Analyzing Ischemic Stroke with the Clinical Reasoning Cycle Framework
VerifiedAdded on 2022/11/25
|10
|2434
|139
Report
AI Summary
This report presents a comprehensive analysis of an ischemic stroke case study, utilizing the clinical reasoning cycle to guide nursing care. The assignment begins by considering the patient's situation and collecting relevant cues, including the patient's medical history of hypertension, gout, and acute myocardial infarction, lifestyle factors like smoking and excessive working hours, and clinical findings such as elevated cholesterol and blood glucose levels. The report then identifies ischemic stroke as the primary complication, supported by the patient's history and clinical presentation. The pathophysiology of ischemic stroke is discussed, emphasizing the abrupt cessation of blood supply to the brain. Based on this, the report establishes goals, including maintaining airway, breathing, and circulation and preventing further complications. Nursing interventions, both pharmacological (e.g., Metoprolol, Aspirin) and non-pharmacological (lifestyle modifications), are outlined. The report concludes with an evaluation of the nursing care, highlighting positive outcomes and the patient's understanding of their condition. The reflection emphasizes the value of the clinical reasoning cycle in providing effective nursing care for ischemic stroke.
Clinical reasoning cycle – Ischemic stroke
Introduction
Clinical reasoning cycle is the process helps the nurse to execute the nursing care for better
outcomes. There are eight steps involved in the clinical reasoning cycle, The possibility
developing the complication, The complications that are related to the case scenario, The
complications that are related to the case scenario, Discussion on the Pathophysiology of
ischemic stroke, setting goals to reduce the risk of developing the complication, Evaluation of
the nursing care are implemented for the better outcome of the patient and for the learning
purpose. (Thampy,2019). This assignment assists in executing the nursing care using clinical
reasoning cycle. The case study of Mr. Tomasi Joni shows that he is suffering from ischemic
stroke. He has a history of hypertension, gout and had acute myocardial Infarction in2016.
The nurse was planning nursing care based on the clinical reasoning cycle. Clinical reasoning
is the essential nursing skill used in this case to critically analyse the patient’s condition. The
critical analysis helps to plan medical treatment and nursing interventions. Evaluation is the
final process of clinical reasoning cycle that helps the nurse to assess the outcome.
Consider the patient situation and collect information
The possibility of Mr. Joni developing the complication is due to various contributing factors.
(Levett-Jones et al., 2009). Critical analysis of the case study shows that the problem is
accompanied by several contributing factors. The factors that contribute to the problem are
age, work, stress, lack of adequate rest, not able to engage in social activities due to lack of
time, and smoking. Other contributing factors are hypertension, history of acute myocardial
infarction, and family history of hyperlipidemia He has a history of hypertension, gout and
had acute myocardial Infarction in 2016. On average he works 50hours/week. He drinks beer
Introduction
Clinical reasoning cycle is the process helps the nurse to execute the nursing care for better
outcomes. There are eight steps involved in the clinical reasoning cycle, The possibility
developing the complication, The complications that are related to the case scenario, The
complications that are related to the case scenario, Discussion on the Pathophysiology of
ischemic stroke, setting goals to reduce the risk of developing the complication, Evaluation of
the nursing care are implemented for the better outcome of the patient and for the learning
purpose. (Thampy,2019). This assignment assists in executing the nursing care using clinical
reasoning cycle. The case study of Mr. Tomasi Joni shows that he is suffering from ischemic
stroke. He has a history of hypertension, gout and had acute myocardial Infarction in2016.
The nurse was planning nursing care based on the clinical reasoning cycle. Clinical reasoning
is the essential nursing skill used in this case to critically analyse the patient’s condition. The
critical analysis helps to plan medical treatment and nursing interventions. Evaluation is the
final process of clinical reasoning cycle that helps the nurse to assess the outcome.
Consider the patient situation and collect information
The possibility of Mr. Joni developing the complication is due to various contributing factors.
(Levett-Jones et al., 2009). Critical analysis of the case study shows that the problem is
accompanied by several contributing factors. The factors that contribute to the problem are
age, work, stress, lack of adequate rest, not able to engage in social activities due to lack of
time, and smoking. Other contributing factors are hypertension, history of acute myocardial
infarction, and family history of hyperlipidemia He has a history of hypertension, gout and
had acute myocardial Infarction in 2016. On average he works 50hours/week. He drinks beer
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
once in a week and smokes one packet of cigarettes a week. He eats takeaway three times a
week. He also has the complaints of Obstructive Sleep Apnoea (OSA) and requires CPAP for
overnight sleep. His family history states that his father died of hyperlipidemia and stroke.
Joni’s Age, occupation, family history, past and present medical history are the major factors
that increase the possibility of joni developing the Ischemic stroke. According to his health
assessment findings, his weight is 93kgs and has excess abdominal fat. His cholesterol level
is 9.2mmol/L and fasting BGL is 9.6mmol/L. Albumin to creatinine ratio is 10mg/mmol.
Joni’s clinical findings during the time of admission are the evidence that confirms the
possibility of Ischemic stroke.
Process information and identify the issue
The complications that are related to the case scenario are an ischemic stroke. (Turpin, 2017).
Critical analysis with the support of literature and case scenario aids to conclude the
complication. Patient’s past and present medical history are the primary factors that prove the
possibility of developing the complication. Patient’s blood pressure is increased which is
related to ischemic heart disease. Uncontrolled increased blood pressure can cause the blood
vessels in the brain to burst which leads to ischemic stroke. Hyperlipidemia leads to coronary
atherosclerosis which is the major cause for the ischemic stroke. His saturation on assessment
is 96% on room air which indicates that there is less oxygen concentration in the blood. Less
oxygen in the blood can increase the complications of ischemic stroke. His vital signs are
slightly elevated. He has the family history of hyperlipidemia and he weighs 93 kgs which are
not appropriate for his height and excess abdominal fat and his waist circumference is 104cm
which may increase the chances of ischemic stroke. His Total cholesterol level is 9.2mmol/L
which shows that his cholesterol level is increased. He has excess abdominal fat evident.
Waist circumference 104cm also increases the possibility of developing
week. He also has the complaints of Obstructive Sleep Apnoea (OSA) and requires CPAP for
overnight sleep. His family history states that his father died of hyperlipidemia and stroke.
Joni’s Age, occupation, family history, past and present medical history are the major factors
that increase the possibility of joni developing the Ischemic stroke. According to his health
assessment findings, his weight is 93kgs and has excess abdominal fat. His cholesterol level
is 9.2mmol/L and fasting BGL is 9.6mmol/L. Albumin to creatinine ratio is 10mg/mmol.
Joni’s clinical findings during the time of admission are the evidence that confirms the
possibility of Ischemic stroke.
Process information and identify the issue
The complications that are related to the case scenario are an ischemic stroke. (Turpin, 2017).
Critical analysis with the support of literature and case scenario aids to conclude the
complication. Patient’s past and present medical history are the primary factors that prove the
possibility of developing the complication. Patient’s blood pressure is increased which is
related to ischemic heart disease. Uncontrolled increased blood pressure can cause the blood
vessels in the brain to burst which leads to ischemic stroke. Hyperlipidemia leads to coronary
atherosclerosis which is the major cause for the ischemic stroke. His saturation on assessment
is 96% on room air which indicates that there is less oxygen concentration in the blood. Less
oxygen in the blood can increase the complications of ischemic stroke. His vital signs are
slightly elevated. He has the family history of hyperlipidemia and he weighs 93 kgs which are
not appropriate for his height and excess abdominal fat and his waist circumference is 104cm
which may increase the chances of ischemic stroke. His Total cholesterol level is 9.2mmol/L
which shows that his cholesterol level is increased. He has excess abdominal fat evident.
Waist circumference 104cm also increases the possibility of developing
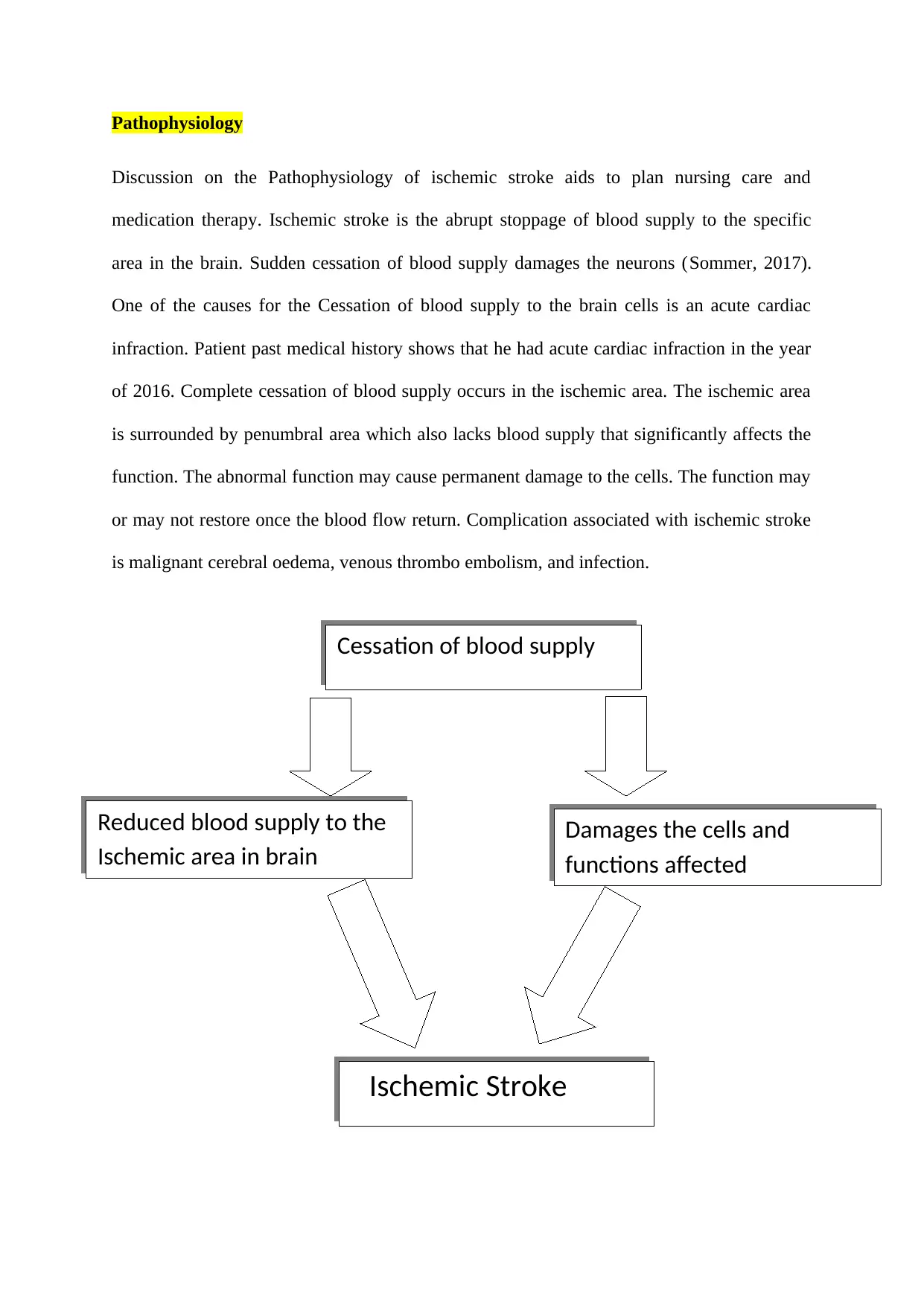
Pathophysiology
Discussion on the Pathophysiology of ischemic stroke aids to plan nursing care and
medication therapy. Ischemic stroke is the abrupt stoppage of blood supply to the specific
area in the brain. Sudden cessation of blood supply damages the neurons (Sommer, 2017).
One of the causes for the Cessation of blood supply to the brain cells is an acute cardiac
infraction. Patient past medical history shows that he had acute cardiac infraction in the year
of 2016. Complete cessation of blood supply occurs in the ischemic area. The ischemic area
is surrounded by penumbral area which also lacks blood supply that significantly affects the
function. The abnormal function may cause permanent damage to the cells. The function may
or may not restore once the blood flow return. Complication associated with ischemic stroke
is malignant cerebral oedema, venous thrombo embolism, and infection.
Cessation of blood supply
Reduced blood supply to the
Ischemic area in brain
Damages the cells and
functions affected
Ischemic Stroke
Discussion on the Pathophysiology of ischemic stroke aids to plan nursing care and
medication therapy. Ischemic stroke is the abrupt stoppage of blood supply to the specific
area in the brain. Sudden cessation of blood supply damages the neurons (Sommer, 2017).
One of the causes for the Cessation of blood supply to the brain cells is an acute cardiac
infraction. Patient past medical history shows that he had acute cardiac infraction in the year
of 2016. Complete cessation of blood supply occurs in the ischemic area. The ischemic area
is surrounded by penumbral area which also lacks blood supply that significantly affects the
function. The abnormal function may cause permanent damage to the cells. The function may
or may not restore once the blood flow return. Complication associated with ischemic stroke
is malignant cerebral oedema, venous thrombo embolism, and infection.
Cessation of blood supply
Reduced blood supply to the
Ischemic area in brain
Damages the cells and
functions affected
Ischemic Stroke
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Establishing the goal
Consulting with Mr. Joni two goals are set to reduce the risk of developing the complication.
Nursing goals for Mr. Joni is formulated based on causes, age, past medical history, and
present medical condition. Ischemic stroke is a medical emergency where the nurse has to set
short term goals. Rule out the cause for the ischemic attack.
Short term goal – Maintain Airway, breathing, and circulation
Short term and initial goal in the treatment of Joni includes maintenance of patent airway
which ensures the oxygen supply to all vital organs including the brain. Maintain normal
breathing and circulation which can be attained by the maintenance of patent airway. Monitor
heart rate, respiratory rate and saturation every half an hour and continue till it stabilizes.
Propose for the initial assessment including physical assessment, laboratory test, and imaging
studies.
Long term goal – prevention of complications
Prevention of further complications is also an essential and long term goal. Restoration of
physical and mental health of the patient is the long term goal which includes prevention of
acute myocardial infarction and ischemic stroke in the future. Limit the damage and
restoration of normal life style (Saver, 2016). Goals are set for the speedy recovery and better
wellbeing of the patient.
Nursing intervention
Non-Pharmacological management
Nursing interventions are implemented to achieve the goals. Nursing interventions are
formulated considering the nurse and the patient’s condition. Nursing interventions are
planned based on the information collected and problem identification. Patient’s life style,
Consulting with Mr. Joni two goals are set to reduce the risk of developing the complication.
Nursing goals for Mr. Joni is formulated based on causes, age, past medical history, and
present medical condition. Ischemic stroke is a medical emergency where the nurse has to set
short term goals. Rule out the cause for the ischemic attack.
Short term goal – Maintain Airway, breathing, and circulation
Short term and initial goal in the treatment of Joni includes maintenance of patent airway
which ensures the oxygen supply to all vital organs including the brain. Maintain normal
breathing and circulation which can be attained by the maintenance of patent airway. Monitor
heart rate, respiratory rate and saturation every half an hour and continue till it stabilizes.
Propose for the initial assessment including physical assessment, laboratory test, and imaging
studies.
Long term goal – prevention of complications
Prevention of further complications is also an essential and long term goal. Restoration of
physical and mental health of the patient is the long term goal which includes prevention of
acute myocardial infarction and ischemic stroke in the future. Limit the damage and
restoration of normal life style (Saver, 2016). Goals are set for the speedy recovery and better
wellbeing of the patient.
Nursing intervention
Non-Pharmacological management
Nursing interventions are implemented to achieve the goals. Nursing interventions are
formulated considering the nurse and the patient’s condition. Nursing interventions are
planned based on the information collected and problem identification. Patient’s life style,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
age, and his work contribute to the disease condition. The nurse has to plan nursing care
according to the contributing factors of the disease condition. Primary and immediate nursing
care includes the maintenance of patent airway by suctioning and insertion of endo tracheal
tube (Middleton, 2017). Patent airway improves breathing and circulation. Do a neurological
assessment to rule out the level of damage and level of consciousness of the patient.
Continuous monitoring of vital signs needs to be executed. Monitor blood pressure
(Threlkeld, 2017). Do physical examination to rule out the related contributing factors and
complications. Plan and implement laboratory tests and imaging studies to rule out the extent
of the damage.
Pharmacological management
Initiate medication therapy. Administer Metoprolol 100mg daily, Aspirin 100mg daily,
Allopurinol 500mg daily as per the direction of the concern doctors. Educate the patient
about the contributing factors of the disease condition. Advice the patient to stop smoking,
encourage home food and advice to reduce the food from taking away. Encourage the patient
to reduce the working hours per week and start exercise, low sodium, and low fat diet (Berge,
2019).
Evaluation
The strategies used for the nursing care of Mr. Joni are useful and effective. Evaluation of
nursing care enabled the nurse to assess the outcome of each nursing intervention
implemented (Purvis, 2017). It also enabled to rule out the effectiveness of each nursing
interventions and helped in finding the ineffective nursing interventions. Patient’s airway was
patent. Vital signs were normal and Spo2 is 99% in room air. On neurological assessment
patient was conscious and alert. The patient was oriented to place, and persons. His blood
pressure was stable. Medication therapy continued as per doctor’s order. The patient was
according to the contributing factors of the disease condition. Primary and immediate nursing
care includes the maintenance of patent airway by suctioning and insertion of endo tracheal
tube (Middleton, 2017). Patent airway improves breathing and circulation. Do a neurological
assessment to rule out the level of damage and level of consciousness of the patient.
Continuous monitoring of vital signs needs to be executed. Monitor blood pressure
(Threlkeld, 2017). Do physical examination to rule out the related contributing factors and
complications. Plan and implement laboratory tests and imaging studies to rule out the extent
of the damage.
Pharmacological management
Initiate medication therapy. Administer Metoprolol 100mg daily, Aspirin 100mg daily,
Allopurinol 500mg daily as per the direction of the concern doctors. Educate the patient
about the contributing factors of the disease condition. Advice the patient to stop smoking,
encourage home food and advice to reduce the food from taking away. Encourage the patient
to reduce the working hours per week and start exercise, low sodium, and low fat diet (Berge,
2019).
Evaluation
The strategies used for the nursing care of Mr. Joni are useful and effective. Evaluation of
nursing care enabled the nurse to assess the outcome of each nursing intervention
implemented (Purvis, 2017). It also enabled to rule out the effectiveness of each nursing
interventions and helped in finding the ineffective nursing interventions. Patient’s airway was
patent. Vital signs were normal and Spo2 is 99% in room air. On neurological assessment
patient was conscious and alert. The patient was oriented to place, and persons. His blood
pressure was stable. Medication therapy continued as per doctor’s order. The patient was
aware of the contributing factors of his disease condition. (Coombes, 2018). Patient
verbalised that he will reduce the number of cigarettes he smokes per week. He started taking
low sodium and low fat diet. The patient was aware of the ill effects of outside food and he
said that he will reduce the intake of food from takeaway. The patient understood the
importance of exercise and he verbalised that he will try to take week off and spend time with
family and involve himself in social activities.
Reflection
Implementation of clinical reasoning cycle in nursing practice helped the nurse to do
effective nursing care planning for the wellbeing and speedy recovery of the patient. Clinical
reasoning ensures health promotion and prevention of complication. Eight steps of the
clinical reasoning are implemented for the execution of the treatment for Mr. Tomasi Joni. He
is presented with Ischemic stroke with several contributing factors. The presentation includes
The possibility of Mr. Joni developing the complication is due to various contributing factors,
The complications that are related to the case scenario are ischemic stroke, Pathophysiology
of ischemic stroke, two goals are set to reduce the risk of developing the complication,
Nursing interventions were implemented to achieve the goals, evaluation of used strategies
used for the nursing care of Mr. Joni. Using the clinical reasoning cycle for the case study
improved my knowledge and understanding of the nursing practice. Speedy recovery of the
patient with limited complication is achieved. This presentation helped me to improve my
clinical knowledge on the history collection, planning the strategies and evaluating the
outcome. It also improved my decision making capability in the medical emergency.
References
Arch, A. E., Weisman, D. C., Coca, S., Nystrom, K. V., Wira III, C. R., & Schindler, J. L.
(2016). Missed ischemic stroke diagnosis in the emergency department by emergency
verbalised that he will reduce the number of cigarettes he smokes per week. He started taking
low sodium and low fat diet. The patient was aware of the ill effects of outside food and he
said that he will reduce the intake of food from takeaway. The patient understood the
importance of exercise and he verbalised that he will try to take week off and spend time with
family and involve himself in social activities.
Reflection
Implementation of clinical reasoning cycle in nursing practice helped the nurse to do
effective nursing care planning for the wellbeing and speedy recovery of the patient. Clinical
reasoning ensures health promotion and prevention of complication. Eight steps of the
clinical reasoning are implemented for the execution of the treatment for Mr. Tomasi Joni. He
is presented with Ischemic stroke with several contributing factors. The presentation includes
The possibility of Mr. Joni developing the complication is due to various contributing factors,
The complications that are related to the case scenario are ischemic stroke, Pathophysiology
of ischemic stroke, two goals are set to reduce the risk of developing the complication,
Nursing interventions were implemented to achieve the goals, evaluation of used strategies
used for the nursing care of Mr. Joni. Using the clinical reasoning cycle for the case study
improved my knowledge and understanding of the nursing practice. Speedy recovery of the
patient with limited complication is achieved. This presentation helped me to improve my
clinical knowledge on the history collection, planning the strategies and evaluating the
outcome. It also improved my decision making capability in the medical emergency.
References
Arch, A. E., Weisman, D. C., Coca, S., Nystrom, K. V., Wira III, C. R., & Schindler, J. L.
(2016). Missed ischemic stroke diagnosis in the emergency department by emergency
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
medicine and neurology services. Stroke, 47(3), 668-673
https://www.ahajournals.org/doi/full/10.1161/STROKEAHA.115.010613
Berge, E., & Sandercock, P. (2019). Specific treatment of acute ischemic stroke. Warlow's
Stroke: Practical Management, 587-656
https://onlinelibrary.wiley.com/doi/abs/10.1002/9781118492390.ch13
Coombes, J. A., Rowett, D., Whitty, J. A., & Cottrell, W. N. (2018). Use of a patient-centred
educational exchange (PCEE) to improve patient’s self-management of medicines
after a stroke: a randomised controlled trial study protocol. BMJ open, 8(8), e022225
https://bmjopen.bmj.com/content/8/8/e022225.abstract
Husain, M. A., Jabbar, L., & Jawad, A. M. (2018). Rational use of Metoprolol: The
Relationship of Its Blood Concentration to Patient Compliance, Poor Quality
Medicines and Side Effects. University of Thi-Qar Journal Of Medicine, 16(2), 132-
141 https://jmed.utq.edu.iq/index.php/main/article/view/21
Levett-Jones et al. (2009). The 'five rights' of clinical reasoning: An educational model to
enhance nursing students' ability to identify and manage clinically 'at risk' patients.
Researchgate.
https://www.researchgate.net/publication/40041506_The_'five_rights'_of_clinical_rea
soning_An_educational_model_to_enhance_nursing_students'_ability_to_identify_an
d_manage_clinically_'at_risk'_patients
Middleton, S., Levi, C., Dale, S., Cheung, N. W., McInnes, E., Considine, J., ... & Craig, L.
(2016). Triage, treatment and transfer of patients with stroke in emergency
department trial (the T 3 Trial): a cluster randomised trial protocol. Implementation
Science, 11(1), 139
https://www.ahajournals.org/doi/full/10.1161/STROKEAHA.115.010613
Berge, E., & Sandercock, P. (2019). Specific treatment of acute ischemic stroke. Warlow's
Stroke: Practical Management, 587-656
https://onlinelibrary.wiley.com/doi/abs/10.1002/9781118492390.ch13
Coombes, J. A., Rowett, D., Whitty, J. A., & Cottrell, W. N. (2018). Use of a patient-centred
educational exchange (PCEE) to improve patient’s self-management of medicines
after a stroke: a randomised controlled trial study protocol. BMJ open, 8(8), e022225
https://bmjopen.bmj.com/content/8/8/e022225.abstract
Husain, M. A., Jabbar, L., & Jawad, A. M. (2018). Rational use of Metoprolol: The
Relationship of Its Blood Concentration to Patient Compliance, Poor Quality
Medicines and Side Effects. University of Thi-Qar Journal Of Medicine, 16(2), 132-
141 https://jmed.utq.edu.iq/index.php/main/article/view/21
Levett-Jones et al. (2009). The 'five rights' of clinical reasoning: An educational model to
enhance nursing students' ability to identify and manage clinically 'at risk' patients.
Researchgate.
https://www.researchgate.net/publication/40041506_The_'five_rights'_of_clinical_rea
soning_An_educational_model_to_enhance_nursing_students'_ability_to_identify_an
d_manage_clinically_'at_risk'_patients
Middleton, S., Levi, C., Dale, S., Cheung, N. W., McInnes, E., Considine, J., ... & Craig, L.
(2016). Triage, treatment and transfer of patients with stroke in emergency
department trial (the T 3 Trial): a cluster randomised trial protocol. Implementation
Science, 11(1), 139
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
https://implementationscience.biomedcentral.com/articles/10.1186/s13012-016-0503-
6
Purvis, T., Moss, K., Francis, L., Borschmann, K., Kilkenny, M. F., Denisenko, S., ... &
Cadilhac, D. A. (2017). Benefits of clinical facilitators on improving stroke care in
acute hospitals: a new programme for Australia. Internal medicine journal, 47(7),
775-784 https://onlinelibrary.wiley.com/doi/abs/10.1111/imj.13458
Sommer, C. J. (2017). Ischemic stroke: experimental models and reality. Acta
neuropathologica, 133(2), 245-261 https://link.springer.com/article/10.1007/s00401-
017-1667-0
Saver, J. L., Goyal, M., Van der Lugt, A. A. D., Menon, B. K., Majoie, C. B., Dippel, D.
W., ... & Cardona, P. (2016). Time to treatment with endovascular thrombectomy and
outcomes from ischemic stroke: a meta-analysis. Jama, 316(12), 1279-1289
https://jamanetwork.com/journals/jama/article-abstract/2556124
Threlkeld, Z. D., Kozak, B., McCoy, D., Cole, S., Martin, C., & Singh, V. (2017).
Collaborative interventions reduce time-to-thrombolysis for acute ischemic stroke in a
public safety net hospital. Journal of Stroke and Cerebrovascular Diseases, 26(7),
1500-1505 https://www.sciencedirect.com/science/article/pii/S1052305717301076
Thampy, H., Willert, E., & Ramani, S. (2019). Assessing Clinical Reasoning: Targeting the
Higher Levels of the Pyramid. Journal of general internal medicine, 1-6
https://link.springer.com/article/10.1007/s11606-019-04953-4
Turpin, M., & Higgs, J. (2017). Clinical reasoning and evidence-based practice. Evidence-
based practice: Across the health professions, 364-383
https://books.google.co.in/books?
6
Purvis, T., Moss, K., Francis, L., Borschmann, K., Kilkenny, M. F., Denisenko, S., ... &
Cadilhac, D. A. (2017). Benefits of clinical facilitators on improving stroke care in
acute hospitals: a new programme for Australia. Internal medicine journal, 47(7),
775-784 https://onlinelibrary.wiley.com/doi/abs/10.1111/imj.13458
Sommer, C. J. (2017). Ischemic stroke: experimental models and reality. Acta
neuropathologica, 133(2), 245-261 https://link.springer.com/article/10.1007/s00401-
017-1667-0
Saver, J. L., Goyal, M., Van der Lugt, A. A. D., Menon, B. K., Majoie, C. B., Dippel, D.
W., ... & Cardona, P. (2016). Time to treatment with endovascular thrombectomy and
outcomes from ischemic stroke: a meta-analysis. Jama, 316(12), 1279-1289
https://jamanetwork.com/journals/jama/article-abstract/2556124
Threlkeld, Z. D., Kozak, B., McCoy, D., Cole, S., Martin, C., & Singh, V. (2017).
Collaborative interventions reduce time-to-thrombolysis for acute ischemic stroke in a
public safety net hospital. Journal of Stroke and Cerebrovascular Diseases, 26(7),
1500-1505 https://www.sciencedirect.com/science/article/pii/S1052305717301076
Thampy, H., Willert, E., & Ramani, S. (2019). Assessing Clinical Reasoning: Targeting the
Higher Levels of the Pyramid. Journal of general internal medicine, 1-6
https://link.springer.com/article/10.1007/s11606-019-04953-4
Turpin, M., & Higgs, J. (2017). Clinical reasoning and evidence-based practice. Evidence-
based practice: Across the health professions, 364-383
https://books.google.co.in/books?
hl=en&lr=&id=yGclDwAAQBAJ&oi=fnd&pg=PA364&dq=considering+present+sit
uation+clinical+reasoning+&ots=X_0Ea4OKCo&sig=vGlVX5K4JZOxjZgz107OVlN
mr8I&redir_esc=y#v=onepage&q=considering%20present%20situation%20clinical
%20reasoning&f=false
uation+clinical+reasoning+&ots=X_0Ea4OKCo&sig=vGlVX5K4JZOxjZgz107OVlN
mr8I&redir_esc=y#v=onepage&q=considering%20present%20situation%20clinical
%20reasoning&f=false
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


