Clinical Scenario: Pathophysiology and Pharmacology
VerifiedAdded on 2020/12/29
|15
|2897
|198
Report
AI Summary
This report provides a comprehensive analysis of a clinical scenario, integrating pathophysiology, pharmacology, and psychosocial aspects within nursing practice. It begins with an introduction to pathophysiology and pharmacology, emphasizing their importance in effective healthcare. The report then addresses a series of questions related to a patient with a history of coronary heart disease, including the interpretation of ECG findings, the pathophysiology of angina and acute coronary syndrome (ACS), and the pharmacological interventions such as GTN, Diltiazem, and Pravastatin. The report also explores the use of medications like Aspirin and Ticagrelor in preventing cardiac events and discusses the controversies surrounding the use of Morphine in ACS. The analysis highlights the integration of these elements to provide effective patient care, addressing the role of nurses in assessing and managing patients with cardiac conditions.
Clinical Scenario
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
TABLE OF CONTENTS
INTRODUCTION...........................................................................................................................1
QUESTIONS ..................................................................................................................................1
QUESTION 1...............................................................................................................................1
QUESTION 2...............................................................................................................................1
QUESTION 3...............................................................................................................................3
QUESTION 4...............................................................................................................................3
QUESTION 5...............................................................................................................................4
QUESTION 6...............................................................................................................................5
QUESTION 7...............................................................................................................................6
QUESTION 8...............................................................................................................................6
CONCLUSION ...............................................................................................................................7
REFERENCES ...............................................................................................................................8
INTRODUCTION...........................................................................................................................1
QUESTIONS ..................................................................................................................................1
QUESTION 1...............................................................................................................................1
QUESTION 2...............................................................................................................................1
QUESTION 3...............................................................................................................................3
QUESTION 4...............................................................................................................................3
QUESTION 5...............................................................................................................................4
QUESTION 6...............................................................................................................................5
QUESTION 7...............................................................................................................................6
QUESTION 8...............................................................................................................................6
CONCLUSION ...............................................................................................................................7
REFERENCES ...............................................................................................................................8
INTRODUCTION
Pathophysiology is defined as the study or analysis of disordered or changed
physiological events associated with any injury or disease. The pharmacology deals with the
effects, use and action mode of drugs and have significant impact on the pathophysiology. For
providing the effective healthcare services nurses must integrate their knowledge and
understanding of pathophysiology and pharmacology (Khonsari & et.al., 2015). However, the
needs of patients cannot be analysed without relating the healthcare practices with psychosocial
elements. The report will analyse the importance and implementation of these elements in
nursing practices through clinical scenario. The evaluation and understanding of the scenario will
help to explore the role of pathophysiological, pharmacological and psychosocial aspects in
nursing practices.
QUESTIONS
QUESTION 1
Betsy has past history of coronary heart diseases and the symptoms like breath shortness
and nausea are very common symptoms of heart failure or other disturbances in working of
heart. It is quite common that most of the patients does not have any kind of chest discomfort
prior to heart attack. Thus, there is quite possibilities that within 10-15 days or one month she
may suffer from heart attack. In such situation it is important to analyse the electrical activities of
heart through electrocardiogram (ECG). The ECG report will show the abnormal rhythms and
any kind of damage to heart muscles (Xavier & et.al., 2016). The past history of patient may
cause disturbance in the normal electrical activities of the heart. In order to avoid any kind of
possibilities of heart failure or disturbances due to the present risk factors like high blood
pressure, dyspnea, coronary heart disease and nausea buddy nurse suggested for performing
ECG.
QUESTION 2
2a. Angina
Pathophysiology: Angina refers to the chest pain due to insufficient blood flow to cardio
muscles. It results due to imbalance between supply and demand of oxygen in heart. Mismatch
between myocardial oxygen needs and supply causes abnormal vasodilation and
vasoconstriction. Thus, endothelial functions and myocardial blood flow becomes impaired.
1
Pathophysiology is defined as the study or analysis of disordered or changed
physiological events associated with any injury or disease. The pharmacology deals with the
effects, use and action mode of drugs and have significant impact on the pathophysiology. For
providing the effective healthcare services nurses must integrate their knowledge and
understanding of pathophysiology and pharmacology (Khonsari & et.al., 2015). However, the
needs of patients cannot be analysed without relating the healthcare practices with psychosocial
elements. The report will analyse the importance and implementation of these elements in
nursing practices through clinical scenario. The evaluation and understanding of the scenario will
help to explore the role of pathophysiological, pharmacological and psychosocial aspects in
nursing practices.
QUESTIONS
QUESTION 1
Betsy has past history of coronary heart diseases and the symptoms like breath shortness
and nausea are very common symptoms of heart failure or other disturbances in working of
heart. It is quite common that most of the patients does not have any kind of chest discomfort
prior to heart attack. Thus, there is quite possibilities that within 10-15 days or one month she
may suffer from heart attack. In such situation it is important to analyse the electrical activities of
heart through electrocardiogram (ECG). The ECG report will show the abnormal rhythms and
any kind of damage to heart muscles (Xavier & et.al., 2016). The past history of patient may
cause disturbance in the normal electrical activities of the heart. In order to avoid any kind of
possibilities of heart failure or disturbances due to the present risk factors like high blood
pressure, dyspnea, coronary heart disease and nausea buddy nurse suggested for performing
ECG.
QUESTION 2
2a. Angina
Pathophysiology: Angina refers to the chest pain due to insufficient blood flow to cardio
muscles. It results due to imbalance between supply and demand of oxygen in heart. Mismatch
between myocardial oxygen needs and supply causes abnormal vasodilation and
vasoconstriction. Thus, endothelial functions and myocardial blood flow becomes impaired.
1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Causes: When sufficient oxygen is not supplied to heart the condition is known as ischemia. The
most common causes which decreases the blood flow is coronary artery disease (CAD). The
fatty deposit known as plaque can narrow the heart artery and thus oxygen supply is reduced.
The emotional stress, hypertension and increased physical exercises can cause stable angina
(Kane-Gill & et.al., 2015). Along with these factors the blood clots, smoking, diabetes mellitus,
obesity, hypertension and dyslipidemia can also increase the risk of angina.
Progression and outcomes: Angina may precede heart attack and thus they must be treated as
priority. Its common symptoms includes chest pain or discomfort, sweating, breathlessness. In
few cases nausea is observed with chest pain. In progressive condition blood pressure and pulse
rate may elevate. In the initial progress of Angina chest pain is experienced and gradually it may
become unstable. In such situation frequency of chest pain is increased and it may also occurs in
rest position.
Types: Acute coronary syndromes can be classified into following categories.
Stable Angina: It is related to myocardial ischemia and is demonstrated as chest discomfort due
to particular physical activities. The symptoms abate after few minutes of abolising the activity.
Along with the exercise other precipitant of stable Angina are heavy meals, hypertension and
cold weather (Kwong & et.al., 2018).
Unstable Angina: This type of Angina worsen with time. It may occur even at resting condition
and with crescendo pattern. Unstable Angima is of changing nature and thus indicates the
impending heart failure or attack. In this type of Angina coronary flow is reduced due to platelet
aggregation. In stable Angina atheroma is protected by fibrous cap which is ruptured in unstable
type. Thus, unstable Angina can develop independently as well irrespective of the type of
activity performed.
NON-ST Segment Elevation Myocardial Infarction (Non STEMI):
It is known as intermediate ACS in which either minor coronary artery is completely
blocked or major coronary artery experiences partial obstruction. The symptoms of both STEMI
and NSTEMI are same but the damage caused by NSTEMI is less extensive.
ST Segment Elevation Myocardial Infarction (STEMI)
In STEMI coronary artery is completely blocked by the ruptured plaque which causes
great damage to heart. The ECG observations of STEMI is flat line during normal condition
while during heart attack elevations are observed (Gao & et.al., 2015).
2
most common causes which decreases the blood flow is coronary artery disease (CAD). The
fatty deposit known as plaque can narrow the heart artery and thus oxygen supply is reduced.
The emotional stress, hypertension and increased physical exercises can cause stable angina
(Kane-Gill & et.al., 2015). Along with these factors the blood clots, smoking, diabetes mellitus,
obesity, hypertension and dyslipidemia can also increase the risk of angina.
Progression and outcomes: Angina may precede heart attack and thus they must be treated as
priority. Its common symptoms includes chest pain or discomfort, sweating, breathlessness. In
few cases nausea is observed with chest pain. In progressive condition blood pressure and pulse
rate may elevate. In the initial progress of Angina chest pain is experienced and gradually it may
become unstable. In such situation frequency of chest pain is increased and it may also occurs in
rest position.
Types: Acute coronary syndromes can be classified into following categories.
Stable Angina: It is related to myocardial ischemia and is demonstrated as chest discomfort due
to particular physical activities. The symptoms abate after few minutes of abolising the activity.
Along with the exercise other precipitant of stable Angina are heavy meals, hypertension and
cold weather (Kwong & et.al., 2018).
Unstable Angina: This type of Angina worsen with time. It may occur even at resting condition
and with crescendo pattern. Unstable Angima is of changing nature and thus indicates the
impending heart failure or attack. In this type of Angina coronary flow is reduced due to platelet
aggregation. In stable Angina atheroma is protected by fibrous cap which is ruptured in unstable
type. Thus, unstable Angina can develop independently as well irrespective of the type of
activity performed.
NON-ST Segment Elevation Myocardial Infarction (Non STEMI):
It is known as intermediate ACS in which either minor coronary artery is completely
blocked or major coronary artery experiences partial obstruction. The symptoms of both STEMI
and NSTEMI are same but the damage caused by NSTEMI is less extensive.
ST Segment Elevation Myocardial Infarction (STEMI)
In STEMI coronary artery is completely blocked by the ruptured plaque which causes
great damage to heart. The ECG observations of STEMI is flat line during normal condition
while during heart attack elevations are observed (Gao & et.al., 2015).
2
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2b. Factors enhancing risk of acute coronary syndrome
Acute coronary syndrome (ACS) refers to conditions causing sudden and rapid reduction
of blood flow to heart. It causes changes in the normal functioning of heart and thus enhances
risks of heart attack. The two key factors which increases the risk of coronary syndrome in Betsy
are high blood pressure and diabetes.
Betsy has past history of hypertension and thus high blood pressure can narrow the
coronary arteries. It increases the risk of heart attack and coronary syndrome.
Diabetes mellitus type 2 is also one of the major risk factor for ACS. Betsy has its history
and changes in insulin resistance, lipid metabolism due to diabetes encourages the
development of atherosclerotic plaque which remodel the vascular wall (Deedwania &
et.al., 2008). As a result, there are high possibilities that person my develop ACS.
QUESTION 3
Rhythm: Betsy had irregular rhythms due to breathing shortness. Thus, to measure the rhythms
in interval of 6 seconds number of RR intervals are counted in rhythm strip.
Rate: When the heart rhythm is irregular then to calculate heart rate number of large squares
between QRS complex is divided by 300. Along with this method heart rate can also be
determined by number of RR interval between two tick marks and then by multiplying this
number with 10.
Presence and regularity of p waves: P waves demonstrates the SA node discharge along with
the polarisation of both atria. V1 is the best lead to observe p wave and in normal condition its
width and height must not be greater than one box. However, in case of abnormal readings its
voltage or duration are greater and indicates the enlargement of both atria.
ST segment: It refers to the initial phase of ventricle polarisation. It initiates from the S end and
terminates at starting point of T wave. This segment is isoelectric. The elevation of ST segment
0.06 seconds after J point indicates the infarction.
ECG interpretation: In the ECG of Betsy T waves are hyperacute and appears peaked. There is
1.5 mm elevation in V2 and V3. Flattening and inversion of T waves is also observed in the ECG
which confirms the ACS.
3
Acute coronary syndrome (ACS) refers to conditions causing sudden and rapid reduction
of blood flow to heart. It causes changes in the normal functioning of heart and thus enhances
risks of heart attack. The two key factors which increases the risk of coronary syndrome in Betsy
are high blood pressure and diabetes.
Betsy has past history of hypertension and thus high blood pressure can narrow the
coronary arteries. It increases the risk of heart attack and coronary syndrome.
Diabetes mellitus type 2 is also one of the major risk factor for ACS. Betsy has its history
and changes in insulin resistance, lipid metabolism due to diabetes encourages the
development of atherosclerotic plaque which remodel the vascular wall (Deedwania &
et.al., 2008). As a result, there are high possibilities that person my develop ACS.
QUESTION 3
Rhythm: Betsy had irregular rhythms due to breathing shortness. Thus, to measure the rhythms
in interval of 6 seconds number of RR intervals are counted in rhythm strip.
Rate: When the heart rhythm is irregular then to calculate heart rate number of large squares
between QRS complex is divided by 300. Along with this method heart rate can also be
determined by number of RR interval between two tick marks and then by multiplying this
number with 10.
Presence and regularity of p waves: P waves demonstrates the SA node discharge along with
the polarisation of both atria. V1 is the best lead to observe p wave and in normal condition its
width and height must not be greater than one box. However, in case of abnormal readings its
voltage or duration are greater and indicates the enlargement of both atria.
ST segment: It refers to the initial phase of ventricle polarisation. It initiates from the S end and
terminates at starting point of T wave. This segment is isoelectric. The elevation of ST segment
0.06 seconds after J point indicates the infarction.
ECG interpretation: In the ECG of Betsy T waves are hyperacute and appears peaked. There is
1.5 mm elevation in V2 and V3. Flattening and inversion of T waves is also observed in the ECG
which confirms the ACS.
3
QUESTION 4
The central findings which leads to the diagnosis of ACS are as follows:
ECG interpretation:
The abnormalities in ECG such as inversion or tenting of T waves, pathologic Q waves
and elevation or depression of ST segment helps in diagnosis of ACS. The persistent elevation in
ST segment can be very crucial in identification of ACS patients. The magnitude and number of
abnormalities in ECG outputs also indicates the specificity and sensitivity of the disease.
Serum cardiac markers:
Another critical diagnosis aid is serum cardiac markers which detects the myocardial
infarction. Creatine kinase (CK) level enhances after myocardial injury and thus it can be used
for the diagnosis purpose (Hausenloy & et.al., 2015). As it has low sensitivity, mostly
practitioners uses CK-MB ISOENZYME and CK-MB SUBFORMS which care detectable in
serum. Along with these value changes in value of MYOGLOBIN and CARDIAC TROPONINS
are also measured for the diagnosis of myocardial injury.
Prediction scores:
The ACI-TIPI score which uses seven variables such as chest pain, coronary syndrome
and other variables in the admission record for the diagnosis purpose. Though as compare to
other two findings method it has less sensitivity but use of prediction scores along with prognosis
helps in accurate diagnosis of ACS. These scores consider patient medical history as well as
clinical measurements for confirmation of ACS.
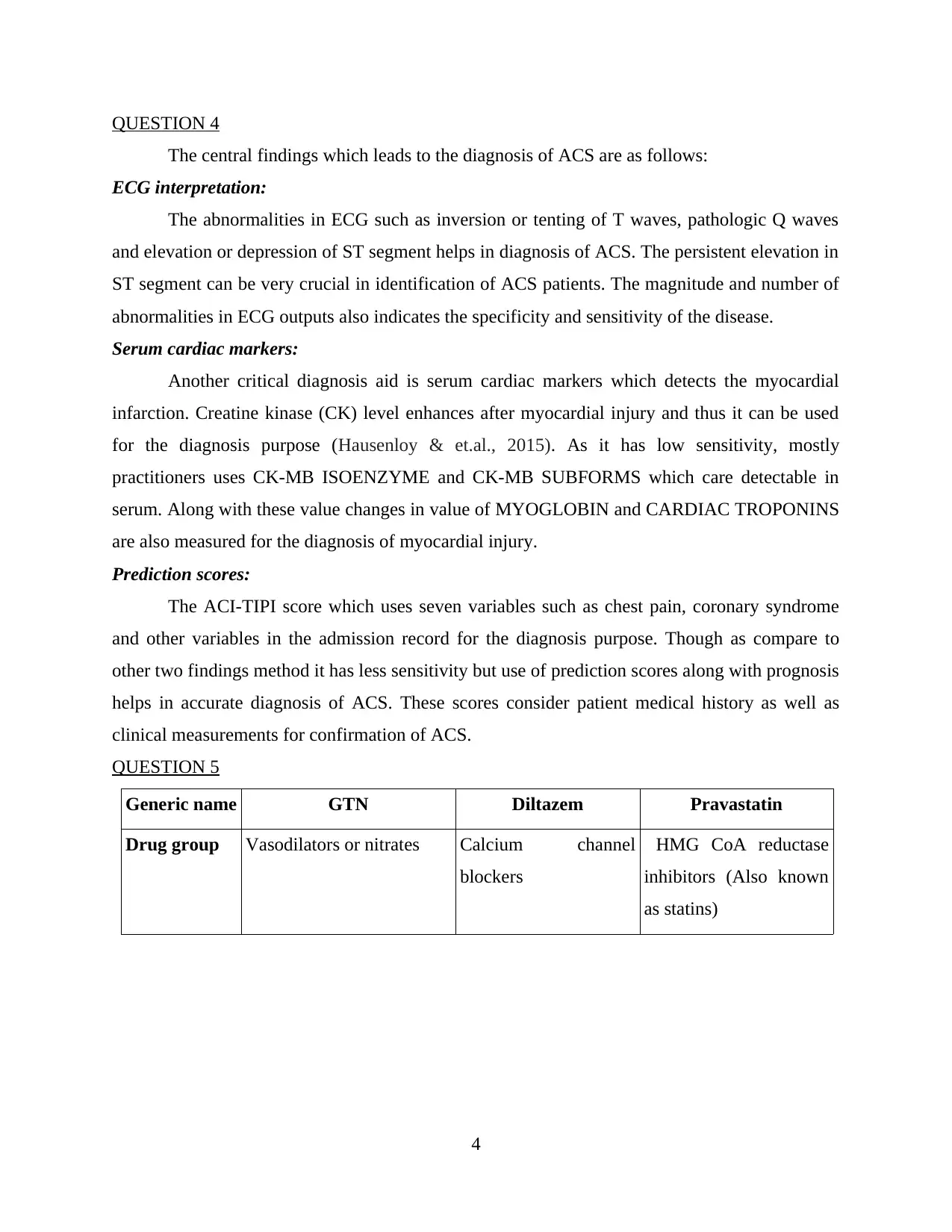
QUESTION 5
Generic name GTN Diltazem Pravastatin
Drug group Vasodilators or nitrates Calcium channel
blockers
HMG CoA reductase
inhibitors (Also known
as statins)
4
The central findings which leads to the diagnosis of ACS are as follows:
ECG interpretation:
The abnormalities in ECG such as inversion or tenting of T waves, pathologic Q waves
and elevation or depression of ST segment helps in diagnosis of ACS. The persistent elevation in
ST segment can be very crucial in identification of ACS patients. The magnitude and number of
abnormalities in ECG outputs also indicates the specificity and sensitivity of the disease.
Serum cardiac markers:
Another critical diagnosis aid is serum cardiac markers which detects the myocardial
infarction. Creatine kinase (CK) level enhances after myocardial injury and thus it can be used
for the diagnosis purpose (Hausenloy & et.al., 2015). As it has low sensitivity, mostly
practitioners uses CK-MB ISOENZYME and CK-MB SUBFORMS which care detectable in
serum. Along with these value changes in value of MYOGLOBIN and CARDIAC TROPONINS
are also measured for the diagnosis of myocardial injury.
Prediction scores:
The ACI-TIPI score which uses seven variables such as chest pain, coronary syndrome
and other variables in the admission record for the diagnosis purpose. Though as compare to
other two findings method it has less sensitivity but use of prediction scores along with prognosis
helps in accurate diagnosis of ACS. These scores consider patient medical history as well as
clinical measurements for confirmation of ACS.
QUESTION 5
Generic name GTN Diltazem Pravastatin
Drug group Vasodilators or nitrates Calcium channel
blockers
HMG CoA reductase
inhibitors (Also known
as statins)
4
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Mechanism
of action
Relaxation of vascular
smooth muscle. The
meication reduces the
vascular resistance or
ventricular filling pressure
and thus enhances cardiac
output.
It acts as calcium
channel antagonist.
The channel
deformation inhibits
extracellular calcium
influx across cell
membrane of vascular
muscles and
myocardial. The
contractile process
results in dilation of
coronary arteries and
oxygen delivery is
improved.
Pravastatin lowers
lipoprotein in 2
pathways. At first
occupy the active site of
enzyme so that action of
HMG-CoA can be
hindered. Secondly it
produces low density
lipoprotein so that
circulating cholestrol
can be reduced (Gao &
et.al., 2015).
Complication
/ side effects
Methemoglobinemi
a (MetHb) disorder
may occur in which
methemoglobin is
produced
abnormally.
It can cause
Tachycardia or
bradycardia in
which heart rate
becomes fast or
slow (Parodi &
et.al., 2015).
Hypotension
Bradycardia
(Reduced heart
rate)
Jaundice
Unusual
bleeding,
memory loss or
bruising
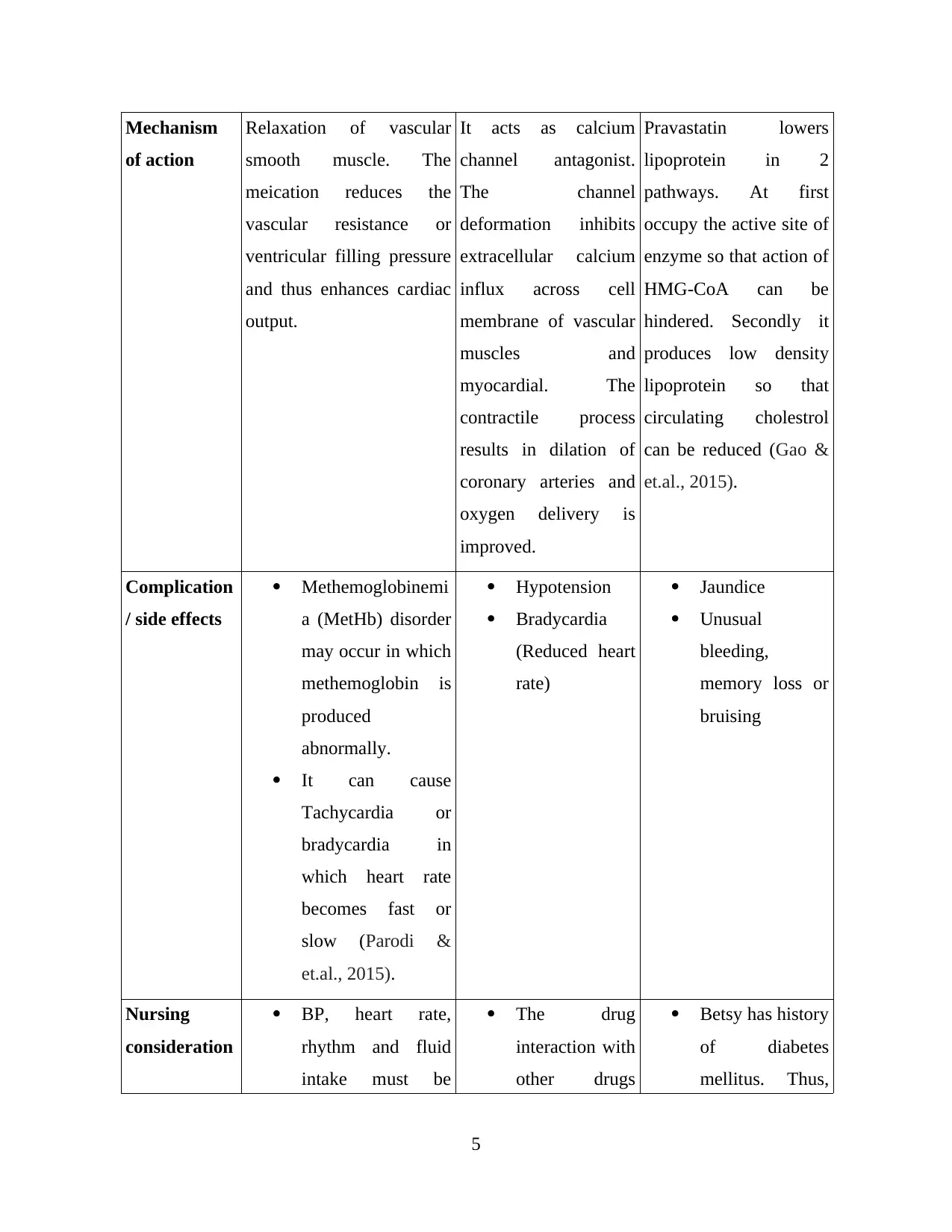
Nursing
consideration
BP, heart rate,
rhythm and fluid
intake must be
The drug
interaction with
other drugs
Betsy has history
of diabetes
mellitus. Thus,
5
of action
Relaxation of vascular
smooth muscle. The
meication reduces the
vascular resistance or
ventricular filling pressure
and thus enhances cardiac
output.
It acts as calcium
channel antagonist.
The channel
deformation inhibits
extracellular calcium
influx across cell
membrane of vascular
muscles and
myocardial. The
contractile process
results in dilation of
coronary arteries and
oxygen delivery is
improved.
Pravastatin lowers
lipoprotein in 2
pathways. At first
occupy the active site of
enzyme so that action of
HMG-CoA can be
hindered. Secondly it
produces low density
lipoprotein so that
circulating cholestrol
can be reduced (Gao &
et.al., 2015).
Complication
/ side effects
Methemoglobinemi
a (MetHb) disorder
may occur in which
methemoglobin is
produced
abnormally.
It can cause
Tachycardia or
bradycardia in
which heart rate
becomes fast or
slow (Parodi &
et.al., 2015).
Hypotension
Bradycardia
(Reduced heart
rate)
Jaundice
Unusual
bleeding,
memory loss or
bruising
Nursing
consideration
BP, heart rate,
rhythm and fluid
intake must be
The drug
interaction with
other drugs
Betsy has history
of diabetes
mellitus. Thus,
5
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
monitored carefully
to avoid precipitous
decrease in blood
pressure.
It must not be
administered with
other drugs.
must be
monitored
regularly.
During position
change nurses
must take
caution so that
orthostatic
hypotension
can be
prevented
(Zheng & et.al.,
2016).
there are chances
of renal
impairment and
thus the dosage
of pravastatin
must be
regularly
monitored and
adjusted.
Nurses must
observe liver
enzyme
elevation with
the
administration of
the drug.
QUESTION 6
Aspirin:
The medicine can lower the risk of heart attack in cardiac patients. Aspirin interfere with
the blood clotting phenomenon. The patients suffering from cardiac diseases when blood vessels
are narrowed due to fatty deposition then blood clot can easily develop and arteries can be
blocked. Aspirin reduces the platelet clumping action and thus heart attack possibilities are
lowered.
Ticagrelor: It is also one of the widely used antiplatelet agent which can prevent ACS.
Ticagrelor prevents platelet activation and signal transduction by interacting with the platelet
receptor. It is used to prevent stroke and heart attack after CABG or other heart surgeries. The
drug block platelets from sticking or making clot (Gao & et.al., 2015).
Betsy also has history of CAG the combination of drug can reduce the stent thrombosis and
ischemic risk. The combination also lowered the drug amount of aspirin without reducing the
6
to avoid precipitous
decrease in blood
pressure.
It must not be
administered with
other drugs.
must be
monitored
regularly.
During position
change nurses
must take
caution so that
orthostatic
hypotension
can be
prevented
(Zheng & et.al.,
2016).
there are chances
of renal
impairment and
thus the dosage
of pravastatin
must be
regularly
monitored and
adjusted.
Nurses must
observe liver
enzyme
elevation with
the
administration of
the drug.
QUESTION 6
Aspirin:
The medicine can lower the risk of heart attack in cardiac patients. Aspirin interfere with
the blood clotting phenomenon. The patients suffering from cardiac diseases when blood vessels
are narrowed due to fatty deposition then blood clot can easily develop and arteries can be
blocked. Aspirin reduces the platelet clumping action and thus heart attack possibilities are
lowered.
Ticagrelor: It is also one of the widely used antiplatelet agent which can prevent ACS.
Ticagrelor prevents platelet activation and signal transduction by interacting with the platelet
receptor. It is used to prevent stroke and heart attack after CABG or other heart surgeries. The
drug block platelets from sticking or making clot (Gao & et.al., 2015).
Betsy also has history of CAG the combination of drug can reduce the stent thrombosis and
ischemic risk. The combination also lowered the drug amount of aspirin without reducing the
6
platelet action. Thus, cardiovascular events are reduced and mortality can be increased by using
the drug combination instead of using only Aspirin.
QUESTION 7
Use of morphine in ACS:
Morphine treats the myocardial inarction by mitigating pain response and damage to
ischemic tissue. The medicine is primarily used for pain relief in ACS.
Controversies:
It has been observed that morphine activate sympathetic nervous system and thus cardiac
work load is increased (Bønaa & et.al., 2016).
Though medicine has beneficial hemodynamic effect during treatment of ACS but it also
reduces myocardial oxygen demand due to simulation of histamine mediated process.
The key controversy related to the drug is its addictive nature and thus its irregular
monitoring and long term usage can make people addictive to it which has harmful effect
on health of cardiac and other patients.
QUESTION 8
Depression is considered as the major risk factor in many chronic diseases. Betsy is
suffering from coronary heart disease which are long lasting and which may not be cured
completely. The complicated physical changes, painful therapies and medications can make any
individual depressed. Especially people who have mood disorders and related vulnerabilities are
more prone to depressions. Betsy is not able to perform the normal routine functions with higher
energy as performed by the others healthy individuals. For instance she may easily get tired by
physical exercises. Prolong use of medications and clinical surroundings can cause depression.
Another major factor related with the chronic diseases is that since these disorders have
minimum possibilities to be completely cure in future Betsy does not have any hope to get
completely recover in future and to live life as earlier. Thus, depression is very common in
coronary and other chronic diseases (White & et.al., 2016).
7
the drug combination instead of using only Aspirin.
QUESTION 7
Use of morphine in ACS:
Morphine treats the myocardial inarction by mitigating pain response and damage to
ischemic tissue. The medicine is primarily used for pain relief in ACS.
Controversies:
It has been observed that morphine activate sympathetic nervous system and thus cardiac
work load is increased (Bønaa & et.al., 2016).
Though medicine has beneficial hemodynamic effect during treatment of ACS but it also
reduces myocardial oxygen demand due to simulation of histamine mediated process.
The key controversy related to the drug is its addictive nature and thus its irregular
monitoring and long term usage can make people addictive to it which has harmful effect
on health of cardiac and other patients.
QUESTION 8
Depression is considered as the major risk factor in many chronic diseases. Betsy is
suffering from coronary heart disease which are long lasting and which may not be cured
completely. The complicated physical changes, painful therapies and medications can make any
individual depressed. Especially people who have mood disorders and related vulnerabilities are
more prone to depressions. Betsy is not able to perform the normal routine functions with higher
energy as performed by the others healthy individuals. For instance she may easily get tired by
physical exercises. Prolong use of medications and clinical surroundings can cause depression.
Another major factor related with the chronic diseases is that since these disorders have
minimum possibilities to be completely cure in future Betsy does not have any hope to get
completely recover in future and to live life as earlier. Thus, depression is very common in
coronary and other chronic diseases (White & et.al., 2016).
7
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

CONCLUSION
From the evaluation of the questions raised in clinical scenario it can be concluded that
for providing the safe and quality care nurses must have in-depth knowledge of pharmacology,
pathophysiology and psychological aspects of the patient.
8
From the evaluation of the questions raised in clinical scenario it can be concluded that
for providing the safe and quality care nurses must have in-depth knowledge of pharmacology,
pathophysiology and psychological aspects of the patient.
8
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
REFERENCES
Books and Journals
Bønaa, K. H. & et.al., (2016). Drug-eluting or bare-metal stents for coronary artery disease. New
England Journal of Medicine, 375(13), 1242-1252.
Gao, R. & et.al., (2015). Bioresorbable vascular scaffolds versus metallic stents in patients with
coronary artery disease: ABSORB China trial. Journal of the American College of
Cardiology, 66(21), 2298-2309.
Hausenloy, D. J. & et.al., (2015). Remote ischemic preconditioning and outcomes of cardiac
surgery. New England Journal of Medicine, 373(15), 1408-1417.
Kane-Gill, S. L. & et.al., (2015). Risk factors for acute kidney injury in older adults with critical
illness: a retrospective cohort study. American journal of kidney diseases, 65(6), 860-869.
Khonsari, S. & et.al., (2015). Effect of a reminder system using an automated short message
service on medication adherence following acute coronary syndrome. European Journal
of Cardiovascular Nursing, 14(2), 170-179.
Kwong, J. C. & et.al., (2018). Acute myocardial infarction after laboratory-confirmed influenza
infection. New England Journal of Medicine, 378(4), 345-353.
Parodi, G. & et.al., (2015). Morphine is associated with a delayed activity of oral antiplatelet
agents in patients with ST-elevation acute myocardial infarction undergoing primary
percutaneous coronary intervention. Circulation: Cardiovascular Interventions, 8(1),
e001593.
White, H. D. & et.al., (2016). Frailty is associated with worse outcomes in non-ST-segment
elevation acute coronary syndromes: Insights from the TaRgeted platelet Inhibition to
cLarify the Optimal strateGy to medicallY manage Acute Coronary Syndromes
(TRILOGY ACS) trial. European Heart Journal: Acute Cardiovascular Care, 5(3), 231-
242.
Xavier, D. & et.al., (2016). Community health worker-based intervention for adherence to drugs
and lifestyle change after acute coronary syndrome: a multicentre, open, randomised
controlled trial. The Lancet Diabetes & Endocrinology, 4(3), 244-253.
Zheng, Z. & et.al., (2016). Perioperative rosuvastatin in cardiac surgery. New England Journal of
Medicine, 374(18), 1744-1753.
Online
9
Books and Journals
Bønaa, K. H. & et.al., (2016). Drug-eluting or bare-metal stents for coronary artery disease. New
England Journal of Medicine, 375(13), 1242-1252.
Gao, R. & et.al., (2015). Bioresorbable vascular scaffolds versus metallic stents in patients with
coronary artery disease: ABSORB China trial. Journal of the American College of
Cardiology, 66(21), 2298-2309.
Hausenloy, D. J. & et.al., (2015). Remote ischemic preconditioning and outcomes of cardiac
surgery. New England Journal of Medicine, 373(15), 1408-1417.
Kane-Gill, S. L. & et.al., (2015). Risk factors for acute kidney injury in older adults with critical
illness: a retrospective cohort study. American journal of kidney diseases, 65(6), 860-869.
Khonsari, S. & et.al., (2015). Effect of a reminder system using an automated short message
service on medication adherence following acute coronary syndrome. European Journal
of Cardiovascular Nursing, 14(2), 170-179.
Kwong, J. C. & et.al., (2018). Acute myocardial infarction after laboratory-confirmed influenza
infection. New England Journal of Medicine, 378(4), 345-353.
Parodi, G. & et.al., (2015). Morphine is associated with a delayed activity of oral antiplatelet
agents in patients with ST-elevation acute myocardial infarction undergoing primary
percutaneous coronary intervention. Circulation: Cardiovascular Interventions, 8(1),
e001593.
White, H. D. & et.al., (2016). Frailty is associated with worse outcomes in non-ST-segment
elevation acute coronary syndromes: Insights from the TaRgeted platelet Inhibition to
cLarify the Optimal strateGy to medicallY manage Acute Coronary Syndromes
(TRILOGY ACS) trial. European Heart Journal: Acute Cardiovascular Care, 5(3), 231-
242.
Xavier, D. & et.al., (2016). Community health worker-based intervention for adherence to drugs
and lifestyle change after acute coronary syndrome: a multicentre, open, randomised
controlled trial. The Lancet Diabetes & Endocrinology, 4(3), 244-253.
Zheng, Z. & et.al., (2016). Perioperative rosuvastatin in cardiac surgery. New England Journal of
Medicine, 374(18), 1744-1753.
Online
9
Deedwania., P., & et.al., (2008). Hyperglycemia and Acute Coronary Syndrome. [Online].
Accessed through
<https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.107.188629>
10
Accessed through
<https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.107.188629>
10
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





