Clinical Interventions in Aging
Added on 2022-08-23
14 Pages11866 Words30 Views
© 2015 Burton et al. This work is published by Dove Medical Press Limited, and licensed under Creative Commons Attribution – Non Commercial (unported, v3.0)
License. The full terms of the License are available at http://creativecommons.org/licenses/by-nc/3.0/. Non-commercial uses of the work are permitted without any further
permission from Dove Medical Press Limited, provided the work is properly attributed. Permissions beyond the scope of the License are administered by Dove Medical Press Limited. Information on
how to request permission may be found at: http://www.dovepress.com/permissions.php
Clinical Interventions in Aging 2015:10 421–434
Clinical Interventions in Aging Dovepress
submit your manuscript | www.dovepress.com
Dovepress
421
R e v I e w
open access to scientific and medical research
Open Access Full Text Article
http://dx.doi.org/10.2147/CIA.S71691
effectiveness of exercise programs to reduce
falls in older people with dementia living in the
community: a systematic review and meta-analysis
elissa Burton1,2
vinicius Cavalheri1
Richard Adams3
Colleen Oakley Browne4
Petra Bovery-Spencer4
Audra M Fenton3
Bruce w Campbell5
Keith D Hill1,6
1School of Physiotherapy and exercise
Science, Curtin University, Perth, wA,
Australia; 2Research Department,
Silver Chain, Perth, wA, Australia;
3Community Services, west Gippsland
Healthcare Group, warragul, vIC,
Australia; 4Falls Prevention for
People Living with Dementia Project,
Central west Gippsland Primary
Care Partnership, Moe, vIC, Australia;
5Allied Health, Latrobe Regional
Hospital, Traralgon, vIC, Australia;
6Preventive and Public Health
Division, National Ageing Research
Institute, Melbourne, vIC, Australia
Objective: The objective of this systematic review and meta-analysis is to evaluate the effec-
tiveness of exercise programs to reduce falls in older people with dementia who are living in
the community.
Method: Peer-reviewed articles (randomized controlled trials [RCTs] and quasi-experimental
trials) published in English between January 2000 and February 2014, retrieved from six elec-
tronic databases – Medline (ProQuest), CINAHL, PubMed, PsycInfo, EMBASE and Scopus –
according to predefined inclusion criteria were included. Where possible, results were pooled
and meta-analysis was conducted.
Results: Four articles (three RCT and one single-group pre- and post-test pilot study) were
included. The study quality of the three RCTs was high; however, measurement outcomes,
interventions, and follow-up time periods differed across studies. On completion of the interven-
tion period, the mean number of falls was lower in the exercise group compared to the control
group (mean difference [MD] [95% confidence interval {CI}] =-1.06 [-1.67 to -0.46] falls).
Importantly, the exercise intervention reduced the risk of being a faller by 32% (risk ratio [95%
CI] =0.68 [0.55–0.85]). Only two other outcomes were reported in two or more of the studies
(step test and physiological profile assessment). No between-group differences were observed
in the results of the step test (number of steps) (MD [95% CI] =0.51 [-1.77 to 2.78]) or the
physiological profile assessment (MD [95% CI] =-0.10 [-0.62 to 0.42]).
Conclusion: Findings from this review suggest that an exercise program may potentially assist
in preventing falls of older people with dementia living in the community. However, further
research is needed with studies using larger sample sizes, standardized measurement outcomes,
and longer follow-up periods, to inform evidence-based recommendations.
Keywords: cognitive impairment, older people, physical activity, fallers, community
dwelling
Introduction
Dementia is a major health issue predominantly affecting older people. It is estimated
that over 44 million people worldwide are living with dementia, and by 2050 there
may be as many as 135.5 million people diagnosed with dementia.1 The world popula-
tion is aging and as such it is expected that the increase in the number of older people
will correspond with an increase in the number of older people living with dementia
(PLWD). Dementia is a syndrome that impairs brain function and cognition. As the
severity of dementia increases over time, the person with dementia often has increased
difficulties with many important functions, including gait impairments, problems with
postural control, reduced participation in activities such as shopping and driving,
Correspondence: elissa Burton
Curtin University, School of Physiotherapy
and exercise Science, GPO Box U 1987,
Perth, wA 6845, Australia
Tel +61 8 9266 3681
Fax +61 8 9266 3699
email e.burton@curtin.edu.au
License. The full terms of the License are available at http://creativecommons.org/licenses/by-nc/3.0/. Non-commercial uses of the work are permitted without any further
permission from Dove Medical Press Limited, provided the work is properly attributed. Permissions beyond the scope of the License are administered by Dove Medical Press Limited. Information on
how to request permission may be found at: http://www.dovepress.com/permissions.php
Clinical Interventions in Aging 2015:10 421–434
Clinical Interventions in Aging Dovepress
submit your manuscript | www.dovepress.com
Dovepress
421
R e v I e w
open access to scientific and medical research
Open Access Full Text Article
http://dx.doi.org/10.2147/CIA.S71691
effectiveness of exercise programs to reduce
falls in older people with dementia living in the
community: a systematic review and meta-analysis
elissa Burton1,2
vinicius Cavalheri1
Richard Adams3
Colleen Oakley Browne4
Petra Bovery-Spencer4
Audra M Fenton3
Bruce w Campbell5
Keith D Hill1,6
1School of Physiotherapy and exercise
Science, Curtin University, Perth, wA,
Australia; 2Research Department,
Silver Chain, Perth, wA, Australia;
3Community Services, west Gippsland
Healthcare Group, warragul, vIC,
Australia; 4Falls Prevention for
People Living with Dementia Project,
Central west Gippsland Primary
Care Partnership, Moe, vIC, Australia;
5Allied Health, Latrobe Regional
Hospital, Traralgon, vIC, Australia;
6Preventive and Public Health
Division, National Ageing Research
Institute, Melbourne, vIC, Australia
Objective: The objective of this systematic review and meta-analysis is to evaluate the effec-
tiveness of exercise programs to reduce falls in older people with dementia who are living in
the community.
Method: Peer-reviewed articles (randomized controlled trials [RCTs] and quasi-experimental
trials) published in English between January 2000 and February 2014, retrieved from six elec-
tronic databases – Medline (ProQuest), CINAHL, PubMed, PsycInfo, EMBASE and Scopus –
according to predefined inclusion criteria were included. Where possible, results were pooled
and meta-analysis was conducted.
Results: Four articles (three RCT and one single-group pre- and post-test pilot study) were
included. The study quality of the three RCTs was high; however, measurement outcomes,
interventions, and follow-up time periods differed across studies. On completion of the interven-
tion period, the mean number of falls was lower in the exercise group compared to the control
group (mean difference [MD] [95% confidence interval {CI}] =-1.06 [-1.67 to -0.46] falls).
Importantly, the exercise intervention reduced the risk of being a faller by 32% (risk ratio [95%
CI] =0.68 [0.55–0.85]). Only two other outcomes were reported in two or more of the studies
(step test and physiological profile assessment). No between-group differences were observed
in the results of the step test (number of steps) (MD [95% CI] =0.51 [-1.77 to 2.78]) or the
physiological profile assessment (MD [95% CI] =-0.10 [-0.62 to 0.42]).
Conclusion: Findings from this review suggest that an exercise program may potentially assist
in preventing falls of older people with dementia living in the community. However, further
research is needed with studies using larger sample sizes, standardized measurement outcomes,
and longer follow-up periods, to inform evidence-based recommendations.
Keywords: cognitive impairment, older people, physical activity, fallers, community
dwelling
Introduction
Dementia is a major health issue predominantly affecting older people. It is estimated
that over 44 million people worldwide are living with dementia, and by 2050 there
may be as many as 135.5 million people diagnosed with dementia.1 The world popula-
tion is aging and as such it is expected that the increase in the number of older people
will correspond with an increase in the number of older people living with dementia
(PLWD). Dementia is a syndrome that impairs brain function and cognition. As the
severity of dementia increases over time, the person with dementia often has increased
difficulties with many important functions, including gait impairments, problems with
postural control, reduced participation in activities such as shopping and driving,
Correspondence: elissa Burton
Curtin University, School of Physiotherapy
and exercise Science, GPO Box U 1987,
Perth, wA 6845, Australia
Tel +61 8 9266 3681
Fax +61 8 9266 3699
email e.burton@curtin.edu.au
Clinical Interventions in Aging 2015:10submit your manuscript | www.dovepress.com
Dovepress
Dovepress
422
Burton et al
and an increase in disability leading to difficulties in eat-
ing, bathing, and dressing.2,3 The impairments in cognition,
gait, and postural control also increase the risk of falls in
people with dementia. Approximately 30% of adults aged
65 years and over living in the community experience one or
more fall each year,4 but up to 50%–80% of PLWD fall in a
12-month period.5,6 There are many identified risk factors for
falls, including intrinsic factors such as postural instability
(gait and balance impairments), medications, neurocardio-
vascular complications, and vision impairment, as well as
extrinsic factors such as the environment (curbs, rugs, or poor
lighting).7 Falls can often lead to a fear of falling or loss of
confidence, which may result in a decline in activity and ulti-
mately a decrease in strength, balance, and mobility, leading
to decreased functional ability and a loss of independence.8,9
Falls are also often a trigger for emergency department or
hospital admission for older people with dementia10 and/or
admission to residential care.10,11
Balance and mobility impairments in older people
have been shown to be a strong independent risk factor for
falling,12 and have been shown to decline at a significantly
faster rate in PLWD than age-matched older people without
cognitive impairment.13 To combat postural instability and
decreases in function, a large number of studies have been
conducted, investigating the effectiveness of exercise or
physical activity programs to prevent falls for older people
with a history of falling.4,14 Reviews of these studies have
shown that strength- and balance-focused exercise programs
have been successful in decreasing the rate of falls for older
people living in the community with no cognitive impair-
ment, using both group- and home-based environments for
exercise. Based on these results, exercise or physical activity
programs are viewed as an important part of falls prevention
programs.3,4,15 However, direct translation of falls prevention
programs that have been shown to be effective in reducing
falls in samples with no cognitive impairment (eg, Close
et al16 multifactorial intervention) may not be effective when
implemented with people with cognitive impairment.17
Despite the higher risk of falls and greater rate of decline
of balance and gait in PLWD in the community, there has
been only a small but growing amount of research investigat-
ing the effect of exercise on improving physical performance
and reducing falls in people with dementia. There have been
nine systematic reviews14,18–25 and four general reviews7,17,26,27
investigating the effects of dementia/Alzheimer’s disease
on falls, and eight systematic reviews exploring the effects
of exercise (types of exercise) on people with cognitive
impairment.3,28–34 Six of the 21 reviews reported earlier
included studies using PLWD in a residential care or hospital
setting, four had a majority of participants living in the
community, nine had a mix of older people living in both
community and residential care, and three were unclear
in describing the setting. Of the four reviews where older
people with dementia living in the community setting were
the majority sample population, one focused on medicine
and falls,21 another recruited participants living in the com-
munity from health care settings (emergency department,
dementia specific service, etc),25 the third looked at falls
risk with no specific emphasis on exercise,19 and the fourth
investigated the relationship between executive function,
falls, and gait abnormalities.32 There is a dearth of research
that specifically explored falls prevention exercise interven-
tions for people with dementia (cognitive impairment) living
in the community.
One systematic review by Hauer et al35 did investigate
the effectiveness of physical training on motor performance
and fall prevention in cognitively impaired older persons
(search strategy was between 1966 and 2004). Again, of the
eleven randomized controlled trials (RCTs) included in this
review, nine were from a residential/long-term care/hospital
setting and one was of people living in the community, and
in the other the setting was unknown. Physical training was
not defined and appeared to represent strength and balance
programs designed by physiotherapists to be conducted in
either an individual or group setting.35 Physical activity
programs such as Tai Chi, which have been shown to be
effective in reducing falls, were not included.
In summary, to date the reviews published in this area are
limited when exploring those that have specifically focused
on older PLWD in the community with exercise and/or physi-
cal activity as the intervention, and with falls as the outcome
of interest. This systematic review seeks to address this gap.
The purpose of this review is to evaluate the available evi-
dence on the effectiveness of exercise or physical activity
programs to reduce falls in older people with dementia who
are living in the community.
Method
eligibility criteria
The review is limited to studies meeting the following eli-
gibility criteria:
• aged 60 years and over (at least 50% of the sample size);
• living in the community;
• PLWD or cognitively impaired. Dementia had to have
been identified by diagnosis by a doctor/specialist, or a
validated test, such as the Mini Mental State Examination
Dovepress
Dovepress
422
Burton et al
and an increase in disability leading to difficulties in eat-
ing, bathing, and dressing.2,3 The impairments in cognition,
gait, and postural control also increase the risk of falls in
people with dementia. Approximately 30% of adults aged
65 years and over living in the community experience one or
more fall each year,4 but up to 50%–80% of PLWD fall in a
12-month period.5,6 There are many identified risk factors for
falls, including intrinsic factors such as postural instability
(gait and balance impairments), medications, neurocardio-
vascular complications, and vision impairment, as well as
extrinsic factors such as the environment (curbs, rugs, or poor
lighting).7 Falls can often lead to a fear of falling or loss of
confidence, which may result in a decline in activity and ulti-
mately a decrease in strength, balance, and mobility, leading
to decreased functional ability and a loss of independence.8,9
Falls are also often a trigger for emergency department or
hospital admission for older people with dementia10 and/or
admission to residential care.10,11
Balance and mobility impairments in older people
have been shown to be a strong independent risk factor for
falling,12 and have been shown to decline at a significantly
faster rate in PLWD than age-matched older people without
cognitive impairment.13 To combat postural instability and
decreases in function, a large number of studies have been
conducted, investigating the effectiveness of exercise or
physical activity programs to prevent falls for older people
with a history of falling.4,14 Reviews of these studies have
shown that strength- and balance-focused exercise programs
have been successful in decreasing the rate of falls for older
people living in the community with no cognitive impair-
ment, using both group- and home-based environments for
exercise. Based on these results, exercise or physical activity
programs are viewed as an important part of falls prevention
programs.3,4,15 However, direct translation of falls prevention
programs that have been shown to be effective in reducing
falls in samples with no cognitive impairment (eg, Close
et al16 multifactorial intervention) may not be effective when
implemented with people with cognitive impairment.17
Despite the higher risk of falls and greater rate of decline
of balance and gait in PLWD in the community, there has
been only a small but growing amount of research investigat-
ing the effect of exercise on improving physical performance
and reducing falls in people with dementia. There have been
nine systematic reviews14,18–25 and four general reviews7,17,26,27
investigating the effects of dementia/Alzheimer’s disease
on falls, and eight systematic reviews exploring the effects
of exercise (types of exercise) on people with cognitive
impairment.3,28–34 Six of the 21 reviews reported earlier
included studies using PLWD in a residential care or hospital
setting, four had a majority of participants living in the
community, nine had a mix of older people living in both
community and residential care, and three were unclear
in describing the setting. Of the four reviews where older
people with dementia living in the community setting were
the majority sample population, one focused on medicine
and falls,21 another recruited participants living in the com-
munity from health care settings (emergency department,
dementia specific service, etc),25 the third looked at falls
risk with no specific emphasis on exercise,19 and the fourth
investigated the relationship between executive function,
falls, and gait abnormalities.32 There is a dearth of research
that specifically explored falls prevention exercise interven-
tions for people with dementia (cognitive impairment) living
in the community.
One systematic review by Hauer et al35 did investigate
the effectiveness of physical training on motor performance
and fall prevention in cognitively impaired older persons
(search strategy was between 1966 and 2004). Again, of the
eleven randomized controlled trials (RCTs) included in this
review, nine were from a residential/long-term care/hospital
setting and one was of people living in the community, and
in the other the setting was unknown. Physical training was
not defined and appeared to represent strength and balance
programs designed by physiotherapists to be conducted in
either an individual or group setting.35 Physical activity
programs such as Tai Chi, which have been shown to be
effective in reducing falls, were not included.
In summary, to date the reviews published in this area are
limited when exploring those that have specifically focused
on older PLWD in the community with exercise and/or physi-
cal activity as the intervention, and with falls as the outcome
of interest. This systematic review seeks to address this gap.
The purpose of this review is to evaluate the available evi-
dence on the effectiveness of exercise or physical activity
programs to reduce falls in older people with dementia who
are living in the community.
Method
eligibility criteria
The review is limited to studies meeting the following eli-
gibility criteria:
• aged 60 years and over (at least 50% of the sample size);
• living in the community;
• PLWD or cognitively impaired. Dementia had to have
been identified by diagnosis by a doctor/specialist, or a
validated test, such as the Mini Mental State Examination

Clinical Interventions in Aging 2015:10 submit your manuscript | www.dovepress.com
Dovepress
Dovepress
423
exercise to reduce falls for community dwelling people with dementia
(MMSE), the Clinical Dementia Rating Scale, or the
National Institute of Neurological and Communicative
Disorders and Stroke, Alzheimer’s Disease and Related
Disorders Association (NINCDS-ADRDA) Alzheimer’s
criteria;
• an exercise or physical activity program (intervention)
targeting a reduction in falls (and/or) risk of falls;
• outcome measures, which include number of falls, rate
of falls, or number of fallers, or time to first fall. Other
outcomes of interest were fear of having a fall, functional,
physical performance (eg, balance or mobility), or cogni-
tive benefits, or adherence to exercise/physical activity
intervention;
• study design: RCTs and quasi-experimental trials.
Information sources
Studies were identified by searching six databases (Medline
[ProQuest], CINAHL, PubMed, PsycInfo, EMBASE, and
Scopus, from January 2000 to February 2014). The search
strategy commenced from 2000, given a detailed review by
Hauer et al35 which searched across residential care, hospital,
and community settings, and did not identify any relevant
papers prior to 2003 in the community setting. In addition,
reference lists of the identified papers were scanned. Only
papers in English were included, no unpublished data,
books, conference proceedings, theses, or poster abstracts
were included.
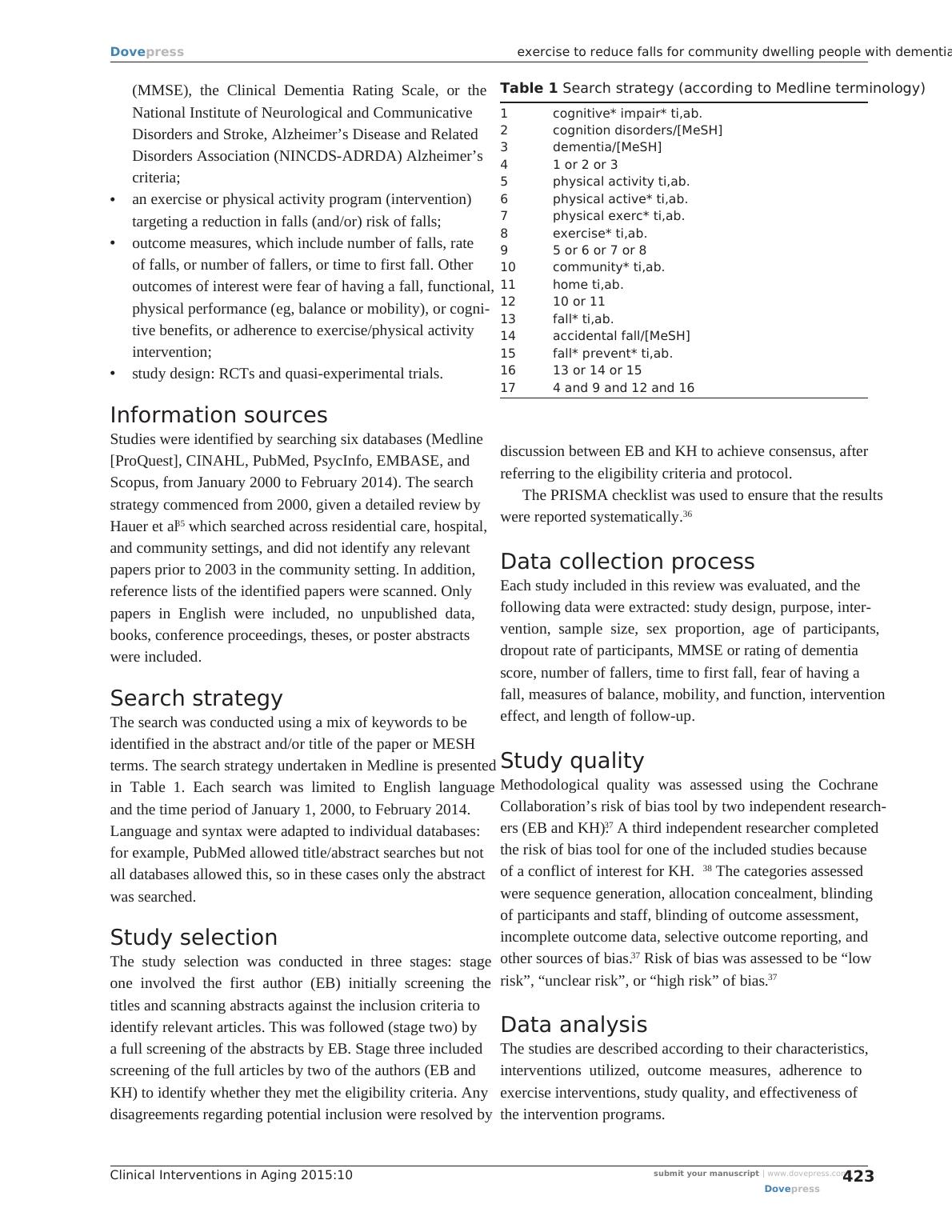
Search strategy
The search was conducted using a mix of keywords to be
identified in the abstract and/or title of the paper or MESH
terms. The search strategy undertaken in Medline is presented
in Table 1. Each search was limited to English language
and the time period of January 1, 2000, to February 2014.
Language and syntax were adapted to individual databases:
for example, PubMed allowed title/abstract searches but not
all databases allowed this, so in these cases only the abstract
was searched.
Study selection
The study selection was conducted in three stages: stage
one involved the first author (EB) initially screening the
titles and scanning abstracts against the inclusion criteria to
identify relevant articles. This was followed (stage two) by
a full screening of the abstracts by EB. Stage three included
screening of the full articles by two of the authors (EB and
KH) to identify whether they met the eligibility criteria. Any
disagreements regarding potential inclusion were resolved by
discussion between EB and KH to achieve consensus, after
referring to the eligibility criteria and protocol.
The PRISMA checklist was used to ensure that the results
were reported systematically.36
Data collection process
Each study included in this review was evaluated, and the
following data were extracted: study design, purpose, inter-
vention, sample size, sex proportion, age of participants,
dropout rate of participants, MMSE or rating of dementia
score, number of fallers, time to first fall, fear of having a
fall, measures of balance, mobility, and function, intervention
effect, and length of follow-up.
Study quality
Methodological quality was assessed using the Cochrane
Collaboration’s risk of bias tool by two independent research-
ers (EB and KH).37 A third independent researcher completed
the risk of bias tool for one of the included studies because
of a conflict of interest for KH.38 The categories assessed
were sequence generation, allocation concealment, blinding
of participants and staff, blinding of outcome assessment,
incomplete outcome data, selective outcome reporting, and
other sources of bias.37 Risk of bias was assessed to be “low
risk”, “unclear risk”, or “high risk” of bias.37
Data analysis
The studies are described according to their characteristics,
interventions utilized, outcome measures, adherence to
exercise interventions, study quality, and effectiveness of
the intervention programs.
Table 1 Search strategy (according to Medline terminology)
1 cognitive* impair* ti,ab.
2 cognition disorders/[MeSH]
3 dementia/[MeSH]
4 1 or 2 or 3
5 physical activity ti,ab.
6 physical active* ti,ab.
7 physical exerc* ti,ab.
8 exercise* ti,ab.
9 5 or 6 or 7 or 8
10 community* ti,ab.
11 home ti,ab.
12 10 or 11
13 fall* ti,ab.
14 accidental fall/[MeSH]
15 fall* prevent* ti,ab.
16 13 or 14 or 15
17 4 and 9 and 12 and 16
Dovepress
Dovepress
423
exercise to reduce falls for community dwelling people with dementia
(MMSE), the Clinical Dementia Rating Scale, or the
National Institute of Neurological and Communicative
Disorders and Stroke, Alzheimer’s Disease and Related
Disorders Association (NINCDS-ADRDA) Alzheimer’s
criteria;
• an exercise or physical activity program (intervention)
targeting a reduction in falls (and/or) risk of falls;
• outcome measures, which include number of falls, rate
of falls, or number of fallers, or time to first fall. Other
outcomes of interest were fear of having a fall, functional,
physical performance (eg, balance or mobility), or cogni-
tive benefits, or adherence to exercise/physical activity
intervention;
• study design: RCTs and quasi-experimental trials.
Information sources
Studies were identified by searching six databases (Medline
[ProQuest], CINAHL, PubMed, PsycInfo, EMBASE, and
Scopus, from January 2000 to February 2014). The search
strategy commenced from 2000, given a detailed review by
Hauer et al35 which searched across residential care, hospital,
and community settings, and did not identify any relevant
papers prior to 2003 in the community setting. In addition,
reference lists of the identified papers were scanned. Only
papers in English were included, no unpublished data,
books, conference proceedings, theses, or poster abstracts
were included.
Search strategy
The search was conducted using a mix of keywords to be
identified in the abstract and/or title of the paper or MESH
terms. The search strategy undertaken in Medline is presented
in Table 1. Each search was limited to English language
and the time period of January 1, 2000, to February 2014.
Language and syntax were adapted to individual databases:
for example, PubMed allowed title/abstract searches but not
all databases allowed this, so in these cases only the abstract
was searched.
Study selection
The study selection was conducted in three stages: stage
one involved the first author (EB) initially screening the
titles and scanning abstracts against the inclusion criteria to
identify relevant articles. This was followed (stage two) by
a full screening of the abstracts by EB. Stage three included
screening of the full articles by two of the authors (EB and
KH) to identify whether they met the eligibility criteria. Any
disagreements regarding potential inclusion were resolved by
discussion between EB and KH to achieve consensus, after
referring to the eligibility criteria and protocol.
The PRISMA checklist was used to ensure that the results
were reported systematically.36
Data collection process
Each study included in this review was evaluated, and the
following data were extracted: study design, purpose, inter-
vention, sample size, sex proportion, age of participants,
dropout rate of participants, MMSE or rating of dementia
score, number of fallers, time to first fall, fear of having a
fall, measures of balance, mobility, and function, intervention
effect, and length of follow-up.
Study quality
Methodological quality was assessed using the Cochrane
Collaboration’s risk of bias tool by two independent research-
ers (EB and KH).37 A third independent researcher completed
the risk of bias tool for one of the included studies because
of a conflict of interest for KH.38 The categories assessed
were sequence generation, allocation concealment, blinding
of participants and staff, blinding of outcome assessment,
incomplete outcome data, selective outcome reporting, and
other sources of bias.37 Risk of bias was assessed to be “low
risk”, “unclear risk”, or “high risk” of bias.37
Data analysis
The studies are described according to their characteristics,
interventions utilized, outcome measures, adherence to
exercise interventions, study quality, and effectiveness of
the intervention programs.
Table 1 Search strategy (according to Medline terminology)
1 cognitive* impair* ti,ab.
2 cognition disorders/[MeSH]
3 dementia/[MeSH]
4 1 or 2 or 3
5 physical activity ti,ab.
6 physical active* ti,ab.
7 physical exerc* ti,ab.
8 exercise* ti,ab.
9 5 or 6 or 7 or 8
10 community* ti,ab.
11 home ti,ab.
12 10 or 11
13 fall* ti,ab.
14 accidental fall/[MeSH]
15 fall* prevent* ti,ab.
16 13 or 14 or 15
17 4 and 9 and 12 and 16
Clinical Interventions in Aging 2015:10submit your manuscript | www.dovepress.com
Dovepress
Dovepress
424
Burton et al
Three continuous outcomes (mean falls, step test, and
physiological profile assessment [PPA]) and one dichoto-
mous outcome (faller status [ie, faller versus non-faller]) were
included in the quantitative analyses. The mean difference
(MD) and 95% confidence intervals (CI) were calculated
for continuous outcomes, whereas risk ratio (RR) and 95%
CI were calculated for dichotomous outcomes. The Review
Manager (RevMan) version 5.2 was used to conduct the anal-
yses and generate the forest plots, and a fixed-effect model
was applied. Heterogeneity was assessed by the I2 statistic
and by visual inspection of the forest plots. For continuous
outcomes, the results of homogeneous studies were subjected
to meta-analysis using the inverse variance DerSimonian and
Laird method.39 For faller status (ie, dichotomous outcome),
the results of homogeneous studies were meta-analyzed using
the Mantel–Haenszel’s fixed effects model.40 Two-sided
value of P,0.05 was the statistically significant level set
for all analyses.
In instances where data provided in the published papers
were insufficient for the meta-analysis, the corresponding
authors for the RCT papers were contacted and asked for
the total number of falls pre and post intervention, the mean
number of falls per group at post intervention, the standard
deviation, the number of fallers per group (post intervention),
and the number of participants for both groups at pre and
post data collection.
Results
Study selection
The search strategy yielded 2,279 articles from six databases.
Duplicate articles within each database were removed,
leaving 446 articles. The 446 articles were then combined
into an excel spreadsheet, with duplicates again removed,
resulting in 286 remaining articles. Articles were then
screened on the basis of title, with 179 articles excluded (rea-
sons for exclusion are reported in Figure 1). The 107 articles
were then checked, and 79 articles were excluded based
on the abstracts. The full manuscripts of the 28 remaining
articles were then examined in detail, and 24 were found not
to meet the inclusion criteria. A total of four articles were
left for inclusion in the review. Three of these were RCTs
and were included in the meta-analyses.
Study characteristics
Three of the four articles included in the review were
RCTs.38,41,42 The fourth was a single-group pre- and post-test
pilot study.43 As presented in Table 2, sample sizes across the
studies ranged from 2242 to 210 participants.41 Three-hundred
and thirty-six participants completed pre-testing in the four
studies, but only 243 completed post-testing (72.3%). The
largest dropout rate was found for Mackintosh and Shep-
pard’s43 study, with half of the participants not continuing
across the 6-month study period. In contrast, Wesson et al42
only had one participant from the intervention group drop
out prior to completing the 12-week intervention (95.2%
completed the follow-up assessment).
All studies included MMSE scores of participants, with an
average score (and standard deviation) of 18.9 (5.5) across all
studies. There was little difference in MMSE scores between
the intervention groups (20.4 [5.1]) and controls (20.6 [5.0])
for the three RCTs.38,41,42 All studies reported the mean age
and standard deviation; the average age of the participants
was 79.8 (5.8) years.
Interventions
Interventions ranged between 3 months and 12 months, and
participants randomized to the intervention group were rec-
ommended to complete the exercises once a week,43 twice
a week,41 three times a week,42 or five times a week.38 The
exercise interventions took place in a group (or individual
assistance where required) at a facility41,43 or at home.38,41,42
Pitkälä et al’s41 study comprised three groups: group-based
exercise, home-based exercise, and usual care (control). Two
studies provided multifactorial programs, which included an
exercise component.42,43 Other interventions included in the
two studies were foot health, medication management, vision
assessments, walking aids and footwear issues,43 and home
hazard reduction.42 The exercise programs predominantly
concentrated on strength, balance, and mobility, and these
programs were established and supervised by physiothera-
pists, occupational therapists, or physiotherapy students who
were trained and supervised by physiotherapists. In two of
the studies,38,42 carers were actively involved in monitoring
and encouraging participation between therapist visits for
the assigned exercise program.
Participants in Mackintosh and Sheppard’s43 study under-
took lower limb strength exercises (hip abductor, knee exten-
sor, and ankle dorsiflexion, bilaterally) using velcro ankle
weights; balance exercises while standing, and walking was
based on time or distance. The falls risk assessment assisted
the physiotherapist to develop individual falls and injury
prevention plans for each participant. Pitkälä et al41 had two
exercise groups (home-based and group-based) with different
programs. The home exercise group was given individually
tailored exercise programs provided by a physiotherapist with
specialist dementia training and the exercises addressed the
Dovepress
Dovepress
424
Burton et al
Three continuous outcomes (mean falls, step test, and
physiological profile assessment [PPA]) and one dichoto-
mous outcome (faller status [ie, faller versus non-faller]) were
included in the quantitative analyses. The mean difference
(MD) and 95% confidence intervals (CI) were calculated
for continuous outcomes, whereas risk ratio (RR) and 95%
CI were calculated for dichotomous outcomes. The Review
Manager (RevMan) version 5.2 was used to conduct the anal-
yses and generate the forest plots, and a fixed-effect model
was applied. Heterogeneity was assessed by the I2 statistic
and by visual inspection of the forest plots. For continuous
outcomes, the results of homogeneous studies were subjected
to meta-analysis using the inverse variance DerSimonian and
Laird method.39 For faller status (ie, dichotomous outcome),
the results of homogeneous studies were meta-analyzed using
the Mantel–Haenszel’s fixed effects model.40 Two-sided
value of P,0.05 was the statistically significant level set
for all analyses.
In instances where data provided in the published papers
were insufficient for the meta-analysis, the corresponding
authors for the RCT papers were contacted and asked for
the total number of falls pre and post intervention, the mean
number of falls per group at post intervention, the standard
deviation, the number of fallers per group (post intervention),
and the number of participants for both groups at pre and
post data collection.
Results
Study selection
The search strategy yielded 2,279 articles from six databases.
Duplicate articles within each database were removed,
leaving 446 articles. The 446 articles were then combined
into an excel spreadsheet, with duplicates again removed,
resulting in 286 remaining articles. Articles were then
screened on the basis of title, with 179 articles excluded (rea-
sons for exclusion are reported in Figure 1). The 107 articles
were then checked, and 79 articles were excluded based
on the abstracts. The full manuscripts of the 28 remaining
articles were then examined in detail, and 24 were found not
to meet the inclusion criteria. A total of four articles were
left for inclusion in the review. Three of these were RCTs
and were included in the meta-analyses.
Study characteristics
Three of the four articles included in the review were
RCTs.38,41,42 The fourth was a single-group pre- and post-test
pilot study.43 As presented in Table 2, sample sizes across the
studies ranged from 2242 to 210 participants.41 Three-hundred
and thirty-six participants completed pre-testing in the four
studies, but only 243 completed post-testing (72.3%). The
largest dropout rate was found for Mackintosh and Shep-
pard’s43 study, with half of the participants not continuing
across the 6-month study period. In contrast, Wesson et al42
only had one participant from the intervention group drop
out prior to completing the 12-week intervention (95.2%
completed the follow-up assessment).
All studies included MMSE scores of participants, with an
average score (and standard deviation) of 18.9 (5.5) across all
studies. There was little difference in MMSE scores between
the intervention groups (20.4 [5.1]) and controls (20.6 [5.0])
for the three RCTs.38,41,42 All studies reported the mean age
and standard deviation; the average age of the participants
was 79.8 (5.8) years.
Interventions
Interventions ranged between 3 months and 12 months, and
participants randomized to the intervention group were rec-
ommended to complete the exercises once a week,43 twice
a week,41 three times a week,42 or five times a week.38 The
exercise interventions took place in a group (or individual
assistance where required) at a facility41,43 or at home.38,41,42
Pitkälä et al’s41 study comprised three groups: group-based
exercise, home-based exercise, and usual care (control). Two
studies provided multifactorial programs, which included an
exercise component.42,43 Other interventions included in the
two studies were foot health, medication management, vision
assessments, walking aids and footwear issues,43 and home
hazard reduction.42 The exercise programs predominantly
concentrated on strength, balance, and mobility, and these
programs were established and supervised by physiothera-
pists, occupational therapists, or physiotherapy students who
were trained and supervised by physiotherapists. In two of
the studies,38,42 carers were actively involved in monitoring
and encouraging participation between therapist visits for
the assigned exercise program.
Participants in Mackintosh and Sheppard’s43 study under-
took lower limb strength exercises (hip abductor, knee exten-
sor, and ankle dorsiflexion, bilaterally) using velcro ankle
weights; balance exercises while standing, and walking was
based on time or distance. The falls risk assessment assisted
the physiotherapist to develop individual falls and injury
prevention plans for each participant. Pitkälä et al41 had two
exercise groups (home-based and group-based) with different
programs. The home exercise group was given individually
tailored exercise programs provided by a physiotherapist with
specialist dementia training and the exercises addressed the

End of preview
Want to access all the pages? Upload your documents or become a member.
Related Documents
Effectiveness of Fall Prevention Programs in Nursing Homes: A Systematic Review and Meta-Analysislg...
|11
|8369
|400
The Effects of Exercise on Falls in Older Peoplelg...
|9
|9665
|32
Annotated Bibliographylg...
|10
|2466
|202