providers,
and whether they
are providing
“best-care”.
Skepticism of
the science
Skepticism of
the patient
Skepticism of
their colleagues
Skepticism of
themselves
“Lack of well designed long term
clinical trials for treatment of pain.”
“There are a lot of guidelines but the
evidence base by which they are
developed is poor.”
“Lack of trust in patient on narcotics
because of prior episodes of
diversion/abuse.”
““Skepticism with patient motivation”
“Current chronic pain service offers
limited and useful recommendations
and management of patients
reffered to them”
“Lack of trust in ‘expert’s’ expertise ”
“Because of the lack of good clinical
research and skepticism of expert
advice, it is difficult to know if you
are providing the best care for your
patient.”
“Feel that the tools I have to monitor
response to therapy are inadequate”
Figure 1: Sample Dendogram.
Qualitative Analysis of Primary Care Providers’ Experiences and Attitudes. J Palliative Care Med S3: 001. doi:10.4172/2165-7386.S3-001
Page 3 of 7
J Palliative Care Med ISSN: 2165-7386 JPCM, an open access journal
Impact of Palliative
Care on Cancer Patients
Systems domain
The systems domain consists of two themes: inadequacies in
medical education and health care system structure.
Theme One: Inadequacies of training: Studies have shown that
PCPs report a lack of knowledge, education, and training in pain
management [16,18,19,24] especially in the area of opioid prescribing.
Our study describes similar perceptions. In particular, respondents
were described to be ill-equipped to manage opioids in complex
patients with co-occurring addiction and behavioral health problems.
“Lack of training in difference in efficacy/safety of different pain
treatments”
“Limited familiarity with maximum doses of medications and
when to switch to LA preparations”
“Managing opioids in many of the patients who have substance
abuse and other psychological issues”
Results of our study provide additional insight into specific areas
where providers lack competence. These areas include certain physical
exam skills and maneuvers, when to order an imaging study, when to
refer to specialty care, how to choose between various treatments, and
tools to use to monitor response to therapy.
“inadequate training to perform types of physical exams necessary
to identify A) cause of pain (which muscle, tendon, etc.), B) rule out
malingering, C) correlate physical exam with MRI and other imaging”
(difficulty) “Exploring both surgical (neurosurgical for back),
psychological (behavioral), physical therapy options in a rational and
responsible manner” “not always clear when surgery/interventional
options are appropriate”
Theme two: Health care systems structure: Respondents identified
barriers in our organizations that decrease efficiency of practice and
result in increased PCP workload. Some structural issues cited by
providers are unique to the VA setting, including formulary restrictions,
a prohibition against accessing state prescription monitoring programs,
the requirement to handwrite opioid prescriptions, and the challenge
of communicating with other providers outside the VA [barriers
include the] “inability to prescribe pain medications that might be
costly without referral to pain management” “incredible time it takes
to contact outside providers who are prescribing opioid narcotics in
patients who are comanaged”
An additional issue more common to other primary care settings
includes the challenge of coordinating opioid refills and urine drug
testing, and limited ancillary staff to assist with this process. Other
structural barriers refer to “limited access to pain medicine specialists,”
restricted pain clinic hours, and lack of convenient location for CNCP
patients “not enough ancillary staff for observed urines” “limited
availability/convenience because of distance to physical therapy, other
adjunctive services for some patients”. Providers’ comments suggest
a desire for more administrative and systems assistance both to help
them manage patients clinically and for coordinating the care of
complex patients.
“Lack of support group to manage patients with chronic pain on
narcotics”
“No forum to discuss challenging patients with specialists on a
regular basis”
“difficulty in coordinating treatment modalities –e.g. Physical
therapy (infrastructure); system is poorly designed for patients with
complex chronic pain disorders “Uniform protocols, i.e., “uniform
prescribing and follow-up” were viewed as positive system features that
facilitate management aspects such as prescribing and monitoring of
patients on opioids.
Personal/Professional domain
The personal/professional domain consists of four themes that
reflect the daily practice of PCPs managing patients with CNCP, and
the impact of this work on them as individuals and clinicians.
Theme three: Clinical quandaries: The clinical quandaries PCPs
face daily relate to “diagnostic dilemmas” and difficulties managing
patients with CNCP who have multiple co-morbidities, and “so many
disease processes to manage.” Their comments note that “many patients
have contraindications to most non-opioid pain alternatives (especially
the elderly),” which adds to the complexity of care management.
As a result, PCPs “fear (they are) missing something.” The PCPs’
comments detail that many of their patients with CNCP have co-
morbid mental health disorders, which triggers a concern whether
patients were using opioids to treat their mental health or substance
abuse problems. A “lack of objective findings (unclear the cause of
pain in many instances)” only seems to heighten this concern. PCPs
also describe quandaries such as “deciphering issues of abuse, misuse,
and/or diversion,” “inheriting patients on chronic opiates because
(they were) unhappy with previous providers” and “managing patients
expectations with pain control.” “High prevalence of substance abuse
and psychiatric disease in veterans” “tendency in some patients to ease
psychosocial problems (with opioids) and difficulty teasing this out
from pain”, “ability to localize nature of pain (especially individuals on
chronic opioids without radiographic evidence of pathology or severe
pathology).”
Theme four: The challenge: A particularly interesting theme
emerged in which the challenges of solving difficult diagnostic or
management problems in chronic pain were viewed as intellectually
stimulating and satisfying. “Challenges to look further in obtaining
a correct diagnosis”, “challenges me to think outside the box”, “ego
gratification involved in dealing with or even resolving difficult
problems”, others found the challenge of providing holistic care for
patients to be gratifying.
“Enjoy the challenge in attempting to meet the needs of the patient,
not only his/her physical but psychosocial as well.”
Skepticism of the
science, patients,
other providers,
and whether they
are providing
“best-care”.
Skepticism of
the science
Skepticism of
the patient
Skepticism of
their colleagues
Skepticism of
themselves
“Lack of well designed long term
clinical trials for treatment of pain.”
“There are a lot of guidelines but the
evidence base by which they are
developed is poor.”
“Lack of trust in patient on narcotics
because of prior episodes of
diversion/abuse.”
““Skepticism with patient motivation”
“Current chronic pain service offers
limited and useful recommendations
and management of patients
reffered to them”
“Lack of trust in ‘expert’s’ expertise ”
“Because of the lack of good clinical
research and skepticism of expert
advice, it is difficult to know if you
are providing the best care for your
patient.”
“Feel that the tools I have to monitor
response to therapy are inadequate”
Figure 1: Sample Dendogram.
End of preview
Want to access all the pages? Upload your documents or become a member.
Related Documents
Role of Nurses in Cancer Care: A Qualitative Studylg...
|4
|1516
|417
Primary Health Care - NUR115 - Northern Health Hospitallg...
|6
|1453
|60
Informal Care Givers - PDFlg...
|4
|666
|67
