Clinical Leadership to Develop Nursing Practice
VerifiedAdded on 2023/05/28
|15
|3677
|422
AI Summary
The article discusses the importance of clinical leadership in developing nursing practice and improving patient outcomes. It highlights the use of SBAR communication tool and transformational leadership in nursing. The article also provides evidence-based research to support the implementation of these practices.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: CLINICAL LEADERSHIP TO DEVELOP NURSING PRACTICE
CLINICAL LEADERSHIP TO DEVELOP NURSING PRACTICE
Name of student:
Name of university:
Author Note:
CLINICAL LEADERSHIP TO DEVELOP NURSING PRACTICE
Name of student:
Name of university:
Author Note:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1CLINICAL LEADERSHIP TO DEVELOP NURSING PRACTICE
I am a registered nurse working in the emergency department. Our nursing challenges involve
to improve patient satisfaction and quality of health care. A patient Julie has been admitted
with injuries due to road traffic accident. She has developed infections at the injury site and
received antibiotic administration after a gap of 8 hours post presentation. This resulted in
serious consequences with manifestations of sepsis and cellulites due to lack of
communication and team work coordination in transitional care. I have performed research
on transitional care errors; I will discuss that evidence based practice can benefit health care
professionals to increase patient outcomes by improving patient safety and reducing
treatment accidents. Accurate nursing practice is brought about through transformational
leadership skills in nursing profession, which can bring significant improvement in patient
health quality (Beckett et al., 2013). I will provide a summary and analysis of evidences
unfolded during my literature research. Finally, I will provide an implementation plan on new
nursing practice with the help of transformational leadership qualities to minimize the
transitional care errors.
In Julie’s case, she reported with injuries in face, legs and jaws in the emergency
department where she underwent a delay in antibiotic administration and shifted to a medical
ward. She was manifested with sepsis and cellulites. At the point of emergency admission,
there was a delayed approach by the health care staffs. Adequate immediate supportive
therapy to manage the accidental trauma was lacking; a generalised evaluation approach was
performed by the emergency management team. The patient was thereafter shifted to the
general ward and prescribed antibiotics to relieve associated fever and infections.
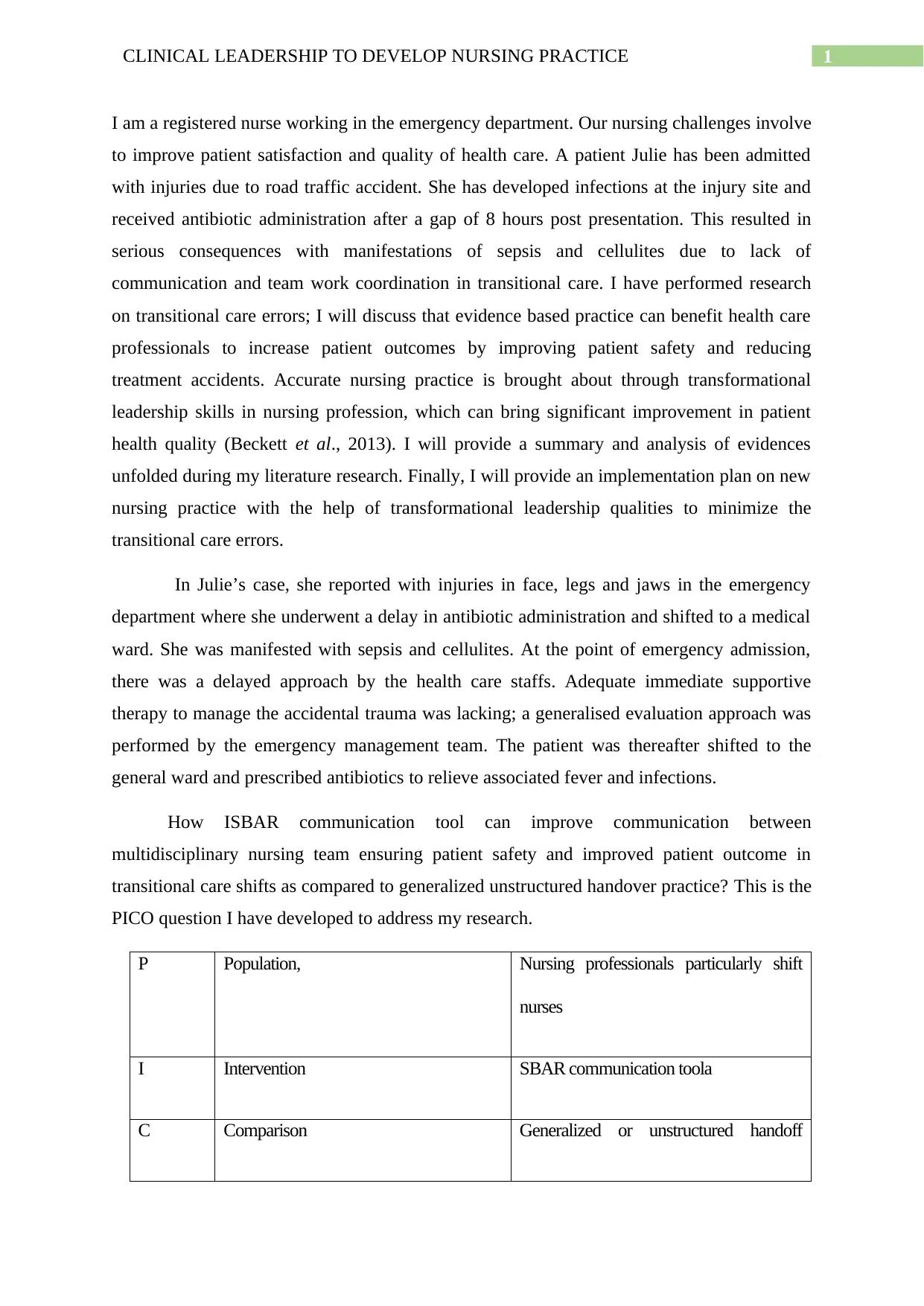
How ISBAR communication tool can improve communication between
multidisciplinary nursing team ensuring patient safety and improved patient outcome in
transitional care shifts as compared to generalized unstructured handover practice? This is the
PICO question I have developed to address my research.
P Population, Nursing professionals particularly shift
nurses
I Intervention SBAR communication toola
C Comparison Generalized or unstructured handoff
I am a registered nurse working in the emergency department. Our nursing challenges involve
to improve patient satisfaction and quality of health care. A patient Julie has been admitted
with injuries due to road traffic accident. She has developed infections at the injury site and
received antibiotic administration after a gap of 8 hours post presentation. This resulted in
serious consequences with manifestations of sepsis and cellulites due to lack of
communication and team work coordination in transitional care. I have performed research
on transitional care errors; I will discuss that evidence based practice can benefit health care
professionals to increase patient outcomes by improving patient safety and reducing
treatment accidents. Accurate nursing practice is brought about through transformational
leadership skills in nursing profession, which can bring significant improvement in patient
health quality (Beckett et al., 2013). I will provide a summary and analysis of evidences
unfolded during my literature research. Finally, I will provide an implementation plan on new
nursing practice with the help of transformational leadership qualities to minimize the
transitional care errors.
In Julie’s case, she reported with injuries in face, legs and jaws in the emergency
department where she underwent a delay in antibiotic administration and shifted to a medical
ward. She was manifested with sepsis and cellulites. At the point of emergency admission,
there was a delayed approach by the health care staffs. Adequate immediate supportive
therapy to manage the accidental trauma was lacking; a generalised evaluation approach was
performed by the emergency management team. The patient was thereafter shifted to the
general ward and prescribed antibiotics to relieve associated fever and infections.
How ISBAR communication tool can improve communication between
multidisciplinary nursing team ensuring patient safety and improved patient outcome in
transitional care shifts as compared to generalized unstructured handover practice? This is the
PICO question I have developed to address my research.
P Population, Nursing professionals particularly shift
nurses
I Intervention SBAR communication toola
C Comparison Generalized or unstructured handoff
2CLINICAL LEADERSHIP TO DEVELOP NURSING PRACTICE
practice
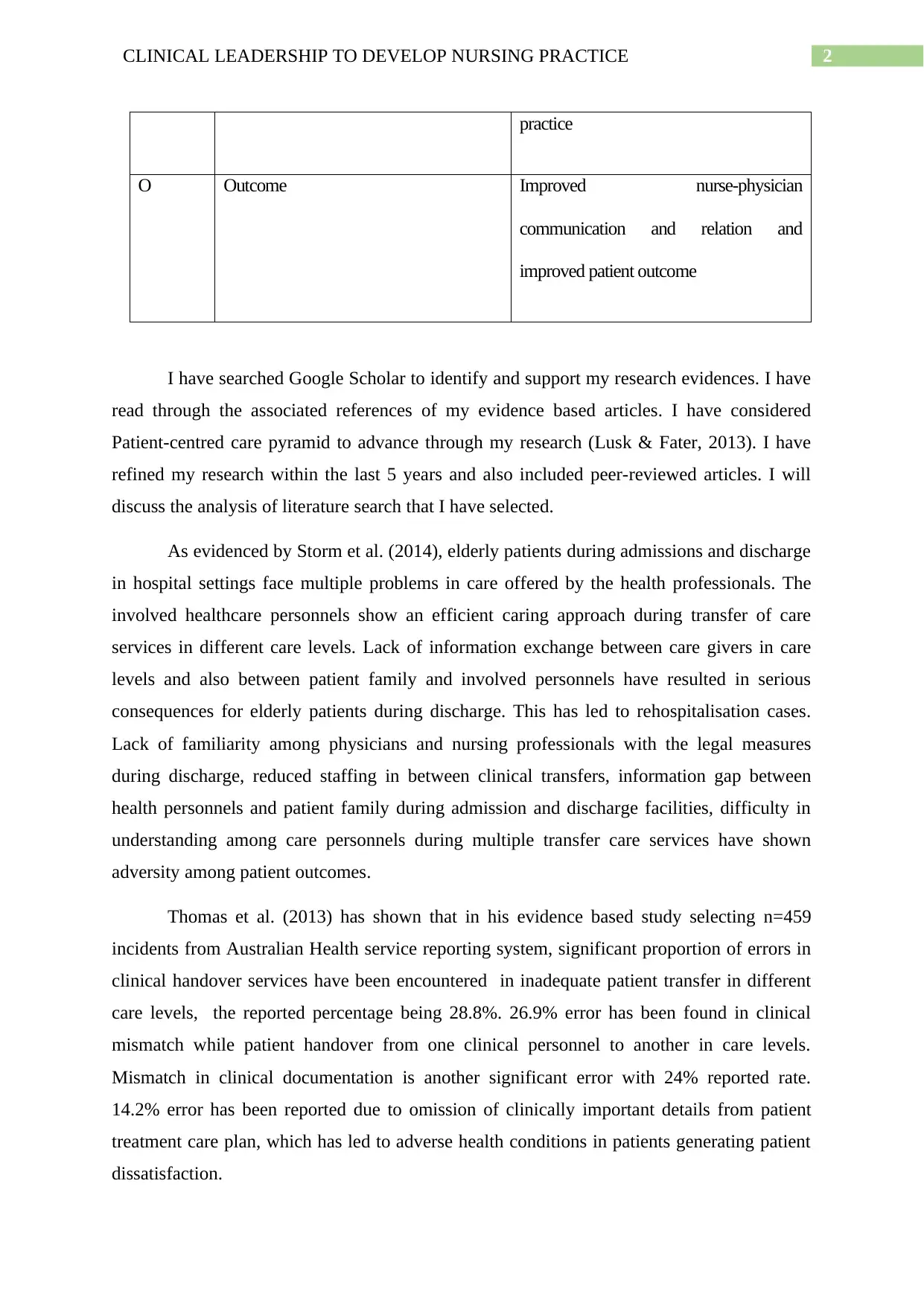
O Outcome Improved nurse-physician
communication and relation and
improved patient outcome
I have searched Google Scholar to identify and support my research evidences. I have
read through the associated references of my evidence based articles. I have considered
Patient-centred care pyramid to advance through my research (Lusk & Fater, 2013). I have
refined my research within the last 5 years and also included peer-reviewed articles. I will
discuss the analysis of literature search that I have selected.
As evidenced by Storm et al. (2014), elderly patients during admissions and discharge
in hospital settings face multiple problems in care offered by the health professionals. The
involved healthcare personnels show an efficient caring approach during transfer of care
services in different care levels. Lack of information exchange between care givers in care
levels and also between patient family and involved personnels have resulted in serious
consequences for elderly patients during discharge. This has led to rehospitalisation cases.
Lack of familiarity among physicians and nursing professionals with the legal measures
during discharge, reduced staffing in between clinical transfers, information gap between
health personnels and patient family during admission and discharge facilities, difficulty in
understanding among care personnels during multiple transfer care services have shown
adversity among patient outcomes.
Thomas et al. (2013) has shown that in his evidence based study selecting n=459
incidents from Australian Health service reporting system, significant proportion of errors in
clinical handover services have been encountered in inadequate patient transfer in different
care levels, the reported percentage being 28.8%. 26.9% error has been found in clinical
mismatch while patient handover from one clinical personnel to another in care levels.
Mismatch in clinical documentation is another significant error with 24% reported rate.
14.2% error has been reported due to omission of clinically important details from patient
treatment care plan, which has led to adverse health conditions in patients generating patient
dissatisfaction.
practice
O Outcome Improved nurse-physician
communication and relation and
improved patient outcome
I have searched Google Scholar to identify and support my research evidences. I have
read through the associated references of my evidence based articles. I have considered
Patient-centred care pyramid to advance through my research (Lusk & Fater, 2013). I have
refined my research within the last 5 years and also included peer-reviewed articles. I will
discuss the analysis of literature search that I have selected.
As evidenced by Storm et al. (2014), elderly patients during admissions and discharge
in hospital settings face multiple problems in care offered by the health professionals. The
involved healthcare personnels show an efficient caring approach during transfer of care
services in different care levels. Lack of information exchange between care givers in care
levels and also between patient family and involved personnels have resulted in serious
consequences for elderly patients during discharge. This has led to rehospitalisation cases.
Lack of familiarity among physicians and nursing professionals with the legal measures
during discharge, reduced staffing in between clinical transfers, information gap between
health personnels and patient family during admission and discharge facilities, difficulty in
understanding among care personnels during multiple transfer care services have shown
adversity among patient outcomes.
Thomas et al. (2013) has shown that in his evidence based study selecting n=459
incidents from Australian Health service reporting system, significant proportion of errors in
clinical handover services have been encountered in inadequate patient transfer in different
care levels, the reported percentage being 28.8%. 26.9% error has been found in clinical
mismatch while patient handover from one clinical personnel to another in care levels.
Mismatch in clinical documentation is another significant error with 24% reported rate.
14.2% error has been reported due to omission of clinically important details from patient
treatment care plan, which has led to adverse health conditions in patients generating patient
dissatisfaction.
3CLINICAL LEADERSHIP TO DEVELOP NURSING PRACTICE
The systemic review performed by Roughead et al. (2016) showed that medication
errors leading to adverse drug reactions among patients are concerned areas where proper
interpretation and improved efficiency are necessary to reduce deterioration of patients’
health quality. Medical drug errors are due to inefficient knowledge and lack of
communication among health care staffs operating at different health care levels. Lack of
well documented approach on medication during discharge of patients has been significantly
higher. Medication errors during a patient’s stay in hospital has therefore resulted in
considerable increase in medication costs.
Considering the reviews of Allen et al. (2014), database search and literature reviews
have shown that transitional care inefficiency has resulted in rehospitalisation of patients;
patients have to stay for longer periods during rehospitalisation. There was lack of
involvement of patients and their families during decision making regarding patient
assistance. Lack of coordinated and collaborative efforts among nursing officials and
involved multidisciplinary team have resulted in inefficient multiple transfer care facilities.
Evidence based nursing practice to improve patient care during transitional care shifts
is to implement SBAR communication tool to enable a collaborative communication strategy
among health care teams (DeMeester et al., 2013). Collaborative communication and
efficient coordination among a multidisciplinary team are essential for successful treatment
care and patient safety. Lack of communication among health care team members during shift
transfers is a major cause for patients’ health adversity (Robinson & Dearmon, 2013). SBAR
communication tool gives a description of the situation (S) with which the patient has been
reported in hospitals. The background (B) section of the tool gives a description of medical
details of the patient relating to current medical issue and the assessment (A) section
determines the patient health status in current scenario and new assessment data. (R) section
provides a recommendation in terms of treatment changes, consultation requirements or
transfers (Martin & Ciurzynski, 2015). This communication handover tool bridges the
communication gap between physician and nurse in a multidisciplinary assistance. The
SBAR handoff tool maintains a continuous flow of information during multiple transfer
activities (Cornell et al., 2014). The SBAR method of communication increases the
confidence of the nurses in between shift transfer and enable them to have a detailed
knowledge of individual patient. This eliminates adverse patient outcomes by reducing
medication errors and improving timed management of patient care by shift nurses.
The systemic review performed by Roughead et al. (2016) showed that medication
errors leading to adverse drug reactions among patients are concerned areas where proper
interpretation and improved efficiency are necessary to reduce deterioration of patients’
health quality. Medical drug errors are due to inefficient knowledge and lack of
communication among health care staffs operating at different health care levels. Lack of
well documented approach on medication during discharge of patients has been significantly
higher. Medication errors during a patient’s stay in hospital has therefore resulted in
considerable increase in medication costs.
Considering the reviews of Allen et al. (2014), database search and literature reviews
have shown that transitional care inefficiency has resulted in rehospitalisation of patients;
patients have to stay for longer periods during rehospitalisation. There was lack of
involvement of patients and their families during decision making regarding patient
assistance. Lack of coordinated and collaborative efforts among nursing officials and
involved multidisciplinary team have resulted in inefficient multiple transfer care facilities.
Evidence based nursing practice to improve patient care during transitional care shifts
is to implement SBAR communication tool to enable a collaborative communication strategy
among health care teams (DeMeester et al., 2013). Collaborative communication and
efficient coordination among a multidisciplinary team are essential for successful treatment
care and patient safety. Lack of communication among health care team members during shift
transfers is a major cause for patients’ health adversity (Robinson & Dearmon, 2013). SBAR
communication tool gives a description of the situation (S) with which the patient has been
reported in hospitals. The background (B) section of the tool gives a description of medical
details of the patient relating to current medical issue and the assessment (A) section
determines the patient health status in current scenario and new assessment data. (R) section
provides a recommendation in terms of treatment changes, consultation requirements or
transfers (Martin & Ciurzynski, 2015). This communication handover tool bridges the
communication gap between physician and nurse in a multidisciplinary assistance. The
SBAR handoff tool maintains a continuous flow of information during multiple transfer
activities (Cornell et al., 2014). The SBAR method of communication increases the
confidence of the nurses in between shift transfer and enable them to have a detailed
knowledge of individual patient. This eliminates adverse patient outcomes by reducing
medication errors and improving timed management of patient care by shift nurses.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4CLINICAL LEADERSHIP TO DEVELOP NURSING PRACTICE
Transformational leadership development in nursing provides an organisational
approach to improve the nursing performance and improve patient outcomes.
Transformational leadership skills are integral to the nursing management to enable the
nursing officials to arrange a workforce and identify the required change in practice.
Transformational leadership style enables the nurses to work effectively and guide a vision to
improve nursing practice to increase patient safety and outcomes. Transformational
leadership is rooted to four components: idealized influence, inspirational motivation,
intellectual stimulation and individual consideration (Zhu et al., 2013). The transformational
leader possessing idealized influence characteristic provide themselves as a role model to
other team members and encourage them to meet the patient needs overcoming all obstacles.
The component of inspirational motivation enables optimistic approach to a change
adaptation in nursing practice and guides through a compelling vision. It gives a confidence
to all the nurses to accept challenges with enthusiasm and instills a high team spirit
(Giltinane, 2013). Intellectual stimulation factor of transformational leadership allows the
nurses to seek different perspectives in critical analysis and solving problems. Non-traditional
thinking approaches are also allowed in changed practice. The final component of
transformational leadership is individualized consideration where the transformational leader
provides education to the team members and followers and promote self-development. This
allows consideration of individual concerns and help team members to develop strengths in
promoting changed nursing practice (Wong, Cummings & Bucharme, 2013). All these
components of transformational leadership are integrated to develop patient centred care
approach.
Transformational leadership in new nursing practice is possible in supportive and
optimistic environments, where every team member engage with each other to allow for
blending of their creative imagination and vision to develop organisational capacity (Wang &
Liu., 2015).
Transformational leadership is obtained with accuracy through application of
Registered nurse standards to incorporate new nursing practice in hospital settings (Ross et
al., 2013). Standard 1, 2, 4, 5 and 7 are critical for implementing a new nursing practice and
achieve improved patient outcomes.
In clinical settings under my supervision, I would implement SBAR communication
tool to promote patient centred care through maintaining streamline flow of information
Transformational leadership development in nursing provides an organisational
approach to improve the nursing performance and improve patient outcomes.
Transformational leadership skills are integral to the nursing management to enable the
nursing officials to arrange a workforce and identify the required change in practice.
Transformational leadership style enables the nurses to work effectively and guide a vision to
improve nursing practice to increase patient safety and outcomes. Transformational
leadership is rooted to four components: idealized influence, inspirational motivation,
intellectual stimulation and individual consideration (Zhu et al., 2013). The transformational
leader possessing idealized influence characteristic provide themselves as a role model to
other team members and encourage them to meet the patient needs overcoming all obstacles.
The component of inspirational motivation enables optimistic approach to a change
adaptation in nursing practice and guides through a compelling vision. It gives a confidence
to all the nurses to accept challenges with enthusiasm and instills a high team spirit
(Giltinane, 2013). Intellectual stimulation factor of transformational leadership allows the
nurses to seek different perspectives in critical analysis and solving problems. Non-traditional
thinking approaches are also allowed in changed practice. The final component of
transformational leadership is individualized consideration where the transformational leader
provides education to the team members and followers and promote self-development. This
allows consideration of individual concerns and help team members to develop strengths in
promoting changed nursing practice (Wong, Cummings & Bucharme, 2013). All these
components of transformational leadership are integrated to develop patient centred care
approach.
Transformational leadership in new nursing practice is possible in supportive and
optimistic environments, where every team member engage with each other to allow for
blending of their creative imagination and vision to develop organisational capacity (Wang &
Liu., 2015).
Transformational leadership is obtained with accuracy through application of
Registered nurse standards to incorporate new nursing practice in hospital settings (Ross et
al., 2013). Standard 1, 2, 4, 5 and 7 are critical for implementing a new nursing practice and
achieve improved patient outcomes.
In clinical settings under my supervision, I would implement SBAR communication
tool to promote patient centred care through maintaining streamline flow of information

5CLINICAL LEADERSHIP TO DEVELOP NURSING PRACTICE
exchange. I would initially discuss with the healthcare team about the use of SBAR
communication tool as a handoff approach during multiple shift transfers. A formatted
standard protocol would be designed on how to use SBAR tool during shift transfers. I would
ensure that short term training sessions are arranged to develop and improve the
communication style between shift clinicians. I would allocate specific roles to shift nurses as
a part of SBAR implementation program. A checklist criteria would be maintained as a part
of SBAR tool use. The nursing management team would be responsible for initial monitoring
to check whether the shift nurses are performing efficiently and accurately according to the
checklist criteria (Hutchinson & Jackson, 2013). Frequent training on communication style
development would be arranged for bridging the communication gap among different shift
nurses (Curtis et al., 2013). A team of nurses would be appointed to take regular follow ups
immediately after patient transfers to check whether accurate diagnostic assessment of
patients are followed according to (S) and (B) sections of SBAR communication tool. A web
based transfer of patients’ medical details would be allowed between multiple shift rooms to
minimise documentation mismatch, thereby promoting greater screening and assessing time
to individual patients.
exchange. I would initially discuss with the healthcare team about the use of SBAR
communication tool as a handoff approach during multiple shift transfers. A formatted
standard protocol would be designed on how to use SBAR tool during shift transfers. I would
ensure that short term training sessions are arranged to develop and improve the
communication style between shift clinicians. I would allocate specific roles to shift nurses as
a part of SBAR implementation program. A checklist criteria would be maintained as a part
of SBAR tool use. The nursing management team would be responsible for initial monitoring
to check whether the shift nurses are performing efficiently and accurately according to the
checklist criteria (Hutchinson & Jackson, 2013). Frequent training on communication style
development would be arranged for bridging the communication gap among different shift
nurses (Curtis et al., 2013). A team of nurses would be appointed to take regular follow ups
immediately after patient transfers to check whether accurate diagnostic assessment of
patients are followed according to (S) and (B) sections of SBAR communication tool. A web
based transfer of patients’ medical details would be allowed between multiple shift rooms to
minimise documentation mismatch, thereby promoting greater screening and assessing time
to individual patients.
6CLINICAL LEADERSHIP TO DEVELOP NURSING PRACTICE
Reference Author
validity
Method
& where it fits on
the evidence
pyramid
Aim/Question Setting Results Limitations Implication
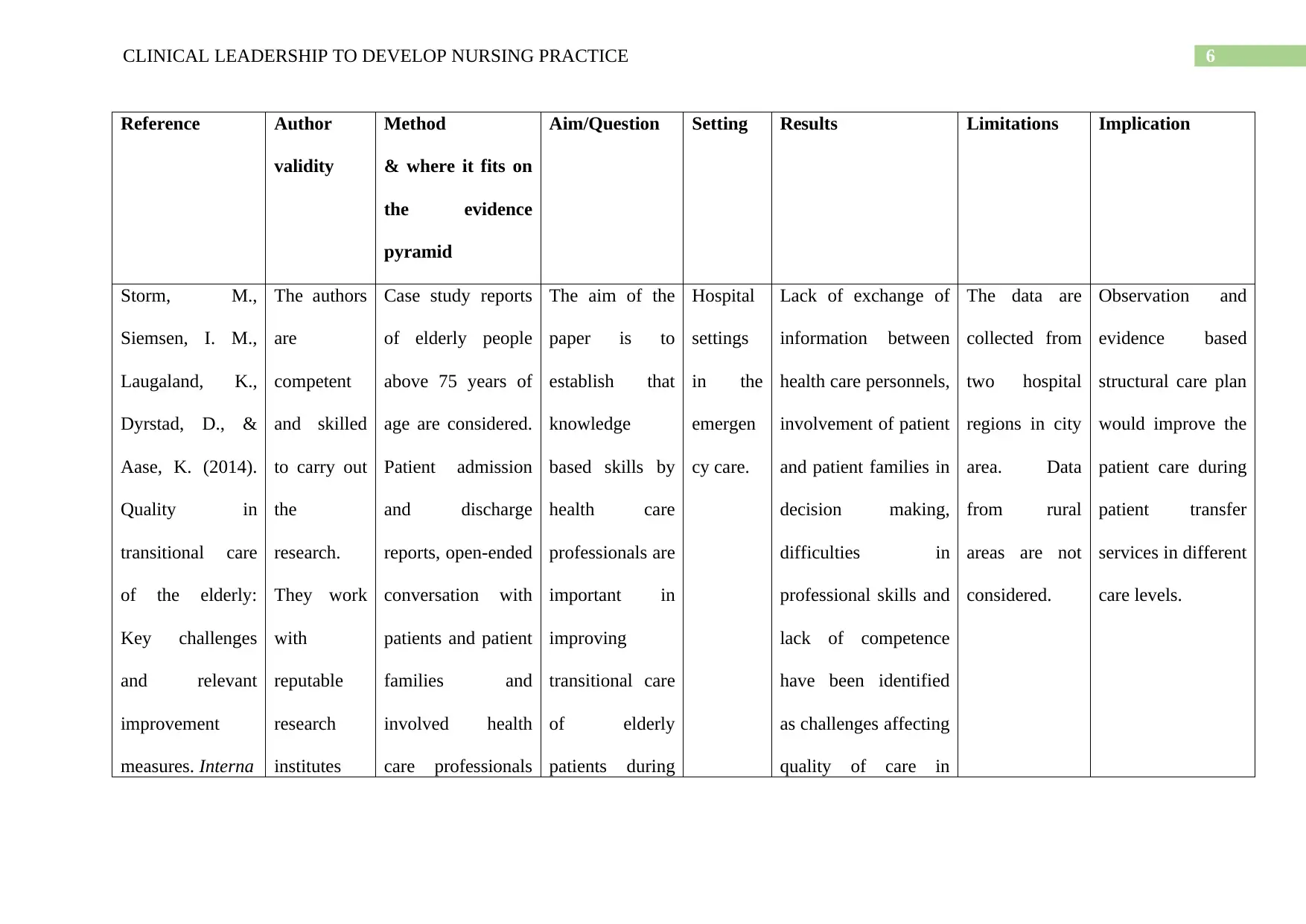
Storm, M.,
Siemsen, I. M.,
Laugaland, K.,
Dyrstad, D., &
Aase, K. (2014).
Quality in
transitional care
of the elderly:
Key challenges
and relevant
improvement
measures. Interna
The authors
are
competent
and skilled
to carry out
the
research.
They work
with
reputable
research
institutes
Case study reports
of elderly people
above 75 years of
age are considered.
Patient admission
and discharge
reports, open-ended
conversation with
patients and patient
families and
involved health
care professionals
The aim of the
paper is to
establish that
knowledge
based skills by
health care
professionals are
important in
improving
transitional care
of elderly
patients during
Hospital
settings
in the
emergen
cy care.
Lack of exchange of
information between
health care personnels,
involvement of patient
and patient families in
decision making,
difficulties in
professional skills and
lack of competence
have been identified
as challenges affecting
quality of care in
The data are
collected from
two hospital
regions in city
area. Data
from rural
areas are not
considered.
Observation and
evidence based
structural care plan
would improve the
patient care during
patient transfer
services in different
care levels.
Reference Author
validity
Method
& where it fits on
the evidence
pyramid
Aim/Question Setting Results Limitations Implication
Storm, M.,
Siemsen, I. M.,
Laugaland, K.,
Dyrstad, D., &
Aase, K. (2014).
Quality in
transitional care
of the elderly:
Key challenges
and relevant
improvement
measures. Interna
The authors
are
competent
and skilled
to carry out
the
research.
They work
with
reputable
research
institutes
Case study reports
of elderly people
above 75 years of
age are considered.
Patient admission
and discharge
reports, open-ended
conversation with
patients and patient
families and
involved health
care professionals
The aim of the
paper is to
establish that
knowledge
based skills by
health care
professionals are
important in
improving
transitional care
of elderly
patients during
Hospital
settings
in the
emergen
cy care.
Lack of exchange of
information between
health care personnels,
involvement of patient
and patient families in
decision making,
difficulties in
professional skills and
lack of competence
have been identified
as challenges affecting
quality of care in
The data are
collected from
two hospital
regions in city
area. Data
from rural
areas are not
considered.
Observation and
evidence based
structural care plan
would improve the
patient care during
patient transfer
services in different
care levels.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7CLINICAL LEADERSHIP TO DEVELOP NURSING PRACTICE
tional Journal of
Integrated
Care, 14(2).
and their
qualificatio
ns are valid.
They have
no conflict
of interest.
are performed.
Thematic
observational
approach is
considered.
transfer of
patient services.
It provides a
suggestion of
implementation
measures
considering the
issues affecting
transitional care
of elderly
patients.
transitional settings
during transfer of
patient services in
different health care
levels. Gap in
knowledge skills
among health care
professionals have
been identified as
major challenge in
transitional care
inefficiency.
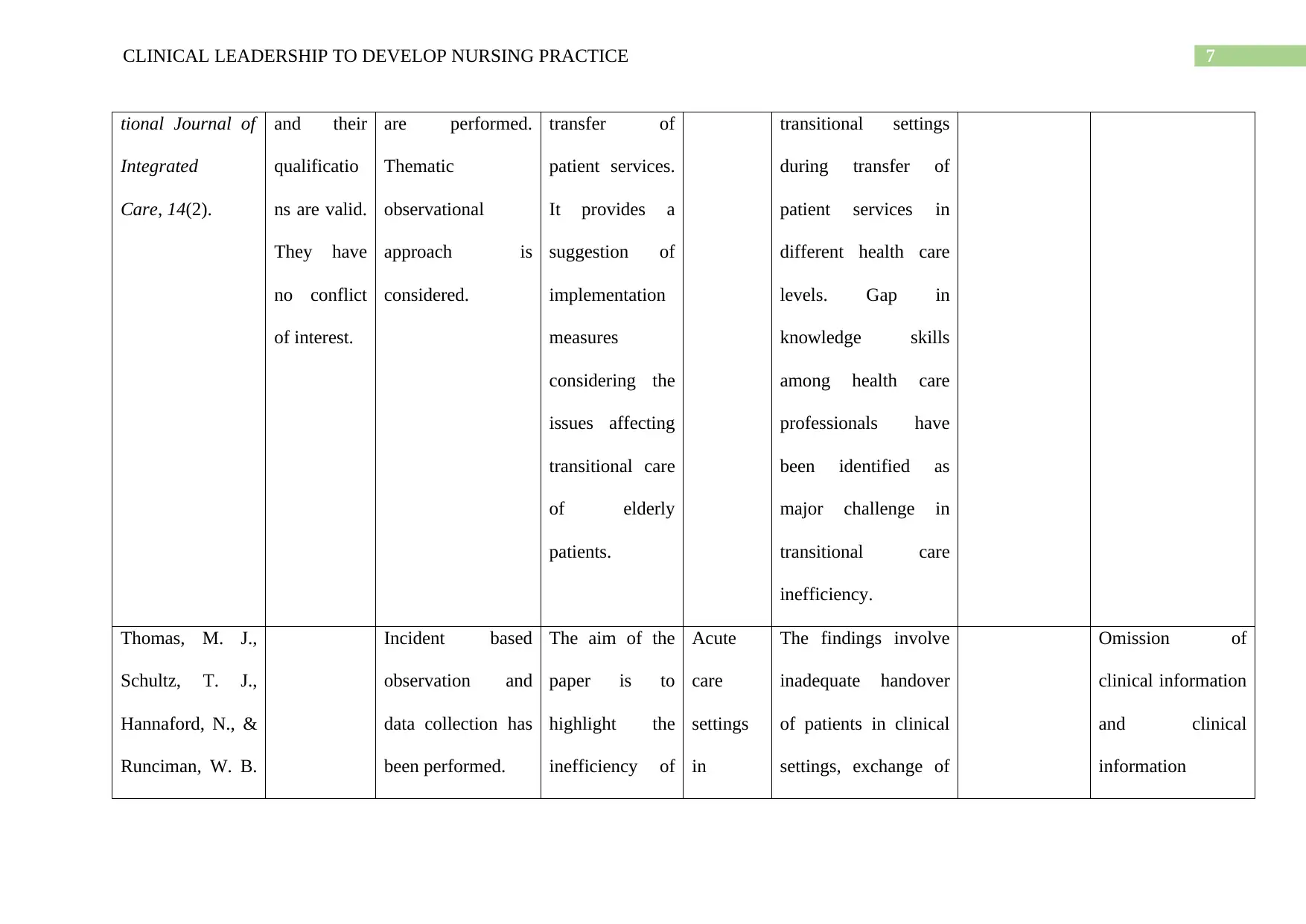
Thomas, M. J.,
Schultz, T. J.,
Hannaford, N., &
Runciman, W. B.
Incident based
observation and
data collection has
been performed.
The aim of the
paper is to
highlight the
inefficiency of
Acute
care
settings
in
The findings involve
inadequate handover
of patients in clinical
settings, exchange of
Omission of
clinical information
and clinical
information
tional Journal of
Integrated
Care, 14(2).
and their
qualificatio
ns are valid.
They have
no conflict
of interest.
are performed.
Thematic
observational
approach is
considered.
transfer of
patient services.
It provides a
suggestion of
implementation
measures
considering the
issues affecting
transitional care
of elderly
patients.
transitional settings
during transfer of
patient services in
different health care
levels. Gap in
knowledge skills
among health care
professionals have
been identified as
major challenge in
transitional care
inefficiency.
Thomas, M. J.,
Schultz, T. J.,
Hannaford, N., &
Runciman, W. B.
Incident based
observation and
data collection has
been performed.
The aim of the
paper is to
highlight the
inefficiency of
Acute
care
settings
in
The findings involve
inadequate handover
of patients in clinical
settings, exchange of
Omission of
clinical information
and clinical
information

8CLINICAL LEADERSHIP TO DEVELOP NURSING PRACTICE
(2013). Failures
in transition:
learning from
incidents relating
to clinical
handover in acute
care. Journal for
Healthcare
Quality, 35(3),
49-56.
clinical
handover care
due to errors
during patient
handover of
patient details
between health
care personnels
in acute care
settings to
provide the
basis of strategic
implementation
of improved
clinical practice.
hospitals. patients’ clinical
documented reports
with other patients,
omission of clinical
information of
patients’ clinical
health care plan as the
major challenges in
clinical handover of
patients among
different health
personnels.
mismatch can be
prevented through
a structured
approach of
standardised
information set to
ensure that clinical
details of patients
are not mismatched
or omitted.
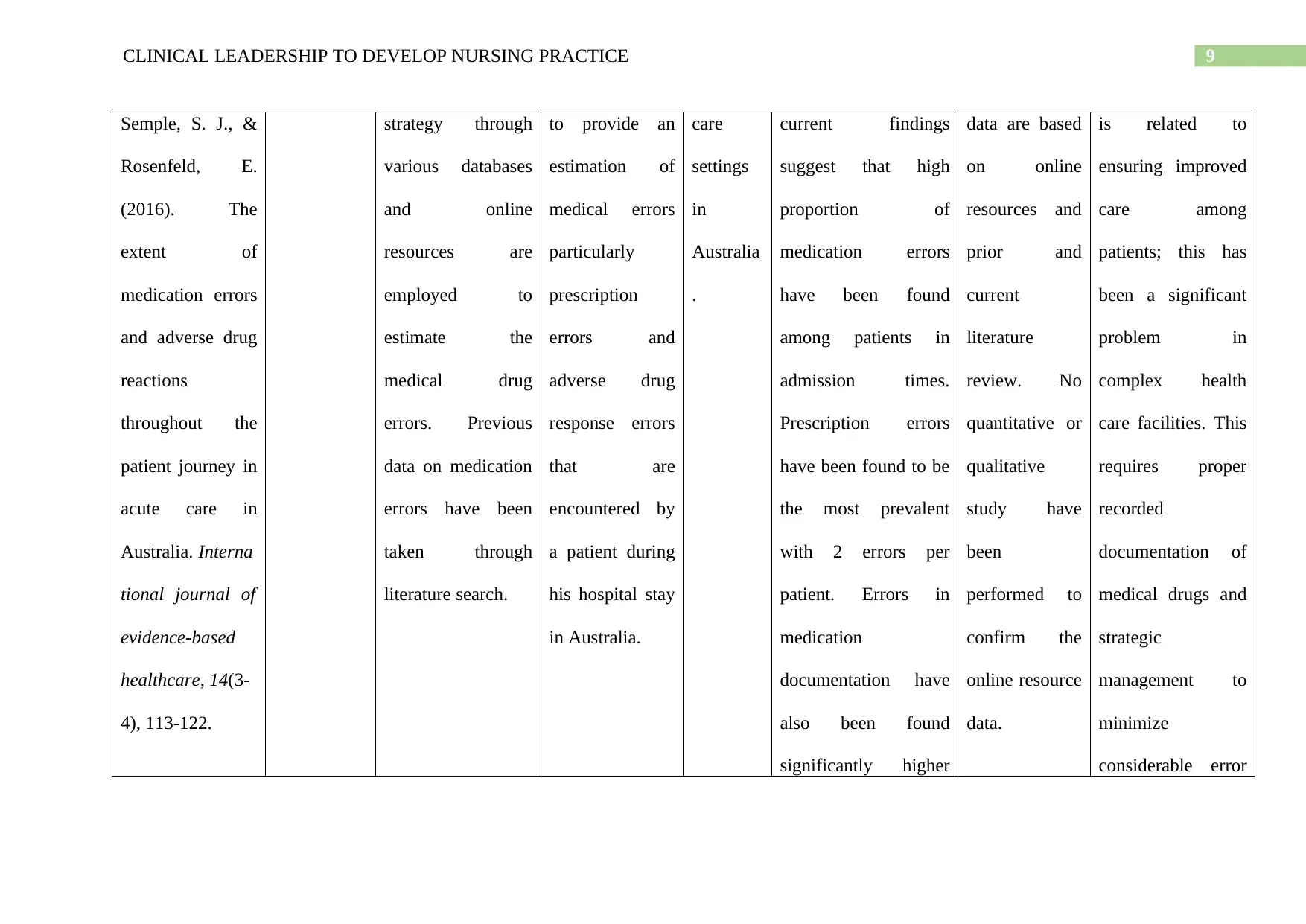
Roughead, E. E., Online search The paper aims Acute The previous and The research Medication safety
(2013). Failures
in transition:
learning from
incidents relating
to clinical
handover in acute
care. Journal for
Healthcare
Quality, 35(3),
49-56.
clinical
handover care
due to errors
during patient
handover of
patient details
between health
care personnels
in acute care
settings to
provide the
basis of strategic
implementation
of improved
clinical practice.
hospitals. patients’ clinical
documented reports
with other patients,
omission of clinical
information of
patients’ clinical
health care plan as the
major challenges in
clinical handover of
patients among
different health
personnels.
mismatch can be
prevented through
a structured
approach of
standardised
information set to
ensure that clinical
details of patients
are not mismatched
or omitted.
Roughead, E. E., Online search The paper aims Acute The previous and The research Medication safety
9CLINICAL LEADERSHIP TO DEVELOP NURSING PRACTICE
Semple, S. J., &
Rosenfeld, E.
(2016). The
extent of
medication errors
and adverse drug
reactions
throughout the
patient journey in
acute care in
Australia. Interna
tional journal of
evidence-based
healthcare, 14(3-
4), 113-122.
strategy through
various databases
and online
resources are
employed to
estimate the
medical drug
errors. Previous
data on medication
errors have been
taken through
literature search.
to provide an
estimation of
medical errors
particularly
prescription
errors and
adverse drug
response errors
that are
encountered by
a patient during
his hospital stay
in Australia.
care
settings
in
Australia
.
current findings
suggest that high
proportion of
medication errors
have been found
among patients in
admission times.
Prescription errors
have been found to be
the most prevalent
with 2 errors per
patient. Errors in
medication
documentation have
also been found
significantly higher
data are based
on online
resources and
prior and
current
literature
review. No
quantitative or
qualitative
study have
been
performed to
confirm the
online resource
data.
is related to
ensuring improved
care among
patients; this has
been a significant
problem in
complex health
care facilities. This
requires proper
recorded
documentation of
medical drugs and
strategic
management to
minimize
considerable error
Semple, S. J., &
Rosenfeld, E.
(2016). The
extent of
medication errors
and adverse drug
reactions
throughout the
patient journey in
acute care in
Australia. Interna
tional journal of
evidence-based
healthcare, 14(3-
4), 113-122.
strategy through
various databases
and online
resources are
employed to
estimate the
medical drug
errors. Previous
data on medication
errors have been
taken through
literature search.
to provide an
estimation of
medical errors
particularly
prescription
errors and
adverse drug
response errors
that are
encountered by
a patient during
his hospital stay
in Australia.
care
settings
in
Australia
.
current findings
suggest that high
proportion of
medication errors
have been found
among patients in
admission times.
Prescription errors
have been found to be
the most prevalent
with 2 errors per
patient. Errors in
medication
documentation have
also been found
significantly higher
data are based
on online
resources and
prior and
current
literature
review. No
quantitative or
qualitative
study have
been
performed to
confirm the
online resource
data.
is related to
ensuring improved
care among
patients; this has
been a significant
problem in
complex health
care facilities. This
requires proper
recorded
documentation of
medical drugs and
strategic
management to
minimize
considerable error
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10CLINICAL LEADERSHIP TO DEVELOP NURSING PRACTICE
during patient
discharge from
hospitals.
rates.
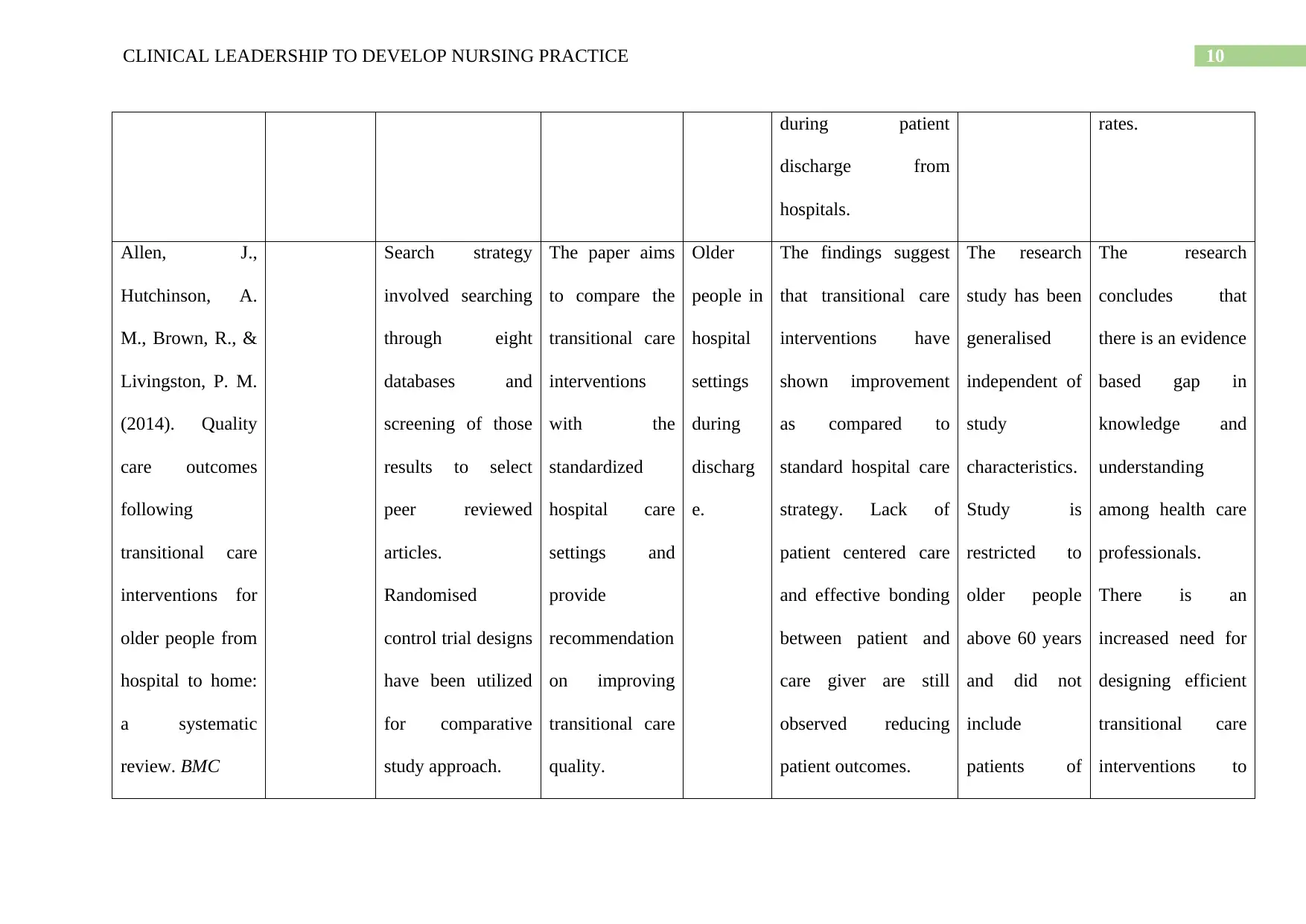
Allen, J.,
Hutchinson, A.
M., Brown, R., &
Livingston, P. M.
(2014). Quality
care outcomes
following
transitional care
interventions for
older people from
hospital to home:
a systematic
review. BMC
Search strategy
involved searching
through eight
databases and
screening of those
results to select
peer reviewed
articles.
Randomised
control trial designs
have been utilized
for comparative
study approach.
The paper aims
to compare the
transitional care
interventions
with the
standardized
hospital care
settings and
provide
recommendation
on improving
transitional care
quality.
Older
people in
hospital
settings
during
discharg
e.
The findings suggest
that transitional care
interventions have
shown improvement
as compared to
standard hospital care
strategy. Lack of
patient centered care
and effective bonding
between patient and
care giver are still
observed reducing
patient outcomes.
The research
study has been
generalised
independent of
study
characteristics.
Study is
restricted to
older people
above 60 years
and did not
include
patients of
The research
concludes that
there is an evidence
based gap in
knowledge and
understanding
among health care
professionals.
There is an
increased need for
designing efficient
transitional care
interventions to
during patient
discharge from
hospitals.
rates.
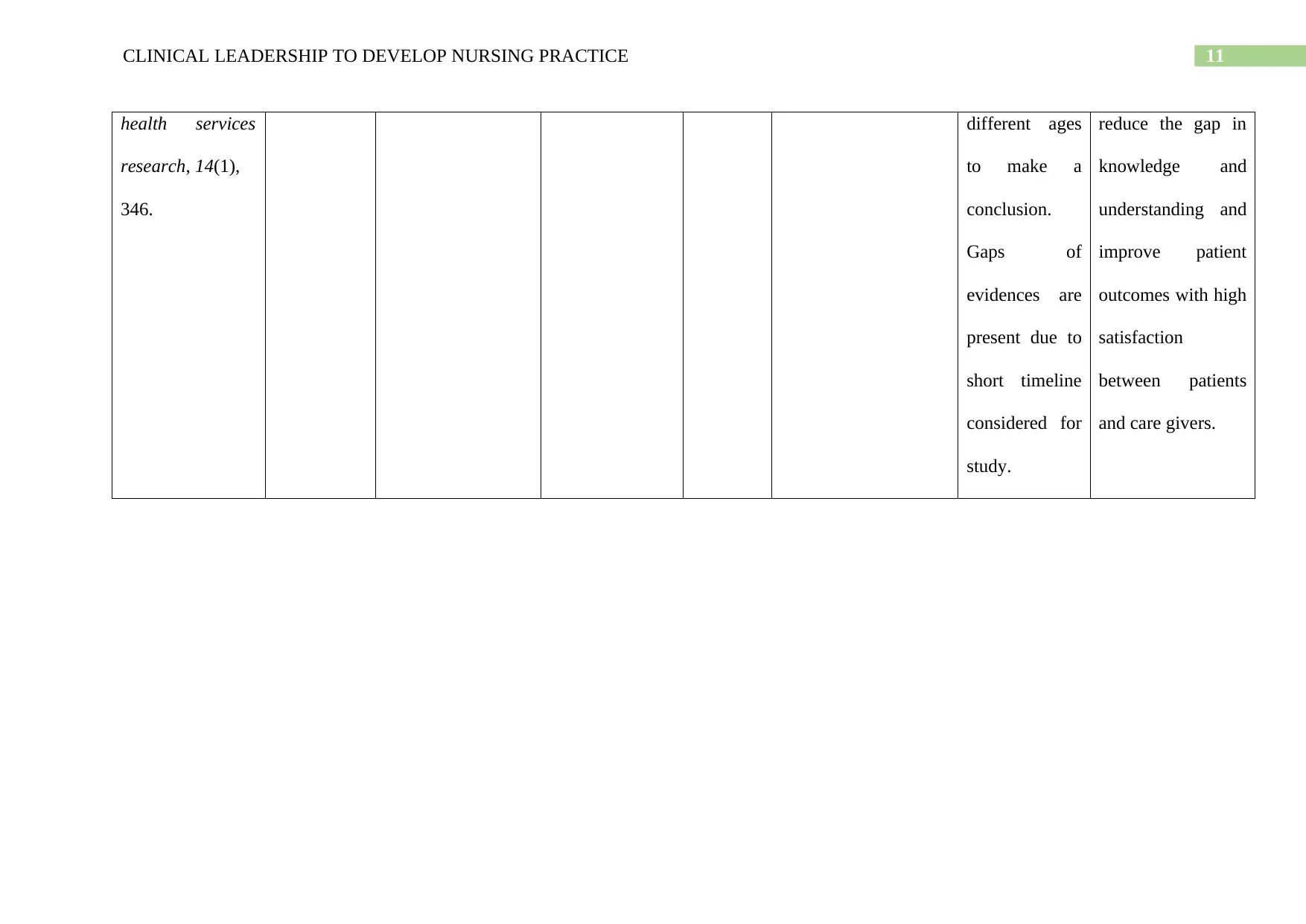
Allen, J.,
Hutchinson, A.
M., Brown, R., &
Livingston, P. M.
(2014). Quality
care outcomes
following
transitional care
interventions for
older people from
hospital to home:
a systematic
review. BMC
Search strategy
involved searching
through eight
databases and
screening of those
results to select
peer reviewed
articles.
Randomised
control trial designs
have been utilized
for comparative
study approach.
The paper aims
to compare the
transitional care
interventions
with the
standardized
hospital care
settings and
provide
recommendation
on improving
transitional care
quality.
Older
people in
hospital
settings
during
discharg
e.
The findings suggest
that transitional care
interventions have
shown improvement
as compared to
standard hospital care
strategy. Lack of
patient centered care
and effective bonding
between patient and
care giver are still
observed reducing
patient outcomes.
The research
study has been
generalised
independent of
study
characteristics.
Study is
restricted to
older people
above 60 years
and did not
include
patients of
The research
concludes that
there is an evidence
based gap in
knowledge and
understanding
among health care
professionals.
There is an
increased need for
designing efficient
transitional care
interventions to
11CLINICAL LEADERSHIP TO DEVELOP NURSING PRACTICE
health services
research, 14(1),
346.
different ages
to make a
conclusion.
Gaps of
evidences are
present due to
short timeline
considered for
study.
reduce the gap in
knowledge and
understanding and
improve patient
outcomes with high
satisfaction
between patients
and care givers.
health services
research, 14(1),
346.
different ages
to make a
conclusion.
Gaps of
evidences are
present due to
short timeline
considered for
study.
reduce the gap in
knowledge and
understanding and
improve patient
outcomes with high
satisfaction
between patients
and care givers.
12CLINICAL LEADERSHIP TO DEVELOP NURSING PRACTICE
References:
Allen, J., Hutchinson, A. M., Brown, R., & Livingston, P. M. (2014). Quality care outcomes
following transitional care interventions for older people from hospital to home: a
systematic review. BMC health services research, 14(1), 346.
Beckett, P., Field, J., Molloy, L., Yu, N., Holmes, D., & Pile, E. (2013). Practice what you
preach: developing person-centred culture in inpatient mental health settings through
strengths-based, transformational leadership. Issues in mental health nursing, 34(8),
595-601.
Cornell, P., Gervis, M. T., Yates, L., & Vardaman, J. M. (2014). Impact of SBAR on nurse
shift reports and staff rounding. Medsurg nursing, 23(5), 334.
Curtis, J. R., Back, A. L., Ford, D. W., Downey, L., Shannon, S. E., Doorenbos, A. Z., ... &
Arnold, R. W. (2013). Effect of communication skills training for residents and nurse
practitioners on quality of communication with patients with serious illness: a
randomized trial. Jama, 310(21), 2271-2281.
De Meester, K., Verspuy, M., Monsieurs, K. G., & Van Bogaert, P. (2013). SBAR improves
nurse–physician communication and reduces unexpected death: A pre and post
intervention study. Resuscitation, 84(9), 1192-1196.
Giltinane, C. L. (2013). Leadership styles and theories. Nursing Standard, 27(41).
Hutchinson, M., & Jackson, D. (2013). Transformational leadership in nursing: towards a
more critical interpretation. Nursing inquiry, 20(1), 11-22.
Lusk, J. M., & Fater, K. (2013). A concept analysis of patient‐centered care. In Nursing
Forum (Vol. 48, No. 2, pp. 89-98).
References:
Allen, J., Hutchinson, A. M., Brown, R., & Livingston, P. M. (2014). Quality care outcomes
following transitional care interventions for older people from hospital to home: a
systematic review. BMC health services research, 14(1), 346.
Beckett, P., Field, J., Molloy, L., Yu, N., Holmes, D., & Pile, E. (2013). Practice what you
preach: developing person-centred culture in inpatient mental health settings through
strengths-based, transformational leadership. Issues in mental health nursing, 34(8),
595-601.
Cornell, P., Gervis, M. T., Yates, L., & Vardaman, J. M. (2014). Impact of SBAR on nurse
shift reports and staff rounding. Medsurg nursing, 23(5), 334.
Curtis, J. R., Back, A. L., Ford, D. W., Downey, L., Shannon, S. E., Doorenbos, A. Z., ... &
Arnold, R. W. (2013). Effect of communication skills training for residents and nurse
practitioners on quality of communication with patients with serious illness: a
randomized trial. Jama, 310(21), 2271-2281.
De Meester, K., Verspuy, M., Monsieurs, K. G., & Van Bogaert, P. (2013). SBAR improves
nurse–physician communication and reduces unexpected death: A pre and post
intervention study. Resuscitation, 84(9), 1192-1196.
Giltinane, C. L. (2013). Leadership styles and theories. Nursing Standard, 27(41).
Hutchinson, M., & Jackson, D. (2013). Transformational leadership in nursing: towards a
more critical interpretation. Nursing inquiry, 20(1), 11-22.
Lusk, J. M., & Fater, K. (2013). A concept analysis of patient‐centered care. In Nursing
Forum (Vol. 48, No. 2, pp. 89-98).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13CLINICAL LEADERSHIP TO DEVELOP NURSING PRACTICE
Martin, H. A., & Ciurzynski, S. M. (2015). Situation, background, assessment, and
recommendation–Guided huddles improve communication and teamwork in the
emergency department. Journal of Emergency Nursing, 41(6), 484-488.
Robinson, B. K., & Dearmon, V. (2013). Evidence-based nursing education: Effective use of
instructional design and simulated learning environments to enhance knowledge
transfer in undergraduate nursing students. Journal of Professional Nursing, 29(4),
203-209.
Ross, E. J., Fitzpatrick, J. J., Click, E. R., Krouse, H. J., & Clavelle, J. T. (2014).
Transformational leadership practices of nurse leaders in professional nursing
associations. Journal of Nursing Administration, 44(4), 201-206.
Roughead, E. E., Semple, S. J., & Rosenfeld, E. (2016). The extent of medication errors and
adverse drug reactions throughout the patient journey in acute care in
Australia. International journal of evidence-based healthcare, 14(3-4), 113-122.
Storm, M., Siemsen, I. M., Laugaland, K., Dyrstad, D., & Aase, K. (2014). Quality in
transitional care of the elderly: Key challenges and relevant improvement
measures. International Journal of Integrated Care, 14(2).
Thomas, M. J., Schultz, T. J., Hannaford, N., & Runciman, W. B. (2013). Failures in
transition: learning from incidents relating to clinical handover in acute care. Journal
for Healthcare Quality, 35(3), 49-56.
Wang, S., & Liu, Y. (2015). Impact of professional nursing practice environment and
psychological empowerment on nurses' work engagement: test of structural equation
modelling. Journal of Nursing Management, 23(3), 287-296.
Martin, H. A., & Ciurzynski, S. M. (2015). Situation, background, assessment, and
recommendation–Guided huddles improve communication and teamwork in the
emergency department. Journal of Emergency Nursing, 41(6), 484-488.
Robinson, B. K., & Dearmon, V. (2013). Evidence-based nursing education: Effective use of
instructional design and simulated learning environments to enhance knowledge
transfer in undergraduate nursing students. Journal of Professional Nursing, 29(4),
203-209.
Ross, E. J., Fitzpatrick, J. J., Click, E. R., Krouse, H. J., & Clavelle, J. T. (2014).
Transformational leadership practices of nurse leaders in professional nursing
associations. Journal of Nursing Administration, 44(4), 201-206.
Roughead, E. E., Semple, S. J., & Rosenfeld, E. (2016). The extent of medication errors and
adverse drug reactions throughout the patient journey in acute care in
Australia. International journal of evidence-based healthcare, 14(3-4), 113-122.
Storm, M., Siemsen, I. M., Laugaland, K., Dyrstad, D., & Aase, K. (2014). Quality in
transitional care of the elderly: Key challenges and relevant improvement
measures. International Journal of Integrated Care, 14(2).
Thomas, M. J., Schultz, T. J., Hannaford, N., & Runciman, W. B. (2013). Failures in
transition: learning from incidents relating to clinical handover in acute care. Journal
for Healthcare Quality, 35(3), 49-56.
Wang, S., & Liu, Y. (2015). Impact of professional nursing practice environment and
psychological empowerment on nurses' work engagement: test of structural equation
modelling. Journal of Nursing Management, 23(3), 287-296.
14CLINICAL LEADERSHIP TO DEVELOP NURSING PRACTICE
Wong, C. A., Cummings, G. G., & Ducharme, L. (2013). The relationship between nursing
leadership and patient outcomes: a systematic review update. Journal of nursing
management, 21(5), 709-724.
Zhu, W., Newman, A., Miao, Q., & Hooke, A. (2013). Revisiting the mediating role of trust
in transformational leadership effects: Do different types of trust make a
difference?. The Leadership Quarterly, 24(1), 94-105.
Wong, C. A., Cummings, G. G., & Ducharme, L. (2013). The relationship between nursing
leadership and patient outcomes: a systematic review update. Journal of nursing
management, 21(5), 709-724.
Zhu, W., Newman, A., Miao, Q., & Hooke, A. (2013). Revisiting the mediating role of trust
in transformational leadership effects: Do different types of trust make a
difference?. The Leadership Quarterly, 24(1), 94-105.
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





