ATHC 1 Assessment: Clinical Reasoning Cycle for Bowel Resection
VerifiedAdded on 2023/06/11
|10
|1593
|188
Case Study
AI Summary
This case study presents a clinical reasoning cycle applied to a 72-year-old patient, Mr. Cyril Smith, admitted for bowel resection surgery following a bowel cancer diagnosis. The study includes observations of the patient's condition, collection of cues related to his COPD, osteoarthritis, type II diabetes, and recent weight loss. It interprets data related to dizziness, tachycardia, and blood sugar levels, identifying issues such as potential hypoglycemia and dehydration. The analysis extends to discussing factors compromising safe medication practices, emphasizing communication and prescription errors. Furthermore, it highlights the importance of therapeutic communication in nursing practice and reflects on lessons learned regarding patient communication and understanding. The case study concludes by outlining actions to be implemented in clinical practice, focusing on clear and patient-centered communication. Desklib offers a platform to explore similar solved assignments and past papers for students.

TITLE
Name of Student
Name of Course
Professor
Institution
State
Date
Name of Student
Name of Course
Professor
Institution
State
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
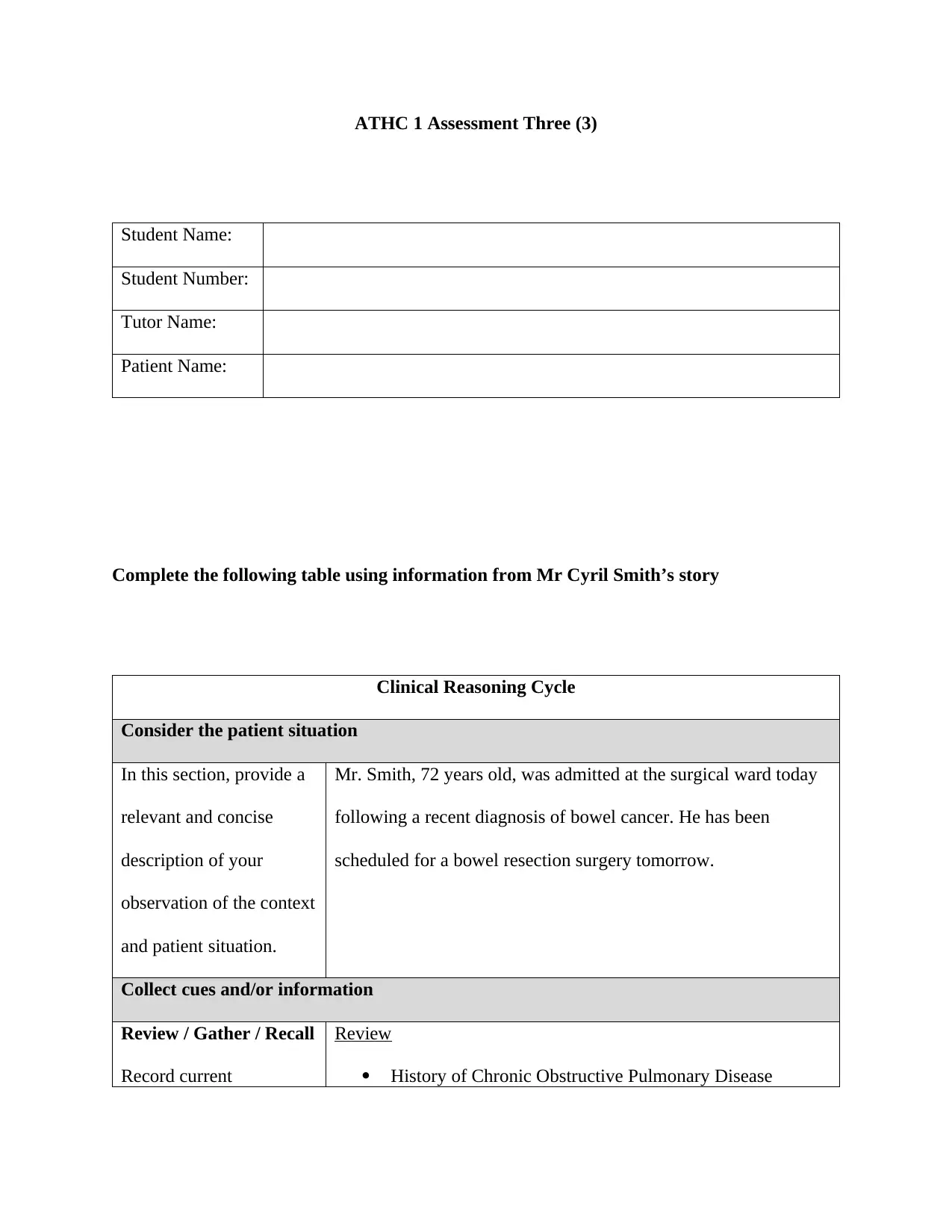
ATHC 1 Assessment Three (3)
Student Name:
Student Number:
Tutor Name:
Patient Name:
Complete the following table using information from Mr Cyril Smith’s story
Clinical Reasoning Cycle
Consider the patient situation
In this section, provide a
relevant and concise
description of your
observation of the context
and patient situation.
Mr. Smith, 72 years old, was admitted at the surgical ward today
following a recent diagnosis of bowel cancer. He has been
scheduled for a bowel resection surgery tomorrow.
Collect cues and/or information
Review / Gather / Recall
Record current
Review
History of Chronic Obstructive Pulmonary Disease
Student Name:
Student Number:
Tutor Name:
Patient Name:
Complete the following table using information from Mr Cyril Smith’s story
Clinical Reasoning Cycle
Consider the patient situation
In this section, provide a
relevant and concise
description of your
observation of the context
and patient situation.
Mr. Smith, 72 years old, was admitted at the surgical ward today
following a recent diagnosis of bowel cancer. He has been
scheduled for a bowel resection surgery tomorrow.
Collect cues and/or information
Review / Gather / Recall
Record current
Review
History of Chronic Obstructive Pulmonary Disease
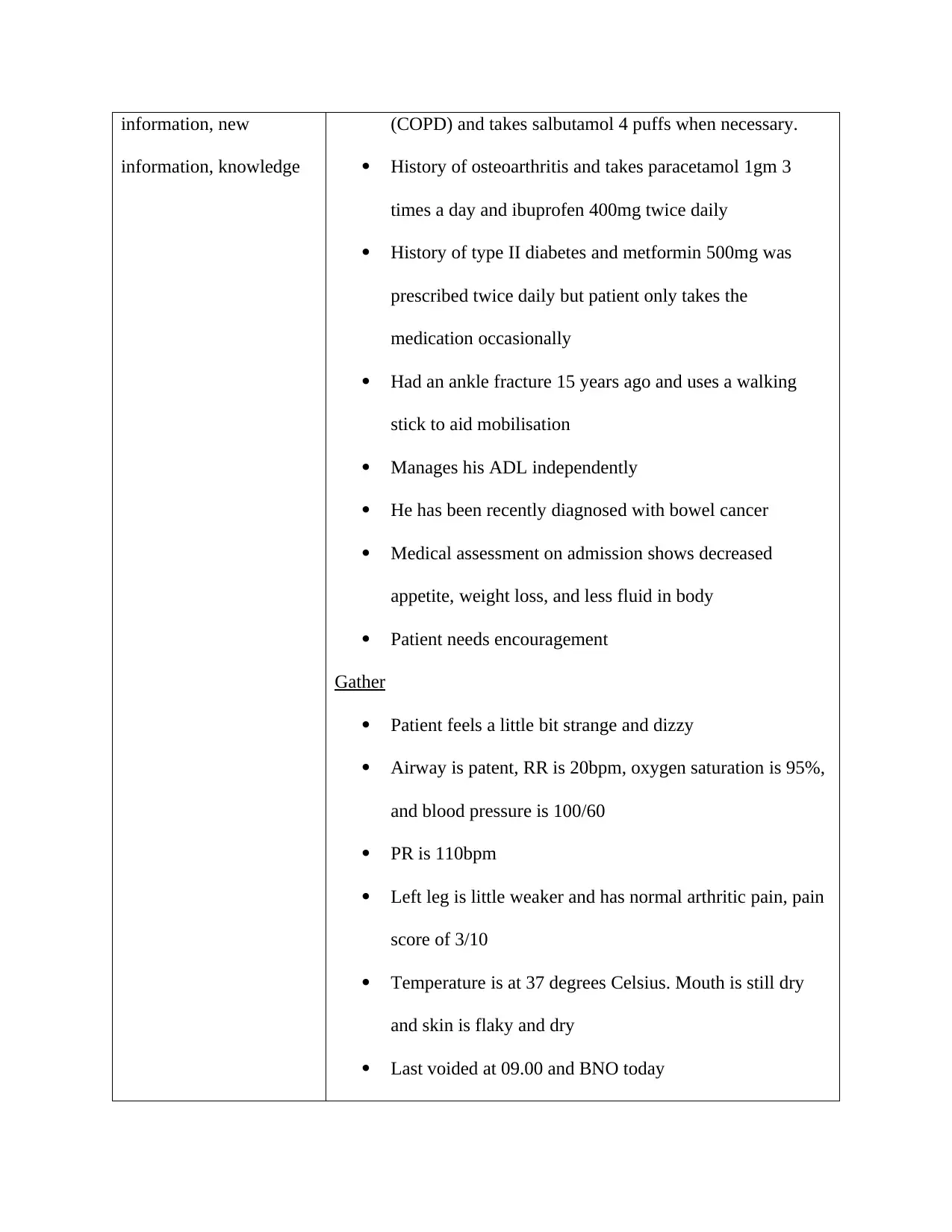
information, new
information, knowledge
(COPD) and takes salbutamol 4 puffs when necessary.
History of osteoarthritis and takes paracetamol 1gm 3
times a day and ibuprofen 400mg twice daily
History of type II diabetes and metformin 500mg was
prescribed twice daily but patient only takes the
medication occasionally
Had an ankle fracture 15 years ago and uses a walking
stick to aid mobilisation
Manages his ADL independently
He has been recently diagnosed with bowel cancer
Medical assessment on admission shows decreased
appetite, weight loss, and less fluid in body
Patient needs encouragement
Gather
Patient feels a little bit strange and dizzy
Airway is patent, RR is 20bpm, oxygen saturation is 95%,
and blood pressure is 100/60
PR is 110bpm
Left leg is little weaker and has normal arthritic pain, pain
score of 3/10
Temperature is at 37 degrees Celsius. Mouth is still dry
and skin is flaky and dry
Last voided at 09.00 and BNO today
information, knowledge
(COPD) and takes salbutamol 4 puffs when necessary.
History of osteoarthritis and takes paracetamol 1gm 3
times a day and ibuprofen 400mg twice daily
History of type II diabetes and metformin 500mg was
prescribed twice daily but patient only takes the
medication occasionally
Had an ankle fracture 15 years ago and uses a walking
stick to aid mobilisation
Manages his ADL independently
He has been recently diagnosed with bowel cancer
Medical assessment on admission shows decreased
appetite, weight loss, and less fluid in body
Patient needs encouragement
Gather
Patient feels a little bit strange and dizzy
Airway is patent, RR is 20bpm, oxygen saturation is 95%,
and blood pressure is 100/60
PR is 110bpm
Left leg is little weaker and has normal arthritic pain, pain
score of 3/10
Temperature is at 37 degrees Celsius. Mouth is still dry
and skin is flaky and dry
Last voided at 09.00 and BNO today
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
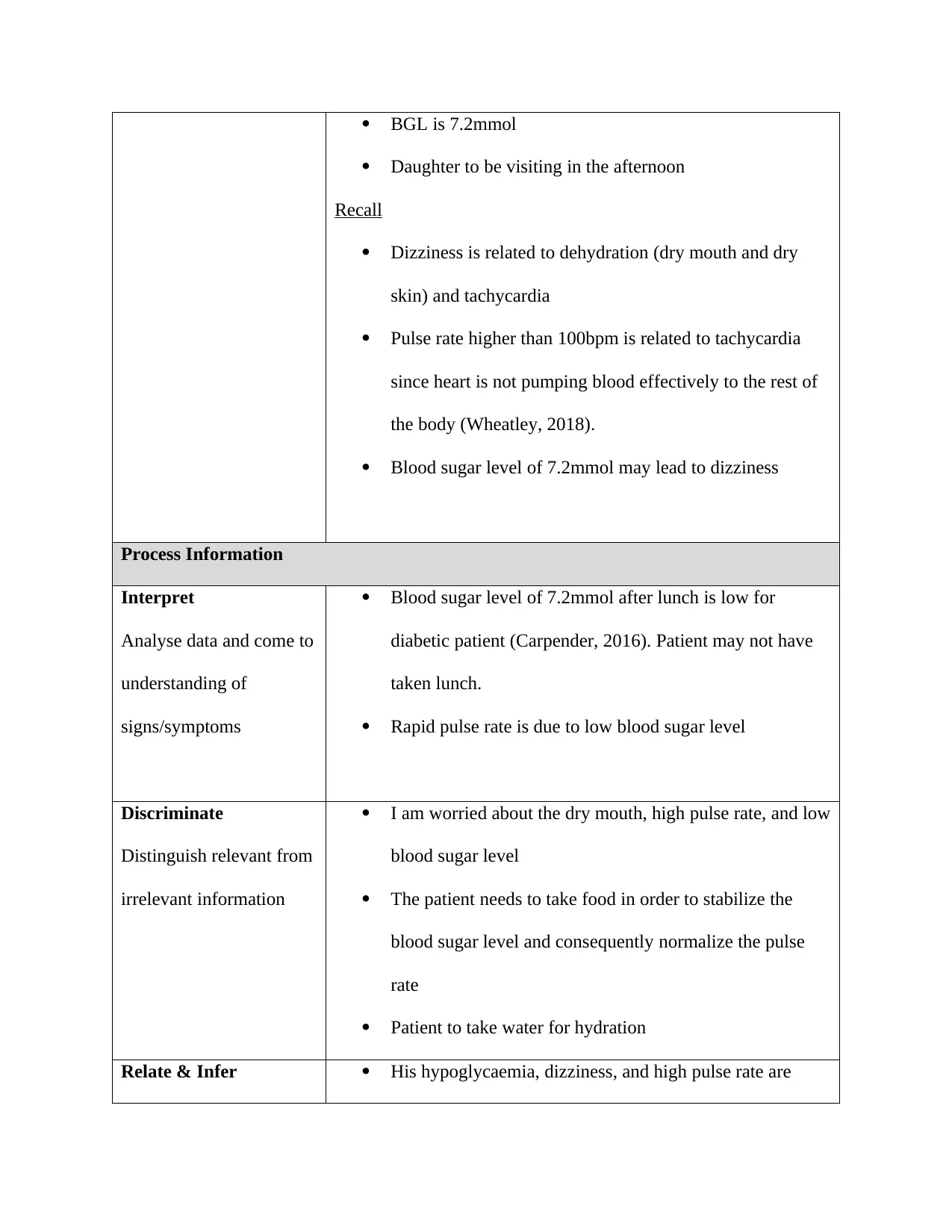
BGL is 7.2mmol
Daughter to be visiting in the afternoon
Recall
Dizziness is related to dehydration (dry mouth and dry
skin) and tachycardia
Pulse rate higher than 100bpm is related to tachycardia
since heart is not pumping blood effectively to the rest of
the body (Wheatley, 2018).
Blood sugar level of 7.2mmol may lead to dizziness
Process Information
Interpret
Analyse data and come to
understanding of
signs/symptoms
Blood sugar level of 7.2mmol after lunch is low for
diabetic patient (Carpender, 2016). Patient may not have
taken lunch.
Rapid pulse rate is due to low blood sugar level
Discriminate
Distinguish relevant from
irrelevant information
I am worried about the dry mouth, high pulse rate, and low
blood sugar level
The patient needs to take food in order to stabilize the
blood sugar level and consequently normalize the pulse
rate
Patient to take water for hydration
Relate & Infer His hypoglycaemia, dizziness, and high pulse rate are
Daughter to be visiting in the afternoon
Recall
Dizziness is related to dehydration (dry mouth and dry
skin) and tachycardia
Pulse rate higher than 100bpm is related to tachycardia
since heart is not pumping blood effectively to the rest of
the body (Wheatley, 2018).
Blood sugar level of 7.2mmol may lead to dizziness
Process Information
Interpret
Analyse data and come to
understanding of
signs/symptoms
Blood sugar level of 7.2mmol after lunch is low for
diabetic patient (Carpender, 2016). Patient may not have
taken lunch.
Rapid pulse rate is due to low blood sugar level
Discriminate
Distinguish relevant from
irrelevant information
I am worried about the dry mouth, high pulse rate, and low
blood sugar level
The patient needs to take food in order to stabilize the
blood sugar level and consequently normalize the pulse
rate
Patient to take water for hydration
Relate & Infer His hypoglycaemia, dizziness, and high pulse rate are
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
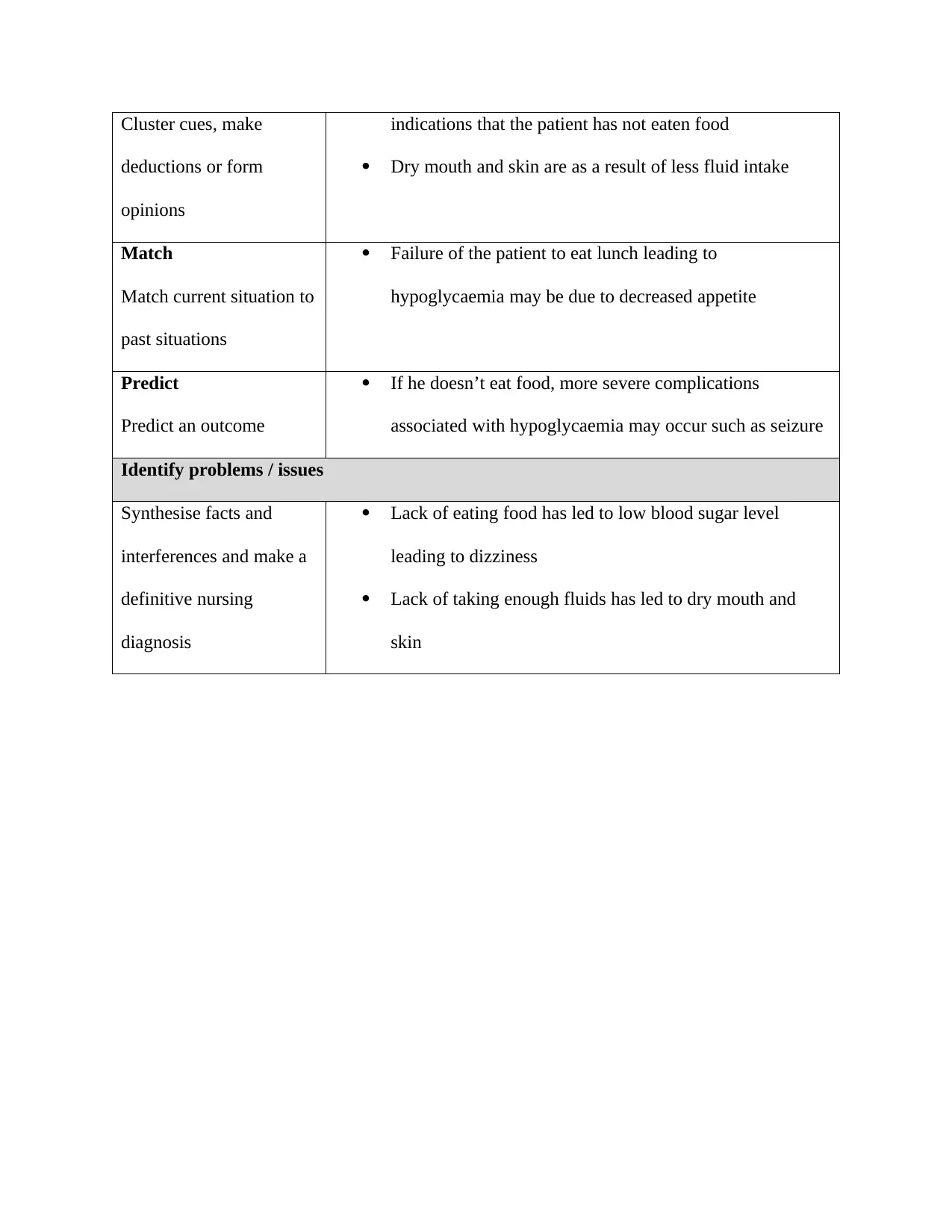
Cluster cues, make
deductions or form
opinions
indications that the patient has not eaten food
Dry mouth and skin are as a result of less fluid intake
Match
Match current situation to
past situations
Failure of the patient to eat lunch leading to
hypoglycaemia may be due to decreased appetite
Predict
Predict an outcome
If he doesn’t eat food, more severe complications
associated with hypoglycaemia may occur such as seizure
Identify problems / issues
Synthesise facts and
interferences and make a
definitive nursing
diagnosis
Lack of eating food has led to low blood sugar level
leading to dizziness
Lack of taking enough fluids has led to dry mouth and
skin
deductions or form
opinions
indications that the patient has not eaten food
Dry mouth and skin are as a result of less fluid intake
Match
Match current situation to
past situations
Failure of the patient to eat lunch leading to
hypoglycaemia may be due to decreased appetite
Predict
Predict an outcome
If he doesn’t eat food, more severe complications
associated with hypoglycaemia may occur such as seizure
Identify problems / issues
Synthesise facts and
interferences and make a
definitive nursing
diagnosis
Lack of eating food has led to low blood sugar level
leading to dizziness
Lack of taking enough fluids has led to dry mouth and
skin
Critical thinking questions
Identify and discuss two factors that could potentially compromise safe medication practices
(provide references) 100 words:
1 Faulty communication
General communication between clinicians and nurses as well, about the details of
administering medication is very important in the procedure of safe medication
administration. When there is a communication breakdown such as misunderstanding of
verbal order by telephone concerning a certain medication or not following the steps in
the procedure of the medication, medication errors are prone to occur (Shitu, Hassan,
Thwe Aung, Tuan Kamaruzaman & Musa, 2018).
2 Prescription error
These are errors which occur due to faults made by physicians in the directions in the
prescription charts. These errors may include information that is incorrect, inappropriate
doses, and prescription that is not complete. These errors mostly occur from the mistakes
and faults committed by the physicians (Shrestha and Ramanath, 2015).
Outline the importance of effective therapeutic communication and how it relates to safe nursing
practice (provide references) (200 words)
Effective therapeutic communication gives the patient self-confidence to be able to play a role
in his or her wellness. Therapeutic communication such as actively listening to the patient
Identify and discuss two factors that could potentially compromise safe medication practices
(provide references) 100 words:
1 Faulty communication
General communication between clinicians and nurses as well, about the details of
administering medication is very important in the procedure of safe medication
administration. When there is a communication breakdown such as misunderstanding of
verbal order by telephone concerning a certain medication or not following the steps in
the procedure of the medication, medication errors are prone to occur (Shitu, Hassan,
Thwe Aung, Tuan Kamaruzaman & Musa, 2018).
2 Prescription error
These are errors which occur due to faults made by physicians in the directions in the
prescription charts. These errors may include information that is incorrect, inappropriate
doses, and prescription that is not complete. These errors mostly occur from the mistakes
and faults committed by the physicians (Shrestha and Ramanath, 2015).
Outline the importance of effective therapeutic communication and how it relates to safe nursing
practice (provide references) (200 words)
Effective therapeutic communication gives the patient self-confidence to be able to play a role
in his or her wellness. Therapeutic communication such as actively listening to the patient
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
enables the patient to be more independent and self-confident. Instead making assumptions
concerning the patient, therapeutic communication will enable the healthcare provider to
initiate therapeutic expression. The patient will then be able to share comfortably any difficult
information he or she may be experiencing. The shared information will help the healthcare
provider to do more investigations concerning the feelings and the options of the patient.
Therefore, the patient will gain more independence and confidence in making his own
decisions concerning his care (Maame Kissiwaa Amoah et al., 2018).
Additionally, effective therapeutic communication leads to the development of trust. Trust
creates a non-judgemental environment where communication is constructive and encourages
the patient to be confident. When the healthcare provider is non-judgemental, both the verbal
and non-verbal cues are taken care of. Individuals in general are usually keen to notice any
non-verbal cues that may infer something different from what has been communicated.
Similarly, when trust is enhanced through effective therapeutic communication, the patient is
able to be more independent and is able to make sound decisions concerning his wellbeing
(Rørtveit et al., 2015).
What have you learned from this assessment? What actions will you take into clinical practice as
a result of what you have learned? (provide references) (200 words)
I have learnt that communication is very important when dealing with patients. Effective
communication enables the patient to be able to express themselves well regarding any issue
concerning the patient, therapeutic communication will enable the healthcare provider to
initiate therapeutic expression. The patient will then be able to share comfortably any difficult
information he or she may be experiencing. The shared information will help the healthcare
provider to do more investigations concerning the feelings and the options of the patient.
Therefore, the patient will gain more independence and confidence in making his own
decisions concerning his care (Maame Kissiwaa Amoah et al., 2018).
Additionally, effective therapeutic communication leads to the development of trust. Trust
creates a non-judgemental environment where communication is constructive and encourages
the patient to be confident. When the healthcare provider is non-judgemental, both the verbal
and non-verbal cues are taken care of. Individuals in general are usually keen to notice any
non-verbal cues that may infer something different from what has been communicated.
Similarly, when trust is enhanced through effective therapeutic communication, the patient is
able to be more independent and is able to make sound decisions concerning his wellbeing
(Rørtveit et al., 2015).
What have you learned from this assessment? What actions will you take into clinical practice as
a result of what you have learned? (provide references) (200 words)
I have learnt that communication is very important when dealing with patients. Effective
communication enables the patient to be able to express themselves well regarding any issue
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
or question concerning their health. For example, from the assessment, the patient reported
that the nurse had asked him a lot of questions and that he did not understand the words that
the nurse used while communicating to him. Additionally, the patient reported that he did not
know what the nurse was talking about and that he was not sure about the answers he gave.
From this report I learnt that when inquiring about the health status of a patient, it is important
to use an easy language or language that is best understood by the patient. Some of the patients
do not understand medical terms and may end up giving wrong information about their health
or may give information they are not sure about as in the case of Mr. Smith (Sassen, 2018). I
will make sure that when getting information from a patient, I will make the patient understand
why I am asking the questions and the importance of giving correct information. It is also
necessary that I let the patient know that it is right to get a clarification in case they do not
understand the questions (Perry, Potter and Ostendorf, 2015).
References
that the nurse had asked him a lot of questions and that he did not understand the words that
the nurse used while communicating to him. Additionally, the patient reported that he did not
know what the nurse was talking about and that he was not sure about the answers he gave.
From this report I learnt that when inquiring about the health status of a patient, it is important
to use an easy language or language that is best understood by the patient. Some of the patients
do not understand medical terms and may end up giving wrong information about their health
or may give information they are not sure about as in the case of Mr. Smith (Sassen, 2018). I
will make sure that when getting information from a patient, I will make the patient understand
why I am asking the questions and the importance of giving correct information. It is also
necessary that I let the patient know that it is right to get a clarification in case they do not
understand the questions (Perry, Potter and Ostendorf, 2015).
References
Carpender, D. (2016). Low-carb diabetes solution cookbook - prevent and heal type 2 diabetes
with. Fair Winds Press, p.14.
Maame Kissiwaa Amoah, V., Anokye, R., Boakye, D. and Gyamfi, N. (2018). Perceived barriers
to effective therapeutic communication among nurses and patients at Kumasi South
Hospital. Cogent Medicine, 5(1), p.2.
Perry, A., Potter, P. and Ostendorf, W. (2015). Nursing Interventions & Clinical Skills. Saint
Louis: Elsevier Health Sciences, p.19.
Rørtveit, K., Sætre Hansen, B., Leiknes, I., Joa, I., Testad, I. and Severinsson, E. (2015).
Patients’ Experiences of Trust in the Patient-Nurse Relationship—A Systematic Review of
Qualitative Studies. Open Journal of Nursing, 05(03), pp.195-209.
Sassen, B. (2018). Nursing: Health Education and Improving Patient Self-Management. Cham:
Springer International Publishing, p.159.
Shitu, Z., Hassan, I., Thwe Aung, M., Tuan Kamaruzaman, T. and Musa, R. (2018). Avoiding
medication errors through effective communication in healthcare environment. Malaysian
Journal of Movement, Health & Exercise, 7(1), pp.115-128.
Shrestha, S. and Ramanath, K. (2015). Study and Evaluation of Medication Errors in Medicine
and Orthopedic Wards of a Tertiary Care Hospital. British Journal of Pharmaceutical
Research, 7(3), pp.183-195.
Wheatley, D. (2018). Psychopharmacology in family practice. London: Heinemann Medical,
p.36.
with. Fair Winds Press, p.14.
Maame Kissiwaa Amoah, V., Anokye, R., Boakye, D. and Gyamfi, N. (2018). Perceived barriers
to effective therapeutic communication among nurses and patients at Kumasi South
Hospital. Cogent Medicine, 5(1), p.2.
Perry, A., Potter, P. and Ostendorf, W. (2015). Nursing Interventions & Clinical Skills. Saint
Louis: Elsevier Health Sciences, p.19.
Rørtveit, K., Sætre Hansen, B., Leiknes, I., Joa, I., Testad, I. and Severinsson, E. (2015).
Patients’ Experiences of Trust in the Patient-Nurse Relationship—A Systematic Review of
Qualitative Studies. Open Journal of Nursing, 05(03), pp.195-209.
Sassen, B. (2018). Nursing: Health Education and Improving Patient Self-Management. Cham:
Springer International Publishing, p.159.
Shitu, Z., Hassan, I., Thwe Aung, M., Tuan Kamaruzaman, T. and Musa, R. (2018). Avoiding
medication errors through effective communication in healthcare environment. Malaysian
Journal of Movement, Health & Exercise, 7(1), pp.115-128.
Shrestha, S. and Ramanath, K. (2015). Study and Evaluation of Medication Errors in Medicine
and Orthopedic Wards of a Tertiary Care Hospital. British Journal of Pharmaceutical
Research, 7(3), pp.183-195.
Wheatley, D. (2018). Psychopharmacology in family practice. London: Heinemann Medical,
p.36.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





