Clinical Investigations: Fall Prevention Programs in Nursing Homes
VerifiedAdded on 2022/10/04
|11
|8369
|400
Report
AI Summary
This report presents a systematic review and meta-analysis investigating the characteristics and effectiveness of fall prevention programs in nursing homes. The study analyzed 13 randomized controlled trials, evaluating single, multiple, and multifactorial interventions. The primary outcomes were the number of falls, fallers, and recurrent fallers. The meta-analysis revealed that multifactorial interventions significantly reduced falls and recurrent fallers, while single or multiple interventions did not show significant effects. Training and education components showed a harmful effect by increasing the number of falls. The research found that fall prevention interventions significantly reduced the number of recurrent fallers by 21%. The study emphasizes the importance of tailored, multifactorial approaches in preventing falls among nursing home residents, providing valuable insights for improving patient care and reducing fall-related injuries. This analysis contributes to evidence-based practice in geriatric care and the development of more effective fall prevention strategies.
CLINICAL INVESTIGATIONS
Characteristics and Effectiveness of Fall Prevention Programs
Nursing Homes: A Systematic Review and Meta-Analysis of
Randomized Controlled Trials
Ellen Vlaeyen, MSN,a Joke Coussement, MSN,a,b Greet Leysens, MSN,a Elisa Van der Elst, MSN,a
Kim Delbaere, MPT, PhD,c Dirk Cambier, MPT, PhD,d Kris Denhaerynck, MSN, PhD,e
Stefan Goemaere, MD,f Arlette Wertelaers, MD,g Fabienne Dobbels, PhD,a
Eddy Dejaeger, MD, PhD,h and Koen Milisen, MSN, PhD,a,h on behalf of the Center of Expertise
for Fall and Fracture Prevention Flanders
OBJECTIVES: To determine characteristics and effective-
ness of prevention programs on fall-related outcomes in a
defined setting.
DESIGN: Systematic review and meta-analysis.
SETTING: A clearly described subgroup of nursing homes
defined as residentialfacilities thatprovide 24-hour-a-day
surveillance,personalcare, and limited clinicalcare for
persons who are typically elderly and infirm.
PARTICIPANTS: Nursing home residents (N = 22,915).
MEASUREMENTS: The primary outcomes were number
of falls, fallers, and recurrent fallers.
RESULTS: Thirteen studies met the inclusion criteria.
Six fall prevention programswere single (one interven-
tion componentprovided to the residents),one was mul-
tiple (two or more intervention components not
customized to individualfall risk), and six were multi-
factorial(two or more intervention componentscustom-
ized to each resident’sfall risk). Meta-analysisfound
significantlyfewer recurrentfallers in the intervention
groups(4 studies,relative risk (RR) = 0.79,95% confi-
dence interval(CI) = 0.65–0.97)but no significanteffect
of the interventionon fallers (6 studies, RR = 0.97,
95% CI = 0.84–1.11) or falls (10 studies,RR = 0.93,
95% CI = 0.76–1.13).Multifactorialinterventions signifi-
cantly reduced falls (4 studies, RR = 0.67, 95%
CI = 0.55–0.82)and the numberof recurrentfallers (4
studies,RR = 0.79, CI = 0.65–0.97),whereassingle or
multiple interventionsdid not. Training and education
showed a significantharmful effect in the intervention
groups on the number of falls (2 studies, RR = 1.29,
95% CI = 1.23–1.36).
CONCLUSION: This meta-analysisfailed to reveal a
significant effect of fall prevention interventions on falls or
fallers but,for the firsttime,showed thatfall prevention
interventions significantly reduced the number of recurrent
fallers by 21%. J Am Geriatr Soc 63:211–221, 2015.
Key words: accidentalfalls; prevention;multifactorial
interventions;residentialaged care facilities; meta-
analysis
Nursing home residents have a high risk of falling. The
average fallincidence is estimated to be 1.6 falls per
bed per year,with almosthalf of residentsfalling more
than once a year.1–3 Falls in nursing homes often lead to
serious injuries,with for example,an estimated hip frac-
ture incidencerate of 4% annually.3–5 Previousstudies
showed that, within 1 year after a fall-related hip fracture,
12% of residents incur a new fracture,and 31% die as a
result.5,6 Apart from the physicalburden,falls often have
psychologicalconsequencessuch as fear of falling and
poor quality of life.Falls also have a significant economic
burden.7,8
The Prevention ofFalls Network Europe (ProFaNE)
taxonomy divides fall prevention programs into three types:
single programs, which include one intervention component
From theaDepartment of Public Health and Primary Care, Health Services
and Nursing Research, KU Leuven, Leuven, Belgium;bVzw Rusthuizen
Zusters van Berlaar, Berlaar, Belgium;cNeuroscience Research Australia,
University of New South Wales, Sydney, Australia;dRehabilitation
Sciences and Physiotherapy, Ghent University, Ghent, Belgium;eInstitute
of Nursing Science, University of Basel, Basel, Switzerland;fUnit for
Osteoporosis and Metabolic Bone Disease, Department of Rheumatology
and Endocrinology, Ghent University Hospital, Ghent, Belgium;gDomus
Medica, Society of Flemish General Practitioners, Antwerpen, Belgium;
and hDivision of Geriatric Medicine, University Hospitals Leuven, Leuven,
Belgium.
Address correspondence to Koen Milisen, KU Leuven, Department of
Public Health and Primary Care, Health Services and Nursing Research,
Kapucijnenvoer 35, 4th floor, P.B. 7001, Leuven 3000, Belgium.
E-mail: koen.milisen@med.kuleuven.be
DOI: 10.1111/jgs.13254
JAGS 63:211–221, 2015
© 2015, Copyright the Authors
Journal compilation © 2015, The American Geriatrics Society 0002-8614/15/$15.00
Characteristics and Effectiveness of Fall Prevention Programs
Nursing Homes: A Systematic Review and Meta-Analysis of
Randomized Controlled Trials
Ellen Vlaeyen, MSN,a Joke Coussement, MSN,a,b Greet Leysens, MSN,a Elisa Van der Elst, MSN,a
Kim Delbaere, MPT, PhD,c Dirk Cambier, MPT, PhD,d Kris Denhaerynck, MSN, PhD,e
Stefan Goemaere, MD,f Arlette Wertelaers, MD,g Fabienne Dobbels, PhD,a
Eddy Dejaeger, MD, PhD,h and Koen Milisen, MSN, PhD,a,h on behalf of the Center of Expertise
for Fall and Fracture Prevention Flanders
OBJECTIVES: To determine characteristics and effective-
ness of prevention programs on fall-related outcomes in a
defined setting.
DESIGN: Systematic review and meta-analysis.
SETTING: A clearly described subgroup of nursing homes
defined as residentialfacilities thatprovide 24-hour-a-day
surveillance,personalcare, and limited clinicalcare for
persons who are typically elderly and infirm.
PARTICIPANTS: Nursing home residents (N = 22,915).
MEASUREMENTS: The primary outcomes were number
of falls, fallers, and recurrent fallers.
RESULTS: Thirteen studies met the inclusion criteria.
Six fall prevention programswere single (one interven-
tion componentprovided to the residents),one was mul-
tiple (two or more intervention components not
customized to individualfall risk), and six were multi-
factorial(two or more intervention componentscustom-
ized to each resident’sfall risk). Meta-analysisfound
significantlyfewer recurrentfallers in the intervention
groups(4 studies,relative risk (RR) = 0.79,95% confi-
dence interval(CI) = 0.65–0.97)but no significanteffect
of the interventionon fallers (6 studies, RR = 0.97,
95% CI = 0.84–1.11) or falls (10 studies,RR = 0.93,
95% CI = 0.76–1.13).Multifactorialinterventions signifi-
cantly reduced falls (4 studies, RR = 0.67, 95%
CI = 0.55–0.82)and the numberof recurrentfallers (4
studies,RR = 0.79, CI = 0.65–0.97),whereassingle or
multiple interventionsdid not. Training and education
showed a significantharmful effect in the intervention
groups on the number of falls (2 studies, RR = 1.29,
95% CI = 1.23–1.36).
CONCLUSION: This meta-analysisfailed to reveal a
significant effect of fall prevention interventions on falls or
fallers but,for the firsttime,showed thatfall prevention
interventions significantly reduced the number of recurrent
fallers by 21%. J Am Geriatr Soc 63:211–221, 2015.
Key words: accidentalfalls; prevention;multifactorial
interventions;residentialaged care facilities; meta-
analysis
Nursing home residents have a high risk of falling. The
average fallincidence is estimated to be 1.6 falls per
bed per year,with almosthalf of residentsfalling more
than once a year.1–3 Falls in nursing homes often lead to
serious injuries,with for example,an estimated hip frac-
ture incidencerate of 4% annually.3–5 Previousstudies
showed that, within 1 year after a fall-related hip fracture,
12% of residents incur a new fracture,and 31% die as a
result.5,6 Apart from the physicalburden,falls often have
psychologicalconsequencessuch as fear of falling and
poor quality of life.Falls also have a significant economic
burden.7,8
The Prevention ofFalls Network Europe (ProFaNE)
taxonomy divides fall prevention programs into three types:
single programs, which include one intervention component
From theaDepartment of Public Health and Primary Care, Health Services
and Nursing Research, KU Leuven, Leuven, Belgium;bVzw Rusthuizen
Zusters van Berlaar, Berlaar, Belgium;cNeuroscience Research Australia,
University of New South Wales, Sydney, Australia;dRehabilitation
Sciences and Physiotherapy, Ghent University, Ghent, Belgium;eInstitute
of Nursing Science, University of Basel, Basel, Switzerland;fUnit for
Osteoporosis and Metabolic Bone Disease, Department of Rheumatology
and Endocrinology, Ghent University Hospital, Ghent, Belgium;gDomus
Medica, Society of Flemish General Practitioners, Antwerpen, Belgium;
and hDivision of Geriatric Medicine, University Hospitals Leuven, Leuven,
Belgium.
Address correspondence to Koen Milisen, KU Leuven, Department of
Public Health and Primary Care, Health Services and Nursing Research,
Kapucijnenvoer 35, 4th floor, P.B. 7001, Leuven 3000, Belgium.
E-mail: koen.milisen@med.kuleuven.be
DOI: 10.1111/jgs.13254
JAGS 63:211–221, 2015
© 2015, Copyright the Authors
Journal compilation © 2015, The American Geriatrics Society 0002-8614/15/$15.00
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
provided to all residents (e.g., supervised exercises); multiple
programs, which include two or more intervention compo-
nents provided to all residents (e.g., supervised exercise and
staff training);and multifactorialprograms,which include
two or more customized intervention components that tar-
get each resident’s fall risk profile.9 No conclusive evidence
exists on the effectiveness offall prevention programs in
nursing homes, partly because of differing study
approaches.10–16 For example,five of sevenpublished
reviewsused a narrativeapproach,10–14 one of which
reviewed only multifactorialinterventions.13 Two recent
systematic reviews15,16 used a meta-analyticalmethod and
reported no effectof any type of intervention,with the
exception of one single intervention that showed improve-
ment in number of falls and fallers after supplementing resi-
dents’ diets with vitamin D.15
These reviews did not distinguish between fallers and
recurrentfallers.This is a missed opportunity,given the
high frequency ofrecurrentfallers and their influence on
the total numberof falls. Furthermore,previousreviews
compared studies thatused heterogeneous groups ofresi-
dents from various care settings that had major differences
in care intensity or used vague terminology to define the
care settings (e.g.,residentialor nursing care facilities,13,15
nursing homes,10–12 care homes,16 and long-term care
facilities14). This could partly explain why evidenceon
effective fallprevention strategies in nursing homes is less
conclusive than reviewsspecifically focusing on a more-
clear-cut delineatedpopulation of community-dwelling
elderly adults.17
The current review aimed to determine the characteris-
tics and effectiveness of single, multiple, and multifactorial
fall prevention programson the numberof falls, fallers,
and recurrentfallers in older personswho permanently
reside in a nursing home.A nursing home was defined as
“a residentialfacility thatprovides 24-hour-a-day surveil-
lance,personalcare,and limited clinicalcare for persons
who are typically elderly and infirm” and excluded post-
hospitalskilled nursing care,rehabilitation,and long-term
care for younger people with illnesses,injuries,functional
disabilities, or cognitive impairment.7
METHODS
The review protocol was registeredon PROSPERO
(CRD42011001687)18 and conducted in concordance with
PRISMA guidelines.19,20
Search Strategy
A systematic literature search wasconducted in multiple
databases (MEDLINE,EMBASE, Cochrane CentralRegis-
ter of Controlled Trials,PEDro, CINAHL, SportDiscus),
restricting the search to articlespublished from database
inception to September2013. Depending on the selected
database,Medical SubjectHeadings,a thesaurus,or free
text was combined with theBoolean operators“AND/
OR” to build a search strategy.Search terms were “acci-
dental falls,” “falls,” “faller*,” “aged,” “older,” “elderly,”
“nursing homes,” “residential facilities,” “long-term care,”
“institutionalization,” “residential*,” and “prevention and
control.”
Relevantstudieswere identifiedusing three steps.
First, two independentreviewers(EV, JC) conducted an
initial study selection based on title and abstract.Second,
three reviewers (EV,JC, KM) obtained and examined full-
text copies ofall articles meeting initialselection criteria.
Disagreementwas resolved through discussion with three
additional reviewers (GL, EVdE, ED). Third, reference lists
of articles meeting the inclusion criteria were screened for
additional relevant papers.
Inclusion Criteria
Studies had to meet the following criteria.
Setting
The study had to be conducted in a nursing home,as
defined previously;7 other kinds of residential care facilities
were excluded. If the setting was in doubt, an attempt was
made to contact the authors for clarification. When studies
included nursing homes and other facilities (e.g.,assisted
living facilities),the study was included only when sepa-
rate results for the nursing home population were available
in the article.
Design
The study had to be an original or a priori secondary
analysisof individual-levelor cluster randomized con-
trolled trials (RCT).
Objective
The intervention had to include single,multiple,or multi-
factorial fall preventionprogramsdesignedto prevent
falls.
Outcomes
The study had to examine intervention effecton number
of falls, fallers, or recurrentfallers. The term “faller”
included all residents sustaining at least one fall during the
intervention or follow-up period.In the same way,recur-
rent fallers were defined asresidentssustaining two or
more falls.
Duration
The duration from the start of the intervention (including
follow-up) had to be 6 months or longer.
Language
Only publicationsin English, French,German,or Dutch
were considered.
Risk of Bias Assessment
The methodologicalquality of each study wasassessed
using the Cochrane methodologicalquality assessment
scheme(Table 1).21 One loss-to-follow-up criterion was
added and evaluated according to the question:“Were the
majority of participants stillin the sample atthe end of
the study?” Majority was operationally defined as 80% or
higher.
212 VLAEYEN ET AL. FEBRUARY 2015–VOL. 63, NO. 2 JAGS
programs, which include two or more intervention compo-
nents provided to all residents (e.g., supervised exercise and
staff training);and multifactorialprograms,which include
two or more customized intervention components that tar-
get each resident’s fall risk profile.9 No conclusive evidence
exists on the effectiveness offall prevention programs in
nursing homes, partly because of differing study
approaches.10–16 For example,five of sevenpublished
reviewsused a narrativeapproach,10–14 one of which
reviewed only multifactorialinterventions.13 Two recent
systematic reviews15,16 used a meta-analyticalmethod and
reported no effectof any type of intervention,with the
exception of one single intervention that showed improve-
ment in number of falls and fallers after supplementing resi-
dents’ diets with vitamin D.15
These reviews did not distinguish between fallers and
recurrentfallers.This is a missed opportunity,given the
high frequency ofrecurrentfallers and their influence on
the total numberof falls. Furthermore,previousreviews
compared studies thatused heterogeneous groups ofresi-
dents from various care settings that had major differences
in care intensity or used vague terminology to define the
care settings (e.g.,residentialor nursing care facilities,13,15
nursing homes,10–12 care homes,16 and long-term care
facilities14). This could partly explain why evidenceon
effective fallprevention strategies in nursing homes is less
conclusive than reviewsspecifically focusing on a more-
clear-cut delineatedpopulation of community-dwelling
elderly adults.17
The current review aimed to determine the characteris-
tics and effectiveness of single, multiple, and multifactorial
fall prevention programson the numberof falls, fallers,
and recurrentfallers in older personswho permanently
reside in a nursing home.A nursing home was defined as
“a residentialfacility thatprovides 24-hour-a-day surveil-
lance,personalcare,and limited clinicalcare for persons
who are typically elderly and infirm” and excluded post-
hospitalskilled nursing care,rehabilitation,and long-term
care for younger people with illnesses,injuries,functional
disabilities, or cognitive impairment.7
METHODS
The review protocol was registeredon PROSPERO
(CRD42011001687)18 and conducted in concordance with
PRISMA guidelines.19,20
Search Strategy
A systematic literature search wasconducted in multiple
databases (MEDLINE,EMBASE, Cochrane CentralRegis-
ter of Controlled Trials,PEDro, CINAHL, SportDiscus),
restricting the search to articlespublished from database
inception to September2013. Depending on the selected
database,Medical SubjectHeadings,a thesaurus,or free
text was combined with theBoolean operators“AND/
OR” to build a search strategy.Search terms were “acci-
dental falls,” “falls,” “faller*,” “aged,” “older,” “elderly,”
“nursing homes,” “residential facilities,” “long-term care,”
“institutionalization,” “residential*,” and “prevention and
control.”
Relevantstudieswere identifiedusing three steps.
First, two independentreviewers(EV, JC) conducted an
initial study selection based on title and abstract.Second,
three reviewers (EV,JC, KM) obtained and examined full-
text copies ofall articles meeting initialselection criteria.
Disagreementwas resolved through discussion with three
additional reviewers (GL, EVdE, ED). Third, reference lists
of articles meeting the inclusion criteria were screened for
additional relevant papers.
Inclusion Criteria
Studies had to meet the following criteria.
Setting
The study had to be conducted in a nursing home,as
defined previously;7 other kinds of residential care facilities
were excluded. If the setting was in doubt, an attempt was
made to contact the authors for clarification. When studies
included nursing homes and other facilities (e.g.,assisted
living facilities),the study was included only when sepa-
rate results for the nursing home population were available
in the article.
Design
The study had to be an original or a priori secondary
analysisof individual-levelor cluster randomized con-
trolled trials (RCT).
Objective
The intervention had to include single,multiple,or multi-
factorial fall preventionprogramsdesignedto prevent
falls.
Outcomes
The study had to examine intervention effecton number
of falls, fallers, or recurrentfallers. The term “faller”
included all residents sustaining at least one fall during the
intervention or follow-up period.In the same way,recur-
rent fallers were defined asresidentssustaining two or
more falls.
Duration
The duration from the start of the intervention (including
follow-up) had to be 6 months or longer.
Language
Only publicationsin English, French,German,or Dutch
were considered.
Risk of Bias Assessment
The methodologicalquality of each study wasassessed
using the Cochrane methodologicalquality assessment
scheme(Table 1).21 One loss-to-follow-up criterion was
added and evaluated according to the question:“Were the
majority of participants stillin the sample atthe end of
the study?” Majority was operationally defined as 80% or
higher.
212 VLAEYEN ET AL. FEBRUARY 2015–VOL. 63, NO. 2 JAGS
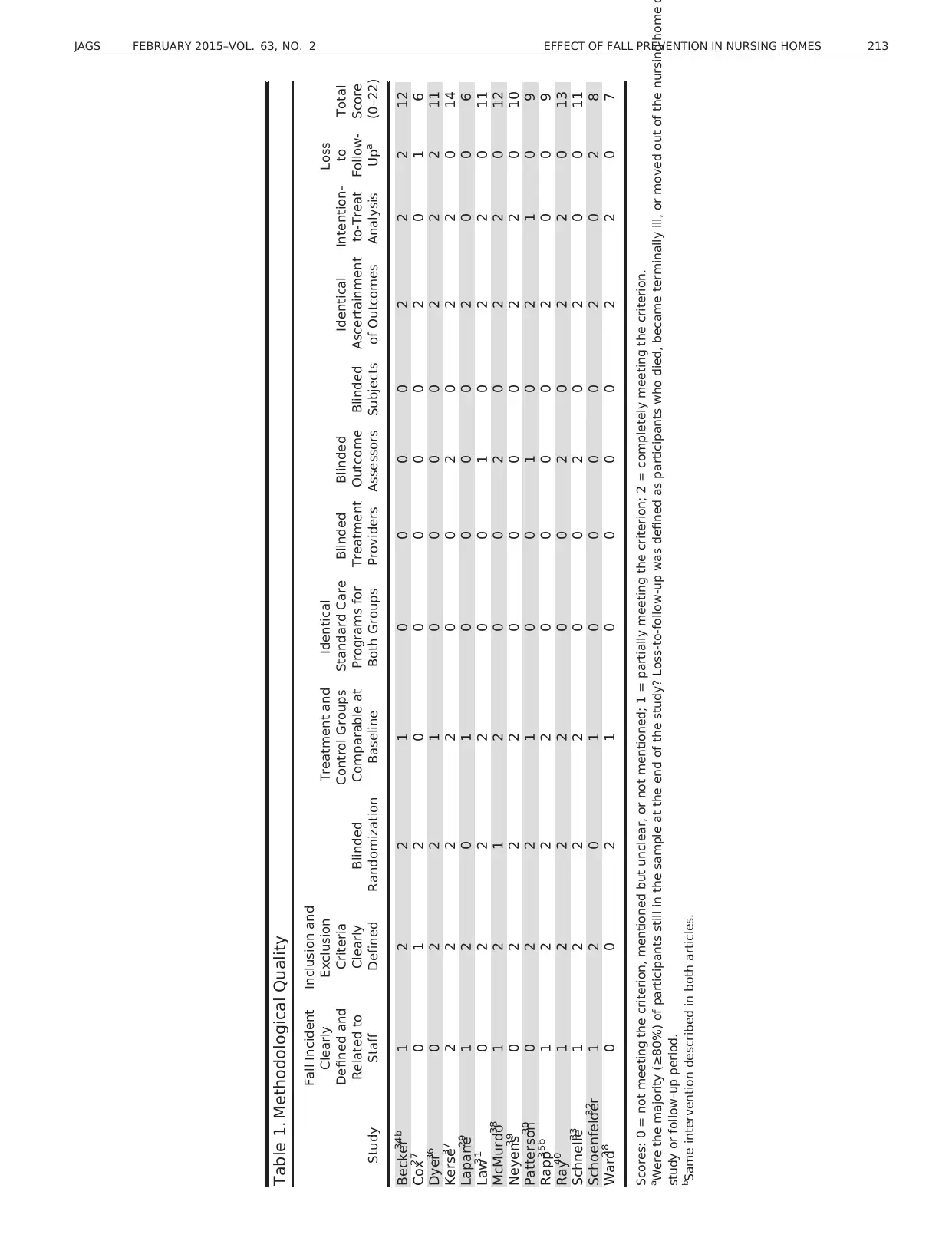
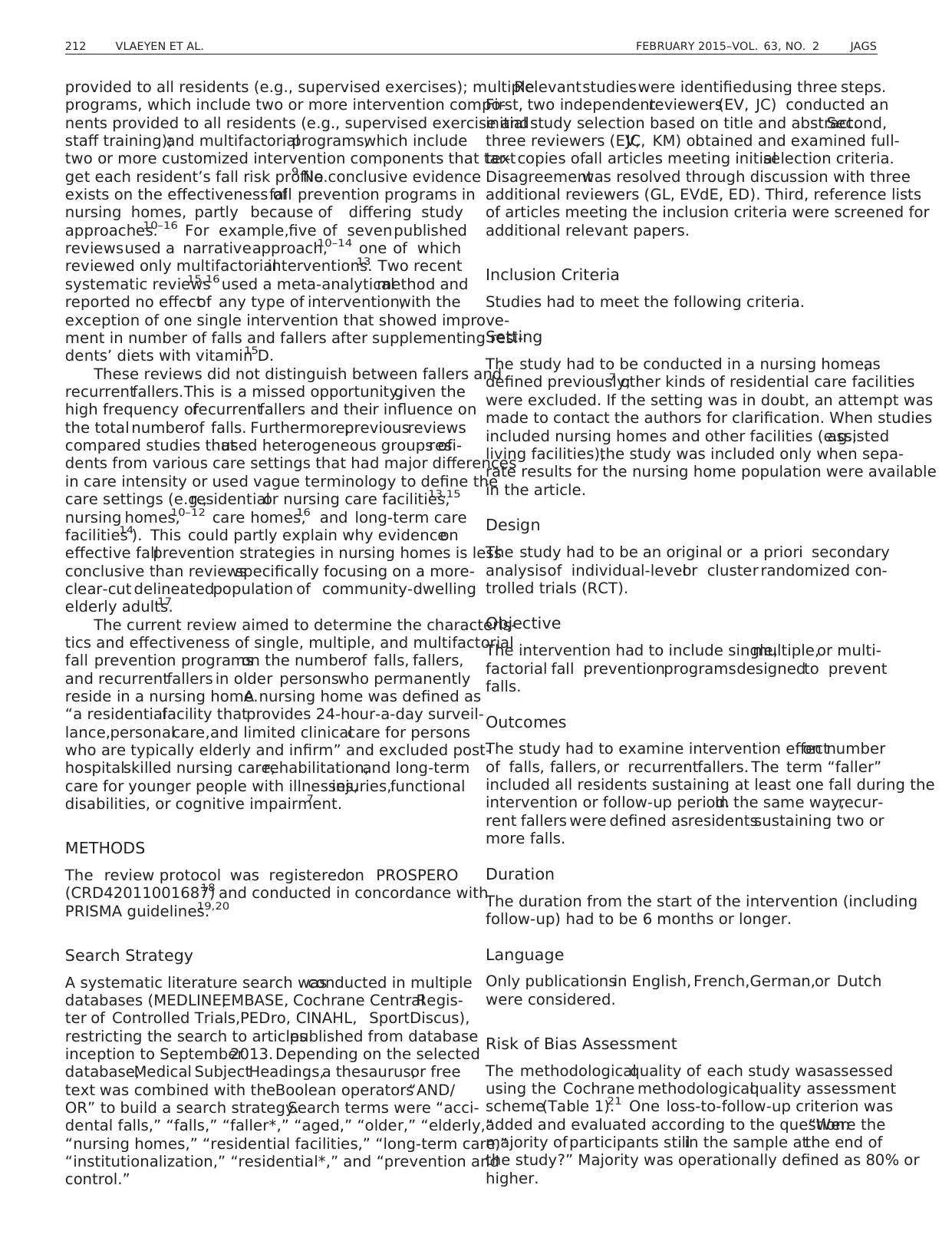
Table 1. Methodological Quality
Study
Fall Incident
Clearly
Defined and
Related to
Staff
Inclusion and
Exclusion
Criteria
Clearly
Defined
Blinded
Randomization
Treatment and
Control Groups
Comparable at
Baseline
Identical
Standard Care
Programs for
Both Groups
Blinded
Treatment
Providers
Blinded
Outcome
Assessors
Blinded
Subjects
Identical
Ascertainment
of Outcomes
Intention-
to-Treat
Analysis
Loss
to
Follow-
Upa
Total
Score
(0–22)
Becker34b 1 2 2 1 0 0 0 0 2 2 2 12
Cox27 0 1 2 0 0 0 0 0 2 0 1 6
Dyer36 0 2 2 1 0 0 0 0 2 2 2 11
Kerse37 2 2 2 2 0 0 2 0 2 2 0 14
Lapane29 1 2 0 1 0 0 0 0 2 0 0 6
Law31 0 2 2 2 0 0 1 0 2 2 0 11
McMurdo38 1 2 1 2 0 0 2 0 2 2 0 12
Neyens39 0 2 2 2 0 0 0 0 2 2 0 10
Patterson30 0 2 2 1 0 0 1 0 2 1 0 9
Rapp35b 1 2 2 2 0 0 0 0 2 0 0 9
Ray40 1 2 2 2 0 0 2 0 2 2 0 13
Schnelle33 1 2 2 2 0 0 2 0 2 0 0 11
Schoenfelder32 1 2 0 1 0 0 0 0 2 0 2 8
Ward28 0 0 2 1 0 0 0 0 2 2 0 7
Scores: 0 = not meeting the criterion, mentioned but unclear, or not mentioned; 1 = partially meeting the criterion; 2 = completely meeting the criterion.
a
Were the majority (≥80%) of participants still in the sample at the end of the study? Loss-to-follow-up was defined as participants who died, became terminally ill, or moved out of the nursing home d
study or follow-up period.
b
Same intervention described in both articles.
JAGS FEBRUARY 2015–VOL. 63, NO. 2 EFFECT OF FALL PREVENTION IN NURSING HOMES 213
Study
Fall Incident
Clearly
Defined and
Related to
Staff
Inclusion and
Exclusion
Criteria
Clearly
Defined
Blinded
Randomization
Treatment and
Control Groups
Comparable at
Baseline
Identical
Standard Care
Programs for
Both Groups
Blinded
Treatment
Providers
Blinded
Outcome
Assessors
Blinded
Subjects
Identical
Ascertainment
of Outcomes
Intention-
to-Treat
Analysis
Loss
to
Follow-
Upa
Total
Score
(0–22)
Becker34b 1 2 2 1 0 0 0 0 2 2 2 12
Cox27 0 1 2 0 0 0 0 0 2 0 1 6
Dyer36 0 2 2 1 0 0 0 0 2 2 2 11
Kerse37 2 2 2 2 0 0 2 0 2 2 0 14
Lapane29 1 2 0 1 0 0 0 0 2 0 0 6
Law31 0 2 2 2 0 0 1 0 2 2 0 11
McMurdo38 1 2 1 2 0 0 2 0 2 2 0 12
Neyens39 0 2 2 2 0 0 0 0 2 2 0 10
Patterson30 0 2 2 1 0 0 1 0 2 1 0 9
Rapp35b 1 2 2 2 0 0 0 0 2 0 0 9
Ray40 1 2 2 2 0 0 2 0 2 2 0 13
Schnelle33 1 2 2 2 0 0 2 0 2 0 0 11
Schoenfelder32 1 2 0 1 0 0 0 0 2 0 2 8
Ward28 0 0 2 1 0 0 0 0 2 2 0 7
Scores: 0 = not meeting the criterion, mentioned but unclear, or not mentioned; 1 = partially meeting the criterion; 2 = completely meeting the criterion.
a
Were the majority (≥80%) of participants still in the sample at the end of the study? Loss-to-follow-up was defined as participants who died, became terminally ill, or moved out of the nursing home d
study or follow-up period.
b
Same intervention described in both articles.
JAGS FEBRUARY 2015–VOL. 63, NO. 2 EFFECT OF FALL PREVENTION IN NURSING HOMES 213
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

Five reviewers (EV,JC, KD, ED, KM) independently
scored methodologicalquality on a scale ranging from 0
to 2, depending on whether the criterion was not fulfilled
or not mentioned (0),partially met (1),or completely met
(2). The totalscore ranged between 0 and 22,with higher
scores indicating better quality. Disagreement was resolved
through discussion and consensus.
Data Synthesis and Analysis
Data were synthesized to collate and summarize individual
study results.One reviewer (EV) collected data on charac-
teristics and effectiveness ofthe fall prevention programs.
Two reviewers (GL, EV & E) independently confirmed the
accuracy ofthe data synthesis.The ProFaNE taxonomy
for fall prevention interventions was used to classify and
describe the intervention programs.9 The programswere
categorized according to the ProFaNE taxonomy: interven-
tion type (single,multiple,or multifactorial) and interven-
tion component(e.g.,exercise,medication).9 Effectiveness
was classified according to outcome.For number offalls,
the relative risk offalls per residentyears was calculated
(ratio of the number of falls per resident year in the inter-
vention group to number offalls per residentyear in the
control group). For number of fallers and recurrent fallers,
the relativerisk was calculated (ratio ofproportion of
(recurrent)fallersin intervention group to corresponding
proportion in control group).
Effect size pooling was followed by regression analyses
using a random effectsapproach.22 Publication biaswas
checked using the trim and fillmethod,which alertsfor
publication bias ifmore than three studies on the funnel
plot are estimated to be concealed (assuming b > 0.80 and
a = 0.05).23,24 Heterogeneityof variance tests were
used to examinewhetherbetween-study variability was
significantly differentfrom 0 using weighted error sum of
squares Q.25 Calculated I² parameters reflected the propor-
tion of between-study variability to total variability.26
An a priori subgroup analysis was conducted accord-
ing to ProFaNE intervention type (single,multiple,multi-
factorial) and to determineany possible effects the
intervention mighthave had on residentswith dementia.
For the latter analysis, dementia was converted into a cate-
gorical variable,based on the methodology thatOliver
and colleagues used.16 Studies were categorized into three
groups ranging from 1 to 3 according to the prevalence of
dementia,with 1 being assigned to studies with less than
40% prevalence,2 being assigned to studies with a preva-
lence between 40% to 69%, and 3 being assigned to stud-
ies with 70% or more of residentswith dementia being
included in the study.Studies with an unspecified number
of participants with dementia were excluded from the sub-
group analysis.Regression analyseswere conducted to
determinewhetherdementia prevalencepredicted effect
size in this subgroup analysis.
RESULTS
Selected Studies
Figure 1 summarizes the results ofthe differentsteps for
identifying appropriatearticlesfor review.19,20 Fourteen
articles, describing 13 studies, met the inclusion criteria.27–40
Two studies34,35 were combined as one study in the meta-
analysis because they reported data on the same cohort of
individuals.
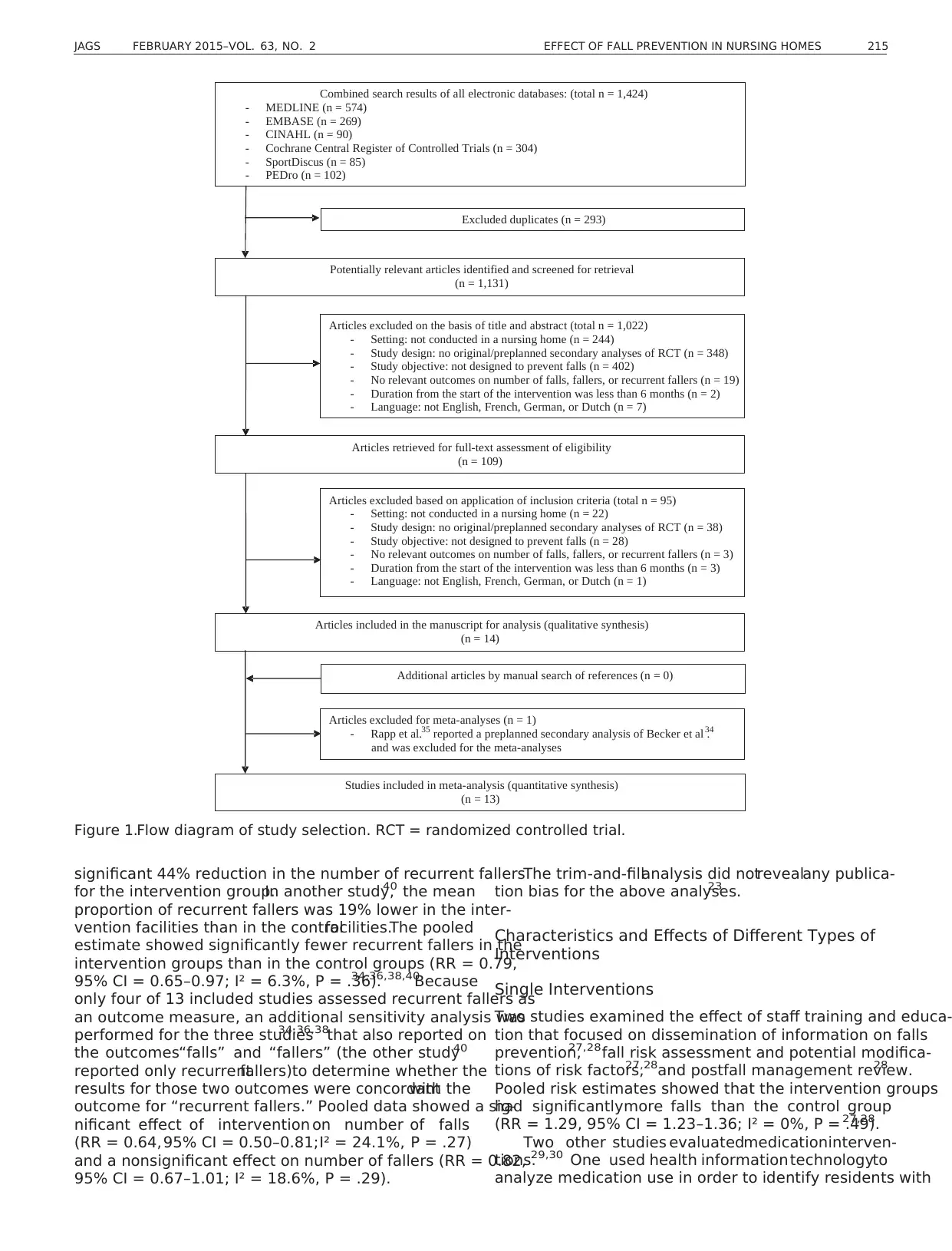
Risk of Bias Assessment
Overallquality scores ranged from 6 to 14 (Table 1).The
definition of a fall was reported in eight studies,29,32–
35,37,38,40
but in only one study was the definition clearly
explained to the staffcollecting and reporting the data.37
Inclusion and exclusion criteria were clearly defined in all
but two studies.27,28 None of the included studieshad
identical standard care programs for both intervention and
control groups, neither did they employ treatment blinding
for the treatment providers or participants. Outcome asses-
sors were blinded in fourstudies.33,37,38,40Eight studies
used intention-to-treatanalysis.28,31,34,36–40
The majority
of participants were stillin the sample atthe end ofthe
study in three studies.32,34,36
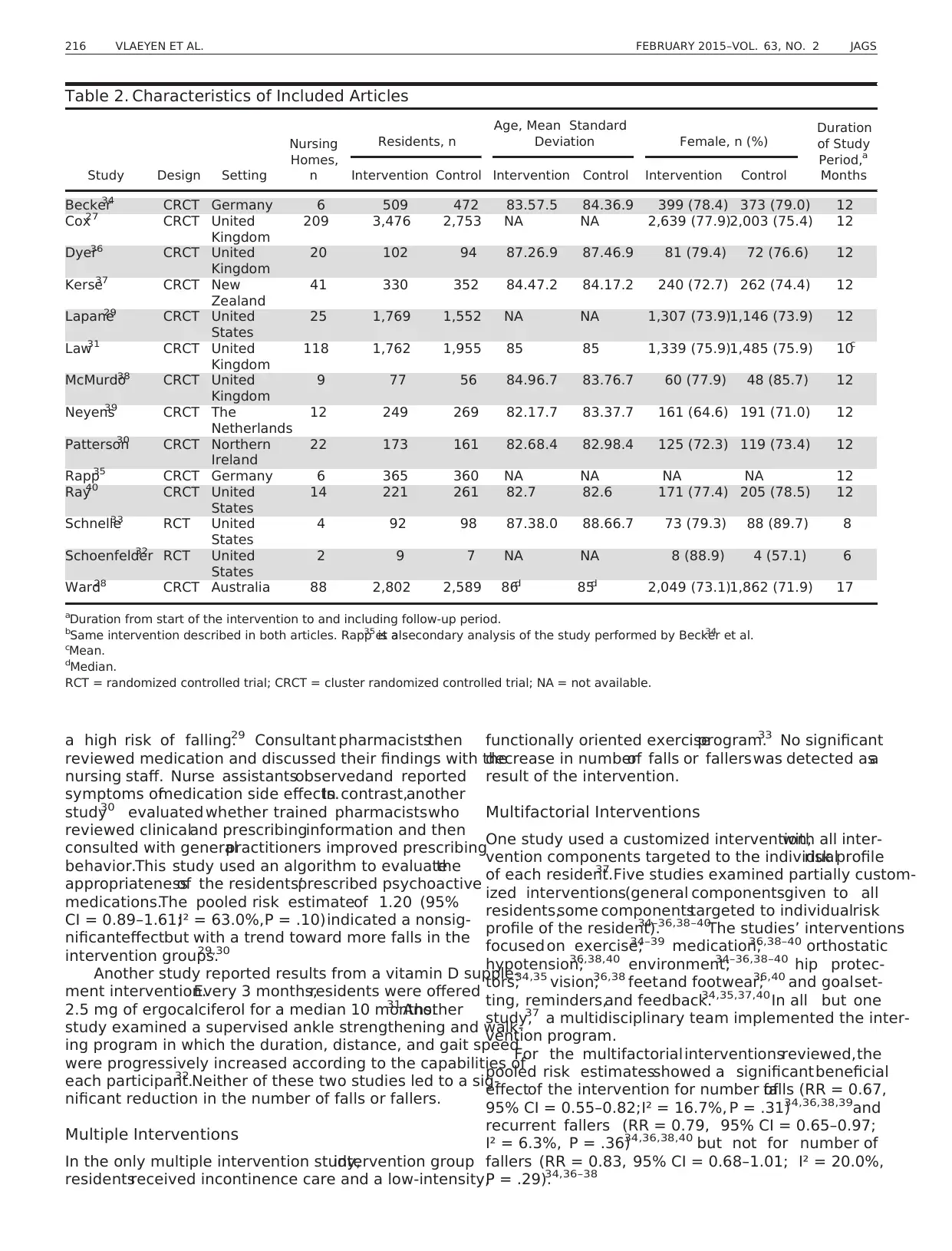
Study Characteristics
Seven studieswere conducted in Europe,27,30,31,34–36,38,39
four of which were in the United Kingdom.27,31,36,38
Four
were conducted in the United States29,32,33,40and two in
Australia/Oceania28,37 (Table 2). Follow-up ranged from
6 to 17 months. Two studieswere categorized asbeing
individualRCTs,32,33and 12 were cluster RCTs.27–31,34–40
With regard to ProFaNE intervention type,there were six
single,27–32 one multiple,33 and six multifactorial34–40 fall
prevention programs (Table 3).The included articles had
22,915 residents,with an overall mean age range of82
to 88.
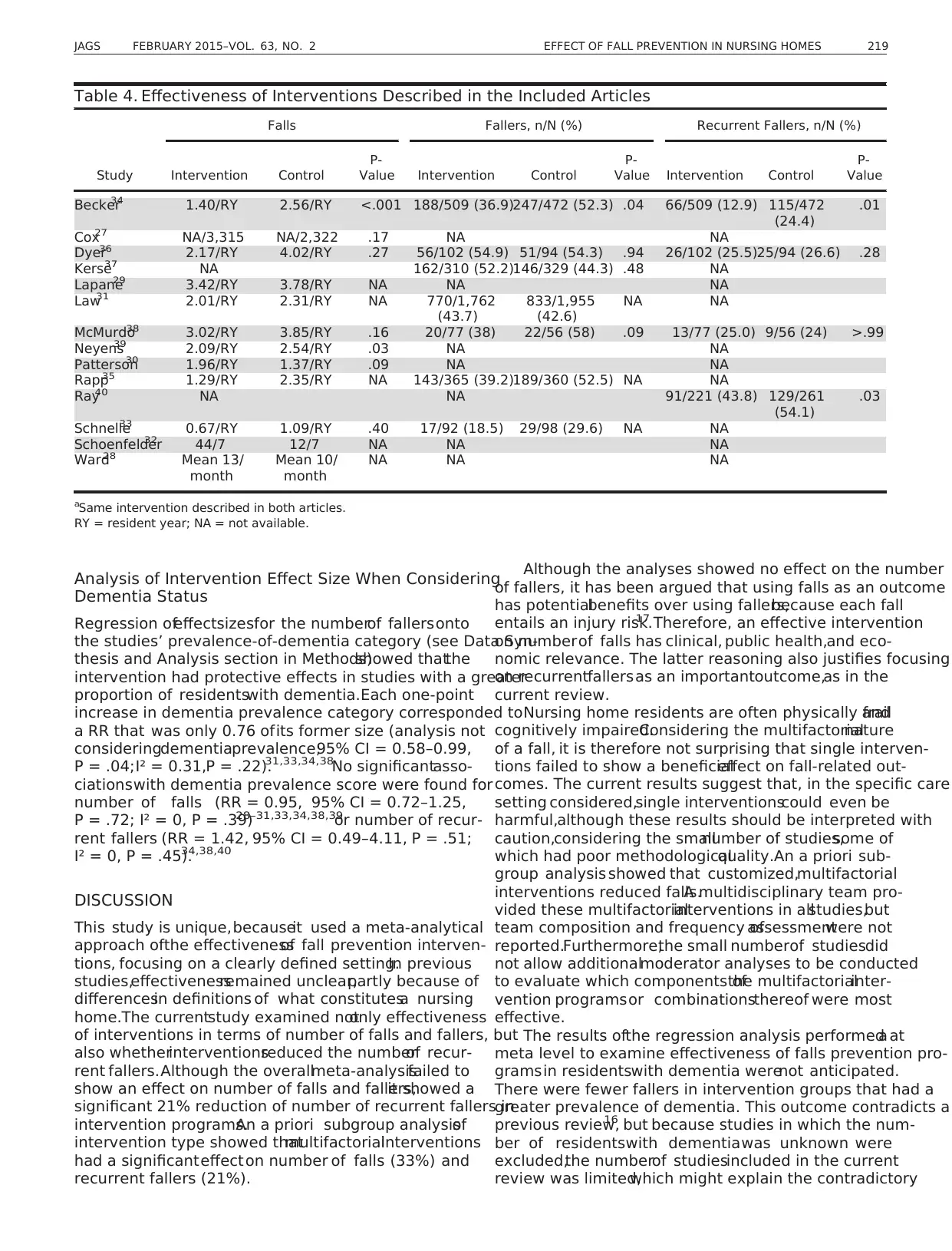
Overall Effects on Number of Falls, Fallers, and
Recurrent Fallers
The number of falls was reported in 12 studies
(Table 4).27–36,38,39In nine studies,the intervention and
control groupsdid not differ significantly in numberof
falls.27–33,36,38Two multifactorial studies34,39 showed a
significant decrease in falls of 36% and 45%,respectively,
over a 12-month period for the intervention groups.An a
priori secondarysubgroup analysis35 of one study34
showed thatthe effectwas only significantin cognitively
impaired residents(relative risk (RR) = 0.49,95% confi-
denceinterval (CI) = 0.35–0.69)and not in cognitively
intact residents (hazard rate (HR) = 0.91, 95% CI = 0.68–
1.22). Pooled data from 10 studies showed no effect
on number of falls (RR = 0.93, 95% CI = 0.76–1.13;
I² = 89.8%, P < .001).27–31,33,34,36,38,39
Seven studies assessed the number of fallers as an out-
come measure,31,33–38of which two multifactorialstudies
showed significantly fewer fallers in the intervention group
than in the control group. These two studies reported
25%34 and 30%35 fewer fallers,although the pooled risk
estimatesfailed to demonstratea beneficialeffect of
the intervention on numberof fallers (RR = 0.97,95%
CI = 0.84–1.11; I² = 47.9%, P = .09).31,33,34,36–38
The number ofrecurrentfallers was assessed in four
multifactorialstudies.34,36,38,40One study34 described a
214 VLAEYEN ET AL. FEBRUARY 2015–VOL. 63, NO. 2 JAGS
scored methodologicalquality on a scale ranging from 0
to 2, depending on whether the criterion was not fulfilled
or not mentioned (0),partially met (1),or completely met
(2). The totalscore ranged between 0 and 22,with higher
scores indicating better quality. Disagreement was resolved
through discussion and consensus.
Data Synthesis and Analysis
Data were synthesized to collate and summarize individual
study results.One reviewer (EV) collected data on charac-
teristics and effectiveness ofthe fall prevention programs.
Two reviewers (GL, EV & E) independently confirmed the
accuracy ofthe data synthesis.The ProFaNE taxonomy
for fall prevention interventions was used to classify and
describe the intervention programs.9 The programswere
categorized according to the ProFaNE taxonomy: interven-
tion type (single,multiple,or multifactorial) and interven-
tion component(e.g.,exercise,medication).9 Effectiveness
was classified according to outcome.For number offalls,
the relative risk offalls per residentyears was calculated
(ratio of the number of falls per resident year in the inter-
vention group to number offalls per residentyear in the
control group). For number of fallers and recurrent fallers,
the relativerisk was calculated (ratio ofproportion of
(recurrent)fallersin intervention group to corresponding
proportion in control group).
Effect size pooling was followed by regression analyses
using a random effectsapproach.22 Publication biaswas
checked using the trim and fillmethod,which alertsfor
publication bias ifmore than three studies on the funnel
plot are estimated to be concealed (assuming b > 0.80 and
a = 0.05).23,24 Heterogeneityof variance tests were
used to examinewhetherbetween-study variability was
significantly differentfrom 0 using weighted error sum of
squares Q.25 Calculated I² parameters reflected the propor-
tion of between-study variability to total variability.26
An a priori subgroup analysis was conducted accord-
ing to ProFaNE intervention type (single,multiple,multi-
factorial) and to determineany possible effects the
intervention mighthave had on residentswith dementia.
For the latter analysis, dementia was converted into a cate-
gorical variable,based on the methodology thatOliver
and colleagues used.16 Studies were categorized into three
groups ranging from 1 to 3 according to the prevalence of
dementia,with 1 being assigned to studies with less than
40% prevalence,2 being assigned to studies with a preva-
lence between 40% to 69%, and 3 being assigned to stud-
ies with 70% or more of residentswith dementia being
included in the study.Studies with an unspecified number
of participants with dementia were excluded from the sub-
group analysis.Regression analyseswere conducted to
determinewhetherdementia prevalencepredicted effect
size in this subgroup analysis.
RESULTS
Selected Studies
Figure 1 summarizes the results ofthe differentsteps for
identifying appropriatearticlesfor review.19,20 Fourteen
articles, describing 13 studies, met the inclusion criteria.27–40
Two studies34,35 were combined as one study in the meta-
analysis because they reported data on the same cohort of
individuals.
Risk of Bias Assessment
Overallquality scores ranged from 6 to 14 (Table 1).The
definition of a fall was reported in eight studies,29,32–
35,37,38,40
but in only one study was the definition clearly
explained to the staffcollecting and reporting the data.37
Inclusion and exclusion criteria were clearly defined in all
but two studies.27,28 None of the included studieshad
identical standard care programs for both intervention and
control groups, neither did they employ treatment blinding
for the treatment providers or participants. Outcome asses-
sors were blinded in fourstudies.33,37,38,40Eight studies
used intention-to-treatanalysis.28,31,34,36–40
The majority
of participants were stillin the sample atthe end ofthe
study in three studies.32,34,36
Study Characteristics
Seven studieswere conducted in Europe,27,30,31,34–36,38,39
four of which were in the United Kingdom.27,31,36,38
Four
were conducted in the United States29,32,33,40and two in
Australia/Oceania28,37 (Table 2). Follow-up ranged from
6 to 17 months. Two studieswere categorized asbeing
individualRCTs,32,33and 12 were cluster RCTs.27–31,34–40
With regard to ProFaNE intervention type,there were six
single,27–32 one multiple,33 and six multifactorial34–40 fall
prevention programs (Table 3).The included articles had
22,915 residents,with an overall mean age range of82
to 88.
Overall Effects on Number of Falls, Fallers, and
Recurrent Fallers
The number of falls was reported in 12 studies
(Table 4).27–36,38,39In nine studies,the intervention and
control groupsdid not differ significantly in numberof
falls.27–33,36,38Two multifactorial studies34,39 showed a
significant decrease in falls of 36% and 45%,respectively,
over a 12-month period for the intervention groups.An a
priori secondarysubgroup analysis35 of one study34
showed thatthe effectwas only significantin cognitively
impaired residents(relative risk (RR) = 0.49,95% confi-
denceinterval (CI) = 0.35–0.69)and not in cognitively
intact residents (hazard rate (HR) = 0.91, 95% CI = 0.68–
1.22). Pooled data from 10 studies showed no effect
on number of falls (RR = 0.93, 95% CI = 0.76–1.13;
I² = 89.8%, P < .001).27–31,33,34,36,38,39
Seven studies assessed the number of fallers as an out-
come measure,31,33–38of which two multifactorialstudies
showed significantly fewer fallers in the intervention group
than in the control group. These two studies reported
25%34 and 30%35 fewer fallers,although the pooled risk
estimatesfailed to demonstratea beneficialeffect of
the intervention on numberof fallers (RR = 0.97,95%
CI = 0.84–1.11; I² = 47.9%, P = .09).31,33,34,36–38
The number ofrecurrentfallers was assessed in four
multifactorialstudies.34,36,38,40One study34 described a
214 VLAEYEN ET AL. FEBRUARY 2015–VOL. 63, NO. 2 JAGS
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
significant 44% reduction in the number of recurrent fallers
for the intervention group.In another study,40 the mean
proportion of recurrent fallers was 19% lower in the inter-
vention facilities than in the controlfacilities.The pooled
estimate showed significantly fewer recurrent fallers in the
intervention groups than in the control groups (RR = 0.79,
95% CI = 0.65–0.97; I² = 6.3%, P = .36).34,36,38,40
Because
only four of 13 included studies assessed recurrent fallers as
an outcome measure, an additional sensitivity analysis was
performed for the three studies34,36,38that also reported on
the outcomes“falls” and “fallers” (the other study40
reported only recurrentfallers)to determine whether the
results for those two outcomes were concordantwith the
outcome for “recurrent fallers.” Pooled data showed a sig-
nificant effect of intervention on number of falls
(RR = 0.64,95% CI = 0.50–0.81;I² = 24.1%, P = .27)
and a nonsignificant effect on number of fallers (RR = 0.82,
95% CI = 0.67–1.01; I² = 18.6%, P = .29).
The trim-and-fillanalysis did notrevealany publica-
tion bias for the above analyses.23
Characteristics and Effects of Different Types of
Interventions
Single Interventions
Two studies examined the effect of staff training and educa-
tion that focused on dissemination of information on falls
prevention,27,28fall risk assessment and potential modifica-
tions of risk factors,27,28and postfall management review.28
Pooled risk estimates showed that the intervention groups
had significantlymore falls than the control group
(RR = 1.29, 95% CI = 1.23–1.36; I² = 0%, P = .49).27,28
Two other studies evaluatedmedicationinterven-
tions.29,30 One used health information technologyto
analyze medication use in order to identify residents with
Potentially relevant articles identified and screened for retrieval
(n = 1,131)
Articles excluded on the basis of title and abstract (total n = 1,022)
- Setting: not conducted in a nursing home (n = 244)
- Study design: no original/preplanned secondary analyses of RCT (n = 348)
- Study objective: not designed to prevent falls (n = 402)
- No relevant outcomes on number of falls, fallers, or recurrent fallers (n = 19)
- Duration from the start of the intervention was less than 6 months (n = 2)
- Language: not English, French, German, or Dutch (n = 7)
Articles retrieved for full-text assessment of eligibility
(n = 109)
Articles excluded based on application of inclusion criteria (total n = 95)
- Setting: not conducted in a nursing home (n = 22)
- Study design: no original/preplanned secondary analyses of RCT (n = 38)
- Study objective: not designed to prevent falls (n = 28)
- No relevant outcomes on number of falls, fallers, or recurrent fallers (n = 3)
- Duration from the start of the intervention was less than 6 months (n = 3)
- Language: not English, French, German, or Dutch (n = 1)
Articles included in the manuscript for analysis (qualitative synthesis)
(n = 14)
Combined search results of all electronic databases: (total n = 1,424)
- MEDLINE (n = 574)
- EMBASE (n = 269)
- CINAHL (n = 90)
- Cochrane Central Register of Controlled Trials (n = 304)
- SportDiscus (n = 85)
- PEDro (n = 102)
Excluded duplicates (n = 293)
Articles excluded for meta-analyses (n = 1)
- Rapp et al.35 reported a preplanned secondary analysis of Becker et al .34
and was excluded for the meta-analyses
Studies included in meta-analysis (quantitative synthesis)
(n = 13)
Additional articles by manual search of references (n = 0)
Figure 1.Flow diagram of study selection. RCT = randomized controlled trial.
JAGS FEBRUARY 2015–VOL. 63, NO. 2 EFFECT OF FALL PREVENTION IN NURSING HOMES 215
for the intervention group.In another study,40 the mean
proportion of recurrent fallers was 19% lower in the inter-
vention facilities than in the controlfacilities.The pooled
estimate showed significantly fewer recurrent fallers in the
intervention groups than in the control groups (RR = 0.79,
95% CI = 0.65–0.97; I² = 6.3%, P = .36).34,36,38,40
Because
only four of 13 included studies assessed recurrent fallers as
an outcome measure, an additional sensitivity analysis was
performed for the three studies34,36,38that also reported on
the outcomes“falls” and “fallers” (the other study40
reported only recurrentfallers)to determine whether the
results for those two outcomes were concordantwith the
outcome for “recurrent fallers.” Pooled data showed a sig-
nificant effect of intervention on number of falls
(RR = 0.64,95% CI = 0.50–0.81;I² = 24.1%, P = .27)
and a nonsignificant effect on number of fallers (RR = 0.82,
95% CI = 0.67–1.01; I² = 18.6%, P = .29).
The trim-and-fillanalysis did notrevealany publica-
tion bias for the above analyses.23
Characteristics and Effects of Different Types of
Interventions
Single Interventions
Two studies examined the effect of staff training and educa-
tion that focused on dissemination of information on falls
prevention,27,28fall risk assessment and potential modifica-
tions of risk factors,27,28and postfall management review.28
Pooled risk estimates showed that the intervention groups
had significantlymore falls than the control group
(RR = 1.29, 95% CI = 1.23–1.36; I² = 0%, P = .49).27,28
Two other studies evaluatedmedicationinterven-
tions.29,30 One used health information technologyto
analyze medication use in order to identify residents with
Potentially relevant articles identified and screened for retrieval
(n = 1,131)
Articles excluded on the basis of title and abstract (total n = 1,022)
- Setting: not conducted in a nursing home (n = 244)
- Study design: no original/preplanned secondary analyses of RCT (n = 348)
- Study objective: not designed to prevent falls (n = 402)
- No relevant outcomes on number of falls, fallers, or recurrent fallers (n = 19)
- Duration from the start of the intervention was less than 6 months (n = 2)
- Language: not English, French, German, or Dutch (n = 7)
Articles retrieved for full-text assessment of eligibility
(n = 109)
Articles excluded based on application of inclusion criteria (total n = 95)
- Setting: not conducted in a nursing home (n = 22)
- Study design: no original/preplanned secondary analyses of RCT (n = 38)
- Study objective: not designed to prevent falls (n = 28)
- No relevant outcomes on number of falls, fallers, or recurrent fallers (n = 3)
- Duration from the start of the intervention was less than 6 months (n = 3)
- Language: not English, French, German, or Dutch (n = 1)
Articles included in the manuscript for analysis (qualitative synthesis)
(n = 14)
Combined search results of all electronic databases: (total n = 1,424)
- MEDLINE (n = 574)
- EMBASE (n = 269)
- CINAHL (n = 90)
- Cochrane Central Register of Controlled Trials (n = 304)
- SportDiscus (n = 85)
- PEDro (n = 102)
Excluded duplicates (n = 293)
Articles excluded for meta-analyses (n = 1)
- Rapp et al.35 reported a preplanned secondary analysis of Becker et al .34
and was excluded for the meta-analyses
Studies included in meta-analysis (quantitative synthesis)
(n = 13)
Additional articles by manual search of references (n = 0)
Figure 1.Flow diagram of study selection. RCT = randomized controlled trial.
JAGS FEBRUARY 2015–VOL. 63, NO. 2 EFFECT OF FALL PREVENTION IN NURSING HOMES 215
a high risk of falling.29 Consultant pharmaciststhen
reviewed medication and discussed their findings with the
nursing staff. Nurse assistantsobservedand reported
symptoms ofmedication side effects.In contrast,another
study30 evaluated whether trained pharmacistswho
reviewed clinicaland prescribinginformation and then
consulted with generalpractitioners improved prescribing
behavior.This study used an algorithm to evaluatethe
appropriatenessof the residents’prescribed psychoactive
medications.The pooled risk estimateof 1.20 (95%
CI = 0.89–1.61;I² = 63.0%,P = .10)indicated a nonsig-
nificanteffectbut with a trend toward more falls in the
intervention groups.29,30
Another study reported results from a vitamin D supple-
ment intervention.Every 3 months,residents were offered
2.5 mg of ergocalciferol for a median 10 months.31 Another
study examined a supervised ankle strengthening and walk-
ing program in which the duration, distance, and gait speed
were progressively increased according to the capabilities of
each participant.32 Neither of these two studies led to a sig-
nificant reduction in the number of falls or fallers.
Multiple Interventions
In the only multiple intervention study,intervention group
residentsreceived incontinence care and a low-intensity,
functionally oriented exerciseprogram.33 No significant
decrease in numberof falls or fallerswas detected asa
result of the intervention.
Multifactorial Interventions
One study used a customized intervention,with all inter-
vention components targeted to the individualrisk profile
of each resident.37 Five studies examined partially custom-
ized interventions(general componentsgiven to all
residents,some componentstargeted to individualrisk
profile of the resident).34–36,38–40
The studies’ interventions
focused on exercise;34–39 medication;36,38–40 orthostatic
hypotension;36,38,40 environment;34–36,38–40 hip protec-
tors;34,35 vision;36,38 feetand footwear;36,40 and goalset-
ting, reminders,and feedback.34,35,37,40In all but one
study,37 a multidisciplinary team implemented the inter-
vention program.
For the multifactorialinterventionsreviewed,the
pooled risk estimatesshowed a significantbeneficial
effectof the intervention for number offalls (RR = 0.67,
95% CI = 0.55–0.82;I² = 16.7%, P = .31)34,36,38,39and
recurrent fallers (RR = 0.79, 95% CI = 0.65–0.97;
I² = 6.3%, P = .36)34,36,38,40 but not for number of
fallers (RR = 0.83, 95% CI = 0.68–1.01; I² = 20.0%,
P = .29).34,36–38
Table 2. Characteristics of Included Articles
Study Design Setting
Nursing
Homes,
n
Residents, n
Age, Mean Standard
Deviation Female, n (%)
Duration
of Study
Period,a
MonthsIntervention Control Intervention Control Intervention Control
Becker34 CRCT Germany 6 509 472 83.57.5 84.36.9 399 (78.4) 373 (79.0) 12
Cox27 CRCT United
Kingdom
209 3,476 2,753 NA NA 2,639 (77.9)2,003 (75.4) 12
Dyer36 CRCT United
Kingdom
20 102 94 87.26.9 87.46.9 81 (79.4) 72 (76.6) 12
Kerse37 CRCT New
Zealand
41 330 352 84.47.2 84.17.2 240 (72.7) 262 (74.4) 12
Lapane29 CRCT United
States
25 1,769 1,552 NA NA 1,307 (73.9)1,146 (73.9) 12
Law31 CRCT United
Kingdom
118 1,762 1,955 85 85 1,339 (75.9)1,485 (75.9) 10c
McMurdo38 CRCT United
Kingdom
9 77 56 84.96.7 83.76.7 60 (77.9) 48 (85.7) 12
Neyens39 CRCT The
Netherlands
12 249 269 82.17.7 83.37.7 161 (64.6) 191 (71.0) 12
Patterson30 CRCT Northern
Ireland
22 173 161 82.68.4 82.98.4 125 (72.3) 119 (73.4) 12
Rapp35 CRCT Germany 6 365 360 NA NA NA NA 12
Ray40 CRCT United
States
14 221 261 82.7 82.6 171 (77.4) 205 (78.5) 12
Schnelle33 RCT United
States
4 92 98 87.38.0 88.66.7 73 (79.3) 88 (89.7) 8
Schoenfelder32 RCT United
States
2 9 7 NA NA 8 (88.9) 4 (57.1) 6
Ward28 CRCT Australia 88 2,802 2,589 86d 85d 2,049 (73.1)1,862 (71.9) 17
aDuration from start of the intervention to and including follow-up period.
bSame intervention described in both articles. Rapp et al.35 is a secondary analysis of the study performed by Becker et al.34
cMean.
dMedian.
RCT = randomized controlled trial; CRCT = cluster randomized controlled trial; NA = not available.
216 VLAEYEN ET AL. FEBRUARY 2015–VOL. 63, NO. 2 JAGS
reviewed medication and discussed their findings with the
nursing staff. Nurse assistantsobservedand reported
symptoms ofmedication side effects.In contrast,another
study30 evaluated whether trained pharmacistswho
reviewed clinicaland prescribinginformation and then
consulted with generalpractitioners improved prescribing
behavior.This study used an algorithm to evaluatethe
appropriatenessof the residents’prescribed psychoactive
medications.The pooled risk estimateof 1.20 (95%
CI = 0.89–1.61;I² = 63.0%,P = .10)indicated a nonsig-
nificanteffectbut with a trend toward more falls in the
intervention groups.29,30
Another study reported results from a vitamin D supple-
ment intervention.Every 3 months,residents were offered
2.5 mg of ergocalciferol for a median 10 months.31 Another
study examined a supervised ankle strengthening and walk-
ing program in which the duration, distance, and gait speed
were progressively increased according to the capabilities of
each participant.32 Neither of these two studies led to a sig-
nificant reduction in the number of falls or fallers.
Multiple Interventions
In the only multiple intervention study,intervention group
residentsreceived incontinence care and a low-intensity,
functionally oriented exerciseprogram.33 No significant
decrease in numberof falls or fallerswas detected asa
result of the intervention.
Multifactorial Interventions
One study used a customized intervention,with all inter-
vention components targeted to the individualrisk profile
of each resident.37 Five studies examined partially custom-
ized interventions(general componentsgiven to all
residents,some componentstargeted to individualrisk
profile of the resident).34–36,38–40
The studies’ interventions
focused on exercise;34–39 medication;36,38–40 orthostatic
hypotension;36,38,40 environment;34–36,38–40 hip protec-
tors;34,35 vision;36,38 feetand footwear;36,40 and goalset-
ting, reminders,and feedback.34,35,37,40In all but one
study,37 a multidisciplinary team implemented the inter-
vention program.
For the multifactorialinterventionsreviewed,the
pooled risk estimatesshowed a significantbeneficial
effectof the intervention for number offalls (RR = 0.67,
95% CI = 0.55–0.82;I² = 16.7%, P = .31)34,36,38,39and
recurrent fallers (RR = 0.79, 95% CI = 0.65–0.97;
I² = 6.3%, P = .36)34,36,38,40 but not for number of
fallers (RR = 0.83, 95% CI = 0.68–1.01; I² = 20.0%,
P = .29).34,36–38
Table 2. Characteristics of Included Articles
Study Design Setting
Nursing
Homes,
n
Residents, n
Age, Mean Standard
Deviation Female, n (%)
Duration
of Study
Period,a
MonthsIntervention Control Intervention Control Intervention Control
Becker34 CRCT Germany 6 509 472 83.57.5 84.36.9 399 (78.4) 373 (79.0) 12
Cox27 CRCT United
Kingdom
209 3,476 2,753 NA NA 2,639 (77.9)2,003 (75.4) 12
Dyer36 CRCT United
Kingdom
20 102 94 87.26.9 87.46.9 81 (79.4) 72 (76.6) 12
Kerse37 CRCT New
Zealand
41 330 352 84.47.2 84.17.2 240 (72.7) 262 (74.4) 12
Lapane29 CRCT United
States
25 1,769 1,552 NA NA 1,307 (73.9)1,146 (73.9) 12
Law31 CRCT United
Kingdom
118 1,762 1,955 85 85 1,339 (75.9)1,485 (75.9) 10c
McMurdo38 CRCT United
Kingdom
9 77 56 84.96.7 83.76.7 60 (77.9) 48 (85.7) 12
Neyens39 CRCT The
Netherlands
12 249 269 82.17.7 83.37.7 161 (64.6) 191 (71.0) 12
Patterson30 CRCT Northern
Ireland
22 173 161 82.68.4 82.98.4 125 (72.3) 119 (73.4) 12
Rapp35 CRCT Germany 6 365 360 NA NA NA NA 12
Ray40 CRCT United
States
14 221 261 82.7 82.6 171 (77.4) 205 (78.5) 12
Schnelle33 RCT United
States
4 92 98 87.38.0 88.66.7 73 (79.3) 88 (89.7) 8
Schoenfelder32 RCT United
States
2 9 7 NA NA 8 (88.9) 4 (57.1) 6
Ward28 CRCT Australia 88 2,802 2,589 86d 85d 2,049 (73.1)1,862 (71.9) 17
aDuration from start of the intervention to and including follow-up period.
bSame intervention described in both articles. Rapp et al.35 is a secondary analysis of the study performed by Becker et al.34
cMean.
dMedian.
RCT = randomized controlled trial; CRCT = cluster randomized controlled trial; NA = not available.
216 VLAEYEN ET AL. FEBRUARY 2015–VOL. 63, NO. 2 JAGS
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
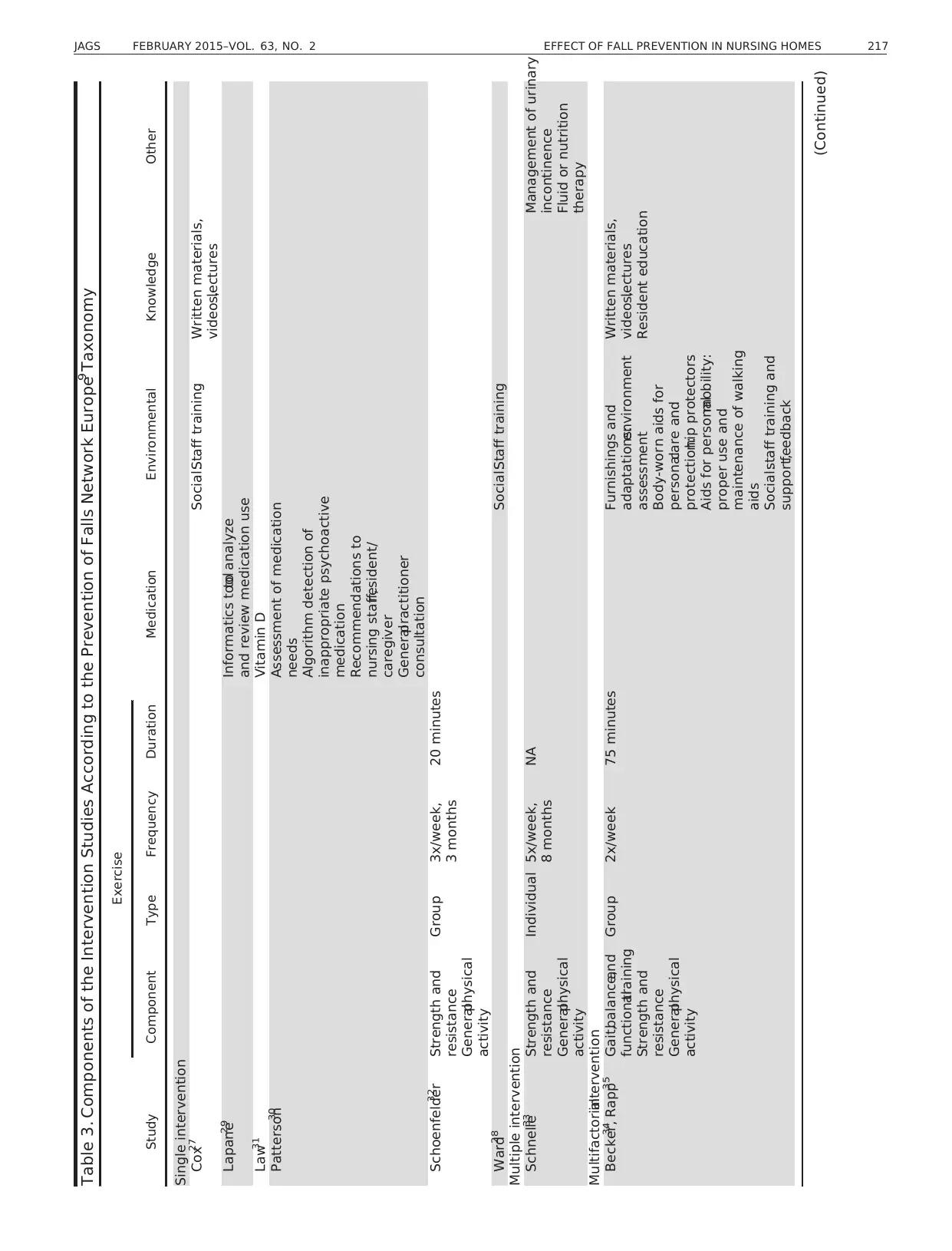
Table 3. Components of the Intervention Studies According to the Prevention of Falls Network Europe Taxonomy9
Study
Exercise
Medication Environmental Knowledge OtherComponent Type Frequency Duration
Single intervention
Cox27 Social:Staff training Written materials,
videos,lectures
Lapane29 Informatics toolto analyze
and review medication use
Law31 Vitamin D
Patterson30 Assessment of medication
needs
Algorithm detection of
inappropriate psychoactive
medication
Recommendations to
nursing staff,resident/
caregiver
Generalpractitioner
consultation
Schoenfelder32 Strength and
resistance
Generalphysical
activity
Group 3x/week,
3 months
20 minutes
Ward28 Social:Staff training
Multiple intervention
Schnelle33 Strength and
resistance
Generalphysical
activity
Individual 5x/week,
8 months
NA Management of urinary
incontinence
Fluid or nutrition
therapy
Multifactorialintervention
Becker34
, Rapp35 Gait,balance,and
functionaltraining
Strength and
resistance
Generalphysical
activity
Group 2x/week 75 minutes Furnishings and
adaptations:environment
assessment
Body-worn aids for
personalcare and
protection:hip protectors
Aids for personalmobility:
proper use and
maintenance of walking
aids
Social:staff training and
support,feedback
Written materials,
videos,lectures
Resident education
(Continued)
JAGS FEBRUARY 2015–VOL. 63, NO. 2 EFFECT OF FALL PREVENTION IN NURSING HOMES 217
Study
Exercise
Medication Environmental Knowledge OtherComponent Type Frequency Duration
Single intervention
Cox27 Social:Staff training Written materials,
videos,lectures
Lapane29 Informatics toolto analyze
and review medication use
Law31 Vitamin D
Patterson30 Assessment of medication
needs
Algorithm detection of
inappropriate psychoactive
medication
Recommendations to
nursing staff,resident/
caregiver
Generalpractitioner
consultation
Schoenfelder32 Strength and
resistance
Generalphysical
activity
Group 3x/week,
3 months
20 minutes
Ward28 Social:Staff training
Multiple intervention
Schnelle33 Strength and
resistance
Generalphysical
activity
Individual 5x/week,
8 months
NA Management of urinary
incontinence
Fluid or nutrition
therapy
Multifactorialintervention
Becker34
, Rapp35 Gait,balance,and
functionaltraining
Strength and
resistance
Generalphysical
activity
Group 2x/week 75 minutes Furnishings and
adaptations:environment
assessment
Body-worn aids for
personalcare and
protection:hip protectors
Aids for personalmobility:
proper use and
maintenance of walking
aids
Social:staff training and
support,feedback
Written materials,
videos,lectures
Resident education
(Continued)
JAGS FEBRUARY 2015–VOL. 63, NO. 2 EFFECT OF FALL PREVENTION IN NURSING HOMES 217
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
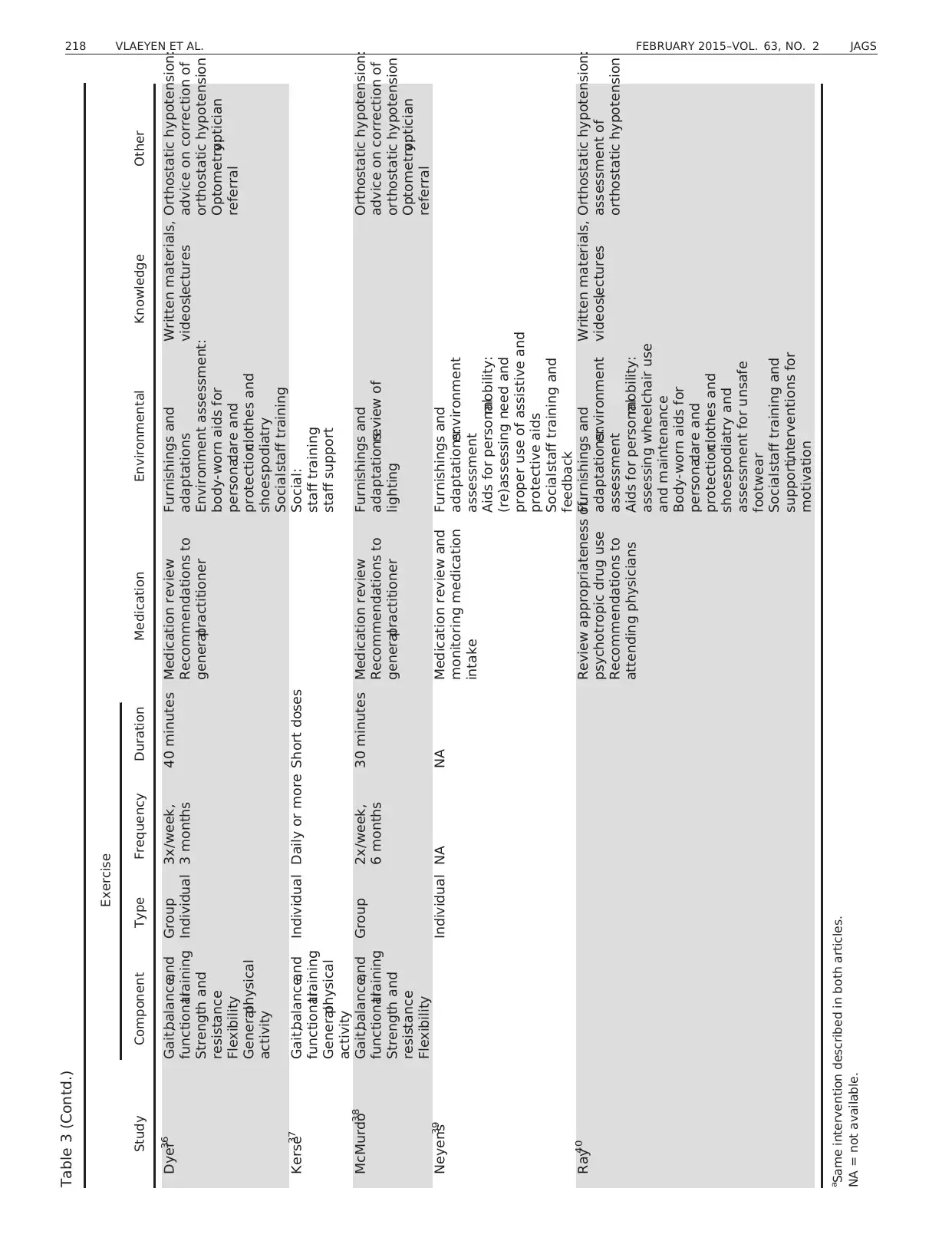
Table 3 (Contd.)
Study
Exercise
Medication Environmental Knowledge OtherComponent Type Frequency Duration
Dyer36 Gait,balance,and
functionaltraining
Strength and
resistance
Flexibility
Generalphysical
activity
Group
Individual
3x/week,
3 months
40 minutes Medication review
Recommendations to
generalpractitioner
Furnishings and
adaptations
Environment assessment:
body-worn aids for
personalcare and
protection:clothes and
shoes:podiatry
Social:staff training
Written materials,
videos,lectures
Orthostatic hypotension:
advice on correction of
orthostatic hypotension
Optometry:optician
referral
Kerse37 Gait,balance,and
functionaltraining
Generalphysical
activity
Individual Daily or more Short doses Social:
staff training
staff support
McMurdo38 Gait,balance,and
functionaltraining
Strength and
resistance
Flexibility
Group 2x/week,
6 months
30 minutes Medication review
Recommendations to
generalpractitioner
Furnishings and
adaptations:review of
lighting
Orthostatic hypotension:
advice on correction of
orthostatic hypotension
Optometry:optician
referral
Neyens39 Individual NA NA Medication review and
monitoring medication
intake
Furnishings and
adaptations:environment
assessment
Aids for personalmobility:
(re)assessing need and
proper use of assistive and
protective aids
Social:staff training and
feedback
Ray40 Review appropriateness of
psychotropic drug use
Recommendations to
attending physicians
Furnishings and
adaptations:environment
assessment
Aids for personalmobility:
assessing wheelchair use
and maintenance
Body-worn aids for
personalcare and
protection:clothes and
shoes:podiatry and
assessment for unsafe
footwear
Social:staff training and
support,interventions for
motivation
Written materials,
videos,lectures
Orthostatic hypotension:
assessment of
orthostatic hypotension
a
Same intervention described in both articles.
NA = not available.
218 VLAEYEN ET AL. FEBRUARY 2015–VOL. 63, NO. 2 JAGS
Study
Exercise
Medication Environmental Knowledge OtherComponent Type Frequency Duration
Dyer36 Gait,balance,and
functionaltraining
Strength and
resistance
Flexibility
Generalphysical
activity
Group
Individual
3x/week,
3 months
40 minutes Medication review
Recommendations to
generalpractitioner
Furnishings and
adaptations
Environment assessment:
body-worn aids for
personalcare and
protection:clothes and
shoes:podiatry
Social:staff training
Written materials,
videos,lectures
Orthostatic hypotension:
advice on correction of
orthostatic hypotension
Optometry:optician
referral
Kerse37 Gait,balance,and
functionaltraining
Generalphysical
activity
Individual Daily or more Short doses Social:
staff training
staff support
McMurdo38 Gait,balance,and
functionaltraining
Strength and
resistance
Flexibility
Group 2x/week,
6 months
30 minutes Medication review
Recommendations to
generalpractitioner
Furnishings and
adaptations:review of
lighting
Orthostatic hypotension:
advice on correction of
orthostatic hypotension
Optometry:optician
referral
Neyens39 Individual NA NA Medication review and
monitoring medication
intake
Furnishings and
adaptations:environment
assessment
Aids for personalmobility:
(re)assessing need and
proper use of assistive and
protective aids
Social:staff training and
feedback
Ray40 Review appropriateness of
psychotropic drug use
Recommendations to
attending physicians
Furnishings and
adaptations:environment
assessment
Aids for personalmobility:
assessing wheelchair use
and maintenance
Body-worn aids for
personalcare and
protection:clothes and
shoes:podiatry and
assessment for unsafe
footwear
Social:staff training and
support,interventions for
motivation
Written materials,
videos,lectures
Orthostatic hypotension:
assessment of
orthostatic hypotension
a
Same intervention described in both articles.
NA = not available.
218 VLAEYEN ET AL. FEBRUARY 2015–VOL. 63, NO. 2 JAGS
Analysis of Intervention Effect Size When Considering
Dementia Status
Regression ofeffectsizesfor the numberof fallersonto
the studies’ prevalence-of-dementia category (see Data Syn-
thesis and Analysis section in Methods)showed thatthe
intervention had protective effects in studies with a greater
proportion of residentswith dementia.Each one-point
increase in dementia prevalence category corresponded to
a RR that was only 0.76 ofits former size (analysis not
consideringdementiaprevalence;95% CI = 0.58–0.99,
P = .04;I² = 0.31,P = .22).31,33,34,38No significantasso-
ciationswith dementia prevalence score were found for
number of falls (RR = 0.95, 95% CI = 0.72–1.25,
P = .72; I² = 0, P = .39)28–31,33,34,38,39
or number of recur-
rent fallers (RR = 1.42, 95% CI = 0.49–4.11, P = .51;
I² = 0, P = .45).34,38,40
DISCUSSION
This study is unique,becauseit used a meta-analytical
approach ofthe effectivenessof fall prevention interven-
tions, focusing on a clearly defined setting.In previous
studies,effectivenessremained unclear,partly because of
differencesin definitions of what constitutesa nursing
home.The currentstudy examined notonly effectiveness
of interventions in terms of number of falls and fallers, but
also whetherinterventionsreduced the numberof recur-
rent fallers.Although the overallmeta-analysisfailed to
show an effect on number of falls and fallers,it showed a
significant 21% reduction of number of recurrent fallers in
intervention programs.An a priori subgroup analysisof
intervention type showed thatmultifactorialinterventions
had a significanteffecton number of falls (33%) and
recurrent fallers (21%).
Although the analyses showed no effect on the number
of fallers, it has been argued that using falls as an outcome
has potentialbenefits over using fallers,because each fall
entails an injury risk.17 Therefore, an effective intervention
on numberof falls has clinical, public health,and eco-
nomic relevance. The latter reasoning also justifies focusing
on recurrentfallersas an importantoutcome,as in the
current review.
Nursing home residents are often physically frailand
cognitively impaired.Considering the multifactorialnature
of a fall, it is therefore not surprising that single interven-
tions failed to show a beneficialeffect on fall-related out-
comes. The current results suggest that, in the specific care
setting considered,single interventionscould even be
harmful,although these results should be interpreted with
caution,considering the smallnumber of studies,some of
which had poor methodologicalquality.An a priori sub-
group analysis showed that customized,multifactorial
interventions reduced falls.A multidisciplinary team pro-
vided these multifactorialinterventions in allstudies,but
team composition and frequency ofassessmentwere not
reported.Furthermore,the small numberof studiesdid
not allow additionalmoderator analyses to be conducted
to evaluate which components ofthe multifactorialinter-
vention programsor combinationsthereof were most
effective.
The results ofthe regression analysis performed ata
meta level to examine effectiveness of falls prevention pro-
gramsin residentswith dementia werenot anticipated.
There were fewer fallers in intervention groups that had a
greater prevalence of dementia. This outcome contradicts a
previous review,16 but because studies in which the num-
ber of residentswith dementiawas unknown were
excluded,the numberof studiesincluded in the current
review was limited,which might explain the contradictory
Table 4. Effectiveness of Interventions Described in the Included Articles
Study
Falls Fallers, n/N (%) Recurrent Fallers, n/N (%)
Intervention Control
P-
Value Intervention Control
P-
Value Intervention Control
P-
Value
Becker34 1.40/RY 2.56/RY <.001 188/509 (36.9)247/472 (52.3) .04 66/509 (12.9) 115/472
(24.4)
.01
Cox27 NA/3,315 NA/2,322 .17 NA NA
Dyer36 2.17/RY 4.02/RY .27 56/102 (54.9) 51/94 (54.3) .94 26/102 (25.5)25/94 (26.6) .28
Kerse37 NA 162/310 (52.2)146/329 (44.3) .48 NA
Lapane29 3.42/RY 3.78/RY NA NA NA
Law31 2.01/RY 2.31/RY NA 770/1,762
(43.7)
833/1,955
(42.6)
NA NA
McMurdo38 3.02/RY 3.85/RY .16 20/77 (38) 22/56 (58) .09 13/77 (25.0) 9/56 (24) >.99
Neyens39 2.09/RY 2.54/RY .03 NA NA
Patterson30 1.96/RY 1.37/RY .09 NA NA
Rapp35 1.29/RY 2.35/RY NA 143/365 (39.2)189/360 (52.5) NA NA
Ray40 NA NA 91/221 (43.8) 129/261
(54.1)
.03
Schnelle33 0.67/RY 1.09/RY .40 17/92 (18.5) 29/98 (29.6) NA NA
Schoenfelder32 44/7 12/7 NA NA NA
Ward28 Mean 13/
month
Mean 10/
month
NA NA NA
aSame intervention described in both articles.
RY = resident year; NA = not available.
JAGS FEBRUARY 2015–VOL. 63, NO. 2 EFFECT OF FALL PREVENTION IN NURSING HOMES 219
Dementia Status
Regression ofeffectsizesfor the numberof fallersonto
the studies’ prevalence-of-dementia category (see Data Syn-
thesis and Analysis section in Methods)showed thatthe
intervention had protective effects in studies with a greater
proportion of residentswith dementia.Each one-point
increase in dementia prevalence category corresponded to
a RR that was only 0.76 ofits former size (analysis not
consideringdementiaprevalence;95% CI = 0.58–0.99,
P = .04;I² = 0.31,P = .22).31,33,34,38No significantasso-
ciationswith dementia prevalence score were found for
number of falls (RR = 0.95, 95% CI = 0.72–1.25,
P = .72; I² = 0, P = .39)28–31,33,34,38,39
or number of recur-
rent fallers (RR = 1.42, 95% CI = 0.49–4.11, P = .51;
I² = 0, P = .45).34,38,40
DISCUSSION
This study is unique,becauseit used a meta-analytical
approach ofthe effectivenessof fall prevention interven-
tions, focusing on a clearly defined setting.In previous
studies,effectivenessremained unclear,partly because of
differencesin definitions of what constitutesa nursing
home.The currentstudy examined notonly effectiveness
of interventions in terms of number of falls and fallers, but
also whetherinterventionsreduced the numberof recur-
rent fallers.Although the overallmeta-analysisfailed to
show an effect on number of falls and fallers,it showed a
significant 21% reduction of number of recurrent fallers in
intervention programs.An a priori subgroup analysisof
intervention type showed thatmultifactorialinterventions
had a significanteffecton number of falls (33%) and
recurrent fallers (21%).
Although the analyses showed no effect on the number
of fallers, it has been argued that using falls as an outcome
has potentialbenefits over using fallers,because each fall
entails an injury risk.17 Therefore, an effective intervention
on numberof falls has clinical, public health,and eco-
nomic relevance. The latter reasoning also justifies focusing
on recurrentfallersas an importantoutcome,as in the
current review.
Nursing home residents are often physically frailand
cognitively impaired.Considering the multifactorialnature
of a fall, it is therefore not surprising that single interven-
tions failed to show a beneficialeffect on fall-related out-
comes. The current results suggest that, in the specific care
setting considered,single interventionscould even be
harmful,although these results should be interpreted with
caution,considering the smallnumber of studies,some of
which had poor methodologicalquality.An a priori sub-
group analysis showed that customized,multifactorial
interventions reduced falls.A multidisciplinary team pro-
vided these multifactorialinterventions in allstudies,but
team composition and frequency ofassessmentwere not
reported.Furthermore,the small numberof studiesdid
not allow additionalmoderator analyses to be conducted
to evaluate which components ofthe multifactorialinter-
vention programsor combinationsthereof were most
effective.
The results ofthe regression analysis performed ata
meta level to examine effectiveness of falls prevention pro-
gramsin residentswith dementia werenot anticipated.
There were fewer fallers in intervention groups that had a
greater prevalence of dementia. This outcome contradicts a
previous review,16 but because studies in which the num-
ber of residentswith dementiawas unknown were
excluded,the numberof studiesincluded in the current
review was limited,which might explain the contradictory
Table 4. Effectiveness of Interventions Described in the Included Articles
Study
Falls Fallers, n/N (%) Recurrent Fallers, n/N (%)
Intervention Control
P-
Value Intervention Control
P-
Value Intervention Control
P-
Value
Becker34 1.40/RY 2.56/RY <.001 188/509 (36.9)247/472 (52.3) .04 66/509 (12.9) 115/472
(24.4)
.01
Cox27 NA/3,315 NA/2,322 .17 NA NA
Dyer36 2.17/RY 4.02/RY .27 56/102 (54.9) 51/94 (54.3) .94 26/102 (25.5)25/94 (26.6) .28
Kerse37 NA 162/310 (52.2)146/329 (44.3) .48 NA
Lapane29 3.42/RY 3.78/RY NA NA NA
Law31 2.01/RY 2.31/RY NA 770/1,762
(43.7)
833/1,955
(42.6)
NA NA
McMurdo38 3.02/RY 3.85/RY .16 20/77 (38) 22/56 (58) .09 13/77 (25.0) 9/56 (24) >.99
Neyens39 2.09/RY 2.54/RY .03 NA NA
Patterson30 1.96/RY 1.37/RY .09 NA NA
Rapp35 1.29/RY 2.35/RY NA 143/365 (39.2)189/360 (52.5) NA NA
Ray40 NA NA 91/221 (43.8) 129/261
(54.1)
.03
Schnelle33 0.67/RY 1.09/RY .40 17/92 (18.5) 29/98 (29.6) NA NA
Schoenfelder32 44/7 12/7 NA NA NA
Ward28 Mean 13/
month
Mean 10/
month
NA NA NA
aSame intervention described in both articles.
RY = resident year; NA = not available.
JAGS FEBRUARY 2015–VOL. 63, NO. 2 EFFECT OF FALL PREVENTION IN NURSING HOMES 219
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

finding.In addition,the lack of objective measurement of
dementia in the included studies prevents firm conclusions
from being drawn.
Some methodological aspects deserve further attention.
First, inherent to this type of research, high loss to follow-
up caused by death or sudden illness and difficulty main-
taining blinding of participantsor treatmentproviders
results in poor overall methodologicalquality of the
included studies.Second,although this review is the first
to suggest that it is possible to reduce the number of recur-
rent fallers in nursing homes,only four studies were eligi-
ble for this analysis.One might wonder whetherthis
significant finding is not the result of multiple testing,but
the subsequent sensitivity analysis results for falls and fal-
lers are concordantwith the effectsize for recurrentfal-
lers, which suggeststhat some unique featuresof those
studies and not random chance might have influenced the
effecton recurrentfallers.More specifically,all included
studiesused a customized,multifactorialapproach con-
ducted by multidisciplinary teams;included an environ-
mentalassessmentand adaptation component;and had a
minimum follow-up of 12 months,as recommended in
ProFaNE.9 This approach wasalso found to be more
effectivein a priori subgroup analyses,although more
research is needed to confirm these findings and to better
understand which components are responsible for this sig-
nificant reduction in recurrent fallers.
Third, despite verifying with the authors of the origi-
nal articlesthat their research setting met,or failed to
meet,the “nursing home” definition,7 this definition is not
as refined and explicit as it could be. For example, it could
be interpreted in different ways.For example,what is the
meaning of “limited care”? This further points toward an
overalllack of a robust conceptualdefinition of what con-
stitutes a nursing home.
Fourth,fall-related outcomes were often inconsistently
reported, and vague definitions were sometimes used. More
specifically, fall definitions were often extended with one or
more specifications,such as “regardless/whateverthe
cause,”34,35 “whether or not an injury resulted,”29 or “the
potentialfor injury exists.”32 The same problem arose for
recurrentfallers.Definitionsvaried from specifying more
than one fall to more than three falls within the last
year.34,36,38,40
The adoption of a more-uniform and -univer-
sally accepted operational definition of fall incidents or recur-
rent fallers (e.g.,9,41
) will undoubtedlyfacilitate the
interpretation of newly conducted studies and meta-analyses.
Finally, previousresearch showsthat fall prevention
programs require a minimum follow-up of12 months to
ensure that a sufficient number of falls occurred for analy-
sis so that delayed,long-term effectsof the intervention
program can be detected.41,42Some of the included studies
had a shorter follow-up time,which could have hampered
the likelihood of detecting a positive effect on outcome.
In terms of clinical implications, the results of this sys-
tematic review suggestthat nursing homesshould try to
implementmultidisciplinary,customized,multifactorial
interventionsto reduce falls in their residents.Such an
intervention requires a large amount of time and effort but
is necessary if nursing homes want to invest in fall preven-
tion, especially because simple,single interventionshave
no effect or even can be harmful.For this reason,further
research is needed on the type of fallprevention interven-
tions being used in nursing homes.Furthermore,imple-
mentation researchis needed to determinepotential
barriers to implementation of evidence-based multifactorial
interventions and to evaluate how nursing homes can be
supported in implementing more-effective,but more-com-
plex and time-consuming,multifactorialfall prevention
interventions.This will aid in avoiding implementing triv-
ial and potentially dangerous single interventions.In addi-
tion, future intervention studiesshould includea more-
detailed description ofeach of the intervention compo-
nents to allow faster implementation and permit compari-
son of intervention effectiveness of studies.
In conclusion,multifactorialfall prevention programs
can reduce the number of falls and recurrent fallers in resi-
dentialfacilitiesthat provide 24-hour-a-day surveillance,
personalcare, and limited clinicalcare for personswho
are typically elderly and infirm,whereassingle interven-
tions, such as education, may be harmful.
ACKNOWLEDGMENTS
The authors would like to thank allthe members ofthe
workgroup “ResidentialCare Facilities” of the Flanders
Centerof Expertise forFall and Fracture Prevention.In
particular, we acknowledgeProf. Dr. Steven Boonen
(deceased) for his valuable contribution to the study.
Conflict of Interest:This study was funded by the
Flemish Ministry of Welfare,Public Health and Family,
Belgium,and the UniversiteitDerde Leeftijd Leuven vzw.
The editor in chief has reviewed the conflictof interest
checklist provided by the authors and has determined that
the authors have no financial or any other kind of personal
conflicts with this paper.
Author Contributions:All authors participated in the
design of the study. Data collection:Vlaeyen, Coussement,
Leysens,Van der Elst.Methodologicalquality assessment:
Vlaeyen,Coussement,Delbaere,Dejaeger,Milisen. Data
interpretation and analysis:Vlaeyen,Coussement,Leysens,
Van der Elst, Dobbels,Dejaeger,Milisen. Meta-analysis:
Denhaerynck.Verification ofcalculations:Vlaeyen,Milis-
en. Drafting the manuscript:Vlaeyen.Critical revision of
manuscript,revisions,approvalof final manuscript:All
authors. Supervision: Milisen.
Sponsor’s Role: Neither the Ministry nor the Universi-
teit Derde Leeftijd Leuven vzw played a role in the elabo-
ration of this review.
REFERENCES
1. Rubenstein L,Josephson K.The epidemiology offalls and syncope.Clin
Geriatr Med 2002;18:141–158.
2. Nyberg L,Gustafson Y,Janson A et al.Incidence of falls in three different
types of geriatric care. Scand J Soc Med 1997;25:8–13.
3. KannusP, Siev€anen H, Palvanen M et al.Prevention offalls and conse-
quent injuries in elderly people. Lancet 2005;366:1885 –1893.
4. Sawka AM, Ismaila N,Cranney A et al.A scoping review of strategies for
the prevention of hip fracture in elderly nursing home residents. PLoS ONE
2010;5:e9515.
5. Rapp K, Becker C,Lamb SE et al.Hip fractures in institutionalized elderly
people: Incidence rates and excess mortality. J Bone Miner Res
2008;23:1825–1831.
6. Berry SD,Samelson EJ,Ngo L et al. Subsequent fracture in nursing home
residents with a hip fracture:A competing risks approach.J Am Geriatr
Soc 2008;56:1887–1892.
220 VLAEYEN ET AL. FEBRUARY 2015–VOL. 63, NO. 2 JAGS
dementia in the included studies prevents firm conclusions
from being drawn.
Some methodological aspects deserve further attention.
First, inherent to this type of research, high loss to follow-
up caused by death or sudden illness and difficulty main-
taining blinding of participantsor treatmentproviders
results in poor overall methodologicalquality of the
included studies.Second,although this review is the first
to suggest that it is possible to reduce the number of recur-
rent fallers in nursing homes,only four studies were eligi-
ble for this analysis.One might wonder whetherthis
significant finding is not the result of multiple testing,but
the subsequent sensitivity analysis results for falls and fal-
lers are concordantwith the effectsize for recurrentfal-
lers, which suggeststhat some unique featuresof those
studies and not random chance might have influenced the
effecton recurrentfallers.More specifically,all included
studiesused a customized,multifactorialapproach con-
ducted by multidisciplinary teams;included an environ-
mentalassessmentand adaptation component;and had a
minimum follow-up of 12 months,as recommended in
ProFaNE.9 This approach wasalso found to be more
effectivein a priori subgroup analyses,although more
research is needed to confirm these findings and to better
understand which components are responsible for this sig-
nificant reduction in recurrent fallers.
Third, despite verifying with the authors of the origi-
nal articlesthat their research setting met,or failed to
meet,the “nursing home” definition,7 this definition is not
as refined and explicit as it could be. For example, it could
be interpreted in different ways.For example,what is the
meaning of “limited care”? This further points toward an
overalllack of a robust conceptualdefinition of what con-
stitutes a nursing home.
Fourth,fall-related outcomes were often inconsistently
reported, and vague definitions were sometimes used. More
specifically, fall definitions were often extended with one or
more specifications,such as “regardless/whateverthe
cause,”34,35 “whether or not an injury resulted,”29 or “the
potentialfor injury exists.”32 The same problem arose for
recurrentfallers.Definitionsvaried from specifying more
than one fall to more than three falls within the last
year.34,36,38,40
The adoption of a more-uniform and -univer-
sally accepted operational definition of fall incidents or recur-
rent fallers (e.g.,9,41
) will undoubtedlyfacilitate the
interpretation of newly conducted studies and meta-analyses.
Finally, previousresearch showsthat fall prevention
programs require a minimum follow-up of12 months to
ensure that a sufficient number of falls occurred for analy-
sis so that delayed,long-term effectsof the intervention
program can be detected.41,42Some of the included studies
had a shorter follow-up time,which could have hampered
the likelihood of detecting a positive effect on outcome.
In terms of clinical implications, the results of this sys-
tematic review suggestthat nursing homesshould try to
implementmultidisciplinary,customized,multifactorial
interventionsto reduce falls in their residents.Such an
intervention requires a large amount of time and effort but
is necessary if nursing homes want to invest in fall preven-
tion, especially because simple,single interventionshave
no effect or even can be harmful.For this reason,further
research is needed on the type of fallprevention interven-
tions being used in nursing homes.Furthermore,imple-
mentation researchis needed to determinepotential
barriers to implementation of evidence-based multifactorial
interventions and to evaluate how nursing homes can be
supported in implementing more-effective,but more-com-
plex and time-consuming,multifactorialfall prevention
interventions.This will aid in avoiding implementing triv-
ial and potentially dangerous single interventions.In addi-
tion, future intervention studiesshould includea more-
detailed description ofeach of the intervention compo-
nents to allow faster implementation and permit compari-
son of intervention effectiveness of studies.
In conclusion,multifactorialfall prevention programs
can reduce the number of falls and recurrent fallers in resi-
dentialfacilitiesthat provide 24-hour-a-day surveillance,
personalcare, and limited clinicalcare for personswho
are typically elderly and infirm,whereassingle interven-
tions, such as education, may be harmful.
ACKNOWLEDGMENTS
The authors would like to thank allthe members ofthe
workgroup “ResidentialCare Facilities” of the Flanders
Centerof Expertise forFall and Fracture Prevention.In
particular, we acknowledgeProf. Dr. Steven Boonen
(deceased) for his valuable contribution to the study.
Conflict of Interest:This study was funded by the
Flemish Ministry of Welfare,Public Health and Family,
Belgium,and the UniversiteitDerde Leeftijd Leuven vzw.
The editor in chief has reviewed the conflictof interest
checklist provided by the authors and has determined that
the authors have no financial or any other kind of personal
conflicts with this paper.
Author Contributions:All authors participated in the
design of the study. Data collection:Vlaeyen, Coussement,
Leysens,Van der Elst.Methodologicalquality assessment:
Vlaeyen,Coussement,Delbaere,Dejaeger,Milisen. Data
interpretation and analysis:Vlaeyen,Coussement,Leysens,
Van der Elst, Dobbels,Dejaeger,Milisen. Meta-analysis:
Denhaerynck.Verification ofcalculations:Vlaeyen,Milis-
en. Drafting the manuscript:Vlaeyen.Critical revision of
manuscript,revisions,approvalof final manuscript:All
authors. Supervision: Milisen.
Sponsor’s Role: Neither the Ministry nor the Universi-
teit Derde Leeftijd Leuven vzw played a role in the elabo-
ration of this review.
REFERENCES
1. Rubenstein L,Josephson K.The epidemiology offalls and syncope.Clin
Geriatr Med 2002;18:141–158.
2. Nyberg L,Gustafson Y,Janson A et al.Incidence of falls in three different
types of geriatric care. Scand J Soc Med 1997;25:8–13.
3. KannusP, Siev€anen H, Palvanen M et al.Prevention offalls and conse-
quent injuries in elderly people. Lancet 2005;366:1885 –1893.
4. Sawka AM, Ismaila N,Cranney A et al.A scoping review of strategies for
the prevention of hip fracture in elderly nursing home residents. PLoS ONE
2010;5:e9515.
5. Rapp K, Becker C,Lamb SE et al.Hip fractures in institutionalized elderly
people: Incidence rates and excess mortality. J Bone Miner Res
2008;23:1825–1831.
6. Berry SD,Samelson EJ,Ngo L et al. Subsequent fracture in nursing home
residents with a hip fracture:A competing risks approach.J Am Geriatr
Soc 2008;56:1887–1892.
220 VLAEYEN ET AL. FEBRUARY 2015–VOL. 63, NO. 2 JAGS
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7. Sorensen S,de Lissovoy G, Kunaprayoon D et al.A taxonomy and eco-
nomic consequencesof nursing homefalls. Drugs Aging 2006;23:251–
262.
8. Scheffer AC,Schuurmans MJ,van Dijk N et al. Fear of falling:Measure-
ment strategy,prevalence,risk factors and consequences among older per-
sons. Age Ageing 2008;37:19–24.
9. Lamb SE, Becker C, Gillespie LD et al. Reporting of complex interventions
in clinicaltrials:Development of a taxonomy to classify and describe fall-
prevention interventions. Trials 2011;12:125.
10. BeckerC, Rapp K. Fall prevention in nursing homes.Clin Geriatr Med
2010;26:693–704.
11. Vu MQ, Weintraub N, Rubenstein LZ. Falls in the nursing home: Are they
preventable? J Am Med Dir Assoc 2006;7:S53–S58.
12. Quigley P, Bulat T, Kurtzman E et al. Fall prevention and injury protection
for nursing home residents. J Am Med Dir Assoc 2010;11:284–293.
13. Cusimano MD, Kwok J, Spadafora K.Effectivenessof multifaceted fall-
prevention programs for elderly in residentialcare.Inj Prev 2008;14:113–
122.
14. NeyensJC, van HaastregtJC, Dijcks BP et al. Falls in elderly people in
long-term care facilities:A systematic review of RCTs.J Am Med Dir As-
soc 2011;12:410–425.
15. Cameron ID,Gillespie LD,Robertson MC et al.Interventions for prevent-
ing falls in older people in nursing care facilities and hospitals.Cochrane
Database Syst Rev 2012;12:CD005465.
16. Oliver D, Connelly JB, Victor CR et al. Strategies to prevent falls and frac-
tures in hospitals and care homes and effect of cognitive impairment:Sys-
tematic review and meta-analyses. BMJ 2007;334:82.
17. Gillespie LD,Robertson MC,Gillespie WJ et al.Interventions for prevent-
ing falls in older people in the community.Cochrane Database SystRev
2012;9:CD007146.
18. InternationalProspective Register of Systematic Reviews,PROSPERO [on-
line]. Available at www.crd.york.ac.uk/prospero/AccessedAugust 12,
2012.
19. Liberati A, Altman D, Tetzlaff J et al. The PRISMA statement for reporting
systematic reviewsand meta-analysesof studiesthat evaluate healthcare
interventions: Explanation and elaboration. BMJ 2009;339:b2700.
20. Moher D, LiberatiA, Tetzlaff J et al.Preferred reporting items for system-
atic review and meta-analyses:The PRISMA statement.PLoS Med 2009;6:
e1000097.
21. Cameron I, Murray GR, Gillespie LD et al. Interventionsfor preventing
falls in older people in residentialcare facilities and hospitals (protocol).
Cochrane Database Syst Rev 2005;3:CD005465.
22. Wang MC, Bushman BJ. IntegratingResults Through Meta-Analytic
Review Using SASâ Software. Cary, NC: SAS Institute Inc, 1999.
23. Rendina-Gobioff G, Kromrey JD. PUB_BIAS: A SASâ Macro for Detecting.
Publication Biasin Meta-Analysis[on-line].Available at www.analytics.
ncsu.edu/sesug/2006/PO04_06.PDF Accessed January 20, 2013.
24. Duval S, Tweedie R. A simple funnel-plot-based method oftesting and
adjusting for publication bias in meta-analysis.Biometrics 2000;56:
455–463.
25. Cooper H, HedgesLV, eds.The Handbook of Research Synthesis.New
York: Russell Sage Foundation, 1994.
26. Huedo-Medina T,Sanchez-Meca J,Marın-Martınez F et al.Assessing het-
erogeneityin meta-analysis:Q statistic or I2 index? Psychol Methods
2006;11:193–206.
27. Cox H, Puffer S, Morton V et al. Educating nursing home staff on fracture
prevention: A cluster randomized trial. Age Ageing 2008;37:167 –172.
28. Ward JA, Harden M, Gibson RE et al. A cluster randomised controlled
trial to preventinjury due to falls in a residentialaged care population.
Med J Aust 2010;192:319–322.
29. Lapane K,Hughes CM,Daiello LA et al.Effect of a pharmacist-led multi-
componentintervention focusing on the medication monitoring phase to
prevent potentialadverse drug events in nursing homes.J Am Geriatr Soc
2011;59:1238–1245.
30. Patterson SM,Hughes CM, Crealey G et al.An evaluation of an adapted
U.S. modelof pharmaceuticalcare to improve psychoactive prescribing for
nursing home residents in Northern Ireland (Fleetwood Northern Ireland
Study). J Am Geriatr Soc 2010;58:44–53.
31. Law M, WithersH, Morris J et al. Vitamin D supplementation and the
prevention offractures and falls:Results ofa randomized trialin elderly
people in residential accommodation. Age Ageing 2006;35:482 –486.
32. Schoenfelder DP.A fall prevention program for elderly individuals:Exer-
cise in long-term care settings. J Gerontol Nurs 2000;26:43–51.
33. Schnelle JF,Kapur K, Alessi C et al. Does an exercise and incontinence
intervention save healthcare costs in a nursing home population? J Am Ge-
riatr Soc 2003;51:161–168.
34. BeckerC, Kron M, Lindemann U et al. Effectivenessof a multifaceted
interventionon falls in nursing home residents.J Am Geriatr Soc
2003;51:306–313.
35. Rapp K, Lamb SE, B€uchele G et al.Prevention offalls in nursing homes:
Subgroup analysesof a randomized controlled trial.J Am Geriatr Soc
2008;56:1092–1097.
36. Dyer CA, Taylor GJ, Reed M et al. Falls prevention in residentialcare
homes: A randomized controlled trial. Age Ageing 2004;33:596 –602.
37. Kerse N, Peri K, Robinson E et al.Does a functionalactivity programme
improve function,quality of life,and falls for residents in long term care?
BMJ 2008;337:a1445.
38. McMurdo ME, Millar AM, Daly F. A randomized controlled trialof fall
prevention strategies in old peoples’ homes. Gerontology 2000;46:83 –87.
39. Neyens JC, Dijcks BP, Twisk J et al. A multifactorialintervention for the
prevention of falls in psychogeriatric nursing home patients,a randomized
controlled trial. Age Ageing 2009;38:194–199.
40. Ray WA, Taylor JA, Meador KG et al. A randomized trialof a consulta-
tion service to reduce falls in nursing homes. JAMA 1997;278:557 –562.
41. Lamb S, Jørstad-Stein E,Hauer K et al. Developmentof a common out-
come data set for fallinjury prevention of falls network Europe consensus.
J Am Geriatr Soc 2005;53:1618–1622.
42. Hauer K, Lamb S, Jorstad E et al. Systematic review ofdefinitionsand
methods of measuring falls in randomized controlled fallprevention trials.
Age Ageing 2006;35:5–10.
JAGS FEBRUARY 2015–VOL. 63, NO. 2 EFFECT OF FALL PREVENTION IN NURSING HOMES 221
nomic consequencesof nursing homefalls. Drugs Aging 2006;23:251–
262.
8. Scheffer AC,Schuurmans MJ,van Dijk N et al. Fear of falling:Measure-
ment strategy,prevalence,risk factors and consequences among older per-
sons. Age Ageing 2008;37:19–24.
9. Lamb SE, Becker C, Gillespie LD et al. Reporting of complex interventions
in clinicaltrials:Development of a taxonomy to classify and describe fall-
prevention interventions. Trials 2011;12:125.
10. BeckerC, Rapp K. Fall prevention in nursing homes.Clin Geriatr Med
2010;26:693–704.
11. Vu MQ, Weintraub N, Rubenstein LZ. Falls in the nursing home: Are they
preventable? J Am Med Dir Assoc 2006;7:S53–S58.
12. Quigley P, Bulat T, Kurtzman E et al. Fall prevention and injury protection
for nursing home residents. J Am Med Dir Assoc 2010;11:284–293.
13. Cusimano MD, Kwok J, Spadafora K.Effectivenessof multifaceted fall-
prevention programs for elderly in residentialcare.Inj Prev 2008;14:113–
122.
14. NeyensJC, van HaastregtJC, Dijcks BP et al. Falls in elderly people in
long-term care facilities:A systematic review of RCTs.J Am Med Dir As-
soc 2011;12:410–425.
15. Cameron ID,Gillespie LD,Robertson MC et al.Interventions for prevent-
ing falls in older people in nursing care facilities and hospitals.Cochrane
Database Syst Rev 2012;12:CD005465.
16. Oliver D, Connelly JB, Victor CR et al. Strategies to prevent falls and frac-
tures in hospitals and care homes and effect of cognitive impairment:Sys-
tematic review and meta-analyses. BMJ 2007;334:82.
17. Gillespie LD,Robertson MC,Gillespie WJ et al.Interventions for prevent-
ing falls in older people in the community.Cochrane Database SystRev
2012;9:CD007146.
18. InternationalProspective Register of Systematic Reviews,PROSPERO [on-
line]. Available at www.crd.york.ac.uk/prospero/AccessedAugust 12,
2012.
19. Liberati A, Altman D, Tetzlaff J et al. The PRISMA statement for reporting
systematic reviewsand meta-analysesof studiesthat evaluate healthcare
interventions: Explanation and elaboration. BMJ 2009;339:b2700.
20. Moher D, LiberatiA, Tetzlaff J et al.Preferred reporting items for system-
atic review and meta-analyses:The PRISMA statement.PLoS Med 2009;6:
e1000097.
21. Cameron I, Murray GR, Gillespie LD et al. Interventionsfor preventing
falls in older people in residentialcare facilities and hospitals (protocol).
Cochrane Database Syst Rev 2005;3:CD005465.
22. Wang MC, Bushman BJ. IntegratingResults Through Meta-Analytic
Review Using SASâ Software. Cary, NC: SAS Institute Inc, 1999.
23. Rendina-Gobioff G, Kromrey JD. PUB_BIAS: A SASâ Macro for Detecting.
Publication Biasin Meta-Analysis[on-line].Available at www.analytics.
ncsu.edu/sesug/2006/PO04_06.PDF Accessed January 20, 2013.
24. Duval S, Tweedie R. A simple funnel-plot-based method oftesting and
adjusting for publication bias in meta-analysis.Biometrics 2000;56:
455–463.
25. Cooper H, HedgesLV, eds.The Handbook of Research Synthesis.New
York: Russell Sage Foundation, 1994.
26. Huedo-Medina T,Sanchez-Meca J,Marın-Martınez F et al.Assessing het-
erogeneityin meta-analysis:Q statistic or I2 index? Psychol Methods
2006;11:193–206.
27. Cox H, Puffer S, Morton V et al. Educating nursing home staff on fracture
prevention: A cluster randomized trial. Age Ageing 2008;37:167 –172.
28. Ward JA, Harden M, Gibson RE et al. A cluster randomised controlled
trial to preventinjury due to falls in a residentialaged care population.
Med J Aust 2010;192:319–322.
29. Lapane K,Hughes CM,Daiello LA et al.Effect of a pharmacist-led multi-
componentintervention focusing on the medication monitoring phase to
prevent potentialadverse drug events in nursing homes.J Am Geriatr Soc
2011;59:1238–1245.
30. Patterson SM,Hughes CM, Crealey G et al.An evaluation of an adapted
U.S. modelof pharmaceuticalcare to improve psychoactive prescribing for
nursing home residents in Northern Ireland (Fleetwood Northern Ireland
Study). J Am Geriatr Soc 2010;58:44–53.
31. Law M, WithersH, Morris J et al. Vitamin D supplementation and the
prevention offractures and falls:Results ofa randomized trialin elderly
people in residential accommodation. Age Ageing 2006;35:482 –486.
32. Schoenfelder DP.A fall prevention program for elderly individuals:Exer-
cise in long-term care settings. J Gerontol Nurs 2000;26:43–51.
33. Schnelle JF,Kapur K, Alessi C et al. Does an exercise and incontinence
intervention save healthcare costs in a nursing home population? J Am Ge-
riatr Soc 2003;51:161–168.
34. BeckerC, Kron M, Lindemann U et al. Effectivenessof a multifaceted
interventionon falls in nursing home residents.J Am Geriatr Soc
2003;51:306–313.
35. Rapp K, Lamb SE, B€uchele G et al.Prevention offalls in nursing homes:
Subgroup analysesof a randomized controlled trial.J Am Geriatr Soc
2008;56:1092–1097.
36. Dyer CA, Taylor GJ, Reed M et al. Falls prevention in residentialcare
homes: A randomized controlled trial. Age Ageing 2004;33:596 –602.
37. Kerse N, Peri K, Robinson E et al.Does a functionalactivity programme
improve function,quality of life,and falls for residents in long term care?
BMJ 2008;337:a1445.
38. McMurdo ME, Millar AM, Daly F. A randomized controlled trialof fall
prevention strategies in old peoples’ homes. Gerontology 2000;46:83 –87.
39. Neyens JC, Dijcks BP, Twisk J et al. A multifactorialintervention for the
prevention of falls in psychogeriatric nursing home patients,a randomized
controlled trial. Age Ageing 2009;38:194–199.
40. Ray WA, Taylor JA, Meador KG et al. A randomized trialof a consulta-
tion service to reduce falls in nursing homes. JAMA 1997;278:557 –562.
41. Lamb S, Jørstad-Stein E,Hauer K et al. Developmentof a common out-
come data set for fallinjury prevention of falls network Europe consensus.
J Am Geriatr Soc 2005;53:1618–1622.
42. Hauer K, Lamb S, Jorstad E et al. Systematic review ofdefinitionsand
methods of measuring falls in randomized controlled fallprevention trials.
Age Ageing 2006;35:5–10.
JAGS FEBRUARY 2015–VOL. 63, NO. 2 EFFECT OF FALL PREVENTION IN NURSING HOMES 221
1 out of 11
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.