Clinical Reasoning Cycle and Vital Signs Measurement
VerifiedAdded on 2023/06/13
|7
|2033
|138
AI Summary
This article discusses the importance of clinical reasoning cycle and vital signs measurement in nursing practice. It includes a case study and a table on vital signs measurement. It also identifies errors in vital signs measurement and the importance of accurate documentation. The article is relevant to nursing students and professionals.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Clinical reasoning
Student Name:
Student Number:
Tutor Name:
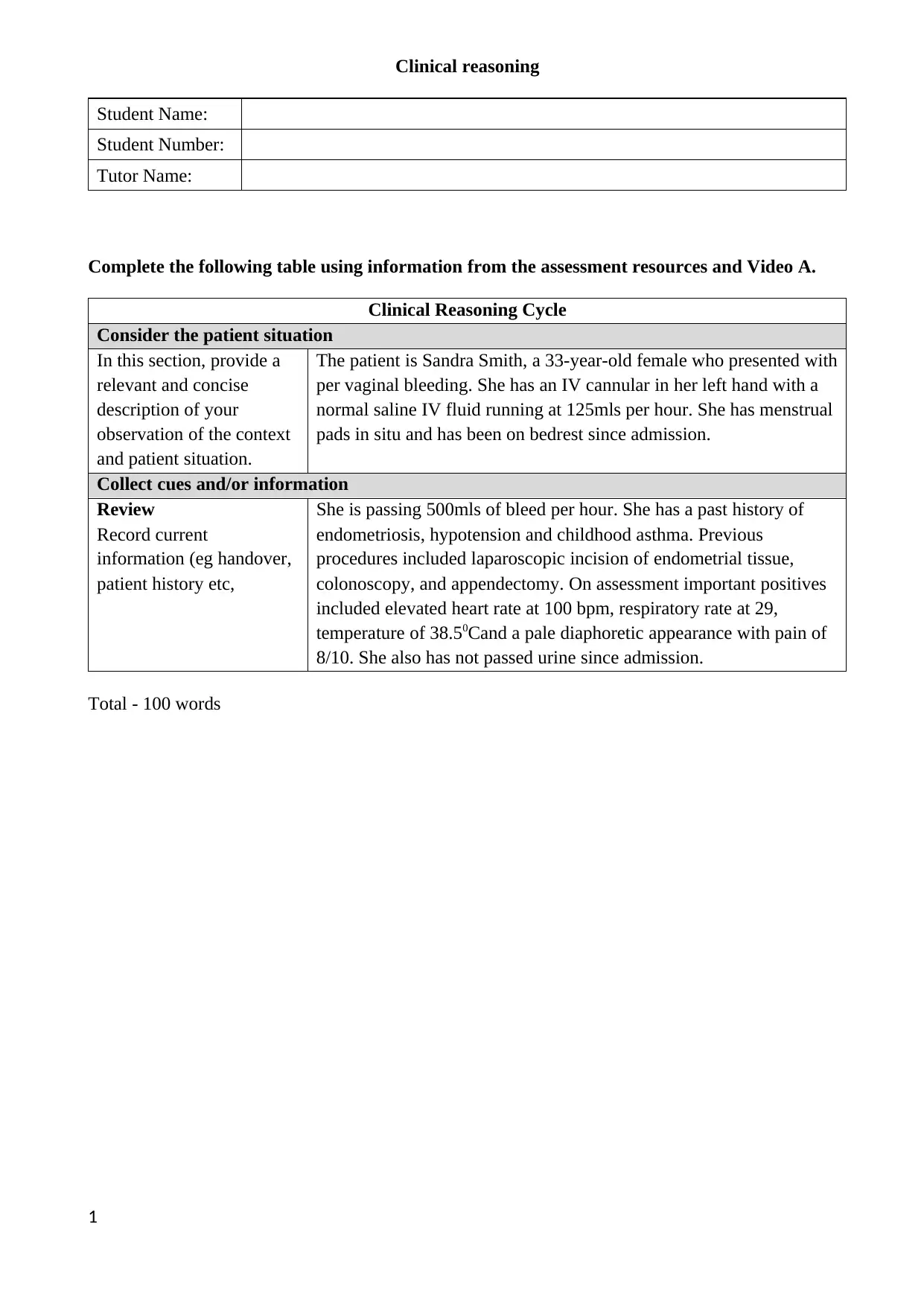
Complete the following table using information from the assessment resources and Video A.
Clinical Reasoning Cycle
Consider the patient situation
In this section, provide a
relevant and concise
description of your
observation of the context
and patient situation.
The patient is Sandra Smith, a 33-year-old female who presented with
per vaginal bleeding. She has an IV cannular in her left hand with a
normal saline IV fluid running at 125mls per hour. She has menstrual
pads in situ and has been on bedrest since admission.
Collect cues and/or information
Review
Record current
information (eg handover,
patient history etc,
She is passing 500mls of bleed per hour. She has a past history of
endometriosis, hypotension and childhood asthma. Previous
procedures included laparoscopic incision of endometrial tissue,
colonoscopy, and appendectomy. On assessment important positives
included elevated heart rate at 100 bpm, respiratory rate at 29,
temperature of 38.50Cand a pale diaphoretic appearance with pain of
8/10. She also has not passed urine since admission.
Total - 100 words
1
Student Name:
Student Number:
Tutor Name:
Complete the following table using information from the assessment resources and Video A.
Clinical Reasoning Cycle
Consider the patient situation
In this section, provide a
relevant and concise
description of your
observation of the context
and patient situation.
The patient is Sandra Smith, a 33-year-old female who presented with
per vaginal bleeding. She has an IV cannular in her left hand with a
normal saline IV fluid running at 125mls per hour. She has menstrual
pads in situ and has been on bedrest since admission.
Collect cues and/or information
Review
Record current
information (eg handover,
patient history etc,
She is passing 500mls of bleed per hour. She has a past history of
endometriosis, hypotension and childhood asthma. Previous
procedures included laparoscopic incision of endometrial tissue,
colonoscopy, and appendectomy. On assessment important positives
included elevated heart rate at 100 bpm, respiratory rate at 29,
temperature of 38.50Cand a pale diaphoretic appearance with pain of
8/10. She also has not passed urine since admission.
Total - 100 words
1
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
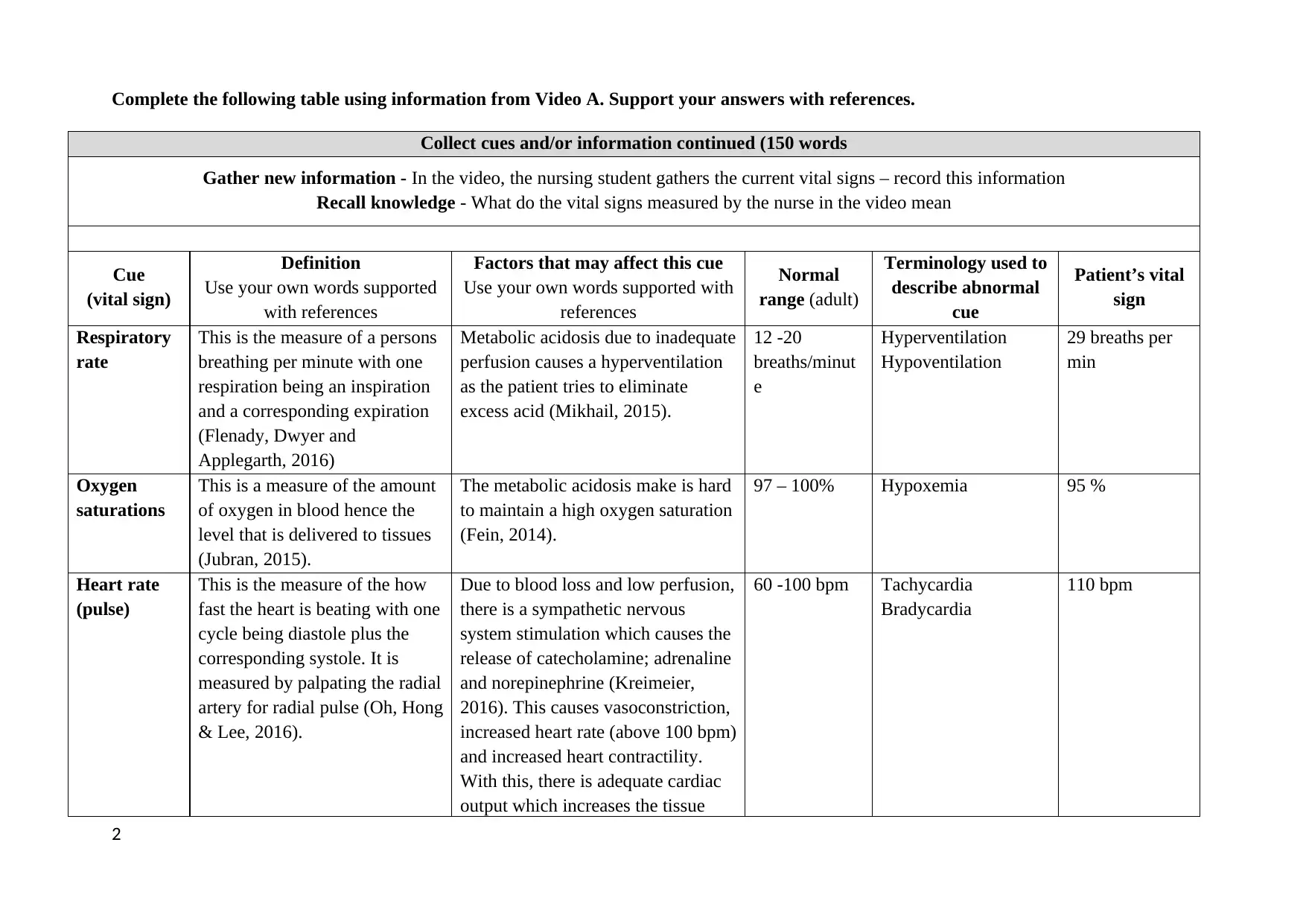
Complete the following table using information from Video A. Support your answers with references.
Collect cues and/or information continued (150 words
Gather new information - In the video, the nursing student gathers the current vital signs – record this information
Recall knowledge - What do the vital signs measured by the nurse in the video mean
Cue
(vital sign)
Definition
Use your own words supported
with references
Factors that may affect this cue
Use your own words supported with
references
Normal
range (adult)
Terminology used to
describe abnormal
cue
Patient’s vital
sign
Respiratory
rate
This is the measure of a persons
breathing per minute with one
respiration being an inspiration
and a corresponding expiration
(Flenady, Dwyer and
Applegarth, 2016)
Metabolic acidosis due to inadequate
perfusion causes a hyperventilation
as the patient tries to eliminate
excess acid (Mikhail, 2015).
12 -20
breaths/minut
e
Hyperventilation
Hypoventilation
29 breaths per
min
Oxygen
saturations
This is a measure of the amount
of oxygen in blood hence the
level that is delivered to tissues
(Jubran, 2015).
The metabolic acidosis make is hard
to maintain a high oxygen saturation
(Fein, 2014).
97 – 100% Hypoxemia 95 %
Heart rate
(pulse)
This is the measure of the how
fast the heart is beating with one
cycle being diastole plus the
corresponding systole. It is
measured by palpating the radial
artery for radial pulse (Oh, Hong
& Lee, 2016).
Due to blood loss and low perfusion,
there is a sympathetic nervous
system stimulation which causes the
release of catecholamine; adrenaline
and norepinephrine (Kreimeier,
2016). This causes vasoconstriction,
increased heart rate (above 100 bpm)
and increased heart contractility.
With this, there is adequate cardiac
output which increases the tissue
60 -100 bpm Tachycardia
Bradycardia
110 bpm
2
Collect cues and/or information continued (150 words
Gather new information - In the video, the nursing student gathers the current vital signs – record this information
Recall knowledge - What do the vital signs measured by the nurse in the video mean
Cue
(vital sign)
Definition
Use your own words supported
with references
Factors that may affect this cue
Use your own words supported with
references
Normal
range (adult)
Terminology used to
describe abnormal
cue
Patient’s vital
sign
Respiratory
rate
This is the measure of a persons
breathing per minute with one
respiration being an inspiration
and a corresponding expiration
(Flenady, Dwyer and
Applegarth, 2016)
Metabolic acidosis due to inadequate
perfusion causes a hyperventilation
as the patient tries to eliminate
excess acid (Mikhail, 2015).
12 -20
breaths/minut
e
Hyperventilation
Hypoventilation
29 breaths per
min
Oxygen
saturations
This is a measure of the amount
of oxygen in blood hence the
level that is delivered to tissues
(Jubran, 2015).
The metabolic acidosis make is hard
to maintain a high oxygen saturation
(Fein, 2014).
97 – 100% Hypoxemia 95 %
Heart rate
(pulse)
This is the measure of the how
fast the heart is beating with one
cycle being diastole plus the
corresponding systole. It is
measured by palpating the radial
artery for radial pulse (Oh, Hong
& Lee, 2016).
Due to blood loss and low perfusion,
there is a sympathetic nervous
system stimulation which causes the
release of catecholamine; adrenaline
and norepinephrine (Kreimeier,
2016). This causes vasoconstriction,
increased heart rate (above 100 bpm)
and increased heart contractility.
With this, there is adequate cardiac
output which increases the tissue
60 -100 bpm Tachycardia
Bradycardia
110 bpm
2
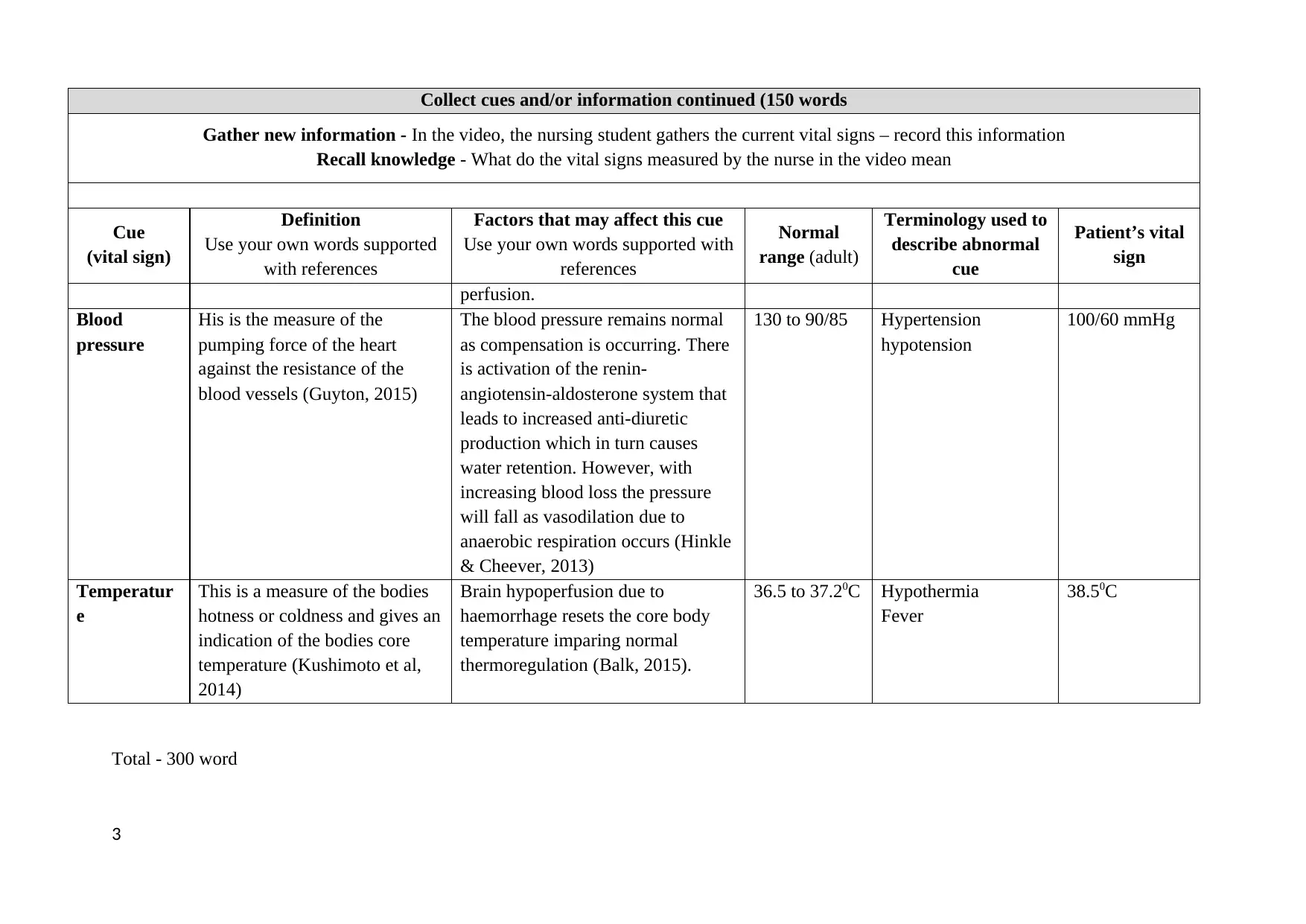
Collect cues and/or information continued (150 words
Gather new information - In the video, the nursing student gathers the current vital signs – record this information
Recall knowledge - What do the vital signs measured by the nurse in the video mean
Cue
(vital sign)
Definition
Use your own words supported
with references
Factors that may affect this cue
Use your own words supported with
references
Normal
range (adult)
Terminology used to
describe abnormal
cue
Patient’s vital
sign
perfusion.
Blood
pressure
His is the measure of the
pumping force of the heart
against the resistance of the
blood vessels (Guyton, 2015)
The blood pressure remains normal
as compensation is occurring. There
is activation of the renin-
angiotensin-aldosterone system that
leads to increased anti-diuretic
production which in turn causes
water retention. However, with
increasing blood loss the pressure
will fall as vasodilation due to
anaerobic respiration occurs (Hinkle
& Cheever, 2013)
130 to 90/85 Hypertension
hypotension
100/60 mmHg
Temperatur
e
This is a measure of the bodies
hotness or coldness and gives an
indication of the bodies core
temperature (Kushimoto et al,
2014)
Brain hypoperfusion due to
haemorrhage resets the core body
temperature imparing normal
thermoregulation (Balk, 2015).
36.5 to 37.20C Hypothermia
Fever
38.50C
Total - 300 word
3
Gather new information - In the video, the nursing student gathers the current vital signs – record this information
Recall knowledge - What do the vital signs measured by the nurse in the video mean
Cue
(vital sign)
Definition
Use your own words supported
with references
Factors that may affect this cue
Use your own words supported with
references
Normal
range (adult)
Terminology used to
describe abnormal
cue
Patient’s vital
sign
perfusion.
Blood
pressure
His is the measure of the
pumping force of the heart
against the resistance of the
blood vessels (Guyton, 2015)
The blood pressure remains normal
as compensation is occurring. There
is activation of the renin-
angiotensin-aldosterone system that
leads to increased anti-diuretic
production which in turn causes
water retention. However, with
increasing blood loss the pressure
will fall as vasodilation due to
anaerobic respiration occurs (Hinkle
& Cheever, 2013)
130 to 90/85 Hypertension
hypotension
100/60 mmHg
Temperatur
e
This is a measure of the bodies
hotness or coldness and gives an
indication of the bodies core
temperature (Kushimoto et al,
2014)
Brain hypoperfusion due to
haemorrhage resets the core body
temperature imparing normal
thermoregulation (Balk, 2015).
36.5 to 37.20C Hypothermia
Fever
38.50C
Total - 300 word
3

Critical thinking questions
Assessment is a key component of nursing practice, required for planning and provision of person
centred care. The Nursing and Midwifery Board of Australia (NMBA) Registered Nurse Standards
for Practice (2016) consist of seven standards and Standard 4 - Comprehensively Conducts
Assessments states:
“RNs accurately conduct comprehensive and systematic assessments. They analyse
information and data and communicate outcomes as the basis for practice”.
Identify four (4) errors made by the nursing student in Video B and describe how these errors may
contribute to inaccurate measuring and recording of patient vital signs (provide references) (50 words
each - 200 words)
Error 1 During blood pressure measurement, the student placed the blood pressure cuff below the
cubital fossa, at the upper forearm instead of the required position just above the cubital
fossa. This error leads to overestimation, underestimation or even guessing of values since
the correct sounds cannot be heard correctly (Handler, 2009).
Error 2 During pulse rate measurement the thumb was used to measure which is incorrect. The
thumb having its own pulsation interferers with the pulse being measured making the
reading inaccurate (Glynn and Drake, 2014).
Error 3 The method of measuring respiratory rate was incorrect as she made the patient aware of
the process. The awareness of breathing by the patient makes the reading inaccurate
compared to if the rate was counted while the patient is un aware (Glynn and Drake, 2014)
Error 4 Inappropriate documentation protocol as the student did not record her results after every
measurement but waited till the end of the assessment to do so. This is not standard
practice as she could forget the correct readings and instead document incorrect figures
(Fuller, Fox, Lake, & Crawford, 2018).
Outline the importance of accurate documentation and how it relates to Standard 4 of the Registered
Nurse Standards for Practice (2016) (provide references) (200 words)
The standard 4 provides for comprehensive assessment to guide decisions. Inappropriate
documentation of assessments will impair this principle. If an assessment is done but not
documented accurately, it renders the assessment inaccurate and an inaccurate assessment should
not be used to inform nursing practice (Stevens & Pickering, 2010). The assessment won’t be
holistic, relevant or accurate (Collins et al, 2013). As a general rule in nursing, something not
documented is considered not done. Good documentation is also crucial for clinical
communication. Working in partnership with others to assess, prioritize and manage patients is
required by the standards of practice no 4. This involves handover reports, patient information,
previous assessment and results. This ensure continuity of care without loss of information
(Stevens & Pickering, 2010). Another requirement of the standard is the assessment of resources
available to inform planning. This involves accurate documentation of all available resources, the
management of this resources and their use.
4
Assessment is a key component of nursing practice, required for planning and provision of person
centred care. The Nursing and Midwifery Board of Australia (NMBA) Registered Nurse Standards
for Practice (2016) consist of seven standards and Standard 4 - Comprehensively Conducts
Assessments states:
“RNs accurately conduct comprehensive and systematic assessments. They analyse
information and data and communicate outcomes as the basis for practice”.
Identify four (4) errors made by the nursing student in Video B and describe how these errors may
contribute to inaccurate measuring and recording of patient vital signs (provide references) (50 words
each - 200 words)
Error 1 During blood pressure measurement, the student placed the blood pressure cuff below the
cubital fossa, at the upper forearm instead of the required position just above the cubital
fossa. This error leads to overestimation, underestimation or even guessing of values since
the correct sounds cannot be heard correctly (Handler, 2009).
Error 2 During pulse rate measurement the thumb was used to measure which is incorrect. The
thumb having its own pulsation interferers with the pulse being measured making the
reading inaccurate (Glynn and Drake, 2014).
Error 3 The method of measuring respiratory rate was incorrect as she made the patient aware of
the process. The awareness of breathing by the patient makes the reading inaccurate
compared to if the rate was counted while the patient is un aware (Glynn and Drake, 2014)
Error 4 Inappropriate documentation protocol as the student did not record her results after every
measurement but waited till the end of the assessment to do so. This is not standard
practice as she could forget the correct readings and instead document incorrect figures
(Fuller, Fox, Lake, & Crawford, 2018).
Outline the importance of accurate documentation and how it relates to Standard 4 of the Registered
Nurse Standards for Practice (2016) (provide references) (200 words)
The standard 4 provides for comprehensive assessment to guide decisions. Inappropriate
documentation of assessments will impair this principle. If an assessment is done but not
documented accurately, it renders the assessment inaccurate and an inaccurate assessment should
not be used to inform nursing practice (Stevens & Pickering, 2010). The assessment won’t be
holistic, relevant or accurate (Collins et al, 2013). As a general rule in nursing, something not
documented is considered not done. Good documentation is also crucial for clinical
communication. Working in partnership with others to assess, prioritize and manage patients is
required by the standards of practice no 4. This involves handover reports, patient information,
previous assessment and results. This ensure continuity of care without loss of information
(Stevens & Pickering, 2010). Another requirement of the standard is the assessment of resources
available to inform planning. This involves accurate documentation of all available resources, the
management of this resources and their use.
4
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

What have you learned from this assessment? How will it inform your clinical practice? (200 words)
The lessons learned in this assessment are numerous. The first important lesson is the use of the
clinical reasoning cycle in the approach and management of a patient. This systematic approach as
used in this assessment is more holistic, appropriate and simple to follow. The cycle follows eight
simple steps that if applied to different clinical scenarios help in the management of patients. The
second lesson is the importance of vital signs measurement in the assessment of patients, the
identification of normal and abnormal vitals, and how errors in the measurement can greatly affect
these readings. From this, good clinical skills in the measurement of vital signs need to be learned
or improved to provide quality measurements. Also, the importance of vital signs will not be
underestimated. The third lesson is the importance of accurate documentation in provision of
quality nursing care and meeting nursing standards of practice. With this information,
implementation of good, concise and regular documentation shall be a priority in the clinical
setting. The final lesson is the use of evidence-based research in clinical practice and the
importance of evidence-based resources in clinical nursing. This will help inform my clinical
reasoning in the clinical area.
5
The lessons learned in this assessment are numerous. The first important lesson is the use of the
clinical reasoning cycle in the approach and management of a patient. This systematic approach as
used in this assessment is more holistic, appropriate and simple to follow. The cycle follows eight
simple steps that if applied to different clinical scenarios help in the management of patients. The
second lesson is the importance of vital signs measurement in the assessment of patients, the
identification of normal and abnormal vitals, and how errors in the measurement can greatly affect
these readings. From this, good clinical skills in the measurement of vital signs need to be learned
or improved to provide quality measurements. Also, the importance of vital signs will not be
underestimated. The third lesson is the importance of accurate documentation in provision of
quality nursing care and meeting nursing standards of practice. With this information,
implementation of good, concise and regular documentation shall be a priority in the clinical
setting. The final lesson is the use of evidence-based research in clinical practice and the
importance of evidence-based resources in clinical nursing. This will help inform my clinical
reasoning in the clinical area.
5
References
Balk, A., (2015). Pathogenesis and management of multiple organ dysfunctions or failure in severe
hypovolemia and hypovolemic shock. Critical Care Clinics, 16(2), 337–351
Collins, S. A., Cato, K., Albers, D., Scott, K., Stetson, P. D., Bakken, S., & Vawdrey, D. K. (2013).
Relationship Between Nursing Documentation and Patients’ Mortality, American Association
of Critical-Care Nurses, 22(4), 306-313.
Fein, A. M., (2014). Acute lung injury and acute respiratory distress syndrome in sepsis and septic
shock. Critical Care Clinics, 16(2), 289–313.
Flenady, T., Dwyer, T., & Applegarth, J. Accurate respiratory rates count: So should you!
Australasian Emergency Nursing Journal, 20(1), 45-47.
Fuller, T., Fox, B., Lake, D., & Crawford, K. (2018). Improving real-time vital signs documentation.
Nursing Management, 49(1), 28-33.
Glynn, M. & Drake, W. (2014). Hutchinson’s Clinical Methods: an integrated approach to clinical
practice. London: Elsevier.
Guyton, A. C. (2015). Textbook of Medical Physiology. (13th ed.). Philadelphia: W. B. Saunders
Handler, J. (2009). The Importance of Accurate Blood Pressure Measurement. The Permanente
Journal, 13(3), 51-54.
Hinkle, J.L, Cheever, K.H. (2013). Brunner and Saddarth’s Textbook of Medical and Surgical
Nursing, (13th ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
Jubran, A. (2015). Pulse oximetry. Critical Care, 19(1), 272.
Kreimeier, U. (2016). Pathophysiology of fluid imbalance. Critical Care, 8,2: S3–S7
Kushimoto, S., Yamanouchi, S., Endo, T., Sato, T., Nomura, R., Fujita, M. et al. (2014). Body
temperature abnormalities in non-neurological critically ill patients: a review of the literature.
Journal of Intensive Care, 2(1), 14.
6
Balk, A., (2015). Pathogenesis and management of multiple organ dysfunctions or failure in severe
hypovolemia and hypovolemic shock. Critical Care Clinics, 16(2), 337–351
Collins, S. A., Cato, K., Albers, D., Scott, K., Stetson, P. D., Bakken, S., & Vawdrey, D. K. (2013).
Relationship Between Nursing Documentation and Patients’ Mortality, American Association
of Critical-Care Nurses, 22(4), 306-313.
Fein, A. M., (2014). Acute lung injury and acute respiratory distress syndrome in sepsis and septic
shock. Critical Care Clinics, 16(2), 289–313.
Flenady, T., Dwyer, T., & Applegarth, J. Accurate respiratory rates count: So should you!
Australasian Emergency Nursing Journal, 20(1), 45-47.
Fuller, T., Fox, B., Lake, D., & Crawford, K. (2018). Improving real-time vital signs documentation.
Nursing Management, 49(1), 28-33.
Glynn, M. & Drake, W. (2014). Hutchinson’s Clinical Methods: an integrated approach to clinical
practice. London: Elsevier.
Guyton, A. C. (2015). Textbook of Medical Physiology. (13th ed.). Philadelphia: W. B. Saunders
Handler, J. (2009). The Importance of Accurate Blood Pressure Measurement. The Permanente
Journal, 13(3), 51-54.
Hinkle, J.L, Cheever, K.H. (2013). Brunner and Saddarth’s Textbook of Medical and Surgical
Nursing, (13th ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
Jubran, A. (2015). Pulse oximetry. Critical Care, 19(1), 272.
Kreimeier, U. (2016). Pathophysiology of fluid imbalance. Critical Care, 8,2: S3–S7
Kushimoto, S., Yamanouchi, S., Endo, T., Sato, T., Nomura, R., Fujita, M. et al. (2014). Body
temperature abnormalities in non-neurological critically ill patients: a review of the literature.
Journal of Intensive Care, 2(1), 14.
6
Oh, D.-J., Hong, H.-O., & Lee, B.-A. (2016). The effects of strenuous exercises on resting heart rate,
blood pressure, and maximal oxygen uptake. Journal of Exercise Rehabilitation, 12(1), 42-46
Stevens, S., & Pickering, D. (2010). Keeping good nursing records: a guide. Community Eye Health,
23(74), 44-45.
7
blood pressure, and maximal oxygen uptake. Journal of Exercise Rehabilitation, 12(1), 42-46
Stevens, S., & Pickering, D. (2010). Keeping good nursing records: a guide. Community Eye Health,
23(74), 44-45.
7
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.




