ATHC 1: Clinical Reasoning, Vital Signs, and Nursing Standards Review
VerifiedAdded on 2023/06/13
|6
|2304
|432
Report
AI Summary
This assignment presents a clinical reasoning assessment based on a patient scenario involving Sandra Smith, a 33-year-old female presenting with PV bleeding. The assessment utilizes the clinical reasoning cycle to analyze the patient's situation, collect relevant cues and information, and identify potential errors in vital sign measurement. It delves into the importance of accurate documentation in nursing practice, relating it to Standard 4 of the Registered Nurse Standards for Practice (2016). The student reflects on the learning experience, emphasizing the significance of accurate documentation, systematic assessment, and therapeutic communication in improving patient outcomes. The assignment also includes relevant references to support the analysis and conclusions.
ATHC 1 Assessment Two (2) template
Student Name: Devika gurung
Student Number: 12858585
Tutor Name:
Complete the following table using information from the assessment resources and Video A.
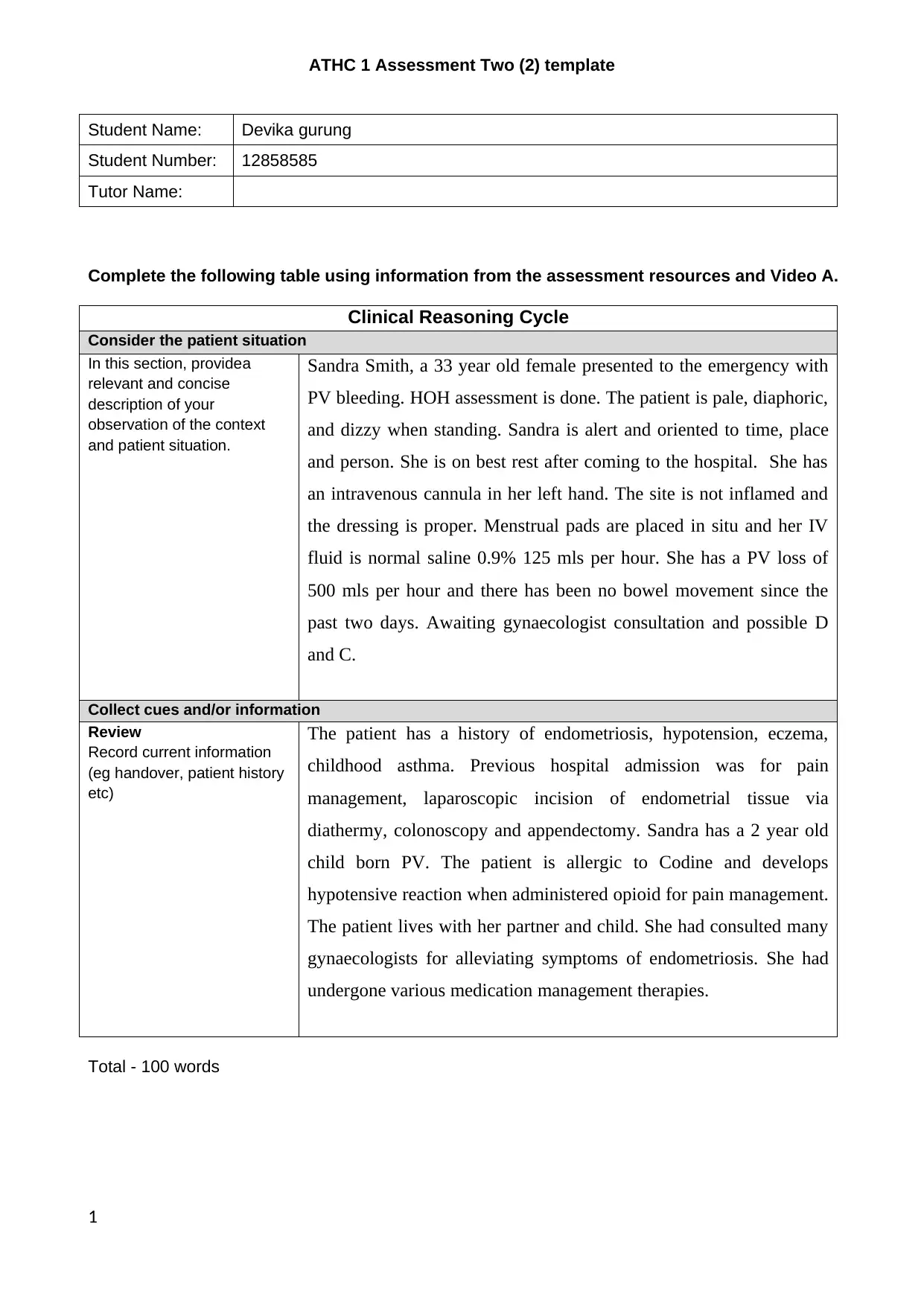
Clinical Reasoning Cycle
Consider the patient situation
In this section, providea
relevant and concise
description of your
observation of the context
and patient situation.
Sandra Smith, a 33 year old female presented to the emergency with
PV bleeding. HOH assessment is done. The patient is pale, diaphoric,
and dizzy when standing. Sandra is alert and oriented to time, place
and person. She is on best rest after coming to the hospital. She has
an intravenous cannula in her left hand. The site is not inflamed and
the dressing is proper. Menstrual pads are placed in situ and her IV
fluid is normal saline 0.9% 125 mls per hour. She has a PV loss of
500 mls per hour and there has been no bowel movement since the
past two days. Awaiting gynaecologist consultation and possible D
and C.
Collect cues and/or information
Review
Record current information
(eg handover, patient history
etc)
The patient has a history of endometriosis, hypotension, eczema,
childhood asthma. Previous hospital admission was for pain
management, laparoscopic incision of endometrial tissue via
diathermy, colonoscopy and appendectomy. Sandra has a 2 year old
child born PV. The patient is allergic to Codine and develops
hypotensive reaction when administered opioid for pain management.
The patient lives with her partner and child. She had consulted many
gynaecologists for alleviating symptoms of endometriosis. She had
undergone various medication management therapies.
Total - 100 words
1
Student Name: Devika gurung
Student Number: 12858585
Tutor Name:
Complete the following table using information from the assessment resources and Video A.
Clinical Reasoning Cycle
Consider the patient situation
In this section, providea
relevant and concise
description of your
observation of the context
and patient situation.
Sandra Smith, a 33 year old female presented to the emergency with
PV bleeding. HOH assessment is done. The patient is pale, diaphoric,
and dizzy when standing. Sandra is alert and oriented to time, place
and person. She is on best rest after coming to the hospital. She has
an intravenous cannula in her left hand. The site is not inflamed and
the dressing is proper. Menstrual pads are placed in situ and her IV
fluid is normal saline 0.9% 125 mls per hour. She has a PV loss of
500 mls per hour and there has been no bowel movement since the
past two days. Awaiting gynaecologist consultation and possible D
and C.
Collect cues and/or information
Review
Record current information
(eg handover, patient history
etc)
The patient has a history of endometriosis, hypotension, eczema,
childhood asthma. Previous hospital admission was for pain
management, laparoscopic incision of endometrial tissue via
diathermy, colonoscopy and appendectomy. Sandra has a 2 year old
child born PV. The patient is allergic to Codine and develops
hypotensive reaction when administered opioid for pain management.
The patient lives with her partner and child. She had consulted many
gynaecologists for alleviating symptoms of endometriosis. She had
undergone various medication management therapies.
Total - 100 words
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Complete the following table using information from Video A. Support your answers with references.
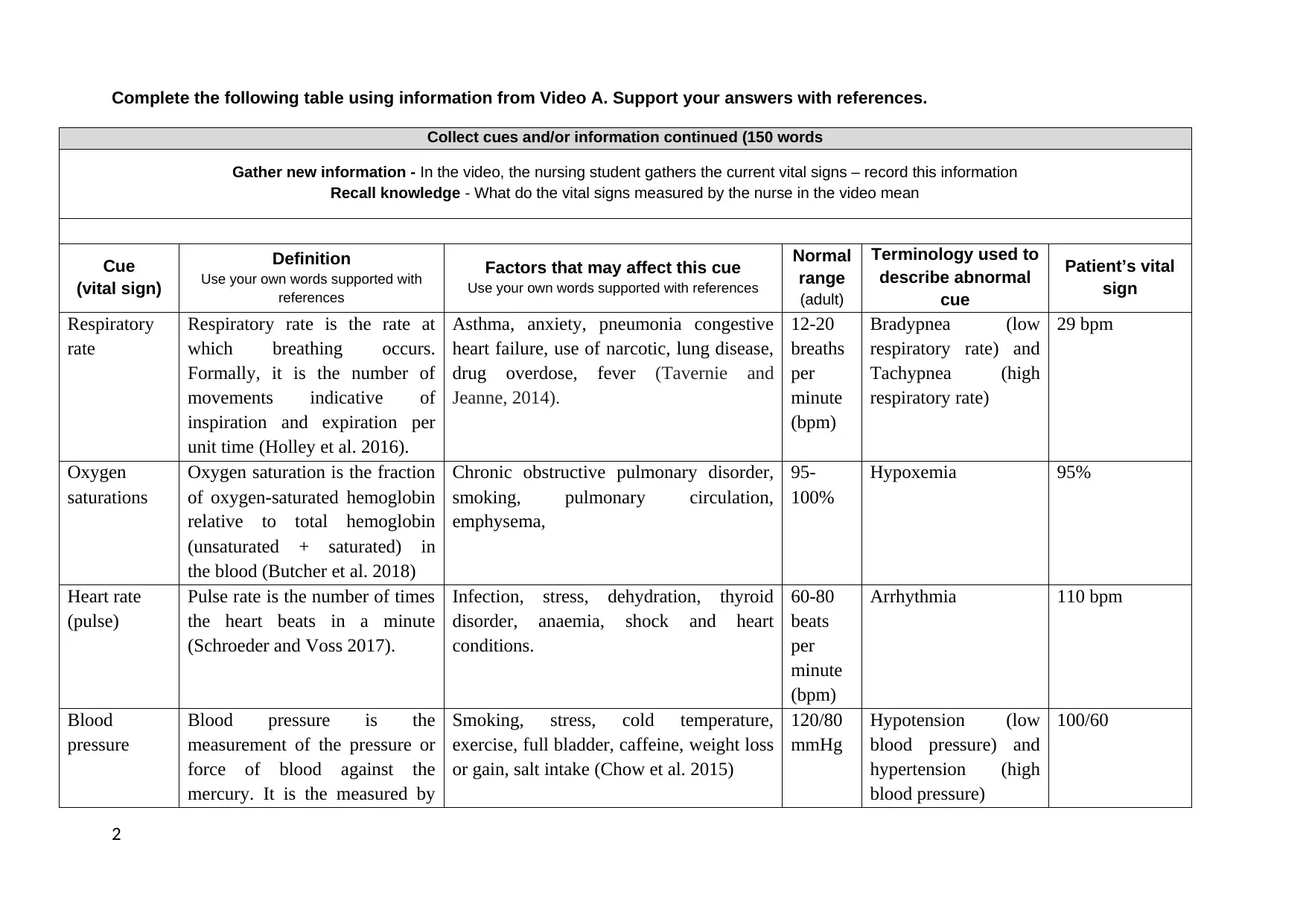
Collect cues and/or information continued (150 words
Gather new information - In the video, the nursing student gathers the current vital signs – record this information
Recall knowledge - What do the vital signs measured by the nurse in the video mean
Cue
(vital sign)
Definition
Use your own words supported with
references
Factors that may affect this cue
Use your own words supported with references
Normal
range
(adult)
Terminology used to
describe abnormal
cue
Patient’s vital
sign
Respiratory
rate
Respiratory rate is the rate at
which breathing occurs.
Formally, it is the number of
movements indicative of
inspiration and expiration per
unit time (Holley et al. 2016).
Asthma, anxiety, pneumonia congestive
heart failure, use of narcotic, lung disease,
drug overdose, fever (Tavernie and
Jeanne, 2014).
12-20
breaths
per
minute
(bpm)
Bradypnea (low
respiratory rate) and
Tachypnea (high
respiratory rate)
29 bpm
Oxygen
saturations
Oxygen saturation is the fraction
of oxygen-saturated hemoglobin
relative to total hemoglobin
(unsaturated + saturated) in
the blood (Butcher et al. 2018)
Chronic obstructive pulmonary disorder,
smoking, pulmonary circulation,
emphysema,
95-
100%
Hypoxemia 95%
Heart rate
(pulse)
Pulse rate is the number of times
the heart beats in a minute
(Schroeder and Voss 2017).
Infection, stress, dehydration, thyroid
disorder, anaemia, shock and heart
conditions.
60-80
beats
per
minute
(bpm)
Arrhythmia 110 bpm
Blood
pressure
Blood pressure is the
measurement of the pressure or
force of blood against the
mercury. It is the measured by
Smoking, stress, cold temperature,
exercise, full bladder, caffeine, weight loss
or gain, salt intake (Chow et al. 2015)
120/80
mmHg
Hypotension (low
blood pressure) and
hypertension (high
blood pressure)
100/60
2
Collect cues and/or information continued (150 words
Gather new information - In the video, the nursing student gathers the current vital signs – record this information
Recall knowledge - What do the vital signs measured by the nurse in the video mean
Cue
(vital sign)
Definition
Use your own words supported with
references
Factors that may affect this cue
Use your own words supported with references
Normal
range
(adult)
Terminology used to
describe abnormal
cue
Patient’s vital
sign
Respiratory
rate
Respiratory rate is the rate at
which breathing occurs.
Formally, it is the number of
movements indicative of
inspiration and expiration per
unit time (Holley et al. 2016).
Asthma, anxiety, pneumonia congestive
heart failure, use of narcotic, lung disease,
drug overdose, fever (Tavernie and
Jeanne, 2014).
12-20
breaths
per
minute
(bpm)
Bradypnea (low
respiratory rate) and
Tachypnea (high
respiratory rate)
29 bpm
Oxygen
saturations
Oxygen saturation is the fraction
of oxygen-saturated hemoglobin
relative to total hemoglobin
(unsaturated + saturated) in
the blood (Butcher et al. 2018)
Chronic obstructive pulmonary disorder,
smoking, pulmonary circulation,
emphysema,
95-
100%
Hypoxemia 95%
Heart rate
(pulse)
Pulse rate is the number of times
the heart beats in a minute
(Schroeder and Voss 2017).
Infection, stress, dehydration, thyroid
disorder, anaemia, shock and heart
conditions.
60-80
beats
per
minute
(bpm)
Arrhythmia 110 bpm
Blood
pressure
Blood pressure is the
measurement of the pressure or
force of blood against the
mercury. It is the measured by
Smoking, stress, cold temperature,
exercise, full bladder, caffeine, weight loss
or gain, salt intake (Chow et al. 2015)
120/80
mmHg
Hypotension (low
blood pressure) and
hypertension (high
blood pressure)
100/60
2
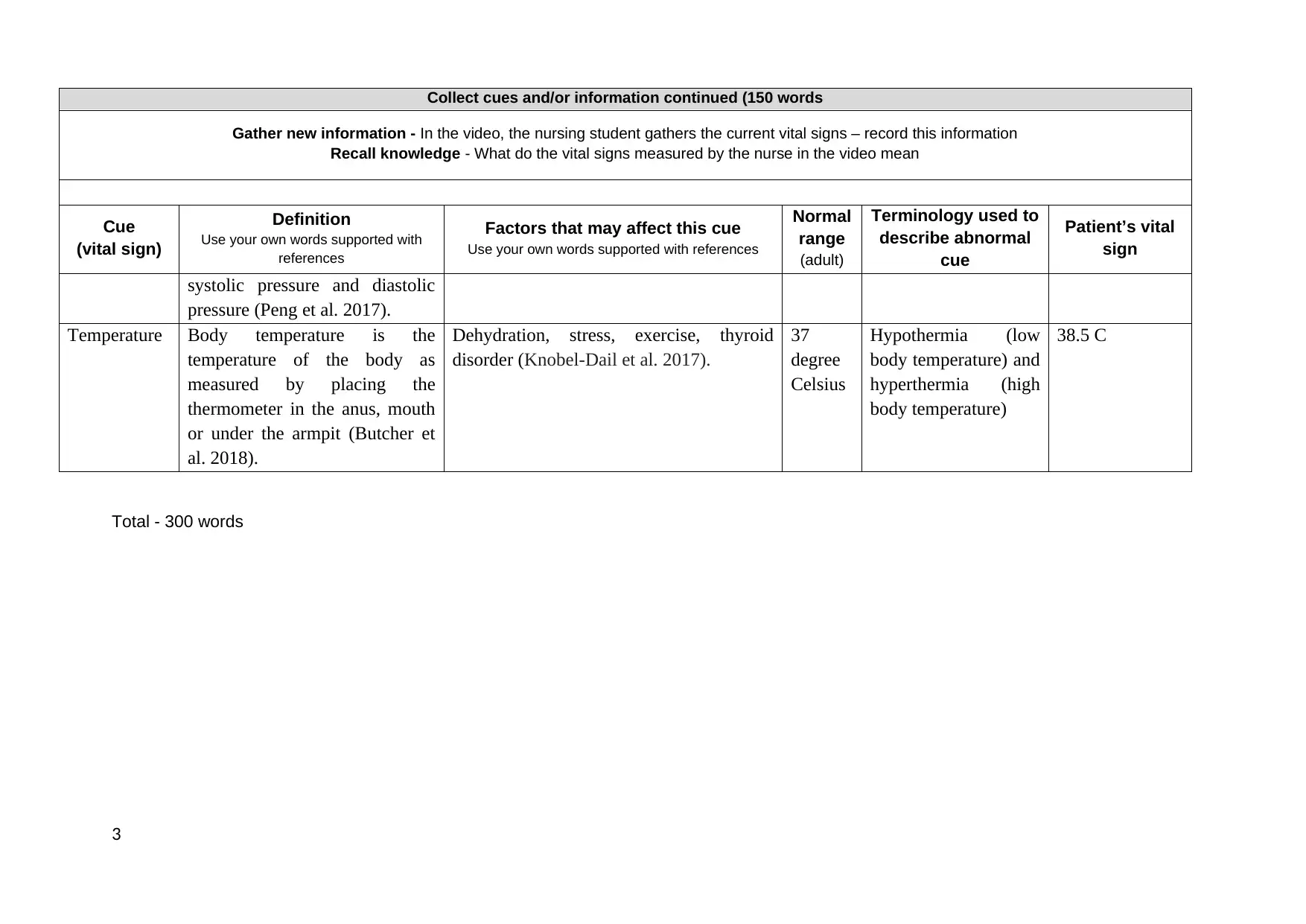
Collect cues and/or information continued (150 words
Gather new information - In the video, the nursing student gathers the current vital signs – record this information
Recall knowledge - What do the vital signs measured by the nurse in the video mean
Cue
(vital sign)
Definition
Use your own words supported with
references
Factors that may affect this cue
Use your own words supported with references
Normal
range
(adult)
Terminology used to
describe abnormal
cue
Patient’s vital
sign
systolic pressure and diastolic
pressure (Peng et al. 2017).
Temperature Body temperature is the
temperature of the body as
measured by placing the
thermometer in the anus, mouth
or under the armpit (Butcher et
al. 2018).
Dehydration, stress, exercise, thyroid
disorder (Knobel-Dail et al. 2017).
37
degree
Celsius
Hypothermia (low
body temperature) and
hyperthermia (high
body temperature)
38.5 C
Total - 300 words
3
Gather new information - In the video, the nursing student gathers the current vital signs – record this information
Recall knowledge - What do the vital signs measured by the nurse in the video mean
Cue
(vital sign)
Definition
Use your own words supported with
references
Factors that may affect this cue
Use your own words supported with references
Normal
range
(adult)
Terminology used to
describe abnormal
cue
Patient’s vital
sign
systolic pressure and diastolic
pressure (Peng et al. 2017).
Temperature Body temperature is the
temperature of the body as
measured by placing the
thermometer in the anus, mouth
or under the armpit (Butcher et
al. 2018).
Dehydration, stress, exercise, thyroid
disorder (Knobel-Dail et al. 2017).
37
degree
Celsius
Hypothermia (low
body temperature) and
hyperthermia (high
body temperature)
38.5 C
Total - 300 words
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
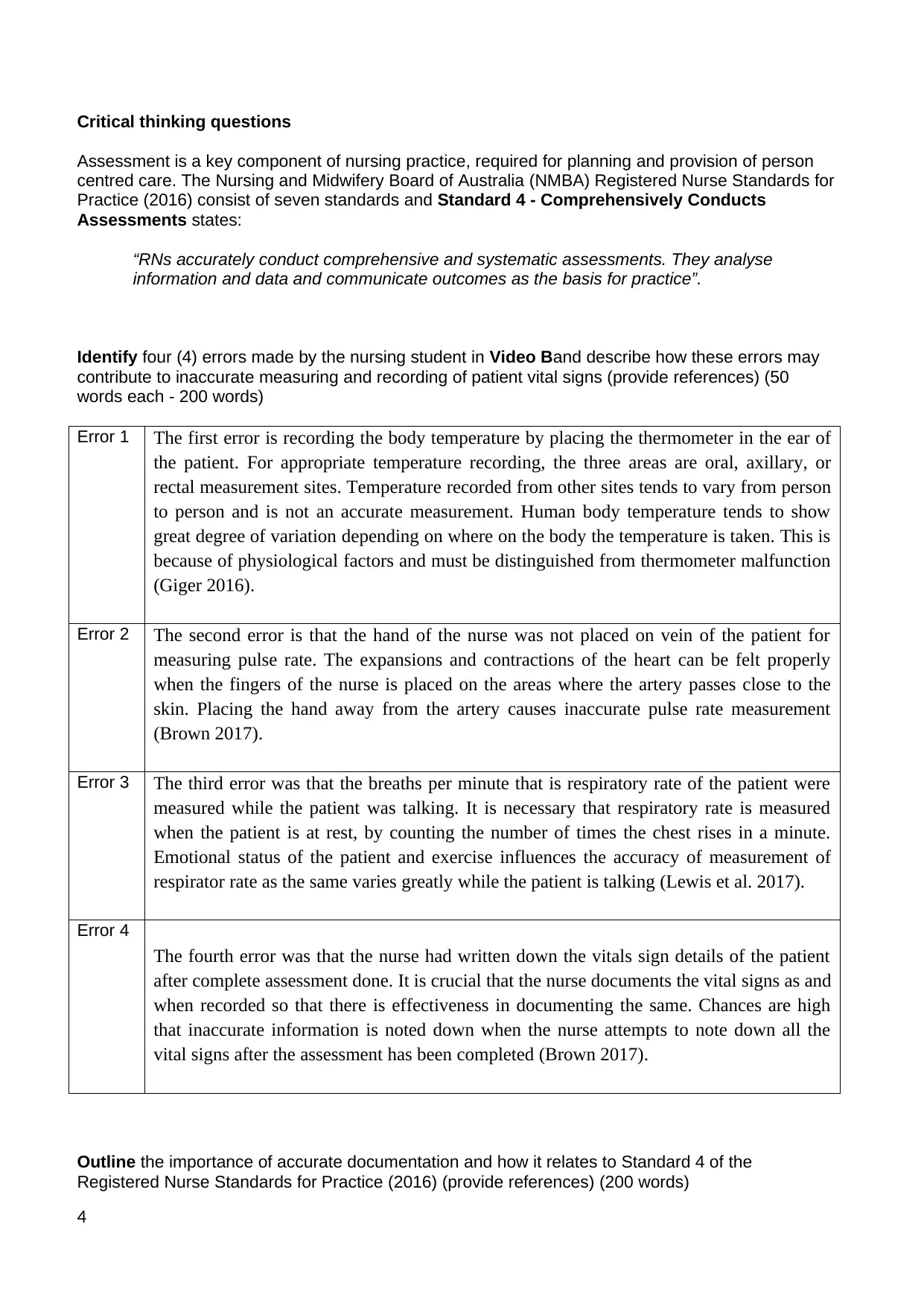
Critical thinking questions
Assessment is a key component of nursing practice, required for planning and provision of person
centred care. The Nursing and Midwifery Board of Australia (NMBA) Registered Nurse Standards for
Practice (2016) consist of seven standards and Standard 4 - Comprehensively Conducts
Assessments states:
“RNs accurately conduct comprehensive and systematic assessments. They analyse
information and data and communicate outcomes as the basis for practice”.
Identify four (4) errors made by the nursing student in Video Band describe how these errors may
contribute to inaccurate measuring and recording of patient vital signs (provide references) (50
words each - 200 words)
Error 1 The first error is recording the body temperature by placing the thermometer in the ear of
the patient. For appropriate temperature recording, the three areas are oral, axillary, or
rectal measurement sites. Temperature recorded from other sites tends to vary from person
to person and is not an accurate measurement. Human body temperature tends to show
great degree of variation depending on where on the body the temperature is taken. This is
because of physiological factors and must be distinguished from thermometer malfunction
(Giger 2016).
Error 2 The second error is that the hand of the nurse was not placed on vein of the patient for
measuring pulse rate. The expansions and contractions of the heart can be felt properly
when the fingers of the nurse is placed on the areas where the artery passes close to the
skin. Placing the hand away from the artery causes inaccurate pulse rate measurement
(Brown 2017).
Error 3 The third error was that the breaths per minute that is respiratory rate of the patient were
measured while the patient was talking. It is necessary that respiratory rate is measured
when the patient is at rest, by counting the number of times the chest rises in a minute.
Emotional status of the patient and exercise influences the accuracy of measurement of
respirator rate as the same varies greatly while the patient is talking (Lewis et al. 2017).
Error 4
The fourth error was that the nurse had written down the vitals sign details of the patient
after complete assessment done. It is crucial that the nurse documents the vital signs as and
when recorded so that there is effectiveness in documenting the same. Chances are high
that inaccurate information is noted down when the nurse attempts to note down all the
vital signs after the assessment has been completed (Brown 2017).
Outline the importance of accurate documentation and how it relates to Standard 4 of the
Registered Nurse Standards for Practice (2016) (provide references) (200 words)
4
Assessment is a key component of nursing practice, required for planning and provision of person
centred care. The Nursing and Midwifery Board of Australia (NMBA) Registered Nurse Standards for
Practice (2016) consist of seven standards and Standard 4 - Comprehensively Conducts
Assessments states:
“RNs accurately conduct comprehensive and systematic assessments. They analyse
information and data and communicate outcomes as the basis for practice”.
Identify four (4) errors made by the nursing student in Video Band describe how these errors may
contribute to inaccurate measuring and recording of patient vital signs (provide references) (50
words each - 200 words)
Error 1 The first error is recording the body temperature by placing the thermometer in the ear of
the patient. For appropriate temperature recording, the three areas are oral, axillary, or
rectal measurement sites. Temperature recorded from other sites tends to vary from person
to person and is not an accurate measurement. Human body temperature tends to show
great degree of variation depending on where on the body the temperature is taken. This is
because of physiological factors and must be distinguished from thermometer malfunction
(Giger 2016).
Error 2 The second error is that the hand of the nurse was not placed on vein of the patient for
measuring pulse rate. The expansions and contractions of the heart can be felt properly
when the fingers of the nurse is placed on the areas where the artery passes close to the
skin. Placing the hand away from the artery causes inaccurate pulse rate measurement
(Brown 2017).
Error 3 The third error was that the breaths per minute that is respiratory rate of the patient were
measured while the patient was talking. It is necessary that respiratory rate is measured
when the patient is at rest, by counting the number of times the chest rises in a minute.
Emotional status of the patient and exercise influences the accuracy of measurement of
respirator rate as the same varies greatly while the patient is talking (Lewis et al. 2017).
Error 4
The fourth error was that the nurse had written down the vitals sign details of the patient
after complete assessment done. It is crucial that the nurse documents the vital signs as and
when recorded so that there is effectiveness in documenting the same. Chances are high
that inaccurate information is noted down when the nurse attempts to note down all the
vital signs after the assessment has been completed (Brown 2017).
Outline the importance of accurate documentation and how it relates to Standard 4 of the
Registered Nurse Standards for Practice (2016) (provide references) (200 words)
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
As per the Standard 4 of the Registered Nurse Standards for Practice (2016), nurses are to
comprehensively carry out patient assessments. Going by this standard, the nurse is expected to use
a wide range of assessment techniques to systematically collect relevant and accurate information
and data to inform practice. Accurate documentation of patient information ensures that the
assessment process is useful as proper and comprehensive information is documented based on
which interventions can be applied. Documentation is a crucial component of the healthcare
delivery process. It enables continuity of care by serving as a communication tool for care
providers. Further accurate documentation eliminates chances of errors that could have been
otherwise made by professionals. Evaluation of the patient’s condition is only possible when there
is proper documentation of needs. Planning of services is also enabled by accurate documentation,
and a permanent record for the patient’s future care is needed. A database is created that promotes
evaluation of effectiveness of treatment (Lavin, Harper and Barr 2015). Care provided can be
defended at a later time when accurate documentation after patient assessment is present. Such
information is very useful for the process of carrying out clinical audit and reports on clinical
activity. In addition, there is a great contribution to research and performance data which can be
used to monitor improvement in service delivery and outcomes (Blais 2015).
What have you learned from this assessment? How will it inform your clinical practice? (200 words)
The assessment has been a learning experience and insights drawn would guide my future practice.
From the assessment, I have learnt that vital signs measurements are a key element of collecting
patient information. I believe that one of the most important nursing responsibilities is carrying out
accurate nursing documentation. Documentation is the reflection of the quality of care delivered to
the patient. Without such a clear record keeping process, nursing intervention cannot be proper. I
therefore would attempt to enable best patient outcomes for wellbeing of the patient.
I strive to use a standardised format for accurate documentation. This would help in ensuring
consistency and improving the quality of information collected. A systematic approach would be
taken for providing care based on the clinical presentations of the patient. Vitals signs enable a
nurse to understand the needs of patient care. These are therefore to be recorded properly. A
checklist would be used for ensuring that all aspects of assessment are covered. Communication
with the patient while assessment would b based on therapeutic relationships so that the maximal
information is extracted from the patient. Good nursing record keeping allows a nurse to identify
problems that have arisen and the action taken to rectify them.
5
comprehensively carry out patient assessments. Going by this standard, the nurse is expected to use
a wide range of assessment techniques to systematically collect relevant and accurate information
and data to inform practice. Accurate documentation of patient information ensures that the
assessment process is useful as proper and comprehensive information is documented based on
which interventions can be applied. Documentation is a crucial component of the healthcare
delivery process. It enables continuity of care by serving as a communication tool for care
providers. Further accurate documentation eliminates chances of errors that could have been
otherwise made by professionals. Evaluation of the patient’s condition is only possible when there
is proper documentation of needs. Planning of services is also enabled by accurate documentation,
and a permanent record for the patient’s future care is needed. A database is created that promotes
evaluation of effectiveness of treatment (Lavin, Harper and Barr 2015). Care provided can be
defended at a later time when accurate documentation after patient assessment is present. Such
information is very useful for the process of carrying out clinical audit and reports on clinical
activity. In addition, there is a great contribution to research and performance data which can be
used to monitor improvement in service delivery and outcomes (Blais 2015).
What have you learned from this assessment? How will it inform your clinical practice? (200 words)
The assessment has been a learning experience and insights drawn would guide my future practice.
From the assessment, I have learnt that vital signs measurements are a key element of collecting
patient information. I believe that one of the most important nursing responsibilities is carrying out
accurate nursing documentation. Documentation is the reflection of the quality of care delivered to
the patient. Without such a clear record keeping process, nursing intervention cannot be proper. I
therefore would attempt to enable best patient outcomes for wellbeing of the patient.
I strive to use a standardised format for accurate documentation. This would help in ensuring
consistency and improving the quality of information collected. A systematic approach would be
taken for providing care based on the clinical presentations of the patient. Vitals signs enable a
nurse to understand the needs of patient care. These are therefore to be recorded properly. A
checklist would be used for ensuring that all aspects of assessment are covered. Communication
with the patient while assessment would b based on therapeutic relationships so that the maximal
information is extracted from the patient. Good nursing record keeping allows a nurse to identify
problems that have arisen and the action taken to rectify them.
5
References
Blais, K., 2015. Professional nursing practice: Concepts and perspectives. Pearson.
Brown, D., Edwards, H., Seaton, L. and Buckley, T., 2017. Lewis's Medical-Surgical Nursing:
Assessment and Management of Clinical Problems. Elsevier Health Sciences.
Butcher, H.K., Bulechek, G.M., Dochterman, J.M.M. and Wagner, C., 2018. Nursing Interventions
classification (NIC)-E-Book. Elsevier Health Sciences.
Chow, C.K., Redfern, J., Hillis, G.S., Thakkar, J., Santo, K., Hackett, M.L., Jan, S., Graves, N., de
Keizer, L., Barry, T. and Bompoint, S., 2015. Effect of lifestyle-focused text messaging on risk factor
modification in patients with coronary heart disease: a randomized clinical trial. Jama, 314(12),
pp.1255-1263.
Giger, J.N., 2016. Transcultural Nursing-E-Book: Assessment and Intervention. Elsevier Health
Sciences.
Holley, K., MacNabb, C.M., Georgiadis, P., Minasyan, H., Shukla, A. and Mathews, D., 2016.
Monitoring minute ventilation versus respiratory rate to measure the adequacy of ventilation in
patients undergoing upper endoscopic procedures. Journal of clinical monitoring and
computing, 30(1), pp.33-39.
Knobel-Dail, R.B., Holditch-Davis, D., Sloane, R., Guenther, B.D. and Katz, L.M., 2017. Body
temperature in premature infants during the first week of life: Exploration using infrared thermal
imaging. Journal of thermal biology, 69, pp.118-123.
Lavin, M.A., Harper, E. and Barr, N., 2015. Health information technology, patient safety, and
professional nursing care documentation in acute care settings. Online J Issues Nurs, 20(6).
Lewis, S.L., Bucher, L., Heitkemper, M.M., Harding, M.M., Kwong, J. and Roberts, D.,
2016. Medical-Surgical Nursing-E-Book: Assessment and Management of Clinical Problems, Single
Volume. Elsevier Health Sciences.
Peng, M., Chen, G., Tange, K., Campbell, N., Smith, E., Faris, P. and Quan, H., 2017. Midlife and
late-life blood pressure and vascular dementia: a population based observational study. International
Journal for Population Data Science, 1(1).
Schroeder, R. and Voss, A., 2017. Age and Gender Dependency of Complexity Measures of Short-
Term Heart Rate Time Series. In Complexity and Nonlinearity in Cardiovascular Signals (pp. 469-
502). Springer, Cham.
Tavernier, B. and Jeanne, M., 2014. Heart Rate Variability. In Monitoring Technologies in Acute
Care Environments (pp. 109-115). Springer, New York, NY.
6
Blais, K., 2015. Professional nursing practice: Concepts and perspectives. Pearson.
Brown, D., Edwards, H., Seaton, L. and Buckley, T., 2017. Lewis's Medical-Surgical Nursing:
Assessment and Management of Clinical Problems. Elsevier Health Sciences.
Butcher, H.K., Bulechek, G.M., Dochterman, J.M.M. and Wagner, C., 2018. Nursing Interventions
classification (NIC)-E-Book. Elsevier Health Sciences.
Chow, C.K., Redfern, J., Hillis, G.S., Thakkar, J., Santo, K., Hackett, M.L., Jan, S., Graves, N., de
Keizer, L., Barry, T. and Bompoint, S., 2015. Effect of lifestyle-focused text messaging on risk factor
modification in patients with coronary heart disease: a randomized clinical trial. Jama, 314(12),
pp.1255-1263.
Giger, J.N., 2016. Transcultural Nursing-E-Book: Assessment and Intervention. Elsevier Health
Sciences.
Holley, K., MacNabb, C.M., Georgiadis, P., Minasyan, H., Shukla, A. and Mathews, D., 2016.
Monitoring minute ventilation versus respiratory rate to measure the adequacy of ventilation in
patients undergoing upper endoscopic procedures. Journal of clinical monitoring and
computing, 30(1), pp.33-39.
Knobel-Dail, R.B., Holditch-Davis, D., Sloane, R., Guenther, B.D. and Katz, L.M., 2017. Body
temperature in premature infants during the first week of life: Exploration using infrared thermal
imaging. Journal of thermal biology, 69, pp.118-123.
Lavin, M.A., Harper, E. and Barr, N., 2015. Health information technology, patient safety, and
professional nursing care documentation in acute care settings. Online J Issues Nurs, 20(6).
Lewis, S.L., Bucher, L., Heitkemper, M.M., Harding, M.M., Kwong, J. and Roberts, D.,
2016. Medical-Surgical Nursing-E-Book: Assessment and Management of Clinical Problems, Single
Volume. Elsevier Health Sciences.
Peng, M., Chen, G., Tange, K., Campbell, N., Smith, E., Faris, P. and Quan, H., 2017. Midlife and
late-life blood pressure and vascular dementia: a population based observational study. International
Journal for Population Data Science, 1(1).
Schroeder, R. and Voss, A., 2017. Age and Gender Dependency of Complexity Measures of Short-
Term Heart Rate Time Series. In Complexity and Nonlinearity in Cardiovascular Signals (pp. 469-
502). Springer, Cham.
Tavernier, B. and Jeanne, M., 2014. Heart Rate Variability. In Monitoring Technologies in Acute
Care Environments (pp. 109-115). Springer, New York, NY.
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 6
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





